Abstract
Public stigma surrounding HIV is related to heightened emotional distress, poor psychological functioning, and reduced subjective well-being in people living with HIV. For men who have sex with men (MSM) living with HIV, they may also face stigmatizing attitudes within the gay community, which create an additional burden to their health. Grounded in the psychological mediation framework, the present study examined the underlying psychological processes through which HIV stigma from the public and within the gay community influences the mental and social health of MSM living with HIV. Findings from 206 Chinese MSM living with HIV in Hong Kong indicated that negative self-concept, maladaptive coping, and peer isolation mediated the effect of HIV stigma on mental and social health. The study revealed the cognitive, regulatory, and interpersonal processes underlying HIV stigma and health. Feeling intense HIV stigma from the public and within the gay community may render MSM living with HIV more vulnerable to negative self-concept, maladaptive coping, and peer isolation, which contribute to poor mental and social health. To combat prejudice and discrimination against people living HIV, stigma reduction initiatives should be implemented not only in the public, but also in the gay community. Cognitive-behavioral interventions can also be used to restructure negative self-beliefs and build adaptive emotion regulation skills, which can improve stigma-related health outcomes among MSM living with HIV.
Keywords: HIV stigma, gay community, MSM living with HIV, mental health, social health
Due to their dual stigmatized identities, men who have sex with men (MSM) living with HIV are often marginalized in society (Dowshen, Binns, & Garofalo, 2009; Tsang et al., 2019). MSM living with HIV not only face stigma arising from their same-sex attraction and behavior, but also encounter rejection and discrimination on the basis of their HIV status (Reilly et al., 2016; Rendina et al., 2016; Smit et al., 2012). Apart from the “double stigma” from the public, earlier studies also documented the stigmatizing attitudes toward people living with HIV (PLHIV) within the gay community (Chong, Mak, Tam, Zhu, & Chung, 2017; Courtenay–Quirk, Wolitski, Parsons, Gomez, & Seropositive Urban Men’s Study Team, 2006). Given that the stigmatization is multisourced, MSM living with HIV are highly vulnerable to negative health outcomes (Hatzenbuehler, O’cleirigh, Mayer, Mimiaga, & Safren, 2011). Although a large body of research has identified the detrimental effects of HIV stigma from the general public on PLHIV, less is known about the HIV stigma that occurs in the gay community and how it affects the health status among MSM living with HIV. The present study simultaneously examined the HIV stigma from the public and within the gay community, and investigated the mechanisms underlying the effects of HIV stigma on the mental and social health of MSM living with HIV.
HIV Stigma Within the Gay Community
Fear and stigma of HIV emerged in the gay community since the early 1980s when HIV was labeled as the “gay plague” and “Gay-Related Immune Deficiency” (Herek & Glunt, 1988). The advent of HIV testing in the mid-1980s further divided the gay community into two groups, that is, people living with HIV and HIV-unknown (Sheon & Crosby, 2004). After three decades, stigmatizing attitudes toward PLHIV are still highly prevalent in the gay community (Goldenberg, Vansia, & Stephenson, 2016). MSM living with HIV encountered experiences of prejudice, avoidance, and discrimination from members of the gay community (Courtenay–Quirk et al., 2006). In a sample of gay men living with HIV, Stutterheim et al. (2008) reported that 66.7% (n = 290) of the respondents have encountered HIV stigma in the gay community, which was even more prevalent than HIV stigma in other contexts (including family, friends, workplace, school, healthcare services, and faith community).
In Hong Kong, a vast majority of the HIV infections was reported in male (84.9% in 2018; n = 530), with same-sex sexual contacts (49.4% in 2018; n = 308) being the major modes of transmission (Virtual AIDS Office Hong Kong, 2019). Although it has been around 35 years since the first diagnosis of HIV infection, HIV stigma continues to be a pervasive problem in Hong Kong society and significantly impacts the life of PLHIV. HIV stigma is manifested as a fear of infection, which cause people to avoid interacting with PLHIV (Mak et al., 2007). It was evidenced in the results of a population-based random household survey that around one-third of the general public respondents in Hong Kong did not want PLHIV living in their neighborhood and would avoid contacting PLHIV (Equal Opportunities Commission, 2010). Over three-fourths of them considered that PLHIV might cause dangers or adverse effects to residents in the vicinity. In addition, a recent study on 100 MSM living with HIV in Hong Kong reported that 60% (n = 60) perceived moderate-to-high levels of HIV stigma within the gay community (Chong et al., 2017). Around 89% (n = 89) indicated that there was discrimination against PLHIV even among MSM (Chong et al., 2017).
Despite that HIV stigma within the gay community was severe and prevalent, its psychosocial consequences on MSM living with HIV have rarely been explored, compared with that of HIV stigma from the general public (Hatzenbuehler et al., 2011). Courtenay–Quirk et al. (2006) identified that HIV stigma within the gay community was related to higher levels of depressive symptoms and suicidal ideation among MSM living with HIV in the United States. Chong et al. (2017) reported that PLHIV in Hong Kong who perceived greater levels of HIV stigma from the gay community were more vulnerable to psychological distress.
In addition to the impact on mental health, HIV stigma within the gay community may also undermine one’s social health, which is defined as the “ability to interact effectively with others and develop satisfying personal relationships to accomplish social roles” (Rezaei, Khalili, & Inalo, 2016). MSM who endorse HIV stigma may avoid contacting MSM living with HIV, which keeps them isolated and marginalized in the gay community (Smit et al., 2012). On the other hand, MSM living with HIV may estrange themselves from other MSM peers and withdraw from social interaction to avoid being stigmatized (Skinta, Brandrett, Schenk, Wells, & Dilley, 2014).
Whereas there was an increasing number of studies documented the adverse effects of HIV stigma within the gay community, only one study has recently explored the mediating mechanisms of how it contributes to poor mental health (Chong et al., 2017). Building upon earlier conceptual models by Berger, Ferrans, and Lashley (2001) and Earnshaw and Chaudoir (2009), Chong et al. (2017) examined the mediating effects of internalized stigma, serostatus disclosure concerns, and negative reactions toward ingroup HIV stigma. The results indicated that only negative emotional reactions explained the association between HIV stigma within the gay community and psychological distress, while the other two mediators were nonsignificant (Chong et al., 2017). Given that the mediating mechanism between HIV stigma within the gay community and health among MSM living with HIV is largely unknown, it presents a significant barrier to developing strategies for addressing stigma and promoting health in the gay community. Thus, the present study was designed to fill in this gap by examining the mediating pathways through which HIV stigma from the public and within the gay community impacts the mental and social health of MSM living with HIV in Hong Kong. A thorough understanding of the relationship between HIV stigma and health among MSM will inform the development of psychosocial interventions and care for this population.
