Introduction
Cutaneous lupus erythematosus (LE) is subdivided into acute, subacute, and chronic forms, each with distinct morphologies. Chronic cutaneous lupus erythematosus (CCLE) most commonly presents in the form of discoid lupus erythematosus (DLE) with pink-to-violaceous coin-shaped plaques with hyperkeratosis and follicular plugging that heal with atrophy, scarring, hyperpigmentation, and telangiectasias. Lesions most commonly occur on the face, ears, scalp, and in sun-exposed areas. On hair-bearing skin, DLE results in cicatricial alopecia.
Although the lesions of DLE are often quite distinct, more than 20 other rare clinical variants of CCLE, such as hypertrophic LE and verrucous LE, have been described that can mimic other dermatologic conditions.1 In 1972, one such variant consisting of acneiform lesions was introduced by Haroon and Fleming.2 This variant, although exceedingly rare, is perhaps one of the most critical to recognize, as it can easily be mistaken for one of the most common diseases seen by dermatologists and general practitioners. Here we present a case of comedonal CCLE that was previously misdiagnosed and treated as acne vulgaris.
Case report
A 57-year-old postmenopausal African-American woman presented to our clinic with recalcitrant acne on the face for 1 year and hair loss for 6 months. The patient's acne did not respond to treatment with topical clindamycin, tretinoin and benzoyl peroxide, and oral doxycycline. Her hair loss was resistant to treatment with clobetasol. She took no other medications. She denied joint pain, oral ulcerations, or photosensitivity. A physical examination found brown papulonodules and cystic acneiform lesions on the bilateral upper neck, cheeks, chin, and forehead (Figs 1 and 2) and purple/brown papules and plaques in the bilateral conchal bowls with follicular plugging (Fig 3). The latter morphologically resembled lesions of DLE. Her scalp examination was significant for nonscarring alopecia of the frontotemporal scalp along with discrete circular patches of scarring alopecia of the parietal scalp.
Fig 1.
Comedonal CCLE on the cheek, chin, and jawline depicted by cystic pink and tan acneiform papules and pustules.
Fig 2.
Higher-powered view of acneiform papules and pustules on the left cheek.
Fig 3.
Left conchal bowl with purple/brown comedonal papules with follicular plugging.
Biopsy of the left conchal bowl showed a follicular infundibular cyst with a lymphocyte-mediated interface dermatitis involving the interfollicular epidermis and the hair follicle. An accompanying moderately dense perivascular lymphocytic infiltrate was also present. A biopsy of the right side of the upper neck found dermal fibrosis consistent with a cicatrix with chronic inflammation and hemosiderin deposition. A third biopsy of the left parietal scalp found mild fibrosing lymphocytic folliculitis with an attendant reduction in terminal hair density. Because of the strong suspicion of discoid LE, a myxovirus protein stain, the surrogate type I interferon marker, was conducted and was strikingly positive in epithelial structures, the endothelium, and amidst inflammatory cells in all specimens. Overall the findings were interpreted as discoid LE manifesting an unusual hyperkeratotic acneiform diathesis compatible with comedomal CCLE (Figs 4 and 5). Despite an antinuclear antibody of 1:80 with speckled pattern, systemic involvement was deemed unlikely given a negative review of systems, negative double-stranded DNA, and normal basic laboratory panels. Although the patient started taking hydroxychloroquine, 200 mg daily, she was lost to follow-up, precluding further laboratory workup, direct immunofluorescence, or monitoring for response to therapy.
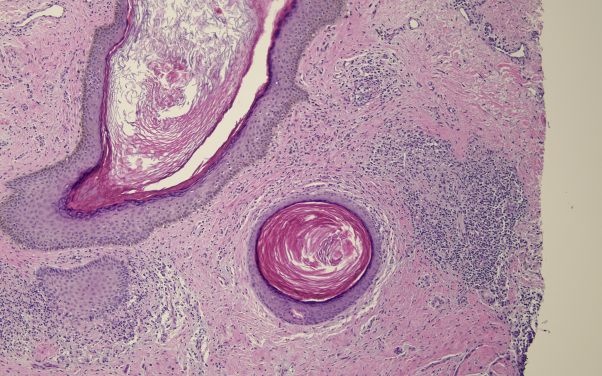
Fig 4.
Low-power image shows comedonal dilation of the follicle; however, there is a supervening lymphocyte-mediated interface dermatitis affecting the outer root sheath epithelium.
