Abstract
Background:
A near vision game has been developed for the autostereoscopic screen of the Nintendo 3DS console. Ease of use and time for testing by non–English-speaking patients was not known.
Methods:
Adult and pediatric patients in a remote Burma clinic were compared with US military staff with each performing conventional near acuity, Stereo Fly, and Ishihara color in addition to PDI Check game, so results could be correlated and timed.
Results:
Seventeen Burma adults (aged 19–58), 20 Burma children (aged 7–15), and 14 US military staff (aged 21–36) completed the testing. Conventional testing correlated with PDI Check for stereo (P < 0.001), acuity oculo dexter (P < 0.01), acuity oculo sinister (P < 0.01). For visual acuity and stereopsis, the intraclass coefficient was 0.55 [95% confidence interval (CI) 0.28–0.72] and 0.62 (95% CI 0.41–0.77) respectively, but with few color deficient cases color was 0.30 (95% CI –0.05 to 0.60). The time in seconds to complete near vision testing with PDI Check (172 ± 27, overall; 198 ± 34, Burma; 99 ± 20, military) was significantly (25% ± 18%) briefer than conventional testing (226 ± 31, overall; 270 ± 34, Burma; 126 ± 20, military). The Burma patients took significantly longer than the military staff (234 ± 25 vs 112 ± 14, P < 0.01). Time for Burma children did not differ from Burma adults for PDI (109 ± 47 vs 217 ± 54, P = 0.42) and for conventional testing (266 ± 51 vs 275 ± 52, P = 0.80).
Conclusions:
Non–English-speaking Burma children and adults were able to reliably perform 3 types of near vision testing with a Nintendo 3DS game 25% quicker than the 2 to 3 minutes for conventional methods. They were slower than experienced US military staff adults.
Keywords: amblyopia, deuteranopia, presbyopia, stereopsis, vision screening
The 3 primary near vision modalities screened during a comprehensive eye examination are monocular visual acuity, stereopsis, and color. Quality sensory screening usually requires an experienced technician and substantial time compared with objective photoscreening.1,2
Portable electronic devices can aid in sensory vision testing. The PEEK Tumbling “E” smart-phone distance visual acuity application has been validated in adults3 and children.4 Monocular near acuity has been screened with a smart phone and an occluder.5 Patients may prefer smartphone near color vision testing compared with Ishihara color plates.6 Depth perception in young children has recently been investigated with large specialized computer screens7; however, practical portable electonic screening of stereopsis had not yet been available.
A near vision screening game called “PDI Check” has recently been developed for the color autostereoscopic barrier screen of the Nintendo 3DS (Kyoto, Japan) hand-held, sturdy clam-shell console. PDI Check is a valid, dynamic, forced choice game. Conventional clinical tests have served as calibration of PDI Check: Rosenbaum Pocket chart for monocular visual acuity, Titmus Stereo Fly test for stereopsis, and Ishihara concise test for deuteranomaly color screening.8 Due to the unique nature of the Nintendo 3DS screen, patching is not required for monocular and suppression testing and goggles are not required to convey the impression of depth.9
The purpose of this study was to determine whether the PDI Check game could reliably be used by a group of non–English-speaking patients who are otherwise unfamiliar with near vision testing. The PDI Check game was compared with conventional testing in a group of pediatric and adult patients attending an eye clinic in the Karen State of Burma (Myanmar). The Karen have suffered over 6 decades of civil war leaving their healthcare delivery wanting.10 Medics from the relief organization Free Burma Rangers offered a free vision clinic dispensing custom spherocylinder spectacles and providing cataract surgery. The older Karen patients often have against-the-rule hyperopic astigmatism.11
The control group for the Burma adults and children was a group of US military staff simultaneously screened with the identical version of PDI Check game.
METHODS
This HIPAA-compliant, prospective study has IRB approval from Pacific University. Patients gave written consent or assent as needed; parents provided written consent. Translators were used for non–English-speaking families.