Psychological Mediation Framework
Hatzenbuehler (2009) developed the psychological mediation framework to explain how sexual stigma “gets under the skin” and underpins psychopathology among sexual minority individuals. It postulates that stigma-related stress leads to emotional dysregulation, interpersonal problems, and cognitive processes, which elevate the risk of negative health outcomes in sexual minorities. The framework has been empirically tested and supported in different sexual minority populations (Martin-Storey & Crosnoe, 2012; Schwartz, Stratton, & Hart, 2016; Szymanski, Dunn, & Ikizler, 2014), but has rarely been applied among PLHIV. Grounded in the psychological mediation framework (Hatzenbuehler, 2009), the present study investigated the cognitive, regulatory, and interpersonal mechanisms through which HIV stigma from the public and within the gay community negatively affects mental and social health by examining the mediating roles of negative self-concept, maladaptive coping, and peer isolation respectively in MSM living with HIV. The framework is particularly relevant in light of the dearth of research on understanding how HIV stigma within the gay community renders MSM more prone to poor mental and social health.
Cognitive process
Negative self-concept has been consistently reported among sexual minority populations as an outcome of stigma and discrimination (Skinta et al., 2014). Self-concept refers to the cognitive representation of the individual’s beliefs, attitudes, knowledge, and perceptions about the self (Markus & Wurf, 1987). Previous studies indicated that PLHIV who were affected by stigma were likely to incorporate the societal devaluation into their own personal value system (Lee, Kochman, & Sikkema, 2002). Also, PLHIV are often preoccupied with negative self-concept, which causes them to view themselves in a pessimistic light (Fife & Wright, 2000). They may hold negative beliefs about self as being worthless and incompetent, leading to negative mental health outcomes (Kalichman et al., 2009; Mak et al., 2007). In a sample of sexual minority adolescents, Martin-Storey and Crosnoe (2012) further revealed that those who experienced sexual orientation-based harassment were more likely to report negative self-perception, which predisposed them to depression. Similarly, findings reported that having a negative sense of self might disrupt social functioning in sexual minorities (Crawford, Allison, Zamboni, & Soto, 2002; Yang, Mak, Ho, & Chidgey, 2017).
Regulatory process
Maladaptive coping is one of the common ways to respond to stigmatizing experiences among socially marginalized populations (Ashton et al., 2005). It refers to the adoption of negative and dysfunctional strategies to regulate stress-related emotions (Lazarus, 1999). Given that HIV stigma is highly distressing and overwhelming, PLHIV often use maladaptive coping to orient themselves away from the stressors (Sanjuán, Molero, Fuster, & Nouvilas, 2013). Maladaptive coping was often observed among MSM living with HIV who perceived higher levels of HIV stigma within the gay community (Courtenay–Quirk et al., 2006). Kaysen et al. (2014) reported that sexual minority young women who experienced homophobia tended to employ maladaptive coping strategies, such as denial and self-blame, which were linked to greater levels of psychological distress. Rumination is also another maladaptive strategy frequently used when facing stigma (Szymanski et al., 2014). It is characterized by a passive and repetitive self-focused reflection on one’s negative experience and its possible causes and consequences (Nolen-Hoeksema, Wisco, & Lyubomirsky, 2008). Schwartz et al. (2016) identified that gay and bisexual men who responded to sexual stigma with rumination were more vulnerable to depression and anxiety.
Interpersonal process
Social connection with peers has also been identified as a key protective mechanism in stigmatized populations such as PLHIV and sexual minorities (Li, Lee, Thammawijaya, Jiraphongsa, & Rotheram-Borus, 2009; McConnell, Birkett, & Mustanski, 2015). A large body of research has consistently demonstrated that stigma can cause stigmatized individuals to be isolated from their friends and family (Parker & Aggleton, 2003). It was reported that social isolation significantly mediated the effect of stigma on mental health outcomes among PLHIV (Herek, Saha, & Burack, 2013) as well as gay and bisexual men (Schwartz et al., 2016). Qualitative findings from Reece and Dodge (2004) indicated that establishing a social network with other gay and bisexual men was conducive to better social well-being.
The Present Study
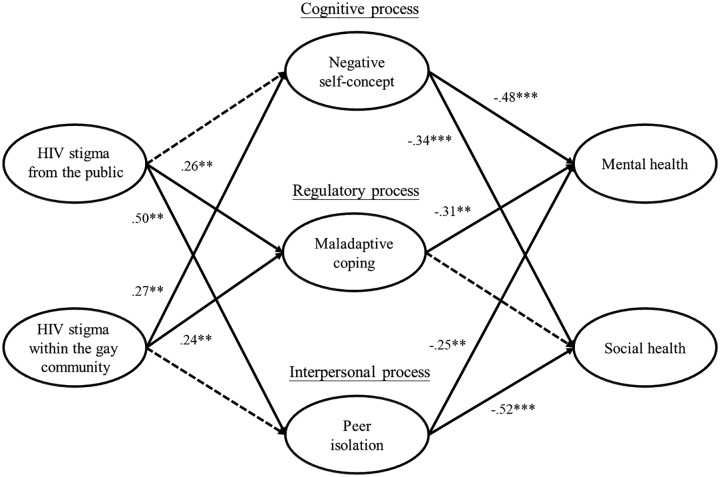
While negative self-concept, maladaptive coping, and peer isolation are considered as psychological mechanisms that explain the effects of stigma on mental health in sexual minorities, their mediating roles have never been empirically tested in MSM living with HIV (Hatzenbuehler, 2009). Bridging the literature on HIV stigma and sexual minority stress, the present study applied the psychological mediation framework to investigate the cognitive, regulatory, and interpersonal processes through which HIV stigma from the public and within the gay community undermines health outcomes among MSM living with HIV in Hong Kong. Specifically, this study proposed and examined a mediation model (see Figure 1) to understand how HIV stigma adversely affects mental and social health among MSM living with HIV. First, it was hypothesized that HIV stigma from the public and within the gay community would be negatively related to mental and social health. Second, it was hypothesized that negative self-concept, maladaptive coping, and peer isolation would mediate the effect of HIV stigma from the public and within the gay community on mental and social health.
Figure 1.
A mediation model of HIV stigma from the public and within the gay community on mental and social health.
Note. Solid lines denote significant paths with standardized coefficients shown, while dotted lines denote nonsignificant paths; * p < .05, ** p < .01, *** p < .001; controlling for age, education, employment status, marital status, sexual orientation, and length of being diagnosed with HIV infection.
