Abstract
According to GLOBOCAN 2018 data, gallbladder cancer (GBC) accounts for 1.2% of all global cancer diagnoses, but 1.7% of all cancer deaths. Only 1 in 5 GBC cases in the United States is diagnosed at an early stage, and median survival for advanced stage cancer is no more than about a year. The incidence of the disease is increasing in the developed world. Gallstones, biliary cysts, carcinogen exposure, typhoid, and Helicobacter pylori infection, and abnormal pancreaticobiliary duct junctions are all risk factors, many of which account for its geographical, ethnic and sex distribution. Genetics also plays a strong role, as about a quarter of GBC cases are considered familial, and certain ethnicities, such as Native Americans, are at far higher risk for the neoplasm. Prevention includes weight loss, vaccination against and treatment of bacterial infections, early detection and elimination of polyps and cysts, and avoidance of oral estrogen replacement therapy.
Keywords: risk factor, survival, incidence, etiology, mortality
Introduction
While the gallbladder is no more than an inch (2 cm) wide, cancers of the gallbladder account for about 165,000 cancer deaths annually, which is 1.7% of all global cancer deaths [1, 2]. The gallbladder is a small, pear-shaped organ tucked under the liver. Like the liver, it is found behind the right, lower ribs. Its function is to store and concentrate the bile produced by the liver before releasing it into the small intestine, where the bile aids in digestion. Bile from the gallbladder travels to the small intestine via the cystic duct, which joins with the hepatic duct (from the liver) to form the common bile duct. The common bile duct, in turn, joins with the pancreatic duct (which carries enzymes necessary for digestion) to empty into the duodenum at the ampulla of Vater [1]. The gallbladder is considered non-essential, and many lead healthy lives after having their gallbladder removed [1].
Cancers of the gallbladder are nearly all adenocarcinomas, which arise from the secretory cells. The gallbladder is the most common primary cancer site among the biliary tracts. A rare form of gallbladder adenocarcinoma is papillary adenocarcinoma, which arises from papillary cells that help to promote the motility of bile in the gallbladder. While rare, papillary cancers typically have a better prognosis than other gallbladder carcinomas [3].
According to GLOBOCAN 2018 data, gallbladder cancer is the 22nd most incident but 17th most deadly cancer worldwide [2]. Gallbladder cancer is disproportionately deadly because it is rarely found before it has advanced or metastasized. In fact, in the United States (US), only about 1 in 5 gallbladder cancers are diagnosed in the early stages [4]. A better understanding of the etiology and risk factors for the disease will allow patients to make modifications to prevent the disease, and clinicians to target and diagnose populations at high risk of the deadly carcinoma.
Epidemiology
Incidence
In 2018, about 219,000 people were estimated to have been diagnosed with gallbladder cancer. This constitutes 1.2% of all cancer diagnoses [2].
Gallbladder cancer is the only digestive system cancer that is more common among women than men. In 2018, the estimated incidence was 97,000 for men and 122,000 for women. One factor behind the disparity is women’s tendency to live longer. However, the age-standardized incidence rate of gallbladder cancer for women, at 2.4 (per 100,000), is still higher than that for men, at 2.2. The cumulative risk of gallbladder cancer, from birth to age 74, is 0.26% for women and 0.25% for men [2].
The incidence in the US is lower than that around the world, with a rate of 1.4 per 100,000 among women and 0.8 among men. The disparity between men and women is also greater in the US than around the world. The incidence rate in the US was highest among American Indians and Alaskan Native people (3.2/100,000), likely due to limited access to healthcare, as well as differences in genetics, diet, and lifestyle. Geographically, cancer incidence was highest in the Northeast and Midwest US Census regions [5]. Incidence rates are highest in Eastern Europe, East Asia and Latin America (Fig. 1) [6, 7].
Fig. 1.
Map showing estimated age-standardized incidence rates (ASR) in 2018 for gallbladder cancer, both sexes, all ages. Created with mapchart.net. Data obtained from Globocan 2018 [7]
Countries with the top five highest age-standardized incidence rates per 100,000 for males in 2018 are Bolivia (12.8), Thailand (9.0), Republic of Korea (8.4), Chile (6.6) and Nepal (6.0). Countries with the top five highest age-standardized incidence rates per 100,000 for females in 2018 are Bolivia (15.1), Chile (11.7), Bangladesh (7.3), Nepal (7.3) and Peru (6.0) [7]. The geographic differences in incidence are likely attributable to differences in environmental exposures to various chemicals, genetic predisposition and regional intrinsic risk factors that predispose to carcinogenesis [8].
Mortality
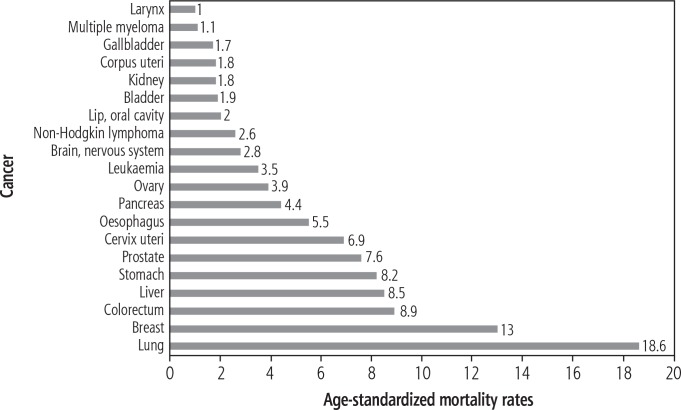
Gallbladder cancer is among the minority of cancers that present with a greater proportion of cancer mortality than incidence. While the incidence accounts for 1.2% of all cancer diagnoses, gallbladder cancer mortality accounts for 1.7% of all cancer deaths. Estimated age-standardized mortality rates (per 100,000) of other gastrointestinal cancers are colorectum (8.9), liver (8.5), stomach (8.2), esophagus (5.5) and pancreas (4.4) (Fig. 2) [2, 7]. About 165,000 people died of gallbladder cancer in 2018. Of them, about 70,000 were male and 95,000 were females. The gender disparity is about on par with the disparity in incidence. The age-standardized mortality was 1.6/100,000 for men and 1.8 for women. The cumulative risk of dying from gallbladder cancer stands at 0.17% for men and 0.19% for women [2].
Fig. 2.
