Abstract
This study was to investigate the effects of Tai Chi (TC) and whole-body vibration (WBV) exercise in sarcopenic men in advanced old age. Ninety sarcopenic men (mean age 88.6 years; age range 85–101 years) were divided into three groups: TC group, WBV group, and control (CON) group. Patients in the two treatment groups received 8 weeks of training in either TC or WBV, while the control group received reminders not to change their level of physical exercise or lifestyle. Patients in all groups also received health information related to sarcopenia. Muscle mass, muscle strength, and physical performance [balance, gait speed, timed-up-and-go test (TUGT), and five-times-sit-to-stand test (FTSST)] were analyzed and compared among the three groups. Finally, seventy-nine subjects completed the study (TC n = 24; WBV n = 28; and CON 27). Muscle strength was significantly increased in the TC and WBV groups compared to the control group (P < 0.01). Following 8 weeks of exercise, improvements were observed in all physical performance tests for the TC and WBV groups (P < 0.05). The improvement in balance was greater in the TC group than the WBV group. Time × Group effects revealed significant improvements in muscle strength in the lower extremities (P < 0.05) and physical performance (P < 0.01) in both the TC and WBV groups. Changes in muscle mass, as measured by dual-energy X-ray absorptiometry, did not significantly differ between groups. These findings indicate that TC and WBV are effective treatments for improving muscle strength and physical performance in sarcopenic men in advanced old age.
Keywords: Tai Chi, Whole-body vibration, Sarcopenia, Advanced old age
Introduction
Sarcopenia is characterized by low muscle mass, low muscle strength, and poor physical performance (Alfonso et al. 2010). Effective, economical interventions to alleviate these symptoms are limited. Sarcopenia has emerged as a significant health problem in the elderly Asian population, with high prevalence and harmfulness, leading to a variety of acute and chronic diseases such as osteoporosis, fatigue, falling, physical disability, and even death (Lee et al. 2007; Roubenoff 2003; Morley et al. 2001; Xue et al. 2011; Laurentani et al. 2003; Kim et al. 2016). Studies evaluating sarcopenia in Japan (Tanimoto et al. 2012a), Hong Kong (Lau et al. 2005), Taiwan (Chien et al. 2008), and Korea (Kim et al. 2012) have reported prevalence rates ranging between 5 and 13% in people aged 70–80 years and 50% in people > 80 years (Baumgartner et al. 1998; Tanimoto et al. 2012b; Janssen et al. 2004). In a study of 4000 elderly Chinese patients, Lee et al. (2007) found various disorders, such as chronic pulmonary disease, atherosclerosis, hypertension, diabetes, and heart disease, to be associated with sarcopenia. In a cross-sectional study of 679 people aged 40–79 years, Verschueren et al. (2013) found that sarcopenic patients have a twofold increase in the risk of osteoporosis. Li et al. (2015) studied 562 cases of hospitalized older adults and found osteoporosis and skeletal muscle reduction to be related to gender; in elderly men, a significant correlation was observed between skeletal muscle loss and osteoporosis. Sarcopenic men have also been found to have increased risks of falling and higher disability rates (Moreland et al. 2004; Fan 2014). In a study observing 364 elderly adults (aged 80–85 years) for 7 years, the death rate was higher in sarcopenic men (67.4%) than non-sarcopenic men (41.2%) (Landi et al. 2013). In the United States, the cost of health problems caused by reduced muscle mass and strength was reported to be ~ 18.5 billion dollars (based on data from 2000), of which 58.4% was spent on males (Landi et al. 2013). Sarcopenia is an important health issue, and it is imperative to investigate methods to prevent and treat this disorder.
Currently, there is no clear consensus on the appropriate clinical intervention for sarcopenia. In China, Tai Chi (TC) practice is common and, in older adults, has better compliance rates compared with simple resistance training (Chang et al. 2011). The semi-squat position is used in TC in a series of movements, in a slow and flowing manner (Nomura et al. 2011), which can strengthen muscles of the lower extremities. It has been shown that, during TC, oxygen consumption is 55% of peak oxygen consumption, and heart rate is 58% of the maximum heart rate (Field 2011). Therefore, TC is considered a moderately intensive aerobic exercise, which is more suitable for older adults. Several studies have shown that people practicing TC have better muscle strength, balance, coordination, and concentration abilities (Li et al. 2009; Gao et al. 2014; Pei et al. 2008; Chen et al. 2008); these qualities help to improve physical function and prevent falling in older adults.
Whole-body vibration (WBV) exercise is a novel approach for treating various physical disorders in elderly patients. For those unable to perform resistance exercises, WBV exercise can be performed with limited weight and low dynamic joint movement (Roelants et al. 2004a). WBV exercise is a safe and low-impact training method, with a relatively low involvement threshold and has been shown to have a significant influence on geriatric health care (Tsuji et al. 2014). WBV may also be suitable for frail individuals (e.g., those in long-term care or rehabilitation programs) (Bautmans et al. 2005) and can be easily carried out in the community. In the present study, the efficacy and safety of TC and WBV were investigated in elderly sarcopenic men. Outcomes of interest included muscle mass, muscle strength, and physical function.
Materials and methods
Study design and subjects
The prospective randomized controlled trial for elderly sarcopenic men was approved by the Clinical Research Ethics Committee of the PLA General Hospital. The study design and performance were based on the principles of the Helsinki Declaration. A total of 90 patients were recruited and randomly assigned to one of three treatment groups: (1) TC group (n = 30); (2) WBV group (n = 30); and (3) the control (CON) group (n = 30). This was done by assigning 30 random numbers, from 1 to 90, to each group without duplication. Patients in all groups received health information related to sarcopenia. All patients provided prior written informed consent. Prior to treatment, subjects were asked to complete a physical examination and questionnaire (which included the following: name, age, height, weight, smoking history, drinking history, exercise history, current illnesses, and medication history). The inpatient sections and test sites were located in the PLA General Hospital. Patients were required to participate in the exercises and tests on a daily basis (see highlight below).
The inclusion criteria were as follows: men aged 85 years and above; diagnosis of sarcopenia (Asian Working Group for Sarcopenia, AWGS) (Chen et al. 2014); living at a single residence for over 2 years; and could move on their own [i.e., they could walk and sit without assistance and could complete the timed-up-and-go test (TUGT) and five-times-sit-to-stand test (FTSST)]. None of the subjects had engaged in a systematic exercise program for at least 1 year prior to data collection. Exclusion criteria included: insulin-dependent diabetes mellitus, cardiovascular diseases, uncontrolled hypertension (> 150/90 mmHg), gallstones, kidney stone, infectious diseases, recent thrombosis, knee or hip prosthesis, pacemaker, musculoskeletal disorders, psychiatric disorders, epilepsy, undergoing any medical treatment that affects muscle mass, muscle strength, and balance, upper/lower extremity fracture in the previous 6 months, and any critical cognitive (Mini–Mental State Examination, MMSE score < 23) or physical dysfunctions that may interfere with the test or procedures.