Method
Participants
A sample of 206 Chinese men who have sex with men living with HIV participated in the present study. Inclusion criteria include: (1) being at least 18 years of age, (2) being assigned as male at birth, (3) living with HIV (as confirmed by the nurses at the HIV clinic), and (4) having had sex with men in the lifetime. The participants had a mean age of 39.36 years (SD = 10.13, range = 22–68). Majority of the participants were single (77.6%, n = 159) and completed tertiary education (41.2%, n = 85). Over two-thirds were full-time employed (69.4%, n = 143). Most of the participants identified as gay (62.1%, n = 128), followed by bisexual (32.0%, n = 66), heterosexual (2.9%, n = 6), and questioning (2.9%, n = 6). The participants had an average of 4.76 years since HIV diagnosis (SD = 4.41 years, range = 1 month – 20 years). The details of participant demographics are summarized in Table 1.
Table 1.
Demographic Characteristics of the Participants (N = 206).
| Variables | n (%)/Mean (SD) |
|---|---|
| Age | 39.36 (10.13) |
| Education | |
| Junior secondary or below | 9 (4.4%) |
| Senior secondary | 80 (38.8%) |
| Tertiary or above | 117 (56.8%) |
| Marital status | |
| Single | 159 (77.6%) |
| Married/cohabitated | 41 (20.0%) |
| Divorced/separated/widowed | 5 (2.4%) |
| Employment status | |
| Full-time employment | 143 (69.4%) |
| Part-time/temporary employment | 25 (12.2%) |
| Unemployed | 20 (9.7%) |
| Retired | 10 (4.9%) |
| Student | 4 (1.9%) |
| Other | 4 (1.9%) |
| Sexual orientation | |
| Heterosexual | 6 (2.9%) |
| Bisexual | 66 (32.0%) |
| Gay | 128 (62.1%) |
| Questioning | 6 (2.9%) |
| Length of being diagnosed with HIV infection | |
| Less than 1 year | 39 (21.1%) |
| 1–5 years | 72 (38.9%) |
| 5–10 years | 45 (24.3%) |
| More than 10 years | 29 (15.7%) |
Procedure
Participants were recruited and referred by the nurses at the only community-based HIV clinic in Hong Kong. Eligible participants provided written informed consent prior to the commencement of the study. The participants were asked to fill in a self-report questionnaire and received HK$60 (US$ 7.70) as compensation for their time spent. The study procedures and materials were approved by the clinical research ethics committees of the authors’ institution and of the clinic involved in participant recruitment.
Measures
HIV stigma from the public
Three items from Perceived Devaluation-Discrimination Scale (Link, Cullen, Frank, & Wozniak, 1987) were used to assess the extent to which the participants perceive stigmatizing attitudes and behaviors from the public on a 6-point Likert scale from 1 (strongly agree) to 6 (strongly disagree). Sample item includes “If I disclose my HIV status, most people would treat me with a worsened attitude, exclude or reject me.” Higher scores represent higher levels of HIV stigma from the public. The items were translated from English into Chinese and subsequently back-translated into English by two independent bilingual researchers. Discrepancies between the two versions of the items were discussed and resolved to ensure accuracy and equivalency of meaning. The internal consistency (Cronbach’s α) of the measure was .78 in the present study.
HIV stigma within the gay community
Ten items developed by Courtenay–Quirk et al. (2006) and Chong et al. (2017) were used to measure the perception of HIV stigma in the gay community on a 6-point Likert scale from 1 (strongly agree) to 6 (strongly disagree). A sample item includes “HIV-negative MSM treat you differently when they know you’re positive.” Higher scores indicate greater perceptions of HIV stigma in the gay community. The scale has been translated into Chinese and used in MSM living in HIV in Hong Kong (Chong et al., 2017). The internal consistency (Cronbach’s α) of the measure was reported as .90 (Chong et al., 2017). For the present study, the internal consistency of the measure was .84.
Negative self-concept
Two items by Marschall, Sanftner, and Tangney (1994) were used to assess the thoughts and beliefs about the self on a 4-point Likert scale from 1 (not feeling this way at all) to 4 (feeling this way very strongly). The items are “I feel worthwhile, valuable” and “I feel capable, useful.” The items were reversely scored, with higher scores indicating more negative sense of self. The items were translated following the procedure reported above. The internal consistency (Cronbach’s α) of the measure was .70 in the present study.
Maladaptive coping
Three items were adapted from the brief COPE (Carver, 1997) to measure the use of maladaptive coping strategies to deal with the stress associated with HIV infection. Participants rated the items on a 4-point Likert scale from 1 (I’ve not done this at all) to 4 (I’ve been doing this a lot). The items are “I’ve been saying to myself ‘this isn’t real’” (denial), “I’ve been criticizing myself” (self-blame), and “I have been constantly thinking about why I have these sufferings” (rumination). Higher scores indicate more frequent use of maladaptive coping. The items were previously translated into Chinese and examined among PLHIV in China (Su et al., 2015). The internal consistency (Cronbach’s α) of the measure in this study was .78.
Peer isolation
The friend subscale of the Multidimensional Scale of Perceived Social Support (MSPSS) (Zimet, Dahlem, Zimet, & Farley, 1988) consists of four items assessing social support from peers. The items were rated on a 7-point Likert scale from 1 (very strongly disagree) to 7 (very strongly agree). Sample items include “I have friends with whom I can share my joys and sorrows.” The items were reversely coded, with higher scores representing higher levels of peer isolation. The scale has been translated into Chinese and its psychometric properties have been evaluated (Chou, 2000). The internal consistency (Cronbach’s α) of the measure was reported as .85 (Zimet et al., 1988). For the present study, the internal consistency was .91.
Mental health
The 5-item World Health Organization Well-Being Index (WHO-5) (Psychiatric Research Unit, 1998) was used to measure positive mental health. Participants were asked to evaluate the five statements on a 6-point Likert scale from 0 (at no time) to 5 (all of the time). Sample item includes “I have felt active and vigorous.” Higher scores indicate higher levels of mental health. The scale has been translated into Chinese (Psychiatric Research Unit, 2007) and used in previous studies in Hong Kong (Mak, Chio, Chan, Lui, & Wu, 2017). The internal consistency (Cronbach’s α) of the measure was .83 in the present study.
Social health
The social relationships subscale of Satisfaction With Life Scale (SWLS) (Test, Greenberg, Long, Brekke, & Burke, 2005) consists of six items assessing the functioning and satisfaction in the area of social relationships. The items were rated on a 5-point Likert scale from 1 (not at all) to 5 (a great deal). Sample item includes “How satisfied are you with your current social life?” Higher scores reflect higher levels of social health. The scale has been translated into Chinese and used in previous studies (Chan & Mak, 2016). The internal consistency (Cronbach’s α) of the measure was reported as .80 (Test et al., 2005). For the present study, the internal consistency was .79.
