Supplemental Digital Content is Available in the Text.
Keywords: Low-back pain, Primary care, Patients' needs, Patients' experiences
Abstract
Introduction:
There is a knowledge gap about the current experiences and needs of people with low back pain (LBP) seeking primary care in Australia.
Objectives:
The aim of this study was to understand the experiences and needs of Australians who have received treatment for LBP in primary care.
Methods:
This was a prospective, cross-sectional internet survey conducted between July 2017 and September 2017. Participants were adults who had experienced an episode of LBP in the past year, had sought primary care in Australia, and were proficient in English. Outcomes were patient-reported experiences about primary care treatment, including reasons for seeking care, health care practitioners consulted, components of care received, and patients' evaluations of the importance and helpfulness of treatment.
Results:
A total of 426 Australians completed the survey. The response rate of survey completion was 50%. Participants reported seeking primary care for LBP not only for pain relief, but for difficulties with activities and participation with usual social roles as well as quality of life and mood. Participants consulted multiple health care practitioners and used numerous treatment modalities. Only half reported they received education and a very low proportion were aware of receiving guideline-based advice. The level of satisfaction with care was below moderate for 42% of respondents. Participants reported that they want LBP care to be more person-centred and better tailored to their needs; they also reported wanting more education, particularly about prevention of future episodes and self-management.
Conclusions:
The needs of people currently seeking primary care for LBP in Australia do not seem to be adequately met. Improving patients' experiences and outcomes may require better integration of health care across providers and delivery of more person-centred care.
1. Introduction
The Global Burden of Disease Study 2016 reports that low-back pain (LBP) is the highest cause of years lived with a disability in Australia and globally, and that this burden is worsening.5 According to the 2014 to 2015 National Health Survey, 1 in 6 Australians report suffering from LBP during the previous year.25 The 2018 Lancet series identified that LBP now poses a major global challenge and advocated for low-value care that is ineffective or potentially harmful to be reduced, and for high-value guideline-based care to be implemented.3 However, it is widely recognised that the translation of evidence from guidelines into clinical practice is challenging. One contributor to this problem may be that the domains of clinical expertise, and patient values are frequently overlooked when implementing evidence-based practice (EBP), with a disproportionate focus on the third element of the EBP model, research evidence.12
For clinicians to successfully implement high-value guideline-based care for people with LBP within an EBP framework, it is critical to understand the health care needs and experiences of patients. Although efforts have been made to understand factors related to primary care clinicians in LBP care in Australia,8,19 relatively little is known about patient-related factors. A systematic scoping review of studies investigating patients' health care needs and experiences for LBP4 found that only 2 studies have been conducted in Australia, both exploring patients' experiences in specific clinical settings beyond primary care.2,20,21 Therefore, a knowledge gap exists about the broader experiences and needs of people with LBP seeking primary care in Australia.
The aim of this study was to understand the experiences and needs of patients seeking primary care for LBP in Australia. This is the first of a series of studies to develop a codesigned model of care for acute LBP that meets consumers' needs and addresses local health system factors.
2. Methods
2.1. Study design
This study was a prospective cross-sectional internet survey of Australians who had received primary care treatment for LBP. The survey design, including quantitative and qualitative responses, is a widely accepted methodological approach to investigate people's experience of health care (eg, Measuring Patient Experiences, The U.K. Health Foundation, Evidence Scan, June 2013). The survey was hosted by Qualtrics (Provo, UT), licensed to Macquarie University. The study was approved by Macquarie University Human Research Ethics Committee (Ref: 520170078) and is reported using the Checklist for Reporting Results of Internet E-Surveys (CHERRIES, Appendix 1, available at http://links.lww.com/PR9/A46).
2.2. Participants
Participants consisted of respondents to an internet survey conducted between July 1 and September 30, 2017. Participants were eligible if they were an Australian resident, aged 18 years or older, had experienced an episode of LBP in the past 12 months, had adequate proficiency in English, and had sought primary care treatment for their LBP. People were invited to complete the survey through advertising through professional networks (eg, Australian Pain Society, Australian Physiotherapy Association, NSW Agency for Clinical Innovation, and Painaustralia) and other networks (eg, university communities), using electronic and manual methods in health care clinics (community general practice and physiotherapy clinics, hospitals) and notice boards in the community (eg, shopping centres, gyms, and libraries) as well as through social media posts (eg, LinkedIn and Facebook). Participation in the survey study was voluntary and anonymous.
