Abstract
Exposure to secondhand smoke (SHS) can result in several adverse health consequences. SHS concentrations in vehicles can significantly exceed levels present in other enclosed spaces. Years after the adoption of smoke-free car laws, this study examined the prevalence of exposure to SHS in vehicles among adolescents. Data were utilized from the 2016–2017 Canadian Student Tobacco, Alcohol and Drugs Survey (n = 48,444). The prevalence of exposure to SHS in cars was estimated by grade level and demographic characteristics. The results showed a gradient by grade level in exposure to SHS with students in upper-grade levels reporting a higher prevalence of SHS in cars. SHS varied by province, with the lowest rate found in British Columbia (15.6%) and the highest in Saskatchewan (36.9%). The provinces with laws that extend protections to older children also had high rates of SHS exposure among students in upper-grade levels. Students exposed to SHS were more likely to engage in risky behaviors, including the use of marijuana, alcohol, cigarettes, and e-cigarettes. Despite laws prohibiting smoking in vehicles carrying children, SHS prevalence remains high. While enforcement of these laws may be challenging, persuasion campaigns highlighting that children are especially vulnerable to the health risks of SHS may be beneficial.
Keywords: Secondhand smoke exposure, Environmental tobacco smoke, Tobacco smoke concentrations, Adolescents, Smoke-free car laws
Highlights
-
•
Results showed a grade gradient in exposure to SHS in cars.
-
•
Students in upper-grades showed higher rates of SHS exposure.
-
•
Students exposed to SHS were more likely to engage in risky behaviors.
-
•
Areas with laws covering older children also had high SHS rates among upper-grades.
-
•
Despite laws prohibiting smoking in cars carrying children, SHS rates appear high.
1. Introduction
Tobacco use causes 7 million deaths each year, making it the leading cause of preventable death worldwide (World Health Organization, 2017). In Canada, tobacco use was the leading cause of all substance use attributable deaths in 2014, accounting for 47,562 deaths, more than double the next leading substance (Canadian Substance Use Costs and Harms Scientific Working Group, 2018). Tobacco smoke is recognized as a Group 1 carcinogen by the International Agency for Research on Cancer (IARC Working Group on the Evaluation of Carcinogenic Risks to Humans, 2012; World Health Organization & International Agency for Research on Cancer, 2004), and even the negative health effects of exposure to secondhand smoking (SHS) have been found to be a factor in >800 deaths annually in Canada (Rehm, Gnam, Popova, et al., 2007). The presence of SHS can lead to several adverse health consequences, including coronary heart disease, stroke, and lung cancer (U.S. Department of Health and Human Services, 2014). Infants and children are more vulnerable to the adverse health effects of SHS, as they have no control over the exposure from their caregivers, have immature immune systems, and have higher respiratory rates (Action on Smoking & Health, n.d.). Some of the damaging effects of childhood exposure to SHS include respiratory tract infection, asthma, cancer, and sudden infant death syndrome (Cheraghi & Salvi, 2009; Dybing & Sanner, 1999; Håberg, Stigum, Nystad, & Nafstad, 2007; Lam, Leung, & Ho, 2001; Olivo-Marston, Yang, Mechanic, et al., 2009). SHS remains a significant public health issue, with an estimated 40% of children globally exposed to SHS in 2004 (Öberg, Jaakkola, Woodward, Peruga, & Prüss-Ustün, 2011).
Although exposure to SHS can occur in a myriad of locations, including bars, restaurants, homes, vehicles are one of the top sources of exposure to SHS among children (U.S. Department of Health and Human Services, 2006). This is troubling because SHS concentrations in vehicles have been found to significantly exceed levels present in other enclosed spaces such as bars, restaurants, and casinos (Northcross, Trinh, Kim, et al., 2014). One study found that nicotine concentrations in the air were higher in vehicles compared to other venues in the 24-hours after smoking had ceased (Jones, Navas-Acien, Yuan, & Breysse, 2009). Even with car windows down and the ventilation systems operating in attempts to clear the smoke, SHS levels may remain high (Jones et al., 2009; Sendzik, Fong, Travers, & Hyland, 2009). There is evidence linking SHS in vehicles with an increased incidence of persistent wheezing in adolescents 14 years of age (Sly, Deverell, Kusel, & Holt, 2007). In addition to the health risks, smoking in cars may act as a distraction with evidence suggesting a possible association with motor-vehicle accidents (Lam, 2002; Vafaee-Najar, Khabbazkhoob, Alidadi-Soltangholi, Asgari, & Ibrahimipour, 2011). There is no safe level of SHS exposure (Potera, 2010; Strulovici-Barel, Omberg, O'Mahony, et al., 2010; U.S. Department of Health and Human Services, 2006), and recent action in the form of smoke-free laws prohibiting smoking in vehicles carrying children has been undertaken (American Nonsmokers' Rights Foundation, n.d.; Department of Health, 2015; Department of Health and Social Care, 2017; DeRosenroll & Cunningham, 2007). Similar public smoking bans in other venues are commonplace in many jurisdictions and share the goal of reducing the health risks associated with SHS. Smoke-free laws that ban smoking in public places such as schools, bars, restaurants, and workplaces have been shown to reduce exposure to SHS (Akhtar, Currie, Currie, & Haw, 2007; Azagba, 2015; Azagba, Kennedy, & Baskerville, 2016; Dove, Dockery, & Connolly, 2010), and thus are generally considered successful.
