Abstract
Previous research from our laboratory has demonstrated that V1 vasopressin receptor agonist (V1 agonist) induces a complex intracellular Ca2+-signaling cascade in cortical astrocytes that is initiated by G-protein-coupled V1a vasopressin receptor-mediated cytoplasmic and nuclear Ca2+ rise and converges during activation of the nuclear transcription factor cAMP response element-binding protein (CREB). In the current study, we pursued the downstream functional consequences of V1 agonist-induced Ca2+-signaling cascade for gene expression. Because astrocytes can exert immune effects analogous to immune cells in the periphery, we investigated V1 agonist regulation of cytokine gene expression in astrocytes. Results from gene array studies indicated that V1 agonist dramatically decreased the mRNA level of five cytokines. Two prominent proinflammatory cytokines, interleukin-1β (IL-1β) and tumor necrosis factor-α (TNF-α), were selected for detailed analysis, and their expression was also confirmed with reverse transcriptase-PCR. Furthermore, ELISA analyses demonstrated that the peptide level of IL-1β and TNF-α in the astrocyte medium was also decreased in response to V1 agonist. Using CREB antisense to determine the causal relationship between V1 agonist-induced CREB activation and suppression of IL-1β and TNF-α, we demonstrated that decreased IL-1β and TNF-α gene expression was dependent on upstream CREB activation. V1 agonist-induced decrease of cytokine release from cortical astrocytes was also shown to be neuroprotective in cortical neurons. To our knowledge, this is the first documentation of V1 agonist modulation of cytokine gene expression in any cell type. Implications for vasopressin as an antipyretic agent and the role of vasopressin in neurodegeneration, autoimmune diseases, stress, and neuropsychiatric behaviors are discussed.
Keywords: vasopressin, V1a vasopressin receptor, fever, stress, calcium signaling, cortical astrocytes, cytokines, interleukin-1β, IL-1β, tumor necrosis factor-α, TNF-α, cyclic-AMP response element-binding protein, CREB, CREB antisense, gene array, neuroprotection
Introduction
One of the most important functions of vasopressin that has received considerable attention within the last several years is its immune modulatory capabilities. It has been suggested that brain vasopressin is involved in stress-induced suppression of the immune function in rats by suppressing the proliferative response of splenic T cells and natural killer cell cytotoxicity (Shibasaki et al., 1998). Moreover, rabbits immunized against vasopressin develop autoimmune alterations in neurohypophysis, as evidenced by infiltration by immune cells and extracellular deposits of immunoglobulins (Cau and Rougon-Rapuzzi, 1979), and the lack of vasopressin in Brattleboro rats elevates baseline natural killer cell activity (Yirmiya et al., 1989).
The long-held theory of vasopressin immunomodulation proposes that vasopressin modulates adrenocorticotropin (ACTH) release, which in turn stimulates the adrenal glands to release glucocorticoids that suppress the immune system by suppressing proinflammatory cytokines (Sternberg, 1997). Despite the findings of vasopressin receptor localization in immune cells in the brain, such as astrocytes and microglia, and in immune tissues in the periphery, such as in the human thymus, which plays a pivotal role in the maturation and differentiation of T-lymphocytes (Melis et al., 1993), investigation of direct effects of vasopressin on immune cells has been minimal.
One of the cell types in the CNS that regulates immune response in brain is astrocytes (Dong, 2001). Although still controversial, mounting evidence indicates that astrocytes can express major histocompatability complex class II molecules that play a critical role in the induction of immune responses through presentation of processed antigens to cluster of differentiation 4+ (CD4+) T-helper cells (Wong et al., 1984), suggesting that astrocytes could function as antigen-presenting cells. During stimulation, astrocytes can also express costimulatory molecules, including CD40, B7-1, and B7-2, that are essential for activation of naive T cells (Nikcevich et al., 1997). Furthermore, astrocytes are potent producers of a number of cytokines and chemokines (Dong, 2001). Among the cytokines expressed by astrocytes, interleukin-1β (IL-1β) and tumor necrosis factor-α (TNF-α) have received considerable attention recently because of their proinflammatory effects in the CNS.