2.3. Survey design
The survey (Appendix 2, available at http://links.lww.com/PR9/A46) was designed to take approximately 15 minutes to complete and consisted of questions in the following categories:
2.3.1. Sociodemographic characteristics and clinical information
Descriptive sociodemographic data were collected and clinical information about participants' LBP, including episode duration and recurrence, using single-item questions. In this survey, an episode was defined as LBP that lasted at least 24 hours. Participants rated their average pain during their most recent LBP episode on an 11-point numerical rating scale (0 = no pain at all, 10 = worst pain imaginable). Levels of interference of LBP with daily functioning were assessed using the Brief Pain Inventory (BPI), which has been validated in an LBP population.13
2.3.2. Primary care–seeking behaviour
Data were obtained about health care provider participants had consulted for their LBP, including the number of consults to each provider and reasons for seeking care.
2.3.3. Primary care treatments received
Participants reported what types of treatment they received, how important they considered each treatment component (on a 4-point Likert scale, not at all to extremely) and the perceived helpfulness of those treatments (on a 4-point Likert scale, not at all to extremely). Participants who reported receiving education were further asked (1) whether they received any of the key educational messages recommended in current LBP clinical guidelines16–18 and (2) whether they received any educational resources, such as a booklet or video. Data were also obtained about whether participants received self-management advice, defined in the survey as “a way in which you can manage your symptoms or condition in your own time, eg, at home or outside the home to manage your low-back symptoms.” Those who had were asked whether they implemented these strategies and how helpful these were in managing their LBP.
2.3.4. Satisfaction with care
Participants were asked to rate their overall satisfaction with the treatment they had received on a 5-point Likert scale (extremely dissatisfied to extremely satisfied).
2.3.5. Qualitative responses
Participants could provide free text responses about aspects of treatment for their LBP. Two authors (M.A. and J.M.H.) independently reviewed the responses and identified common themes, which were grouped into (1) treatment gaps and barriers and (2) treatment facilitators. Illustrative quotes were extracted for each theme.
2.4. Data analysis
Participants' data were only included in the analysis if they completed the whole survey. Descriptive statistics (means or percentages with appropriate measures of variance) were used to analyse all outcomes. Data were analysed using SPSS, version 22 (SPSS, Inc, Chicago, IL).
3. Results
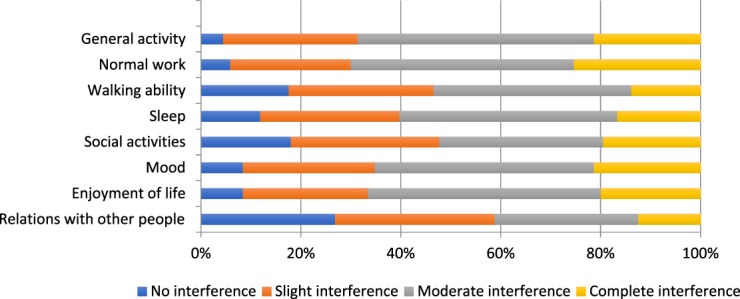
3.1. Sociodemographic and clinical characteristics of participants
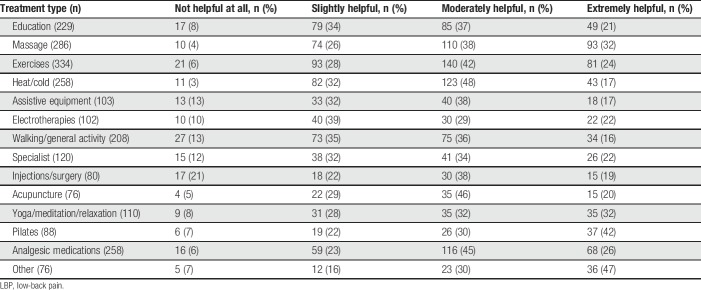
A total of 426 participants completed the survey. The 95% margin of error was 5%, based on National Health survey data from the Australian Institute of Health and Welfare.25 The response rate of survey completion was 50%. Participants were included from all 6 states of Australia and from the Australian Capital Territory. Table 1 summarises the demographic and clinical characteristics of the sample. Participants' age ranged from 18 to 82 years (mean: 43 years, SD 15); a high proportion of the sample was female and had a tertiary or postgraduate education level. Moderately high pain severity of the last LBP episode was reported (mean: 6.3 on 0–10 numerical rating scale, SD 1.9), and episode recurrence was common. Moderate to complete interference of back pain was reported with work (70% of participants), general activity (69%), enjoyment of life (67%), mood (65%), and sleep (60%) (Fig. 1). The mean BPI interference score for the sample was 5.5/10 (SD 2.5), indicating moderately high pain interference, given that people with complex chronic pain seeking specialist pain services in Australia have BPI scores of 7.0/10.22
Table 1.
