Abstract
Introduction:
Metal toxicity secondary to corrosion and wear has been reviewed in the arthroplasty literature with evidence supporting dermatologic, neurologic, and cardiac involvement. This is the first report of a novel case with the occurrence of systemic pathology with only mildly elevated serum cobalt (Co) and chromium (Cr) levels due to trunnion wear in a metal-on-polyethylene articulation.
Case Report:
A 45-year-old female who had undergone a revision total hip arthroplasty developed concerning dermatologic, neurologic, and cardiac symptoms. Symptoms were initially attributed to an unknown autoimmune etiology. She had mildly elevated cobalt and chromium levels and subsequently underwent a second revision, this time with complete exchange of the cobalt/chromium components. By her 2-month follow-up, she reported partial resolution of symptoms. She continues to improve more than a year postoperatively.
Conclusion:
Consideration should be given to metal ion toxicity due to trunnion wear in patients with cobalt/chromium femoral components, even with relatively low ion levels.
Keywords: Total hip arthroplasty, Metal ion toxicity, Trunnion wear
Learning Point of the Article:
Following total hip arthroplasty, consideration should be given to metal ion toxicity due to trunnion wear in patients with cobalt/chromium femoral components, even with relatively low ion levels.
Introduction
Modularity in total hip arthroplasty (THA) design has introduced surgical flexibility and implant options for both the surgeon and patient. With more widespread use, concerns of implant interaction at the modular junctions have been raised [1, 2]. More recently, the phenomenon of head-neck junction corrosion has been recognized as a cause of hip pain following arthroplasty [3, 4]. Reports of clinical symptoms, implant failure, and elevated metal ion levels causing adverse local tissue reactions (ALTRs), similar to previously described presentations in metal-on-metal (MoM) hip designs have been reported [5, 6, 7]. While these parallels have been explored, systemic manifestations including allergic dermatitis, neurological complications, and cardiac pathology due to metal toxicity have been less common and isolated almost exclusively to MoM articulations [8, 9]. We discuss a patient who presented with signs of systemic metal toxicity including dermatologic, neurologic, and cardiac manifestations secondary to metallosis at the head-neck junction of a modular implant. She went on to have improvement in her clinical symptoms following revision arthroplasty.
Case Report
The patient was verbally informed of the intent to publish the findings and consent was obtained through independent discussion for deidentified clinical images and clinical data to be published. The patient is now a 47-year-old female with a family history of rheumatoid arthritis, Hashimoto’s thyroiditis, and Grave’s disease. She had a non-contributory personal medical history before the onset of the symptoms described below, except for having developmental dysplasia of the right hip, multiple reconstructive surgeries as a child, and ultimately undergoing a right THA at age 22. She denied a metal allergy. She initially did well after her primary THA but went on to develop acetabular osteolysis which was treated with revision of her acetabular component with femoral head exchange 11 years later. The retained femoral component was an anatomic medullary locking (AML) hip stem (DePuy, Warsaw, Indiana), a cobalt-chromium-molybdenum alloy porous-coated femoral implant. This stem was retained along with implantation of a new 32 +5mm cobalt (Co)/chromium (Cr) femoral head. There was no gross evidence of corrosion or wear at the trunnion at the time of the revision surgery. Two years after her revision surgery, she sought care from rheumatology, cardiology, and her primary care physician. Her constellation of symptoms included polymyalgia, polyarthralgia, oral ulcers, body aches, headaches, intermittent low-grade fevers, fatigue, and a malar rash. She saw a cardiologist for lightheadedness and syncope, and her tilt-table test was positive. She denied dry eyes, dry mouth, kidney problems, venous thromboembolism, or joint swelling/redness. She was diagnosed with systemic lupus erythematosus, mixed connective tissue disease, fibromyalgia, and postural orthostatic tachycardia syndrome (POTS). Treatments included oral and topical steroids, anti-inflammatory medications, doxycycline, escitalopram, tacrolimus ointment, hydroxychloroquine, and midodrine. She reported mild but inadequate relief with these medications. Still symptomatic nearly 8 years later (10 years after her revision), she was reevaluated by rheumatology and dermatology. In addition to her previous symptoms, she had now also developed non-dermatomal paresthesia in her upper and lower