Abstract
A wide number of disorders, including pathologies outside the hip, can cause and refer pain to hip. However, determining the cause of a painful hip can be a major challenge to orthopedic surgeons. Failure to diagnose and appropriately investigate pathologies of the hip in adults may result in delayed management and prolonged patient morbidity. A systematic approach to investigating the etiology of hip pain in adults (e.g., history, careful clinical and radiographic examination), will help identify the majority of clinically important pathologies which can cause hip pain. Conservative treatment and selective use of injection therapies has proven quite successful for the treatment of most causes of hip pain.
Keywords: Hip, Femoroacetabulum impingement, Osteoarthritis, Dysplasia
OVERVIEW
The causes of hip pain in adults has received less attention than those in children and older patients, and orthopedic surgeons have reported that the diagnoses and surgical care of these patients is deficient1,2). As these patients present with symptoms originating from different disease processes, lack of awareness among treating orthopods may result in delayed diagnoses. There has been an evolution in the field's understanding of hip pain in adults and it is now known that causes like femoroacetabular impingement (FAI) and dysplasia are treatable2,3). This review article aims to simplify etiological classification of hip pain in adults and summarize the diagnosis and management of these conditions.
INCIDENCE
An annual incidence of 0.44% has been reported in the Netherlands for groin or hip pain in patients between the ages of 15 to 60 years4).
HISTORY
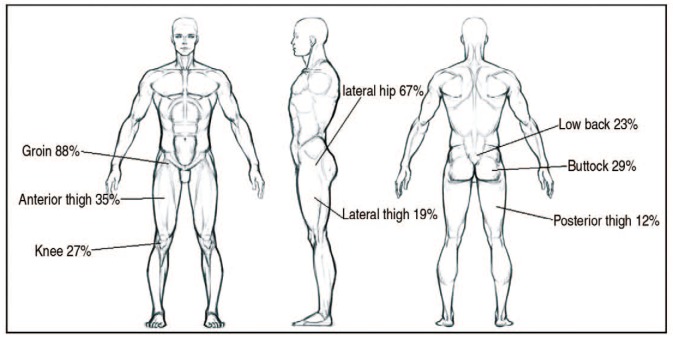
Pain is the most common presenting symptom of hip pain in adults; although this pain is most commonly located in the groin (88%), it may also occur anywhere around the hip, thigh or be referred to the knee via the obturator nerve (Fig. 1)2). Patients with intra-articular hip pathologies cup the trochanter making a C-sign (Fig. 2)5). Trochanteric pain may be a result of bursitis or iliotibial band friction syndrome while adductor pathologies result in medial thigh pain. Spinal causes have to be ruled out if pain is predominantly in the buttock and burning pain results from neural causes.
Fig. 1. Location of pain generated from hip pathology.
Fig. 2. C-sign in patients with hip pain. Patient with hip pathology usually point to the site of pain by cupping the thumb and index finger in the shape of the letter C.

Hip pain exacerbated by sitting for a prolonged period of time indicates impingement. Snapping or locking can be caused by labral tears, loose bodies or rubbing tendons. History of childhood diseases may suggest possible sequelae of Perthes or slipped capital femoral epiphysis (SCFE). Risk factors for avascular necrosis need to be screened during history. Participation in specific sports and recreational activities may also be important risk factors. For instance, labral tears are seen in footballers, gymnasts and surfers, runners often present with iliotibial band friction syndrome and cyclists may experience piriformis syndrome6).
EXAMINATION
Adult patients with hip pain typically have an antalgic gait; abductor weakness can result in a trendlenburg gait. Change in foot progression angle results from femoral anteversion anomalies. Hip examination is done standing and then supine following the usual routine look, feel and move7).
A patient can be screened for intra-articular pathologies using a Stinchfield (resisted hip flexion), log roll or heel strike (hit on the heel with palm) tests. Flexion abduction and external rotation (FABER Test) can diagnose sacroilitis or posterior impingement depending on the site of induced pain. Similarly flexion adduction and internal rotation is seen with anterior femoral impingement or piriformis syndrome (PACE test) depending on the area of symptom reproduction. Ober test is effective at diagnosing tightness in the iliotibial band and the Thomas test is positive in those with tight iliopsoas tendon. Location of tenderness can help to diagnose bursitis, avulsions and tendinitis around the hip8).