Patient Selection
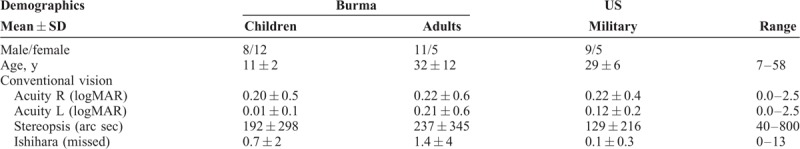
Adults and children attending a vision/hearing clinic in the Karen State, Burma (Myanmar), were informed of the study in their preferred language (Karen or Burmese) and invited to participate after written consent/assent. A comparison group of adult US Military reserve staff served as controls. Demographic and conventional vision characteristics of each group are presented in Table 1.
TABLE 1.
Demographics of Burma and US Military Subjects Including Mean and Standard Deviation Values for Conventional Near Vision Abilities
Procedures
Conventional Testing
Near visual acuity was tested with a standardized Rosenbaum Pocket card with termination criteria the smallest line read (assisted by translators) and the nontested eye patched or covered with an occluder.
Stereopsis was tested with the Titmus Stereo Fly test determining how many of the 9 circles the patient could detect while wearing polarized spectacles.
Color was tested with Ishihara Concise booklet. Burmese patients traced the camouflaged numbers and lines with a finger; US military adults verbally answered. The number of completely or partially missed plates was recorded.
PDI Check version 0.1.7 is a forced multiple choice test with dynamic, linear presentation. Two Nintendo 3DS XL development kits were used. An orientation phase determines lag-time by utilizing 3 matching screen images of objects and 1 grossly different object displayed on the upper autostereoscopic barrier screen of the 3DS. One object is displayed per quadrant of the upper screen. The subject selects the quadrant with the unique object by selecting the corresponding quadrant on the lower touch screen. For acuity 3 Landholt “C”s are compared to 1 Landholt “C” rotated to the “U” orientation. For stereopsis, the unique quadrant has 2 overlapping rings with the right-eye and left-eye viewed discs separated to make it appear as if a single ring is levitating when viewed binocularly (Fig. 1). For color, 3 matching discs with hue corresponding to the deuteranopia confusion axis of the Farnsworth-Munsell D-100 test are compared with a unique, random quadrant with the disc hue varied 10 FM D-100 units. The PDI check test and the conventional tests were done from a uniform distance of 35 cm.
FIGURE 1.

PDI Check near vision game on the Nintendo 3DS employed by Jungle School of Medicine Kawthoolei medics at the Cross Border Clinic near the Thai-Burma border.
For the testing phase, each randomly selected quadrant object gradually undergoes a dynamic linear change: acuity optotype with only one eye “C” rotated to “U” orientation and all 4 increased in size from logMAR 0.0 to 1.6, for stereo the horizontal disparity of the rings gradually increasing from about 10-second arc to 800-second arc, and for color, the random target disc color-shifted linearly away from the deuteranopia confusion axis. The subject's time to select the lower touch screen is recorded. The score is obtained by subtracting the shortest orientation phase lag-time from each vision modality select-time to obtain the visual perception time. Each subject was tested once to determine threshold for visual acuity of each eye, stereopsis, and percent green cone color; no test re-test evaluation was made.
The time to complete color, stereo, and monocular visual acuity was carefully recorded for PDI Check as well as the combination of conventional tests.
An example of the PDI Check game on the Nintendo 3DS XL can be viewed at: https://vimeo.com/robertarnold/pdicheck0-1-7.
Statistical Analyses
The primary outcome was the time to complete the conventional and PDI Check tests. Secondary outcome was a comparison of the 2 testing methods for each visual modality using Bland-Altman plot (Figs. 2 and 3), intraclass correlation (ICC) and Spearman correlation.
FIGURE 2.