Interventions
Simplified eight-style TC was performed in the rehabilitation hall at a specified time, 5 days per week for 8 weeks. Each TC session lasted 40 min and included a 10-min warm-up, 20-min practice, and 10-min relaxation. The exercise procedures included: (1) brachial rewinding; (2) left- and right-knee kyphosis step; (3) left and right mustangmane; (4) cloud hand; (5) left and right Golden Rooster; (6) right and left foot pedal; (7) right- and left-wing finger tips; and (8) crossing hands. Taking into account the potential and closing forces, there were a total of 10 movements. The training load was progressively increased over the 8-week period (Table 1). The program was organized by a TC expert with over 10 years of experience.
Table 1.
The exercise load for the TC group
| Weeks | Time | Frequency | Exercise groups |
|---|---|---|---|
| 1–2 | Morning | 1 | 2 |
| 3–4 | Morning | 1 | 2 |
| 5–6 | Morning | 1 | 2 |
| Afternoon | 1 | 2 | |
| 7–8 | Morning | 1 | 2 |
| Afternoon | 1 | 2 |
TC the Tai Chi group
For the WBV exercise, a Wellengang Excellence reciprocating vibration platform (SVG, Wellengang, Germany) was used. WBV exercise was performed in the rehabilitation hall at a specified time, 5 days per week for 8 weeks. Each WBV session lasted 40 min and included a 10-min warm-up, 20-min vibration exercise (5 groups/time, and 3 min/group, with 1-min resting between groups), and 10-min relaxation. Prior to the WBV exercise, subjects were familiarized with the exercise instrument and method. Subjects were instructed to stand on the vibration plate, with legs and knees slightly bent and hands clasping the vibration rope. In accordance with the overload principle, the training load was progressively increased, covering a frequency range of 12–16 Hz and peak-to-peak amplitude of 3–5 mm (Table 2). All sessions were closely supervised by qualified instructors.
Table 2.
The exercise load for the WBV group
| Weeks | Time | Frequency | Exercise group | Vibration frequency (HZ) | Amplitude (mm) |
|---|---|---|---|---|---|
| 1–2 | Morning/afternoon | 1 | 5 | 12 | 3 |
| 3–4 | Morning/afternoon | 1 | 5 | 14 | 4 |
| 5–6 | Morning/afternoon | 1 | 5 | 14 | 4 |
| 7–8 | Morning/afternoon | 1 | 5 | 16 | 5 |
WBV the whole-body vibration group
For the CON group, subjects were continually reminded not to change their level of physical exercise or lifestyle. They also participated in sarcopenia health education sessions and outcome evaluation. Subjects in the TC and WBV groups also participated in the health education sessions. Sessions were taught by a single researcher (once per month for 40 min), and topics included sarcopenia and its causes, pathogenesis, clinical performance, adverse impacts, disease prevention, and treatments.
During each exercise session, participants in all treatment groups were instructed to report any side effects. Compliance rates for each session were determined based on participant attendance. At the end of each session, the subjects and/or their family members were asked whether they had complied with the doctor’s advice (TC and WBV groups: no exercise other than the TC or WBV provided; CON: physical activity/lifestyle unchanged).
Measurements
All subjects were tested prior to all the experiments. The test equipments were as follows: (1) Dual-energy X-ray absorptiometry (DXA), measuring the muscle mass; (2) handheld JAMAR dynamometer (Sammons Preston, Bolingbrook, Illinois, USA), measuring the handgrip strength; and (3) handheld dynamometer FET3 (Hoggan Health Industries, West Jordan, UT, USA), measuring the lower-limb muscle strength.
Handgrip strength measurement (Stark et al. 2011)
The subjects’ grips were adjusted before testing. Subjects were in sitting position, with feet naturally flatting on the ground and the elbow angle of 90°, leaving a gap between the upper arm and the thorax (no more than 30°). The subjects held the grip with the maximum strength for 5 s, and the values were recorded. Measurement was performed two times for each of the left and right hands, with the interval time of 1–2 min, and the mean value was recorded.
Lower-limb strength measurement (Goonetilleke et al. 1994)
Subjects were seated on a chair (45 cm in height), with the trunk–thigh and knee joint angles of 90°. The lower-limb strength measurement was performed as follows: (1) iliopsoas (hip flexion muscle): hips were flexed at 45° and the dynamometer was placed at the distal thigh, near the knee joint; (2) quadriceps femoris (knee extension muscle): hip and knee were flexed at 90° and the dynamometer was placed at the tibial surface, proximal to the ankle joint; (3) tibialis (foot dorsiflexion muscle): hip and knee were flexed at 90° and the dynamometer was placed over metatarsals; and (4) hamstring (knee flexion muscle): hip and knee were flexed at 90° and 45°, respectively, and the dynamometer was placed at 1/3 of the distal calf. During the test, the subjects were asked to maintain 5-s maximal isometric contraction strength. Subjects performed the maximal voluntary isometric contraction of these four muscle groups for two times. The time interval was 2 min, and the mean value was recorded.
Physical performance measurement
The 6-m gait speed test (Lund et al. 2017)
A straight line of 12 m was marked on the ground. The starting point, as well the 3-m, 9-m, and 12-m points, was marked. The subjects were informed to walk at normal speed and pace. The time between the patient’s front foot touching the 3-m point to the back foot leaving the 9-m point was recorded. The test was performed for two times, with the interval resting time for 2–3 min, and the mean value was recorded.
Timed-up-and-go test (TUGT) (Barbat-Artigas et al. 2014)
The time was recorded while the subject rose from the arm chair (45 cm in height; standing up with the arms crossing over the chest), headed ahead for 3 m (as quickly as they could, with the normal pace), bypassed the obstacles, walked back, and sat down again. This test did not require any special equipment or training. The test was performed for two times, with the interval resting time for 2–3 min, and the mean value was recorded.
Five-times-sit-to-stand test (FTSST) (Fragala et al. 2015)
Subjects were asked to stand up from a chair (45 cm in height), with their arms crossed over the chest. They needed to complete the sit-to-stand test, for five times, as fast as possible. The time of completing the whole process was recorded. The test was performed for two times, with the interval resting time for 2–3 min, and the mean value was recorded.