Bar chart showing the estimated age-standardized cancer mortality rates (world) in 2018, worldwide, both sexes, all ages (reproduced from http://globocan.iarc.fr/ [7])
About 2000 people die annually in the US from gallbladder cancer. This constitutes a rate of 0.7/100,000 among women and 0.5/100,000 among men, which is 2-3 times lower than the global average (and more disparate when it comes to gender). In fact, in the US two thirds of gallbladder cancer cases and deaths occurred among women. As with incidence, mortality in the US was highest among Americans Indians and Alaskan Native people and in the Northeast and Midwest regions [5].
Around the world, gallbladder cancer age standardized mortality rates for both sexes (per 100,000) were highest in Central and Eastern Europe (Slovakia 3.2, Hungary 2.5, Poland 2.2), Eastern Asia (Republic of Korea 4.1, Japan 3.3, Cambodia 2.6), and Latin America (Bolivia 10.6, Chile 5.4, Peru 3.1). Bolivia had the highest mortality rate (Fig. 3) [2, 7]. A few countries, including Japan and South Korea, showed greater mortality among men than women, though this was a strong deviation from the norm of a female to male ratio between 1.1 and 2.6 [6].
Fig. 3.
Map showing estimated age-standardized mortality rates (ASR) in 2018 for gallbladder cancer, both sexes, all ages. Created with mapchart.net. Data obtained from Globocan 2018 [7]
Countries with the top five highest age-standardized mortality rates per 100,000 for males in 2018 are Bolivia (9.6), Thailand (7.8), Republic of Korea (5.0), Chile (4.3) and Japan (4.2). Countries with the top five highest age-standardized mortality rates per 100,000 for females in 2018 are Bolivia (11.5), Chile (6.4), Bangladesh (5.0), Thailand (5.7) and Nepal (4.9) [7].
Trends
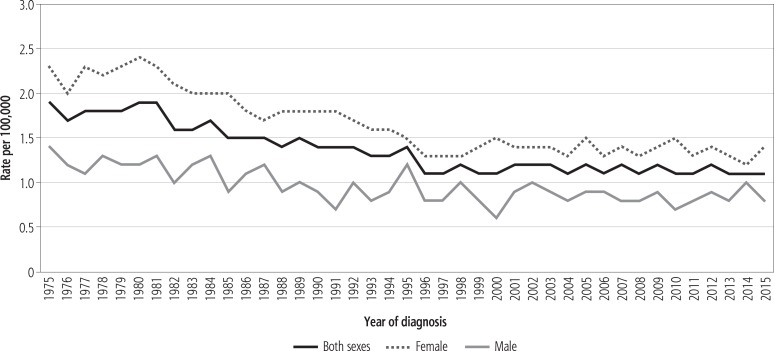
In the US gallbladder cancer incidence has decreased over the past decades among all racial and ethnic groups except non-Hispanic blacks [9]. Among this group, the incidence rate increased by 2.2% annually. Among US women, incidence rates decreased about 0.5% annually, while incidence has remained about stable for men (Fig. 4) [5, 9].
Fig. 4.
Trends in gallbladder cancer incidence (1975-2015) rates by sex, US [9]
Of all the histologies, only the rate of mucinous adenocarcinoma has significantly decreased in the US since 1999. However, in 1999, mucinous adenocarcinoma was the most common gallbladder adenocarcinoma, with an incidence of over 0.05/100,000, and today it has dropped to about 0.03/100,000 in the US. Papillary adenocarcinoma is now the most common, with an incidence rate of around 0.04 [5].
Gallbladder cancer mortality has decreased significantly over the past several decades in women in 80% of countries and men in more than 50% of countries. However, since the 2000s, this decrease has stalled or even reversed in many countries. While obesity has been considered the primary cause of the reversal, a case study in Greece demonstrated that the recent increase in gallbladder cancer mortality could not be fully explained by an increase in the prevalence of obesity [6].
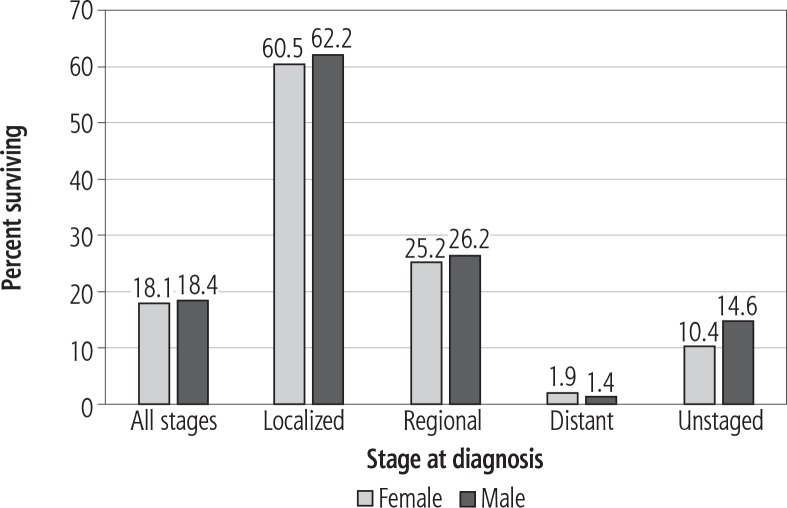
Survival
Gallbladder cancer has historically had a poor prognosis due to its late diagnosis. In the US, 43% of gallbladder cancers were found after cancer had spread to regional organs or lymph nodes, while 42% were found after spreading to distant organs or lymph nodes [5]. The median survival in the US is 12-14 months for patients undergoing resection, and six months for patients treated with palliative stenting [10].
The average 5-year survival rate in the US for gallbladder cancer is 18%. For those with stage I cancer, where the cancer is confined to the gallbladder, the 5-year survival rate is 60% [9]. These rates apply to only the 1 out of 5 cases that are diagnosed prior to cancer metastasis. For those whose cancer has spread to nearby lymph nodes, the survival rate is 25%, while for those with distant metastases, the 5-year survival rate is below 2% (Fig. 5) [9, 11]. While the proportion of distant/regional metastasized diagnoses had been decreasing for decades, it has recently increased, in line with the recent spikes in incidence and mortality in the developed world [6].
Fig. 5.