Characteristics of participants (n = 426).
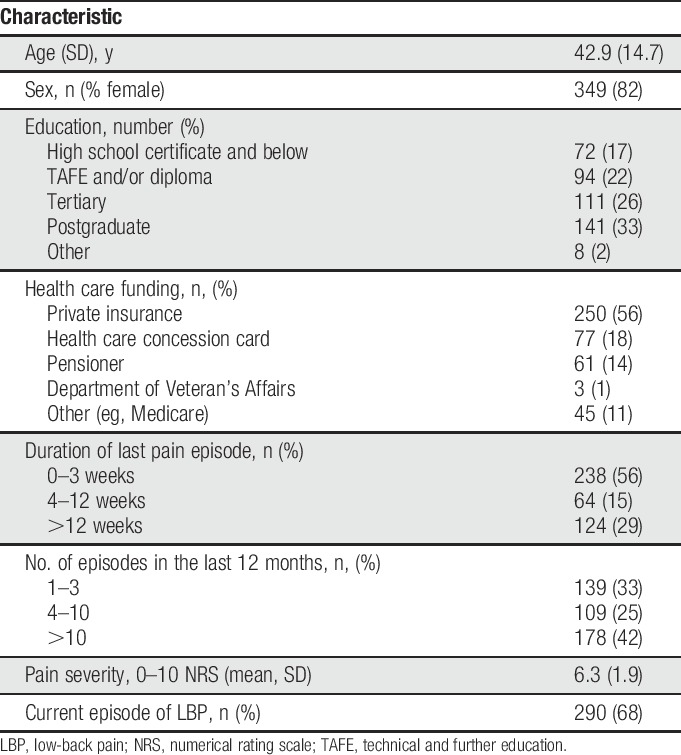
Figure 1.
Level of pain interference from LBP (measured with the Brief Pain Inventory) with daily functioning (percentage of participants endorsing interference categories). LBP, low-back pain.
3.2. Primary care–seeking behaviour
Most patients reported consulting multiple health care providers for their LBP in the past 12 months (Fig. 2) including general practitioners, physiotherapists, chiropractors, osteopaths, massage therapists, psychologists, pharmacists, acupuncturists, and specialists. The most common health care providers consulted were general practitioners and physiotherapists, at 65% and 61%, respectively; the lowest reported provider was osteopaths at 9% (Fig. 2). Analysis revealed that 79% of patients consulted 2 or more different types of health care practitioners for treatment of LBP, with more than a quarter (28%) consulting 4 to 8 different practitioners. When 2 practitioners were consulted, the most common professionals were general practitioners and physiotherapists (31% of participants). Most health care providers were consulted 2 to 4 times each for an episode of care (Appendix 3, available at http://links.lww.com/PR9/A46). The level of pain was the most common reason for seeking primary care, but other common reasons were reduced general activity, walking ability, and ability to do normal work (Appendix 4, available at http://links.lww.com/PR9/A46).
Figure 2.
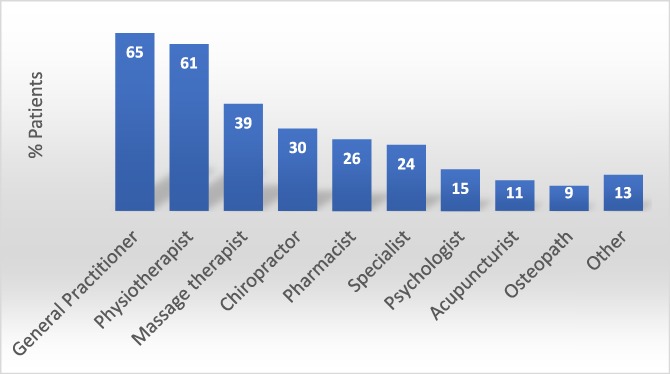
Percentage of health care practitioners consulted by patients for LBP in the past 12 months (multiple practitioners could be reported). LBP, low-back pain.