extremities and “brain fog.” This led to extensive laboratory studies over the ensuing year, including complete blood count with differential, C-reactive protein, erythrocyte sedimentation rate, creatine kinase, magnesium, coenzyme Q10, thyroid-stimulating immunoglobulin, free thyroxine (T4 free), T3, thyroid peroxidase antibody, zinc, parathyroid hormone, serum protein electrophoresis, free testosterone, follicle-stimulating hormone, luteinizing hormone, estradiol, progesterone, cortisol, Vitamin B6, tissue transglutaminase antibody, serum porphyrins, C3 and C4 complement levels, immunoglobulin E, and MTHFR mutation polymerase chain reaction - all of which were within normal limits. Anticardiolipin antibody, anti-smooth muscle antibody, antimitochondrial antibody, anti-liver-kidney microsomal antibody, anti-double-stranded DNA, Sjogren’s antibodies, celiac disease serology, cytomegalovirus antibody, Epstein-Barr antibody, human immunodeficiency virus antibody, hepatitis panel, and autoimmune small vessel vasculitis panel were all negative. Antinuclear antibody test was positive (15 IU/mL, ref: <7.5 IU/mL). Her dermatological symptoms included an intermittent, disseminated, and pruritic facial, hand, and arm rash that worsened with sun exposure and consisted of erythematous papules coalescing into plaques (Fig. 1a and b). The rash was biopsied with findings of spongiotic dermatitis. The pathologist noted that given the patient’s history of THA and elevated serum Co levels, an allergic dermatitis such as hers could present as a reaction to metal prosthetic implants. She returned to her orthopedic surgeon 12 years after her revision. She described right groin and thigh pain, made worse with weight-bearing. Radiographs obtained demonstrated osteolysis at the medial calcar, greater trochanter, and the proximal femoral diaphysis (Fig. 2). Bone scan showed activity in the peritrochanteric region of the femur (Fig. 3). The myriad of symptoms combined with her imaging was concerning for trunnionosis and metal ions were ordered. Cobalt was 10.1 mcg/L (ref: <3.9 mcg/L) and chromium was 5.7 mcg/L (ref: <5.0 mcg/L), our laboratory reports ion levels in mcg/L, however, 1 mcg/L = 1 ppb [10]. A month later, her levels were 7.6 mcg/L and 5.5 mcg/L, respectively. She was also seen by a toxicologist who confirmed that metal ion toxicity could indeed be responsible for her symptoms. She obtained a second opinion from another orthopedic surgeon who reaffirmed the diagnosis. Before her surgery, she suffered a greater trochanteric fracture through the osteolytic lesion. A long discussion was conducted with the patient regarding revision surgery, especially given the fact that her femoral stem was well fixed and ingrown. Options including retaining the femoral stem and using a titanium sleeve versus complete femoral component exchange were discussed. Given her desire to remove all sources of metal debris from her body, we came to a bipartisan decision to perform complete revision of the femoral component. The patient underwent revision surgery within only a few months of her representation to our office, 12 years after her first revision, at age 45. The hip was approached through the previous posterior approach (Fig. 4a) which was lengthened distally to allow full access to the femur to perform an extended trochanteric osteotomy (ETO). After the hip was exposed and the prosthetic head disengaged, clear evidence of metallosis was encountered at the trunnion (Fig. 4b and c). Utilizing the ETO, the prosthesis was exposed and using a combination of flexible osteotomes, gigli saws, and implant removal instruments. The stem was removed with minimal bone loss (Fig. 4d). The hip was revised utilizing a Stryker Restoration (Stryker Inc., Kalamazoo, Michigan) revision stem (Fig. 5a and b). The stem is made of titanium alloy (Ti-6Al-4V) and we used a 36 +2.5mm ceramic head (Biolox delta Ceramic Femoral Head, CeramTec, Lauf, Germany). Postoperatively, the patient progressed well. By her 2-month follow-up visit, she reported complete resolution of her skin rash (Fig. 6). Her Co level was 3.2 mcg/L and her Cr was 4.3 mcg/L at 3 months postoperatively. At 6 months postoperatively, she stated her ability to think had improved. She healed her ETO without issue. 15 months after surgery, she noted subtle improvement regarding her POTS symptoms and remained symptom free with respect to her rash and mentation. She did, however, still have residual hip pain, attributable to a greater trochanter fracture nonunion, and she had persistent lower extremity paresthesia.
Figure 1.

The dermatological manifestations on the elbow (a) and hand (b) of the patient recorded in a pre-operative clinical visit.
Figure 2.

Pre-operative radiographs showed osteolysis at the medial calcar, greater trochanter, and the proximal femoral diaphysis.
Figure 3.