Gallbladder cancer 5-year SEER relative survival rates, 2008-2014 by sex and stage at diagnosis [9]
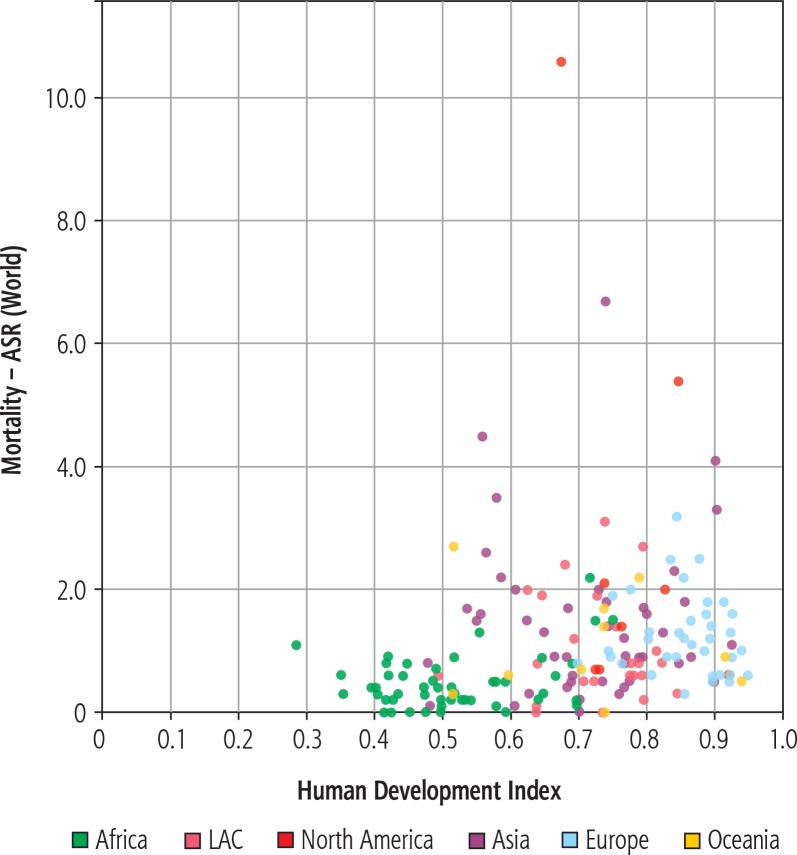
Unlike most cancers, gallbladder carcinoma mortality does not show a negative association with the human development index (HDI). In fact, nations with higher HDI tend to suffer from greater mortality rates (Fig. 6) [2, 7].
Fig. 6.
Mortality – age-standardized rates (world) vs. Human Development Index, gallbladder, in 2018, both sexes, all ages (reproduced from http://globocan.iarc.fr/ [7])
Etiology and risk factors
As with all cancers, gallbladder adenocarcinoma is often preceded by chronic inflammation in the gallbladder that disrupts normal cell signaling and growth. The accumulation of gallstones, known as cholelithiasis, often precedes gallbladder cancer by about 20 years, resulting in chronic inflammation. However, recent increases in gallbladder cancer prevalence among those below 45 call into question gallstones as the only driver of gallbladder cancer. Other major etiological factors for gallbladder cancer include age, obesity, genetics, occupational exposure to mutagens and chronic infection (Table 1).
Table 1.
Risk factors for gallbladder cancer (adapted with permission from [23])
| Risk factor | Relative risk | Reference |
|---|---|---|
| Gallstones | 3.01-23.8 | [28-31] |
| Size of gallstones (cm) | ||
| 2.0-2.9 | 2.4 | [32,34] |
| > 3.0 | 9.2-10.1 | |
| Duration of gallstones (years) | ||
| 5-19 | 4.9 | [37] |
| > 20 | 6.2 | |
| Body mass index | Males Females | |
| 30.0-34.9 | 1.8 2.1 | [71] |
| Infections | ||
| Chronic typhoid and paratyphoid carriers | 12.7-167 | [51, 52] |
| Helicobacter bilis | 2.6-6.5 | [48, 50] |
Age and sex
Gallbladder cancer rates become more common with age, likely because the malignancy takes decades to develop. The average age of diagnosis in the US is 72. Gallbladder cancer is common after the age of 60 years [1]. The Surveillance, Epidemiology, and End Results (SEER) database from the US from 2015 reveals that age-adjusted incidence rates (per 100,000) in 2015 rose from 0.2 for those aged 20-49 years, to 1.6 for those aged 50-64 years, to 4.3 for those aged 65-74 years, and to 8.1 for individuals aged 75 years and older. This corresponded with mortality rates (per 100,000), which increased from 0.1 for those aged 20-49 years, to 0.7 for those aged 50-64 years and to 2.1 for those aged 65-74 years. The highest mortality rate was 4.9/100,000, for individuals aged 75 years and older [9].
Gallbladder cancer is more common in females than males [12]. Women are two to six times more commonly affected than men [13]. The female hormone estrogen is known to increase the saturation of cholesterol in bile, thus increasing the risk of gallstone formation. This pathogenesis is believed to be the primary culprit behind the greater risk of gallbladder cancer among females [14].
Genetics and family history
A family history of gallbladder cancer can increase a person’s risk of developing gallbladder cancer [15, 16]. Reports regarding the familial risk of gallbladder cancer have been contradictory. Familial clustering of gallbladder cancer has been noted in some studies [15]. A Swedish study showed that the standardized incidence ratio (SIR) for gallbladder cancer in offspring of parents diagnosed with gallbladder cancer was 2.47 [17]. But results from the Biliary Tract Cancers Pooling Project recently did not show any association between family history of cancer and gallbladder cancer [18]. Multiple genetic mutations have been implicated among gallbladder cancer cases, including KRAS, P16, c-erb-B2, and TP53. Most are common oncogenes or tumor suppressor genes implicated in many cancers; hence, it is not clear which are driving mutations unique to gallbladder cancer. Certain mutations are associated with other cancer risk factors; for instance, gallbladder cancer in those with an anomalous pancreaticobiliary duct junction frequently presents with KRAS mutations and relatively late onset of p53 mutations, while in patients with cholelithiasis and chronic cholecystitis, KRAS mutations are rare and p53 mutations arise early [19-21].
Gallstones
A history of gallstones carries the highest risk for gallbladder cancer, with the relative risk (RR) being 4.9 [22]. About 85% of people who develop gallbladder cancer have cholelithiasis; however, this statistic may be inflated because those undergoing treatment for gallstones are more likely to be diagnosed with gallbladder cancer [23]. While gallstones are strongly associated with gallbladder cancer etiology, their role as a cause of cancer remains uncertain [24]. The common theory is that chronic irritation due to gallstones and local production of carcinogens such as secondary bile acids leads to sequential development of metaplasia/hyperplasia, dysplasia and finally carcinoma [25].
