Abstract
Purpose:
The aim of the current study was to compare visco-trabeculotomy (VT) with standard trabeculectomy with mitomycin C (Trab-MMC) in the treatment of quiescent neovascular glaucoma (NVG).
Methods:
The study was conducted on 51 eyes of 51 patients presenting with NVG and treated at an Ophthalmic Center in Egypt between March 2014 and April 2017. All study eyes were subjected to a standard protocol of intravitreal injection of ranibizumab followed by panretinal photocoagulation. Eyes were then randomized to either VT or Trab-MMC. Study eyes were followed up for at least 18 months. Success was defined as an intraocular pressure of ≤21 mm Hg and without vision-threatening complications. Complications were noted.
Results:
The mean ± SD (range, median) age of the study patients was 54.1 ± 6.4 (40–67, 54.5) and 52.4 ± 8.8 (38–66, 53) years in the VT (26 eyes) and Trab-MMC (25 eyes) groups, respectively (P = 0.45). The mean ± SD (range, median) intraocular pressure (IOP) of the study eyes was 45.19 ± 2.97 (39–52, 45.5) and 45.64 ± 3.56 (3–53, 45) mm Hg on maximal medical therapy in the VT and Trab-MMC groups, respectively (P = 0.61). At 18 months’ follow-up, the mean ± SD (range, median) IOP of the study eyes was 18.19 ± 2.0 (16–23, 17) and 19.92 ± 2.6 (18–26, 19) mm Hg in the VT and Trab-MMC groups, respectively (P = 0.004). There was no difference in postoperative antiglaucoma medication between the 2 groups (P = 0.62). Complications included hyphema and Descemet split in the VT group and an IOP spike in the Trab-MMC group. Success rates were 84.6% and 80% in the VT and Trab-MMC groups, respectively (P = 0.726).
Conclusions:
Both VT and Trab-MMC groups are effective in reducing the IOP in cases of NVG after control of neovascularization with anti-vascular endothelial growth factor and pan retinal photocoagulation.
Keywords: mitomycin C, neovascular glaucoma, panretinal photocoagulation, ranibizumab, visco-trabeculotomy, trabeculectomy
Neovascular glaucoma (NVG) is the term reserved for the subset of glaucomas in which proliferation of a fibrovascular tissue is the culprit behind intraocular pressure (IOP) elevation.1 The most common inciting factor for the neovascular proliferation is retinal ischemia,2 which results in the production of vasoproliferative factors, most notably vascular endothelial growth factor (VEGF).3 Obstruction of aqueous outflow, initially by the fibrovascular proliferation and eventually by synechial angle closure, results in IOP elevation. Treatment of this difficult type of glaucoma necessitates the management of the cause (the retinal ischemia stimulating VEGF production) and the effect (the elevated IOP). The current standard treatment for neovascularization of the retina (not elsewhere and not NVG) is the intravitreal injection of anti-VEGF agents4,5 like ranibizumab, bevacizumab, and others, coupled with ablation of the ischemic retina, classically by panretinal photocoagulation (PRP). Although this therapy generally abolishes the stimulus for neovascularization, it does not usually bring about reduction of the IOP which necessitates definitive surgery. Available options include filtering surgery with antimetabolites,6 glaucoma drainage devices,7 and cyclodestructive procedures.8 Variable success rates have been reported with surgery for NVG. As the pathology may—at least in part—be present in the angle, it would be reasonable to hypothesize that an angle procedure may provide a solution to this refractory elevation of IOP, and given the possibility of compromised corneal clarity (edema), ab-externo angle surgery could be a viable option. This study was conducted to compare trabeculotomy ab-externo assisted with ophthalmic viscosurgical device [also known as visco-trabeculotomy (VT)] with standard trabeculectomy with antimetabolite (mitomycin C) (Trab-MMC) in the treatment of quiescent NVG (after anti-VEGF and PRP).
