Abstract
Background
We aimed to assess the dose needed to achieve the propofol effect-site concentration using target-controlled infusion in intellectually disabled patients and to detail the most effective method for achieving a safe level of consciousness without hemodynamic changes as well as detail any resulting adverse effects.
Methods
We performed a retrospective review of sedation service records of 138 intellectually disabled patients (51, mental retardation; 36, autism; 30, brain lesion, 12 genetic diseases, 9 dementia) aged over 15 years and weighing over 30 kg. These patients had received propofol via target-controlled infusion in the special care dental clinic of Seoul National University Dental Hospital from May 2008 to September 2018 for restorative treatment (112), minor surgery (13), prosthodontics (7), periodontics treatment (5), and implant (1).
Results
For all groups, the duration of dental treatments was 43 ± 18 minutes, total sedation time was 73 ± 23 minutes, and total BIS values was 57 ± 12. The propofol maintenance dosage values for each group were: mental retardation, 3 ± 0.5 (2–4) µg/ml; autism, 3.1 ± 0.7 (2–5) µg/ml; brain lesion, 2.8 ± 0.7 (1.5–5) µg/ml; genetic disease, 2.9 ± 0.9 (1–4) µg/ml; and dementia 2.3 ± 0.7 (1–3.4) µg/ml.
Conclusions
The dementia group needed a lower dosage to reach a safe, effective propofol effect-site concentration than the other groups. Since there were no complications, deep sedation is a great alternative to general anesthesia for dental treatment of intellectually disabled patients.
Keywords: Bispectral Index, Deep Sedation, Dental Treatment, Intellectual Disability, Propofol, Target Control Infusion
INTRODUCTION
The lack of oral health in disabled patients is one of the biggest problems in the dental area, the prevalence and severity of oral diseases are higher than other groups of people in general, since there are many factors that influence this deficit of oral care like: low physical skills or reasoning to understand the importance of oral health and the type of pharmacological treatment that is being administered, this must be added that most oral care depends on their caregivers [1]. All these characteristics increase the time and lack quality of dental treatment because individuals cannot attend to their oral health, also these individuals frequently refuse dental treatment and cooperate, because the anxiety or fear [2]. Thereby, one of the main purposes of providing anesthesia for patients with intellectually impairment is to establish and maintain a state of cooperation and to reduce the risk of some complication as well as to provide a treatment without pain, which would reduce the fear and the anxiety to the dental treatment [3].
Today, many associations such as the ADA (American Dental Association), ADSA (American Dental Society of Anesthesiology), KDSA (The Korean Dental Society of Anesthesiology), among others, have proposed a series of guidelines for safety procedure of sedation according to the degree of depth and also for anesthesia, these guidelines, the advancement of technology, the amount of information and continuing education for dentists has helped to improve the conditions of private clinics that has allowed the use of outpatient general anesthesia and sedation by highly qualified dentist and fulfilling the requirements according to the guidelines of your country of residence [4]. It has been shown that deep sedation is recommended for disabled patients who are difficult to treat and allows a better management of the patient, since the patient is in a state of reduced body movement and responding only to painful or repeated stimuli, which make the dental treatment comfortable for the dentist as the patient [5].
Among the drugs used for sedation, propofol is one of the most popular intravenous anesthetic agents in modern medicine, both for general anesthesia and sedation [6]. Propofol has an onset of action: 30–45 seconds and a duration of between 3 and 10 minutes (the dissipation is a function of redistribution of the CNS drug); Metabolized by hepatic conjugation to inactive compound and excreted for the most part in urine has a half-life of 40 minutes. Due to these characteristics, propofol has many advantages over other anesthetics such as: providing a faster anesthetic induction, a recovery of less time, therefore, this allows an earlier discharge of the patient and a faster recovery of the neurological functions and social, less postoperative nausea and vomiting (PONV) and emergency delirium [7]. These characteristics can improve thanks to the advance in the intravenous anesthetic techniques that has conceived the development of the target controlled infusion (TCI) that have demonstrated efficacy and safety in the anesthetic maintenance through different pharmacological models that permit to achieve the peak effect of the drug, helped with the bispectral index (BIS) that, while we are titrating an specific anesthetic agents, this allows the anesthetist to adjust the amount of anesthetic agent needed, resulting in a more rapid awaking from anesthesia, also, help to avoid a state of over sedation or any cardiopulmonary complication.