The overall incidence of gallbladder cancer in patients with gallstones was found to be 0.5% in a Swedish study recently [26]. The RR of developing gallbladder cancer in patients with gallstones ranges between 3 and 24 [27-31]. Increasing size of the gallstones is associated with increased risk for gallbladder cancer. RR of gallbladder cancer with gallstone diameters of 2.0 to 2.9 cm (vs. stone size less than 1 cm) is 2.4; for stones 3 cm or larger, the risk increases to 10.1 [32-34]. In gallbladder cancer patients cholesterol stones seem to be more common than pigment stones [35]. A high incidence of gallbladder carcinoma is seen in American Indians, who have quite a high prevalence of cholesterol gallstones [23]. High rates of gallbladder cancer incidence and gallstone prevalence are also seen in Pima Indian females, Chilean Mapuche Indian females, East Indian females and New Zealand Maori [36].
As the duration of gallstones increases the RR of gallbladder cancer increases, with RR being 4.9 for gallstones with duration of 5-19 years and RR of 6.2 for duration > 20 years [37]. In a large cohort study of 396,720 patients conducted in South Korea, the multivariable-adjusted hazard ratios for gallbladder cancer mortality comparing those with gallstones and without gallstones was 7.35 (95% confidence interval [CI] 2.60-20.8) [38]. This study showed that gallstones were significantly associated with an increased risk of gallbladder cancer and subsequent mortality.
Gallbladder calcification, also known as porcelain gallbladder due to its appearance on X-ray imaging, is a condition caused by excessive gallstones. It is especially common in middle-aged, overweight females. While porcelain gallbladder has historically been associated with gallbladder cancer (prior studies suggested sufferers of the disorder had a cancer incidence of over 60%), recent research has indicated a much lower concomitant incidence of below 6% [39]. In a study by Khan et al. the incidence of gallbladder carcinoma in porcelain gallbladder patients was found to be as low as 2% to 3% [40].
Gallbladder polyps
Polyps in the gallbladder have the potential to grow and become cancerous over many decades. It remains uncertain how many ultimately progress and become cancerous. Among ten studies, 1% to 23% of polyps displayed growth in the follow-up period. Malignancy is significantly more common among polyps more than 10 mm long [41]. There is currently no official recommendation regarding the follow-up schedule for asymptomatic polyps less than 10 mm in length, although studies suggest they do have the capacity to become cancerous [42].
Cholecystectomy should be strongly considered in patients with gallbladder polyps 10 mm in size or greater. Ultrasound imaging should be performed in patients with polyps less than 10 mm in size for at least 2 years until stability is documented, or if growth is documented, then the cholecystectomy option should be discussed with the patient [43].
Primary sclerosis cholangitis
Primary sclerosis cholangitis (PSC) is believed to be an autoimmune disease in which the bile ducts inside and outside the liver are attacked by the body’s immune system, leading to inflammation, scarring, and ultimate blockage. Certain genetic loci have been identified to predispose to the condition. Those with a first-degree relative with PSC have a 9- to 39-fold greater risk of developing the disease [44].
The build-up of bile and the inflammation can lead to gallbladder carcinogenesis. PSC is a relatively rare disorder, estimated to occur in somewhere between 6 and 16 per 100,000 people, with a male predominance. Those with PSC are at a higher risk of gallstones and inflammatory bowel disorder, which can independently predispose an individual to gallbladder cancer [44]. In a study of 286 patients with PSC, 6% were found to have gallbladder mass lesions, of which 56% were found to be gallbladder carcinoma [45]. Cholecystectomy is recommended in these patients regardless of the size of the mass lesion. Routine annual ultrasound screening of the gallbladder can be helpful in these patients [45, 46].
Chronic infection
Chronic infection by Salmonella (e.g., S. typhi and S. paratyphi) or Helicobacter (H. pylori and H. bilis) has been associated with gallbladder cancer [47-52]. More than 75% of patients with gallbladder cancer test positive for the stomach bacterium H. pylori in their bile. It is believed that the bacterium may similarly promote inflammation in the liver and bile ducts, thus increasing the odds of gallbladder carcinogenesis. In a study in Egypt, patients with chronic cholecystitis who had H. pylori in their gallbladder mucosa had 28% metaplasia of gallbladder mucosa compared to patients who did not have H. pylori [53]. H. bilis also has been implicated in gallbladder cancer [48, 49].
Salmonella enterica serovar Typhi, the bacterium behind typhoid fever, has likewise been associated with gallbladder cancer. One study found that those with the presence of antibodies for typhoid had a 4.6-fold increased risk of gallbladder cancer. Latin American countries such as Bolivia and Chile, where typhoid fever is endemic, also have the highest rates of gallbladder cancer around the world [54].
Congenital biliary cysts
Congenital biliary cysts are especially prevalent in women and in Asian populations, both of which are groups at an increased risk of gallbladder cancer. While most cases are surgically resolved in infancy, about 20% of cases are recognized in adults. Biliary cysts are usually identified via ultrasound, computed tomography (CT) scan or magnetic resonance imaging (MRI), and are usually removed surgically via Roux-Y hepaticojejunostomy. Studies suggest that biliary tract cancer, of which gallbladder cancer is the most common, occurs in 2.5-28% of those with biliary cysts. Reports indicate that gallbladder cancer can occur even if an infant has undergone radical biliary cyst removal [55].
Anomalous pancreaticobiliary duct junction
An anomalous junction of the pancreaticobiliary duct is a congenital malformation in which the pancreatic duct drains into the biliary tract outside the duodenal wall. An anomalous pancreatic and bile duct junction can impact the degree of pancreatic fluid regurgitation, thus increasing the risk of biliary tract malignancy. Gallbladder cancers associated with abnormal pancreaticobiliary junction occur at a younger age, have a lower incidence of associated cholelithiasis and show less female gender bias [56]. Among 29 patients treated with biliary tract cancers whose pancreaticobiliary junctions were visualized, 45% presented with an abnormal junction. In the USA, the anatomy of the pancreaticobiliary junction is rarely identified on cholangiopancreatograms. Prospective identification of this risk factor may help clinicians diagnose gallbladder cancer at an earlier stage [57]. An abnormal pancreaticobiliary junction is particularly common in the Asian population and may explain the increased burden of the disease in East Asia [58].