3.3. Primary care treatment received
Patients reported receiving multiple treatments for their LBP (Table 2). Most (61%) had received analgesic medications. A high proportion of participants reported being prescribed exercises (78%), although only half (49%) were advised to do general activity or walking. Passive therapies were very common, including massage therapy (67%), heat and cold therapies (61%), electrotherapies (24%), and acupuncture (18%).
Table 2.
Number and percentage of participants who received each treatment component for LBP (multiple treatment types could be reported).
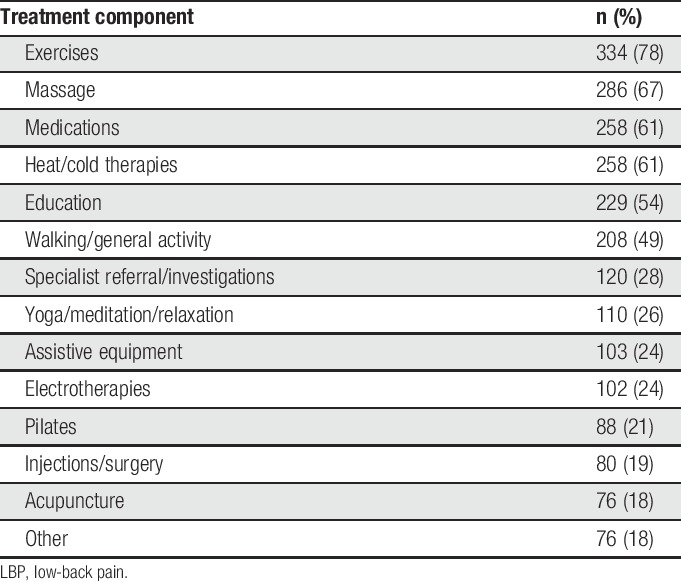
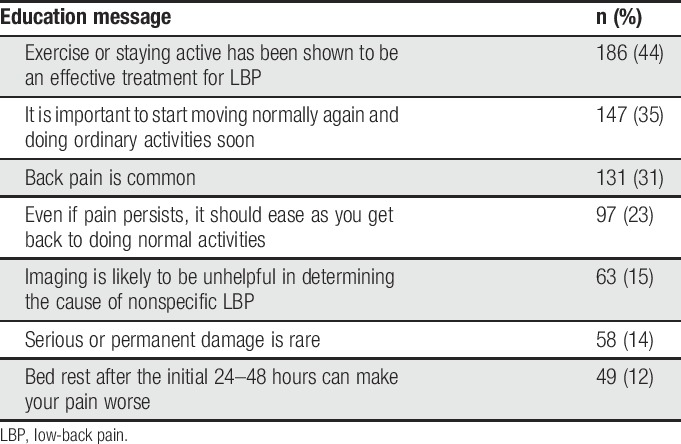
Approximately half of the participants reported receiving education. Of those that did, low proportions recalled being advised about key educational messages recommended in current LBP clinical guidelines, such as returning to normal activities (35%), avoiding prolonged bed rest (12%), and that LBP is common and serious damage is rare (14%); very few patients (15%) were advised that imaging is unlikely to be helpful (Table 3). More than half of patients (58%) reported receiving educational resources from their provider. The most common were exercise sheets (82%), then less frequently pamphlets (16%), online resources (15%), and smart phone apps (11%). Almost 60% of participants reported these resources were moderately or extremely helpful.
Table 3.
Number and percentage of participants who received educational messages recommended in current guidelines, for the 236 patients who received education (multiple education messages could be reported).
A high proportion (78%) of patients reported they were advised about self-management strategies, and of these, most stated they used them. The most common self-management approaches recommended were exercises to improve strength, range of motion, or muscle coordination (67%–81%).