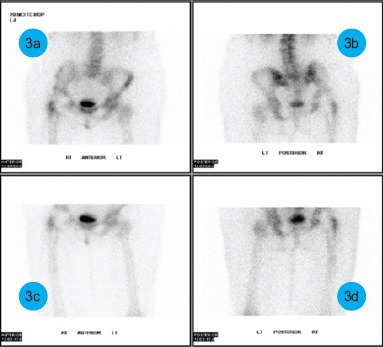
Pre-operative bone scan demonstrating increased activity in the peritrochanteric region of the proximal femur.
Figure 4.
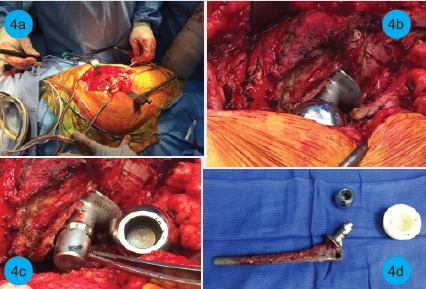
Intraoperative images demonstrate metallosis and evidence of trunnionosis. The approach to the implant (a), operative view of head and tissue around it (b), inspection of the neck showing trunnion wear with a black discoloration at the tip of the taper (c), and explanted femoral implant, head, and liner (d) are all shown.
Figure 5.
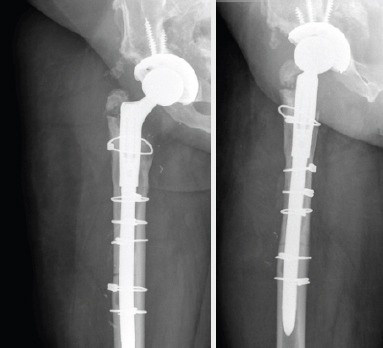
Anterior-posterior (a) and lateral (b) post-operative radiographs with Stryker Restoration femoral component.
Figure 6.

The patient presents for her 3-month follow-up visit demonstrating full resolution of her dermatological manifestations.
Discussion
While metal toxicity has been described in the arthroplasty literature, novel to this case is the occurrence of systemic pathology with only mildly elevated serum Co and Cr levels due to trunnion wear in a metal-on-polyethylene articulation. Furthermore, this represents the first report of clinically significant systemic metal toxicity linked to trunnion wear with the AML stem, though under revision circumstances, a widely implanted femoral stem with excellent long-term survivorship, and clinical outcomes reported at 20 years [11, 12]. Thresholds for concerning Co and Cr levels are still debated. For the evaluation of ALTR, some propose 4, 5, or 7 mcg/L as the cutoff for what should prompt further workup[10, 11, 13]. Systemic cobalt toxicity has been reported before with marginally elevated ion levels[14, 15], but levels <10 mcg/L should not lead to systemic symptoms[13]. Extensive laboratory studies were performed on our patient to evaluate for rheumatologic disorders, but in the end, the only notable findings were the patient’s dermatopathology and elevated Co and Cr levels. The patient’s dermatologist, rheumatologist, cardiologist, toxicologist, and two unaffiliated orthopedic surgeons all concurred that the patient’s presentation could be reflective of systemic metal ion toxicity. Reports of systemic symptoms in the setting of a metal-on-polyethylene articulation, with the causative source most likely wear at the head-neck junction, remain uncommon. A certain subset of patients may exist with clinical syndromes similar to the ones described in this case report whose symptoms could have been overlooked in the past. As in this case, these manifestations may be directly linked to chronic and low-level Co and Cr exposure. Consideration should be given to the possibility of trunnion wear in this stem as a cause of low-level metal toxicity. This becomes especially important in patients with similar clinical manifestations for whom the etiology of their symptoms have eluded definitive diagnosis.
Conclusion
This novel case of a 45-year-old female with the occurrence of systemic pathology with only mildly elevated serum cobalt (Co) and chromium (Cr) levels in a revised hip with metal-on-polyethylene articulation indicates that consideration should be given to metal ion toxicity due to trunnion wear, even with relatively low ion levels.
Clinical Message.
In patients experiencing dermatologic, neurologic, and cardiac symptoms following total hip arthroplasty with cobalt/chromium femoral components, consideration should be given to metal ion toxicity due to trunnion wear, even in patients with relatively low ion levels.
