Objective
The aim of this study was to compare quick Sepsis-related Organ Failure Assessment (qSOFA) and Systemic Inflammatory Response Syndrome (SIRS) scores for predicting mortality.
Patients and methods
A single-center, retrospective study of adult patients with suspected infection was conducted. Area under the curve (AUC) and multivariate analyses were used to explore associations between the qSOFA and SIRS scores and mortality.
Results
Of the 69 115 patients enrolled, 1798 died within 72 h and 5640 within 28 days. The qSOFA scores were better than SIRS scores at predicting 72-h mortality (AUC: 0.77 vs. 0.64). However, the discriminatory power of both scores was low in terms of 28-day mortality (AUC: 0.69 vs. 0.60). Patients with qSOFA score of at least 2 had a higher hazard ratio for 72-h mortality than for 28-day mortality (2.64 vs. 1.91).
Conclusion
The qSOFA scores are more accurate than SIRS scores for predicting 72-h mortality and are better at predicting 72-h mortality than 28-day mortality.
Keywords: infection, mortality, Quick Sepsis-related Organ Failure Assessment, sepsis
Introduction
In the emergency department (ED), sepsis is a time-dependent disease. Within 72 h, a significant proportion of patients with milder severity progress to severe sepsis or death [1]. The most common preventable medical error leading to unexpected death within 72 h is inappropriate treatment for sepsis [2]. Early recognition of patients at risk of early mortality is important, as such patients may benefit from aggressive and prompt therapeutic intervention. According to a recent meta-analysis of heterogeneous populations of patients with sepsis [3], early and quantitative resuscitation strategies confer a survival benefit.
The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3) [4] recommends a new scoring system, the quick Sepsis-related Organ Failure Assessment (qSOFA), for screening patients with suspected sepsis. In the original study [5], qSOFA scores were better than SOFA scores at predicting mortality. Moreover, it is simple, comprising only three clinical components (hypotension, tachypnea, and altered consciousness).
Several studies [6–9] showed that qSOFA scores were better than systemic Inflammatory Response Syndrome (SIRS) scores for predicting mortality; qSOFA scores have better areas under the receiver operating characteristic curve (AUCs) for mortality than SIRS scores. In contrast, other studies [10,11] have demonstrated that qSOFA scores are no better than SIRS scores and have lower sensitivity. We hypothesized that the ability of qSOFA scores to predict in-hospital mortality may be affected by a time factor (i.e. it more effectively detects early mortality within 72 h of ED presentation). This study aimed to compare qSOFA and SIRS scores for predicting early and late mortality in ED patients with suspected infection.
Patients and methods
Design and setting
We conducted a single-center, retrospective, observational cohort study at Kaohsiung Chang Gung Memorial Hospital, a 2300-bed medical center providing primary and tertiary level care in southern Taiwan. It receives more than 100 000 ED visits per year. The hospital’s Institutional Review Committee on Human Research (103-0053B) approved the study with a waiver of informed consent.
Patients
Patients presenting with suspected infection between January 2007 and December 2013 were included if older than 18 years of age and if blood samples were collected for culture and antibiotics were initiated within 24 h of ED triage.
Measurements
Demographic data, vital signs, and laboratory results were extracted from the electronic medical record. Information on underlying disease(s) and site of infection was obtained by identifying International Statistical Classification of Diseases and Related Health Problems (9th revision) codes [12].
To calculate qSOFA scores, one point was awarded for each of the following: systolic blood pressure of 100 mmHg or less, respiratory rate of at least 22 breaths/min, and Glasgow Coma Scale score of up to 13, giving a score of 0–3 [5]. To calculate SIRS scores, one point was awarded for each of the following: body temperature of more than 38 or less than 36°C, heart rate of more than 90 beats/min, respiratory rate of more than 20 breaths/min, and abnormal white blood cell count [ > 12 000 or < 4000/µl or > 10.0% immature forms (bands)], giving a score of 0–4 [13]. For both scores, the initial values (vital signs at triage and first blood test results) were used. However, patients without vital signs at the time of triage were not excluded. Medical records were reviewed to add the first value (all within 1 h of triage).