However, it is difficult to evaluate and maintain an adequate depth of sedation in patients with severe intellectual disability due to the different communication difficulties and sometimes may have other medical disease, for this reason these patients may be more sensitive to sedative such propofol. Therefore, because of this, the sedative dose needed for an adequate depth of sedation cannot be estimated in patients with intellectual disability, this makes sedation sometimes higher than expected, which sometimes delays the recovery, also there are probabilities of a respiratory tract obstruction and an overdose of propofol [8].
Therefore, there are advantages of propofol as a sedative agent and its titration through TCI with the help of BIS during the sedation process, which allows monitoring of changes in the level of consciousness and allows maintenance of stable doses and attainment of the effect-site concentration; thus, help to preventing any complications while performing the dental treatment. Given this, there is a need for further investigation of deep sedation with propofol in intellectually disabled patients to improve the quality of dental care for these patients.
We aimed to provide data regarding the dose needed to achieve the propofol effect-site concentration using TCI in these patients. Moreover, we aimed to detail the effective method for achieving a safe level of consciousness without hemodynamic change as well as detail any occurring adverse effects. This study provides clinically useful data on patients with different types of intellectual impairments undergoing deep sedation during dental treatment. Although, we assessed whether there were differences in the dose necessary to achieve the site effect concentration among the different mental illness groups.
MATERIALS AND METHODS
This study was approved by the IRB No. S-D20190002 of Seoul National University School of Dentistry. We performed a retrospective review of sedation service records of intellectually disabled patients aged above 15 years and weighing over 30 kg. We reviewed all the charts of patients receiving propofol via TCI for deep sedation in the special care dental clinic of Seoul National University Dental Hospital from May 2008 to September 2018.
1. Patients
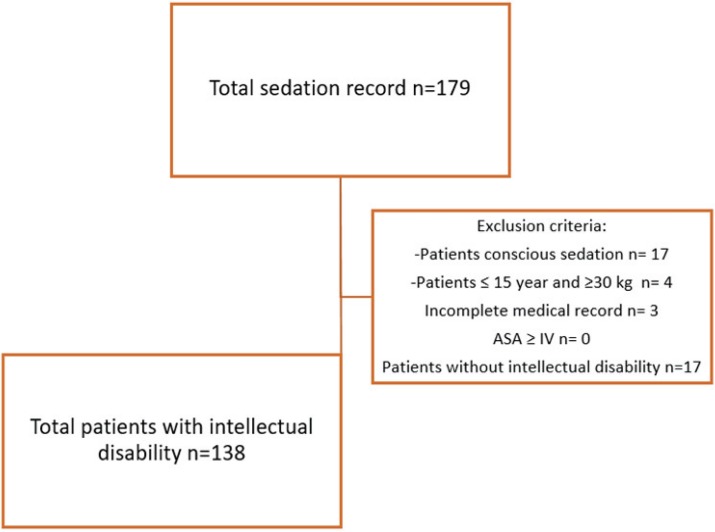
The databases were examined to identify all patients who underwent in deep sedation, we included all the records of patients with intellectual disability over the age of 15 years and receiving propofol using TCI for dental treatment in the Special care clinic for patients with Intellectual impairment, resulting 138 patients attended at Seoul National University Dental Hospital, from May 1, 2008 to September 30, 2018 (Fig. 1).
Fig. 1. Population flow chart.
Inclusion criteria were:
Age ≥ 15 years
American Society of Anesthesiologists (ASA) physical status ≤ III
Weight ≥ 30 kg
Intellectually disabled patients receiving dental treatment (restorative, endodontic, periodontics, minor surgery, dental extraction, and prosthodontics)
Intellectually disabled patients not fully cooperating with dental treatment. In addition, some of these patients had a history of seizures and were receiving anticonvulsant medication.
Exclusion criteria were as follows:
Patients who underwent conscious sedation.
Patients with an ASA status > IV and an uncontrolled or severe medical condition (uncontrolled epilepsy, uncontrolled heart disease, and any other uncontrolled chronic disease).
Patients with incomplete medical records.
2. Propofol administration using TCI
Once disabled patient was admitted to outpatients, an anesthetist and dentist surgeon performed an anesthetic pre-treatment evaluation. The appointment day, the anesthetist informed the patient's guardian all the recommendations regarding indication after procedure and also provided details about the deep sedation procedure (possible risks and post-anesthetic care). The anesthetist properly inserted an intravenous catheter in cooperative patients and administered any other sedative drugs or performed sevoflurane induction in uncooperative patients. Propofol was infused using the Orchestra TCI apparatus (Base Primia, Fresinius Kabi, France) with Schnider's pharmacokinetic model. The initial propofol effect-site target concentration was selected according to each patient's medical condition.