METHODS
The study was conducted on 51 eyes of 51 patients diagnosed with NVG attending Mansoura Ophthalmic Center in Mansoura, Egypt, between March 2014 and April 2017. The study was approved by the ethics committee of the Faculty of Medicine of Mansoura University and all the study participants gave written informed consent for participation in the study. Inclusion criteria included patients with NVG who demonstrated neovascularization of the iris and/or the anterior chamber (AC) angle, goniosynechia that was <360 degrees, IOP >30 mm Hg on maximal tolerated topical and systemic IOP-lowering therapy, and with no apparent dense media opacity that would preclude adequate delivery of laser energy to the retina. Patients with concomitant ocular disease (eg, tractional retinal detachment) were excluded, and patients with poor general condition or those not willing or unable to attend the follow-up period of the study. The study patients were subjected to thorough history-taking including patient demographics (age, sex), general medical condition (eg, systemic diseases such as diabetes and hypertension), history of surgical interventions including previous retinal laser therapy, and medication use, including IOP-lowering therapy. We conducted ophthalmic examination including best-corrected visual acuity (BCVA) testing (logMAR) and slit lamp examination of the anterior segment to ascertain the diagnosis of NVG. We also evaluated the angle of the AC using gonioscopy and fundus examination by indirect ophthalmoscopy. If both eyes of a patient were eligible for inclusion, only 1 eye was randomly chosen in the study.
All study eyes then received intravitreal injection of ranibizumab (IVR) according to the standard protocol. In brief, topical levofloxacin eye drops were prescribed for 3 days before the injection which was conducted under sterile conditions in the operating room under topical anesthesia. After prepping of the skin, 0.5 mg/0.05 mL of ranibizumab (Lucentis, Novartis, Basel, Switzerland) was injected into the vitreous cavity through the pars plana, 4 mm posterior to the limbus using a 30 G needle taking care to compress slightly the injection site after needle withdrawal. A paracentesis was performed only if the IOP was precipitously elevated by digital palpation. Patients were continued on the same preoperative antibiotics for 2 weeks and on their previous topical IOP-lowering therapy.
One week after IVR, PRP was applied in 2 to 3 sessions over 6 to 8 days with the following parameters: 200 to 300 ms pulse duration, 200 to 500 μm spot size, and 200 to 400 mW power. Every session involved the application of 800 to 1000 shots attempting to cover the whole peripheral retina. All IVR and PRP (and subsequent surgeries) were performed by the same Professor of Ophthalmology (ASE). Patients were then randomized (2 weeks after the date of the IVR, about 1 week after the PRP) to receive either of the 2 surgical procedures: VT or Trab-MMC. The surgical techniques are already reported in previous studies.9–12 In brief, in Trab-MMC, trabeculectomy was performed through a limbal-based conjunctival flap, followed by creation of a 3 × 4 rectangular half-thickness sclera flap. MMC was applied in a concentration of 0.03% for 3 minutes through soaked surgical sponge inserted underneath the conjunctival flap and spread of a large surface area posterior to the limbus and planned scleral flap site then thoroughly irrigated by 200 mL of sterile normal saline. The procedure was completed in the usual manner with both sclera and conjunctiva closed by 10/0 nylon sutures. Postoperative treatment consisted of topical steroids and antibiotics for 2 weeks followed by gradual taper of steroids over 5 weeks.
For VT patients a partial thickness triangular (4 mm side) scleral flap was created. Schlemm canal was identified by radial incisions at the limbus, cannulated, and both open ends injected with high viscosity sodium hyaluronate (Healon GV, Pfizer, NY). Right and left trabeculotomies ensued using Harms trabeculotome and were followed by 10/0 nylon suture closure of the scleral and conjunctival flaps. Postoperative treatment was the same in both groups. Cycloplegia was used 3 times a day only for the first postoperative week. A topical beta-blocker (timolol) with or without a carbonic anhydrase inhibitor (dorzolamide) eye drops was used twice daily to control any postoperative IOP spike.
Patients were followed up at day 1 and day 7 for early postoperative events, then at months 1, 2, 3, 6, 9, 12, and 18. IOP was measured as part of the routine ophthalmic examination; complications were noted and managed accordingly.
Success was defined as an IOP of 6 to 21 mm Hg without any vision-threatening complications and without the need for additional glaucoma surgical procedures, whether this was achieved with (qualified success, with IOP-lowering medications) or without (true success, without IOP-lowering medications) IOP-lowering therapy.