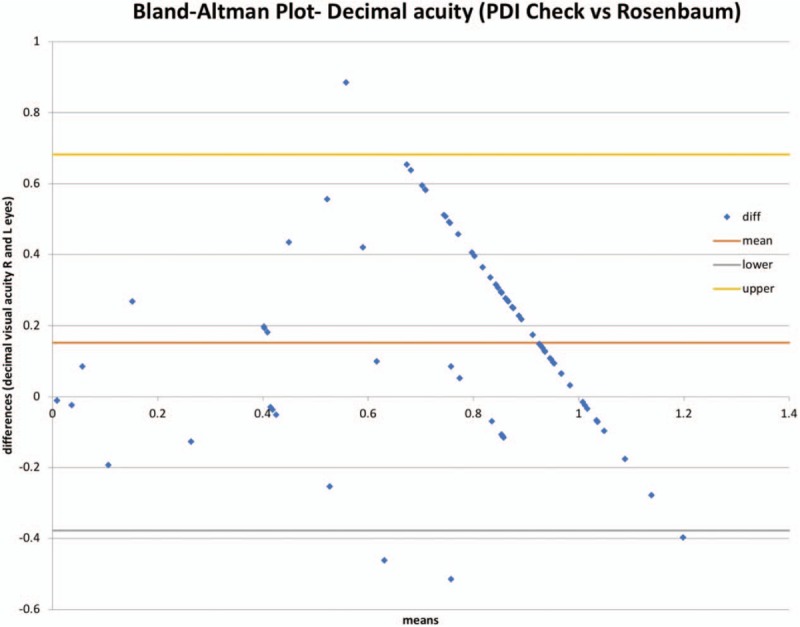
Bland-Altman Plot for Visual acuity comparing Nintendo 3DS PDI Check game with conventional testing with Rosenbaum near card at 35 cm. The PDI Check version 0.1.7 underestimates decimal acuity by 0.15.
FIGURE 3.
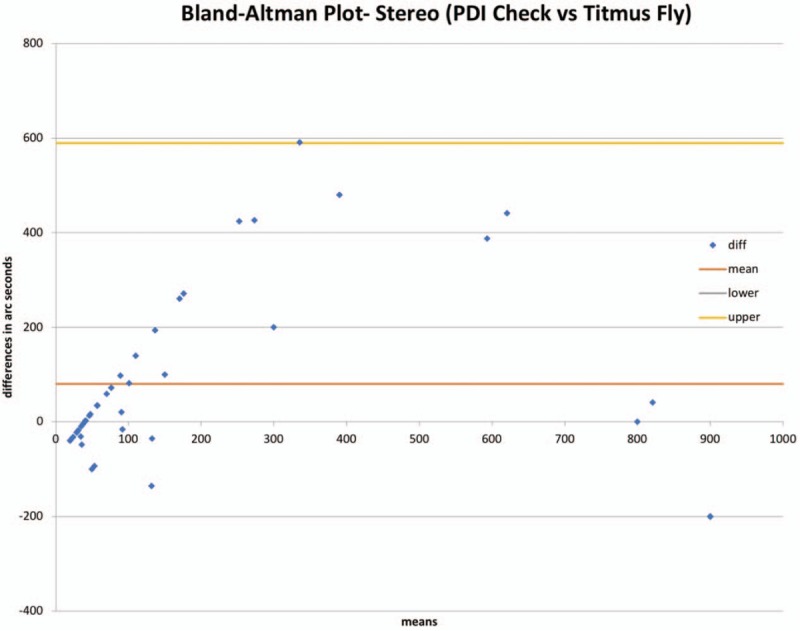
Bland-Altman Plot for stereopsis comparing PDI Check game with Titmus Fly stereo. The PDI Check formula in version 0.1.7 overestimates stereo by about 80 arc seconds.
Sample Size Calculation for Primary Outcome
To detect a 20% difference from a predicted testing time of about 100 seconds, and a standard deviation of 30 seconds, with power 0.8 and alpha 5%, a sample size of 36 is needed. Given other studies,8,9 we did not enhance the prescreening probability in our subjects particularly for color deficiency.
RESULTS
Thirty-seven Karen Burma ethnic patients and 14 US Military staff completed the timed Conventional near vision tests (Table 1) and also the PDI Check game. The US military were new to this version of the game but familiar with occupational and health vision screening. The Burma patients were inexperienced with any forms of vision testing but had medics as translators.
