Abstract
With a resurgence of syphilis with human immunodeficiency virus (HIV) infection in last few years, various ocular manifestations of syphilis have been described in literature. This case report described an HIV-positive patient on anti-retroviral therapy who was diagnosed and treated for posterior uveitis secondary to ocular syphilis in the recent past presented to our clinic with cystoid macular edema (CME). CME, which did not respond to periocular corticosteroid, resolved with intravitreal sustained release dexamethasone implant. There was a recurrence CME 9 months later and repeat injection of intravitreal implant showed complete resolution. A long-term follow-up did not reveal reactivation of the infection with intravitreal corticosteroid. Intravitreal sustained release dexamethasone implant can be an effective treatment for refractory CME in patients with regressed syphilitic uveitis.
Keywords: Cystoid macular edema, human immunodeficiency virus, intravitreal corticosteroid, ocular syphilis, rapid plasma reagin
With a resurgence of syphilis with human immunodeficiency virus (HIV) infection in last few years, various ocular manifestations of syphilis have been described in literature.[1,2] Syphilis is a great masquerader and has plethora of presentations.[3] Cystoid macular edema (CME) has been described in association with neurosyphilis.[4] Macular edema was one of the leading factors associated with worse initial visual acuity in a series of patients with ocular syphilis.[5] CME following resolution of primary lesions of ocular syphilis is rare, but has been reported in literature.[6,7,8] Management of inflammatory CME secondary to infectious disease process always remains a challenge for the ophthalmologists. The chances of reactivation of the infection with local use of immunosuppressive often precludes the use of intravitreal corticosteroid. We describe herein the case of a HIV-positive patient who presented with inflammatory CME secondary to ocular syphilis and was subsequently treated with intravitreal dexamethasone sustained-release implant.
Case Report
A 30-year-old, known HIV-positive male, who was diagnosed and treated as syphilitic posterior uveitis earlier, came for a follow-up visit with blurring of vision in right eye for last one month. His rapid plasma reagin (RPR) was reactive for a titre of 1:128 and Treponema pallidum hemagglutination test was positive. He had already completed 14 days of intravenous penicillin G along with continuation highly active antiretroviral therapy (HAART). His CD4 count showed a rise from 160 cells/mm3 at initial presentation to 309 cells/mm3. On examination, his best corrected visual acuity (BCVA) in right eye was 6/18 and 6/6 in left eye. Slit-lamp examination of both eyes was unremarkable. Intraocular pressure (IOP) measured with Goldman applanation tonometry in both eyes was 12 mm of Hg. Fundus examination of the both eyes revealed pallor of the disc and sclerosed vessels with areas of chorioretinal atrophy and right eye had cystoid macular edema (CME) with minimal vitritis (Grade 1) [Fig. 1]. Spectral domain optical coherence tomography (OCT) confirmed the presence CME with a foveal thickness of 672 μ in right eye [Fig. 2a]. A posterior subtenon injection of triamcinolone acetonide (40 mg in 1 mL) was administered in right eye and he was advised to continue oral corticosteroid (40 mg/day) in tapering doses. He was seen again after 1 month, when his BCVA in right eye was 6/15 and a repeat RPR revealed a decreased titre of 1:4. Intraocular pressures were 16 mm Hg in right eye and 17 mm Hg in the left eye. Fundus examination of the right eye revealed persistent CME, which was confirmed by OCT with a decrease of foveal thickness 596 μ [Fig. 2b]. Intravitreal injection of sustained-release dexamethasone implant (Ozurdex®) was administered in the right eye. The patient came back after a month with an improvement in his BCVA in right eye, which was recorded 6/9. Clinical examination and subsequent OCT of the right eye revealed a resolving CME [Fig. 3a and b] with a decrease in foveal thickness to 201 μ [Fig. 2c]. His IOP was recorded 34 mm Hg in right eye and 16 mm of Hg in the left eye, for which he was started on topical anti-glaucoma medications. At subsequent follow up after 4 months of post-Ozurdex® injection, patient's vision was maintained at 6/9 and his IOP in right eye was under control with medications. His CD4 count was 347 cells/mm3. The patient returned to the clinic after nine months of intravitreal injection with a similar complaint of blurred vision in right eye. BCVA of the right eye was 6/12. Fundus examination of the right eye revealed CME, which was also confirmed by OCT with an increase in foveal thickness (565 μ) [Fig. 2d]. His IOP in right eye was 13 mm of Hg with anti-glaucoma medications. Second dose of intravitreal injection of Ozurdex® was administered in right eye. Fundus examination of the right eye after a month showed a resolved CME [Fig. 3c and d]. with decrease in foveal thickness to 189 μ in OCT [Fig. 2e]. Intraocular pressure in the right eye was 16 mm of Hg with one-drug anti-glaucoma medication. He is under follow-up with us for last 8 months and did not have any recurrence of CME or inflammation till date.