Data were analyzed with IBM SPSS version 20. Repeated measure analysis of variance and paired t tests were used to compare between the preoperative and postoperative variables in each group. The comparison between the 2 groups was done by independent samples t test for numerical variables and χ2 test for categorical variables. Fisher exact P values were chosen where there was an expected count of <5. Kaplan-Meier survival curves were plotted to estimate the mean survival time and probabilities of failure at different follow-up stages in both groups. For all tests, a P value of <0.05 was considered significant.
RESULTS
The study was conducted on 51 eyes (27 right) of 51 patients (28 males) presenting with NVG and treated at Mansoura Ophthalmic Center in Mansoura, Egypt. The patient demographics and baseline clinical characteristics are presented in Table 1. There was no statistically significant differences between the 2 groups regarding the age (P = 0.45), follow-up duration (P = 0.58), IOP treated (P = 0.63) and untreated (P = 0.61), BCVA (P = 0.9), and glaucoma diagnosis (P = 1.0). Gonioscopy of the study eyes reveals neovascularization of the angle in 24 eyes (92%) in VT and in 22 eyes (88%) in Trab-MMC and peripheral anterior synechia in 9 eyes (35%) of the study eyes in either group. Table 2 demonstrates the IOP preoperatively and at different follow-up time points. There was a statistically significant reduction of IOP from the preoperative values in both groups at all follow-up time points. There was no statistically significant difference between both study groups at months 1, 2, and 3, whereas at 6, 9, 12, and 18 months of follow-up time points, the reduction in IOP in VT was statistically significantly lower than in Trab-MMC (P = 0.001, 0.01, 0.02, and 0.004, respectively). The preoperative and postoperative IOP values for both groups are shown in Figures 1–3. Table 3 demonstrates the status of the study eyes at the end of the study duration of 18 months. There was a statistically significant reduction in the number of IOP-lowering medications compared with the preoperative values in both groups (P < 0.005), whereas there was no statistically significant change in BCVA from the preoperative values in both groups (P = 0.034 and P = 0.046). There was no statistically significant difference between the 2 groups regarding the number of IOP-lowering medications (P = 0.62) and BCVA (P = 0.66) at the end of 18 months. Qualified success was noticed in about one-third of the study eyes and true success in about half of the study eyes in either group. Failure was noticed in 15% and 20% of VT and Trab-MMC, respectively. The cumulative probability of success in VT group was 96.2% at 9 months, 88.5% at 12 months, and 84.6% at 18 months and in Trab-MMC group was 100% at 9 months, 84% at 12 months, and 80% at 18 months. Figure 4 demonstrates the Kaplan-Meier survival curves for both study groups. There was no statistically significant difference between both groups in the success rates at the end of 18 months (P = 0.726).
TABLE 1.
Demographic and Baseline Clinical Characteristics of the Study Patients
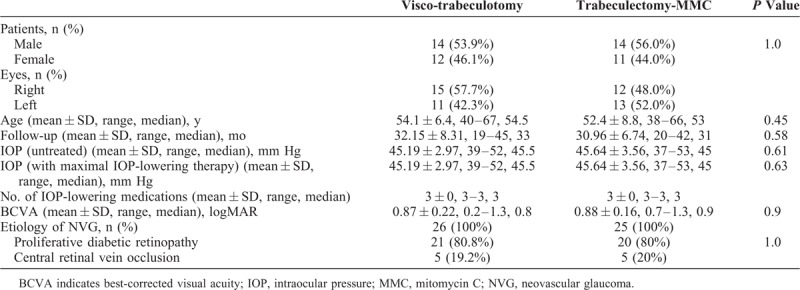
TABLE 2.
IOP of the Study Eyes at Different Follow-Up Time Points
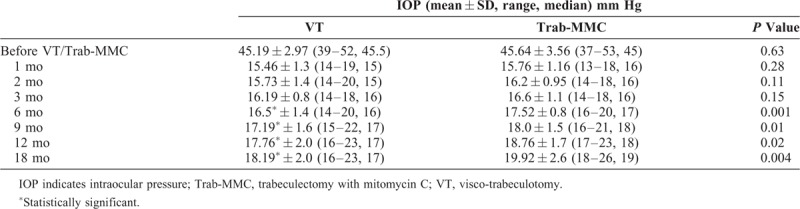
FIGURE 1.