Medications
Post-menopausal women undergoing oral estrogen or estrogen-progesterone therapy are at increased risk of gallstones and gallbladder cancer [59], although the association between oral contraceptives and gallbladder cancer is unclear [33]. Further studies have suggested that transdermal estrogen replacement therapy presents with a lower risk for gallbladder diseases than oral therapy [60]. Since oral estrogen is ingested, it likely finds its way into the liver and bile in greater concentration than transdermal applications. Methyldopa and isoniazid have been implicated in biliary carcinogenesis [61, 62].
Carcinogens
Toxic substances that are ingested are often filtered by the liver and excreted into the bile, where they come into contact with the lining of the gallbladder. Workers in rubber plants or textile factories, or those exposed to nitrosamines, are at an increased risk of gallbladder cancer [1]. Those living in the Gangetic belt in India, an industrial region with a high load of pollutants, have a nearly 10-fold increased risk of developing gallbladder cancer relative to the average in the country [63]. Cigarette smoking has also been associated with the neoplasm [64-66]. A meta-analysis by Bagnardi et al. of 8 studies showed that heavy drinking (> 50 γ of alcohol/day) was associated with a RR of 2.64 for gallbladder cancer [67]. Aflatoxin exposure has also been associated with an increased risk of gallbladder cancer [27].
Obesity
Obese people, those with a body mass index (BMI) > 30 kg/m2, have an increased risk of developing gallbladder cancer [23, 68-70]. Overweight and obese individuals have a 1.15 and 1.66 RR, respectively, of developing gallbladder cancer. Potential biological mechanisms for the association include an increased concentration of hormones such as estrogen or insulin, which increases the formation of gallstones. The association is stronger among women than men, perhaps because women already have a higher level of estrogen in the circulation [71]. A meta-analysis of 15 studies with 5902 cases showed that the risk increased by 4% for each 1 kg/m2 increase in BMI above 25 kg/m2 [72]. In another meta-analysis of 20 studies it was found that compared with nondiabetics, diabetic individuals had 1.56 times increased risk of gallbladder cancer [73].
Prevention
While gallbladder cancer does have a heritable component, research indicates that about 75% of cases are acquired, and thus could be largely preventable [19]. Some of the primary risk factors, including obesity, carcinogen exposure, and estrogen therapy, are within an individual’s power to control. Those postmenopausal women undergoing estrogen therapy can reduce their risk by up to 33% by switching from oral to transdermal therapy [60].
Higher rates of obesity and physical inactivity in the developed world appear correlated with the growing gallbladder cancer incidence. The prevalence of obesity in the US has more than doubled, from 15% in 1979 to 35% in 2014 [74]. As many as 70% of Americans today are overweight or obese. However, in many developed countries, this proportion has stopped growing and is even beginning to decline. The proportion of US adults who met physical activity guidelines increased from 41% in 2006 to 50% in 2012 [75]. Further education on the benefits of healthy eating and exercise can have a serious impact in curbing gallbladder cancer.
Typhoid and H. pylori infection is endemic to parts of Latin America and Asia, where gallbladder cancer is especially incident. Typhoid is preventable via an oral or injectable vaccine, while both bacteria can be treated and resolved within weeks with antibiotics [55]. Better hygiene and sanitation can also prevent the spread of these bacteria, as evidenced by their eradication in the developed world [76].
Early detection can likewise prove life-saving when it comes to gallbladder cancer. Those with a history of gallstones or gallbladder polyps can practice secondary prevention by undergoing regular imaging of the gallbladder, biliary ducts, and pancreaticobiliary junction. Gallbladder polyps, especially those larger than 10 mm, ought to be removed. Those with hereditary biliary cysts should seek surgical removal upon diagnosis, especially in infancy, as this can lessen (though not eliminate) the risk of developing gallbladder cancer later in life.
Conclusions
While the gallbladder is a small organ unessential for life, adenocarcinoma of the gallbladder is a deadly and often untreatable cancer. Gallbladder cancers often do not go diagnosed until advanced stages, when virtually nothing can be done to extend life expectancy beyond several months. Only 1 in 5 gallbladder cancers in the US are diagnosed in early stages, and the median survival for those with advanced cases undergoing resection is only 12-14 months. Gallbladder cancers are especially prevalent in Latin America, Eastern Europe, and East Asia, and in almost all countries, are more prevalent among women than men. The greatest risk factors include gallstones, which form in women more often due to high estrogen levels, and an abnormal pancreaticobiliary junction, which is more common in Asian populations. Over a quarter of gallbladder cancers are considered familial, and many oncogenes and tumor suppressor genes have been linked to gallbladder cancer development. However, prevention is possible, and necessary to decrease global mortality rates. Many crucial risk factors for the neoplasm are behavioral or environmental, including obesity, exposure to carcinogens and estrogen replacement therapy. Typhoid and H. pylori infection, which are the likely culprits behind the heightened risk in Latin America, are preventable with vaccination and treatable with antibiotics. Gallbladder cancer prevention can also take the form of earlier detection via imaging technologies, or surgical removal of polyps and cysts.
Disclosure
Authors report no conflict of interest.
