Introduction
Leukemia cutis (LC) and eosinophilic dermatosis of hematologic malignancy (EDHM) are rare cutaneous manifestations of hematologic malignancies. Various therapeutic options have been reported, with largely underwhelming responses. We present a patient with chronic lymphocytic leukemia (CLL) with concomitant LC and EDHM who was treated with dupilumab.
Case report
An 81-year-old Hispanic man with CLL presented for “sores” on his arms, back, and face. The patient had been treated with acyclovir and valacyclovir for presumed varicella zoster infection a few weeks prior. No improvement of his rash was noted. Prior biopsy by an outside dermatologist showed acantholysis and spongiosis concerning for pemphigus vulgaris, but direct immunofluorescence results were negative. The rash had improved with prednisone but recurred shortly afterward.
Physical examination showed erythematous erosions with scaling and crusting in a dermatomal distribution on the left chest and face; a single ulcerated nodule on the scalp; and several well-demarcated, faintly pink dermal nodules on the back and left neck (Fig 1). Biopsy results for samples from the left neck and back were consistent with LC (Fig 2), whereas biopsy results for samples from the left chest, left sideburn, and scalp were consistent with EDHM (Fig 3). The patient received rituximab and chlorambucil for the LC and started a slow, 6-week prednisone taper for the EDHM, with resolution of his lesions. Once the patient was receiving less than 10 mg of prednisone daily, his eruption quickly flared. Repeat biopsy again confirmed EDHM. After numerous failed attempts to wean the patient off oral steroids, the patient was started on dupilumab off-label, with a loading dose of 600 mg subcutaneously followed by 300 mg once every 2 weeks. The lesions resolved after 2 injections (Fig 4). The patient remained clear while receiving dupilumab for more than 6 months as his CLL was treated.
Fig 1.
Confluent erythematous macules and patches on left chest and proximal aspect of the left arm before treatment with dupilumab.
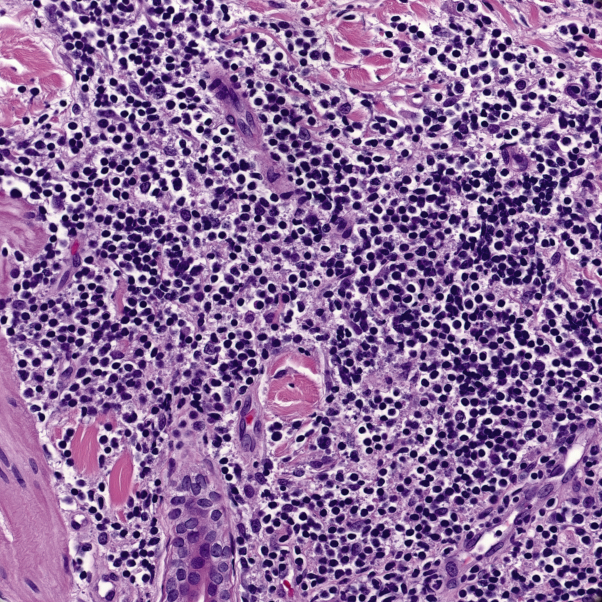
Fig 2.
Dense, lymphocytic infiltrate composed of hyperchromatic lymphocytes, many of which coexpress CD5, Bcl2, and CD23 on immunohistochemical staining. No eosinophils were noted.
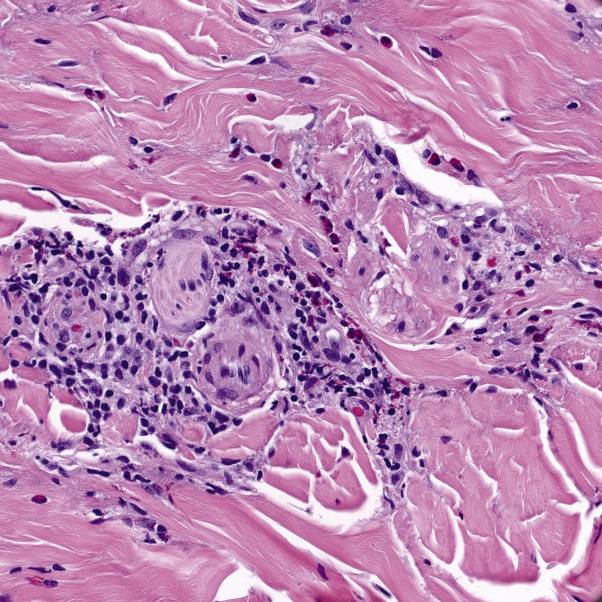
Fig 3.
