Abstract
An analysis of data for 2014 about forty-four low-value health services in the Virginia All Payer Claims Database revealed more than $586 million in unnecessary costs. Among these low-value services, those that were low and very low cost ($538 or less per service) were delivered far more frequently than services that were high and very high cost ($539 or more). The combined costs of the former group were nearly twice those of the latter (65 percent versus 35 percent).
A substantial proportion of health care costs in the United States is allocated to low-value care, defined as patient care that provides no net health benefit in specific clinical scenarios—such as early diagnostic imaging for uncomplicated low-back pain.1–3 Despite decades of attention to this issue, US expenditures on low-value care persist.2–9 While many studies have focused on high-cost low-value services, such as arthroscopic knee surgery for osteoarthritis, few have examined which low-value services contribute the most to unnecessary costs. A better understanding of the distribution and costs associated with low-value care would inform ongoing efforts to reduce its provision.
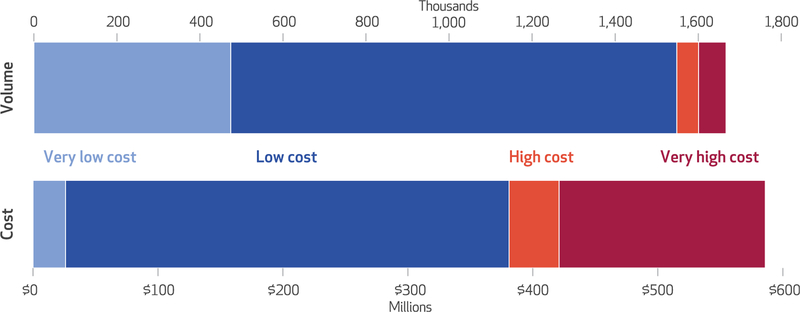
Using 2014 data from the Virginia All Payer Claims Database, we determined that 93 percent of services used were low cost ($100–$538 per service) and very low cost (less than $100) low-value services, compared to 7 percent that were high cost ($539–$1,315) and very high cost (more than $1,315) low-value services (Exhibit 1). The total cost for low- and very-low-cost services was nearly twice the total cost for high- and very-high-cost services (65 percent versus 35 percent).
EXHIBIT 1. Use and cost of low-value services in Virginia in 2014, by quartiles of cost.
SOURCE Authors’ analysis of data for 2014 from the Virginia All Payer Claims Database. NOTES “Low-value services” refers to forty-four specific health services in specific clinical settings from which the patient is expected to receive no net benefit. The costs for the quartiles of low-value services are less than $100 per very-low-cost service, $100–$538 per low-cost service, $539–$1,315 per high-cost service, and more than $1,315 per very-high-cost service. Costs are the average (mean) amount of money per service paid to a health care provider across all payers, including patients’ out-of-pocket spending, multiplied by the frequency of that service.
Study Data And Methods
The Virginia All Payer Claims Database includes administrative claims data about state residents insured through fee-for-service Medicare, Medicare Advantage, Medicaid, and private commercial insurers. We used claims from 2014, which included data for 5.5 million beneficiaries.
We examined forty-four pre-specified clinical services among those determined to be of low value by the ABIM Foundation’s Choosing Wisely campaign,10 the US Preventive Services Task Force,11 Medicare’s Healthcare Effectiveness Data and Information Set (HEDIS) criteria,12 and other clinical guidelines2 (for a list of the low-value clinical services used in this study, see online Appendix Exhibit 1).13 It is important to note that the forty-four services selected for this analysis likely represent a small portion of low-value care. We chose these services based on previous work6,7 and because their clinical attributes predicted a high degree of accuracy in differentiating between high- and low-value indications in the claims data—not for the services’ expected impact on reducing costs.
To quantify low-value care, we used the Milliman MedInsight Health Waste Calculator, a proprietary, algorithm-based software program designed to determine whether a particular use of a prespecified service was high value, potentially low value, or very likely low value.7,14 In this study we deemed a service to be low value if it was either potentially or very likely low value, according to the expert guidelines. For example, if cervical cancer screening was performed on a woman younger than age twenty-one, we considered it to be low value.15 For each of the forty-four services we calculated a waste index, defined as the number of low-value services divided by the number of total services. Appendix Exhibit 2 provides measure specifications for the five most commonly delivered low-value services.13 A detailed report about the low-value services for which data are included in the Virginia database is available elsewhere.16
We defined health care costs as the average (mean) amount of money paid to a health care provider for each service across all payers, public and private, and including patients’ out-of-pocket spending. The median cost of the forty-four low-value services we analyzed was $538. We categorized costs mathematically by dividing the services into quartiles by cost (two quartiles below and two quartiles above the median), as follows: quartile 1: very low cost (eleven services, typically labs or medications costing less than $100 each); quartile 2: low cost (eleven services, typically labs or medications costing $100–$538 each); quartile 3: high cost (eleven services, typically imaging exams costing $539–$1,315 each); and quartile 4: very high cost (eleven services, typically advanced diagnostic imaging or procedures costing more than $1,315 each).