DIFFERENTIAL DIAGNOSIS8)
1. Pathologic Conditions Outside the Hip
Lumbar radiculopathy, genitourinary and intra-abdominal conditions may present with pain around the hip. Sports hernia results from abdominal hyperextension and thigh adduction. Compression neuropathies of genitofemoral (L1, L2, L3), iliohypogastric (T12, L1), ilio inguinal (T12, L1), lateral cutaneous nerve of thigh, obturator or pudendal nerve may present as hip pain.
2. Extra-articular Pathologies around the Hip
Bursae around the hip (trochanteric, iliopsoas, ischiogluteal) may get inflamed resulting in pain. Painful extra-articular impingement can be caused by sub-spine, greater trochantrictpelvic and ischio gluteal structures striking against each other. Acute injury may cause muscular strain or avulsions around hip tendon attachments and chronic overuse causes tendinitis, stress fractures. Piriformis syndrome, sacroilitis (e.g., ankylosing spondylitis), transient osteoporosis and snapping hips due to internal or external causes discomfort around the hip.
3. Intra-articular Causes: Soft Tissues
Labral tears, most commonly the result of acetabular dysplasia, can cause pain and/or snapping around the hip. Synovial chondromatosis and pigmented villonodular synovitis are some examples of synovial pathologies. Capsular tears and laxity, chondral defects and ligamentum teres pathologies are other intra-articular soft tissue causes of hip pain.
BONY CAUSES
FAI may be caused by proximal femur or acetabular rim deformities; dysplasias are a subset of treatable bony causes of hip pain. Sequelae of childhood diseases (Perthes, SCFE), septic arthritis, transient osteoporosis, osteonecrosis, and osteoarthritis are other bone-related causes of hip pain.
IMAGING
Anteroposterior (AP) and lateral X-rays are requested initially. On a standard AP view, the pelvic lines, joint space, sphericity of femoral head should be identified. Next, the center edge angle (25–40°) and Tonnis angle (0–10°) are calculated. Cross over sign and prominent ischial spine are seen in retroverted acetabulum (Fig. 3). Posterior wall medial to center of femoral head (posterior wall sign) indicates retroversion. A lateral view can be obtained either in frog leg or cross table-lateral positions, however, both reveal a different profile of the femoral head. Alpha angle (>45°) is measured on a frog leg view whereas the crosstable lateral view may reveal anterior cam lesions and aid in the measurement of head neck offset (<0.17)9,10). A false profile view reveals anterior osteophytes and anterior coverage of the femoral head11).
Fig. 3. Anteroposterior radiograph of the pelvis and both hips revealing cross over sign and ischial spine sign.

Ultrasound – a user dependent investigation modality is helpful in diagnosing tendinitis and bursitis. This approach may also help to demonstrate real-time fascial or tendon snapping in coxa saltans.
A standard magnetic resonance imaging (MRI) aids in the diagnoses of osteonecrosis, infections, stress fractures and neoplasms. Intra-articular pathologies are better seen in magnetic resonance (MR) arthrography and para axial MR arthrography12). There can be high inter-observer variation in interpretation of MR arthrography. T1-rho and dGEMERIC (delayed gadolinium enhanced MRI) reveals articular cartilage and early osteoarthritis. Computed tomography (CT) scan is used to define osseous anatomy, acetabular version and impingement13). CT arthrography can also be used to assess cartilage and labral tears, however its use is limited due to increased exposure to radiation14).
Comparison of MR arthrography with arthroscopic findings revealed that when evaluating labral tears, MR is associated with a: i) sensitivity of 71%, ii) specificity of 44%, iii) positive predictive value of 93%, iv) negative predictive value of 13%, and v) accuracy of 69%15).
HIP INJECTION
A fluoroscopic-guided intra-articular hip injection of local anaesthetic can help identify the source of pain (Fig. 4)16).
Fig. 4. Intra-articular injection of right hip. The hip was approached anteriorly with spinal needle. Contrast was injected to confirm intra-articular position.

Electromyography and nerve conduction studies help in differentiating compression neuropathies from other causes of hip pain.
