Abstract.
Infectious diarrhea cases have increased during the past years in the Anhui Province of China, but little is known about its spatial cluster pattern and associated socioeconomic factors. We obtained county-level total cases of infectious diarrhea in 105 counties of Anhui in 2016 and computed age-adjusted rates. Socioeconomic factors were collected from the Statistical Yearbook. Hot spot analysis was used to identify hot and cold spot counties for infectious diarrhea incidence. We then applied binary logistic regression models to determine the association between socioeconomic factors and hot spot or cold spot clustering risk. Hot spot analysis indicated there were both significant hot spot (29 counties) and cold spot (18 counties) clustering areas for infectious diarrhea in Anhui (P < 0.10). Multivariate binary logistic regression results showed that infectious diarrhea hot spots were positively associated with per capita gross domestic product (GDP), with an adjusted odds ratio (AOR): 3.51, 95% CI: 2.09–5.91, whereas cold spots clustering were positively associated with the number of medical staffs (AOR: 1.18, 95% CI: 1.08–1.29) and negatively associated with the number of public health physicians (AOR: 0.27, 95% CI: 0.09–0.86). We identified locations for hot and cold spot clusters of infectious diarrhea incidence in Anhui, and the clustering risks were significantly associated with health workforce resources and the regional economic development. Targeted interventions should be carried out with considerations of regional socioeconomic conditions.
INTRODUCTION
The Global Burden of Disease (GBD) 2016 reported that diarrheal diseases was the 4th leading cause group of total years of life losts,1 of the greatest burden to low-income people and children. Infectious diarrhea is a gastrointestinal infection that can be caused by a variety of pathogens, including bacteria, viruses, and protozoa, and it is usually transmitted through food or water contaminated with feces and person-to-person contact.2,3 Furthermore, 2016 GBD reported that for high-income countries and regions, outpatient visits and hospital admissions for acute infectious diarrhea posed a considerable burden to the health-care system.1
In China, the incidence of infectious diarrhea was the second highest only after respiratory diseases. Also, in Anhui Province, the number of commonly reported infectious diarrhea, which is other than cholera, dysentery, typhoid, and paratyphoid has risen since 2007, ranking as the second highest group among the C class–notifiable infectious diseases in terms of incidence and mortality.4
Previous studies had examined spatial patterns of diarrhea existed in different countries, such as in Vietnam5 and Thailand.6 In particular, spatial analyses had shown that childhood diarrhea did not occur randomly but rather clustered spatially in different geographical locations.3,7,8 Sociodemographic variables,9 personal hygiene,10 and environmental and climatic changing11–13 were considered to be the relevant factors for incidence of diarrhea. As time and space changes, the burden of diarrheal diseases on the health-care system continues to be a significant topic. Using geographic analysis methods, spatiotemporal scanning,3 and hot spot analysis methods9 we analyze changes in the temporal and spatial patterns of diseases and identify high-risk areas, to provide geographic-based evidence.
Yet, there are very few studies on the spatial cluster pattern for infectious diarrhea and associated socioeconomic factors in China. The present study attempted to use spatial hot spot analysis to identify county-level hot spots and cold spots for infectious diarrhea incidence in the Anhui Province of China, and examined associations between socioeconomic factors and hot spot or cold spot clustering risks, thus to provide information for appropriate allocation of health resources, better prevention, and control of infectious diseases.
MATERIALS AND METHODS
Study area.
Anhui Province is located in east China between long. 114°54′ and 119°37′E and lat. 29°41′ and 34°38′N, which consisted of 105 counties overall. It is located in a semihumid warm temperate and continental monsoon climate zone, with a rainy weather in summer seasons.14 Anhui Province had a population of about 60.8 million people (Department of Anhui provincial administration, 2015), which ranked the middle level of economic development across China and had a relatively high proportion of rural population (61.3%).14
Disease data.
In this study, cases of infectious diarrhea referred to the reported case data of “other infectious diarrheal diseases” as a C class–notifiable infectious disease, according to the law of the People’s Republic of China on Prevention and Treatment of Infectious Diseases (2013 Amendment), which was infectious diarrhea other than cholera, dysentery, typhoid, and paratyphoid. An infectious diarrhea case was diagnosed based on clinical diagnosis and/or etiological examination of diarrhea and according to diagnostic criteria for infectious diarrhea (WS271-2007, China).15
Infectious diarrhea surveillance dataset was obtained from Anhui Provincial CDC. All cases were reported by hospitals, clinics, and CDCs through the China’s National Notifiable Disease Surveillance System. Disease case information included age, gender, occupation, the onset date of infectious diarrhea, and family address. The records of 896 cases whose family addresses were registered outside Anhui Province or missing were excluded from the analysis. The final 89,578 cases of people with infectious diarrhea in 2016 were analyzed, of which 34,093 cases were children younger than 5 years. We aggregated the numbers of diarrheal cases for all population and for children younger than 5 years at the county level, respectively.