Definitions
The diagnosis of suspected infection by the treating emergency physicians was based on obvious sources of infection (including laboratory and image data) or potential infection (e.g. fever and inflammatory reaction). According to the clinical protocol of our hospital, most patients with suspected infection or sepsis received intravenous antibiotics, and blood cultures were taken. Patients were defined as having suspected infection if blood cultures were sent before intravenous antibiotics were administered, within 24 h of ED triage. Septic shock was defined as the persistence of sepsis-induced hypotension requiring vasoactive drug administration despite adequate fluid resuscitation [14,15]. The primary and secondary outcomes were 72-h and 28-day mortality, respectively. The primary objective was to compare qSOFA and SIRS scores for predicting 72-h mortality. The secondary objective was to compare qSOFA scores for predicting 72-h and 28-day mortality.
Statistical analyses
Statistical analyses were performed using Statistical Package for the Social Sciences for Windows (software, version 20.0; IBM Corp., Armonk, New York, USA) and MedCalc 2015 statistical software (version 15.8). Continuous variables (mean ± SD) were analyzed using Student’s t-tests. Categorical variables [n (%)] were compared using the χ2-test or Fisher’s exact test, as appropriate. Sensitivity, specificity, and AUCs were calculated for qSOFA and SIRS scores of at least 2 to compare their ability to predict mortality. AUCs for both scores were compared using the DeLong test. Multivariate analysis was performed to determine hazard ratios (HRs), adjusted for age, sex, septic shock, and comorbidities. A P value less than 0.05 was considered statistically significant.
Results
During the study period, 77 942 patients with suspected infection were identified. After exclusions [ < 18 years of age (n = 8827)], 69 115 patients were enrolled: 1798 (2.6%) died within 72 h and 5640 (8.2%) died within 28 days (Fig. 1).
Fig. 1.
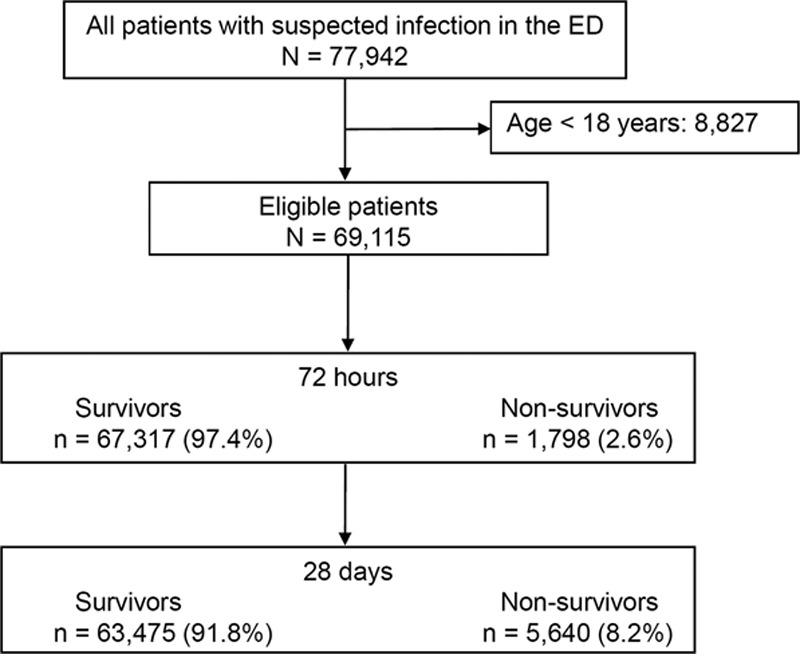
Study flow chart. ED, emergency department.