1. Labral Injuries
The hip labrum is a fibrocartilaginous structure which helps to improve the surface area of the hip and provide stable articulation. FAI and dysplasia are common causes of labral tear3,17). Torn labrums in athletes can be a source of debilitating pain and may result in reduced performance, although one should be aware of high incidence of asymptomatic tears in this subgroup18,19).
The concept of hip microinstability is gaining acceptance; the labrum has been found to play an important role underlining its importance20,21). Labral tears presents with pain, snapping and the sensation of hip locking; provocative test (pain if hip is brought from a fully flexed, externally rotated, and abducted position to a position of extension, internal rotation, and adduction) can help in diagnosing this condition18,22).
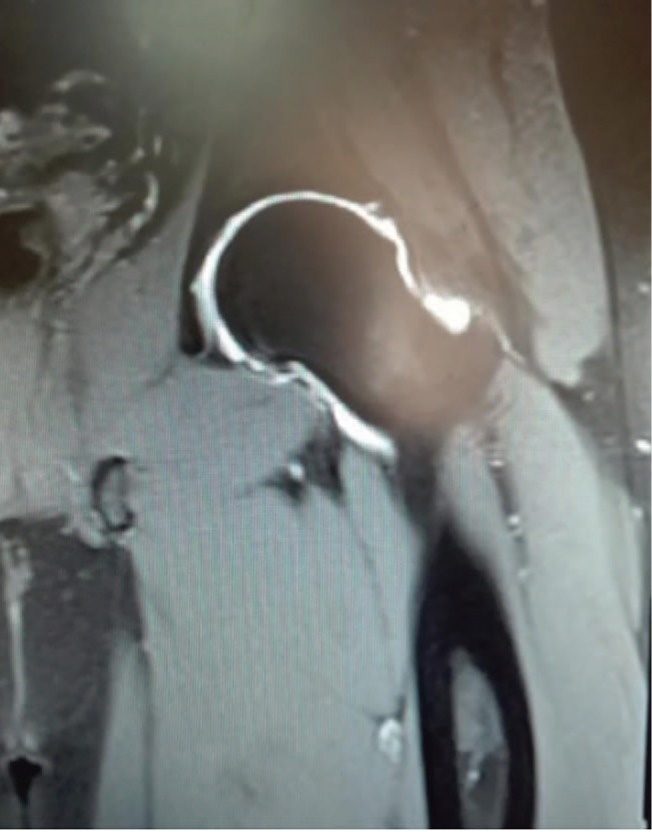
MR arthrography is the imaging modality of choice (Fig. 5)23,24). Conservative treatment should be attempted initially; if symptoms are persisting after adequate conservative treatment, surgery is considered18,25). Following labral debridement, a patient satisfaction rate of approximately 67% at 3.5 years follow-up, good results by a modified Harris Hip Score in patients who are subjectively satisfied with their outcome; and a complete resolution of mechanical symptoms in nearly 50% of patients with this complaint23). Partial arthroscopic resection of symptomatic acetabular labral tears has a reported success rate of between 70% and 85%5,18,23,26). There have been reports of improved hip functional score with repair versus debridement but most are level IV evidence27).
Fig. 5. Magnetic resonance arthrogram of left hip showing thickening of superior labrum with focal area of high signal intensity indicating superior labrum tear.
2. Femoroacetabular Impingement
FAI is a cause of early hip dysfunction that can lead to secondary osteoarthritis. An association between presence of FAI and development of osteoarthritis has been reported, but there are asymptomatic patients with radiological findings suggestive of FAI reported in other studies3,4,19,22,28,29). Cam impingement is due to a femur-based deformity associated with loss of spherecity of the femoral head, reduced head neck offset ratio and retroverted neck. Pincer impingement presents with morphological changes on the acetabular side with over-coverage, retro-verted acetabulum, coxaprofunda or protrusion; patient may also suffer from combined lesions3).
Morphological changes as described above may cause cartilage delamination and flap tears, labral degeneration and tears; patients with these changes present with pain in the groin, exacerbated by flexion of the hip and examination may reveal limited hip flexion and a positive FADIR (flexion adduction and internal rotation) test. Radiological findings are pistol grip deformity (cam lesions) and cross over sign and prominent ischial spine sign (Pincer lesions); reduced head neck offset (<0.17 measured in cross table lateral view) and reduced alpha angle (<45° measured in frog leg view)30). MR is the most effective modality to assess head neck junction anomalies as well as labral and cartilage degeneration and tears. CT scans may aid in defining structural morphology of the hip.