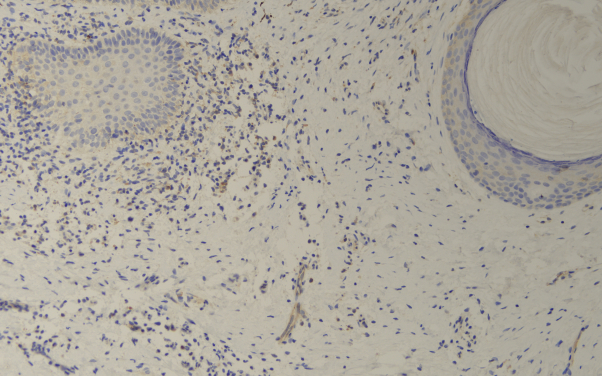
Fig 5.
The myxovirus protein stain is a surrogate type I interferon marker that is significantly upregulated in this tissue sample. Normally, the signal for myxovirus protein staining is negative. In this photomicrograph there is a mildly upregulated signal in the follicular epithelium, inflammatory cells, and endothelium.
Discussion
Comedonal CCLE is an especially rare but documented variant of cutaneous LE. A review of the English-language literature finds only 8 previous cases (Table I).2, 3, 4, 5, 6, 7, 8 An analysis of the reported cases in Table I is helpful in characterizing the distinctive features that define this apparently rare variant of CCLE. First, it predominates in young women (78% of reported cases occurred in women, 86% of whom were in their third or fourth decade of life). Akin to DLE, this subtype of CCLE also tends to favor the face, ears, scalp, and sun-exposed areas. The mean time to diagnosis among reported cases is 3.7 years, reflecting the diagnostic challenge posed by its resemblance to acne vulgaris. Pruritus appears to be a significant symptom in many previously reported cases.8 Two of 9 cases reported concomitant systemic involvement. Regarding treatment, antimalarials such as hydroxychloroquine and chloroquine have the best-reported efficacy, perhaps in combination with intralesional steroids and manual extraction for resistant cases.6 Notably, as with our patient, typical acne treatments do not appear to be effective in the treatment of comedonal CCLE. Like many subtypes of CCLE, the pathogenesis behind this acneiform variant is not well elucidated. Because DLE can demonstrate a Koebner response, perhaps an isomorphic DLE response in a lesion that is otherwise characteristic for acne vulgaris is possible.3 Others have suggested that acneiform lesions result from the destructive process of mononuclear cell infiltration of the pilosebaceous units.4 Intrinsic to the pathology of both DLE and acne vulgaris is follicular hyperkeratosis. In this regard, it would not be surprising that on occasion an exaggeration of the follicular hyperkeratosis intrinsic to DLE could translate clinically and histologically into a comedonal process. Finally, there is already substantial precedent regarding other T-cell lymphocyte–rich reactions that can result in a follicular cystic pattern of hyperkeratosis resembling a comedone such as the striking comedonal lesions seen in follicular mycosis fungoides.9 It has been shown that a critical event that presages ductal hypercornification in the setting of acne vulgaris is one of follicular epithelial hyperplasia stimulated by T cells primarily of the CD4 subset.10 The role of T cells in the pathogenesis of acne is also reflected by the association of acne with T-cell–rich autoinflammatory and autoimmune T-cell disorders such as pyoderma gangrenosum and inflammatory bowel disease.
Table I.
Summary of reported cases of comedonal lupus in the English-language literature
| Case | Age/sex | Time to diagnosis (y) | Sites of acneiform lesions | DIF | Concurrent SLE | Antinuclear antibody | Treatments | Follow-up |
|---|---|---|---|---|---|---|---|---|
| Haroon and Fleming2 | 28/F | 6 | Upper arms, shoulders, back | Positive | No | Negative | — | — |
| Motel et al3 | 29/F | 7 | Face, upper trunk | Negative | Yes | Positive (1:2560) homogenous | Tetracycline, erythromycin | No improvement |
| Motel et al3 | 24/F | — | Face, neck | IgG in nucleoli of focal keratinocytes | Yes | Positive (1:5120) nucleolar | Erythromycin 250 mg QID | No improvement |
| Chang et al4 | 32/M | 3 | Right nasolabial fold | IgG + C3 along BMZ | No | Negative | — | — |
| Stavrakoglou et al5 | 38/M | 7 | Face, chest, back | Negative | No | Negative |
|
|
| Hemmati et al6 | 33/F | 1.5 | Scalp | — | No | — |
|
|
| Farias et al7 | 35/F | 2 | Face, ear | — | No | — |
|
|
| Vieira et al8 | 32/F | 2 | Face | IgM along BMZ and upper dermal vessels | No | Negative | Prednisone 40 mg × 1 mo then tapered over 4 mo + chloroquine, 250 mg daily | Significant improvement at 3 mo, no new lesions at 4 ys |
| Current case | 57/F | 1 | Face, ears, neck | — | No | Positive (1:80) speckled | Topical clindamycin, tretinoin, benzoyl peroxide, oral doxycycline | No improvement |
BID, Twice daily; BMZ, basement membrane zone; DIF, direct immunofluorescence; ILTAC, intralesional triamcinolone; SLE, systemic lupus erythematosus; QID, 4 times daily.