All the patient was monitored with noninvasive arterial blood pressure, ECG, pulse oximetry, carbon dioxide capnography, respiratory monitoring unit, and BIS (Bispectral index) monitors. To provide an adequate deep sedation state, the anesthetist titrated the effect target concentration of propofol according to the state of unconsciousness through BIS, patient stimulus response and vital signs monitoring according to condition of dental treatment. To maintain airway patency and avoid respiratory distress, we provided 3–5 liters/min of oxygen through the nasal cannula. Airway intervention was applied when necessary.
After finalization of the dental procedure, propofol infusion was stopped and the patient was moved to the Post Anesthetic Care Unit (PACU). Here, the patient was kept under observation to identify and address any adverse post anesthetic effects. In addition, the patient received oxygen therapy through a mask with a reservoir of 5–6 liters of oxygen for 10 to 15 minutes to prevent a hypoxic state while the patient regained consciousness before being discharged from the clinic.
3. BIS Monitor setting
To monitor the patients' consciousness while under deep sedation, all the patients were monitored for BIS scores using the BIS VISTA Monitoring System (Covidien, Mansfield, MA, USA) and a specific BIS Quatro Sensor (Aspect Medical Systems, Newton, Massachusetts, USA). The front sensor was placed on each patient's forehead according to the manufacturer's guidelines and connected to a BIS Vista monitor. During the procedure, BIS scores, which indicate a patient's arousal state as a score of 0-100 points, were monitored continuously and recorded every 10 minutes to prevent complications associated with overdosing and maintain proper sedation depth. We adjusted the propofol dose according to the value on the BIS scale.
4. Data Analysis
We analyzed medical records of all the enrolled patients, and obtained details on: types of mental impairment, propofol titration (changes in target concentration, duration of each change, and total infusion duration), vital signs, total sedation duration, dental treatment type, duration of dental treatment, complications during sedation, and other induction drugs administrated. Based on these records, we grouped the patients according to the type of intellectual disability (autism, mental retardation, dementia, genetic disease, and brain lesion). We also obtained basic patient demographic information, e.g., gender, age, weight, height, and any other organ complication.
Moreover, from these records, we obtained the following information regarding propofol:
1) Initial propofol target concentration.
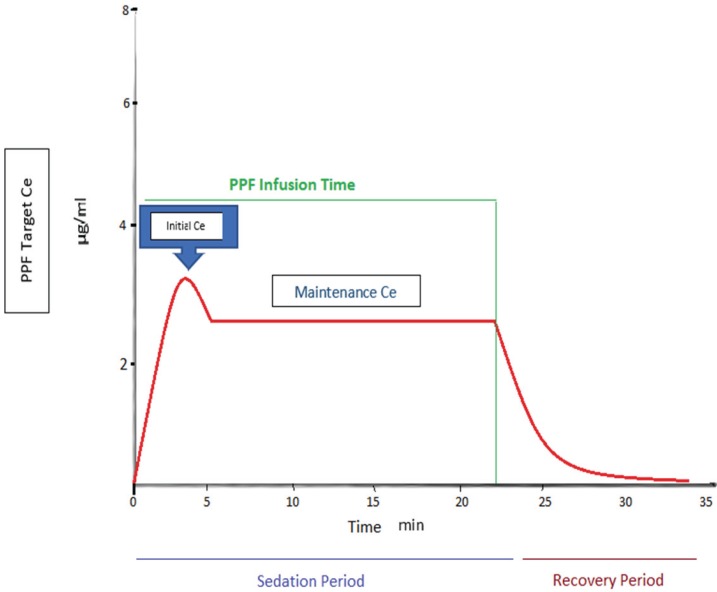
2) Changes in propofol effect-site concentration during the dental treatment period, which was obtained by reviewing the chart of each patient (Fig. 2).
Fig. 2. Propofol effect site concentration evaluation of change according time variables (Effect-site concentration (Ce)), initial Ce stands for an initial set target concentration in effect-site, Maintenance Ce means effect-site target concentration during dental treatment procedure with the patient in a state of immobilization with no side effect.
3) Duration of the stable propofol dose.