Demographic and socioeconomic variables.
We obtained the total population of each county and the population by age group in 2015 from Anhui Provincial CDC. We calculated crude incidence rate per 10,000 persons at the county level. Applying 2010 Census population data of Anhui Province16 as the standard population, we computed age-adjusted incidence rate using the direct method by dividing ages into under-five and other age groups.
Socioeconomic variables were selected based on previous research and data availability.14,17 We collected four socioeconomic factors in all 105 counties of Anhui in the year of 2015: population density (×100 persons/km2), per capita gross domestic product (GDP, ×10,000 renminbi [RMB]),18 number of medical staffs, including doctors and nurses (per 1,000 persons), and number of public health physicians (per 10,000 persons). Per capita GDP was a comprehensively representative indicator of social economy. Medical staffs, including doctors and nurses were the main health workforce for treating patients with infectious diseases, and public health physicians played an important role in preventing the transmission of infectious diseases. The population density was considered in the study because the population had an unevenly spatial distribution in different areas of Anhui Province, and population density was associated with infectious disease’s transmission. In general, because of the large mountainous area in the southern Anhui, the population density in the north was higher than that in the south.
Spatial analysis.
All cases’ count, rates, and socioeconomic variables were aggregated to the county level, and then we arranged county code for geocoding and linked with Anhui county shapefile. First, we created geographic information system (GIS) maps to show the initial spatial distribution of infectious diarrhea rates and age-adjusted rates, also for socioeconomic variables. Then, we conducted hot spot analysis using Getis-Ord Gi* statistics to identify the cluster locations of age-adjusted rates per 10,000 persons.19 The Getis-Ord Gi* hot spot analysis statistic itself was a z-score that followed a standard normal distribution, and the statistic could find and verify whether there was a high-value or a low-value clustering area in the spatial distribution. From the perspective of disease prevention and control and policy-making, the advantage of hot spot analysis was that it could describe specific geographic units according to statistically significant differences.9
Using ArcGIS 10.2 (ESRI, Redlands, CA), we conducted incremental spatial autocorrelation at 30 different distances and selected the distance at which rate clustering was most intense and z-score peaked. The spatial distance obtained was entered as a parameter in the subsequent Getis-Ord Gi* hot spot analysis. We used hot spot analysis to identify the locations of statistically significant clusters of counties with higher or lower values for infectious diarrhea incidence rates. In our study, a hot spot or cold spot was defined as a location with a statistically significant cluster of counties with higher or lower rates of diarrhea than the average rate for all counties in Anhui in 2016 (Getis-Ord Gi* at α = 0.10 significance level).20
Previously, Getis-Ord Gi* hot spot analysis had been used to target the locations of statistically significant clusters of sexually transmitted infections9 and hepatitis C virus infections.21 In these two studies, the regression analysis method was selected to explore the relationship between hot spots and regional characteristics.
Statistical analyses.
After identifying infectious diarrhea hot and cold spot counties, we conducted cluster categories. According to the clustering result of county whether it was a hot spot, we categorized counties into hot spots and non–hot spots group. Similarly, according to the clustering result of cold spots, we divided counties into cold spots and non–cold spots group. Then, applying binary logistic regression, we analyzed whether the socioeconomic factors were related to hot spot or cold spot clustering risks, respectively.
We conducted binary logistic regression analyses to find the factors that predisposed diseases to hot spots or cold spots clustering by SPSS 17.0 (IBM, Armonk, NY).21 First, we regressed clustering status on each of the socioeconomic variables. Second, we computed Spearman’s correlations among independent variables, also variance inflation factor for each variable to collinearity diagnosis and found that no variance inflation factors was more than 2. Then, we constructed multivariate binary logistic regression model to include all socioeconomic variables. We fitted binary logistic models by selecting the Logit link function and assessed the goodness of fit by χ2 statistics, pseudo-R2, in SPSS software. Applying the multivariate model, we could get the predicted category that had the maximum estimated probability and constructed cross tables to evaluate the accuracy of prediction classification.