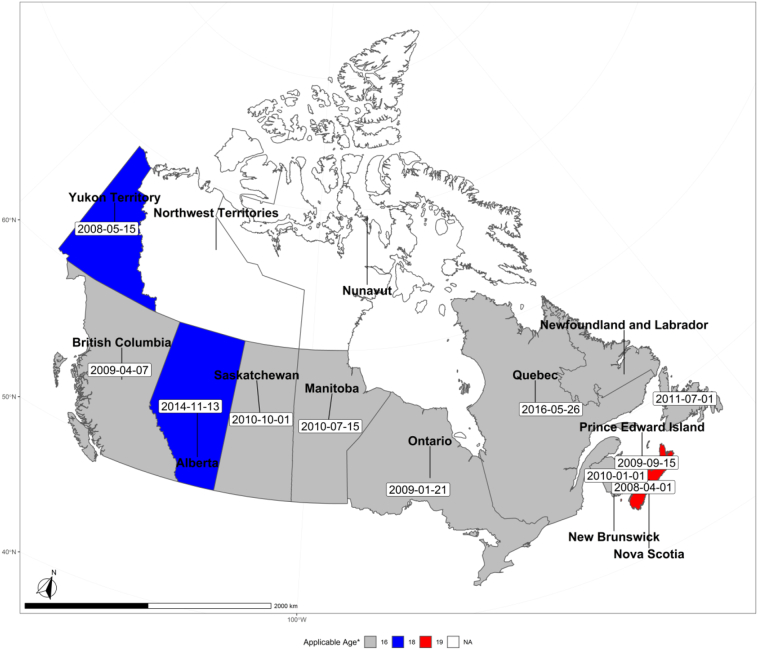
Policies banning smoking in vehicles with children have been widely implemented in many Canadian municipalities and provinces (see Fig. 1). There is strong public support for the ban on smoking in vehicles carrying children, with 74% of Canadian smokers supporting the ban (Hitchman, Fong, Zanna, Hyland, & Bansal-Travers, 2010). In 2008, Nova Scotia became the first province to adopt laws prohibiting smoking in vehicles carrying children. By 2016, all provinces (except the Northwest Territories and Nunavut) in Canada had implemented the ban (Fig. 1). This study examined the prevalence of SHS exposure in vehicles among Canadian students in Grades 7–12 in 2018, years after policy implementation. Continuous surveillance of children's exposure to SHS in vehicles is particularly important given that, at a minimum, it will provide a gauge of this policy's strength of enforcement.
Fig. 1.
Smoking restriction policy in vehicles carrying children in Canada.
*Applicable age refers to under the age (i.e., 16 means smoking is prohibited in a vehicle carrying someone under 16).
2. Method
2.1. Data
Data from the 2016–2017 Canadian Student Tobacco, Alcohol and Drugs Survey (CSTADS; formerly the Youth Smoking Survey) were used for this study. The CSTADS is a biennial, cross-sectional, school-based survey of a representative sample of Canadian students attending schools in 7 through 12 (secondary I through V in Quebec) grade and is intended to track adolescent and youth substance use behavior. The survey excluded those living on First Nations reserves, Canada's three northern Territories (i.e., Yukon, Nunavut, and Northwest Territories), and those attending special schools or schools on military bases. CSTADS uses a stratified single-stage cluster design (except the province of Quebec), with strata based on health-region smoking rate and type of school. For each province, two or three health-region smoking rate strata and two school-level strata were defined. Random selection of schools within each stratum allowed for a generalizable sample for each province.
All eligible students within selected schools were administered the survey. Research ethics boards at multiple levels approved the study (e.g., Health Canada, the University of Waterloo, institutions and school boards in each participating province). Consistent with school board requirements, parents provided permission for their child to participate in the study via active parent permission or existing information-passive permission protocols. Only students with parental permission were invited to participate on the day the survey was administered. All schools that participated in the 2016–2017 survey, except for schools in Quebec, received a $100 honorarium. Students were not rewarded and could stop answering the survey at any time. The 2016–2017 CSTADS was implemented in schools between October 2016 and June 2017. The province of New Brunswick declined participation in the 2016–2017 cycle. A total of 52,103 students in Grades 7 through 12 completed the survey, corresponding to 76% of the eligible student population in participating schools.
2.2. Measures
The outcome variable was SHS exposure in a vehicle during the past 30 days, which was derived from the survey question “During the last 30 days, did you ride in a car with someone who was smoking cigarettes?” The possible responses included “I did not ride in a car in the last 30 days,” “Yes,” “No,” and “Not Stated.” Those who did not ride in a vehicle in the last 30 days before the survey and did not respond to the SHS question were excluded from the analysis.