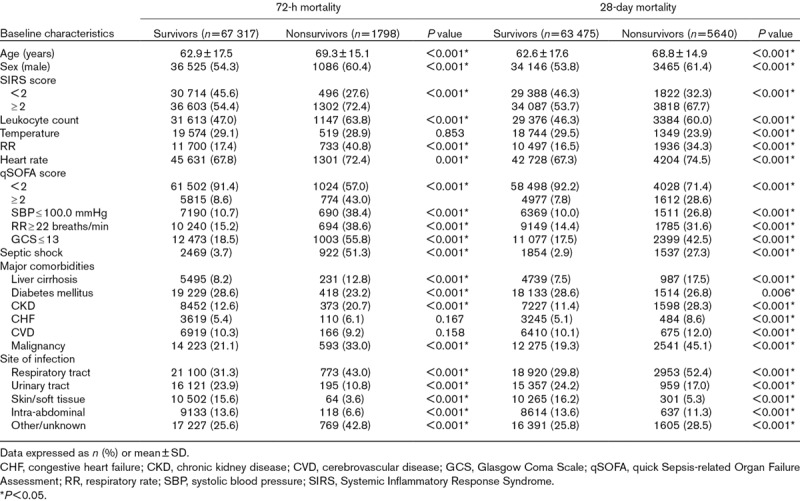
Several differences were noted between survivors and nonsurvivors (Table 1). Nonsurvivors were older and included a greater proportion of men with qSOFA and SIRS scores of at least 2 and septic shock. Liver cirrhosis, chronic kidney disease, and malignancies were the predominant comorbidities among nonsurvivors, whereas diabetes mellitus was more common among survivors. The respiratory tract was the most common site of infection among nonsurvivors.
Table 1.
Baseline characteristics
Among patients with SIRS scores of at least 2, the 72-h mortality rate (3.4%) was approximately one-third that of the 28-day mortality rate (10.1%). Among patients with qSOFA scores of at least 2, the 72-h mortality rate (11.7%) was almost half that of the 28-day mortality rate (24.5%).
The qSOFA score was a better predictor of 72-h mortality than the SIRS score (AUC: 0.77 vs. 0.64). The AUC for both scores reduced for 28-day mortality (0.69 vs. 0.60) (Fig. 2a and b). The sensitivity and specificity of qSOFA scores of at least 2 for predicting 72-h and 28-day mortality were 0.43 and 0.91 and 0.29 and 0.92, respectively. The corresponding values of SIRS scores of at least 2 were 0.72 and 0.45 and 0.67 and 0.46, respectively. The difference in the AUCs for qSOFA and SIRS scores was greater for 72-h mortality than for 28-day mortality (0.13 vs. 0.09).
Fig. 2.
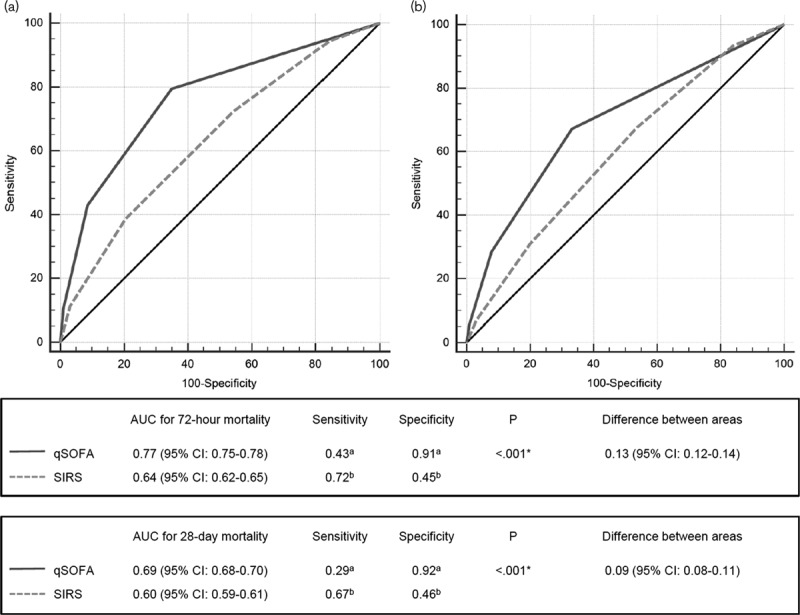
Receiver operating characteristic curves for qSOFA and SIRS scores for predicting (a) 72-h and (b) 28-day mortality. Sensitivity and specificity for aqSOFA and bSIRS scores of at least 2. Asterisks indicate statistical significance. AUC, area under the receiver operating characteristic curve; CI, confidence interval; qSOFA, quick Sepsis-related Organ Failure Assessment; SIRS, Systemic Inflammatory Response Syndrome.
