Abstract
Introduction:
Para-articular osteochondromas are rare osteocartilaginous tumors arising adjacent to the joint, more common around the knee. In contrast to osteochondroma, they occur in elderly patients.
Case Report:
We report a 60-year-old female with slow-growing, extraosseous soft tissue mass in the infrapatellar fat pad region with coexisting osteoarthritis. Total excision of the mass with total knee arthroplasty (TKA) done. The patient had excellent functional outcome with no recurrence at 2-year follow-up.
Conclusion:
The incidence of para-articular osteochondromas in elderly patients with coexisting osteoarthritis is very rare. Clinicoradiological features along with histopathology confirm its diagnosis. Total excision is the mainstay of treatment along with TKA if there is coexisting arthritis and its recurrence is very rare.
Keywords: Para-articular osteochondroma, Extraskeletal osteochondroma, Patellar tendinopathy, Hoffa’s disease
Learning Point of the Article:
Para-articular osteochondroma should be considered as a differential diagnosis in patients who present with extra-articular mass in the infra-patellar fat pad region of the knee.
Introduction
Osteochondroma is the most common benign tumor, usually presents in the metaphyseal area around the growth plate of long bones, and grows away from the joints in a growing skeleton [1]. In contrast, para-articular or juxta-articular osteochondroma is rare osteocartilaginous tumors present adjacent to the joint and more commonly appear in elderly patients [2, 3]. Osteochondral lesion in the infrapatellar fat pad region described as “Para-articular osteochondroma” by Milgram and Dunn, in 1980 [4]. Since then, different terminologies used to describe these para-articular masses such as patellar osteochondroma, intracapsular chondroma, para-articular chondroma, giant extrasynovial osteochondroma, Hoffa’s disease, and giant intra-articular osteochondroma [5, 6, 7, 8]. Most of the literature describe para-articular osteochondroma without osteoarthritis and in the younger patients. We report a patient with an extraosseous osteochondroma-like mass beneath the patellar tendon in the anterior portion of the knee joint with advanced osteoarthritis and restricted range of motion.
Case Report
A 60-year-old female presented with bilateral knee pain, right more than left for 10 years. She complains of pain affecting her daily activities and not able to bend the knee completely. She was aware of the mass which she noticed before 10 years and gradually progressed to attain the present size. There was no previous history of trauma, features suggestive of metabolic or rheumatoid disease. On clinical examination, bony hard mass felt just below the patella and the mass found moving with the patella. Range of motion was 25–90° with Grade II instability and varus deformity. Neurovascular examination was normal. Plain radiographs (Fig. 1a) revealed well-defined bony mass just below the patella just posterior to patellar tendon. Skyline view showed a mass medial to patella displacing the patella laterally. There was also collapse of medial joint space with opening of lateral joint space with marginal osteophytes suggestive of advanced osteoarthritis. Computed tomography scan (Fig. 1b) examination revealed well-circumscribed mass with pedicle attached to inferior pole of patella. Laboratory parameters were normal. Through midline longitudinal incision and medial parapatellar arthrotomy, joint cavity opened. Mass found lying behind the patellar tendon attached to inferior pole of patella. Mass totally resected carefully without damaging the patellar tendon. Mass was about 7 cm × 7 cm in size and covered with cartilage (Fig. 2). Then, total knee replacement done in standard manner(Fig.3). Weight-bearing started from post-operative day 1. Post-operative period was uneventful. The patient regained flexion and asymptomatic. Follow-up review at 2 years showed component in good alignment with no recurrence. Histopathological examination showed mature bony trabeculae surrounded by hyaline cartilage. There was no evidence of malignant features.
Figure 1.
