Abstract
Objectives. To determine what role the 88 000 Housing and Urban Development–Veterans Affairs Supportive Housing (HUD-VASH) vouchers for permanent supportive housing among US veterans distributed between 2008 and 2017 played in the significant fall in veterans’ homelessness over the same time period.
Methods. Using a panel data set at the Continuum of Care level over the 2007 to 2017 period, we correlated changes in vouchers with permanent supportive housing units and measures of homelessness. To reduce concerns about omitted variables bias, we used a 2-stage least-squares procedure. The instrument is a Bartik-type shift-share variable. Specifically, for the cumulative vouchers received at the local level, we used the share of the nation's homeless veterans from the local level in the year before the HUD-VASH program multiplied by the cumulative number of vouchers distributed at the national level up to that point.
Results. For each additional voucher, permanent supportive housing units increased by 0.9 and the number of homeless veterans decreased by 1.
Conclusions. Our results indicate the HUD-VASH program worked as intended and veterans’ homelessness would have risen substantially over the past decade without the program.
The Housing and Urban Development–Veterans Affairs Supportive Housing (HUD-VASH) program was started in 1992 for homeless veterans with psychiatric and substance abuse disorders.1 The program aimed to demonstrate that “health and other supportive services, combined with decent, safe and sanitary affordable housing, can help homeless veterans with severe psychiatric or substance abuse disorders lead healthy, productive lives in the community, and avoid becoming permanent members of the nation’s homeless.”2(p9956) The HUD-VASH program was expanded greatly in 2008 when 10 150 vouchers were distributed and in 2009 became the cornerstone of the Obama administration’s initiative to end veterans’ homelessness.3,4 Through 2017, the program has funded 87 864 vouchers with an annual cost of $675 million in fiscal year 2017.5 The program’s enlargement was a response to the rising number of veterans returning from Iraq and Afghanistan to a declining US economy.6,7 The expansion was also driven in part by a randomized controlled trial showing that HUD-VASH reduced homelessness.1
To be eligible for HUD-VASH, veterans must be homeless as defined by the McKinney-Vento Homeless Assistance Act, be eligible for Department of Veterans Affairs (VA) health care, agree to intensive case management, and have no prior convictions for arson or sex offenses.8 In the case of a limited supply of vouchers, priority is given to veterans who are chronically homeless or have dependent children.6 To receive a voucher, veterans must first contact their local VA Medical Center to determine program eligibility. If approved, veterans must then submit their HUD-VASH application to the public housing authority, which then provides them with the voucher. The veteran is responsible for paying rent of up to 30% of his or her income and the voucher covers the rest. Eighty-five percent of veterans offered a voucher take up the program and 90% of vouchers lead to housing. Eighty percent of recipients are chronically homeless and 56% come from unsheltered arrangements. About 42% of recipients leave the program for a lease and another 20% exit without a lease in place.9
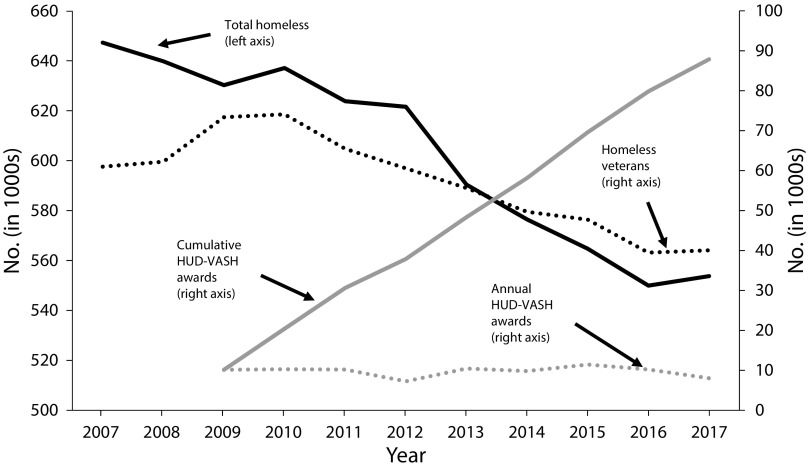
As the program grew between 2010 and 2017, the number of homeless veterans declined by 46%, and many homeless advocacy groups have attributed these declines to the HUD-VASH program.10,11 Figure 1 reports the basic facts surrounding these claims. The solid black line represents annual point-in-time estimates of the total homeless in the United States from 2007 to 2017. This number fell 15% or by 93 000 homeless. The dotted black line graphs veterans’ homelessness, which fell by 33 000 from its peak in 2010: a 46% decline. The dotted gray line at the bottom of the graph shows the HUD-VASH vouchers added to the market on an annual basis, which averages about 9800 per year. As these vouchers are permanent and transferable, the effective number of vouchers is the cumulative amount distributed, which is the solid gray line in Figure 1, reaching about 88 000 by 2017.