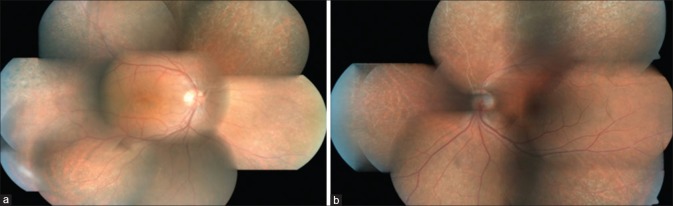
Figure 1.
(a) Fundus photo showing pallor of the disc and sclerosed vessels with areas of chorioretinal atrophy with vitritis and cystoid macular edema (CME) in the right eye at presentation (b) Fundus photo showing pallor of the disc and sclerosed vessels with areas of chorioretinal atrophy in the left eye
Figure 2.
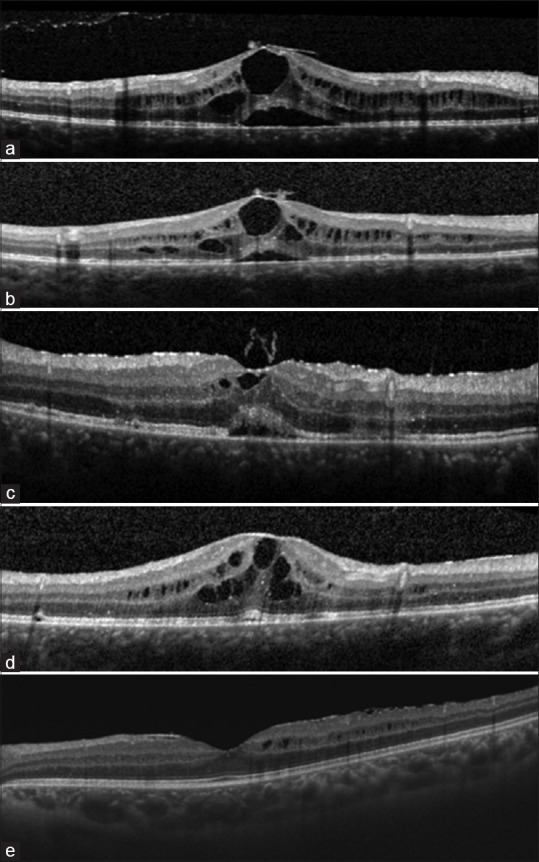
Serial optical coherence tomography (OCT) of the right eye (a) at presentation with cystoid macular edema (CME) (b) after 1-month of posterior subtenon injection in right eye; (c) resolving CME after 1-month of intravitreal injection of sustained release dexamethasone implant (Ozurdex®); (d) recurrence of CME 9 months after first injection of Ozurdex®; (e) resolution of CME 1-month after second intravitreal injection of sustained release dexamethasone implant
Figure 3.
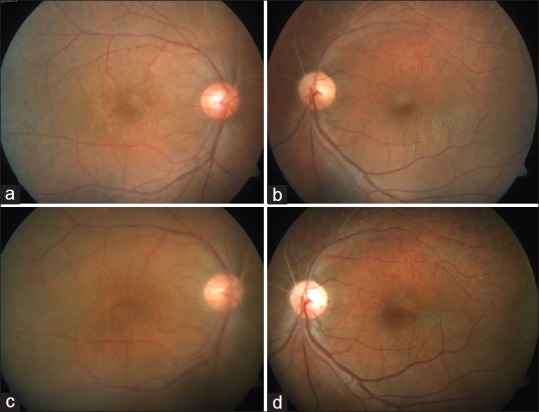
Fundus photograph of the right and left eye after 1 month of first (a and b) and second (c and d) intravitreal injection of sustained release dexamethasone implant (Ozurdex®
Discussion
The index case report represents a challenging case scenario where intravitreal sustained-release dexamethasone implant was proved to be a useful adjuvant in the management of CME secondary to a healed infectious disease process treated with proper and effective anti-microbial therapy. The introduction of Highly Active Antiretroviral Therapy (HAART) has resulted in stronger immunity in patients with HIV infection. However, patients who have had cytomegalovirus (CMV) retinitis can experience an increase in intraocular inflammation causing immune-recovery uveitis (IRU) and is the leading cause of severe vision loss in these patients. A possibility of CME due to IRU-like phenomenon can also be considered in our patient.[9] A step-wise approach was followed while managing CME in our patients. The CME in our patient did not respond to initial therapy with topical non-steroidal anti-inflammatory, periocular corticosteroid and oral corticosteroid. A complete resolution of ocular syphilis was achieved as evident by clinical findings and lower titres of RPR. Intravitreal corticosteroid may be an effective approach in the management of inflammatory CME in ocular syphilis, if the initial infection is treated properly and effectively.[7,10] Intravitreal corticosteroid with concomitant anti-CMV treatment has been also reported in the management of CME secondary to IRU in HIV positive patients with CMV retinitis.[11] Reports on the use of sustained release intravitreal dexamethasone implant as an adjuvant for the treatment for CME secondary to syphilitic uveitis are sparse.[7,12] Lautredou et al.[7] reported successful management of a case of CME in a HIV-positive patient, which was resistant to three subsequent sub-tenon injections and topical, oral steroid. Another retrospective analysis, which assessed the safety and efficacy of intravitreal dexamethasone implants on eight eyes from seven patients with infectious uveitis which also included a case of ocular syphilis.[12] Visual acuity improved in all the eyes with complete resolution of macular edema. There were no cases of reactivation of the infectious ocular disease.[12]