RESULTS
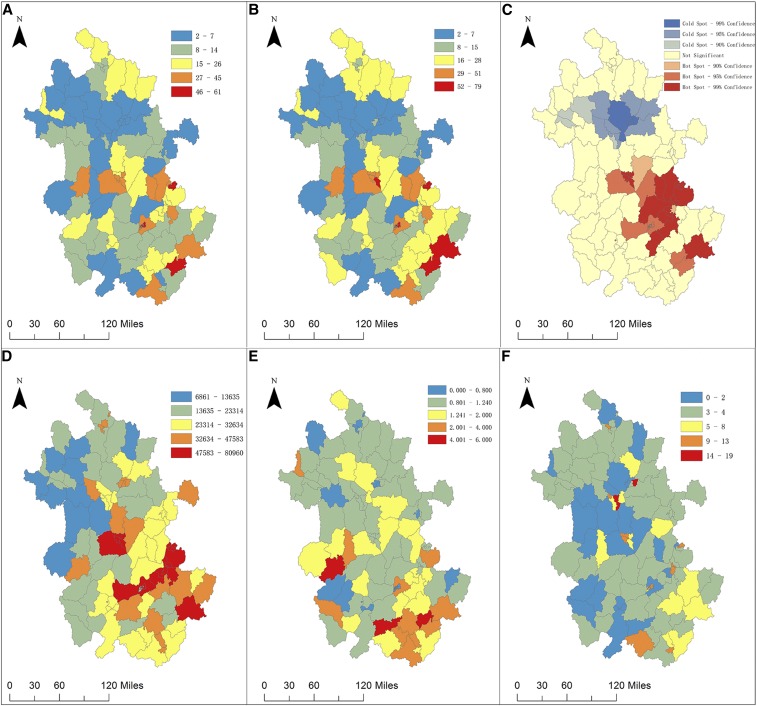
Descriptive maps figured the incidence rate, the age-adjusted rate of infectious diarrhea in 2016 across Anhui by counties (Figure 1A and B), indicating that southern and central counties had the larger initial disease burden. Figure 1D–F portrayed the spatial distributions for per capita GDP, proportions for number of public health physicians and number of medical staffs, respectively. We observed that GDP fell gradually from south-central to north and south, and number of public health physicians decreased from south to north. The proportion of medical staffs was generally low in Anhui, and the proportion seemed higher in small-area counties.
Figure 1.
Maps of county-level infectious diarrhea incidence and socioeconomic factors in 105 counties in the Anhui Province of China. (A): Crude incidence rate (1/10,000), (B): age-adjusted incidence rate (1/10,000), (C): hot and cold spots, (D): per capita GDP (RMB, ¥), (E): number of public health physicians per 10,000 persons, (F): number of medical staffs per 1,000 persons. This figure appears in color at www.ajtmh.org.
When conducting incremental spatial autocorrelation, the distance at which clustering of infectious diarrhea incidence was 47.3 km (z-score = 6.3, P < 0.001). Figure 1C showed the locations of statistically significant hot or cold spots clustering for age-adjusted rates. Red counties (n = 29, mainly in Hefei, Wuhu and Ma’anshan cities in Anhui) denoted significant hot spot clusters with higher age-adjusted rates of infectious diarrhea than the mean rate for all counties (P < 0.10). Yellow counties (n = 58) represented counties that had rates which were not significantly different from the mean rate. Blue counties (n = 18, mainly in Bengbu and Huainan cities in Anhui) denoted cold spots, indicating lower rates than the mean rate (P < 0.10).
In Table 1, descriptive statistics are shown for hot spots, cold spots, and nonsignificant clustering counties for infectious diarrhea. We noted the differences across socioeconomic variables among three different clusters of counties. Table 2 showed the Spearman’s correlation (r) between the independent variables. Per capita GDP was weakly positively correlated with population density (r = 0.264, P = 0.007) and number of medical staffs (r = 0.259, P = 0.010), respectively. Population density was negatively correlated with number of public health physicians (r = −0.557, P < 0.001).
Table 1.