FIGURE 1—
Counts of Homeless Groups and Housing and Urban Development–Veterans Affairs Supportive Housing Awards Over Time: United States, 2000–2016
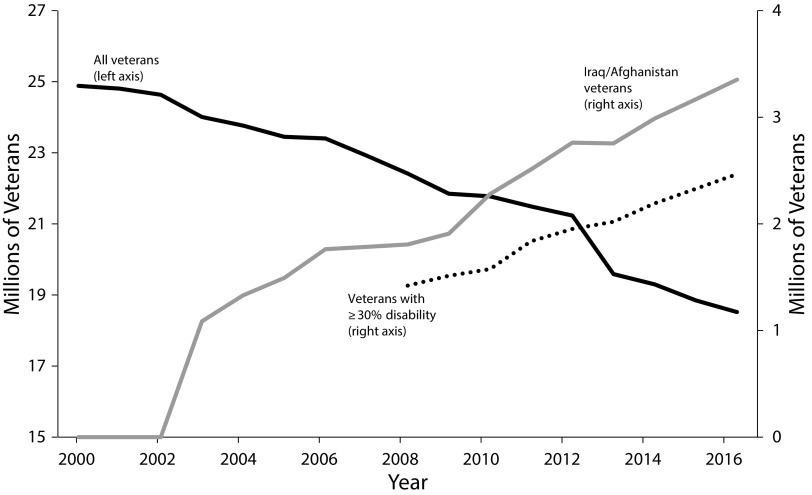
Despite the praise for the program, there has been no systematic attempt to identify how much of the decline in homelessness is attributable to the HUD-VASH program. There is reason to suspect the benefits of the program might be overstated. First, the total decline in veterans’ homelessness is only about a third of the number of HUD-VASH vouchers distributed. Second, the voucher program expansion coincided with improving economic trends as the effects of the Great Recession waned. We calculated that the unemployment rate for veterans aged 25 to 54 years fell by almost 50% between 2010 and 2016, from 9.8% to 4.7%, which could explain some decrease in homelessness.12 Third, veterans’ homelessness could be declining because there are fewer veterans. The top line in Figure 2 indicates that the total number of veterans has been declining since 2001 as the World War II generation dies out. One author, citing these facts, concluded: “This great initiative appears to have accomplished little.”13(p21) Finally, some previous research found that increased expenditures on permanent supportive housing programs has not led to a reduction in general homelessness.14,15
FIGURE 2—
Counts of Veterans in the American Community Survey: United States, 2007–2017
Conversely, it is plausible that homelessness rates among veterans would have increased if the HUD-VASH program had not been in effect. Although the veteran population is declining, the number of veterans at risk for homelessness may be rising. In particular, veterans of the post-9/11 Gulf Wars are more likely to enter homelessness than veterans from other wars.16 Post-9/11 Gulf War veterans also have historically high levels of use of VA medical services for factors such as mental illness and posttraumatic stress disorder.17 Disabled veterans are also at greater risk for homelessness. These subgroups of veterans grew rapidly over this period, as illustrated in Figure 2. The solid gray line shows that post-9/11 veterans have more than tripled to 3.5 million since 2003. The dotted black line tracks the number of veterans with a 30% or more service disability, which rose 67% to 2.9 million between 2008 and 2017. These numbers call for a more detailed assessment of the HUD-VASH’s impact on homelessness.