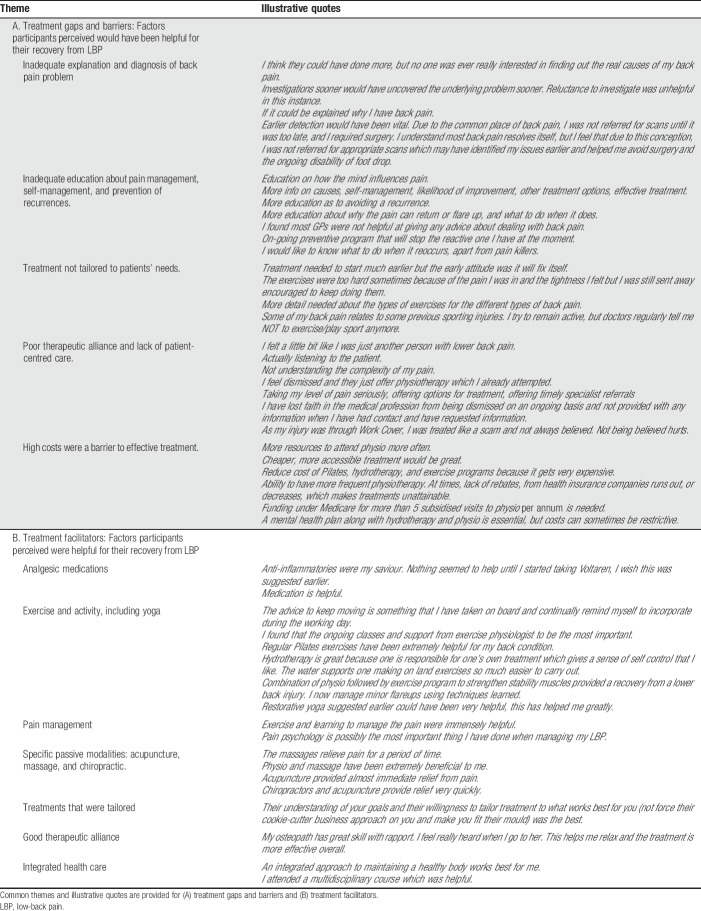
Participants rated how helpful different aspects of treatment were for their LBP (Table 4). Treatments that had the highest ratings of being moderately or extremely helpful (by ≥70% of participants) were massage, analgesic medications, and pilates. Treatments that were reported as being moderately or extremely helpful for between 60% to 69% of participants included exercise, heat and cold therapies, acupuncture, and yoga/relaxation/meditation.
Table 4.
Participants' ratings of helpfulness of treatments received for LBP.
Participants reported that the components of primary care for LBP they considered moderately or extremely important were education about their condition (78%); management of recurrence or flare ups (88%); learning self-management strategies (92%), and advice about when to access further treatment (83%) (Fig. 3).
Figure 3.

Patients' ratings of the importance of specific LBP treatment components (percentage of participants endorsing importance categories). LBP, low-back pain.
3.4. Satisfaction with primary care treatment for low-back pain
Two hundred forty-three (57%) patients reported they were moderately (33%) or extremely (24%) satisfied with their primary care treatment for LBP. However, 183 patients (43%) reported satisfaction was below moderate, with 16% slightly satisfied, 10% neither satisfied nor dissatisfied, and 17% dissatisfied with care.
3.5. Qualitative responses
Of the 426 participants, 52% (n = 221) provided free text responses about their needs and experiences of health care for LBP. Common themes are summarised in Table 5, and illustrative quotes are provided for each theme. Factors that participants identified as gaps or barriers in their LBP treatment included inadequate explanation and diagnosis of their LBP; insufficient education about pain management, self-management skills, and how to prevent or deal with LBP recurrence; inadequate tailoring of treatment to patients' needs; a lack of person-centred care and/or poor therapeutic alliance; and high costs of treatment. Treatment facilitators that participants reported included: analgesic medications; exercises and active approaches, including yoga; learning about pain management; modalities such as acupuncture and massage; treatments that were tailored to the individual; a good therapeutic alliance; and an integrated or multidisciplinary health care approach.
Table 5.
Qualitative responses from participants (n = 221, 52%) about their needs and experiences of health care for LBP.
4. Discussion
The results of this survey provide valuable insights into the recent experiences and needs of people seeking primary health care for LBP in Australia. The data show that satisfaction with LBP care in this Australian sample was relatively low, compared with a previous report of satisfaction in primary care for musculoskeletal conditions in Australia.11 Given that LBP is so common, affecting 1 in 6 Australians,25 this suggests that there is significant scope to improve patient satisfaction in primary care for LBP.