Data Analysis
Descriptive statistics were conducted to understand the demographic characteristics of the participants. Pearson correlation coefficients were used to determine the association between the variables of interest. The preliminary analysis was performed with SPSS 22.0.
A two-step approach to structural equation modeling (SEM) was used to examine the hypothesized relationships among the latent variables presented in Figure 1 (Anderson & Gerbing, 1988). A measurement model was examined with confirmatory factor analysis (CFA) to determine whether the factor structure of the variables fits the data. The latent variables of HIV stigma from the public, negative self-concept, maladaptive coping, and peer isolation were indicated by their corresponding items. Three sets of item parcel were created to represent the latent construct of HIV stigma within the gay community, mental health, and social health, based on the recommendations by Russell et al. (1998). It was then followed by the examination of a structural model that tests the relationships between the exogenous and endogenous latent variables in the hypothesized model, controlling for participant demographics (i.e., age, education, employment status, marital status, sexual orientation, and length of being diagnosed with HIV infection). The goodness-of-fit for the models were evaluated using chi-square (χ2) statistics, comparative fit index (CFI), Tucker Lewis Index (TLI), the root mean square error of approximation (RMSEA), and the standardized root mean square residual (SRMR). CFI and TLI values above 0.90 indicate acceptable model fit (Hu & Bentler, 1999). RMSEA and SRMR values of 0.06 or less are considered as a close model fit (Hu & Bentler, 1999). MPlus 7.1 was used to analyze the data.
Results
Preliminary Analyses
The means, standard deviations, and intercorrelations of the variables are described in Table 2. HIV stigma from the public and HIV stigma within the gay community were positively associated with negative self-concept, maladaptive coping, and peer isolation (rs ranged from .17 to .46, ps < .05). HIV stigma from the public and HIV stigma within the gay community were also negatively associated with mental health and social health (rs ranged from −.19 to −36, ps < .01). In addition, mental health and social health were negatively related to negative self-concept, maladaptive coping, and peer isolation (rs ranged from −.28 to −.56, ps < .001).
Table 2.
Descriptive Statistics and Intercorrelations of the Variables (N = 206).
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | |
|---|---|---|---|---|---|---|---|
| 1. HIV stigma from the public | – | ||||||
| 2. HIV stigma within the gay community | .33*** | – | |||||
| 3. Negative self-concept | .17* | .24** | – | ||||
| 4. Maladaptive coping | .24** | .27*** | .25*** | – | |||
| 5. Peer isolation | .46*** | .17* | .24** | .29*** | – | ||
| 6. Mental health | −.33*** | −.19** | −.46*** | −.43*** | −.42*** | – | |
| 7. Social health | −.36*** | −.20** | −.34*** | −.28*** | −.56*** | .61*** | – |
| Range of scale | 1–6 | 1–6 | 1–4 | 1–4 | 1–7 | 0–5 | 1–5 |
| Mean | 3.80 | 4.30 | 2.11 | 1.94 | 2.97 | 2.52 | 3.44 |
| SD | 1.04 | .78 | .77 | .82 | 1.27 | .90 | .62 |
Note. *p < .05; **p < .01; ***p < .001.
Measurement and Structural Models
Results of measurement model showed a good model fit, χ2 (168) = 233.31, p < .001, CFI = .97, TLI =.96, RMSEA = .04, SRMR = .04. All loadings of the items or parcels on their latent constructs (β = .57 – .91) were statistically significant (p < .001). As presented in Figure 1, structural equation modeling was conducted to examine the hypothesized relationship among HIV stigma from the public, HIV stigma within the gay community, negative self-concept, maladaptive coping, peer isolation, mental health, and social health, adjusting for demographics. Results showed a satisfactory model fit χ2 (342) = 502.97, p < .001, CFI = .92, TLI =.91, RMSEA = .05, SRMR = .07. The unstandardized and standardized path loadings for the model are reported in Table 3. The model explained 52.9% and 57.8% of the variance of mental health and social health respectively.
Table 3.
Unstandardized and Standardized Path Loadings for the Hypothesized Model.
| Parameter estimates | Unstandardized |
Standardized |
|---|---|---|
| b (SE) | Β | |
| Direct effect | ||
| HIV stigma from the public → Negative self-concept | .06 (.07) | .09 (.10) |
| HIV stigma from the public → Maladaptive coping | .17 (.07)** | .26 (.09)** |
| HIV stigma from the public → Peer isolation | .49 (.09)*** | .51 (.08)*** |
| HIV stigma from the public → Mental health | −.10 (.10) | −.11 (.10) |
| HIV stigma from the public → Social health | −.08 (.05) | −.15 (.09) |
| HIV stigma within the gay community → Negative self-concept | .26 (.11)* | .27 (.10)** |
| HIV stigma within the gay community → Maladaptive coping | .23 (.09)* | .24 (.09)** |
| HIV stigma within the gay community → Peer isolation | .01 (.12) | .01 (.08) |
| HIV stigma within the gay community → Mental health | .18 (.12) | .13 (.09) |
| HIV stigma within the gay community → Social health | .08 (.06) | .12 (.08) |
| Negative self-concept → Mental health | −.67 (.15)*** | −.48 (.08)*** |
| Negative self-concept → Social health | −.25 (.07)*** | −.34 (.08)*** |
| Maladaptive coping → Mental health | −.44 (.14)** | −.31 (.09)** |
| Maladaptive coping → Social health | −.09 (.07) | −.12 (.09) |
| Peer isolation → Mental health | −.24 (.09)** | −.25 (.09)** |
| Peer isolation → Social health | −.26 (.05)*** | −.52 (.08)*** |
| HIV stigma from the public ↔ HIV stigma within the gay community | .28 (.07)*** | .41 (.07)*** |
| Mental health ↔ Social health | .12 (.03)*** | .60 (.10)*** |
| Indirect effect | ||
| HIV stigma from the public → Mental health | ||
| via Negative self-concept | −.04 (.05) | −.04 (.05) |
| via Maladaptive coping | −.07 (.04)* | −.08 (.04)* |
| via Peer isolation | −.12 (.05)* | −.13 (.05)* |
| HIV stigma from the public → Social health | ||
| via Negative self-concept | −.02 (.02) | −.03 (.04) |
| via Maladaptive coping | −.02 (.01) | −.03 (.03) |
| via Peer isolation | −.13 (.03)*** | −.27 (.06)*** |
| HIV stigma within the gay community → Mental health | ||
| via Negative self-concept | −.17 (.08)* | −.13 (.06)* |
| via Maladaptive coping | −.10 (.05)* | −.08 (.04)* |
| via Peer isolation | −.003 (.03) | −.002 (.02) |
| HIV stigma within the gay community → Social health | ||
| via Negative self-concept | −.06 (.03)* | −.09 (.04)* |
| via Maladaptive coping | −.02 (.02) | −.03 (.02) |
| via Peer isolation | −.003 (.03) | −.004 (.04) |
Note. *p < .05; **p < .01; ***p < .001.