In this study, we used a panel data set at the Continuum of Care level from 2007 to 2017 to examine how the greater availability of HUD-VASH vouchers affected total permanent supportive housing beds and measures of homelessness. We employed an instrumental variables procedure and estimated that the addition of 1 HUD-VASH voucher increased permanent supportive housing beds within that area by 0.9, reduced veterans’ homeless by slightly more than 1, and reduced chronic homelessness by 0.7. In contrast to some earlier findings on the ineffectiveness of permanent supportive housing vouchers on general homelessness, we found that HUD-VASH grants worked as intended.
METHODS
We used 4 sets of data in this analysis: annual point-in-time estimates of the homeless population, the annual Housing Inventory Count Report of resources devoted to fighting homelessness, counts of HUD-VASH grants distributed to public housing authorities, and control variables used in our regression models. The first 2 data sets provided information at the Continuum of Care level, which are local areas that coordinate resources to combat homelessness. We created a crosswalk to match public housing authorities to Continuums of Care and Continuums of Care to counties. The Appendix (available as a supplement to the online version of this article at http://www.ajph.org) provides an outline of how we constructed this mapping to deal with changing and sometimes overlapping Continuum of Care boundaries.
The result is a panel data set with 11 years of data (2007–2017) for 350 Continuum of Care areas. These data represent 98% of both the nation’s population and of the homeless in 2017. In 2017, Continuums of Care varied in population from 29 000 in Garret County, Maryland, to more than 10 million for Los Angeles County. The average population of a Continuum of Care increased from 841 000 in 2007 to 910 000 in 2017. Because the point-in-time survey is conducted in January and vouchers are reported on a fiscal-year basis (October–September), and given the time to distribute grant funds and recruit grant recipients, a grant distributed in fiscal year 2008 will likely not alter homelessness counts until 2009. As a result, we matched homelessness data for calendar year t to voucher data as of fiscal year t–1.
In Table 1 we report descriptive statistics for key variables for 2008 (the last year before HUD-VASH vouchers) and 2017. We scaled all variables by 100 000 in total current population (not just veterans) within the Continuum of Care. The only variables that were specific to veterans were cumulative homeless veterans per 100 000 of population, plus the sheltered and unsheltered rates for this group. All other variables were measuring aggregates for the entire population. Over this period, total homeless rates fell by 21% while homeless veteran rates fell by 42%. Permanent supportive housing beds per 100 000 increased by 45%, and 60% of this increase was from HUD-VASH vouchers. Although vouchers per 100 000 increased by 27, the veteran homelessness rate fell by about one third of that total.
TABLE 1—
Descriptive Statistics From Balanced Panel of Continuum of Care Areas: United States, 2008 and 2017
| Variable | Source | 2008 Mean (SD) | 2017 Mean (SD) |
| Cumulative VASH awards/100 000 | HUD-VASH Program | 0 (0) | 27.0 (31.3) |
| Permanent supportive housing beds/100 000 | Housing inventory counts | 63.8 (75.1) | 108.5 (104.6) |
| Homeless veterans/100 000 | Point-in-time data | 20.5 (23.6) | 11.9 (13.0) |
| Sheltered homeless veterans/100 000 | Point-in-time data | 12.8 (14.2) | 7.4 (7.4) |
| Unsheltered homeless veterans/100 000 | Point-in-time data | 7.7 (16.5) | 4.6 (8.3) |
| Chronically homeless/100 000 | Point-in-time data | 38.5 (51.0) | 26.1 (38.5) |
| Total homeless/100 000 | Point-in-time data | 210.7 (180.2) | 168.8 (181.8) |
Note. HUD = Housing and Urban Development; VASH = Veterans Affairs Supportive Housing. Sample means are weighted by annual population within the Continuum of Care.
Our baseline statistical model exploited the panel nature of the data. The outcomes of interest were measures such as homeless veterans per 100 000 and permanent supportive housing beds per 100 000, which varied across Continuum of Care (i) and year (t) and are denoted as yit. Because vouchers are permanent and transferable, the key covariate of interest is CVit, the cumulative HUD-VASH vouchers per 100 000.