The management of FAI has been summarized in the Warwick international consensus statement31), and per this consensus, FAI can be managed by different modalities including conservative measures, rehabilitation or surgery31).
There is currently no high-level evidence to support the choice of a definitive treatment for FAI syndrome32,33). Conservative care of patients with FAI syndrome include patient education, activity and lifestyle modification, oral analgesia including non-steroidal anti-inflammatory drugs, intra-articular steroid injection and muscle strengthening around the hip33). Surgery is considered in patients with persistent pain and mechanical symptoms. The labrum or cartilage can be resected, repaired or reconstructed. An arthroscopic approach may be preferable in many patients to allow for a more rapid recovery, but some of these procedures will require an open approach. Cam morphology can be reshaped and femoral torsion or neck angle adjusted; the acetabulum can be reorientated or its rim trimmed. There is no evidence that treating people who do not have pain, but who do have cam or pincer morphology, will alter the risk of them developing FAI syndrome or osteoarthritis, and so it is rarely indicated to offer surgery to these patients31).
DYSPLASIA
Hip dysplasia is a condition of abnormal hip development secondary to capsular laxity and mechanical factors. Despite widespread screening programmes, some cases are not diagnosed until adulthood. An incidence of 0.1% has been reported in the United States34). A shallow acetabulum leads to supraphysiologic mechanical stress on articular cartilage35) leading to osteoarthritis changes with a reported incidence of between 20% and 40% (Fig. 6)36,37,38).
Fig. 6. Anteroposterior view of pelvis with hips showing bilateral hip dysplasia.

Groin pain is the most common presenting symptom with trendlenburg gait pattern35). Radiologically, an increased center edge angle of wiberg (>25°) extrusion index >25%, Tonnis angle >10°, are seen on AP view images38). Anterior center edge angle in measured in false profile view and values <20° are diagnostic of dysplasia11,13). Abnormal superior position of the fovea capitis femoris on MRI, also referred to as fovea alta, is seen in the adult dysplastic hip39). CT scans have enabled a more precise evaluation of the severity of acetabular dysplasia, but has the disadvantages of radiation exposure of the patient and relative insensitivity to early changes of cartilage damage13,14). MRI findings of labral disease in hip dysplasia include morphologic alterations (e.g., labral hypertrophy and tear, labral intrasubstance signal change, labral chondral junction disruption)40). Advanced MRI techniques (T1-rho, dGEMERIC) may help in identifying biochemical changes of articular cartilage and serve as prognosicators of periacetabular osteotomy.
Periacetabular osteotomy involving orthogonal cuts without disrupting the posterior columns or altering the shape of true pelvis has become a widely accepted surgical procedure for treatment of hip dysplasia41). A proximal femoral osteotomy can be added during surgery to optimize congruency and range of motion8,42).
CHONDRAL INJURIES
A thorough understanding of chondral injuries encountered during hip preservation is helpful for preoperative planning and intraoperative treatment. Conditions such as FAI, acetabular dysplasia, trauma, and avascular necrosis frequently involve damage to the chondral surface and subsequent clinical symptoms in young adults43). It is important to recognize that chondral damage may be an effect, not a cause3). Chondroplasty is a frequently performed technique for partial-thickness chondral injuries at the time of hip arthroscopy44). Small chondral defects of the femur and acetabulum are treated using microfracture surgery43). Osteochondral autograft transplantation and matrix-induced autologous chondrocyte implantation are performed for larger cartilage defects45,46).
SUMMARY
In recent years there has been improved understanding of hip disease in young adults along and innovations in the surgical techniques used to manage these conditions. An awareness of the causative conditions among orthopaedic surgeons may help ensure early intervention and improved patient satisfaction. Improved symptomatic relief is possible in patients waiting to develop end stage arthritis before undergoing total hip replacement; in some cases, this eventuality can be delayed or even averted.
Footnotes
CONFLICT OF INTEREST: The authors declare that there is no potential conflict of interest relevant to this article.