Our data source had one principal limitation: Administrative data are an imperfect tool to use in measuring quality of care. Nonetheless, they represented our best opportunity to measure quality of care in large, representative samples, and they provided reasonable validity for a selected group of services.6
Study Results
VOLUME OF LOW-VALUE SERVICES
In 2014, Virginia beneficiaries received 5.4 million of the forty-four health care services measured (data not shown). Of these services, the algorithm determined that 1.7 million were low value and 3.7 million were high value (the aggregate waste index was about 31 percent). Among the 1.7 million low-value services, 1.6 million were low and very low cost (93 percent), compared with only about 119,000 such services that were high and very high cost (7 percent) (Exhibit 1). Approximately one in five of the 5.5 million beneficiaries received at least one low-value service in 2014.
COSTS OF LOW-VALUE SERVICES
The total cost for the low- and very-low-cost low-value services (65 percent of costs, or $381 million) was nearly twice as much as the total cost of high- and very-high-cost low-value services (35 percent of costs, or $205 million) (Exhibit 1). Six of the ten most expensive low-value services were low or very low cost (Exhibit 2). For example, low-cost preoperative lab testing for low-risk patients undergoing low-risk surgery accounted for nearly half of un-necessary spending (see Appendix Exhibit 1 for a full description of each service).13
EXHIBIT 2.
The 10 most costly low-value services in Virginia, 2014
| Low-value service | Mean cost per servicea | Total unnecessary costs (millions)b | Total services measured | Services deemed low value | Ranking by use | Waste indexc |
|---|---|---|---|---|---|---|
| Baseline lab tests for low risk patients having low-risk surgery | $487 | $227.8 | 595,552 | 467,884 | 1 | 78.6% |
| Stress cardiac or other cardiac imaging in low-risk, asymptomatic patients | $3,404 | $93.2 | 244,487 | 27,385 | 13 | 11.2% |
| Annual EKGs or other cardiac screening for low-risk, asymptomatic patients | $298 | $41.0 | 2,823,557 | 137,666 | 5 | 4.9% |
| Routine head CT scans for ED visits for severe dizziness | $1,569 | $24.6 | 29,816 | 15,724 | 15 | 52.7% |
| EKGs, chest x-rays, or pulmonary function tests in low-risk patients having low-risk surgery | $646 | $21.3 | 33,754 | 32,900 | 11 | 97.5% |
| Population-based screening for vitamin D deficiency | $125 | $20.6 | 165,034 | 165,031 | 4 | 100.0% |
| PSA-based screening for prostate cancer in all men, regardless of age | $144 | $18.9 | 341,554 | 131,419 | 6 | 38.5% |
| Routine imaging for uncomplicated acute rhinosinusitis | $2,365 | $17.1 | 14,196 | 7,220 | 19 | 50.9% |
| Routine annual cervical cancer screening in women ages 21–65 | $91 | $15.3 | 220,241 | 167,252 | 3 | 75.9% |
| Imaging for low-back pain within the first six weeks of symptom onset, in absence of red flags | $330 | $13.9 | 48,857 | 42,110 | 9 | 86.2% |
SOURCE Authors’ analysis of data for 2014 from the Virginia All Payer Claims Database. NOTES “Low-value services” are defined in the Notes to Exhibit 1. EKG is electrocardiogram. CT is computed tomography scan. ED is emergency department. PSA is prostate specific antigen.
Average (mean) amount of money per service paid to a health care provider across all payers (including patients’ out-of-pocket spending).
Mean cost per service multiplied by total number of low-value services.
Number of low-value services divided by the number of total services measured.
More than $586 million, or $9.90 per beneficiary per month, was spent unnecessarily on these low-value services, accounting for 2.1 percent of Virginia’s total health care costs—which were about $28 billion, according to information from the Virginia All Payer Claims Database.
Discussion
Shared, nonpartisan health policy goals are to improve quality of care, enhance patient experience, and lower health care costs in the United States. One straightforward strategy for achieving these goals is to identify, measure, and reduce the use of low-value care. Doing so has been elusive for many reasons, particularly because the value of a specific clinical service is not always high or low but depends upon who receives the service, who provides it, and where it is provided. Thus, a more nuanced approach to identifying the precise clinical circumstances where low-value care is delivered is warranted.