The basic model is described by the equation
where xit is a vector of control variables;  and
and  are Continuum of Care and year effects, respectively; and
are Continuum of Care and year effects, respectively; and  is a random error. The Continuum of Care fixed effects are necessary to control for permanent differences in homelessness rates across geographic areas, and the year effects controlled for factors such as the economic recovery that affects all areas in a given year. The coefficient of interest was α but ordinary least-square (OLS) estimates of Equation 1 are potentially subject to an omitted variables bias if areas received more vouchers because of an anticipated changing need for resources. In this case, the positive correlation between annual vouchers and the omitted need factor generated an upward bias in OLS estimates.
is a random error. The Continuum of Care fixed effects are necessary to control for permanent differences in homelessness rates across geographic areas, and the year effects controlled for factors such as the economic recovery that affects all areas in a given year. The coefficient of interest was α but ordinary least-square (OLS) estimates of Equation 1 are potentially subject to an omitted variables bias if areas received more vouchers because of an anticipated changing need for resources. In this case, the positive correlation between annual vouchers and the omitted need factor generated an upward bias in OLS estimates.
Consistent estimates of α can be obtained if there is an instrumental variable that alters vouchers but has no direct impact on outcomes. In this case, we exploited a feature of the way vouchers were distributed to construct the instrument. The number of vouchers awarded to each public housing authority was based on geographic need and performance data from both the public housing authority and partnering VA Medical Centers. Need was determined in part from Continuum of Care data on point-in-time veteran homeless counts. The overriding factor appeared to be the previous year’s homeless levels in the local area. Across all Continuums of Care over the 2009 to 2017 period, the lagged fraction of homeless veterans from a Continuum of Care explained 77% of the variation in the share of HUD-VASH awards received by a Continuum of Care for that year. Exploiting this fact, we could construct a “shift-share” instrument used frequently to identify causal impact.18 This type of instrument has been used in a variety of health contexts, including estimating the impact of immigration on health19 and the role of employment changes in the opioid crisis20 and in other deaths of despair.21
The formation of the instrument was as follows. Let  be the share of the nation’s veterans from Continuum of Care i in 2008, the year before vouchers were first distributed. Let CVt be the cumulative number of vouchers distributed to the nation as a whole by year t. A good predictor of the number of vouchers received through year t by Continuum of Care i is
be the share of the nation’s veterans from Continuum of Care i in 2008, the year before vouchers were first distributed. Let CVt be the cumulative number of vouchers distributed to the nation as a whole by year t. A good predictor of the number of vouchers received through year t by Continuum of Care i is  . The instrument is then this value scaled by population, as shown by the equation
. The instrument is then this value scaled by population, as shown by the equation
The instrument identifies a consistent estimate of the vouchers if it satisfies 2 conditions: (1) the instrument INSTit is strongly correlated with CVit (relevance condition) and (2) INSTit is only correlated with current measures of homelessness through its influence on CVit (the exclusion restriction). Condition 1 was confirmed by a strong first-stage regression as demonstrated in Table 2. Condition 2 was satisfied given the way the instrument was constructed. There are annual “shifts” in the aggregate number of vouchers distributed that are determined by the federal government on the basis of budgetary considerations. Distribution of these amounts to local areas is largely determined by their pre–HUD-VASH “share” of veteran homeless. Because neither the pre–HUD-VASH share nor the aggregate shift in voucher cumulative totals are determined by contemporaneous local characteristics, the instrument provides exogenous variation in the per-capita vouchers received at the local level in a particular period.