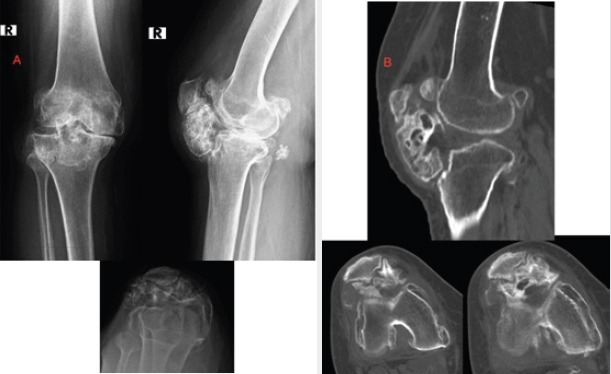
(a) Pre-operative radiograph showing para-articular osteochondroma involving the entire infrapatellar fat pad region and attached to inferior pole of patella with coexisting osteoarthritis. (b) Sagittal and axial computed tomography sections showing mass occupying the whole anterior knee joint cavity.
Figure 2.
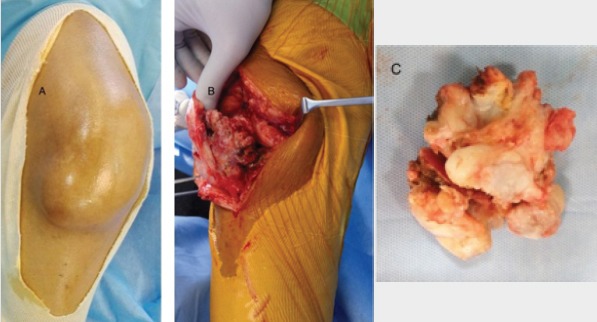
(a) Pre-operative clinical picture.(b)Intraoperative picture after arthrotomy showing the entire mass.(c)Excised mass.
Figure 3.

Post-operative follow-up radiograph showing removal of entire mass with total knee arthroplasty components in situ.
Discussion
Conventional osteochondromas develop from the bone that forms by endochondral ossification. They are solitary lesions, present more commonly around the knee, and grow away from the joint [1]. In contrast, extraskeletal osteochondroma comprises a group of tumors that arise from the soft tissues, commonly adjacent to the joint, and classified into synovial chondromatosis, soft tissue chondroma, and para-articular osteochondroma [9]. Para-articular osteochondroma of the knee is extra-articular and usually arises from infrapatellar fat pad region. Other common sites are hip, knee, foot, and elbow [3]. To avoid confusion in describing various terminologies associated with para-articular osteochondroma, Reith et al. [3] proposed diagnostic criteria which help to differentiate from other para-articular masses. The lesion typically arises as a single dominant mass from the soft tissues near the joint without synovial involvement and histologically similar to conventional osteochondroma. Various theories proposed regarding pathogenesis of para-articular osteochondroma such ascartilaginous metaplasia of the articular and para-articular connective tissue [9], metaplasia following traumatic event of Hoffa’s fat pad [10], and chronic impingement of the infrapatellar fat pad [6] but still controversial. In our patient, slow growth and 10-year duration to attain its present size were indicative of its benign nature. Patellar tendinopathy caused by a para-articular extraskeletal osteochondroma located in the infrapatellar region of the knee was described [11], but in our patient due to its very slow growth, tendinopathy not seen. In contrast to other case reports [2, 3], in our case, the bony mass found to be attached to the inferior pole of patella. Recurrences are extremely rare[2, 3]. Therefore, in these tumors, total excision of the mass represents the treatment of choice. We have done total resection and found no recurrence in the 2-year follow-up. The most common differential diagnosis for these lesions are synovial chondromatosis and low-grade chondrosarcoma. Careful histological and radiographic correlation helps to distinguish these tumors from the benign para-articular osteochondroma. Several authors reported no clinical or radiographic signs of degenerative joint disease after surgical resection of osteochondroma, although mild osteoarthritis may coexist in some cases [3, 9, 10]. Our patient had severe coexisting osteoarthritis, which required mass removal along with total knee arthroplasty (TKA). To the best of our knowledge, only one case report [12] published with coexisting severe osteoarthritis where they have done TKA.