The initial effect-site concentration allows quick achievement of a therapeutic concentration while the maintenance effect-site concentration maintains the propofol pharmacological effect and allows dental treatment that is uninterrupted, less painful, more comfortable for the patient, and without secondary effects.
4) Total propofol infusion time and total dosage evaluation
5) Adverse effects that occurred during sedation.
6) Type and duration of dental treatment
7) Hemodynamic information during the intraoperative period.
8) Depth of sedation according to the BIS information.
9) Administration of additional sedation drugs and emergency aid.
5. Statistical analysis
We included both descriptive and analytical data. All the data were analyzed using SPSS version 25 for Windows (SPSS Inc., USA) software and expressed as means ± SD. P < 0.05 was considered statistically significant. We used repeated-measures analysis of variance (ANOVA) to compare the propofol infusion dosage in each impairment group (group and propofol TCI factors), and LSD multiple comparison post hoc test to compare the propofol steady/mean values among the groups.
RESULTS
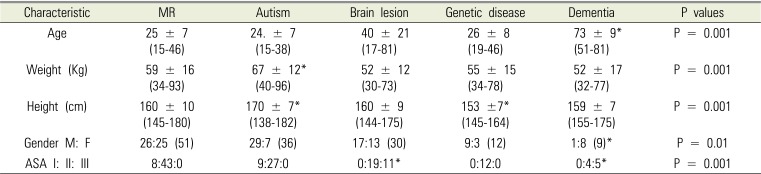
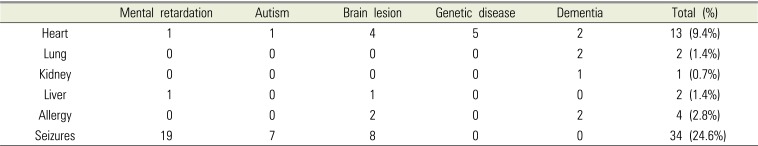
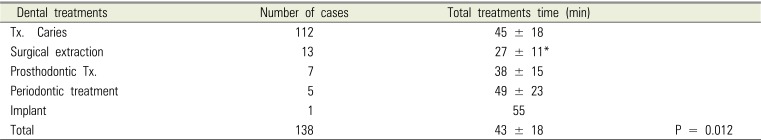
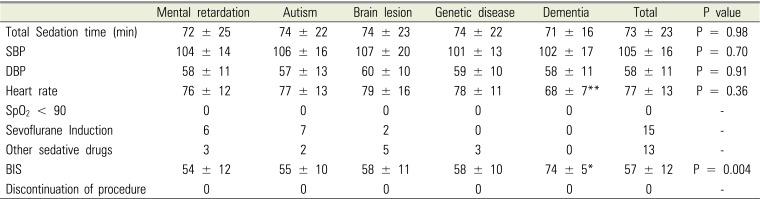
Basic demographical data (gender, weight, height, and ASA classes) for each group are shown in Table 1. Patients in the dementia group had a significantly older age (P < 0.05) than those in the other groups. In addition, patients in the autism group had significantly higher weight and height (P < 0.05) than those in the other groups. The clinical records also revealed organ complications in some patients with problems involving the lungs, kidneys, heart, allergies, and seizures. Patients with these organ complications accounted for 10 percent of the enrolled patients (see on Table 2); however, they did not present a high-risk factor for not performing the sedation procedure. The patients underwent different dental treatments according to their diagnosis as follows: 112 restoratives (caries treatment), 13 minor surgeries (tooth extraction), 7 prosthodontics, 5 periodontics treatments, and 1 implant; the total duration of the dental treatments was 43 ± 18 minutes (Table 3). For all the groups, the total sedation time was 73 ± 23 minutes and the total of the BIS values was 57 ± 12; other parameters are shown in Table 4 based on the intellectual disability type and include: systolic blood pressure, diastolic blood pressure, heart rate, pulse oximetry < 90, other sedative drugs, sevoflurane induction, and discontinuation of the procedure. From these records, there were no abnormal hemodynamic values indicating complications during the procedure, 15 patients received sevoflurane induction, and 13 patients received another sedative drug during the procedure. These findings affirm that the sedation procedure was successful and allowed completion of the dental treatments.
Table 1. Patients' demographic characteristics.
Values are mean ± SD.
*Mean statistically significant than the other groups (P < 0.05). MR; Mental retardation.
Table 2. Comorbidities involved.
Other complications that patients present according to each group. Values are mean ± SD.