Management of cystoid macular edema following infectious uveitis is challenging. Unfortunately, even with robust advancements in therapeutics and diagnostic modalities, there is no definitive and completely effective treatment for uveitic CME till date and lack of proper understanding of the pathogenesis of CME in patients with uveitis is partly responsible for it.[13] Nonsteroidal anti-inflammatory drugs, corticosteroids, immunosuppressive and biological agents have all been used to treat uveitic CME; however, literature on the management of uveitic CME secondary to infectious disease is sparse. For recalcitrant cases of uveitic CME, acetazolamide[14] vitrectomy[15,16] intravitreal corticosteroid[17] and biological agents[18] have been reported. However, agents which lowers the host immunity due to immunosuppressive action, need to be used with caution in patients with infectious uveitis. Vitrectomy may be another good alternative in these situation where removal of bulk of vitreous itself may reduce the load of inflammatory cytokine resulting in resolution of uveitic CME. Various studies have reported to have a beneficial effect of pars plana vitrectomy on the course of uveitis and associated CME.[19] However the role of vitrectomy in the management of CME following infectious uveitis remains largely unexplored and proper studies are needed to define the role and indications of vitrectomy in these patients.
As we report about successful use of intravitreal sustained-release dexamethasone implant for persistent, recalcitrant uveitic CME in a HIV patient on HAART therapy with regressed syphilitic uveitis, our observation should be interpreted cautiously and translated in clinical practice. Use of intravitreal corticosteroid in infectious uveitis is not advocated through this report and one should be very careful as there are plenty of evidences on unmasking of ocular syphilis following intravitreal corticosteroid injection for the management of CME.[20,21] To conclude, intravitreal dexamethasone implant can be successfully used for the treatment of persistent cystoid macular edema in healed ocular syphilis.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Chao JR, Khurana RN, Fawzi AA, Reddy HS, Rao NA. Syphilis: Reemergence of an old adversary. Ophthalmology. 2006;113:2074–9. doi: 10.1016/j.ophtha.2006.05.048. [DOI] [PubMed] [Google Scholar]
- 2.Doherty L, Fenton KA, Jones J, Paine TC, Higgins SP, Williams D, et al. Syphilis: Old problem, new strategy. BMJ. 2002;325:153–6. doi: 10.1136/bmj.325.7356.153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dutta Majumder P, Chen EJ, Shah J, Ching Wen Ho D, Biswas J, See Yin L, et al. Ocular syphilis: An update. Ocul Immunol Inflamm. 2017;11:1–9. doi: 10.1080/09273948.2017.1371765. [DOI] [PubMed] [Google Scholar]
- 4.Martin NF, Fitzgerald CR. Cystoid macular edema as the primary sign of neurosyphilis. Am J Ophthalmol. 1979;88:28–31. doi: 10.1016/0002-9394(79)90747-5. [DOI] [PubMed] [Google Scholar]
- 5.Balaskas K, Sergentanis TN, Giulieri S, Guex-Crosier Y. Analysis of significant factors influencing visual acuity in ocular syphilis. Br J Ophthalmol. 2011;95:1568–72. doi: 10.1136/bjo.2010.194498. [DOI] [PubMed] [Google Scholar]
- 6.Halperin LS, Lewis H, Blumenkranz MS, Gass JD, Olk RJ, Fine SL. Choroidal neovascular membrane and other chorioretinal complications of acquired syphilis. Am J Ophthalmol. 1989;108:554–62. doi: 10.1016/0002-9394(89)90433-9. [DOI] [PubMed] [Google Scholar]
- 7.Lautredou CC, Hardin JS, Chancellor JR, Uwaydat SH, Ellabban AA, Sallam AB. Repeat intravitreal dexamethasone implant for refractory cystoid macular edema in syphilitic uveitis. Case Rep Ophthalmol Med 2018. 2018:7419823. doi: 10.1155/2018/7419823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fonollosa A, Giralt J, Pelegrín L, Sánchez-Dalmau B, Segura A, García-Arumí J, et al. Ocular syphilis—back again: Understanding recent increases in the incidence of ocular syphilitic disease. Ocul Immunol Inflamm. 2009;17:207–12. doi: 10.1080/09273940902741709. [DOI] [PubMed] [Google Scholar]