2.3. Statistical analysis
Demographic characteristics were described by the full sample as well as by SHS groups (SHS in the vehicle vs. no SHS in the vehicle). Demographic variables were reported with unweighted counts and weighted percentage. Descriptive statistics and Rao-Scott Chi-Square tests were used for comparing characteristics between groups. Prevalence of exposure to SHS was estimated by grade levels (7–9 lower grade and 10–12 upper grade) since provincial policies vary slightly by age. However, all students in Grades 7–9 should be protected from exposure to SHS in vehicles according to the smoke-free policies. For each grade level, the analysis also examined exposure to SHS by demographic characteristics (sex, level of urbanization, and province of residence).
Additionally, we examined the correlates of exposure to SHS with the following included in the analysis: grade level, sex, involvement in risky behavior (i.e., use of tobacco, e-cigarettes, alcohol, and marijuana), level of urbanization, and province of residence. All analyses took account of the sample design by using the bootstrap weights provided in the 2016–2017 CSTADS. All tests were two-sided and used a 5% significance level. All of the statistical analyses were performed using SAS 9.4 (SAS Institute, Inc., Cary, NC).
3. Results
Of all 48,444 students included in our study, 15,001 (25.6%) were exposed to SHS in a vehicle during the 30 days prior to the survey, 51.0% were male, and 83.1% lived in an urban area. The descriptive statistics and weighted percentage by SHS status are shown in Table 1. Compared to no exposure to SHS in a vehicle, students in the SHS group tended to be an upper grade and living in a rural area. Additionally, students in the SHS group were more likely to engage in risky behaviors such as cigarette use, e-cigarette use, alcohol use, and marijuana use.
Table 1.
Descriptive statistics of study population, Grades 7–12 students in Canada.
| Full sample | SHS in car | No SHS in car | p-Value | |
|---|---|---|---|---|
| n | 48,444 | 15,001 (26.56) | 33,443 (73.44) | |
| Grade | <0.0001 | |||
| 7 | 8186 (16.19) | 1687 (10.23) | 6499 (18.34) | |
| 8 | 8594 (16.21) | 2115 (12.85) | 6479 (17.42) | |
| 9 | 9922 (17.04) | 2933 (16.42) | 6989 (17.27) | |
| 10 | 8154 (17.17) | 2829 (19.02) | 5325 (16.50) | |
| 11 | 7726 (17.12) | 2927 (19.73) | 4799 (16.17) | |
| 12 | 5862 (16.27) | 2510 (21.74) | 3352 (14.29) | |
| Sex | 0.40 | |||
| Female | 24,545 (49.01) | 7725 (49.64) | 16,820 (48.78) | |
| Male | 23,899 (50.99) | 7276 (50.36) | 16,623 (51.22) | |
| Urban/rural | <0.0001 | |||
| Urban | 36,594 (83.14) | 9940 (75.28) | 26,654 (85.98) | |
| Rural | 11,850 (16.86) | 5061 (24.72) | 6789 (14.02) | |
| Province | <0.0001 | |||
| Newfoundland and Labrador | 5615 (1.37) | 2081 (1.99) | 3534 (1.14) | |
| Prince Edward Island | 4227 (0.44) | 1507 (0.64) | 2720 (0.36) | |
| Nova Scotia | 4528 (2.66) | 1685 (3.95) | 2843 (2.19) | |
| Quebec | 3033 (18.30) | 884 (19.34) | 2149 (17.92) | |
| Ontario | 9424 (44.73) | 2540 (39.04) | 6884 (46.79) | |
| Manitoba | 3545 (4.06) | 1086 (5.13) | 2459 (3.68) | |
| Saskatchewan | 3195 (3.33) | 1394 (5.97) | 1801 (2.38) | |
| Alberta | 8893 (12.21) | 2756 (14.36) | 6137 (11.44) | |
| British Columbia | 5984 (12.90) | 1068 (9.58) | 4916 (14.10) | |
| Marijuana use | <0.0001 | |||
| Yes | 5443 (11.18) | 3821 (26.76) | 1622 (5.63) | |
| No | 42,471 (88.82) | 10,866 (73.24) | 31,605 (94.37) | |
| Alcohol use | <0.0001 | |||
| Yes | 12,501 (27.54) | 6778 (49.10) | 5723 (19.88) | |
| No | 34,028 (72.46) | 7395 (50.90) | 26,633 (80.12) | |
| Cigarette use | <0.0001 | |||
| Yes | 3618 (6.33) | 3085 (19.39) | 533 (1.62) | |
| No | 44,771 (93.67) | 11,875 (80.61) | 32,896 (98.38) | |
| E-cigarette use | <0.0001 | |||
| Yes | 6968 (11.14) | 4374 (24.95) | 2594 (6.13) | |
| No | 41,193 (88.86) | 10,548 (75.05) | 30,645 (93.87) |
All descriptive statistic was presented in unweighted counts and weighted column percentage. SHS = second hand smoking. Rao-Scott Chi-Square tests were used for comparing characteristics and significant p-value (p < .05) was presented in bold.