Characteristics description for 105 counties in Anhui Province, China: Mean (95% CI)
| Characteristic | Counties in diarrhea cold spots (n = 18) | Counties of nonsignificant cluster (n = 58) | Counties in diarrhea hot spots (n = 29) |
|---|---|---|---|
| Demographic variables | |||
| Total population (×10,000) | 55.2 (40.0–70.4) | 67.6 (56.2–79.0) | 52.8 (40.7–64.9) |
| Under-five ages, % | 6.4 (5.2–7.5) | 5.7 (5.1–6.3) | 4.3 (4.0–4.7) |
| Diarrhea morbidity | |||
| Crude incidence rate (1/10,000) | 5.6 (3.5–7.7) | 13.5 (10.9–16.1) | 34.7 (26.8–42.7) |
| Age-adjusted incidence rate (1/10,000) | 5.5 (3.4–7.6) | 13.5 (10.9–16.1) | 34.7 (26.8–42.7) |
| Under-five cases, % | 43.5 (32.0–54.9) | 33.9 (28.0–39.7) | 40.7 (33.4–48.1) |
| Socioeconomic variables | |||
| No. of medical staffs (per 1,000 persons) | 5.4 (2.8–8.0) | 3.8 (3.2–4.4) | 4.8 (3.5–6.2) |
| No. of public health physicians (per 10,000 persons) | 1.0 (0.8–1.2) | 1.7 (1.3–2.1) | 1.7 (1.3–2.2) |
| Population density (×100 persons/km2) | 13 (7.7–18.3) | 7 (3.5–11.3) | 21 (8.9–33.2) |
| Per capita GDP, ¥ (×10,000 RMB) | 2.6 (2.2–3.0) | 2.4 (2.1–2.8) | 5.4 (4.7–6.1) |
Table 2.
Spearman’s correlations (r) between the socioeconomic factors
| Factors | Per capita GDP | Population density | No. of medical staffs | No. of public health physicians | |
|---|---|---|---|---|---|
| Per capita GDP | r | 1.000 | 0.264 | 0.259 | 0.046 |
| P | – | 0.007 | 0.010 | 0.654 | |
| Population density | r | 0.264 | 1.000 | 0.167 | -0.557 |
| P | 0.007 | – | 0.099 | 0.000 | |
| No. of medical staffs | r | 0.259 | 0.167 | 1.000 | 0.080 |
| P | 0.010 | 0.099 | – | 0.446 | |
| No. of public health physicians | r | 0.046 | −0.557 | 0.080 | 1.000 |
| P | 0.654 | 0.000 | 0.446 | – | |
Results of univariate analyses of binary logistic regression model were shown in Table 3. For hot spots compared with non–hot spots, two socioeconomic variables, population density and per capita GDP, were positively related to hot spots clustering with odds ratios (OR) > 1, P < 0.05. Results meant that the larger the value of these independent variables, the more likely it would become the hot spot clustering area of infectious diarrhea. For cold spots compared with non–cold spots, two socioeconomic variables, number of medical staffs and number of public health physicians, were associated with cold spot clustering (OR 0.28 and 1.09, respectively).
Table 3.
Associations between socioeconomic factors and diarrheal hot spots or cold spots in Anhui, China
| Variables | Hot spots | Cold spots | ||
|---|---|---|---|---|
| Univariate model OR (95% CI) | Multivariate model AOR (95% CI) | Univariate model OR (95% CI) | Multivariate model AOR (95% CI) | |
| No. of medical staffs (per 1,000 persons) | 1.09 (0.96–1.23) | 0.95 (0.75–1.20) | 1.09 (1.03–1.16)* | 1.18 (1.08–1.29)* |
| No. of public health physicians (per 10,000 persons) | 1.17 (0.80–1.71) | 1.30 (0.77–2.19) | 0.28 (0.10–0.80)* | 0.27 (0.09–0.86)* |
| Population density (×100 persons/km2) | 1.03 (1.01–1.06)* | 0.99 (0.95–1.03) | 1.00 (0.98–1.03) | 0.99 (0.95–1.04) |
| Per capita GDP (×10,000 RMB, ¥) | 3.18 (2.05–4.93)* | 3.51 (2.09–5.91)* | 0.73 (0.50–1.04) | 0.67 (0.42–1.08) |
OR = odds ratio; AOR = adjusted odds ratio.
* P < 0.05.