Conclusion
The incidence of para-articular osteochondromas in elderly patients with coexisting osteoarthritis is very rare. Clinicoradiological features along with histopathology confirm its diagnosis. Total excision is the mainstay of treatment along with TKA if there is coexisting arthritis and its recurrence is very rare.
Clinical Message.
Para-articular osteochondroma should be considered as differential diagnosis in patients who present with extra-articular mass in the infrapatellar fat pad region of the knee. Clinicoradiological features and histopathology help to differentiate from other similar appearing lesions. Total excision of the mass is the treatment of choice and its recurrence is very rare.
Biography

Footnotes
Conflict of Interest: Nil
Consent: The authors confirm that Informed consent of the patient is taken for publication of this case report
Source of Support: Nil
References
- 1.Jaffe HL. Tumors and Tumorous Conditions of the Bones and Joints. Philadelphia, PA: Lea and Febiger; 1958. pp. 558–67. [Google Scholar]
- 2.Bombaci H, Bilgin E. Infrapatellar fat pad para-articular osteochondroma:A ten-year follow-up and review. Arch Trauma Res. 2015;4:e28381. doi: 10.5812/atr.28381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Reith JD, Bauer TW, Joyce MJ. Paraarticularosteochondroma of the knee:Report of 2 cases and review of the literature. ClinOrthopRelat Res. 1997;334:225–32. [PubMed] [Google Scholar]
- 4.Milgram JW, Dunn EJ. Para-articular chondromas and osteochondromas:A report of three cases. ClinOrthopRelat Res. 1980 May;(148):147–51. [PubMed] [Google Scholar]
- 5.Cohen AP, Giannoudis PV, Hinsche A, Smith RM, Matthews SJ. Post-traumatic giant intraarticular synovial osteochondroma of the knee. Injury. 2001;32:87–9. doi: 10.1016/s0020-1383(00)00090-5. [DOI] [PubMed] [Google Scholar]
- 6.Krebs VE, Parker RD. Arthroscopic resection of an extrasynovial ossifying chondroma of the infrapatellar fat pad:End-stage Hoffa's disease? Arthroscopy. 1994;10:301–4. doi: 10.1016/s0749-8063(05)80117-3. [DOI] [PubMed] [Google Scholar]
- 7.Sakai H, Tamai K, Iwamoto A, Saotome K. Para-articular chondroma and osteochondroma of the infrapatellar fat pad:A report of three cases. IntOrthop. 1999;23:114–7. doi: 10.1007/s002640050322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Böstman O, Karaharju E, Heikkonen L, Holmström T. Extraskeletal ossifying chondroma in the knee. A case report. ActaOrthopScand. 1985;56:87–9. doi: 10.3109/17453678508992989. [DOI] [PubMed] [Google Scholar]
- 9.Rodriguez-Peralto JL, Lopez-Barea F, Gonzalez-Lopez J. Intracapsular chondroma of the knee:An unusual neoplasm. Int J SurgPathol. 1997;5:49–53. [Google Scholar]
- 10.Rizzello G, Franceschi F, Meloni MC, Cristi E, Barnaba SA, Rabitti C, et al. Para-articular osteochondroma of the knee. Arthroscopy. 2007;23:910.e1–4. doi: 10.1016/j.arthro.2006.05.030. [DOI] [PubMed] [Google Scholar]
- 11.Ozturan KE, Yucel I, Cakici H, Guven M, Gurel K, Dervisoglu S, et al. Patellar tendinopathy caused by a para-articular/extraskeletal osteochondroma in the lateral infrapatellar region of the knee:A case report. Cases J. 2009;2:9341. doi: 10.1186/1757-1626-2-9341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pandian S, Jayaraman T, Rajendiran C. Osteochondromatosis and osteochondroma involving bilateral patella and patellar tendon:A case report. J OrthopSurg (Hong Kong) 2016;24:125–7. doi: 10.1177/230949901602400128. [DOI] [PubMed] [Google Scholar]