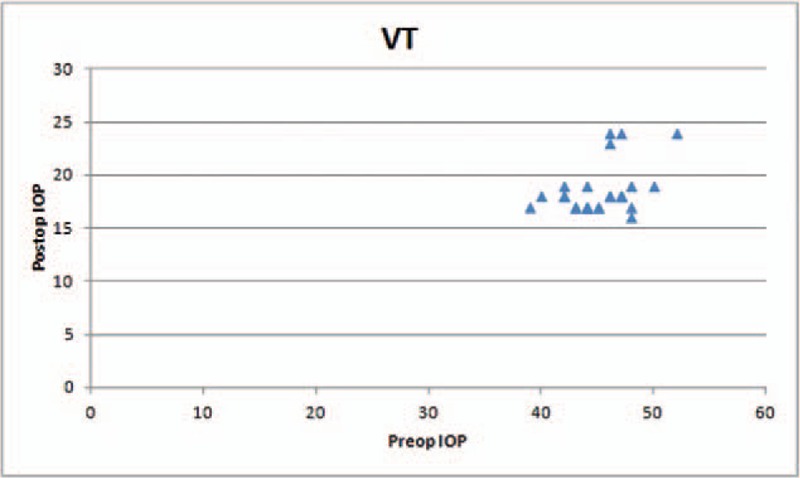
The preoperative and postoperative intraocular pressures for the viscotrabeculotomy group.
FIGURE 3.
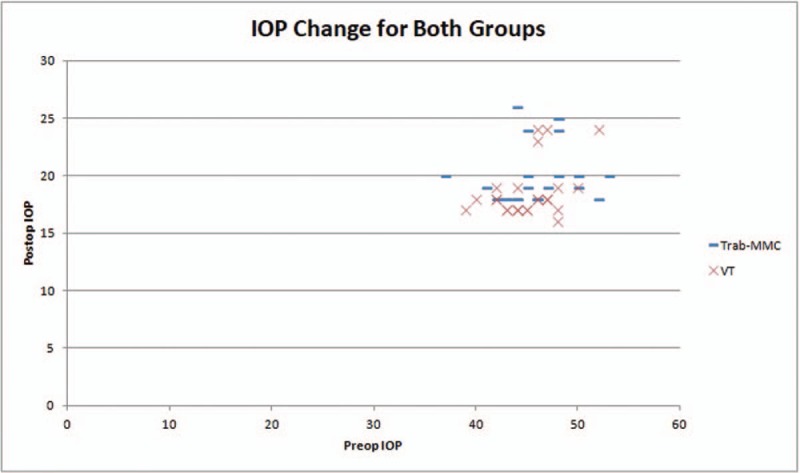
The preoperative and postoperative intraocular pressures for both groups.
TABLE 3.
Clinical Characteristics and Success Rates of the Study Eyes at 18 Months’ Follow-Up

FIGURE 4.
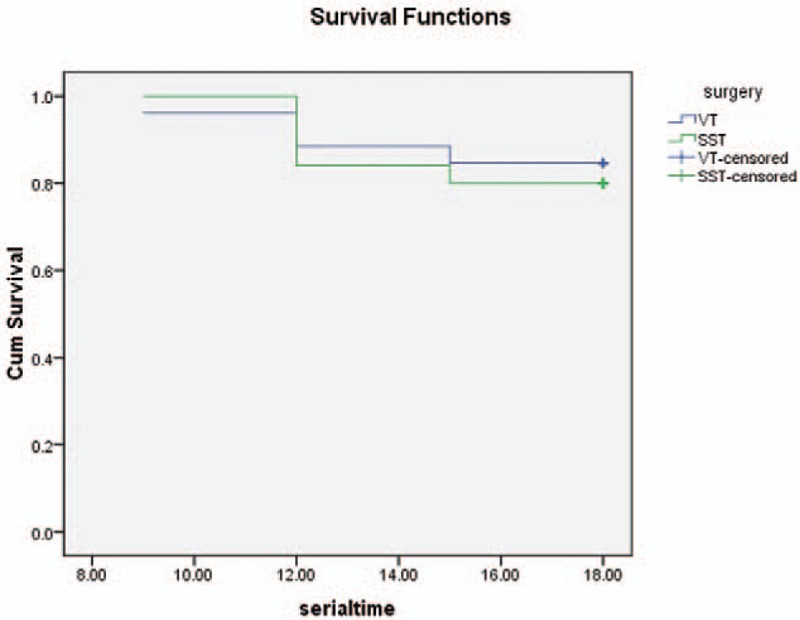
The Kaplan-Meier survival curves for both procedures.