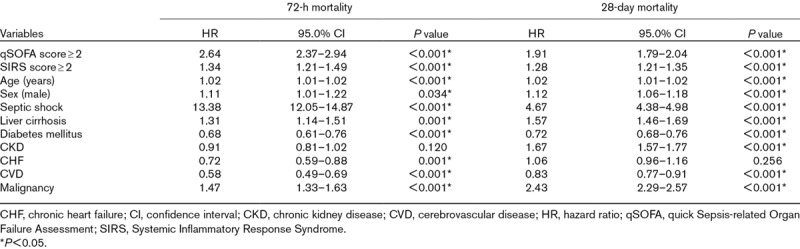
The 72-h and 28-day mortality rates of patients with qSOFA scores of 0, 1, 2, and 3 were 0.8, 3.6, 10.2, and 23.4% and 4.2, 11.9, 22.7, and 37.2%, respectively (both P < 0.001) (Fig. 3). In the multivariate analysis, the HR of a qSOFA score of at least 2 was higher than that of a SIRS score of at least 2 in predicting 72-h mortality (2.64 vs. 1.34). The HRs of both scores reduced for 28-day mortality (1.91 vs. 1.28) (Table 2).
Fig. 3.
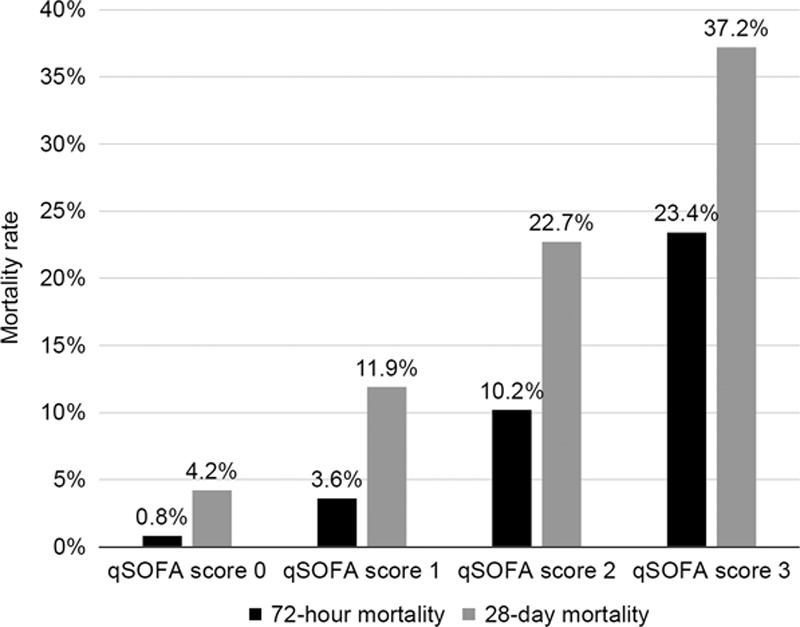
Subgroup analysis of 72-h and 28-day mortality according to qSOFA scores. qSOFA, quick Sepsis-related Organ Failure Assessment.
Table 2.
Multivariate analysis of predictors of 72-h and 28-day mortality
Discussion
The main findings of our study were that qSOFA scores were more accurate than SIRS scores for predicting 72-h mortality and that qSOFA scores were better for predicting 72-h mortality than 28-day mortality.
Several studies [6–9] found that qSOFA scores were better than SIRS scores for predicting mortality. In a large, international, prospective cohort study of 879 patients in the ED (in-hospital mortality rate, 8.0%) [6], the AUC for in-hospital mortality was better for qSOFA scores than for SIRS scores (0.80 vs. 0.65). In a prospective cohort study of 152 critically ill patients with infection (in-hospital mortality rate, 19.0%) [7], the AUC for in-hospital mortality was also better for qSOFA scores than for SIRS scores (0.74 vs. 0.59). Similarly, a retrospective cohort study of 184 875 patients with infection (in-hospital mortality rate, 18.7%) [8] reported AUC values for in-hospital mortality of 0.61 and 0.59 for qSOFA and SIRS scores, respectively. Likewise, in a study of 30 677 patients with suspected infection (in-hospital mortality rate, 5.4%) [9], the AUC for in-hospital mortality was better for qSOFA scores than for SIRS scores (0.69 vs. 0.65).