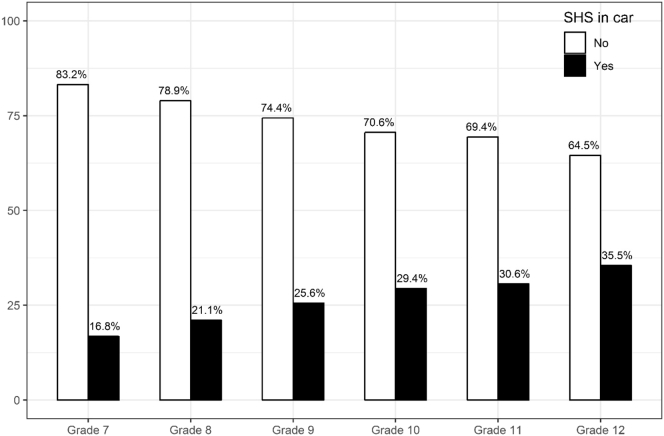
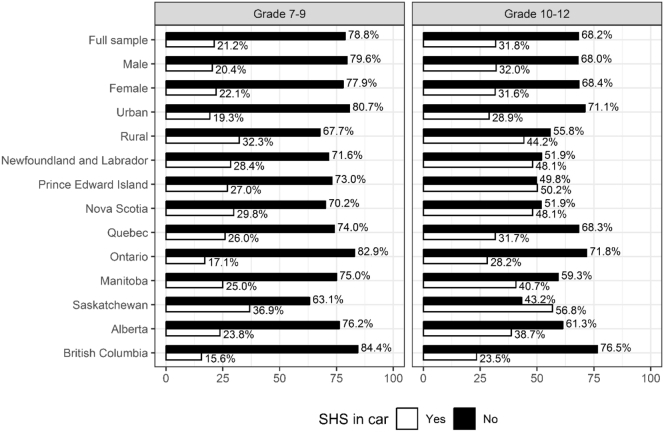
Fig. 2 shows the prevalence of SHS exposure in vehicles by grade level. The results show a gradient in exposure to SHS by grade, with those in high school reporting a higher prevalence of exposure. The prevalence of SHS in Grade 12 (35.5%) was more than twice the prevalence of that in Grade 7 (16.8%). Fig. 3 shows the prevalence of SHS exposure by demographic characteristics for students in lower grades (Action on Smoking & Health, n.d.; Håberg et al., 2007; Lam et al., 2001) and upper grades (Cheraghi & Salvi, 2009; Dybing & Sanner, 1999; Olivo-Marston et al., 2009) separately. The prevalence was higher in all subgroups for upper-grade students compared to lower-grade students. In lower grades, the prevalence was lower in males (20.4% vs 22.1%, respectively) and students living in urban areas (19.3% vs 32.3%, respectively). The prevalence of SHS varied by province with the lowest rate found in British Columbia (15.6%) and the highest in Saskatchewan (36.9%). However, in upper grades, the difference between males and females became marginal, but the prevalence of SHS exposure for both male and female students in urban areas was still lower than that for students in rural areas. The prevalence was lowest in British Columbia (23.5%) and highest in Saskatchewan (56.8%) for upper grades, with the prevalence much higher when compared to lower grades.
Fig. 2.
Exposure to secondhand smoking in vehicles by grade.
Fig. 3.
Exposure to secondhand smoking in vehicles by demographic characteristics.
*Rao-Scott Chi-Square tests were used for comparing SHS exposure in vehicles by demographic characteristics between students in Grades 7–9 and Grades 10–12.
Regression analyses of the correlates of SHS exposure are presented in Table 2. Female students had higher odds of SHS exposure in vehicles (AOR 1.15, 95% CI 1.05–1.27). Involvement in risky behaviors was significantly associated with higher odds of exposure to SHS (cigarette use, AOR 5.39, 95% CI 4.33–6.72; e-cigarette use, AOR 1.89, 95% CI 1.67–2.14; alcohol use, AOR 1.97, 95% CI 1.77–2.18; marijuana use, AOR 2.21, 95% CI 1.91–2.55). Students living in urban areas were less likely to be exposed to SHS in vehicles compared to peers living in rural areas (AOR 0.63, 95% CI 0.50–0.79). Compared to Quebec students, students in Newfoundland and Labrador (AOR 1.32, 95% CI 1.09–1.58), Prince Edward Island (AOR 1.29, 95% CI 1.00–1.67), Nova Scotia (AOR 1.35, 95% CI 1.07–1. 71), and Saskatchewan (AOR 1.84, 95% CI 1. 51–2.25) had higher odds of SHS exposure. Students in British Columbia (AOR 0.59, 95% CI 0.47–0.75) had lower odds of SHS exposure in vehicles. Similar results were found in the analysis stratified by grade level, with fewer significant provincial differences among students in lower grades (Table 2). Students in Grades 7–9 in Saskatchewan had higher odds of SHS exposure. Students in British Columbia still had lower odds of SHS compared to students in Quebec.
Table 2.