TABLE 2—
Two-Stage Least Squares Estimates of Equation 1 Using the Balanced Panel of Continuum of Care Areas: United States, 2007–2017
| Independent Variable, b (95% CI) |
|||
| Dependent Variable | The Instrument for Cumulative VASH Awards/100 000, OLS | Cumulative VASH Awards/100 000, 2SLS | R2 |
| (1) Cumulative VASH awards/100 000 | 0.480 (0.350, 0.609) | 0.798 | |
| (2) Permanent supportive housing beds/100 000 | 0.897 (0.564, 1.230) | 0.945 | |
| (3) Homeless veterans/100 000 | −1.080 (−1.365, −0.794) | 0.499 | |
| (4) Sheltered homeless veterans/100 000 | −0.486 (−0.680, −0.291) | 0.650 | |
| (5) Unsheltered homeless veterans/100 000 | −0.594 (−0.906, −0.281) | 0.475 | |
| (6) Chronically homeless/100 000 | −0.655 (−1.005, −0.305) | 0.745 | |
| (7) Total homeless/100 000 | −1.171 (−2.787, 0.445) | 0.863 | |
Note. 2SLS = 2-stage least squares; CI = confidence interval; OLS = ordinary least squares; VASH = Veterans Affairs Supportive Housing. All models used a balanced panel of 350 Continuum of Care areas from 2007 to 2017 for a total of 3850 observations. Other covariates in the model included year and Continuum of Care fixed effects, total permanent supportive housing awarded to a Continuum of Care by Housing and Urban Development per 100 000, the county unemployment rate, per-capita income, and median rent for a 1-bedroom apartment. All dollar values are in real 2017 dollars. Confidence intervals are calculated allowing the errors in the model to have an arbitrary correlation at the Continuum of Care level. All models are weighted by the Continuum of Care population.
We estimated Equation 1 by 2-stage least squares (2SLS). In the first stage, CVit was regressed on the instrument INSTit and the predicted value of CVit was then used as the covariate in the second stage. The outcomes examined in the second stage—all measured as counts per 100 000 in population within the Continuum of Care—were the following: permanent supportive housing beds filled, total homeless veterans, sheltered homeless veterans, unsheltered homeless veterans, chronically homeless (both veterans and nonveterans), and total homeless individuals (both veterans and nonveterans). We weighted all regressions by the concurrent Continuum of Care population. Standard errors allowed for arbitrary correlation in errors across observations within a Continuum of Care. The covariates in xit included unemployment rate, the fraction of the population that are veterans, real per-capita income, real median rent for a 1-bedroom apartment, and total permanent supportive housing grants per 100 000 people from HUD to the Continuum of Care. The first 4 of these control variables were aggregated from the county to the Continuum of Care level and are defined in detail in the Appendix (available as a supplement to the online version of this article at http://www.ajph.org).
RESULTS
2SLS estimates of Equation 1 are reported in Table 2. For all parameters, we report the coefficient estimates and 95% confidence intervals (CIs). In each case, the parameter can be interpreted as the change in the outcome of interest for a 1-unit increase in HUD-VASH vouchers per 100 000 people.
The first row in Table 2 shows the relevance condition outlined previously and gives the coefficient estimates from the first-stage regression in which the key covariate of interest was the instrument for cumulative HUD-VASH awards. The coefficient estimate on the instrument (INSTit in Equation 2) was statistically significant with magnitude 0.48, meaning that if an area was predicted to get 1 voucher based on its 2008 need then they can expect to get half that amount through the current period. The first-stage F-test on the instrument was 49.2, indicating that there were no finite sample bias concerns.
In column 2 of the table we report the 2SLS estimates for the coefficient estimate on HUD-VASH awards per 100 000 from 6 different regressions with key outcomes of interest. In row 2 we see that for each HUD-VASH voucher awarded, permanent supportive housing beds increased by 0.9, and in row 3, we see that the same voucher reduced veterans’ homelessness by 1. Vouchers reduced veterans’ homelessness 1 for 1.
The importance of estimating the model by 2SLS was illustrated when we estimated Equation 1 by OLS and ignored the potential omitted variables bias in the cumulative vouchers variable. In the OLS estimates of Equation 1 with permanent supportive housing vouchers per 100 000 as the outcome of interest, the coefficient estimate on vouchers per 100 000 was 0.122 (95% CI = 0.073, 0.172), about one seventh the corresponding coefficient estimate in Table 2. Likewise, OLS estimation of Equation 1 when we used homeless veterans per 100 000 as the dependent variable generated a value of −0.037 (95% CI = −0.080, 0.005) for the coefficient on vouchers per 100 000. These contaminated estimates suggest that HUD-VASH vouchers have done little to increase capacity or reduce homelessness. The bias in the OLS estimates is consistent with the hypothesized omitted variable bias we outlined previously.