We focused on results from the multivariate binary logistic regression models (Table 3). For hot spot clustering, the model had χ2 = 52.4, P < 0.001; Nagelkerke’s pseudo-R2 = 0.617. And for cold spot clustering, the model had χ2 = 16.4, P = 0.002; Nagelkerke’s pseudo-R2 = 0.257. Infectious diarrhea hot spots were positively associated with per capita GDP, with an adjusted odds ratio (AOR): 3.51, 95% CI: 2.09–5.91. The results indicated that a 10,000 Yuan/RMB increase in per capita GDP was associated with 251% increase in the odds of being a hot spot county for infectious diarrhea. However, cold spots clustering were positively associated with the number of medical staffs (AOR: 1.18, 95% CI: 1.08–1.29) and negatively associated with the number of public health physicians (AOR: 0.27, 95% CI: 0.09–0.86). When the number of medical staffs per 1,000 persons increased by one, the odds of being a cold spot county increased by 18%. Multivariate logistic model was used for predicting the clusters (Table 4), with a prediction accuracy to predict hot spots (72.4%, 21/29) and cold spots (11.1%, 2/18), respectively.
Table 4.
Cross tables for predicted clustering based on multivariate models
| Observed category | Predicted category | Observed category | Predicted category | ||
|---|---|---|---|---|---|
| Hot spots | Non–hot spots | Cold spots | Non–cold spots | ||
| Hot spots | 21 | 8 | Cold spots | 2 | 16 |
| Non–hot spots | 4 | 72 | Non–Cold spots | 2 | 85 |
DISCUSSION
Applying spatial hot spot analysis, we found statistically significant high/low-risk areas, namely, hot spots/cold spots of infectious diarrhea among all counties of the Anhui Province in China. Regression models revealed that socioeconomic factors, such as per capita GDP, number of medical staffs, and number of public health physicians in the counties, were significantly associated with risk of hot spot or cold spot clustering of infectious diarrhea. Through spatial visualization and clustering analysis, we can obtain valuable information on the spatial disparity of infectious diarrhea in China and explore the factors behind these disparities.
Diarrheal infections could be acquired through multiple exposure pathways, including primary exposures—contaminated food and water, and secondary ones—person-to-person contact transmissions.22 Another study showed that the spatial pattern of non-cholera diarrhea was consistent with secondary transmission. Its epidemics usually began in a community when an infected person brought the disease from the outside, then infected another person with contacts, and so on. The spatial pattern of cases of non-cholera diarrhea was characterized by more clustering in some specific regions.23 Host susceptibility also played a key role in the occurrence of diarrheal diseases.24 Host susceptibility and secondary transmission pathway were more influenced by social demographics and economic factors.11
We found that an increase in the per capita GDP of counties was associated with increased possibility of being a hot spot for infectious diarrhea. Those counties with high GDP and high incidence rates may be the susceptibility areas to outbreaks of diarrhea. Regarding counties with faster economic development and more crowded residential population, limited sanitation conditions may directly affect the incidence of diarrhea, resulting in clusters of cases. There is no doubt that other reasons may also explain this result, such as the environmental pollution because of rapid increase of GDP pursued in China eventually causes the burden of diarrhea-related diseases.25 Therefore, it is necessary to apply early warning and early intervention during high-incidence seasons of diarrheal diseases to effectively reduce case clusters or outbreaks. The results also suggest policymakers that the pursuit of economic progress should be accompanied by improved sanitation and better access to clean water and food, balancing both economic and health development.
Our results showed that cold spots of infectious diarrhea were positively associated with the number of medical staffs in the county, consistently with other study findings in China. Previously in the Sichuan Province of China, it was found that the number of medical technicians per 1,000 people was significantly negatively correlated with the incidence of bacillary dysentery, which was a serious diarrheal disease caused by different species of Shigella bacteria.17 Better health workforce resources may help reduce the spread of infectious diseases with stronger response capacity, and the prevention strategies should focus on areas with limited health resources.
For the socioeconomic factor of population density, previous research showed that clusters with a significantly high risk of diarrhea26 or cholera27 are observed in the very high population density areas. Furthermore, another study analyzed factors influencing clustering of cholera and found that there was a direct spatial relationship between cholera prevalence and density of refuse dumps.28 Therefore, the population density may interact with other factors such as refuse dumps and sewage treatment on the incidence of infectious diarrhea or other infectious diseases. Further research is needed to determine whether efficient refuse dumps and sewage treatment in densely populated areas of China has actually reduced the risk of infectious disease.