Piśmiennictwo
- 1.Abou-Alfa GK, Jarnagin W, Lowery M, et al. In: Abeloff’s Clinical Oncology – Liver and Bile Duct Cancer. 5th. Niederhuber JE, Armitage JO, Doroshow JH, et al., editors. Philadelphia: Sanders; 2014. pp. 1373–1396. [Google Scholar]
- 2.Bray F, Ferlay J, Soerjomataram I, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394–424. doi: 10.3322/caac.21492. [DOI] [PubMed] [Google Scholar]
- 3.Nuzzo G, Clemente G, Cadeddu F, et al. Papillary carcinoma of the gallbladder and anomalous pancreatico-biliary junction. Report of three cases and review of the literature. Hepatogastroenterology. 2005;52:1034–1038. [PubMed] [Google Scholar]
- 4.Howlader N, Noone AM, Krapcho M, et al., editors. SEER Cancer Statistics Review. Bethesda, MD: National Cancer Institute; 1975-2014. Available from: https://seer.cancer.gov/csr/1975_2014/. Accessed 20 December 2018. [Google Scholar]
- 5.Henley SJ, Weir HK, Jim MA, et al. Gallbladder cancer incidence and mortality, United States 1999-2011. Cancer Epidemiol Biomarkers Prev. 2015;24:1319–1326. doi: 10.1158/1055-9965.EPI-15-0199. [DOI] [PubMed] [Google Scholar]
- 6.Torre LA, Siegel RL, Islami F, et al. Worldwide burden of and trends in mortality from gallbladder and other biliary tract cancers. Clin Gastroenterol Hepatol. 2018;16:427–437. doi: 10.1016/j.cgh.2017.08.017. [DOI] [PubMed] [Google Scholar]
- 7.Ferlay J, Ervik M, Lam F, et al. Global cancer observatory: cancer today. Lyon, France: International Agency for Research on Cancer; Available from: https://gco.iarc.fr/today. Accessed 20 December 2018. [Google Scholar]
- 8.Lazcano-Ponce EC, Miquel JF, Munoz N, et al. Epidemiology and molecular pathology of gallbladder cancer. CA Cancer J Clin. 2001;51:349–364. doi: 10.3322/canjclin.51.6.349. [DOI] [PubMed] [Google Scholar]
- 9.SEER*Explorer: An interactive website for SEER cancer statistics [Internet] Surveillance Research Program, National Cancer Institute; Available from https://seer.cancer.gov/explorer/. Accessed December 20 2018. [Google Scholar]
- 10.Misra SP, Dwivedi M. Pancreaticobiliary ductal union. Gut. 1990;31:1144–1149. doi: 10.1136/gut.31.10.1144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.American Cancer Society . Cancer Facts & Figures 2018. Atlanta, Ga: American Cancer Society; 2018. Available from https://www.cancer.org/cancer/gallbladder-cancer/about/key-statistics.html. Accessed December 02 2018. [Google Scholar]
- 12.Konstantinidis IT, Deshpande V, Genevay M, et al. Trends in presentation and survival for gallbladder cancer during a period of more than 4 decades: a single-institution experience. Arch Surg. 2009;144:441–447. doi: 10.1001/archsurg.2009.46. discussion 447. [DOI] [PubMed] [Google Scholar]
- 13.Duffy A, Capanu M, Abou-Alfa GK, et al. Gallbladder cancer (GBC): 10-year experience at Memorial Sloan-Kettering Cancer Centre (MSKCC) J Surg Oncol. 2008;98:485–489. doi: 10.1002/jso.21141. [DOI] [PubMed] [Google Scholar]
- 14.Everson GT, McKinley C, Kern F., Jr Mechanisms of gallstone formation in women. Effects of exogenous estrogen (Premarin) and dietary cholesterol on hepatic lipid metabolism. J Clin Invest. 1991;87:237–246. doi: 10.1172/JCI114977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hemminki K, Li X. Familial liver and gall bladder cancer: a nationwide epidemiological study from Sweden. Gut. 2003;52:592–596. doi: 10.1136/gut.52.4.592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Goldgar DE, Easton DF, Cannon-Albright LA, et al. Systematic population-based assessment of cancer risk in first-degree relatives of cancer probands. J Natl Cancer Inst. 1994;86:1600–1608. doi: 10.1093/jnci/86.21.1600. [DOI] [PubMed] [Google Scholar]
- 17.Hemminki K, Hemminki A, Forsti A, et al. Genetics of gallbladder cancer. Lancet Oncol. 2017;18:e296. doi: 10.1016/S1470-2045(17)30324-8. [DOI] [PubMed] [Google Scholar]
- 18.Van Dyke AL, Langhamer MS, Zhu B, et al. Family history of cancer and risk of biliary tract cancers: results from the biliary tract cancers pooling project. Cancer Epidemiol Biomarkers Prev. 2018;27:348–351. doi: 10.1158/1055-9965.EPI-17-1003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Matsumoto T, Seno H. Updated trends in gallbladder and other biliary tract cancers worldwide. Clin Gastroenterol Hepatol. 2018;16:339–340. doi: 10.1016/j.cgh.2017.11.034. [DOI] [PubMed] [Google Scholar]
- 20.Wistuba II, Sugio K, Hung J, et al. Allele-specific mutations involved in the pathogenesis of endemic gallbladder carcinoma in Chile. Cancer Res. 1995;55:2511–2515. [PubMed] [Google Scholar]
- 21.Wistuba II, Gazdar AF, Roa I, et al. p53 protein overexpression in gallbladder carcinoma and its precursor lesions: an immunohistochemical study. Hum Pathol. 1996;27:360–365. doi: 10.1016/s0046-8177(96)90109-4. [DOI] [PubMed] [Google Scholar]
- 22.Randi G, Franceschi S, La Vecchia C. Gallbladder cancer worldwide: geographical distribution and risk factors. Int J Cancer. 2006;118:1591–1602. doi: 10.1002/ijc.21683. [DOI] [PubMed] [Google Scholar]
- 23.Stinton LM, Shaffer EA. Epidemiology of gallbladder disease: cholelithiasis and cancer. Gut Liver. 2012;6:172–187. doi: 10.5009/gnl.2012.6.2.172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shrikhande SV, Barreto SG, Singh S, et al. Cholelithiasis in gallbladder cancer: coincidence, cofactor, or cause! Eur J Surg Oncol. 2010;36:514–519. doi: 10.1016/j.ejso.2010.05.002. [DOI] [PubMed] [Google Scholar]
- 25.Jain K, Mohapatra T, Das P, et al. Sequential occurrence of preneoplastic lesions and accumulation of loss of heterozygosity in patients with gallbladder stones suggest causal association with gallbladder cancer. Ann Surg. 2014;260:1073–1080. doi: 10.1097/SLA.0000000000000495. [DOI] [PubMed] [Google Scholar]