Balance test (Gusi et al. 2006)
For the static balance test, subjects wore comfortable cloth, with eyes closed (covered by eye mask), hands akimbo, left and right foot rotation standing, the other leg kneeing, and feet lifted off the ground in 10-cm height. Timing began when the foot lifted off the ground, which ended when the standing legs moved, touched the ground, or the body was severely shaken. For the dynamic balance test, subjects stood (with eyes closed) in a 40-cm diameter circle, stepping at a step speed of 120 steps per minute, and the stepping height should be equal to the supporting ankle joint. Time recording was ended when any foot touched the circle line or the body balance fail to continue. The test was performed for two times, with the interval resting time for 2–3 min, and the mean value was recorded.
Statistical analysis
Data were expressed as mean ± SD (standard deviation). Statistical analysis was performed with the SPSS (SPSS Inc., IL, USA) 17.0 software. The Chi-squared test and one-way ANOVA were used for differences between the three groups at baseline. For the tests, the changes were calculated and compared between the 0 weeks and 4 weeks, 0 weeks and 8 weeks, and 4 weeks and 8 weeks. One-way ANOVA with post hoc analysis was used for comparison among groups. Two-factor repeated-measure ANOVA was used for differences among groups at different time points. The effect size of different periods was calculated, and an effect size of 0.8 was usually considered large; 0.5–0.8, moderate; and 0.2–0.5, small (Cohen 1988). P < 0.05 was considered statistically significant.
Results
Baseline assessment
Baseline characteristics of the sample population are displayed in Table 3. No significant differences were found between groups at baseline (P > 0.05). In total, 79 subjects completed the experiment (TC n = 24; WBV n = 28; CON n = 27). Eleven subjects withdrew from the study (two presented with lower back pain after 4 weeks of TC; four did not want to continue with TC exercise; two in the WBV group suffered from other disorders during the study; and three in the CON group developed airway infections). Subjects who completed the trial all had good compliance. There were no severe adverse effects or health problems in subjects from the two treatment groups.
Table 3.
Baseline characteristics of study subjects
| TC | WBV | Con | F/χ2 | P | |
|---|---|---|---|---|---|
| N | 24 | 28 | 27 | – | – |
| Age (year) | 88.8 ± 3.7 | 89.5 ± 4. 4 | 87.5 ± 3.0 | 1.15 | 0.13 |
| Height (m) | 1.68 ± 0.47 | 1.65 ± 0.25 | 1.63 ± 0.06 | 0.12 | 0.89 |
| Weight (kg) | 63.1 ± 6.6 | 64.2 ± 6.7 | 66.2 ± 10.5 | 0.61 | 0.55 |
| BMI (kg/m2) | 22.4 ± 3.1 | 22.5 ± 2.2 | 23.5 ± 3.9 | 0.91 | 0.41 |
| Medications, category | 4.6 ± 3.4 | 5.4 ± 2.7 | 5.8 ± 3.3 | 1.92 | 0.59 |
Medications include: 1) neurological drugs: tranquilizers, hypnotics, antianxiety, antidepressants; 2) cardiovascular drugs: antihypertensive drugs, vasodilators, anticoagulants; 3) analgesics; 4) hypoglycemic agents; 5) antibiotics; and 6) others
TC the Tai Chi group, WBV the whole-body vibration group, CON the control group, BMI body mass index (kg/m2)
Outcome evaluation
Body composition
From baseline to 8 weeks, no significant increase was observed in whole-body weight or muscle mass of the upper extremities, lower extremities, or trunk (Table 4; P > 0.05).
Table 4.
Muscle mass assessment at baseline and after 8 weeks of training
| TC (n = 24) | WBV (n = 28) | CON (n = 27) | Time × group | ||||
|---|---|---|---|---|---|---|---|
| Baseline | 8-week | Baseline | 8-week | Baseline | 8-week | ||
| UM | 4.28 ± 0.59 | 4.30 ± 0.54 | 4.35 ± 0.62 | 4.43 ± 0.51 | 4.46 ± 0.52 | 4.41 ± 0.68 | P > 0.05 |
| LM | 13.52 ± 2.28 | 13.60 ± 2.23 | 13.18 ± 2.77 | 13.35 ± 2.21 | 13.49 ± 2.03 | 13.51 ± 1.92 | P > 0.05 |
| TM | 20.66 ± 1.54 | 21.03 ± 1.57 | 21.74 ± 1.66 | 21.79 ± 1.75 | 21.98 ± 1.63 | 21.47 ± 1.71 | P > 0.05 |
| BM | 41.45 ± 3.44 | 42.11 ± 2.97 | 42.33 ± 3.68 | 42.76 ± 3.35 | 43.52 ± 3.76 | 43.04 ± 3.91 | P > 0.05 |
For time × group effects determined for comparisons of these three intervention groups
UM upper limb muscle mass, LM lower-limb muscle mass, TM trunk muscle mass, BM body muscle mass, TC the Tai Chi training group, WBV the whole-body vibration therapy group, CON the control groups
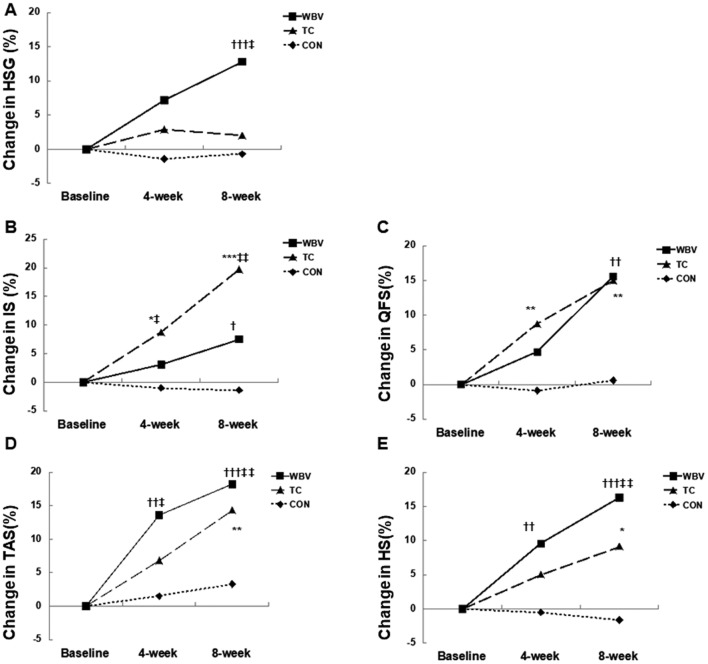
Muscle strength
As shown in Table 5, significant Time × Group effects were observed for handgrip strength,iliopsoas muscle strength,quadriceps femoris muscle strength,tibialis anterior muscle strength,hamstring muscle strength(HGS, IS, QFS, TAS, and HS) (P < 0.05). A significant increase in handgrip strength was observed in the WBV group at 8 weeks (12.8 ± 1.9%; P = 0.003), but not in the TC or CON groups.