The survey reveals that most people with LBP consult multiple practitioners for health care, with more than a quarter of participants consulting 4 to 8 different types of practitioners; the clinicians most commonly consulted are general practitioners and physiotherapists. One reason for this treatment-seeking behaviour may be that patients were dissatisfied with care from an individual practitioner. However, another explanation may be that patients seek interprofessional care from a range of practitioners to address different needs for care of their LBP. This latter explanation is supported by other evidence from the survey: participants reported seeking care not just for pain, but also to address difficulties with activity limitations (eg, walking) and participation restrictions (eg, the ability to do normal work), as well as reduced enjoyment of life, social activities, and difficulties with mood. Furthermore, components of primary care for LBP considered helpful and important by patients were multimodal, including education, massage, analgesic medication, self-management advice, and exercise. These results suggest that people seek care for LBP to address the personal biopsychosocial contributors to their pain.7
Although the use of treatments not recommended by LBP clinical guidelines is often criticised, patients in our study reported they used and valued a wide range of treatment modalities, including those not endorsed by current guidelines. For example, while the National Institute for Health and Care Excellence (NICE) Guidelines for LBP16 state that simple analgesics such as paracetamol should not be offered, 71% of participants in this study reported that they found simple analgesic medication moderately or extremely helpful, in addition to active approaches to management. These findings provide perspective on how patient's preferences and experiences might be incorporated into evidenced-based and person-centred care for LBP.
Although education was rated as important by most participants, only half of the participants reported receiving any education, or being advised to return to general activity, both of which are central elements of guideline-based care.1 Of those who did receive education, very low proportions reported being given recommended guideline-based messages,15 such as to avoid prolonged bed rest, that LBP is common and serious damage is rare, or that imaging is unlikely to be helpful for most LBP patients. These results suggest that greater emphasis on delivering effective education in primary care for LBP is warranted.
This survey suggests there are disparities between guideline-based care for LBP and the treatments that patients are reporting they are using and finding helpful. Two perspectives might explain this finding. The first relates to practitioner behaviour: there is now good evidence that clinicians have difficulty implementing guideline-based care for many reasons, including that they believe guidelines restrict clinical judgement and challenge professional autonomy, and they consider guideline-based care does not adequately empower patients.19 Such factors may influence treatments offered by primary care practitioners to people seeking care for LBP in Australia. The second consideration relates to patients' needs. Although there are guideline-based treatments that patients clearly do want but are not receiving, (eg, education and self-management) there are also nonrecommended treatments (eg, massage or hot and cold therapies) that some patients find very beneficial. This exemplifies potential tensions between EBP guidelines and person-centred care that can impact on clinical practice. For example, in a study of Australian general practitioners treating other common conditions (dementia, chronic obstructive pulmonary disease, and hypertension), clinicians reported they found guideline-based recommendations sometimes inappropriate because their care needed to focus on treating the whole person and meet the priorities and needs of their patients.9 The challenge to deliver person-centred care within the framework of clinical guidelines clearly requires the judicious integration of clinical judgement and shared decision-making.
The qualitative responses from participants in this study show that patients want LBP care to be more person-centred, to receive better diagnostic information, to be better educated about their LBP and self-management skills. The findings also emphasise how patients value being listened to and believed, being treated as an individual, so that care could be better tailored to their needs. These results align closely with an earlier study of patient's perceptions of “a good back consultation”14 and with the systematic review of Chou et al.4 of patient's perceived needs for management of LBP in other countries. This latter review identified that patients' needs included person-centred care with good communication and shared decision-making, provision of more information from clinicians (including a cause of their LBP and legitimising their symptoms) and holistic, individualised care that fosters a good provider–patient relationship.
What are the clinical implications of this study? Health care practitioners may be better positioned to provide more high-value care for LBP if they can better understand individual patient's needs and develop person-centred treatments that address the multidimensional contributors to LBP; for some patients, this may require integrated care from multiple practitioners. The results also indicate that targeting effective and tailored patient education may be a useful priority. Enhanced understanding of patients' needs will also impact on the therapeutic alliance between the patient and clinicians, which is critical for optimising LBP outcomes.6 Finally, embracing a genuinely EBP approach to LBP emphasises not only person-centeredness but enables clinicians to prioritise their clinical reasoning, for example, to prescribe analgesic medication or order imaging in cases where it is deemed most efficacious for that individual patient in that clinical context.