In contrast, several studies [10,11] have found that qSOFA and SIRS scores have similar discriminatory power and that qSOFA scores are poorly sensitive. A retrospective cohort study of 8871 patients with infection (30-day mortality rate, 3.7%) [10] demonstrated that SIRS and qSOFA scores were similar in predicting organ dysfunction (AUC: 0.72 vs. 0.73). Another retrospective cohort study of 24 164 patients with infection (in-hospital mortality rate, 4.9%) [11] also demonstrated that SIRS and qSOFA scores had similar discriminatory power in terms of in-hospital mortality (AUC: 0.66 vs. 0.64) and that the sensitivity of the qSOFA score was lower than that of the SIRS score (AUC: 0.14 vs. 0.68). Thus, the sensitivity of the qSOFA score is inferior to that of the SIRS score, especially when mortality is low. However, when mortality is higher, the sensitivity and specificity of the qSOFA score increase, making it better able to predict mortality. Mortality differences in the aforementioned studies could be because of differences in defining infection. Studies with low mortality may have included a disproportionate number of mild cases or patients who received aggressive treatment.
In the present study, the sensitivity of the qSOFA score for 72-h mortality was lower than that of the SIRS score. The SIRS score, designed by expert consensus, focuses on identifying general systemic manifestations and stratifying severity [13,15]. It is criticized for being too sensitive and unspecific. As the qSOFA score is less sensitive than the SIRS score, it is not very suitable as a screening tool for infected patients. However, a better AUC and higher specificity mean the qSOFA score is more suitable as a prognostic tool to classify severity.
Although the outcomes of patients with sepsis have improved over the past few decades, in-hospital mortality rates remain high (10.0–30.0%) [16,17]. In our study of infected patients in the ED, the 72-h and 28-day mortality rates were 2.6 and 8.2%, respectively; 31.9% of patients who died within 28 days did so within 72 h. Many critically ill septic patients board in the ED for prolonged periods [18,19]. Illness progression during this period is an important determinant of outcome. Increased length of ED stay can affect the total length of hospital stay and in-hospital mortality [20]. Hence, fast and effective risk stratification and the prediction of 72-h mortality are crucial.
Our study has several limitations. First, as in the original qSOFA study [5], we chose all-cause mortality over sepsis-related mortality and selected patients with suspected infection rather than critically ill patients. Second, given its retrospective design, the study may have been subject to selection bias and documentation and data entry errors. For some patients, vital signs were not evaluated at triage. However, we used the first documented vital sign (within 1 h of triage) instead of excluding these patients to avoid selection bias. Third, we did not control for potential confounders, such as laboratory tests, because these would not have been available to the physician calculating qSOFA scores. Finally, the data and results are limited to a single institution and may not be representative of other settings.
Conclusion
The qSOFA more accurately predicted 72-h mortality than the SIRS. The qSOFA also predicted 72-h mortality more accurately than 28-day mortality. In a busy ED with limited resources, physicians could prioritize treating patients with suspected infection and a qSOFA score of at least 2, thereby making effective use of resources and potentially reducing mortality.