Biography



Footnotes
Conflict of Interest: Nil
Source of Support: Nil
Consent: The authors confirm that Informed consent of the patient is taken for publication of this case report
References
- 1.Goldberg JR, Gilbert JL. In vitro corrosion testing of modular hip tapers. J Biomed Mater Res B Appl Biomater. 2003;64:78–93. doi: 10.1002/jbm.b.10526. [DOI] [PubMed] [Google Scholar]
- 2.Royhman D, Patel M, Runa MJ, Jacobs JJ, Hallab NJ, Wimmer MA, et al. Fretting-corrosion in hip implant modular junctions:New experimental set-up and initial outcome. Tribol Int. 2015;91:235–45. doi: 10.1016/j.triboint.2015.04.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mistry JB, Chughtai M, Elmallah RK, Diedrich A, Le S, Thomas M, et al. Trunnionosis in total hip arthroplasty:A review. J Orthop Traumatol. 2016;17:1–6. doi: 10.1007/s10195-016-0391-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jennings JM, Dennis DA, Yang CC. Corrosion of the head-neck junction after total hip arthroplasty. J Am Acad Orthop Surg. 2016;24:349–56. doi: 10.5435/JAAOS-D-15-00111. [DOI] [PubMed] [Google Scholar]
- 5.Gill IP, Webb J, Sloan K, Beaver RJ. Corrosion at the neck-stem junction as a cause of metal ion release and pseudotumour formation. J Bone Joint Surg Br. 2012;94:895–900. doi: 10.1302/0301-620X.94B7.29122. [DOI] [PubMed] [Google Scholar]
- 6.Cooper HJ, Urban RM, Wixson RL, Meneghini RM, Jacobs JJ. Adverse local tissue reaction arising from corrosion at the femoral neck-body junction in a dual-taper stem with a cobalt-chromium modular neck. J Bone Joint Surg Am. 2013;95:865–72. doi: 10.2106/JBJS.L.01042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mao X, Tay GH, Godbolt DB, Crawford RW. Pseudotumor in a well-fixed metal-on-polyethylene uncemented hip arthroplasty. J Arthroplasty. 2012;27:493.e13–7. doi: 10.1016/j.arth.2011.07.015. [DOI] [PubMed] [Google Scholar]
- 8.Bradberry SM, Wilkinson JM, Ferner RE. Systemic toxicity related to metal hip prostheses. Clin Toxicol (Phila) 2014;52:837–47. doi: 10.3109/15563650.2014.944977. [DOI] [PubMed] [Google Scholar]
- 9.Wong CC, Nixon RL. Systemic allergic dermatitis caused by cobalt and cobalt toxicity from a metal on a metal hip replacement. Contact Dermatitis. 2014;71:113–4. doi: 10.1111/cod.12267. [DOI] [PubMed] [Google Scholar]
- 10.Zywiel MG, Cherian JJ, Banerjee S, Cheung AC, Wong F, Butany J, et al. Systemic cobalt toxicity from total hip arthroplasties:Review of a rare condition part 2. Measurement, risk factors, and step-wise approach to treatment. Bone Joint J. 2016;98-B:14–20. doi: 10.1302/0301-620X.98B1.36712. [DOI] [PubMed] [Google Scholar]
- 11.Engh CA, Jr, Claus AM, Hopper RH, Jr, Engh CA. Long-term results using the anatomic medullary locking hip prosthesis. Clinical orthopaedics and related research. 2001;393:137. doi: 10.1097/00003086-200112000-00016. [DOI] [PubMed] [Google Scholar]
- 12.Belmont PJ, Jr, Powers CC, Beykirch SE, Hopper RH, Jr, Engh CA, Jr, Engh CA, et al. Results of the anatomic medullary locking total hip arthroplasty at a minimum of twenty years. A concise follow-up of previous reports. J Bone Joint Surg Am. 2008;90:1524–30. doi: 10.2106/JBJS.G.01142. [DOI] [PubMed] [Google Scholar]
- 13.Paustenbach DJ, Galbraith DA, Finley BL. Interpreting cobalt blood concentrations in hip implant patients. Clin Toxicol (Phila) 2014;52:98–112. doi: 10.3109/15563650.2013.857024. [DOI] [PubMed] [Google Scholar]
- 14.Mao X, Wong AA, Crawford RW. Cobalt toxicityan emerging clinical problem in patients with metal-on-metal hip prostheses? Med J Aust. 2011;194:649–51. doi: 10.5694/j.1326-5377.2011.tb03151.x. [DOI] [PubMed] [Google Scholar]
- 15.Tower SS. Arthroprosthetic cobaltism:Neurological and cardiac manifestations in two patients with metal-on-metal arthroplasty:A case report. J Bone Joint Surg Am. 2010;92:2847–51. doi: 10.2106/JBJS.J.00125. [DOI] [PubMed] [Google Scholar]