This is the first of a series of studies that is using complex intervention development methods to design a model of primary care for acute LBP, called My Back My Plan. The model of care is being designed to align with a contemporary model of health care known as the Quadruple Aim,23 which aims to meet consumers' needs with person-centred care, address clinicians' work life, improve population health, and reduce costs with high-value care. This survey contributes to the first aim of meeting consumers' needs. A second survey has been completed that evaluates primary care clinicians' practices and experiences of delivering care for acute LBP. To ensure codesign with relevant stakeholders, focus groups have been held with LBP patients and primary care clinicians for their input into the new model of care, before feasibility and acceptability testing.
4.1. Strengths and limitations
The sample is representative of people who seek primary care for LBP in Australia, with respect to age, pain severity and recurrence, education level, and interference with function.10,24 There was also representation of people across geographical regions of Australia, including metropolitan and rural or remote areas. The response rate of completion for this study was 50%. Although survey results can be biased if the nonresponse is nonrandom, the ethical requirement of maintaining anonymity of survey participants in this study precluded the reasons underlying nonresponse to be identified. Participants' experiences of treatment for LBP were evaluated from a range of different primary health care providers. In addition, we sought information about recent clinical experiences of guideline-based care, which is of value in exploring patterns of adherence to clinical guidelines for LBP.
A limitation of the study is that it was based on a convenience sample, and as such, it is possible that the sample was biased toward those who were highly dissatisfied or highly satisfied with their care. Another limitation, inherent in attaining self-reported data from a survey, is that recall bias may influence the accuracy of the data; it was not possible to evaluate how accurately our survey sample recalled their experience of health care. Finally, although more females seek care for LBP than males,24 our sample has an unusually high proportion of females.
5. Conclusion
People seeking primary care for LBP in Australia do not report high satisfaction with care and are consulting multiple practitioners for treatment. Patients are using multiple treatment modalities and value many treatments that are not endorsed by current guidelines. The results illustrate that the path between EBP guidelines and person-centred care is difficult to navigate in clinical practice. However, patients with LBP clearly want more person-centred, individualised care, and for clinicians to provide more education about their LBP and how to manage it.
Disclosures
The authors have no conflict of interest to declare.
Acknowledgements
The authors are grateful to the participants who contributed information about their experiences of LBP care.
Appendix A. Supplemental digital content
Supplemental digital content associated with this article can be found online at http://links.lww.com/PR9/A46.
Footnotes
Sponsorships or competing interests that may be relevant to content are disclosed at the end of this article.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Web site (www.painrpts.com).
References
- [1].Almeida M, Saragiotto B, Richards B, Maher CG. Primary care management of non-specific low back pain: key messages from recent clinical guidelines. Med J Aust 2018;208:272–5. [DOI] [PubMed] [Google Scholar]
- [2].Briggs AM, Slater H, Bunzli S, Jordan JE, Davies SJ, Smith AJ, Quintner JL. Consumers' experiences of back pain in rural Western Australia: access to information and services, and self-management behaviours. BMC Health Serv Res 2012;12:357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Buchbinder R, van Tulder M, Öberg B, Costa LM, Woolf A, Schoene M, Croft P; Lancet Low Back Pain Series Working Group. Low back pain: a call for action. Lancet 2018;391:2384–8. [DOI] [PubMed] [Google Scholar]
- [4].Chou L, Ranger TA, Peiris W, Cicuttini FM, Urquhart DM, Sullivan K, Seneviwickrama M, Briggs AM, Wluka AE. Patients' perceived needs of healthcare providers for low back pain management: a systematic scoping review. Spine J 2018;18:691–711. [DOI] [PubMed] [Google Scholar]