Table 5.
Muscle strength data during the intervention (mean ± SD)
| Muscle strength (kg) | TC (n = 24) | WBV (n = 28) | CON (n = 27) | time × group | |||
|---|---|---|---|---|---|---|---|
| Baseline | 8-week | Baseline | 8-week | Baseline | 8-week | ||
| Handgrip | 14.87 ± 5.33 | 15.29 ± 5.38 | 13.41 ± 4.84 | 15.09 ± 4.44** | 15.50 ± 3.97 | 15.16 ± 4.52 | 0.02 |
| Iliopsoas | 22.85 ± 4.23 | 26.78 ± 5.02*** | 20.99 ± 6.65 | 22.17 ± 5.77 | 21.24 ± 6.90 | 20.94 ± 6.33†† | < 0.0001 |
| Quadriceps femoris | 17.07 ± 2.12 | 19.63 ± 3.04** | 17.08 ± 3.63 | 19.74 ± 3.92** | 18.04 ± 4.97 | 18.15 ± 4.75††‡‡ | 0.0016 |
| Tibialis anterior muscle | 17.71 ± 3.42 | 20.25 ± 4.65*** | 16.98 ± 3.57 | 20.07 ± 3.98*** | 17.13 ± 3.46 | 17.69 ± 3.11††‡‡ | < 0.0001 |
| Hamstrings | 21.37 ± 4.37 | 22.80 ± 4.00 | 20.55 ± 3.33 | 23.90 ± 3.42*** | 19.79 ± 6.66 | 19.47 ± 5.76‡‡ | 0.0012 |
TC Tai Chi group, WBV whole-body vibration group, CON control group, HGS handgrip strength, IS iliopsoas muscle strength, QFS quadriceps femoris muscle strength, TAS tibialis anterior muscle strength, HS hamstring muscle strength
For time × group effects determined for comparisons of these three intervention groups. Where significant time × group effects existing in the comparison of the three intervention groups, * indicated significant differences within the group vs. baseline. † Indicated significant differences vs. the same time point in the TC group or ‡ vs. the same time point in the WBV group. Significance indicated by increasing number of symbols (**P < 0.01, ***P < 0.0001, ††P < 0.01, and ‡‡P < 0.01, respectively)
For the IS, significant improvements were observed in the TC group at 8 weeks (17.2 ± 4.4%; P < 0.0001). Similarly, HS was significantly increased in the WBV group at 8 weeks (16.3 ± 3.5%; P < 0.0001). In both cases, there were significant differences compared with the control group (P < 0.01; Table 5).
In both the TC and WBV groups, significant increases were observed in QFS (TC 15.0 ± 3.2%; WBV 15.6 ± 3.0%) and TAS (TC 14.3 ± 3.8%; WBV 18.2 ± 4.1%) (P < 0.01), which were also significantly different from the CON group (P < 0.01; Table 5).
After 4 weeks of exercise, there were no significant changes in handgrip strength between the TC, WBV, and CON groups (Fig. 1a). In the TC group, the increase in the IS (P = 0.04) and QFS (P < 0.01) was significantly higher than in the CON group (Fig. 2). IS was also significantly higher in the TC group compared with the WBV group (P = 0.02).
Fig. 1.
Changes in muscle strength status with the intervention. Figure adjusted for baseline values showed the significant time × group effects. Only intergroup effects were shown. Data were analyzed using repeated-measure ANOVA analysis. Significant differences between: *, TC versus CON; †, WBV versus CON; and ‡, TC versus WBV. Significance was indicated by increasing number of symbols (one, two, and three indicating P < 0.05, P < 0.01, and P < 0.0001, respectively). Within-group significance was not shown in the figure (instead, described in the text)
Fig. 2.
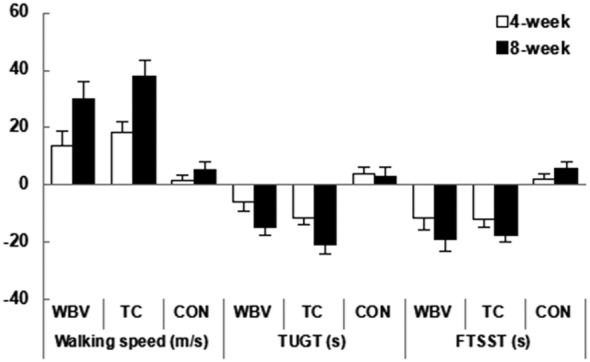
Changes in walking ability with the intervention. Figure adjusted for baseline values showed the significant time × group effects. Only intergroup effects were shown. Data were analyzed using repeated-measure ANOVA analysis. Significant differences between: *, TC versus CON; †, WBV versus CON; and ‡, TC versus WBV. Significance was indicated by increasing number of symbols (one, two, and three indicating P < 0.05, P < 0.01, and P < 0.0001, respectively). Within-group significance was not shown in the figure (instead, described in the text)
In the WBV group, significant increases were observed in TAS (P < 0.01) and HS (P < 0.01), compared with the CON group (Fig. 1D and E). TAS and HS were also significantly higher in the WBV group compared with the TC group (P < 0.01; Fig. 1D and E).
In a comparison of muscle strength change from baseline to 8 weeks between the WBV and TC groups, results were significantly different for HGS (P < 0.01), IS (P < 0.01), TAS (P < 0.01), and HS (P < 0.01). Additionally, QFS level was increased approximately in both treatment groups (Fig. 1C). Table 6 presents the effect sizes at different points of the study for each of the three groups.
Table 6.