FIGURE 2.
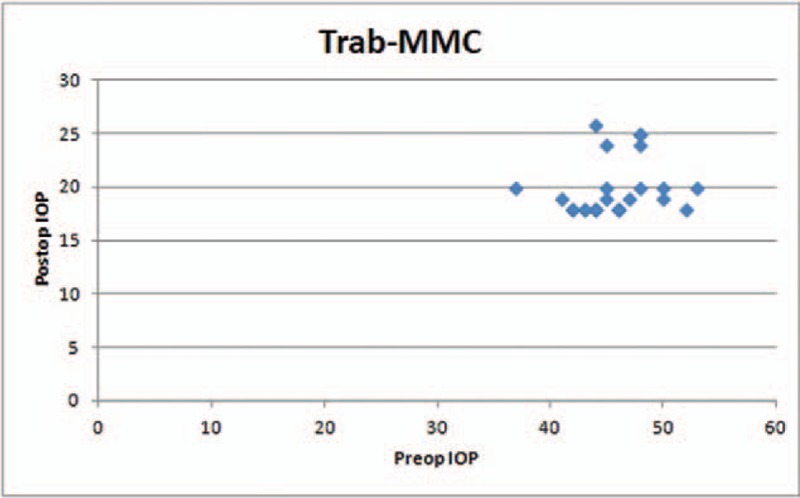
The preoperative and postoperative intraocular pressures for the trabeculectomy with mitomycin C group.
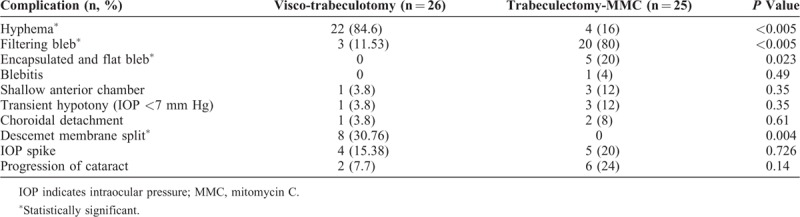
Table 4 demonstrates the complication rates. The most common complication encountered in both groups was a mild self-limited hyphema occurring in 85% of VT eyes and 16% of Trab-MMC eyes (P < 0.005). A partial Descemet membrane split occurred in 31% of the eyes in VT (P = 0.004). Four-fifths of the eyes in Trab-MMC group enjoyed functioning healthy filtering blebs, whereas blebs were encapsulated in the remaining one-fifth. Accidental blebs formed in 12% of eyes in VT (unintended blebs, where the angle surgery does not normally result in creation of a filter). Transient hypotony was more common in Trab-MMC eyes, whereas an IOP spike was almost equally distributed between the 2 study groups.
TABLE 4.
Complications and Repeat Interventions
DISCUSSION
The current study compared the efficacy of VT with Trab-MMC in lowering the IOP in eyes with NVG after the administration of antiVEGF and retina laser ablative therapy (PRP). The study results demonstrate that both procedures are almost equally effective in significantly reducing the IOP in NVG eyes after appropriate therapy for the neovascularization, with slight advantage for VT over Trab-MMC that extends well over 18 months.