Multivariable analysis of secondhand smoke exposure in vehicles.
| Covariates | Exposure to secondhand smoke in vehicles |
||
|---|---|---|---|
| Full sample | Grades 7–9 | Grades 10–12 | |
| Grade | |||
| 7 | 0.82 (0.66, 1.01) | 0.84 (0.70, 1.00) | – |
| 8 | 0.93 (0.75, 1.15) | 0.94 (0.80, 1.11) | – |
| 9 | 1.00 (0.86, 1.16) | ref | – |
| 10 | 0.97 (0.85, 1.09) | – | 0.99 (0.89, 1.11) |
| 11 | 0.87 (0.76, 0.98) | – | 0.89 (0.78, 1.00) |
| 12 | ref | – | ref |
| Sex | |||
| Female | 1.15 (1.05, 1.27) | 1.16 (1.04, 1.30) | 1.15 (1.00, 1.33) |
| Male | ref | ref | ref |
| Marijuana use | 2.21 (1.91, 2.55) | 2.26 (1.73, 2.96) | 2.22 (1.88, 2.62) |
| Alcohol use | 1.97 (1.77, 2.18) | 2.10 (1.80, 2.45) | 1.91 (1.68, 2.18) |
| Cigarette use | 5.39 (4.33, 6.72) | 3.28 (2.26, 4.75) | 6.06 (4.69, 7.82) |
| E-cigarette use | 1.89 (1.67, 2.14) | 2.44 (1.99, 3.01) | 1.69 (1.46, 1.96) |
| Urban/rural | |||
| Urban | 0.63 (0.50, 0.79) | 0.61 (0.50, 0.73) | 0.65 (0.45, 0.93) |
| Rural | ref | ref | ref |
| Province | |||
| Newfoundland and Labrador | 1.32 (1.09, 1.58) | 1.04 (0.85, 1.28) | 1.69 (1.29, 2.22) |
| Prince Edward Island | 1.29 (1.00, 1.67) | 1.05 (0.84, 1.31) | 1.65 (1.06, 2.56) |
| Nova Scotia | 1.35 (1.07, 1.71) | 1.15 (0.88, 1.50) | 1.62 (1.22, 2.15) |
| Ontario | 0.84 (0.70, 1.02) | 0.77 (0.63, 0.94) | 0.96 (0.73, 1.26) |
| Manitoba | 1.09 (0.87, 1.36) | 0.99 (0.80, 1.22) | 1.25 (0.89, 1.76) |
| Saskatchewan | 1.84 (1.51, 2.25) | 1.63 (1.31, 2.04) | 2.17 (1.60, 2.96) |
| Alberta | 1.13 (0.96, 1.34) | 1.07 (0.88, 1.30) | 1.27 (1.00, 1.62) |
| British Columbia | 0.59 (0.47, 0.75) | 0.62 (0.49, 0.77) | 0.61 (0.42, 0.88) |
| Quebec | ref | ref | ref |
ref = reference category and significant odds ratios are presented in bold. Logistic regression was used in estimating the adjusted odds of exposure to SHS (95% CI).
4. Discussion
Recognizing the health risks associated with exposure to SHS in cars, all Canadian provinces have implemented laws prohibiting smoking in vehicles carrying children. This study aimed to examine the prevalence of exposure to secondhand smoke in vehicles among Canadian adolescents in Grades 7–12, years after policy implementation. Our results show that Saskatchewan had the highest prevalence of SHS in vehicles. This remained true when prevalence by demographic characteristics for lower grades and upper grades were examined separately, although rates were much higher in upper grades compared to lower grades. In comparison to other provinces, Saskatchewan has the highest estimates of current smoking among youth aged 15–19 and has some of the highest rates of adult smoking (Reid et al., 2019). Students in Quebec, Newfoundland and Labrador, Prince Edward Island, Nova Scotia, and Saskatchewan had higher odds of SHS exposure. Not surprisingly, some of these provinces (Newfoundland and Labrador, Nova Scotia, Saskatchewan) have also displayed the highest rates of adult smoking in recent years (Reid et al., 2019). British Columbia had the lowest prevalence of SHS exposure in vehicles; this province consistently has one of the lower smoking rates in both adults and youth (Reid et al., 2019), which could indicate that adults are not exposing children to SHS in vehicles as often as provinces with higher rates of smoking. Additionally, past research has found that Saskatchewan has greater prevalence of smoking compared to some other provinces, including British Columbia (https://uwaterloo.ca/tobacco-use-canada/adult-tobacco-use/smoking-provinces, 2017).
Findings show a gradient in exposure to SHS in vehicles by grade, with a higher prevalence of exposure to SHS among upper-grade level students. The prevalence was higher in all subgroups for upper-grade students compared to lower-grade students. The evidence found in our study that students in Grades 10–12 had particularly high prevalence and odds of SHS exposure in vehicles, is consistent with past findings. For example, one prior study found that the prevalence of SHS exposure increased as the grade increased among middle and high school students in Texas, with 65.8% of high school students reporting SHS exposure compared to 50.6% of middle school students (Centers for Disease Control and Prevention (CDC), 2003).