The effect size of the muscle strength at different periods
| Period | HGS | IS | QFS | TAS | HS | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| TC | WBV | Con | TC | WBV | Con | TC | WBV | Con | TC | WBV | Con | TC | WBV | Con | |
| 0–4 weeks | 0.07 | 0.22 | 0.05 | 0.52b | 0.09 | 0.03 | 0.69b | 0.31 | 0.03 | 0.28 | 0.63b | 0.05 | 0.14 | 0.56 | 0.02 |
| 0–8 weeks | 0.09 | 0.63b | 0.08 | 0.84a | 0.22 | 0.05 | 0.95a | 0.81a | 0.02 | 0.81a | 0.85b | 0.10 | 0.34 | 1.00a | 0.11 |
| 4–8 weeks | 0.10 | 0.33 | 0.03 | 0.22 | 0.12 | 0.01 | 0.37 | 0.33 | 0.05 | 0.36 | 0.20 | 0.05 | 0.21 | 0.39 | 0.13 |
The differences in the effect size using Cohen’s d for all outcomes
TC the Tai Chi group, WBV the whole-body vibration group, CON the control group, HGS handgrip strength, IS iliopsoas strength, QFS quadriceps femoris strength, TAS tibialis anterior muscle strength, HS hamstring muscle strength
aThe effect size larger than 0.80, bthe effect size larger than 0.50
Walking ability and static/dynamic balance capacity
Using repeated-measure one-way analysis of variance (ANOVA), walking ability and balance capacity were found to be significantly increased in the TC group from baseline to 4 weeks and baseline to 8 weeks (P < 0.05; Figs. 2 and 3), relative to baseline values. After 8 weeks of TC exercise, TUGT and FTSST times were shortened by 4.20 ± 3.55 s (20.7 ± 4.5%) and 3.55 ± 2.08 s (17.7 ± 5.2%), respectively (Fig. 2). The 6-m gait speed was increased by 0.25 ± 0.28 m/s (37.8 ± 5.4%; Fig. 2). There was an increase in the one-leg standing time with eyes closed (3.68 ± 2.49 s; 150.4 ± 12.7%); however, a number of subjects were not able to complete this test [TC 4 subjects (17%); WBV 5/28 (18%); CON 4/27 (15%)]. Improved performance was also observed in the dynamic balance test (3.41 ± 2.72 s; 54.7 ± 6.2%; Fig. 3).
Fig. 3.
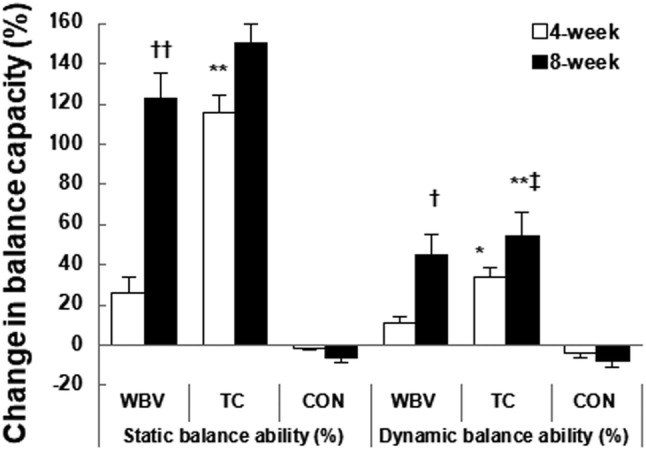
Changes in balance capacity with the intervention. Figure adjusted for baseline values showed the significant time × group effects. Only intergroup effects were shown. Data were analyzed using repeated-measure ANOVA analysis. Significant differences between: *, TC versus CON; †, WBV versus CON; and ‡, TC versus WBV. Significance was indicated by increasing number of symbols (one, two, and three indicating P < 0.05, P < 0.01, and P < 0.0001, respectively). Within-group significance was not shown in the figure (instead, described in the text)
No statistical differences were noted in walking ability or balance capacity after 4 weeks of WBV exercise; however, significant improvements were observed after 8 weeks (P < 0.05, relative to baseline). Additionally, in the WBV group, TUGT and FTSST times were shortened by 2.51 ± 0.71 s (14.7 ± 3.9%) and 3.45 ± 1.22 s (18.9 ± 4.4%), respectively (Fig. 2), and the 6-m walking speed was increased by 0.19 ± 0.23 m/s (30 ± 5.2%; Fig. 2). Static and dynamic balance times were increased by 2.74 ± 1.14 s (123 ± 13.3%) and 2.55 ± 1.36 s (45 ± 6.1%), respectively (Fig. 3).
Repeated-measure two-factor ANOVA was used to analyze differences between the three groups (Fig. 3). The effect sizes for physical performance at different periods are shown in Table 7. Overall, TC exercise led to improvements in both static and dynamic balance; these effects were greater than those observed with WBV exercise (P < 0.05). At 8 weeks, there were no differences in TUGT time, FTSST time, or 6-m walking speed between the TC and WBV groups (Fig. 2). Compared with the CON group, physical performance was significantly improved in both the TC and WBV groups (P < 0.01).
Table 7.
The effect size of the physical performance at different periods
| Period | 6-m gait speed | TUGT | FTSST | Static balance | Dynamic balance | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| TC | WBV | Con | TC | WBV | Con | TC | WBV | Con | TC | WBV | Con | TC | WBV | Con | |
| 0–4 weeks | 0.79b | 0.41 | 0.02 | 0.55b | 0.20 | 0.09 | 0.54b | 0.44 | 0.09 | 0.98a | 0.31 | 0.02 | 0.60b | 0.21 | 0.08 |
| 0–8 weeks | 1.11a | 0.99a | 0.06 | 0.80b | 0.51b | 0.07 | 0.81a | 0.74b | 0.29 | 1.11a | 0.89a | 0.26 | 0.94a | 0.81a | 0.14 |
| 4–8 weeks | 0.57b | 0.42 | 0.04 | 0.45 | 0.27 | 0.03 | 0.22 | 0.27 | 0.17 | 0.24 | 0.60b | 0.22 | 0.27 | 0.56b | 0.06 |
The differences in the effect size using Cohen’s d for all outcomes
TC the Tai Chi group, WBV whole-body vibration group, CON the control group, TUGT the timed-up-and-go test, FTSST the five-times-sit-to-stand test
aThe effect size larger than 0.80, bthe effect size larger than 0.50
Discussion
Sarcopenia is characterized by age-related loss of skeletal muscle, muscle strength, and muscular function. For the Asian population, there is no consistent treatment for sarcopenia. The primary purpose of this study was to investigate the influence of 8 weeks of TC and WBV exercise on the musculoskeletal system and physical performance in elderly sarcopenic men. Our results showed that the muscle mass did not change after 8 weeks of exercise. The findings are consistent with previous studies. For example, a 16-week TC program (Yang-style TC, two times/week, and 60 min/day) did not induce any significant change in the body mass in subjects > 75 years (Manson et al. 2013). Similarly, no changes were observed in lean mass in elderly subjects (75.17 ± 4.70) trained in the squat position on a vibration platform (three times/week for 11 weeks) (Gómez-Cabello et al. 2013). However, several studies have shown increases in the muscle mass in the younger subjects (Figueroa et al. 2012; Milanese et al. 2012; Roelants et al. 2004b) and in women (Milanese et al. 2013), as well as in clinical populations after a period of WBV exercise (Bogaerts et al. 2007; Machado et al. 2010). A 2007 study provided direct evidence that 1 year of WBV exercise could induce a 3–4% increase in muscle mass in men aged ≥ 60 years (Bogaerts et al. 2007). The change of the muscle mass may be influenced by training style, gender, age, population, and training period. In our study, the 8-week period of TC or WBV exercise was insufficient to induce muscle hypertrophy.