Superficial and deep perivascular and interstitial dermatitis with numerous eosinophils. Original magnification, ×400.
Fig 4.
After 2 doses of dupilumab.
Discussion
LC and EDHM are rare cutaneous manifestations of hematologic malignancies. Our case was complicated by the presence of both lesions, which is unusual.
LC typically presents with erythematous, firm papules and nodules and has been reported to have a predilection for sites of previous zoster infection, as in our patient. Treatment is targeted at the underlying malignancy.1
EDHM is most commonly associated with CLL, as seen in our patient, and it often presents as pruritic, tender nodules or papules that are erythematous and indurated.2 Previous studies have reported inadequate responses to topical corticosteroids, systemic antihistamines, ultraviolet B phototherapy, and interferon therapy in the majority of cases.3 Partial or complete response to prednisone has been reported in several studies, which was consistent with our patient's experience.3, 4 Although some studies have also reported positive responses with dapsone, adverse effects ultimately resulted in discontinuation of that drug.4
Cytokine imbalance is theorized to drive the proliferation of malignant B cells in patients with EDHM, due to excessive amounts of interleukin (IL) 4 and IL-5.5 The role of IL-4 in B-cell class switching is well established. Excess IL-4 is thought to also drive the altered immune response with eosinophilic infiltrate seen in EDHM—as shown by lesional EDHM biopsies with prolonged eosinophil survival in culture.3 Dupilumab is a monoclonal antibody that occupies the shared alpha subunit receptor site for IL-4 (IL-4a), thereby blocking the effects of IL-4 and IL-13 signaling pathways.6 We believe that our patient's dramatic response to dupilumab was due to attenuation of excessive IL-4 levels that led to the development of his EDHM lesions.
In conclusion, IL-4 dysregulation plays a role in the development of EDHM, as evidenced by our patient's remarkable response to dupilumab.
Footnotes
Funding sources: None.
Disclosure: Dr Mollanazar and Dr Hsu report serving as an investigators in trials sponsored by Sanofi and Regeneron Pharmaceuticals. Ms Jin, Mr Pousti, Mr Savage, and Dr Lee have no conflicts of interest to declare.
References
- 1.Lee J.I., Park H.J., Oh S.T., Lee J.Y., Cho B.K. A case of leukemia cutis at the site of a prior catheter insertion. Ann Dermatol. 2009;21(2):193–196. doi: 10.5021/ad.2009.21.2.193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Farber M.J., La Forgia S., Sahu J., Lee J.B. Eosinophilic dermatosis of hematologic malignancy. J Cutan Pathol. 2012;39(7):690–695. doi: 10.1111/j.1600-0560.2012.01906.x. [DOI] [PubMed] [Google Scholar]
- 3.Davis M.D., Perniciaro C., Dahl P.R., Randle H.W., McEvoy M.T., Leiferman K.M. Exaggerated arthropod-bite lesions in patients with chronic lymphocytic leukemia: a clinical, histopathologic, and immunopathologic study of eight patients. J Am Acad Dermatol. 1998;39(1):27-35. doi: 10.1016/s0190-9622(98)70398-6. [DOI] [PubMed] [Google Scholar]
- 4.Bairey O., Goldschmidt N., Ruchlemer R. Insect-bite-like reaction in patients with chronic lymphocytic leukemia: a study from the Israeli Chronic Lymphocytic Leukemia Study Group. Eur J Haematol. 2012;89(6):491–496. doi: 10.1111/ejh.12015. [DOI] [PubMed] [Google Scholar]
- 5.Barzilai A., Shapiro D., Goldberg I. Insect bite–like reaction in patients with hematologic malignant neoplasms. Arch Dermatol. 1999;135(12):1503–1507. doi: 10.1001/archderm.135.12.1503. [DOI] [PubMed] [Google Scholar]
- 6.Gooderham M.J., Hong H.C., Eshtiaghi P. Dupilumab: a review of its use in the treatment of atopic dermatitis. J Am Acad Dermatol. 2018;78(3S1):S28–S36. doi: 10.1016/j.jaad.2017.12.022. [DOI] [PubMed] [Google Scholar]