The prevalence of SHS exposure in vehicles appears to remain high, even with laws prohibiting smoking in vehicles carrying children. Past research has found similar findings concerning parental bans of smoking in cars and homes of children with asthma, with many remaining exposed to SHS (Halterman, Fagnano, Conn, & Szilagyi, 2006). Higher rates among the upper-grade levels are less surprising, given that only a few laws cover 18–19-year-olds. However, it is important to note that the provinces that do protect older children (Nova Scotia, Prince Edward Island, and Alberta) still have high rates of SHS. Of particular concern are the rates among lower-grade levels, even though all the existing laws should cover children 16 and under (Grades 7–9). Contributing to these high rates could be the difficulty of enforcing these laws. For example, determining the age of a child in provinces that implement the policy only for children 16 and under may prove difficult. However, given that the majority of the public support the bans, including active smokers (Hitchman et al., 2010), and the intention of the laws to influence behavior and norms in society (Saltman, Hitchman, Sendzik, & Fong, 2010), it is critically important for local authorities to dedicate more resources to enforcement. Additionally, family bans of smoking in cars may be an effective means to limit SHS among adolescents and should be explored in the future. Efforts aimed at reducing smoking and SHS, particularly in homes and cars, also have implications for thirdhand smoke (THS). THS refers to residual tobacco and aged secondhand smoke that remains on surfaces and in the area (Jacob, Benowitz, Destaillats, et al., 2017), and poses a potential health risk, though further research is needed (Díez-Izquierdo et al., 2018; Matt, Quintana, Destaillats, et al., 2011).
Results found that those students involved in risky behaviors may be more likely to be exposed to SHS. One study found that among college students, daily or nondaily smoking, binge drinking, and pledging to a fraternity or sorority were associated with SHS exposure (Wolfson, McCoy, & Sutfin, 2009). Evidence suggests that bar, nightclub, and restaurant workers and owners may have a high prevalence of SHS exposure (Fallin, Neilands, Jordan, & Ling, 2013; Jones, Wipfli, Shahrir, et al., 2013; Liu, Hammond, Hyland, et al., 2011). The results of this study must be considered along with its limitations. The self-reporting nature of the survey introduces the possibility of an inaccurate recall of events. Additionally, comparing results with past studies is challenging, considering most use a measurement of SHS exposure in the past 7 days, and the current study used past 30-day exposure. Another limitation is that we were unable to measure the frequency of SHS; although it should be noted that there is no risk-free level of SHS exposure (U.S. Department of Health and Human Services, 2014), and studies have shown a dose-response relationship between SHS and adverse health outcomes (Huang, Xu, Guo, et al., 2018; Oono, Mackay, & Pell, 2011; IOM (Institute of Medicine), n.d.). Lastly, a grade variable was used in place of age, as age was not publicly available. We likened Grade 9 to be around 14–15 years of age and were, therefore, able to examine the policies based on grade level rather than age.
5. Conclusion
There is a gradient in the prevalence of vehicle SHS exposure by grade level, indicating that upper-grade level students may be disproportionately impacted by SHS in vehicles. SHS prevalence appears to remain high, even with laws prohibiting smoking in vehicles carrying children. While enforcement of these laws may be challenging, an effective strategy needs to be developed, including a mass media campaign highlighting that adolescents are especially vulnerable to the health risks of SHS. Future research should consider variations in enforcement across provinces.
Declaration of competing interest
The authors declare that they have no conflict of interest.
Acknoledgements
The Health Studies Fund in the Department of Family and Preventive Medicine, University of Utah, contributed toward the open access fee.
References
- Action on Smoking & Health Smoke-free vehicles. Smoke-free vehicles. https://www.ash.ca/smoke_free_vehicles
- Akhtar P.C., Currie D.B., Currie C.E., Haw S.J. Changes in child exposure to environmental tobacco smoke (CHETS) study after implementation of smoke-free legislation in Scotland: National cross sectional survey. Bmj. 2007;335(7619):545. doi: 10.1136/bmj.39311.550197.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Nonsmokers' Rights Foundation. Secondhand smoke exposure in cars. Children and adult passengers are at risk. https://no-smoke.org/at-risk-places/cars/. Published n.d. Accessed April 1, 2019.
- Azagba S. Effect of smoke-free patio policy of restaurants and bars on exposure to second-hand smoke. Preventive Medicine. 2015;76:74–78. doi: 10.1016/j.ypmed.2015.04.012. [DOI] [PubMed] [Google Scholar]