- [5].Cooper C. Global, regional, and national, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017;390:1211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Ferreira PH, Ferreira ML, Maher CG, Refshauge KM, Latimer J, Adams RD. The therapeutic alliance between clinicians and patients predicts outcome in chronic low back pain. Phys Ther 2013;93:470–8. [DOI] [PubMed] [Google Scholar]
- [7].Fillingim RB. Individual differences in pain: understanding the mosaic that makes pain personal. PAIN 2017;158(suppl 1):S11–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Gardner T, Refshauge K, Smith L, McAuley J, Hübscher M, Goodall S. Physiotherapists' beliefs and attitudes influence clinical practice in chronic low back pain: a systematic review of quantitative and qualitative studies. J Physiother 2017;63:132–43. [DOI] [PubMed] [Google Scholar]
- [9].Hansen E, Walters J, Howes F. Whole person care, patient-centred care and clinical practice guidelines in general practice. Health Sociol Rev 2016;25:157–70. [Google Scholar]
- [10].Henschke N, Maher CG, Refshauge KM, Herbert RD, Cumming RG, Bleasel J, York J, Das A, McAuley JH. Characteristics of patients with acute low back pain presenting to primary care in Australia. Clin J Pain 2009;25:5–11. [DOI] [PubMed] [Google Scholar]
- [11].Hush JM, Lee HJ, Yung V, Adams R, Mackey M, Wand BM, Nelson R, Beattie P. Intercultural comparison of patient satisfaction with physiotherapy care in Australia and Korea: an exploratory factor analysis. J Man Manip Ther 2013;21:103–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Hush JM, Alison JA. Evidence-based practice: lost in translation? J Physiother 2011;57:207–8. [DOI] [PubMed] [Google Scholar]
- [13].Keller MS, Bann LC, Dodd RS, Schein SJ, Mendoza ST, Cleeland SC. Validity of the brief pain inventory for use in documenting the outcomes of patients with noncancer pain. Clin J Pain 2004;20:309–18. [DOI] [PubMed] [Google Scholar]
- [14].Laerum E, Indahl A, Skouen J. What is “the good back consultation”? A combined qualitative and quantitative study of chronic low back pain paitents' interaction with and perceptions of consultations specialists. J Rehabil Med 2006;38:252–62. [DOI] [PubMed] [Google Scholar]
- [15].Maher C, Underwood M, Buchbinder R. Non-specific low back pain. Lancet 2017;389:736–47. [DOI] [PubMed] [Google Scholar]
- [16].National Institute for Health and Care Excellence (NICE). Low back pain and sciatica in over 16s: assessment and management. 2016. Available at: https://www.nice.org.uk/guidance/ng59. Accessed 4 December 2018. [PubMed] [Google Scholar]
- [17].New South Wales Agency for Clinical Innovation. Model of care: management of people with acute low back pain. 2016. Available at: https://www.aci.health.nsw.gov.au/resources/musculoskeletal/management-of-people-with-acute-low-back-pain/albp-model/albp-moc. Accessed 4 December 2018. [Google Scholar]
- [18].Qaseem A, Wilt TJ, McLean RM, Forciea MA. Noninvasive treatments for acute, subacute, and chronic low back pain: a clinical practice guideline from the American College of Physicians. Ann Intern Med 2017;166:514–30. [DOI] [PubMed] [Google Scholar]
- [19].Slade SC, Kent P, Patel S, Bucknall T, Buchbinder R. Barriers to primary care clinician adherence to clinical guidelines for the management of low back pain. Clin J Pain 2016;32:800–16. [DOI] [PubMed] [Google Scholar]
- [20].Slade SC, Molloy E, Keating JL. Listen to me, tell me': a qualitative study of partnership in care for people with non-specific chronic low back pain. Clin Rehabil 2009;23:270–80. [DOI] [PubMed] [Google Scholar]
- [21].Slade SC, Molloy E, Keating JL. People with non-specific chronic low back pain who have participated in exercise programs have preferences about exercise: a qualitative study. Aust J Physiother 2009;55:115–21. [DOI] [PubMed] [Google Scholar]
- [22].Tardif H, Blanchard M, White J, Bryce M. Normative data for adults referred for specialist pain management in Australia: ePPOC Information Series No. 1. 2018. Available at: https://ahsri.uow.edu.au/eppoc/informationseries. Accessed 6 January 2019. [Google Scholar]
- [23].Wagner EH, LeRoy L, Schaefer J, Bailit M, Coleman K, Zhan C, Meyers D. How do innovative primary care practices achieve the quadruple aim? J Ambul Care Manage 2018;41:288–97. [DOI] [PubMed] [Google Scholar]
- [24].Walker BF, Muller R, Grant WD. Low back pain in Australian adults. Health provider utilization and care seeking. J Manip Physiol Ther 2004;27:327–35. [DOI] [PubMed] [Google Scholar]
- [25].Website of The Australian Insitiute of Health and Welfare. Back problems snapshot: Available at: https://www.aihw.gov.au/reports/arthritis-other-musculoskeletal-conditions/back-problems/what-are-back-problems. Accessed 13 March 2019. [Google Scholar]