Using a large, statewide compendium of information about virtually all public and private insurance beneficiaries in Virginia, we analyzed forty-four low-value services to better identify specific clinical scenarios in which unnecessary costs occurred. An algorithm-driven software program analyzed 5.4 million health care services and found that 1.7 million of them were low value—which cost more than $586 million (2.1 percent of Virginia’s health care costs). Contrary to common belief, low- and very-low-cost low-value services (those costing less than $539 per service) were administered more than thirteen times more frequently than costlier low-value services. Although higher-cost low-value services are frequently showcased in policy deliberations and the media, lower-cost low-value services (those in the bottom two quartiles of our study) accounted for almost twice as much unnecessary cost as did services in the top two quartiles.
The cost distribution of low-value care should have important implications for policy makers, health care systems, and clinicians struggling to find better ways to reduce unnecessary costs without disappointing patients, disrupting practice norms, or reducing the quality of or access to care. Demonstrating the relative excessive use and costs of low-value services is particularly salient because these findings should indicate a pragmatic path to begin their reduction. Although changing any physician practice pattern (including the delivery of routine and low-cost services) is notoriously difficult, even a modest decrease in the use of low- and very-low-cost low-value services could lead to savings7,17 and serve as a feasible strategy for catalyzing a broader movement to tackle low-value care. A focus on reducing low- and very-low-cost services is likely to be less controversial than a policy that targets high- and very-high-cost services, because the former strategy would not present a financial threat to any particular clinical specialty or advocacy group.
The 2.1 percent of total statewide costs identified as unnecessary in this study might seem relatively small compared with previous estimates that 10–30 percent of health care costs are unnecessary.1,5,18 However, it is important to note that our cost estimates are conservative because they do not capture the downstream costs associated with low-value care. For example, an abnormal cardiac stress test in an asymptomatic, low-risk patient can lead to a low-value cardiac catheterization. Moreover, the services we analyzed do not capture the costs and use of all low-value care. Rather, they were chosen because they were most amenable to claims analysis, and they do not include even costlier services—such as low-value subspecialty visits or hospitalizations.19 Estimates of costs of low-value care will likely expand as additional services are identified, and as measurement tools transition from claims databases to electronic health records, which contain richer clinical data.19,20 As health care providers are increasingly held accountable for reducing unnecessary spending,21 future interventions to reduce low-value care should take advantage of the data in electronic health records. However, to be effective, such interventions must be data driven and thoughtful and must have widespread input and support from clinicians.19
Conclusion
Decreasing wasteful health care spending will reduce patient harm and improve the efficiency of delivery by shifting care away from low-value circumstances to clinical scenarios that improve patient-centered outcomes. Instead of pursuing a politically charged strategy to reduce the use of high-profile and higher-cost low-value services, an alternative approach that initially targets the reduction of high-volume and less costly items might be a more strategic way to catalyze the movement to tackle the problem of low-value care. These findings also suggest that in the aggregate, minor actions by all clinicians can have a sizable impact on reducing unnecessary health care spending.
Supplementary Material
Acknowledgments
This work was supported by a Centers for Medicare and Medicaid Services State Innovation Model Initiative (SIM) Grant (Grant No. 1G1CMS331384-01-00). Mark Fendrick is a codeveloper of the Milliman MedInsight Health Waste Calculator and receives royalties from its sale. He also serves as consultant to AbbVie, FMS Inc., Geisinger Health Plan, Janssen, Lilly, MedZed, Merck, Risalto, Sanofi, Sempre Health, Takeda, TriZetto, Wellth, and Zansors. The authors acknowledge the help of Carol Mauldin in citation management and administrative support.
Contributor Information
John N. Mafi, David Geffen School of Medicine, University of California, Los Angeles, and a natural scientist in health policy at the RAND Corporation, in Santa Monica, California..
Kyle Russell, Virginia Health Information, in Richmond..
Beth A. Bortz, CEO of the Virginia Center for Health Innovation, in Henrico..
Marcos Dachary, Milliman in Seattle, Washington..
William A. Hazel, Jr., Commonwealth of Virginia, in Richmond..