Table 3. Dental Treatments according to clinical Diagnostic.
Tx. = Treatment
Data values are Means ± SD.
*Mean statistically significant than the other groups (P < 0.05).
Table 4. Sedation Values.
Systolic blood pressure (SBP), Diastolic blood pressure (DBP), Pulse oximetry (SPO2). We established that pulse oximetry values of less than 90 represent a hypoxic condition of the patient, which is why they were taken as complications within the time of sedation. BIS (Bispectral index score). Values are Means ± SD.
*Mean statistically significant than the other groups (P < 0.05).
**Dementia < Brain lesion post hoc test (LSD P < 0.045)
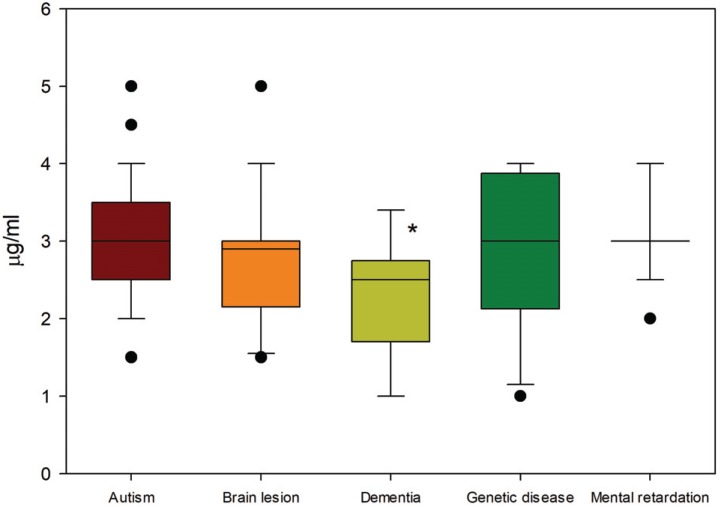
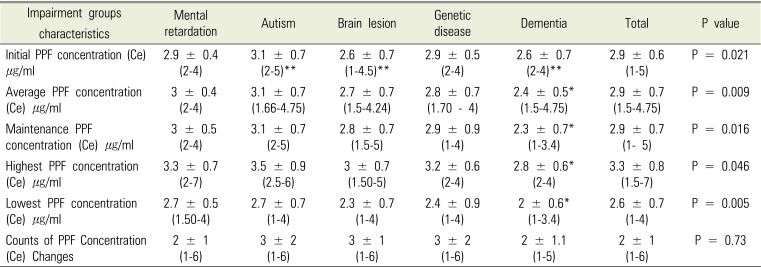
Regarding data on propofol infusion using TCI, the initial propofol dose in each group was: mental retardation, 2.9 ± 0.4 (2–4) µg/ml; autism 3.1 ± 0.7 (2–5) µg/ml; brain lesion, 2.6 ± 0.7 (1–4.5) µg/ml; genetic disease, 2.9 ± 0.5 (2–4) µg/ml; and dementia, 2.6 ± 0.7 (2–4). ANOVA revealed significant differences (P < 0.05) in the dose needed for propofol effect-site concentration, with post hoc LSD analysis showing that patients in the autism group needed higher doses than those in the brain lesion and dementia groups. Regarding the propofol maintenance dosage, the values for each group were: mental retardation, 3 ± 0.5 (2–4) µg/ml; autism, 3.1 ± 0.7 (2–5) µg/ml; brain lesion, 2.8 ± 0.7 (1.5–5) µg/ml; genetic disease, 2.9 ± 0.9 (1–4) µg/ml; and dementia, 2.3 ± 0.7 (1–3.4) µg/ml. The dementia group required a significantly lower dose than the other groups. Fig. 3 shows the maintenance propofol effect-site concentrations in each group, presented median and range as box plots. Table 5 shows the other propofol infusion data according to the group with P value.
Fig. 3. Maintenance effect-site concentration of propofol among the groups. *: P < 0.05 post hoc LSD.
Table 5. Propofol Target Infusion Status.
PPF = Propofol
Values are Means ± SD and ANOVA test P < 0.05 consider like statistically significant.
*Mean statistically significant than the other groups (P < 0.05).