Direct effects
HIV stigma from the public was positively related to maladaptive coping (β = .26, p = .006) and peer isolation (β = .51, p < .001), but not negative self-concept (β = .09, p = .37). HIV stigma within the gay community was positively related to negative self-concept (β = .27, p = .008) and maladaptive coping (β = .24, p = .009), but not peer isolation (β = .01, p = .93). Negative self-concept was associated with poor mental health (β = −.48, p < .001) and social health (β = −.34, p < .001). Maladaptive coping was negatively associated with mental health (β = −.31, p = .001), but not social health (β = −.12, p = .16). Peer isolation was related to lower levels of mental health (β = −.25, p = .005) and social health (β = −.52, p < .001). HIV stigma from the public and HIV stigma within the gay community were not directly related to mental health and social health (ps > .05).
Indirect effects
Results indicated that peer isolation significantly mediated the effect of HIV stigma from the public on mental health (β = −.13, p = .01) and social health (β = −.27, p < .001). Maladaptive coping also mediated the effect of HIV stigma from the public on mental health (β = −.08, p = .03), but not social health (β = −.03, p = .20). Negative self-concept did not significantly mediate the effect of HIV stigma from the public on mental health (β = −.04, p = .37) and social health (β = −.03, p = .38).
In addition, a significant indirect effect was observed for HIV stigma within the gay community on mental health (β = −.13, p = .02) and social health (β = −.09, p = .03) via negative self-concept. Results revealed that maladaptive coping significantly mediated the effect of HIV stigma within the gay community on mental health (β = −.08, p = .045), but not social health (β = −.03, p = .22). Peer isolation did not significantly mediate the effect of HIV stigma within the gay community on mental health (β = −.002, p = .93) and social health (β = −.004, p = .93).
Discussion
The present study applied the psychological mediation framework to understand the relationship between stigma and health among MSM living with HIV. Apart from HIV stigma from the public, this study estimated the effect of HIV stigma within the gay community, which was more prevalent and detrimental to MSM living with HIV than public stigma (Stutterheim et al., 2008). Consistent with earlier studies (Chong et al., 2017; Courtenay–Quirk et al., 2006), this study demonstrated that HIV stigma within the gay community represents a significant risk factor for MSM living with HIV, and showed that the psychological mediation framework is a useful conceptual tool for explaining how stigma influences health outcomes in this population. The findings lend support to the cognitive, regulatory, and interpersonal processes through which HIV stigma within the gay community undermines mental and social health among MSM living with HIV.
Self-concept offers a cognitive explanation for the association of HIV stigma with poor mental and social health. As being MSM is a core aspect of life for many MSM, the HIV stigma within the gay community is particularly impactful to their self-concept (Smit et al., 2012). The current findings indicated that MSM living with HIV who felt greater HIV stigma from the gay community were more vulnerable to a negative sense of self, which made them view themselves as worthless and incapable. Negative self-concept, in turn, contributed to greater psychological distress and lower engagement in fulfilling relationships with others, consistent with the prior findings in sexual minorities (Martin-Storey & Crosnoe, 2012).
Maladaptive coping also constitutes a significant mediating mechanism through which HIV stigma affects mental health. The present results corroborated earlier findings and suggested that MSM living with HIV were likely to adopt maladaptive coping strategies to blunt the negative affective states arising from HIV stigma from the public and within the gay community (Chong et al., 2017; Courtenay–Quirk et al., 2006). While some may deny the distressing experiences and blame themselves for the stigma, others may become trapped in rumination on negative moods and stressors (Sanjuán et al., 2013). These types of coping strategies are not only ineffective in handling the distress, but also involve a continuous expenditure of mental and emotional energy, which evokes an adverse effect on psychological functioning (Szymanski et al., 2014). It is noted that the negative influence of maladaptive coping was only on mental health, but not social health. It might be the fact that MSM living with HIV who adopt maladaptive coping mainly suffer from internal struggles, which do not necessitate an impairment on their social functioning.
Peer isolation, as an outcome of HIV stigma from the public, also contributes to poor mental and social health among MSM living with HIV. The present findings indicated that those who perceived strong stigma from the public were more prone to social isolation. Due to the stigma, it was plausible that MSM living with HIV were rejected by their peers, while at the same time they also restrained themselves from social interaction (Smit et al., 2012). With lower levels of peer support, MSM living with HIV were more likely to experience negative mental health (Herek et al., 2013). On the other hand, as they were less connected to their peers, they were also less likely to build satisfying personal relationships and live a meaningful social life (Reece & Dodge, 2004).
The present study demonstrated that the cognitive, regulatory, and interpersonal processes were distinctive and they jointly operated to produce a synergic effect on MSM living with HIV (Hatzenbuehler, 2009). As supported in the findings, negative self-concept, maladaptive coping, and peer isolation co-occurred as a result of HIV stigma from the public and within the gay community. Instead of serving as independent mechanisms in isolation, the cognitive, regulatory, and interpersonal processes fueled each other to create a mutually reinforcing cluster of risk factors that predisposed MSM living with HIV to poor mental and social health (Dowshen et al., 2009; Hatzenbuehler et al., 2011). It is therefore important to note the synergistic interactions between these psychological processes and recognize how these co-occurring and intertwined processes link stigmatization to adverse health outcomes in MSM living with HIV (Herek et al., 2013; Schwartz et al., 2016). Future research should examine how the cognitive, regulatory, and interpersonal processes interact with each other to produce deleterious effects on MSM living with HIV.
The negative impacts of HIV stigma are particularly prominent in the context of Chinese culture (Li, Lau, Holroyd, & Li, 2016). As the family is the basic unit of social organization in Chinese societies, MSM living with HIV in Hong Kong not only face stigma and discrimination themselves, but may also bring shame and dishonor to their family members because the entire family is stigmatized due to their HIV status (Zang, Guida, Sun, & Liu, 2014). This can create additional strain on familial relationships and weaken the social support system of the MSM living with HIV, which impose psychological burdens on this population (Ho & Mak, 2013). As revealed in the present study, HIV stigma was positively related to maladaptive coping. It is likely because alternative coping mechanisms (e.g., family support) are not available to MSM living with HIV (Li et al., 2006). They may therefore resort to maladaptive coping strategies in response to the stress and negative emotion resulting from HIV stigma, which in turn may compromise their mental health (Sanjuán et al., 2013).