For the factor “the number of public health physicians,” public health physicians’ spatial distribution seemed to be similar to that of infectious diarrheal incidence. In other words, the allocation of public health physicians from policy-making departments was in accordance with the needs of regional incidence of infectious disease. But, the number of public health physicians showed an obvious inverse ratio with cold spot clustering, which told us that simply increasing the number may not reduce the public health risks or enhance prevention of infectious disease. Therefore, spatial clustering research has an important implication for local health departments to better allocate medical and health resources in preventing and controlling the infectious diseases.
Our study had some limitations. First, age-adjusted rates in the study had unequal variances inversely proportional to the population denominator and hence may lead to misleading results. We also tried to implement the empirical Bayesian kriging smoothing in ArcGIS software.29 The results are shown in Supplemental Figure 1. The results of the two methods had similar spatial distribution patterns, and the regions of high- and low-value clustering matched well. Second, based on the data at the county level, the association between socioeconomic factors and the incidence of infectious diarrhea found in this study was an ecological association, which could not be considered as the causal association at the individual level. Last, the intervention measures during the high-incidence season of infectious diarrhea in different counties were different, which could affect the regional disease incidence data and the accuracy of association inference.
In our study, the socioeconomic factors associated with high and low clustering of infectious diarrhea were analyzed. Future studies might use the Bayesian hierarchical spatial model, which can simultaneously model the fixed covariate effect and the random residual effect. The random effect can be modeled by Bayesian prior specification (such as conditional autoregressive model), which reflects the global heterogeneity of space and the relative homogeneity between adjacent regions.30
In conclusion, infectious diarrhea remained a public health problem and had a spatial variation and significant clustering across counties in Anhui. The hot spot of infectious diarrhea was positively associated with per capita GDP in the county, whereas the cold spot was associated with regional health workforce. Water, sanitation, and health–related interventions should be prioritized for hot spots to prevent and control the spread of infectious diarrhea. Targeted and enhanced interventions should be carried out with full consideration of regional socioeconomic conditions.
Supplemental materials
Note: Supplemental figure appear at www.ajtmh.org.
REFERENCES
- 1.Abajobir AA, Abbafati C, Abbas KM, Abd-Allah F, Abera SF, Aboyans V, Adetokunboh O, Afshin A, Agrawal A, Ahmadi A, 2017. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 390: 1151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fischer Walker CL, Sack D, Black RE, 2010. Etiology of diarrhea in older children, adolescents and adults: a systematic review. PLoS Negl Trop Dis 4: e768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Azage M, Kumie A, Worku A, Bagtzoglou AC, 2015. Childhood diarrhea exhibits spatiotemporal variation in northwest Ethiopia: a SaTScan spatial statistical analysis. PLoS One 10: e0144690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gong L, Wu J, Wang A, Zhang J, Zhao X, 2014. Analysis on epidemic characteristics of other infectious diarrhea in Anhui Province, 2007–2012 (in Chinese). Chin J Dis Control Prev 18: 972–975. [Google Scholar]
- 5.Phung D, Huang C, Rutherford S, Chu C, Wang X, Nguyen M, Nguyen NH, Do CM, Nguyen TH, 2015. Temporal and spatial patterns of diarrhoea in the Mekong Delta area, Vietnam. Epidemiol Infect 143: 3488–3497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chaikaew N, Tripathi NK, Souris M, 2009. Exploring spatial patterns and hotspots of diarrhea in Chiang Mai, Thailand. Int J Health Geogr 8: 36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bogale GG, Gelaye KA, Degefie DT, Gelaw YA, 2017. Spatial patterns of childhood diarrhea in Ethiopia: data from Ethiopian demographic and health surveys (2000, 2005, and 2011). BMC Infec Dis 17: 426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fontoura VM, Graepp-Fontoura I, Santos FS, Santos Neto M, Tavares HSA, Bezerra MOL, Feitosa MO, Neves AF, Morais JCM, Nascimento LFC, 2018. Socio-environmental factors and diarrheal diseases in under five-year old children in the state of Tocantins, Brazil. PLoS One 13: e0196702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chang BA, Pearson WS, Owusu-Edusei K, Jr., 2017. Correlates of county-level nonviral sexually transmitted infection hot spots in the US: application of hot spot analysis and spatial logistic regression. Ann Epidemiol 27: 231–237. [DOI] [PubMed] [Google Scholar]