In rows 4 and 5, the negative coefficients represent the effect of a voucher for sheltered and unsheltered homeless veterans, respectively. These numbers indicate that, for each additional HUD-VASH voucher awarded to a local area, sheltered homeless counts fell by 0.49, the unsheltered fell by 0.59, and both estimates are statistically significant. These results indicate that 45% of the reduction in veterans’ homelessness was coming from the sheltered population (−0.486/−1.08) while 55% was coming from the unsheltered homeless (−0.594/−1.08). These results corroborate numbers from the HUD-VASH exit study, which found that around 60% of voucher recipients were unsheltered at the time of program entry.9
Row 6 shows the results of our examination of the effects of vouchers on the total number of chronic homeless, which included veterans and nonveterans. This number is statistically significant and indicates that general chronic homelessness fell by about 0.66 for each additional voucher. Again, this estimate roughly aligns with the HUD-VASH exit study that found that roughly 80% of voucher recipients were chronically homeless.9 The only statistically insignificant result in the table is in row 7, where we show that each voucher reduced total homelessness by 1, but the CI on this is wide. This lack of precision is not a surprise as the between–Continuum of Care standard deviation in total homelessness was about 9 times that of the same variable for veterans’ homelessness. This increase in variation cannot be explained by these vouchers because HUD-VASH is not directed to the general homeless population, and the standard error in the model increases accordingly. The point estimate does suggest that vouchers do not “crowd-out” resources for nonveterans.
DISCUSSION
Our results paint a positive picture of the HUD-VASH program. For each voucher distributed, permanent supportive housing beds increased by 0.9, and veteran homeless fell by 1. The drop in veteran homelessness from sheltered and unsheltered arrangements is consistent with the composition reported in exit surveys of HUD-VASH participants. Given these results, the fact that homelessness among veterans fell by only 30 000 from its peak in 2010 while the number of vouchers in use has expanded by nearly 88 000 suggests that homelessness among veterans would have increased considerably without the HUD-VASH program. Specifically, we estimated that in the absence of HUD-VASH the homeless veteran population would have reached nearly 130 000 by 2017 instead of the observed 40 000.
We can only speculate why we generated such impactful and precise effects of this permanent supportive housing program whereas previous work has found little impact of general HUD permanent supportive housing grants on outcomes. We offer 3 potential explanations. First, some previous work14 generated large standard errors on their 2SLS estimates, so the results cannot say anything definitive about the effectiveness of permanent supportive housing on homelessness. Second, another similar study15 used only cross-sectional data, making it more difficult to find valid instruments for the 2SLS models. Third, the focused targeting of these vouchers to a specific group may have made the program more effective.
Limitations
Despite these positive results, important questions remain about permanent supportive housing-type interventions that we did not address in this article. For instance, permanent supportive housing has been cited as a way to reduce the increased costs on the health care and criminal justice system caused by high rates of chronic homelessness.22–24 However, the evidence that permanent supportive housing improves health outcomes or reduces medical costs is inconclusive.25
Public Health Implications
In 2017, the American Public Health Association (APHA) issued a policy statement to reaffirm its position that homelessness is a fundamental public health issue that leads to higher incidences of mental and physical health conditions, substance abuse, overuse of emergency services, and a major strain on public and private health resources.26 APHA and the housing provider community have recommended the Housing First approach to combat the wide-ranging health issues of homeless individuals. This is because of the fact that the public health problems faced by individuals who experience chronic homelessness cannot be effectively treated until their housing stability is secured: housing is understood to be a prerequisite to recovery.
By identifying the effectiveness of HUD-VASH in treating homelessness among veterans, this research offers a central contribution to policy makers that may have a direct impact on the sustenance of the program. HUD-VASH is dependent on federal appropriations for funding. In recent years, the program has been especially vulnerable to funding cuts. In 2017, the Secretary of the VA proposed to cut $460 million from the program and the program. The White House proposed budget for fiscal year 2020 decreased the funding for all housing voucher contract renewals by $200 million and cut funding for new VASH vouchers from $44 million in 2019 to zero.27,28 Congress eventually passed a budget that maintained 2019 funding at 2018 levels.29 In conjunction with ongoing research into the cost-effectiveness of permanent supportive housing, this study will provide evidence on the program’s efficacy that could directly inform both the US Congress and the Executive Branch.