References
- 1.Dick AG, Houghton JM, Bankes MJK. An approach to hip pain in a young adult. BMJ. 2018;361:k1086. doi: 10.1136/bmj.k1086. [DOI] [PubMed] [Google Scholar]
- 2.Clohisy JC, Beaulé PE, O’Malley A, Safran MR, Schoenecker P. AOA symposium. Hip disease in the young adult: current concepts of etiology and surgical treatment. J Bone Joint Surg Am. 2008;90:2267–2281. doi: 10.2106/JBJS.G.01267. [DOI] [PubMed] [Google Scholar]
- 3.Ganz R, Parvizi J, Beck M, Leunig M, Nötzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;(417):112–120. doi: 10.1097/01.blo.0000096804.78689.c2. [DOI] [PubMed] [Google Scholar]
- 4.Röling MA, Mathijssen NM, Bloem RM. Incidence of symptomatic femoroacetabular impingement in the general population: a prospective registration study. J Hip Preserv Surg. 2016;3(3):203–207. doi: 10.1093/jhps/hnw009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Byrd JWT. Operative hip arthroscopy. New York: Springer; 2013. [Google Scholar]
- 6.Wilson JJ, Furukawa M. Evaluation of the patient with hip pain. Am Fam Physician. 2014;89:27–34. [PubMed] [Google Scholar]
- 7.Ali F. Clinical examination of the knee. Orthop Trauma. 2013;27:50–55. [Google Scholar]
- 8.Ward D, Parvizi J. Management of hip pain in young adults. Orthop Clin North Am. 2016;47:485–496. doi: 10.1016/j.ocl.2016.03.002. [DOI] [PubMed] [Google Scholar]
- 9.Clohisy JC, Nunley RM, Otto RJ, Schoenecker PL. The frog-leg lateral radiograph accurately visualized hip cam impingement abnormalities. Clin Orthop Relat Res. 2007;462:115–121. doi: 10.1097/BLO.0b013e3180f60b53. [DOI] [PubMed] [Google Scholar]
- 10.Meyer DC, Beck M, Ellis T, Ganz R, Leunig M. Comparison of six radiographic projections to assess femoral head/neck asphericity. Clin Orthop Relat Res. 2006;445:181–185. doi: 10.1097/01.blo.0000201168.72388.24. [DOI] [PubMed] [Google Scholar]
- 11.Lequesne M, de Seze. [False profile of the pelvis. A new radiographic incidence for the study of the hip. Its use in dysplasias and different coxopathies] Rev Rhum Mal Osteoartic. 1961;28:643–652. French. [PubMed] [Google Scholar]
- 12.Ito K, Minka MA, 2nd, Leunig M, Werlen S, Ganz R. Femoroacetabular impingement and the cam-effect. A MRI-based quantitative anatomical study of the femoral head-neck offset. J Bone Joint Surg Br. 2001;83:171–176. doi: 10.1302/0301-620x.83b2.11092. [DOI] [PubMed] [Google Scholar]
- 13.Klaue K, Wallin A, Ganz R. CT evaluation of coverage and congruency of the hip prior to osteotomy. Clin Orthop Relat Res. 1988;(232):15–25. [PubMed] [Google Scholar]
- 14.Nishii T, Tanaka H, Sugano N, Miki H, Takao M, Yoshikawa H. Disorders of acetabular labrum and articular cartilage in hip dysplasia: evaluation using isotropic high-resolutional CT arthrography with sequential radial reformation. Osteoarthritis Cartilage. 2007;15:251–257. doi: 10.1016/j.joca.2006.08.002. [DOI] [PubMed] [Google Scholar]
- 15.Keeney JA, Peelle MW, Jackson J, Rubin D, Maloney WJ, Clohisy JC. Magnetic resonance arthrography versus arthroscopy in the evaluation of articular hip pathology. Clin Orthop Relat Res. 2004;(429):163–169. doi: 10.1097/01.blo.0000150125.34906.7d. [DOI] [PubMed] [Google Scholar]
- 16.Pateder DB, Hungerford MW. Use of fluoroscopically guided intra-articular hip injection in differentiating the pain source in concomitant hip and lumbar spine arthritis. Am J Orthop (Belle Mead NJ) 2007;36:591–593. [PubMed] [Google Scholar]