- 9.Urban B, Bakunowicz-Łazarczyk A, Michalczuk M. Immune recovery uveitis: pathogenesis, clinical symptoms, and treatment. Mediators Inflamm 2014. 2014:971417. doi: 10.1155/2014/971417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Solebo AL, Westcott M. Corticosteroids in ocular syphilis. Ophthalmology. 2007;114:1593. doi: 10.1016/j.ophtha.2007.04.017. [DOI] [PubMed] [Google Scholar]
- 11.Hu J, Coassin M, Stewart JM. Fluocinolone acetonide implant (Retisert) for chronic cystoid macular edema in two patients with AIDS and a history of cytomegalovirus retinitis. Ocul Immunol Inflamm. 2011;19:206–9. doi: 10.3109/09273948.2010.538120. [DOI] [PubMed] [Google Scholar]
- 12.Fonollosa A, Llorenç V, Artaraz J, Jimenez B, Ruiz-Arruza I, Agirrebengoa K, et al. Safety and efficacy of intravitreal dexamethasone implants in the management of macular edema secondary to infectious uveitis. Retina Phila Pa. 2016;36:1778–85. doi: 10.1097/IAE.0000000000001001. [DOI] [PubMed] [Google Scholar]
- 13.Markomichelakis NN, Halkiadakis I, Pantelia E, Georgalas I, Georgalas E, Chrysanthi K, et al. Course of macular edema in uveitis under medical treatment. Ocul Immunol Inflamm. 2007;15:71–9. doi: 10.1080/09273940701244509. [DOI] [PubMed] [Google Scholar]
- 14.Whitcup SM, Csaky KG, Podgor MJ, Chew EY, Perry CH, Nussenblatt RB. A randomized, masked, cross-over trial of acetazolamide for cystoid macular edema in patients with uveitis. Ophthalmology. 1996;103:1054–62. doi: 10.1016/s0161-6420(96)30567-8. discussion 1062-1063. [DOI] [PubMed] [Google Scholar]
- 15.Dugel PU, Rao NA, Ozler S, Liggett PE, Smith RE. Pars plana vitrectomy for intraocular inflammation-related cystoid macular edema unresponsive to corticosteroids. A preliminary study. Ophthalmology. 1992;99:1535–41. doi: 10.1016/s0161-6420(92)31769-5. [DOI] [PubMed] [Google Scholar]
- 16.Wiechens B, Nölle B, Reichelt JA. Pars-plana vitrectomy in cystoid macular edema associated with intermediate uveitis. Graefes Arch Clin Exp Ophthalmol Albrecht Von Graefes Arch Klin Exp Ophthalmol. 2001;239:474–81. doi: 10.1007/s004170100254. [DOI] [PubMed] [Google Scholar]
- 17.Antcliff RJ, Spalton DJ, Stanford MR, Graham EM, Ffytche TJ, Marshall J. Intravitreal triamcinolone for uveitic cystoid macular edema: An optical coherence tomography study. Ophthalmology. 2001;108:765–72. doi: 10.1016/s0161-6420(00)00658-8. [DOI] [PubMed] [Google Scholar]
- 18.Markomichelakis NN, Theodossiadis PG, Pantelia E, Papaefthimiou S, Theodossiadis GP, Sfikakis PP. Infliximab for chronic cystoid macular edema associated with uveitis. Am J Ophthalmol. 2004;138:648–50. doi: 10.1016/j.ajo.2004.04.066. [DOI] [PubMed] [Google Scholar]
- 19.Henry CR, Becker MD, Yang Y, Davis JL. Pars plana vitrectomy for the treatment of uveitis. Am J Ophthalmol. 2018;190:142–9. doi: 10.1016/j.ajo.2018.03.031. [DOI] [PubMed] [Google Scholar]
- 20.Erol N, Topbas S. Acute syphilitic posterior placoid chorioretinitis after an intravitreal triamcinolone acetonide injection. Acta Ophthalmol Scand. 2006;84:435. doi: 10.1111/j.1600-0420.2005.00641.x. [DOI] [PubMed] [Google Scholar]
- 21.Mushtaq B, Gupta R, Elsherbiny S, Murray PI. Ocular syphilis unmasked following intravitreal triamcinolone injection. Ocul Immunol Inflamm. 2009;17:213–5. doi: 10.1080/09273940902745411. [DOI] [PubMed] [Google Scholar]