Apart from the strong emphasis on family ties and responsibility, it is also widely recognized that Chinese culture places a high value on collectivism (Zang et al., 2014). Acceptance and support from the community one belongs to is particularly crucial for Chinese people. Since sexual identity is an important facet of self-definition, HIV stigma within the gay community can be detrimental to the mental and social health of MSM living with HIV (Lee et al., 2002; Smit et al., 2012). For those who encountered stigma from the gay community, they were more likely to hold negative beliefs and perceptions toward themselves, which were associated with poor mental and social health. As the results were obtained from a Chinese sample, future studies should replicate the present findings and examine the applicability of the model in individualistic cultures.
Implications
Findings from this study have important implications on intervention strategies for promoting mental and social health among MSM living with HIV. Given the adverse effects of HIV stigma within the gay community, community-level interventions are necessary to address prejudice and stigma toward PLHIV not only in the public, but also in the gay community. It is important to facilitate the awareness of biases among MSM and challenge deeply entrenched stereotypes about PLHIV (Szymanski et al., 2014). By educating MSM about HIV/AIDS knowledge, it can reduce their irrational fear of contagion and mitigate negative judgments about PLHIV (Mak, Mo, Ma, & Lam, 2017). Stigma reduction efforts of this kind are not only likely to bring health benefits to MSM living with HIV, but also crucial for HIV prevention in the gay community (Mahajan et al., 2008).
As the present study revealed the cognitive and regulatory processes underlying the relationship between HIV stigma and health among MSM living with HIV, cognitive-behavioral interventions targeting negative self-concept and maladaptive coping strategies may be helpful for this population (Crepaz et al., 2008). Therapeutic approaches such as cognitive restructuring and self-affirmation can be implemented to change their negative thought patterns (Pachankis, 2014). Developing adaptive emotion regulation skills can enable them to effectively cope with stigmatizing experiences. In addition, recent research indicates that mindfulness and self-compassion interventions can be used to cultivate a nonjudgmental and accepting attitude toward self and negative experiences, which may mitigate rumination and self-blame, and thereby alleviate mental distress (Yang & Mak, 2017).
As informed by the findings, strengthening social support systems in the face of HIV stigma can also foster better psychosocial functioning. This can be achieved through the use of MSM peer support groups. Earlier studies indicated that support groups for PLHIV not only improve quality of life, but also enhance their medication adherence and increase retention in HIV care (Bateganya, Amanyeiwe, Roxo, & Dong, 2015). By engaging in support groups, it provides an opportunity for PLHIV to share their experiences and develop social bonds with peers, which can serve as a source of emotional support. The positive outcomes can even be maximized if the support groups are organized around specific identities such as gay men (World Health Organization, 2016).
Limitations
A few limitations should be noted when interpreting the findings from this study. First, the cross-sectional nature of the study limits the establishment of causal relationships between the variables. Although the hypothesized mediation model was grounded in the theoretical work of Hatzenbuehler (2009) and earlier empirical findings (Kaysen et al., 2014), future studies should address this limitation by adopting a prospective longitudinal research design. Second, since a sampling frame of MSM living with HIV does not exist, the present study relied on a nonprobability sample, which may restrict the generalizability of the findings. Third, this study focused on HIV stigma from the public and within the gay community and did not account for the stigma surrounding sexuality. Further works should build on the current study to estimate the relative contribution of HIV stigma and sexual stigma on the health of MSM living with HIV.
Conclusions
Notwithstanding these limitations, the present study shed important insights on how HIV stigma within the gay community, in tandem with HIV stigma from the public, triggers a cascade of interrelated cognitive, regulatory, and interpersonal processes conferring risk for poor mental and social health among MSM living with HIV in Hong Kong. Findings indicated that HIV stigma was positively related to negative self-concept, maladaptive coping, and peer isolation, which in turn contributed to negative health outcomes among MSM living with HIV. Given that MSM comprise a growing proportion of PLHIV population across the globe, more intervention research is needed to understand and address their mental and social health needs.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was funded by the Direct Grant of the Chinese University of Hong Kong (Ref. No.: 2021091).
ORCID iD: Winnie W. S. Mak  https://orcid.org/0000-0002-9714-7847
https://orcid.org/0000-0002-9714-7847
References
- Anderson J. C., Gerbing D. W. (1988). Structural equation modeling in practice: A review and recommended two-step approach. Psychological Bulletin, 103(3), 411–423. [Google Scholar]
- Ashton E., Vosvick M., Chesney M., Gore-Felton C., Koopman C., O’shea K., . . . Flamm J. (2005). Social support and maladaptive coping as predictors of the change in physical health symptoms among persons living with HIV/AIDS. AIDS Patient Care & STDs, 19(9), 587–598. [DOI] [PubMed] [Google Scholar]
- Bateganya M., Amanyeiwe U., Roxo U., Dong M. (2015). The impact of support groups for people living with HIV on clinical outcomes: A systematic review of the literature. Journal of Acquired Immune Deficiency Syndromes, 68(3), S368–S374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berger B. E., Ferrans C. E., Lashley F. R. (2001). Measuring stigma in people with HIV: Psychometric assessment of the HIV stigma scale. Research in Nursing & Health, 24(6), 518–529. [DOI] [PubMed] [Google Scholar]
- Carver C. S. (1997). You want to measure coping but your protocol’s too long: Consider the brief cope. International Journal of Behavioral Medicine, 4(1), 92–100. [DOI] [PubMed] [Google Scholar]
- Chan R. C. H., Mak W. W. S. (2016). Common sense model of mental illness: Understanding the impact of cognitive and emotional representations of mental illness on recovery through the mediation of self-stigma. Psychiatry Research, 246, 16–24. [DOI] [PubMed] [Google Scholar]