**Induction dose : autism group > brain lesion and dementia group with post hoc test (LSD P < 0.05).
DISCUSSION
Patients with a disability arrived at the dental clinic with deplorable oral health due to either lack of self-reasoning capacity, motor coordination, or medications that mitigate problems related to the increase of oral affections; therefore, good clinical management of these patients is required for successful dental treatment completion. Since these patients are more sensitive to high-stress situations, the use of appropriate anesthesia techniques is recommended.
The implementation of anesthesia provides optimal conditions for dental treatment for disabled patients, so additional care must be taken based on their physical and mental conditions. It is necessary to execute an individualized anesthetic plan and a good teamwork between the dentist and the dental anesthesiologist to get a procedure without any kind of altercations and conclude satisfactorily. Sedation can be classified according to the depth required by the treatment as mild, moderate and deep with respect to their levels of consciousness and the ability to maintain ventilation and cardiovascular functions; then have general anesthesia that is the complete loss of consciousness with incapacity to maintain ventilation and cardiovascular functions [9].
Conscious sedation was the goal of a level of sedation, since the patient can respond to any verbal or tactile stimulus; However, in the case of patients with disabilities who have low levels of cooperation and high levels of anxiety, this type of conscious sedation has a lower success rate [10]. Therefore, the use of deep sedation or general anesthesia in these patients is more suitable for performing dental procedures, therefore, for the selection of which kind anesthetic technic perform we should be taken the risk-benefit factor [11].
The objectives of the deep sedation in patients with intellectual disability are: reduce the patient's anxiety and fear of treatment, decrease the pain sensation making the treatment more comfortable for the patient and in turn produce amnesia during the procedure, also increase the patient's tolerance in those long-term procedures, avoid the risks associated with general anesthesia and achieve a rapid recovery, in addition compared to general anesthesia, less postoperative complications [12]. Moreover, deep sedation is performed to reduce patient movement owing to a lack of cooperation in which dental treatment cannot be carried out with minimal sedation. Deep sedation can be easily and safely achieved intravenously by the ease of handling the doses as we can titrate to achieve the desired effect, among the most commonly used sedative drugs like benzodiazepines between this one, we have midazolam which is considered the drug most commonly used to induce sedation in dental procedures [13]. Despite the sedative, hypnotic, anxiolytic, amnesic, and muscle relaxant effects of midazolam, it has been reported to produce delayed recovery in patients with disabilities after treatment completion. Therefore, given the peculiar pharmacological characteristics of propofol, it is more suitable for deep sedation because sedation can be performed safely and effectively in a dental office setting to patients with disabilities [14].
Advances in intravenous drug delivery techniques have permitted the development of the TCI system, whereby drugs are delivered to reach and sustain specific effect-site drug concentrations. With the assistance of TCI system is possible to adjust and maintain the effect site concentration (Ce) of drugs incorporated in the system. Studies such as J Mu, et al (2018) concludes and demonstrates that the use of TCI allows high doses of propofol to be achieved without causing a prolonged recovery and that it makes the titration method of propofol easier in anesthesia or sedation [15]. As this result, TCIs have begun to be widely used to administer propofol for sedation in various settings, including endoscopy, bronchoscopy, and dental procedures [16]. However, sometimes complications may also arise during or after treatment such as obstruction of the respiratory tract, cardiovascular and respiratory depression, nausea, vomiting, fainting, among others that may appear as side effects. However, there are also studies that show us the effectiveness of both TCI and BIS together to achieve adequate sedation of the patient in an effective and safe way without complications of overdose during the dental procedure [2].
In our study, the dentists were able to successfully complete the different kinds of dental treatment without any intraoperative complications, e.g., hemodynamic changes, hypoxia, interruption of the procedure, etc. The total duration of the different treatments was around one hour, which made the implementation of deep sedation in these patients possible because the treatment time was not too long. Moreover, the local anesthesia technique made the dental treatments less uncomfortable for the patients and since most of the patients were suitable to undergo this procedure since they were in ASA classification II.
Regarding the sedation process, we found significant among-group differences in the dose required to reach effect-site concentrations, with the dementia group requiring significantly lower doses. Futhermore, regarding the induction dosage, the dementia and brain lesion groups required slightly lower propofol doses compared with the autism group. This is because patients in the brain lesion and dementia groups are more sensitive to propofol. Moreover, our study found that the propofol dose required for achieving the propofol maintenance effect-site concentration in patients in the dementia group was lower than for those in the other groups. It has been previously reported that intellectually disabled patients in the dental environment required lower doses (1.0 – 5.0 mcg/ml) to achieve effect-site concentration using titration of the target concentration than those without intellectual disabilities [8]. Another study reported that noncommunicative/nonverbal children with cerebral palsy required lower propofol doses (3.29 mg/kg) than otherwise healthy children [17] ; although, none of these studies compared the required dose between patients with different types of intellectual impairment. However, a study has reported that the propofol dose required for an anesthesia procedure is not affected by the type of intellectual disability but rather by the antiepileptic used and consumption time, since this has been shown to cause patients to become more sensitive to sedative drugs [18].