The growth of the HUD-VASH program was spurred on in part by evidence from randomized controlled trials showing improved outcomes for voucher recipients.1 A common problem with experiments is that they frequently do not replicate and do not perform well at a larger scale.30 The results here are a counter to that notion as the program worked as designed on a national scale.
ACKNOWLEDGMENTS
This work was supported by the Wilson Sheehan Lab for Economic Opportunities.
We thank Maggie Garnett for research assistance.
CONFLICTS OF INTEREST
The authors have no conflicts of interest.
HUMAN PARTICIPANT PROTECTION
This study used publicly available data at the aggregate level and is therefore not considered human participant research.
REFERENCES
- 1.Rosenheck R, Kasprow W, Frisman L, Liu-Mares W. Cost-effectiveness of supported housing for homeless persons with mental illness. Arch Gen Psychiatry. 2003;60(9):940–951. doi: 10.1001/archpsyc.60.9.940. [DOI] [PubMed] [Google Scholar]
- 2.Announcement of funding—Invitation for FY 1992 Section 8 rental voucher set-aside for homeless veterans with severe psychiatric or substance abuse disorders. Fed Regist. 1992;57(55):9956–9959. [Google Scholar]
- 3.Secretary Shinseki details plan to end homelessness for veterans. US Department of Veterans Affairs. November 3, 2009. Available at: https://www.va.gov/opa/pressrel/pressrelease.cfm?id=1807. Accessed May 29, 2019.
- 4.US Interagency Council on Homelessness. Opening doors: federal strategic plan to prevent and end homelessness. 2015. Available at: https://www.usich.gov/resources/uploads/asset_library/USICH_OpeningDoors_Amendment2015_FINAL.pdf. Accessed May 29, 2019.
- 5.National Alliance to End Homelessness. FY 2018 discretionary homelessness budget chart. 2017. Available at: https://endhomelessness.org/wp-content/uploads/2017/06/FY-2018-Discretionary-Homelessness-Budget-Chart_5.24.pdf. Accessed May 29, 2019.
- 6.National Low Income Housing Coalition. Veterans affairs supportive housing vouchers. 2017. Available at: http://nlihc.org/sites/default/files/AG-2017/2017AG_Ch05-S14_Veterans-Affairs-Supportive-Housing-Vouchers.pdf. Accessed May 29, 2019.
- 7. Consolidated Appropriations Act, 2008, Pub L No. 110-161 (2007).
- 8. McKinney-Vento Homeless Assistance Act, 42 USC 11302 (2009).
- 9.Montgomery AE, Cusack M HUD-VASH Exit Study final report. US Department of Housing and Urban Development, Office of Policy Development and Research. 2017. Available at: https://www.huduser.gov/portal/sites/default/files/pdf/HUD-VASH-Exit-Study.pdf. Accessed May 29, 2019.
- 10.The American Legion. VA. HUD and DoL efforts to reduce veteran homelessness. January 18. 2018. Available at: https://www.legion.org/legislative/testimony/240748/va-hud-and-dol-efforts-reduce-veteran-homelessness. Accessed May 29, 2019.
- 11.Keleher K. Addressing veteran homelessness: current position; future course. January 18, 2018. Veterans of Foreign Wars. Available at: https://www.vfw.org/advocacy/national-legislative-service/congressional-testimony/2018/1/addressing-veteran-homelessness-current-position-future-course. Accessed May 29, 2019.
- 12.Ruggles S, Flood S, Goeken R et al. Integrated Public Use Micro Samples USA: Version 8.0. 2018 [Google Scholar]
- 13.O’Flaherty B. Homelessness research: a guide for economists (and friends) J Hous Econ. 2019;44:1–25. [Google Scholar]
- 14.Corinth K. The impact of permanent supportive housing on homeless populations. J Hous Econ. 2017;35(1):69–84. [Google Scholar]
- 15.Lucas DS. The impact of federal homelessness funding on homelessness. South Econ J. 2017;84(2):548–576. [Google Scholar]
- 16.Department of Veterans Affairs. Office of Inspector General. Homeless incidence and risk factors for becoming homeless in veterans. 2012. Available at: https://www.va.gov/oig/pubs/VAOIG-11-03428-173.pdf. Accessed May 29, 2019.