- 26.Muszynska C, Lundgren L, Lindell G, et al. Predictors of incidental gallbladder cancer in patients undergoing cholecystectomy for benign gallbladder disease: Results from a population-based gallstone surgery registry. Surgery. 2017;162:256–263. doi: 10.1016/j.surg.2017.02.009. [DOI] [PubMed] [Google Scholar]
- 27.Koshiol J, Gao YT, Dean M, et al. Association of aflatoxin and gallbladder cancer. Gastroenterology. 2017;153:488–494. doi: 10.1053/j.gastro.2017.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chow WH, Johansen C, Gridley G, et al. Gallstones, cholecystectomy and risk of cancers of the liver, biliary tract and pancreas. Br J Cancer. 1999;79:640–644. doi: 10.1038/sj.bjc.6690101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ishiguro S, Inoue M, Kurahashi N, et al. Risk factors of biliary tract cancer in a large-scale population-based cohort study in Japan (JPHC study); with special focus on cholelithiasis, body mass index, and their effect modification. Cancer Causes Control. 2008;19:33–41. doi: 10.1007/s10552-007-9067-8. [DOI] [PubMed] [Google Scholar]
- 30.Khan ZR, Neugut AI, Ahsan H, et al. Risk factors for biliary tract cancers. Am J Gastroenterol. 1999;94:149–152. doi: 10.1111/j.1572-0241.1999.00786.x. [DOI] [PubMed] [Google Scholar]
- 31.Zatonski WA, La Vecchia C, Przewozniak K, et al. Risk factors for gallbladder cancer: a Polish case-control study. Int J Cancer. 1992;51:707–711. doi: 10.1002/ijc.2910510508. [DOI] [PubMed] [Google Scholar]
- 32.Diehl AK. Gallstone size and the risk of gallbladder cancer. JAMA. 1983;250:2323–2326. [PubMed] [Google Scholar]
- 33.Shaffer EA. Gallstone disease: epidemiology of gallbladder stone disease. Best Pract Res Clin Gastroenterol. 2006;20:981–996. doi: 10.1016/j.bpg.2006.05.004. [DOI] [PubMed] [Google Scholar]
- 34.Lowenfels AB, Walker AM, Althaus DP, et al. Gallstone growth, size, and risk of gallbladder cancer: an interracial study. Int J Epidemiol. 1989;18:50–54. doi: 10.1093/ije/18.1.50. [DOI] [PubMed] [Google Scholar]
- 35.Kimura W, Shimada H, Kuroda A, et al. Carcinoma of the gallbladder and extrahepatic bile duct in autopsy cases of the aged, with special reference to its relationship to gallstones. Am J Gastroenterol. 1989;84:386–390. [PubMed] [Google Scholar]
- 36.Hundal R, Shaffer EA. Gallbladder cancer: epidemiology and outcome. Clin Epidemiol. 2014;6:99–109. doi: 10.2147/CLEP.S37357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zatonski WA, Lowenfels AB, Boyle P, et al. Epidemiologic aspects of gallbladder cancer: a case-control study of the SEARCH Program of the International Agency for Research on Cancer. J Natl Cancer Inst. 1997;89:1132–1138. doi: 10.1093/jnci/89.15.1132. [DOI] [PubMed] [Google Scholar]
- 38.Ryu S, Chang Y, Yun KE, et al. Gallstones and the risk of gallbladder cancer mortality: a cohort study. Am J Gastroenterol. 2016;111:1476–1487. doi: 10.1038/ajg.2016.345. [DOI] [PubMed] [Google Scholar]
- 39.Machado NO. Porcelain gallbladder: Decoding the malignant truth. Sultan Qaboos Univ Med J. 2016;16:e416–e421. doi: 10.18295/squmj.2016.16.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Khan ZS, Livingston EH, Huerta S. Reassessing the need for prophylactic surgery in patients with porcelain gallbladder: case series and systematic review of the literature. Arch Surg. 2011;146:1143–1147. doi: 10.1001/archsurg.2011.257. [DOI] [PubMed] [Google Scholar]
- 41.Okamoto M, Okamoto H, Kitahara F, et al. Ultrasonographic evidence of association of polyps and stones with gallbladder cancer. Am J Gastroenterol. 1999;94:446–450. doi: 10.1111/j.1572-0241.1999.875_d.x. [DOI] [PubMed] [Google Scholar]
- 42.Wiles R, Varadpande M, Muly S, et al. Growth rate and malignant potential of small gallbladder polyps-systematic review of evidence. Surgeon. 2014;12:221–226. doi: 10.1016/j.surge.2014.01.003. [DOI] [PubMed] [Google Scholar]
- 43.Elmasry M, Lindop D, Dunne DF, et al. The risk of malignancy in ultrasound detected gallbladder polyps: A systematic review. Int J Surg. 2016;33(Pt A):28–35. doi: 10.1016/j.ijsu.2016.07.061. [DOI] [PubMed] [Google Scholar]
- 44.Eaton JE, Talwalkar JA, Lazaridis KN, et al. Pathogenesis of primary sclerosing cholangitis and advances in diagnosis and management. Gastroenterology. 2013;145:521–536. doi: 10.1053/j.gastro.2013.06.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Said K, Glaumann H, Bergquist A. Gallbladder disease in patients with primary sclerosing cholangitis. J Hepatol. 2008;48:598–605. doi: 10.1016/j.jhep.2007.11.019. [DOI] [PubMed] [Google Scholar]
- 46.Chapman R, Fevery J, Kalloo A, et al. Diagnosis and management of primary sclerosing cholangitis. Hepatology. 2010;51:660–678. doi: 10.1002/hep.23294. [DOI] [PubMed] [Google Scholar]
- 47.Gonzalez-Escobedo G, Marshall JM, Gunn JS. Chronic and acute infection of the gall bladder by Salmonella Typhi: understanding the carrier state. Nat Rev Microbiol. 2011;9:9–14. doi: 10.1038/nrmicro2490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Matsukura N, Yokomuro S, Yamada S, et al. Association between Helicobacter bilis in bile and biliary tract malignancies: H. bilis in bile from Japanese and Thai patients with benign and malignant diseases in the biliary tract. Jpn J Cancer Res. 2002;93:842–847. doi: 10.1111/j.1349-7006.2002.tb01327.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Fox JG, Dewhirst FE, Shen Z, et al. Hepatic Helicobacter species identified in bile and gallbladder tissue from Chileans with chronic cholecystitis. Gastroenterology. 1998;114:755–763. doi: 10.1016/s0016-5085(98)70589-x. [DOI] [PubMed] [Google Scholar]
- 50.Murata H, Tsuji S, Tsujii M, et al. Helicobacter bilis infection in biliary tract cancer. Aliment Pharmacol Ther. 2004;20(Suppl 1):90–94. doi: 10.1111/j.1365-2036.2004.01972.x. [DOI] [PubMed] [Google Scholar]