- Azagba S., Kennedy R.D., Baskerville N.B. Smoke-free school policy and exposure to secondhand smoke: A quasi-experimental analysis. Nicotine & Tobacco Research. 2016;18(2):170–176. doi: 10.1093/ntr/ntv077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Canadian Substance Use Costs and Harms Scientific Working Group . Prepared by the Canadian Institute for Substance Use Research and the Canadian Centre on Substance Use and Addiction. Canadian Centre on Substance Use and Addiction; Ottawa, Ont: 2018. Canadian substance use costs and harms (2007–2014)http://www.ccsa.ca/Resource%20Library/CSUCH-Canadian-Substance-Use-Costs-Harms-Report-2018-en.pdf [Google Scholar]
- Centers for Disease Control and Prevention (CDC) Secondhand smoke exposure among middle and high school students. Texas, 2001. MMWR. Morbidity and Mortality Weekly Report. 2003;52(8):152–154. [PubMed] [Google Scholar]
- Cheraghi M., Salvi S. Environmental tobacco smoke (ETS) and respiratory health in children. European Journal of Pediatrics. 2009;168(8):897–905. doi: 10.1007/s00431-009-0967-3. [DOI] [PubMed] [Google Scholar]
- Department of Health The smoke-free (private vehicles) regulations 2015. 2015. http://www.legislation.gov.uk/ukdsi/2015/9780111126004/pdfs/ukdsi_9780111126004_en.pdf
- Department of Health and Social Care Towards a Smokefree generation. A tobacco control plan for England. 2017. https://www.gov.uk/government/publications/towards-a-smoke-free-generation-tobacco-control-plan-for-england
- DeRosenroll M., Cunningham R. Laws Banning Smoking in Vehicles Carrying Children – International Overview. Canadian Cancer Society. 2007 http://smokefreekings.org/wp-content/uploads/2011/05/international-overview-2007-10-15.pdf [Google Scholar]
- Díez-Izquierdo A., Cassanello-Peñarroya P., Lidón-Moyano C., Matilla-Santander N., Balaguer A., Martínez-Sánchez J.M. Update on thirdhand smoke: A comprehensive systematic review. Environmental Research. 2018;167:341–371. doi: 10.1016/j.envres.2018.07.020. [DOI] [PubMed] [Google Scholar]
- Dove M.S., Dockery D.W., Connolly G.N. Smoke-free air laws and secondhand smoke exposure among nonsmoking youth. Pediatrics. 2010;126(1):80–87. doi: 10.1542/peds.2009-3462. [DOI] [PubMed] [Google Scholar]
- Dybing E., Sanner T. Passive smoking, sudden infant death syndrome (SIDS) and childhood infections. Human & Experimental Toxicology. 1999;18(4):202–205. doi: 10.1191/096032799678839914. [DOI] [PubMed] [Google Scholar]
- Fallin A., Neilands T.B., Jordan J.W., Ling P.M. Secondhand smoke exposure among young adult sexual minority bar and nightclub patrons. American Journal of Public Health. 2013;104(2):e148–e153. doi: 10.2105/AJPH.2013.301657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Håberg S.E., Stigum H., Nystad W., Nafstad P. Effects of pre-and postnatal exposure to parental smoking on early childhood respiratory health. American Journal of Epidemiology. 2007;166(6):679–686. doi: 10.1093/aje/kwm134. [DOI] [PubMed] [Google Scholar]
- Halterman J.S., Fagnano M., Conn K.M., Szilagyi P.G. Do parents of urban children with persistent asthma ban smoking in their homes and cars? Ambulatory Pediatrics. 2006;6(2):115–119. doi: 10.1016/j.ambp.2005.10.004. [DOI] [PubMed] [Google Scholar]
- Hitchman S.C., Fong G.T., Zanna M.P., Hyland A., Bansal-Travers M. Support and correlates of support for banning smoking in cars with children: Findings from the ITC Four Country Survey. The European Journal of Public Health. 2010;21(3):360–365. doi: 10.1093/eurpub/ckq097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tobacco use in Canada. Smoking in the provinces. Tobacco use in Canada. https://uwaterloo.ca/tobacco-use-canada/adult-tobacco-use/smoking-provinces. Published 2017. (Accessed August 2, 2019).
- Huang J., Xu B., Guo D. Dose–response relationships between second-hand smoke exposure and depressive symptoms among adolescents in Guangzhou, China. International Journal of Environmental Research and Public Health. 2018;15(5) doi: 10.3390/ijerph15050985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- IARC Working Group on the Evaluation of Carcinogenic Risks to Humans . International Agency for Research on Cancer; 2012. Tobacco smoking.https://www.ncbi.nlm.nih.gov/books/NBK304395/ [PMC free article] [PubMed] [Google Scholar]
- IOM (Institute of Medicine) Secondhand smoke exposure and cardiovascular effects: Making sense of the evidence. The National Academies Press; Washington, DC: 2010. Epidemiologic studies of secondhand-smoke exposure and cardiovascular disease. [PubMed] [Google Scholar]
- Jacob P., Benowitz N.L., Destaillats H. Thirdhand smoke: New evidence, challenges, and future directions. Chemical Research in Toxicology. 2017;30(1):270–294. doi: 10.1021/acs.chemrestox.6b00343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones M.R., Navas-Acien A., Yuan J., Breysse P.N. Secondhand tobacco smoke concentrations in motor vehicles: A pilot study. Tobacco Control. 2009;18(5):399–404. doi: 10.1136/tc.2009.029942. [DOI] [PubMed] [Google Scholar]
- Jones M.R., Wipfli H., Shahrir S. Secondhand tobacco smoke: An occupational hazard for smoking and non-smoking bar and nightclub employees. Tobacco Control. 2013;22(5):308–314. doi: 10.1136/tobaccocontrol-2011-050203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lam L.T. Distractions and the risk of car crash injury: The effect of drivers’ age. Journal of Safety Research. 2002;33(3):411–419. doi: 10.1016/s0022-4375(02)00034-8. [DOI] [PubMed] [Google Scholar]