Our results demonstrated that exercise could enhance the muscle strength in sarcopenic men, to varying degrees. For example, we observed a significant increase in handgrip strength following WBV exercise. This is somewhat expected given that the patient holds the vibrating rope in both hands; this activates the muscle spindle receptors of the corresponding muscle group, while the peripheral muscle groups promote sustained muscle contraction and increase grip strength (Hollins and Roy 1996). Our results also showed improvements in lower-limb muscle strength following TC exercise, which may be positively associated with the execution of the semi-squat position (Yang et al. 2015) and the transition of movement from one pattern to another. This causes increased weight to be applied to the quadriceps femoris muscle as well as muscle groups around the calf (Yang et al. 2015; Su et al. 2015).
A recent study of 1-year TC exercise in older adults (mean age 62 years) observed an average increase of 43.3% in quadriceps strength (Xu et al. 2008). These results are consistent with the present study. Our results also showed a clear increasing trend in hamstring strength, though the result did not reach statistical significance. It is important to note that, due to weak lower extremity muscles in older adults, it is difficult to squat down during TC. To maintain the stability of the gravity center while moving, the step range is relatively small, which limits the contraction of the hamstring muscle. Therefore, it would be difficult to improve the hamstring muscle strength over a short time period.
During WBV exercise, vibration was transmitted to the target muscles with an attenuated frequency and amplitude so that the load on the distal muscle groups would not induce a significant enhancement in muscle strength (e.g., 5.6% for iliopsoas). Greater improvements in distal muscle strength may be achieved with longer durations of WBV exercise. Our results showed increasing trends for muscle strength in the three lower-limb muscle groups. Similarly, a previous study using a 30-Hz vibration frequency reported a 10% increase in isometric strength in the lower extremities after 12 weeks of exercise (Machado et al. 2010). Another study observed a significant increase (as high as 38.8%) in maximal voluntary isometric contraction following 10 weeks of lower-limb WBV exercise (Machado et al. 2010). In subjects undergoing 6 months of vibration therapy (35–45 Hz, 3–5 mm amplitude, five times/week), the maximum isometric strength of the quadriceps muscle increased by 13.84% (Tankisheva et al. 2015). A possible explanation for these outcomes may be that subjects are exposed to the vibration stimulus while standing on the vibrating platform, which stimulates the muscle spindles and activates α motor neurons; this contributes to the activation of muscle and nerve fibers and the enhancement of the neuromuscular system (Hung et al. 2009).
The assessment of physical performance mainly consisted of physical mobility and balance. TC and WBV exercise may produce different effects on balance in older individuals. In the present study, balance was significantly improved after 4 weeks of TC, and this effect was stronger than that observed following WBV exercise. This may be explained by the slow movements used in TC, as well as the gravity center shifts and constant joint motion (Li 2014; Nashner 1997). Additionally, more ontological receptors are activated to facilitate exercise control and body coordination (Li 2014; Nashner 1997). At the same time, increased lower extremity muscular strength also plays a key role in balance control (Yang et al. 2015). For the WBV group, quadriceps and anterior tibialis muscle strength was increased in older adults during walking, which provided enough support and ankle dorsal angle to prevent falling. This may be the main reason for the improved walking and balance abilities in the WBV group (Yang et al. 2015). Therefore, exercise interventions are beneficial for physical function in older adults.
The major limitation of this study was that the length of the exercise period (8 weeks) seemed insufficient to produce changes in muscle mass. This study was also limited by its small sample size, as only 79 older adults completed the experiment. Furthermore, the changes in subjects’ lower-limb muscular strength and physical function were not measured in the following weeks or months. Therefore, it is not known how long the improved muscle strength and physical function were maintained. Further in-depth studies are required to address these issues.
In conclusion, our results showed that older men with sarcopenia may benefit from TC and WBV exercise. TC and WBV are non-pharmacological therapies that can improve muscle strength and physical performance in older sarcopenic patients, though the effects on muscle mass are limited. TC may also help to improve balance, but only in patients with good physical fitness who are able to stand on their own; the patients must also have sufficient cognitive ability to be able to understand the trainers/coaches. For WBV exercise, patients can either sit or stand, with no fitness level requirement; this is particularly helpful for the older adults with weak cognitive ability. Thus, TC and WBV programs may be tailored to individual patients, based on their specific needs and abilities.
Funding
This study was supported by the research for early diagnosis indexes and intervention methods of sarcopenia (Grant No., 15BJZ39).