Acknowledgements
The authors thank Editage (http://www.editage.com) for editing and reviewing this manuscript for English language.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Glickman SW, Cairns CB, Otero RM, Woods CW, Tsalik EL, Langley RJ, et al. Disease progression in hemodynamically stable patients presenting to the emergency department with sepsis. Acad Emerg Med. 2010; 17:383–390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Goulet H, Guerand V, Bloom B, Martel P, Aegerter P, Casalino E, et al. Unexpected death within 72 h of emergency department visit: were those deaths preventable? Crit Care. 2015; 19:154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jones AE, Brown MD, Trzeciak S, Shapiro NI, Garrett JS, Heffner AC, et al. The effect of a quantitative resuscitation strategy on mortality in patients with sepsis: a meta-analysis. Crit Care Med. 2008; 36:2734–2739 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA. 2016; 315:801–810 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Seymour CW, Liu VX, Iwashyna TJ, Brunkhorst FM, Rea TD, Scherag A, et al. Assessment of clinical criteria for sepsis: for the third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA. 2016; 315:762–774 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Freund Y, Lemachatti N, Krastinova E, Van Laer M, Claessens YE, Avondo A, et al. Prognostic accuracy of sepsis-3 criteria for in-hospital mortality among patients with suspected infection presenting to the emergency department. JAMA. 2017; 317:301–308 [DOI] [PubMed] [Google Scholar]
- 7.Finkelsztein EJ, Jones DS, Ma KC, Pabon MA, Delgado T, Nakahira K, et al. Comparison of qSOFA and SIRS for predicting adverse outcomes of patients with suspicion of sepsis outside the intensive care unit. Crit Care. 2017; 21:73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Raith EP, Udy AA, Bailey M, McGloughlin S, MacIsaac C, Bellomo R, et al. Prognostic accuracy of the SOFA score, SIRS criteria, and qSOFA score for in-hospital mortality among adults with suspected infection admitted to the intensive care unit. JAMA. 2017; 317:290–300 [DOI] [PubMed] [Google Scholar]
- 9.Churpek MM, Snyder A, Han X, Sokol S, Pettit N, Howell MD, et al. Quick Sepsis-related Organ Failure Assessment, Systemic Inflammatory Response Syndrome, and Early Warning Scores for detecting clinical deterioration in infected patients outside the intensive care unit. Am J Respir Crit Care Med. 2017; 195:906–911 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Williams JM, Greenslade JH, McKenzie JV, Chu K, Brown AFT, Lipman J. Systemic Inflammatory Response Syndrome, quick Sequential Organ Function Assessment, and organ dysfunction: insights from a prospective database of ED patients with infection. Chest. 2017; 151:586–596 [DOI] [PubMed] [Google Scholar]
- 11.Moskowitz A, Patel PV, Grossestreuer AV, Chase M, Shapiro NI, Berg K, et al. Quick Sequential Organ Failure Assessment and Systemic Inflammatory Response Syndrome criteria as predictors of critical care intervention among patients with suspected infection. Crit Care Med. 2017; 45:1813–1819 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi JC, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005; 43:1130–1139 [DOI] [PubMed] [Google Scholar]
- 13.Bone RC, Balk RA, Cerra FB, Dellinger RP, Fein AM, Knaus WA, et al. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine. Chest. 1992; 101:1644–1655 [DOI] [PubMed] [Google Scholar]
- 14.Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal SM, et al. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2012. Crit Care Med. 2013; 41:580–637 [DOI] [PubMed] [Google Scholar]
- 15.Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D, et al. 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Intensive Care Med. 2003; 29:530–538 [DOI] [PubMed] [Google Scholar]
- 16.Gaieski DF, Edwards JM, Kallan MJ, Carr BG. Benchmarking the incidence and mortality of severe sepsis in the United States. Crit Care Med. 2013; 41:1167–1174 [DOI] [PubMed] [Google Scholar]
- 17.Kaukonen KM, Bailey M, Suzuki S, Pilcher D, Bellomo R. Mortality related to severe sepsis and septic shock among critically ill patients in Australia and New Zealand, 2000–2012. JAMA. 2014; 311:1308–1316 [DOI] [PubMed] [Google Scholar]
- 18.Rose L, Scales DC, Atzema C, Burns KE, Gray S, Doing C, et al. Emergency department length of stay for critical care admissions. a population-based study. Ann Am Thorac Soc. 2016; 13:1324–1332 [DOI] [PubMed] [Google Scholar]
- 19.Horwitz LI, Green J, Bradley EH. US emergency department performance on wait time and length of visit. Ann Emerg Med. 2010; 55:133–141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chalfin DB, Trzeciak S, Likourezos A, Baumann BM, Dellinger RP; DELAY-ED Study Group. Impact of delayed transfer of critically ill patients from the emergency department to the intensive care unit. Crit Care Med. 2007; 35:1477–1483 [DOI] [PubMed] [Google Scholar]