Studying the demographic characteristics of the study patients demonstrates almost equal sex distribution with slight male preponderance. This finding is in accordance with other studies,5,13 which demonstrate almost equal occurrence of NVG in both sexes. This may be an inherent property of NVG that does not demonstrate sex predilection, or simply a property of the most common predisposing disease, namely diabetes mellitus, which similarly does not demonstrate sex predilection. The disease also occurs equally in right and left eyes, another characteristic of NVG which demonstrates no laterality predilection as well. The mean follow-up period extended well beyond 2 years, which parallels the mean follow-up in some published reports11,14 and is significantly longer than other reports.5,15 There were no statistically significant differences between the 2 study groups indicating homogeneity of the sampling process. As expected, the most common etiology of NVG in this study was proliferative diabetic retinopathy, already reported by most studies to be the prime player in cases of NVG, with vascular occlusion occupying the second place.13,15
Scrutiny of the clinical characteristics of the study eyes highlights the typical features of NVG, namely a markedly elevated IOP despite maximal tolerated medical therapy7 coupled with relatively poor BCVA. However, studying on the IOP values along the follow-up period of 18 months shows that both procedures were almost equally effective in reducing IOP significantly from the preoperative values. There is a statistically significant advantage for VT over Trab-MMC from the sixth month onwards.
Although the trend is a gradual rise of IOP over time, the IOP remains relatively well controlled into the study follow-up duration of 18 months. The efficacy of Trab-MMC in NVG is reported,5 and the gradual decline of IOP-lowering effect over time.13,15 The efficacy of VT has been reported in other types of glaucoma, namely childhood glaucoma12 and trabeculotomy ab externo in primary open angle and uveitic glaucoma.16 To the best of the authors’ knowledge, this is the first report of VT in NVG. The apparent success of VT in lowering the IOP may be attributed to the fact that the procedure addresses the exact site of the pathology, the angle of the AC. Although Trab-MMC addresses part of the angle, VT definitely opens a larger circumference of the angle of the AC and this may be responsible for the advantage of VT over Trab-MMC. The fact that VT does not normally result into a fistula for aqueous humour—which in case of NVG may be loaded with inflammatory mediators and profibrotic substances—may account for the higher success rate than procedures which normally vent aqueous humour into the subconjunctival space, namely Trab-MMC with all the probabilities of subconjunctival fibrosis. Despite the rise of IOP over time with both procedures, the significant reduction in IOP-lowering medications is an obvious advantage. Success rates in the current study parallel those reported for NVG.11,17 Noteworthy is the fact that qualified success represented a little over 50% with either procedure reflecting the already reported17 need for IOP-lowering medications, albeit reduced in number.
The complications encountered in the current study are similar to those reported in other studies.5,15 The obviously high rate of hyphema with VT reflects the inherent anatomy of the Schlemm canal collector channel system in which there are no valves allowing regurgitation of blood into the Schlemm canal with trabeculotomy. The presence of iris neovascularization may contribute to an increased incidence of hyphema in the current study, even if rubeosis was brought under control before the glaucoma surgical procedure.
The current study had several limitations. The variable glaucoma diagnosis of proliferative diabetic retinopathy and vascular occlusion may pose different therapeutic and prognostic implications. The relatively small number of patients may not allow robust generalization of the study findings. The lack of data on postoperative gonioscopy precludes reporting on the short- and long-term fate of the angle in either procedures, and whether the fistula remains patent or not in cases of Trab-MMC and whether the circumference of the angle opened by VT remains open or was subject—even partly—to reformation of peripheral anterior synechia.
In conclusion, both VT and Trab-MMC are effective in reducing the IOP in cases of NVG after control of neovascularization with anti-VEGF and PRP. VT brings about a greater reduction in IOP than Trab-MMC that is more sustained over time. Complications of both procedures are relatively simple and self-limited, with no vision-threatening events.
Footnotes
The study was conducted in Mansoura Ophthalmic Center, Mansoura Faculty of Medicine, Mansoura University, Egypt.
This study is an original study conducted by the authors. There is no prior publication by any other journal.
The corresponding author had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis and the decision to submit for publication. The study was not funded by any institution or body.
The authors have no funding or conflicts of interest to declare.