- Lam T.-H., Leung G.M., Ho L.-M. The effects of environmental tobacco smoke on health services utilization in the first eighteen months of life. Pediatrics. 2001;107(6):e91. doi: 10.1542/peds.107.6.e91. [DOI] [PubMed] [Google Scholar]
- Liu R., Hammond S.K., Hyland A. Restaurant and bar owners’ exposure to secondhand smoke and attitudes regarding smoking bans in five Chinese cities. International Journal of Environmental Research and Public Health. 2011;8(5):1520–1533. doi: 10.3390/ijerph8051520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matt G.E., Quintana P.J.E., Destaillats H. Thirdhand tobacco smoke: Emerging evidence and arguments for a multidisciplinary research agenda. Environmental Health Perspectives. 2011;119(9):1218–1226. doi: 10.1289/ehp.1103500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Northcross A.L., Trinh M., Kim J. Particulate mass and polycyclic aromatic hydrocarbons exposure from secondhand smoke in the back seat of a vehicle. Tobacco Control. 2014;23(1):14–20. doi: 10.1136/tobaccocontrol-2012-050531. [DOI] [PubMed] [Google Scholar]
- Öberg M., Jaakkola M.S., Woodward A., Peruga A., Prüss-Ustün A. Worldwide burden of disease from exposure to second-hand smoke: A retrospective analysis of data from 192 countries. The Lancet. 2011;377(9760):139–146. doi: 10.1016/S0140-6736(10)61388-8. [DOI] [PubMed] [Google Scholar]
- Olivo-Marston S.E., Yang P., Mechanic L.E. Childhood exposure to secondhand smoke and functional mannose binding lectin polymorphisms are associated with increased lung cancer risk. Cancer Epidemiology and Prevention Biomarkers. 2009;18(12):3375–3383. doi: 10.1158/1055-9965.EPI-09-0986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oono I.P., Mackay D.F., Pell J.P. Meta-analysis of the association between secondhand smoke exposure and stroke. Journal of Public Health (Oxford, England) 2011;33(4):496–502. doi: 10.1093/pubmed/fdr025. [DOI] [PubMed] [Google Scholar]
- Potera C. Smoking and secondhand smoke: Study finds no level of SHS exposure free of effects. Environmental Health Perspectives. 2010;118(11):A474. doi: 10.1289/ehp.118-a474a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rehm J., Gnam W., Popova S. The costs of alcohol, illegal drugs, and tobacco in Canada, 2002. Journal of Studies on Alcohol and Drugs. 2007;68(6):886–895. doi: 10.15288/jsad.2007.68.886. [DOI] [PubMed] [Google Scholar]
- Reid J.L, Hammond D., Tariq U., Burkhalter R., Rynard V.L, Douglas O. Waterloo, ON: Propel Centre for Population Health Impact, University of Waterloo. 2019 Ed. 2019. Tobacco Use in Canada: Patterns and Trends.https://uwaterloo.ca/tobacco-use-canada/tobacco-use-canada-patterns-and-trends [Google Scholar]
- Saltman D., Hitchman S.C., Sendzik T., Fong G.T. 2009–10. CACC: Cancer Advocacy Coalition of Canada, Report Card on Cancer in Canada; Toronto: 2010. The current status of bans on smoking in vehicles carrying children: A Canadian perspective; pp. 6–10. [Google Scholar]
- Sendzik T., Fong G.T., Travers M.J., Hyland A. An experimental investigation of tobacco smoke pollution in cars. Nicotine & Tobacco Research. 2009;11(6):627–634. doi: 10.1093/ntr/ntp019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sly P.D., Deverell M., Kusel M.M., Holt P.G. Exposure to environmental tobacco smoke in cars increases the risk of persistent wheeze in adolescents. The Medical Journal of Australia. 2007;186(6):322. doi: 10.5694/j.1326-5377.2007.tb00915.x. [DOI] [PubMed] [Google Scholar]
- Strulovici-Barel Y., Omberg L., O’Mahony M. Threshold of biologic responses of the small airway epithelium to low levels of tobacco smoke. American Journal of Respiratory and Critical Care Medicine. 2010;182(12):1524–1532. doi: 10.1164/rccm.201002-0294OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2006. The health consequences of involuntary exposure to tobacco smoke: A report of the surgeon general. http://www.ncbi.nlm.nih.gov/books/NBK44324/ [PubMed]
- U.S. Department of Health and Human Services . U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; Atlanta, GA: 2014. The health consequences of smoking: 50 years of progress. A report of the surgeon general.https://www.cdc.gov/tobacco/data_statistics/sgr/50th-anniversary/index.htm [Google Scholar]
- Vafaee-Najar A., Khabbazkhoob M., Alidadi-Soltangholi H., Asgari S., Ibrahimipour H. Investigating the relative risk factors of injuries caused by accidents on roads in the Mashhad area in 2007. Iranian Red Crescent Medical Journal. 2011;13(8):530–536. [PMC free article] [PubMed] [Google Scholar]
- Wolfson M., McCoy T.P., Sutfin E.L. College students’ exposure to secondhand smoke. Nicotine & Tobacco Research. 2009;11(8):977–984. doi: 10.1093/ntr/ntp100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization Geneva: World Health Organization; 2017. WHO report on the global tobacco epidemic 2017: Monitoring tobacco use and prevention policies. https://www.who.int/tobacco/global_report/2017/en/
- World Health Organization, International Agency for Research on Cancer . IARC monographs on the evaluation of carcinogenic risks to humans. Vol. 83. IARCPress, World Health Organization Marketing and Dissemination; 2004. Tobacco smoke and involuntary smoking; p. 1187.https://monographs.iarc.fr/iarc-monographs-on-the-evaluation-of-carcinogenic-risks-to-humans-38/ (Accessed March 28, 2019) [Google Scholar]