A. Mark Fendrick, Department of Internal Medicine, University of Michigan, in Ann Arbor..
NOTES
- 1.Institute of Medicine. Best care at lower cost: the path to continuously learning health care in America Washington (DC): National Academies Press; 2012. [PubMed] [Google Scholar]
- 2.Mafi JN, Wee CC, Davis RB, Landon BE. Comparing use of low-value health care services among U.S. advanced practice clinicians and physicians. Ann Intern Med 2016;165(4):237–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mafi JN, McCarthy EP, Davis RB, Landon BE. Worsening trends in the management and treatment of back pain. JAMA Intern Med 2013; 173(17):1573–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brook RH. Redefining health care systems [Internet] Santa Monica (CA): RAND Corporation; 2015. [cited 2017 Jul 20]. Available from: https://www.rand.org/content/dam/rand/pubs/corporate_pubs/CP700/CP788/RAND_CP788.pdf [Google Scholar]
- 5.Fisher ES, Wennberg DE, Stukel TA, Gottlieb DJ, Lucas FL, Pinder EL. The implications of regional variations in Medicare spending. Part 1: the content, quality, and accessibility of care. Ann Intern Med 2003;138(4): 273–87. [DOI] [PubMed] [Google Scholar]
- 6.Schwartz AL, Landon BE, Elshaug AG, Chernew ME, McWilliams JM. Measuring low-value care in Medicare. JAMA Intern Med 2014; 174(7):1067–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Reid RO, Rabideau B, Sood N. Low-value health care services in a commercially insured population. JAMA Intern Med 2016;176(10):1567–71. [DOI] [PubMed] [Google Scholar]
- 8.Mafi JN, Edwards ST, Pedersen NP, Davis RB, McCarthy EP, Landon BE. Trends in the ambulatory management of headache: analysis of NAMCS and NHAMCS data 1999–2010. J Gen Intern Med 2015; 30(5):548–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mafi JN, Wee CC, Davis RB, Landon BE. Association of primary care practice location and ownership with the provision of low-value care in the United States. JAMA Intern Med 2017;177(6):838–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Choosing Wisely [home page on the Internet] Philadelphia (PA): Choosing Wisely; [cited 2017 Jul 20]. Available from: http://www.choosingwisely.org/ [Google Scholar]
- 11.US Preventive Services Task Force [home page on the Internet] Rockville (MD): USPSTF; 2017. June [cited 2017 Jul 20]. Available from: http://www.uspreventiveservicestaskforce.org/ [Google Scholar]
- 12.National Committee for Quality Assurance. HEDIS 2014 technical specifications for physician measurement: summary table of measure changes [Internet] Washington (DC): NCQA; [cited 2017 Jul 20]. Available from: http://www.ncqa.org/Portals/0/HEDISQM/HEDIS2014/HEDIS_2014%20_List_of_Physician_Measures.pdf [Google Scholar]
- 13.To access the Appendix, click on the Details tab of the article online.
- 14.Milliman. MedInsight tools: Health Waste Calculator [Internet] Seattle (WA): Milliman; c 2017. [cited 2017 Jul 20]. Available from: http://www.medinsight.milliman.com/MedInsight/Products/Medinsight-Tools/?prid=71832 [Google Scholar]
- 15.US Preventive Services Task Force. Cervical cancer: screening: recommendation summary [Internet] Rockville (MD): USPSTF; 2012. March [cited 2017 Jul 20]. Available from: https://www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/cervical-cancer-screening [Google Scholar]
- 16.Virginia Health Information. Virginia APCD MedInsight Health Waste Calculator results: version 2.0 [Internet] Henrico (VA): Virginia Center for Health Innovation; 2016. January [cited 2017 Jul 20]. Available from: http://www.vahealthinnovation.org/wp-content/uploads/2016/10/Virginia-APCD-MedInsight-Health-Waste-Calculator-Results-v2.0.pdf [Google Scholar]
- 17.McWilliams JM, Schwartz AL. Focusing on high-cost patients—the key to addressing high costs? N Engl J Med 2017;376(9):807–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Phillips RL Jr, Petterson SM, Bazemore AW, Wingrove P, Puffer JC. The effects of training institution practice costs, quality, and other characteristics on future practice. Ann Fam Med 2017;15(2):140–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mafi JN, Edwards ST. How can we improve the efficiency of specialty care? J Gen Intern Med 2016; 31(11):1267–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Murff HJ, FitzHenry F, Matheny ME, Gentry N, Kotter KL, Crimin K, et al. Automated identification of postoperative complications within an electronic medical record using natural language processing. JAMA 2011;306(8):848–55. [DOI] [PubMed] [Google Scholar]
- 21.Centers for Medicare and Medicaid Services. Quality Payment Program [home page on the Internet] Balti-more (MD): CMS; [cited 2017 Jul 20]. Available from: https://qpp.cms.gov/ [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.