There are different types of dementia but most of these patients suffer from Alzheimer's disease where they present symptoms like depression and delirium that get worse over time, which is compounded by the advanced age of these patients [19]. Patients with dementia usually take antidepressants or low-dose antipsychotics, which induce a higher sensitivity to sedatives. Moreover, they might receive antiepileptic drugs for their neurological disorders, which make them even more susceptible since it has been demonstrated that antiepileptic drugs diminish hepatic metabolism [20]. In addition, given the multiple comorbidities presented by patients with dementia, the doses of sedatives, such as propofol, tend to be low. Given these reasons, we need to be more caution during sedation procedures through continuous monitoring of vital signs [21] and good preoperative evaluation to achieve the best possible postoperative outcome [22]. Given the conditions of these patients, they might develop postoperative delirium due to the sedative agents used. However, as reported by S. Alcorn et al, 2017, this can be prevented by avoiding benzodiazepines and anticholinergic drugs, careful titration of both volatile and IV anesthetic agents, and ensuring effective multimodal postoperative analgesia [23].
With these factors taken into account, it can be ascertained that deep sedation can be successfully implemented in intellectually disabled patients as an alternative to general anesthesia. This can be guaranteed by always taking into account the patient's medical conditions and safety guidelines for the sedation procedure. Moreover, teamwork between the dentist and anesthetist is an important point to consider to successfully carrying out any procedure, and communication between both professionals is key. Moreover, for successful implementation, an individualized plan for each patient, based on their specific conditions, must be developed [8].
In conclusion, the dosage to reach safe effective propofol effect-site concentration (Ce) was lower in the group of dementia in compared with the other intellectual disability types. Since there were no complications of any kind we can say that deep sedation is a great alternative to general anesthesia in patients with intellectual disabilities for dental treatments taking into account the time factor.
Footnotes
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.
References
- 1.Altun C, Guven G, Akgun OM, Akkurt MD, Basak F, Akbulut E. Oral health status of disabled individuals attending special schools. Eur J Dent. 2010;4:361–366. [PMC free article] [PubMed] [Google Scholar]
- 2.Sakaguchi M, Higuchi H, Maeda S, Miyawaki T. Dental sedation for patients with intellectual disability: a prospective study of manual control versus bispectral index-guided target-controlled infusion of propofol. J Clin Anesth. 2011;23:636–642. doi: 10.1016/j.jclinane.2011.04.008. [DOI] [PubMed] [Google Scholar]
- 3.Caputo AC. Providing deep sedation and general anesthesia for patients with special needs in the dental office-based setting. Spec Care Dentist. 2009;29:26–30. doi: 10.1111/j.1754-4505.2008.00059.x. [DOI] [PubMed] [Google Scholar]
- 4.Corcuera-Flores JR, Delgado-Munoz JM, Ruiz-Villandiego JC, Maura-Solivellas I, Machuca-Portillo G. Dental treatment for handicapped patients; sedation vs general anesthesia and update of dental treatment in patients with different diseases. Med Oral Patol Oral Cir Bucal. 2014;19:e170–e176. doi: 10.4317/medoral.19555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chi SI, Kim HJ, Seo KS, Yang M, Chang J. Use of ADMS™ during sedation for dental treatment of an intellectually disabled patient: A case report. J Dent Anesth Pain Med. 2016;16:217–222. doi: 10.17245/jdapm.2016.16.3.217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Asahi Y, Kubota K, Omichi S. Dose requirements for propofol anaesthesia for dental treatment for autistic patients compared with intellectually impaired patients. Anaesth Intensive Care. 2009;37:70–73. doi: 10.1177/0310057X0903700101. [DOI] [PubMed] [Google Scholar]