- 10.Ferrer SR, Strina A, Jesus SR, Ribeiro HC, Cairncross S, Rodrigues LC, Barreto ML, 2008. A hierarchical model for studying risk factors for childhood diarrhoea: a case-control study in a middle-income country. Int J Epidemiol 37: 805–815. [DOI] [PubMed] [Google Scholar]
- 11.Levy K, Woster AP, Goldstein RS, Carlton EJ, 2016. Untangling the impacts of climate change on waterborne diseases: a systematic review of relationships between diarrheal diseases and temperature, rainfall, flooding, and drought. Environ Sci Technol 50: 4905–4922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dewan AM, Corner R, Hashizume M, Ongee ET, 2013. Typhoid fever and its association with environmental factors in the Dhaka Metropolitan area of Bangladesh: a spatial and time-series approach. PLoS Negl Trop Dis 7: e1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kelly-Hope LA, Alonso WJ, Thiem VD, Anh DD, Canh DG, Lee H, Smith DL, Miller MA, 2007. Geographical distribution and risk factors associated with enteric diseases in Vietnam. Am J Trop Med Hyg 76: 706–712. [PubMed] [Google Scholar]
- 14.Gao L, Zhang Y, Ding G, Liu Q, Jiang B, 2016. Identifying flood-related infectious diseases in Anhui Province, China: a spatial and temporal analysis. Am J Trop Med Hyg 94: 741–749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ministry of Health of the People’s Republic of China , 2008. Diagnostic Criteria for Infectious Diarrhea (WS271–2007). Beijing, China: People’s Medical Publishing House. [Google Scholar]
- 16.National Bureau of Statistics of the People’s Republic of China , 2012. The Sixth National Census. Available at: http://www.stats.gov.cn/tjsj/tjgb/rkpcgb/dfrkpcgb/201202/t20120228_30380.html. Accessed January 26, 2018. [Google Scholar]
- 17.Ma Y, Zhang T, Liu L, Lv Q, Yin F, 2015. Spatio-temporal pattern and socio-economic factors of bacillary dysentery at county level in Sichuan Province, China. Sci Rep 5: 15264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Statistics Bureau of Anhui Province, NBS Survey Office in Anhui , 2016. Anhui Statistical Yearbook. Beijing, China: China Statistical Press. [Google Scholar]
- 19.Ord JK, Getis A, 1995. Local spatial autocorrelation statistics: distributional issues and an application. Geogr Anal 27: 286–306. [Google Scholar]
- 20.Bagstad KJ, Semmens DJ, Ancona ZH, Sherrouse BC, 2016. Evaluating alternative methods for biophysical and cultural ecosystem services hotspot mapping in natural resource planning. Landscape Ecol 32: 77–97. [Google Scholar]
- 21.Stopka TJ, Goulart MA, Meyers DJ, Hutcheson M, Barton K, Onofrey S, Church D, Donahue A, Chui KKH, 2017. Identifying and characterizing hepatitis C virus hotspots in Massachusetts: a spatial epidemiological approach. BMC Infect Dis 17: 294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Emch M, Yunus M, Escamilla V, Feldacker C, Ali M, 2010. Local population and regional environmental drivers of cholera in Bangladesh. Environ Health 9: 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Emch M, Ali M, 2016. Spatial and temporal patterns of diarrheal disease in Matlab, Bangladesh. Environ Plann A 33: 339–350. [Google Scholar]
- 24.Carlton EJ, Woster AP, DeWitt P, Goldstein RS, Levy K, 2016. A systematic review and meta-analysis of ambient temperature and diarrhoeal diseases. Int J Epidemiol 45: 117–130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kan H, 2009. Environment and health in China: challenges and opportunities. Environ Health Perspect 117: A530–A531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pattanayak SK, Wendland KJ, 2007. Nature’s care: diarrhea, watershed protection, and biodiversity conservation in Flores, Indonesia. Biodiversity Conserv 16: 2801–2819. [Google Scholar]
- 27.Kanungo S, et al. 2012. Clinical, epidemiological, and spatial characteristics of Vibrio parahaemolyticus diarrhea and cholera in the urban slums of Kolkata, India. BMC Public Health 12: 830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Osei FB, Duker AA, 2008. Spatial dependency of V. cholera prevalence on open space refuse dumps in Kumasi, Ghana: a spatial statistical modelling. Int J Health Geogr 7: 62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Krivoruchko K, 2011. Spatial Statistical Data Analysis for GIS Users. Redlands, CA: Esri Press. [Google Scholar]
- 30.MacNab YC, 2003. Hierarchical bayesian modeling of spatially correlated health service outcome and utilization rates. Biometrics 59: 305–315. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.