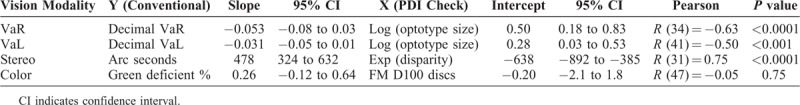
The sensory results from conventional testing are compared to PDI check for near acuity, stereopsis and color in Table 2. The highest grade of conventional acuity and stereopsis was often attained by subjects with PDI Check scores in intermediate ranges, whereas other PDI Check subjects had even better scores. As a result, an exponential function best described the stereopsis and a logarithm best described decimal visual acuity relationships. Bland-Altman Plots are given for visual acuity (Fig. 2) and stereopsis (Fig. 3). With our current formulae, PDI Check underestimates decimal visual acuity (Rosenbaum) by 0.15 and overestimates stereopsis (Titmus) by 87 arc seconds. Spearman rank coefficient showed highly significant correlations for right eye acuity, left eye acuity, and stereopsis. ICC for visual acuity was 0.55 (95% CI 0.27–0.72) and for stereopsis 0.62 (95% CI 0.41–0.77), which are regarded as good. The ICC for color was just 0.30 (95% CI −0.05 to 0.60) which is regarded as low. Due to a low number of color-deficient individuals (males), color was not significantly correlated.
TABLE 2.
Correlations Between Conventional Near Vision tests and PDI Check
The mean and standard deviation times to perform the combined 3 near vision tasks (primary outcome) comparing PDI Check with conventional tests in Burma adults, children, and US military adults is shown in Table 3. The median times with Mann-Whitney comparison scores are shown in Table 4. Compared with conventional testing, PDI Check was about 27% ± 12% faster for Burma patients and about 21% ± 16% faster for US military. The experienced US military were about 52% ± 12% faster than the Burma patients overall. Combining Burma and US military subjects, the time to test near vision with PDI Check (172 ± 27 seconds) was 24% shorter than that for conventional near testing [226 ± 31 seconds, t (92) = 2.6, P = 0.01].
TABLE 3.
Times (in years) to Perform Monocular Near Visual Acuity, Stereopsis, and Deuteranopia Color Screening
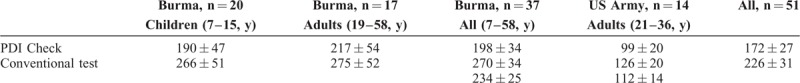
TABLE 4.
Comparison of Times to Perform Near Vision Testing

DISCUSSION
It takes an experienced US military adult 2 to 3 minutes to complete conventional testing of monocular visual acuity, stereopsis, and color. The PDI Check game version 0.1.7 was 21% faster. Children and adults attending a remote Burma clinic, non–English-speaking and unfamiliar with these procedures, took about twice as long, but were able to complete the PDI Check game 27% faster than they completed stereo, color tests, and English-language conventional acuity. We had sufficient cases to demonstrate good correlation of PDI Check with conventional tests for monocular visual acuity and stereopsis. We can further refine our formulae that relate raw time scores to clinical values due to a mild bias to overestimate stereo and underestimate decimal acuity.
The advantages of PDI Check over conventional testing include aspects of convenience, patient engagement, price, and speed. The sturdy clamshell case transported and functioned well in the high heat and humidity of Burma. The luminous color screen was easily viewed in day or night testing. There were no software crashes. Adult and pediatric patients smiled when their correct choice was “rewarded” by the game's “success” musical game animation. Disadvantages of PDI Check included the need to recharge the Nintendo 3DS at least once every 2 clinic days, and the need to orient novice subjects to the lower touch screen interaction despite upper 3D screen viewing. In Burma children, an audience of other patients would crowd around watching an individual perform the game, and some needed to be encouraged not to assist in suggesting answers right or wrong. The Nintendo 3DS screen with eye-tracking is primarily designed to be viewed only by the subject, but the adjacent audience would strain to gain a view presenting a modicum of distraction for the patient being tested. The conventional tests worked similarly in US military and Burma; however, the patients tended to trace Ishihara figures with their finger, and the “No Peeking” eye patches did not stick as well for patients sweating in 35°C heat. Adjacent Burma audience were generally less engaged and less distracting with conventional testing than with the PDI Check game.