- Chong E. S. K., Mak W. W. S., Tam T. C. Y., Zhu C., Chung R. W. Y. (2017). Impact of perceived HIV stigma within men who have sex with men community on mental health of seropositive MSM. AIDS Care, 29(1), 118–124. [DOI] [PubMed] [Google Scholar]
- Chou K.-L. (2000). Assessing Chinese adolescents’ social support: The multidimensional scale of perceived social support. Personality and Individual Differences, 28(2), 299–307. [Google Scholar]
- Courtenay–Quirk C., Wolitski R. J., Parsons J. T., Gomez C. A., & Seropositive Urban Men’s Study Team. (2006). Is HIV/AIDS stigma dividing the gay community? Perceptions of HIV–positive men who have sex with men. AIDS Education & Prevention, 18(1), 56–67. [DOI] [PubMed] [Google Scholar]
- Crawford I., Allison K. W., Zamboni B. D., Soto T. (2002). The influence of dual-identity development on the psychosocial functioning of African-American gay and bisexual men. Journal of Sex Research, 39(3), 179–189. [DOI] [PubMed] [Google Scholar]
- Crepaz N., Passin W. F., Herbst J. H., Rama S. M., Malow R. M., Purcell D. W., Wolitski R. J. (2008). Meta-analysis of cognitive-behavioral interventions on HIV-positive persons’ mental health and immune functioning. Health Psychology, 27(1), 4–14. [DOI] [PubMed] [Google Scholar]
- Dowshen N., Binns H. J., Garofalo R. (2009). Experiences of HIV-related stigma among young men who have sex with men. AIDS Patient Care and STDS, 23(5), 371–376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Earnshaw V. A., Chaudoir S. R. (2009). From conceptualizing to measuring HIV stigma: A review of HIV stigma mechanism measures. AIDS and Behavior, 13(6), 1160–1177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Equal Opportunities Commission. (2010). Baseline survey on public attitudes towards persons with a disability 2010. Retrieved from http://www.eoc.org.hk/EOC/Upload/UserFiles/File/ResearchReport/201109/DisabilityReport(eng).pdf
- Fife B. L., Wright E. R. (2000). The dimensionality of stigma: A comparison of its impact on the self of persons with HIV/AIDS and cancer. Journal of Health and Social Behavior, 41(1), 50–67. [PubMed] [Google Scholar]
- Goldenberg T., Vansia D., Stephenson R. (2016). Intragroup stigma among men who have sex with men: Data extraction from Craigslist ads in 11 cities in the United States. JMIR Public Health and Surveillance, 2(1), e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler M. L. (2009). How does sexual minority stigma “get under the skin”? A psychological mediation framework. Psychological Bulletin, 135(5), 707–730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler M. L., O’cleirigh C., Mayer K. H., Mimiaga M. J., Safren S. A. (2011). Prospective associations between HIV-related stigma, transmission risk behaviors, and adverse mental health outcomes in men who have sex with men. Annals of Behavioral Medicine, 42(2), 227–234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herek G. M., Glunt E. K. (1988). An epidemic of stigma: Public reactions to AIDS. American Psychologist, 43(11), 886–891. [DOI] [PubMed] [Google Scholar]
- Herek G. M., Saha S., Burack J. (2013). Stigma and psychological distress in people with HIV/AIDS. Basic and Applied Social Psychology, 35(1), 41–54. [Google Scholar]
- Ho C. Y. Y., Mak W. W. S. (2013). HIV-related stigma across cultures: Adding family into the equation. In Liamputtong P. (Ed.), Stigma, discrimination and living with HIV/AIDS (pp. 53–69). New York, NY: Springer. [Google Scholar]
- Hu L. T., Bentler P. M. (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal, 6(1), 1–55. [Google Scholar]
- Kalichman S. C., Simbayi L. C., Cloete A., Mthembu P. P., Mkhonta R. N., Ginindza T. (2009). Measuring AIDS stigmas in people living with HIV/AIDS: The internalized AIDS-related stigma scale. AIDS Care, 21(1), 87–93. [DOI] [PubMed] [Google Scholar]
- Kaysen D. L., Kulesza M., Balsam K. F., Rhew I. C., Blayney J. A., Lehavot K., Hughes T. L. (2014). Coping as a mediator of internalized homophobia and psychological distress among young adult sexual minority women. Psychology of Sexual Orientation and Gender Diversity, 1(3), 225–233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazarus R. S. (1999). Stress and emotion: A new synthesis. London: Springer Publishing Company. [Google Scholar]
- Lee R. S., Kochman A., Sikkema K. J. (2002). Internalized stigma among people living with HIV-AIDS. AIDS and Behavior, 6(4), 309–319. [Google Scholar]
- Li H., Lau J. T., Holroyd E., Li X. (2016). Mental health problems and associated socio-ecological factors among HIV-positive young migrant men who have sex with men in China. In Liamputtong P. (Ed.), Children and young people living with HIV/AIDS (pp. 223–239). New York, NY: Springer. [Google Scholar]
- Li L., Lee S.-J., Thammawijaya P., Jiraphongsa C., Rotheram-Borus M. J. (2009). Stigma, social support, and depression among people living with HIV in Thailand. AIDS Care, 21(8), 1007–1013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li L., Wu S., Wu Z., Sun S., Cui H., Jia M. (2006). Understanding family support for people living with HIV/AIDS in Yunnan, China. AIDS and Behavior, 10(5), 509–517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Link B. G., Cullen F. T., Frank J., Wozniak J. F. (1987). The social rejection of former mental patients: Understanding why labels matter. American Journal of Sociology, 92(6), 1461–1500. [Google Scholar]
- Mahajan A. P., Sayles J. N., Patel V. A., Remien R. H., Ortiz D., Szekeres G., Coates T. J. (2008). Stigma in the HIV/AIDS epidemic: A review of the literature and recommendations for the way forward. AIDS, 22(Suppl 2), S67–S69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mak W. W. S., Cheung R. Y. M., Law R. W., Woo J., Li P. C. K., Chung R. W. Y. (2007). Examining attribution model of self-stigma on social support and psychological well-being among people with HIV+/AIDS. Social Science & Medicine, 64(8), 1549–1559. [DOI] [PubMed] [Google Scholar]
- Mak W. W. S., Chio F. H. N., Chan A. T. Y., Lui W. W. S., Wu E. K. Y. (2017). The efficacy of internet-based mindfulness training and cognitive-behavioral training with telephone support in the enhancement of mental health among college students and young working adults: Randomized controlled trial. Journal of Medical Internet Research, 19(3), e84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mak W. W. S., Mo P. K. H., Ma G. Y. M., Lam M. Y. Y. (2017). Meta-analysis and systematic review of studies on the effectiveness of HIV stigma reduction programs. Social Science & Medicine, 188, 30–40. [DOI] [PubMed] [Google Scholar]
- Markus H., Wurf E. (1987). The dynamic self-concept: A social psychological perspective. Annual Review of Psychology, 38(1), 299–337. [Google Scholar]