- 17.Wenger DE, Kendell KR, Miner MR, Trousdale RT. Acetabular labral tears rarely occur in the absence of bony abnormalities. Clin Orthop Relat Res. 2004;(426):145–150. doi: 10.1097/01.blo.0000136903.01368.20. [DOI] [PubMed] [Google Scholar]
- 18.Byrd JWT, Phillips JC. Hip tears of the acetabular labrum. In: Volpi P, editor. Arthroscopy and sport injuries. Cham: Springer; 2016. [Google Scholar]
- 19.Briggs K, Philippon M, Ho C, McNamara S. Prevalence of acetabular labral tears in asymptomatic young athletes. Br J Sports Med. 2017;51:303. [Google Scholar]
- 20.Dangin A, Tardy N, Wettstein M, May O, Bonin N. Microinstability of the hip: a review. Orthop Traumatol Surg Res. 2016;102(8S):S301–S309. doi: 10.1016/j.otsr.2016.09.002. [DOI] [PubMed] [Google Scholar]
- 21.Safran MR. Microinstability of the hip-gaining acceptance. J Am Acad Orthop Surg. 2019;27:12–22. doi: 10.5435/JAAOS-D-17-00664. [DOI] [PubMed] [Google Scholar]
- 22.Beck M, Kalhor M, Leunig M, Ganz R. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br. 2005;87:1012–1018. doi: 10.1302/0301-620X.87B7.15203. [DOI] [PubMed] [Google Scholar]
- 23.Robertson WJ, Kadrmas WR, Kelly BT. Arthroscopic management of labral tears in the hip: a systematic review of the literature. Clin Orthop Relat Res. 2007;455:88–92. doi: 10.1097/BLO.0b013e31802c7e0f. [DOI] [PubMed] [Google Scholar]
- 24.Reurink G, Jansen SP, Bisselink JM, Vincken PW, Weir A, Moen MH. Reliability and validity of diagnosing acetabular labral lesions with magnetic resonance arthrography. J Bone Joint Surg Am. 2012;94:1643–1648. doi: 10.2106/JBJS.K.01342. [DOI] [PubMed] [Google Scholar]
- 25.Narveson JR, Haberl MD, Nathan Vannatta C, Rhon DI. Conservative treatment continuum for managing femoroacetabular impingement syndrome and acetabular labral tears in surgical candidates: a case series. Int J Sports Phys Ther. 2018;13:1032–1048. [PMC free article] [PubMed] [Google Scholar]
- 26.Potter BK, Freedman BA, Andersen RC, Bojescul JA, Kuklo TR, Murphy KP. Correlation of Short Form-36 and disability status with outcomes of arthroscopic acetabular labral debridement. Am J Sports Med. 2005;33:864–870. doi: 10.1177/0363546504270567. [DOI] [PubMed] [Google Scholar]
- 27.Ayeni OR, Adamich J, Farrokhyar F, et al. Surgical management of labral tears during femoroacetabular impingement surgery: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2014;22:756–762. doi: 10.1007/s00167-014-2886-8. [DOI] [PubMed] [Google Scholar]
- 28.Sankar WN, Nevitt M, Parvizi J, Felson DT, Agricola R, Leunig M. Femoroacetabular impingement: defining the condition and its role in the pathophysiology of osteoarthritis. J Am Acad Orthop Surg. 2013;21 Suppl 1:S7–S15. doi: 10.5435/JAAOS-21-07-S7. [DOI] [PubMed] [Google Scholar]
- 29.Thier S, Gerisch D, Weiss C, Fickert S, Brunner A. Prevalence of cam and pincer deformities in the X-rays of asymptomatic individuals. Biomed Res Int. 2017;2017:856232. doi: 10.1155/2017/8562329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Beall DP, Sweet CF, Martin HD, et al. Imaging findings of femoroacetabular impingement syndrome. Skeletal Radiol. 2005;34:691–701. doi: 10.1007/s00256-005-0932-9. [DOI] [PubMed] [Google Scholar]
- 31.Griffin DR, Dickenson EJ, O'Donnell J, et al. The Warwick Agreement on femoroacetabular impingement syndrome (FAI syndrome): an international consensus statement. Br J Sports Med. 2016;50:1169–1176. doi: 10.1136/bjsports-2016-096743. [DOI] [PubMed] [Google Scholar]