- 17.Seal KH, Metzler TJ, Gima KS, Bertenthal D, Maguen S, Marmar CR. Trends and risk factors for mental health diagnoses among Iraq and Afghanistan veterans using Department of Veterans Affairs health care, 2002–2008. Am J Public Health. 2009;99(9):1651–1658. doi: 10.2105/AJPH.2008.150284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bartik TJ. Who Benefits From State and Local Economic Development Policies? Kalamazoo. MI: W. E. Upjohn Institute for Employment Research; 1991. [Google Scholar]
- 19.Giuntella O, Mazzonna F. Do immigrants improve the health of natives? J Health Econ. 2015;43:140–153. doi: 10.1016/j.jhealeco.2015.06.006. [DOI] [PubMed] [Google Scholar]
- 20.Currie J, Jin J, Schnell M. US employment and opioids: is there a connection? National Bureau of Economic Research working paper w24440. March 2018. Available at: http://www.nber.org/papers/w24440.pdf. Accessed May 29, 2019.
- 21.Bound J, Geronimus A, Waidmann T, Rodriguez J Local economic hardship and its role in life expectancy trends. Michigan Retirement Research Center, University of Michigan. January 2018. Working paper 2018-389. Available at: https://deepblue.lib.umich.edu/bitstream/handle/2027.42/148126/wp389.pdf?sequence=1&isAllowed=y. Accessed May 29, 2019.
- 22.Flaming D, Toros H, Burns P. Home not found: the cost of homelessness in Silicon Valley. Economic Roundtable. 2015. Available at: http://rgdoi.net/10.13140/RG.2.1.4780.6327. Accessed May 29, 2019.
- 23.Rosenheck R, Seibyl C. Homelessness: health service use and related costs. Med Care. 1998;36(8):1256–1264. doi: 10.1097/00005650-199808000-00013. [DOI] [PubMed] [Google Scholar]
- 24.Culhane DP, Metraux S, Hadley T. Public service reductions associated with placement of homeless persons with severe mental illness in supportive housing. Hous Policy Debate. 2002;13(1):107–163. [Google Scholar]
- 25.National Academies of Sciences. Permanent Supportive Housing: Evaluating the Evidence for Improving Health Outcomes Among People Experiencing Chronic Homelessness. Washington, DC: National Academies Press; 2018. Engineering, and Medicine. [PubMed] [Google Scholar]
- 26.American Public Health Association. Housing and homelessness as a public health issue. November 7, 2017. Available at: https://www.apha.org/policies-and-advocacy/public-health-policy-statements/policy-database/2018/01/18/housing-and-homelessness-as-a-public-health-issue. Accessed May 29, 2019. [Google Scholar]
- 27.Department of Veterans Affairs. Memorandum: Realignment of specific purpose fund allocations to general purpose. September 2017. Available at: https://www.washingtonpost.com/news/checkpoint/wp-content/uploads/sites/33/2017/12/GeneralPurposefundlist-va.pdf. Accessed May 29, 2019.
- 28.National Low Income Housing Coalition. FY20 budget chart for selected HUD and USDA programs. May 22, 2019. Available at: https://nlihc.org/sites/default/files/NLIHC_HUD-USDA_Budget-Chart.pdf. Accessed May 29, 2019.
- 29.McCarty M HUD FY2019 appropriations: in brief. Congressional Research Service. 2019. Available at: https://www.everycrsreport.com/files/20190402_R45294_2b2d4d95a56b35f15cc9e4331455d3fa2d500116.pdf. Accessed May 29, 2019.
- 30.Deaton A, Cartwright N. Understanding and misunderstanding randomized controlled trials. Soc Sci Med. 2018;210:2–21. doi: 10.1016/j.socscimed.2017.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]