This case lends credence to a slowly growing body of literature supporting the existence of this subtype of CCLE, and it highlights the importance of considering comedonal CCLE in patients with apparently ordinary acne vulgaris not responding to conventional treatment. The scarring nature of CCLE, its preference for cosmetically sensitive areas, and the resultant significant potential morbidity associated with a delay in its diagnosis underscore the importance of diagnostic recognition of CCLE clinically and pathologically.
Footnotes
Funding sources: None.
Conflicts of interest: None disclosed.
References
- 1.Pramatarov K.D. Chronic cutaneous lupus erythematosus—clinical spectrum. Clin Dermatol. 2004;22(2):113–120. doi: 10.1016/j.clindermatol.2003.12.016. [DOI] [PubMed] [Google Scholar]
- 2.Haroon T.S., Fleming K.A. An unusual presentation of discoid lupus erythematosus. Br J Dermatol. 1972;87(6):642–645. doi: 10.1111/j.1365-2133.1972.tb07456.x. [DOI] [PubMed] [Google Scholar]
- 3.Motel P.J., Bernstein E.F., Fazio M., Humeniuk H., Kauh Y.C. Systemic lupus erythematosus in patients diagnosed with treatment-resistant acne. Int J Dermatol. 1995;34(5):338–340. doi: 10.1111/j.1365-4362.1995.tb03615.x. [DOI] [PubMed] [Google Scholar]
- 4.Chang Y.H., Wang S.H., Chi C.C. Discoid lupus erythematosus presenting as acneiform pitting scars. Int J Dermatol. 2006;45(8):944–945. doi: 10.1111/j.1365-4632.2006.02899.x. [DOI] [PubMed] [Google Scholar]
- 5.Stavrakoglou A., Hughes J., Coutts I. A case of discoid lupus erythematosus masquerading as acne. Acta Derm Venereol. 2008;88(2):175–176. doi: 10.2340/00015555-0349. [DOI] [PubMed] [Google Scholar]
- 6.Hemmati I., Otberg N., Martinka M., Alzolibani A., Restrepo I., Shapiro J. Discoid lupus erythematosus presenting with cysts, comedones, and cicatricial alopecia on the scalp. J Am Acad Dermatol. 2009;60(6):1070–1072. doi: 10.1016/j.jaad.2008.11.882. [DOI] [PubMed] [Google Scholar]
- 7.Farias D.F., Gondim R.M., Redighieri I.P., Muller H., Petri V. Comedonic lupus: a rare presentation of discoid lupus erythematosus. An Bras Dermatol. 2011;86(4 Suppl 1):S89–S91. doi: 10.1590/s0365-05962011000700023. [DOI] [PubMed] [Google Scholar]
- 8.Vieira M.L., Marques E., Leda Y.L.A., Noriega L.F., Bet D.L., Pereira G. Chronic cutaneous lupus erythematosus presenting as atypical acneiform and comedonal plaque: case report and literature review. Lupus. 2018;27(5):853–857. doi: 10.1177/0961203317726377. [DOI] [PubMed] [Google Scholar]
- 9.Wilkinson J.D., Black M.M., Chu A. Follicular mucinosis associated with mycosis fungoides presenting with gross cystic changes on the face. Clin Exp Dermatol. 1982;7(3):333–339. doi: 10.1111/j.1365-2230.1982.tb02436.x. [DOI] [PubMed] [Google Scholar]
- 10.Jeremy A.H., Holland D.B., Roberts S.G., Thomson K.F., Cunliffe W.J. Inflammatory events are involved in acne lesion initiation. J Invest Dermatol. 2003;121(1):20–27. doi: 10.1046/j.1523-1747.2003.12321.x. [DOI] [PubMed] [Google Scholar]