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Alfonso CJ, Francesco L, Eva T. Understanding sarcopenia as a geriatric syndrome. Curr Opin Clin Nutr Metab Care. 2010;13(1):1–7. doi: 10.1097/MCO.0b013e328333c1c1. [DOI] [PubMed] [Google Scholar]
- Barbat-Artigas S, Pion CH, Leduc-Gaudet JP, et al. Exploring the role of muscle mass, obesity, and age in the relationship between muscle quality and physical function. J Am Med Dir Assoc. 2014;15(4):303.e13–303.e20. doi: 10.1016/j.jamda.2013.12.008. [DOI] [PubMed] [Google Scholar]
- Baumgartner RN, Koehler KM, Gallagher D, et al. Epidemiology of sarcopenia among the elderly in New Mexico. Am J Epidemiol. 1998;147(8):755–763. doi: 10.1093/oxfordjournals.aje.a009520. [DOI] [PubMed] [Google Scholar]
- Bautmans I, Van Hees E, Lemper JC, et al. The feasibility of whole body vibration in institutionalised elderly persons and its influence on muscle performance, balance and mobility: a randomised controlled trial. BMC Geriatr. 2005;22(5):17. doi: 10.1186/1471-2318-5-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bogaerts A, Delecluse C, Claessens AL, Coudyzer W, Boonen S, Ver-schueren SM. Impact of whole-body vibration training versus fitness training on muscle strength and muscle mass in older men: a 1-year randomized controlled trial. J Gerontol A Biol Sci Med Sci. 2007;62:630–635. doi: 10.1093/gerona/62.6.630. [DOI] [PubMed] [Google Scholar]
- Chang JY, Tsai PF, Woods S, et al. Teaching Tai Chi to elders with osteoarthritis pain and mild cognitive impairment. Am J Recreat Ther. 2011;10(1):11–16. [PMC free article] [PubMed] [Google Scholar]
- Chen CH, Yen MF, Fetzer S, et al. The effects of Tai Chi exercise on elders with osteoarthritis: a longitudinal study. Asian Nurs Res. 2008;2(4):235–241. doi: 10.1016/S1976-1317(09)60005-0. [DOI] [PubMed] [Google Scholar]
- Chen LK, Liu LK, Woo J. Sarcopenia in Asia: consensus report of the Asian working group for sarcopenia. J Am Med Dir Assoc. 2014;15(2):95–101. doi: 10.1016/j.jamda.2013.11.025. [DOI] [PubMed] [Google Scholar]
- Chien MY, Huang TY, Wu YT. Prevalence of sarcopenia estimated using a bioelectrical impedance analysis prediction equation in community-dwelling elderly people in Taiwan. J Am GeriatrSoc. 2008;56(9):1710–1715. doi: 10.1111/j.1532-5415.2008.01854.x. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. Hillsdale: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- Fan L. Relationship between oligospermia and debilitating syndrome in the elderly. Chin J Health Care Med. 2014;16(6):415–416. [Google Scholar]
- Field T. Tai Chi research review. Complement Ther Clin Pract. 2011;17:141–146. doi: 10.1016/j.ctcp.2010.10.002. [DOI] [PubMed] [Google Scholar]
- Figueroa A, Gil R, Wong A, Hooshmand S, Park SY, Vicil F, Sanchez-Gon-zalez MA. Whole-body vibration training reduces arterial stiffness, blood pressure and sympathovagal balance in young overweight/obese women. Hypertens Res. 2012;35:667–672. doi: 10.1038/hr.2012.15. [DOI] [PubMed] [Google Scholar]
- Fragala MS, Dam TT, Barber V, et al. Strength and function response to clinical interventions of older women categorized by weakness and low lean mass using classifications from the foundation for the national institute of health sarcopenia project. J Gerontol A Biol Sci Med Sci. 2015;70(2):202–209. doi: 10.1093/gerona/glu110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao Q, Leung A, Yang Y, et al. Effects of Tai Chi on balance and fall prevention in Parkinson’s disease: a randomized controlled trial. Clin Rehabil. 2014;28(8):748–753. doi: 10.1177/0269215514521044. [DOI] [PubMed] [Google Scholar]
- Gómez-Cabello A, González-Agüero A, Ara I, Casajús JA, Vicente-Rodríguez G. Effects of a short-term whole body vibration intervention on lean mass in elderly people. 2013;28:1255–1258. doi: 10.3305/nh.2013.28.4.6491. [DOI] [PubMed] [Google Scholar]
- Goonetilleke A, Modarres-Sadeghi H, Guiloff RJ, et al. Accuracy, reproducibility, and variability of hand held dynamometry in motor neuron disease. J Neurol Neurosurg Psychiatry. 1994;57(3):326–332. doi: 10.1136/jnnp.57.3.326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gusi N, Raimundo A, Leal A. Low-frequency vibratory exercise reduces the risk of bone fracture more than walking: a randomized controlled trial. BMC Musculoskelet Disord. 2006;30(7):92. doi: 10.1186/1471-2474-7-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollins M, Roy EA. Perceived intensity of vibrotactile stimuli: the role of mechanoceptors channels. Somatosens Mot Res. 1996;13(3–4):273–286. doi: 10.3109/08990229609052583. [DOI] [PubMed] [Google Scholar]
- Hung JW, Liou CW, Wang PW, et al. Effect of 12-week Tai Chi Chuan exercise on peripheral nerve modulation in patients with type 2 diabetes mellitus. J Rehabil Med. 2009;41(11):924–929. doi: 10.2340/16501977-0445. [DOI] [PubMed] [Google Scholar]
- Janssen I, Baumgartner RN, Ross R, et al. Skeletal muscle cutpoints associated with elevated physical disability risk in older men and women. Am J Epidemiol. 2004;159(4):413–421. doi: 10.1093/aje/kwh058. [DOI] [PubMed] [Google Scholar]
- Kim YS, Lee Y, Chung YS, et al. Prevalence of sarcopenia and sarcopenic obesity in the Korean population based on the Fourth Korean National Health and Nutritional Examination Surveys. J Gerontol A Biol Sci Med Sci. 2012;67(10):1107–1113. doi: 10.1093/gerona/gls071. [DOI] [PubMed] [Google Scholar]
- Kim YH, Kim KI, Paik NJ, et al. Muscle strength: a better index of low physical performance than muscle mass in older adults. Geriatr Gerontol Int. 2016;16(5):577–585. doi: 10.1111/ggi.12514. [DOI] [PubMed] [Google Scholar]
- Landi F, Cruz-Jentoft AJ, Liperoti R, et al. Sarcopenia and mortality risk in frail older persons aged 80 years and older: results from ilSIRENTE study. Age Ageing. 2013;42(2):203–209. doi: 10.1093/ageing/afs194. [DOI] [PubMed] [Google Scholar]
- Lau EMC, Lynn HSH, Woo J, et al. Prevalence of and risk factors for sarcopenia in elderly Chinese men and women. J Gerontol A Biol Sci Med Sci. 2005;60(2):213–216. doi: 10.1093/gerona/60.2.213. [DOI] [PubMed] [Google Scholar]
- Laurentani F, Russo CR, Bandinelli S, et al. Age-associated changes in skeletal muscles and their effect on mobility: an operational diagnosis of sarcopenia. J Appl Physiol. 2003;95(5):1851–1860. doi: 10.1152/japplphysiol.00246.2003. [DOI] [PubMed] [Google Scholar]