- 7.Chidambaran V, Costandi A, D'Mello A. Propofol: A review of its role in pediatric anesthesia and sedation. CNS Drugs. 2015;29:543–563. doi: 10.1007/s40263-015-0259-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lee BS, Shin TJ, Kim HJ, Choi YJ, Lee SE, Chang J, et al. Effect site concentrations of propofol for dental treatment under deep sedation in intellectually disabled patients. J Korean Dent Soc Anesthesiol. 2014;14:167–172. [Google Scholar]
- 9.Wang YC, Lin IH, Huang CH, Fan SZ. Dental anesthesia for patients with special needs. Acta Anaesthesiol Taiwan. 2012;50:122–125. doi: 10.1016/j.aat.2012.08.009. [DOI] [PubMed] [Google Scholar]
- 10.Shin B, Yoo S, Kim J, Kim S, Kim J. A survey of dental treatment under general anesthesia in a korean university hospital pediatric dental clinic. J Dent Anesth Pain Med. 2016;16:203–208. doi: 10.17245/jdapm.2016.16.3.203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Messieha Z. Risks of general anesthesia for the special needs dental patient. Spec Care Dentist. 2009;29:21–25. doi: 10.1111/j.1754-4505.2008.00058.x. [DOI] [PubMed] [Google Scholar]
- 12.Morimoto Y, Hayashi M, Yokoe C, Kinugawa T, Iida T, Boku A, et al. Intravenous sedation for dental treatment in patients with intellectual disability-efficacy of nasal airway, pharyngeal suction tube and oxygen tube placement. Biomed Res (Aligarh) 2017;28:4931–4936. [Google Scholar]
- 13.Yoshikawa F, Tamaki Y, Okumura H, Miwa Z, Ishikawa M, Shimoyama K, et al. Risk factors with intravenous sedation for patients with disabilities. Anesth Prog. 2013;60:153–161. doi: 10.2344/0003-3006-60.4.153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Vaessen HH, Schouten AN, van der, Knape JT. The feasibility of office-based propofol sedation for dental care in patients with intellectual disability by sedation practitioners. Spec Care Dentist. 2017;37:93–98. doi: 10.1111/scd.12210. [DOI] [PubMed] [Google Scholar]
- 15.Mu J, Jiang T, Xu XB, Yuen VM, Irwin MG. Comparison of target-controlled infusion and manual infusion for propofol anaesthesia in children. Br J Anaesth. 2018;120:1049–1055. doi: 10.1016/j.bja.2017.11.102. [DOI] [PubMed] [Google Scholar]
- 16.Sheahan CG, Mathews DM. Monitoring and delivery of sedation. Br J Anaesth. 2014;113:ii37–ii47. doi: 10.1093/bja/aeu378. [DOI] [PubMed] [Google Scholar]
- 17.Saricaoglu F, Celebi N, Celik M, Aypar U. The evaluation of propofol dosage for anesthesia induction in children with cerebral palsy with bispectral index (BIS) monitoring. Paediatr Anaesth. 2005;15:1048–1052. doi: 10.1111/j.1460-9592.2005.01658.x. [DOI] [PubMed] [Google Scholar]
- 18.Ouchi K, Sugiyama K. Required propofol dose for anesthesia and time to emerge are affected by the use of antiepileptics: prospective cohort study. BMC Anesthesiol. 2015;15:34. doi: 10.1186/s12871-015-0006-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.So E, Kim HJ, Karm MH, Seo KS, Chang J, Lee JH. A retrospective analysis of outpatient anesthesia management for dental treatment of patients with severe Alzheimer's disease. J Dent Anesth Pain Med. 2017;17:271–280. doi: 10.17245/jdapm.2017.17.4.271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Patsalos PN, Fröscher W, Pisani F, van Rijn CM. The importance of drug interactions in epilepsy therapy. Epilepsia. 2002;43:365–385. doi: 10.1046/j.1528-1157.2002.13001.x. [DOI] [PubMed] [Google Scholar]
- 21.Johansen JW. Update on bispectral index monitoring. Best Pract Res Clin Anaesthesiol. 2006;20:81–99. doi: 10.1016/j.bpa.2005.08.004. [DOI] [PubMed] [Google Scholar]
- 22.Funder KS, Steinmetz J, Rasmussen LS. Anaesthesia for the patient with dementia undergoing outpatient surgery. Curr Opin Anaesthesiol. 2009;22:712–717. doi: 10.1097/ACO.0b013e328331a4eb. [DOI] [PubMed] [Google Scholar]
- 23.Alcorn S, Foo I. Perioperative management of patients with dementia. BJA Educ. 2017;17:94–98. [Google Scholar]