- 51.Strom BL, Soloway RD, Rios-Dalenz JL, et al. Risk factors for gallbladder cancer. An international collaborative case-control study. Cancer. 1995;76:1747–1756. doi: 10.1002/1097-0142(19951115)76:10<1747::aid-cncr2820761011>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- 52.Caygill CP, Hill MJ, Braddick M, et al. Cancer mortality in chronic typhoid and paratyphoid carriers. Lancet. 1994;343:83–84. doi: 10.1016/s0140-6736(94)90816-8. [DOI] [PubMed] [Google Scholar]
- 53.Hassan EH, Gerges SS, El-Atrebi KA, et al. The role of H. pylori infection in gall bladder cancer: clinicopathological study. Tumour Biol. 2015;36:7093–7098. doi: 10.1007/s13277-015-3444-9. [DOI] [PubMed] [Google Scholar]
- 54.Koshiol J, Wozniak A, Cook P, et al. Salmonella enterica serovar Typhi and gallbladder cancer: a case-control study and meta-analysis. Cancer Med. 2016;5:3310–3235. doi: 10.1002/cam4.915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Jablonska B. Biliary cysts: etiology, diagnosis and management. World J Gastroenterol. 2012;18:4801–4810. doi: 10.3748/wjg.v18.i35.4801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Sasatomi E, Tokunaga O, Miyazaki K. Precancerous conditions of gallbladder carcinoma: overview of histopathologic characteristics and molecular genetic findings. J Hepatobiliary Pancreat Surg. 2000;7:556–567. doi: 10.1007/s005340070004. [DOI] [PubMed] [Google Scholar]
- 57.Roukounakis NE, Kuhn JA, McCarty TM. Association of an abnormal pancreaticobiliary junction with biliary tract cancers. Proc (Bayl Univ Med Cent) 2000;13:11–13. doi: 10.1080/08998280.2000.11927636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kamisawa T, Ando H, Suyama M, et al. Japanese clinical practice guidelines for pancreaticobiliary maljunction. J Gastroenterol. 2012;47:731–759. doi: 10.1007/s00535-012-0611-2. [DOI] [PubMed] [Google Scholar]
- 59.Cirillo DJ, Wallace RB, Rodabough RJ, et al. Effect of estrogen therapy on gallbladder disease. JAMA. 2005;293:330–339. doi: 10.1001/jama.293.3.330. [DOI] [PubMed] [Google Scholar]
- 60.Liu B, Beral V, Balkwill A, et al. Gallbladder disease and use of transdermal versus oral hormone replacement therapy in postmenopausal women: prospective cohort study. BMJ. 2008;337:a386. doi: 10.1136/bmj.a386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Broden G, Bengtsson L. Biliary carcinoma associated with methyldopa therapy. Acta Chir Scand Suppl. 1980;500:7–12. [PubMed] [Google Scholar]
- 62.Lowenfels AB, Norman J. Isoniazid and bile duct cancer. JAMA. 1978;240:434–435. doi: 10.1001/jama.1978.03290050024007. [DOI] [PubMed] [Google Scholar]
- 63.Dixit R, Shukla VK. In: Perspectives in Cancer Prevention-Translational Cancer Research - Why Is Gallbladder Cancer Common in the Gangetic Belt? Sudhakaran P, editor. New Delhi: Springer; 2014. pp. 145–151. [Google Scholar]
- 64.Sharma A, Sharma KL, Gupta A, et al. Gallbladder cancer epidemiology, pathogenesis and molecular genetics: Recent update. World J Gastroenterol. 2017;23:3978–3998. doi: 10.3748/wjg.v23.i22.3978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Yagyu K, Kikuchi S, Obata Y, et al. Cigarette smoking, alcohol drinking and the risk of gallbladder cancer death: a prospective cohort study in Japan. Int J Cancer. 2008;122:924–929. doi: 10.1002/ijc.23159. [DOI] [PubMed] [Google Scholar]
- 66.Grainge MJ, West J, Solaymani-Dodaran M, et al. The antecedents of biliary cancer: a primary care case-control study in the United Kingdom. Br J Cancer. 2009;100:178–180. doi: 10.1038/sj.bjc.6604765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Bagnardi V, Rota M, Botteri E, et al. Alcohol consumption and site-specific cancer risk: a comprehensive dose-response meta-analysis. Br J Cancer. 2015;112:580–593. doi: 10.1038/bjc.2014.579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Calle EE, Rodriguez C, Walker-Thurmond K, Thun MJ. Overweight, obesity, and mortality from cancer in a prospectively studied cohort of U.S. adults. N Engl J Med. 2003;348:1625–1638. doi: 10.1056/NEJMoa021423. [DOI] [PubMed] [Google Scholar]
- 69.Bandera E, Fay S. World Cancer Research Fund International Continuous Update Project Panel. The use and interpretation of anthropometric measures in cancer epidemiology: a perspective from the World Cancer Research Fund international continuous update project. Int J Cancer. 2016;139:2391–2397. doi: 10.1002/ijc.30248. [DOI] [PubMed] [Google Scholar]
- 70.Calle EE, Rodriguez C, Jacobs EJ, et al. The American Cancer Society Cancer Prevention Study II Nutrition Cohort: rationale, study design, and baseline characteristics. Cancer. 2002;94:2490–2501. doi: 10.1002/cncr.101970. [DOI] [PubMed] [Google Scholar]
- 71.Larsson SC, Wolk A. Obesity and the risk of gallbladder cancer: a meta-analysis. Br J Cancer. 2007;96:1457–1461. doi: 10.1038/sj.bjc.6603703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Li ZM, Wu ZX, Han B, et al. The association between BMI and gallbladder cancer risk: a meta-analysis. Oncotarget. 2016;7:43669–43679. doi: 10.18632/oncotarget.9664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Gu J, Yan S, Wang B, et al. Type 2 diabetes mellitus and risk of gallbladder cancer: a systematic review and meta-analysis of observational studies. Diabetes Metab Res Rev. 2016;32:63–72. doi: 10.1002/dmrr.2671. [DOI] [PubMed] [Google Scholar]
- 74.Obesity Trends in the United States. J Natl Cancer Inst. 2016;108:djw246. doi: 10.1093/jnci/djw246. [DOI] [PubMed] [Google Scholar]
- 75.Ward BW, Clarke TC, Nugent CN, et al. Early release of selected estimates based on data from the 2015 National Health Interview Survey. National Center for Health Statistics; 2016. May, Available from: https://www.cdc.gov/nchs/data/nhis/earlyrelease/earlyrelease201605.pdf. Accessed Dec 05 2018. [Google Scholar]
- 76.Hoffman SL, Woodward TE, Hornick RB, et al. Effective treatment and prevention of typhoid fever: updated. Trans Am Clin Climatol Assoc. 1984;95:52–65. [PMC free article] [PubMed] [Google Scholar]