REFERENCES
- 1.Weiss DI, Shaffer RN, Nehrenberg TR. Neovascular glaucoma complicating carotid-cavernous fistula. Arch Ophthalmol 1963; 69:304–307. [DOI] [PubMed] [Google Scholar]
- 2.Villacampa P, Menger KE, Abelleira L, et al. Accelerated oxygen-induced retinopathy is a reliable model of ischemia-induced retinal neovascularization. PLoS One 2017; 12:e0179759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tailor R, Kinsella MT, Clarke JC. Bevacizumab followed by ahmed valve implantation inthe management of neovascular glauoma. Semin Ophthalmol 2017; 1–7. [DOI] [PubMed] [Google Scholar]
- 4.Kim KL, Suh W. Apatinib, an inhibitor of vascular endothelial growth factor receptor 2, suppresses pathologic ocular neovascularization in mice. Invest Ophthalmol Vis Sci 2017; 58:3592–3599. [DOI] [PubMed] [Google Scholar]
- 5.Sun JT, Liang HJ, An M, et al. Efficacy and safety of intravitreal ranibizumab with panretinal photocoagulation followed by trabeculectomy compared with Ahmed glaucoma valve implantation in neovascular glaucoma. Int J Ophthalmol 2017; 10:400–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Alkawas AA, Shahien EA, Hussein AM. Management of neovascular glaucoma with panretinal photocoagulation, intravitreal bevacizumab, and subsequent trabeculectomy with mitomycin C. J Glaucoma 2010; 19:622–626. [DOI] [PubMed] [Google Scholar]
- 7.Noor NA, Mustafa S, Artini W. Glaucoma drainage device implantation with adjunctive intravitreal bevacizumab in neovascular glaucoma: 3-year experience. Clin Ophthalmol 2017; 11:1417–1422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fong AW, Lee GA, O’Rourke P, et al. Management of neovascular glaucoma with transscleral cyclophotocoagulation with diode laser alone versus combination transscleral cyclophotocoagulation with diode laser and intravitreal bevacizumab. Clin Exp Ophthalmol 2011; 39:318–323. [DOI] [PubMed] [Google Scholar]
- 9.Kokubun T, Tsuda S, Kunikata H, et al. Prediction of surgical outcome after trabeculectomy for neovascular glaucoma with anterior-segment optical coherence tomography. J Glaucoma 2018; 27:1157–1164. [DOI] [PubMed] [Google Scholar]
- 10.Zhao X, Wang Z, Yang X. Management of neovascular glaucoma with intravitreal ranibizumab, panretinal photocoagulation, and subsequent 5-fluorouracil augmented trabeculectomy: a case report. Medicine 2017; 96:e7221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hong Y, Hu Y, Dou H, et al. Comparison of the safety and efficacy of triple sequential therapy and transscleral cyclophotocoagulation for neovascular glaucoma in the angle-closure stage. Sci Rep 2018; 8:7074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.ElSheikha OZ, Abdelhakim MA, Elhilali HM, et al. Is viscotrabeculotomy superior to conventional trabeculotomy in the management of Egyptian infants with congenital glaucoma? Acta Ophthalmol 2015; 93:e366–e371. [DOI] [PubMed] [Google Scholar]
- 13.Shinohara Y, Akiyama H, Magori M, et al. Short-term outcomes after EX-PRESS implantation versus trabeculectomy alone in patients with neovascular glaucoma. Clin Ophthalmol (Auckland, NZ) 2017; 11:2207–2213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yildirim N, Yalvac IS, Sahin A, et al. A comparative study between diode laser cyclophotocoagulation and the Ahmed glaucoma valve implant in neovascular glaucoma: a long-term follow-up. J Glaucoma 2009; 18:192–196. [DOI] [PubMed] [Google Scholar]
- 15.Wang MH, Li QM, Dong HT, et al. Ahmed valves vs trabeculectomy combined with pars plana vitrectomy for neovascular glaucoma with vitreous hemorrhage. Eur J Ophthalmol 2017; 27:774–780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.William A, Spitzer MS, Doycheva D. Comparison of ab externo trabeculotomy in primary open angle glaucoma and uveitic glaucoma: long-term outcomes. Clin Ophthalmol 2016; 10:929–934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dong Z, Gong J, Liao R, et al. Effectiveness of multiple therapeutic strategies in neovascular glaucoma patients: a PRISMA-compliant network meta-analysis. Medicine 2018; 97:e9897. [DOI] [PMC free article] [PubMed] [Google Scholar]