- 32.Nwachukwu BU, Rebolledo BJ, McCormick F, Rosas S, Harris JD, Kelly BT. Arthroscopic versus open treatment of femoroacetabular impingement: a systematic review of medium- to long-term outcomes. Am J Sports Med. 2016;44:1062–1068. doi: 10.1177/0363546515587719. [DOI] [PubMed] [Google Scholar]
- 33.Wall PD, Fernandez M, Griffin DR, Foster NE. Nonoperative treatment for femoroacetabular impingement: a systematic review of the literature. PM R. 2013;5:418–426. doi: 10.1016/j.pmrj.2013.02.005. [DOI] [PubMed] [Google Scholar]
- 34.Bracken J, Tran T, Ditchfield M. Developmental dysplasia of the hip: controversies and current concepts. J Paediatr Child Health. 2012;48:963–972. doi: 10.1111/j.1440-1754.2012.02601.x. quiz 972-3. [DOI] [PubMed] [Google Scholar]
- 35.Klaue K, Durnin CW, Ganz R. The acetabular rim syndrome. A clinical presentation of dysplasia of the hip. J Bone Joint Surg Br. 1991;73:423–429. doi: 10.1302/0301-620X.73B3.1670443. [DOI] [PubMed] [Google Scholar]
- 36.Harris WH. Etiology of osteoarthritis of the hip. Clin Orthop Relat Res. 1986;(213):20–33. [PubMed] [Google Scholar]
- 37.Solomon L. Patterns of osteoarthritis of the hip. J Bone Joint Surg Br. 1976;58:176–183. doi: 10.1302/0301-620X.58B2.932079. [DOI] [PubMed] [Google Scholar]
- 38.Gala L, Clohisy JC, Beaulé PE. Hip dysplasia in the young adult. J Bone Joint Surg Am. 2016;98:63–73. doi: 10.2106/JBJS.O.00109. [DOI] [PubMed] [Google Scholar]
- 39.Nötzli HP, Müller SM, Ganz R. [The relationship between fovea capitis femoris and weight bearing area in the normal and dysplastic hip in adults: a radiologic study] Z Orthop Ihre Grenzgeb. 2001;139:502–506. doi: 10.1055/s-2001-19231. German. [DOI] [PubMed] [Google Scholar]
- 40.James S, Miocevic M, Malara F, Pike J, Young D, Connell D. MR imaging findings of acetabular dysplasia in adults. Skeletal Radiol. 2006;35:378–384. doi: 10.1007/s00256-006-0082-8. [DOI] [PubMed] [Google Scholar]
- 41.Ganz R, Klaue K, Vinh TS, Mast JW. A new periacetabular osteotomy for the treatment of hip dysplasias. Technique and preliminary results. Clin Orthop Relat Res. 1988;(232):26–36. [PubMed] [Google Scholar]
- 42.Koulouvaris P, Stafylas K, Aznaoutoglou C, Zacharis K, Xenakis T. Isolated varus intertrochanteric osteotomy for hip dysplasia in 52 patients: long-term results. Int Orthop. 2007;31:193–198. doi: 10.1007/s00264-006-0164-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hospital for Special Surgery. Hip conditions: chondral lesions or injuries. New York: HSS; [cited 2019 Feb 23]. Available from: https://www.hss.edu/hip-pain-center-hip-conditions.asp#4. [Google Scholar]
- 44.Yen YM, Kocher MS. Chondral lesions of the hip: microfracture and chondroplasty. Sports Med Arthrosc Rev. 2010;18:83–89. doi: 10.1097/JSA.0b013e3181de1189. [DOI] [PubMed] [Google Scholar]
- 45.Meyers MH. Resurfacing of the femoral head with fresh osteochondral allografts. Long-term results. Clin Orthop Relat Res. 1985;(197):111–114. [PubMed] [Google Scholar]
- 46.Fontana A, de Girolamo L. Sustained five-year benefit of autologous matrix-induced chondrogenesis for femoral acetabular impingement-induced chondral lesions compared with microfracture treatment. Bone Joint J. 2015;97:628–635. doi: 10.1302/0301-620X.97B5.35076. [DOI] [PubMed] [Google Scholar]