- Marschall D., Sanftner J., Tangney J. P. (1994). The State Shame and Guilt Scale. Fairfax, VA: George Mason University. [Google Scholar]
- Martin-Storey A., Crosnoe R. (2012). Sexual minority status, peer harassment, and adolescent depression. Journal of Adolescence, 35(4), 1001–1011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McConnell E. A., Birkett M. A., Mustanski B. (2015). Typologies of social support and associations with mental health outcomes among LGBT youth. LGBT Health, 2(1), 55–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nolen-Hoeksema S., Wisco B. E., Lyubomirsky S. (2008). Rethinking rumination. Perspectives on Psychological Science, 3(5), 400–424. [DOI] [PubMed] [Google Scholar]
- Pachankis J. E. (2014). Uncovering clinical principles and techniques to address minority stress, mental health, and related health risks among gay and bisexual men. Clinical Psychology: Science and Practice, 21(4), 313–330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parker R., Aggleton P. (2003). HIV and AIDS-related stigma and discrimination: A conceptual framework and implications for action. Social Science & Medicine, 57(1), 13–24. [DOI] [PubMed] [Google Scholar]
- Psychiatric Research Unit. (1998). WHO (Five) Well-Being Index. Hillerød, Denmark: WHO Collaborating Center for Mental Health, Frederiksborg General Hospital. [Google Scholar]
- Psychiatric Research Unit (2007). Interpretation of the items of the WHO-five well-being index (WHO-5) questionnaire. Retrieved from https://www.psykiatri-regionh.dk/who-5/Documents/WHO5_Chinese_PR.pdf
- Reece M., Dodge B. (2004). Exploring the physical, mental and social well-being of gay and bisexual men who cruise for sex on a college campus. Journal of Homosexuality, 46(1–2), 111–136. [DOI] [PubMed] [Google Scholar]
- Reilly K. H., Neaigus A., Jenness S. M., Wendel T., Marshall D. M., IV, Hagan H. (2016). Experiences of discrimination and HIV risk among men who have sex with men in New York City. American Journal of Men’s Health, 10(6), 505–514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rendina H. J., Gamarel K. E., Pachankis J. E., Ventuneac A., Grov C., Parsons J. T. (2016). Extending the minority stress model to incorporate HIV-positive gay and bisexual men’s experiences: A longitudinal examination of mental health and sexual risk behavior. Annals of Behavioral Medicine, 51(2), 147–158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rezaei S., Khalili M. R., Inalo A. B. (2016). The effect of emotional intelligence on the personality traits and social health of women in district 12 of Tehran. International Journal of Humanities and Cultural Studies (IJHCS) ISSN 2356-5926, 3(1), 1761–1773. [Google Scholar]
- Russell D. W., Kahn J. H., Spoth R., Altmaier E. M. (1998). Analyzing data from experimental studies: A latent variable structural equation modeling approach. Journal of Counseling Psychology, 45(1), 18–29. [Google Scholar]
- Sanjuán P., Molero F., Fuster M. J., Nouvilas E. (2013). Coping with HIV related stigma and well-being. Journal of Happiness Studies, 14(2), 709–722. [Google Scholar]
- Schwartz D. R., Stratton N., Hart T. A. (2016). Minority stress and mental and sexual health: Examining the psychological mediation framework among gay and bisexual men. Psychology of Sexual Orientation and Gender Diversity, 3(3), 313–324. [Google Scholar]
- Sheon N., Crosby G. M. (2004). Ambivalent tales of HIV disclosure in San Francisco. Social Science & Medicine, 58(11), 2105–2118. [DOI] [PubMed] [Google Scholar]
- Skinta M. D., Brandrett B. D., Schenk W. C., Wells G., Dilley J. W. (2014). Shame, self-acceptance and disclosure in the lives of gay men living with HIV: An interpretative phenomenological analysis approach. Psychology & Health, 29(5), 583–597. [DOI] [PubMed] [Google Scholar]
- Smit P. J., Brady M., Carter M., Fernandes R., Lamore L., Meulbroek M., . . . Rockstroh J. K. (2012). HIV-related stigma within communities of gay men: A literature review. AIDS Care, 24(4), 405–412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stutterheim S. E., Bos A. E., Schaalma H. P. (2008). HIV-related stigma in the Netherlands. Maastricht: AIDS Fonds & Maastricht University. [Google Scholar]
- Su X. Y., Lau J. T. F., Mak W. W. S., Choi K., Feng T.-J., Chen X., . . . Cheng J. (2015). A preliminary validation of the Brief COPE instrument for assessing coping strategies among people living with HIV in China. Infectious Diseases of Poverty, 4, 41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szymanski D. M., Dunn T. L., Ikizler A. S. (2014). Multiple minority stressors and psychological distress among sexual minority women: The roles of rumination and maladaptive coping. Psychology of Sexual Orientation and Gender Diversity, 1(4), 412–421. [Google Scholar]
- Test M. A., Greenberg J. S., Long J. D., Brekke J. S., Burke S. S. (2005). Construct validity of a measure of subjective satisfaction with life of adults with serious mental illness. Psychiatric Services, 56(3), 292–300. [DOI] [PubMed] [Google Scholar]
- Tsang E. Y.-H., Qiao S., Wilkinson J. S., Fung A. L.-C., Lipeleke F., Li X. (2019). Multilayered stigma and vulnerabilities for HIV infection and transmission: A qualitative study on male sex workers in zimbabwe. American Journal of Men’s Health, 13(1), 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Virtual AIDS Office Hong Kong, Department of Health, The Government of the Hong Kong Special Administrative Region. (2019). HIV surveillance and epidemiology. Retrieved from http://www.info.gov.hk/aids/english/surveillance/latest_stat.htm
- World Health Organization (2016). Consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection: Recommendations for a public health approach. Geneva, Switzerland: World Health Organization. [PubMed] [Google Scholar]
- Yang X., Mak W. W. S. (2017). The differential moderating roles of self-compassion and mindfulness in self-stigma and well-being among people living with mental illness or HIV. Mindfulness, 8(3), 595–602. [Google Scholar]
- Yang X., Mak W. W. S., Ho C. Y. Y., Chidgey A. (2017). Self-in-love versus self-in-stigma: Implications of relationship quality and love attitudes on self-stigma and mental health among HIV-positive men having sex with men. AIDS Care, 29(1), 132–136. [DOI] [PubMed] [Google Scholar]
- Zang C., Guida J., Sun Y., Liu H. (2014). Collectivism culture, HIV stigma and social network support in Anhui, China: A path analytic model. AIDS Patient Care and STDS, 28(8), 452–458. [DOI] [PubMed] [Google Scholar]
- Zimet G. D., Dahlem N. W., Zimet S. G., Farley G. K. (1988). The multidimensional scale of perceived social support. Journal of Personality Assessment, 52(1), 30–41. [DOI] [PubMed] [Google Scholar]