- Lee JS, Auyeung TW, Kwok T, et al. Associated factors and health impact of sarcopenia in older chinese men and women: a cross-sectional study. Gerontology. 2007;53(6):404–410. doi: 10.1159/000107355. [DOI] [PubMed] [Google Scholar]
- Li F. The effects of Tai JiQuan training on limits of stability in older adults. Clin Interv Aging. 2014;9:1261–1268. doi: 10.2147/CIA.S65823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li JX, Xu DQ, Hong Y. Changes in muscle strength, endurance, and reaction of the lower extremities with Tai Chi intervention. J Biomech. 2009;42(8):967–971. doi: 10.1016/j.jbiomech.2009.03.001. [DOI] [PubMed] [Google Scholar]
- Li XF, Zhao KX, Xu LJ, et al. Relationship between skeletal muscle loss and bone mineral density in hospitalized elderly patients. Chin J Osteoporos Bone Miner Dis. 2015;8(1):21–26. [Google Scholar]
- Lund C, Dalgas U, Grønborg TK, et al. Balance and walking performance are improved after resistance and aerobic training in persons with chronic stroke. Disabil Rehabil. 2017;9:1–8. doi: 10.1080/09638288.2017.1336646. [DOI] [PubMed] [Google Scholar]
- Machado A, García-López D, González-Gallego J, Garatachea N. Whole-body vibration training increases muscle strength and mass in older women: a randomized-controlled trial. Scand J Med Sci Sports. 2010;20:200–207. doi: 10.1111/j.1600-0838.2009.00919.x. [DOI] [PubMed] [Google Scholar]
- Manson J, Rotondi M, Jamnik V, et al. Effect of tai chi on musculoskeletal health-related fitness and self-reported physical health changes in low income, multiple ethnicity mid to older adults. BMC Geriatr. 2013;13(1):114–124. doi: 10.1186/1471-2318-13-114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milanese C, Piscitelli F, Simoni C, Pugliarello R, Zancanaro C. Effects of whole-body vibration with or without localized radiofrequency on anthropometry, body composition, and motor performance in young nonobese women. J Altern Complement Med. 2012;18:69–75. doi: 10.1089/acm.2010.0324. [DOI] [PubMed] [Google Scholar]
- Milanese C, Piscitelli F, Zenti MG, et al. Ten-week whole-body vibration training improves body composition and muscle strength in obese women. Int J Med Sci. 2013;10(3):307–311. doi: 10.7150/ijms.5161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moreland JD, Richardson JA, Goldsmith CH, et al. Muscle weakness and falls in older adults: a systematic review and meta-analysis. J Am Geriatr Soc. 2004;52(7):1121–1129. doi: 10.1111/j.1532-5415.2004.52310.x. [DOI] [PubMed] [Google Scholar]
- Morley JE, Baumgartner RN, Roubenoff R, et al. Sarcopenia. J Lab Clin Med. 2001;137(4):231–243. doi: 10.1067/mlc.2001.113504. [DOI] [PubMed] [Google Scholar]
- Nashner LM. Practical biomechanics and physiology of balance. In: Jacobson GP, Newman CW, Kartush JM, editors. Handbook of balance of function test. Clifton Park: Thomson Delmar Learning; 1997. pp. 261–279. [Google Scholar]
- Nomura T, Nagano K, Takato J, et al. The development of a Tai Chi exercise regimen for the prevention of conditions requiring long-term care in Japan. Arch Gerontol Geriatr. 2011;52(3):E198–E203. doi: 10.1016/j.archger.2010.11.010. [DOI] [PubMed] [Google Scholar]
- Pei YC, Chou SW, Lin PS, et al. Eye-hand coordination of elderly people who practice Tai Chi Chuan. J Formos Med Assoc. 2008;107(2):103–110. doi: 10.1016/S0929-6646(08)60123-0. [DOI] [PubMed] [Google Scholar]
- Roelants M, Delecluse C, Verschueren SM. Whole-body-vibration training increases knee-extension strength and speed of movement in older women. J Am Geriatr Soc. 2004;52(6):901–908. doi: 10.1111/j.1532-5415.2004.52256.x. [DOI] [PubMed] [Google Scholar]
- Roelants M, Delecluse C, Goris M, Verschueren S. Effects of 24 weeks of whole body vibration training on body composition and muscle strength in untrained females. Int J Sports Med. 2004;25:1–5. doi: 10.1055/s-2003-45238. [DOI] [PubMed] [Google Scholar]
- Roubenoff R. Sarcopenia: effects on body composition and function. J Gerontol A Biol Sci Med Sci. 2003;58(11):1012–1017. doi: 10.1093/gerona/58.11.M1012. [DOI] [PubMed] [Google Scholar]
- Stark T, Walker B, Phillips JK, et al. Hand-held dynamometry correlation with the gold standard isokinetic dynamometry: a systematic review. PM&R. 2011;3(5):472–479. doi: 10.1016/j.pmrj.2010.10.025. [DOI] [PubMed] [Google Scholar]
- Su Z, Zhao J, Wang N, et al. Effects of weighted Tai Chi on leg strength of older adults. J Am Geriatr Soc. 2015;63(10):2208–2210. doi: 10.1111/jgs.13693. [DOI] [PubMed] [Google Scholar]
- Tanimoto Y, Watanabe M, Sun W, et al. Association between sarcopenia and higher-level functional capacity in daily living in community-dwelling elderly subjects in Japan. Arch Gerontol Geriatr. 2012;55(2):e9–e13. doi: 10.1016/j.archger.2012.06.015. [DOI] [PubMed] [Google Scholar]
- Tanimoto Y, Watanabe M, Sun W, et al. Association between muscle mass and disability in performing instrumental activities of daily living (IADL) in communitydwelling elderly in Japan. Arch Gerontol Geriatr. 2012;54(2):e230–e233. doi: 10.1016/j.archger.2011.06.015. [DOI] [PubMed] [Google Scholar]
- Tankisheva E, Bogaerts A, Boonen S, et al. Effects of a 6-month local vibration training on bone density, muscle strength, muscle mass and physical performance in postmenopausal women. J Strength Cond Res. 2015;29(9):2613–2622. doi: 10.1519/JSC.0000000000000895. [DOI] [PubMed] [Google Scholar]
- Tsuji T, Kitano N, Tsunoda K. Short-term effects of whole-body vibration on functional mobility and flexibility in healthy, older adults: a randomized crossover study. J Geriatr Phys Ther. 2014;37(2):58–64. doi: 10.1519/JPT.0b013e318295dacd. [DOI] [PubMed] [Google Scholar]
- Verschueren S, Gielen E, O’Neil TW, et al. Sarcopenia and its relationship with bone mineral density in middle-aged and elderly European men. Osteoporos Int. 2013;24(1):87–98. doi: 10.1007/s00198-012-2057-z. [DOI] [PubMed] [Google Scholar]
- Xu DQ, Hong Y, Li JX. Tai Chi exercise and muscle strength and endurance in older people. Med Sport Sci. 2008;52:20–29. doi: 10.1159/000134281. [DOI] [PubMed] [Google Scholar]
- Xue QL, Walston JD, Fried LP, et al. Prediction of risk of falling, physical disability, and frailty by rate of decline in grip strength: the women’s health and aging study. Arch Intern Med. 2011;171(12):1119–1121. doi: 10.1001/archinternmed.2011.252. [DOI] [PubMed] [Google Scholar]
- Yang F, King GA, Dillon L, et al. Controlled whole-body vibration training reduces risk of falls among community-dwelling older adults. J Biomech. 2015;48(12):3206–3212. doi: 10.1016/j.jbiomech.2015.06.029. [DOI] [PubMed] [Google Scholar]