Strengths of this study include a uniform ethnic study group and a simultaneous western control group with sufficient sample size for testing duration. Matching Nintendo devices were used as initial near-vision tests for all Burma adults and children as well as the control group of US military personnel. The testing environments matched community health clinic screening. Weaknesses of this study include a lack of sufficient pathology (color and stereo deficient individuals) for appropriate validation and a lack of test re-test evaluation.
Near vision impairment is common in many areas of the world.12 The compassionate and efficient delivery of healthcare in developed countries includes the screening and examination of non–English-speaking families and refugees who are not familiar with testing methods. The development of tools that are easily adopted by people from different cultures has practical benefit. It is estimated that an ophthalmic technician evaluating 25 Burma refugee patients per day would be expected to save approximately 30 minutes per day switching from conventional near-vision testing to the version 0.1.7 PDI Check game on Nintendo 3DS for adults and children.
Footnotes
IRB: Pacific University: PDI Check 8-2017, IRB 109-17, INSTITUTIONAL REVIEW BOARD, FWA: 00007392 | IRB: 0004173.
Financial Disclosure: R.W.A. coordinates the Alaska Blind Child Discovery that has received discounted vision screening technology from several vendors. K.A.S. and R.W.A. are on the board of PDI Check, LLC (Anchorage, AK) which markets the PDI Check game on the Nintendo marketplace.
The US Military is not a part of development and that inclusion in the study does not suggest any affiliation of the US government with PDI Check or any other items included in the study.
The other authors have no funding or conflicts of interest to declare.
REFERENCES
- 1.Moganeswari D, Thomas J, Srinivasan K, Jacob GP. Test re-test reliability and validity of different visual acuity and stereoacuity charts used in preschool children. J Clin Diagn Res 2015; 9: NC01-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Leman RE, Clausen MM, Bates J, et al. A comparison of patched HOTV visual acuity and photoscreening. J Sch Nurs 2006; 22:237–243. [DOI] [PubMed] [Google Scholar]
- 3.Bastawrous A, Rono HK, Livingstone IA, et al. Development and validation of a smartphone-based visual acuity test (peek acuity) for clinical practice and community-based fieldwork. JAMA Ophthalmol 2015; 133:930–937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rono HK, Bastawrous A, Macleod D, et al. Smartphone-based screening for visual impairment in Kenyan school children: a cluster randomised controlled trial. Lancet Glob Health 2018; 6:e924–e932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tofigh S, Shortridge E, Elkeeb A, et al. Effectiveness of a smartphone application for testing near visual acuity. Eye (Lond) 2015; 29:1464–1468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ozgur OK, Emborgo TS, Vieyra MB, et al. Validity and acceptance of color vision testing on smartphones. J Neuroophthalmol 2018; 38:13–16. [DOI] [PubMed] [Google Scholar]
- 7.Braun S, Kavsek M. Infants perceive two-dimensional shape from horizontal disparity. Infant Behav Dev 2018; 52:140–145. [DOI] [PubMed] [Google Scholar]
- 8.Arnold RW, Damarjian AG, Molina A, et al. Calibrated measurement of acuity, color and stereopsis on a Nintendo 3DS game console. Clin Optometry 2019; 11:47–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Smith KA, Arnold AW, Sprano JH, et al. Performance of a quick screening version of Nintendo 3DS “PDI Check” game on patients with ocular suppression. JPOS 2019; 56: In Press. [DOI] [PubMed] [Google Scholar]
- 10.Davis WW, Mullany LC, Shwe Oo EK, et al. Health and human rights in Karen State, Eastern Myanmar. PLoS One 2015; 10:e0133822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Arnold RW, Arnold AW. Refractive error in Myanmar. Ophthalmology 2008; 115:1642–1643. [DOI] [PubMed] [Google Scholar]
- 12.He M, Abdou A, Naidoo KS, et al. Prevalence and correction of near vision impairment at seven sites in china, India, Nepal, niger, South Africa, and the United States. Am J Ophthalmol 2012; 154:107–116. e101. [DOI] [PubMed] [Google Scholar]