Previous studies from our laboratory revealed that V1a vasopressin receptor (V1aR) activation induces a significant rise in both cytoplasmic and nuclear Ca2+ concentrations in astrocytes (Zhao and Brinton, 2002). Furthermore, V1aR activation leads to a complex signaling cascade involving activation of PKC, CaMKII (calcium calmodulin-dependent protein kinase II), and ERK1/2 (extracellular signal-regulated kinase), which results in cAMP response element-binding protein (CREB) activation in the nucleus (Zhao and Brinton, 2003). The present study sought to determine the downstream consequences of vasopressin receptor activation of the Ca2+-kinases-CREB cascade. Because of the immune function of astrocytes and the immunoregulatory function of vasopressin in the periphery, we investigated the impact of a V1 agonist (V1a) on the immune function of cortical astrocytes, specifically modulation of cytokine expression. Using gene array, reverse transcriptase (RT)-PCR, and ELISA, we demonstrated that V1 agonist suppressed expression of a number of cytokines, especially the two important proinflammatory cytokines IL-1β and TNF-α at both mRNA and protein levels. Furthermore, suppression of both IL-1β and TNF-α was dependent on upstream CREB activation, and decreased IL-1β and TNF-α release from astrocytes was neuroprotective.
Materials and Methods
Cell culture preparation. Primary cultures of cortical astrocytes and neurons were prepared following the methods described previously (Zhao and Brinton, 2003; Zhao et al., 2003). Briefly, cortices were dissected from the brains of embryonic day 18 (E18) Sprague Dawley rat fetuses. The tissue was treated with 0.05% trypsin in HBSS (5.4 mm KCl, 0.4 mm KH2PO4, 137 mm NaCl, 0.34 mm Na2HPO4·7H2O, 10.0 mm glucose, 10.0 mm HEPES) for 5 min at 37°C. After incubation, trypsin was inactivated with cold 10% fetal bovine serum (FBS; Invitrogen, Carlsbad, CA)-containing DMEM (Invitrogen) supplemented with 10 mm NaHCO3, 5 U/ml penicillin, 5 μg/ml streptomycin, and 10% F12 nutrient medium for 3 min at 37°C. Tissue was then washed with HBSS twice and dissociated by repeated passage through a series of fire-polished constricted Pasteur pipettes. For astrocyte culture, cells were plated at a concentration of 1 × 106 cells/ml in 10% FBS-containing DMEM in 25 mm flasks, and the cultures were maintained at 37°C with 5% CO2. After 3-7 d in culture, glial cells were shaken at 220 rpm for 16 hr to remove oligodendrocytes and microglia. The attached astrocytes were then trypsinized and plated onto poly-d-lysine (10 μg/ml)-coated 60 mm Petri dishes and cultured in the same medium at 37°C with 5% CO2 for 2-5 d before experiments. For neuronal culture, 105 cells/ml were plated onto poly-d-lysine-coated 24-well culture plates for lactate dehydrogenase (LDH) analyses, whereas between 20,000 and 40,000 cells were seeded onto poly-d-lysine-coated 4-well chamber slides for terminal deoxynucleotidyl transferase-mediated biotinylated UTP nick end labeling (TUNEL) analyses. Neurons were grown in neurobasal medium (NBM; Invitrogen) supplemented with B27, 5 U/ml penicillin, 5 μg/ml streptomycin, 0.5 mm glutamine, and 25 μm glutamate at 37°C in 10% CO2. The culture media were exchanged with glutamate-free NBM 3 d after the day of cell culture, and the cortical neurons were fed with glutamate-free NBM twice weekly before experiments.
Inflammatory response cytokine gene array. Cortical astrocytes grown on poly-d-lysine-coated dishes were serum deprived overnight and then treated with V1 agonist or control vehicle for 24 hr. After treatment, astrocytes were rinsed twice with ice-cold PBS, and total RNA was extracted using TRIzol (Invitrogen) according to the instructions of the manufacturer and resuspended in 10 μl of DEPC-treated water. RNA concentration was determined using a BioPhotometer (Eppendorf Scientific, Hamburg, Germany). The gene expression profile of inflammatory cytokines was determined using an inflammatory response cytokine pathway-finder GEArray system (mGEA1013030; Super Array, Bethesda, MD), which detects 23 genes involved in inflammatory responses and two housekeeping genes, β-actin and glyceraldehyde-3-phosphate dehydrogenase (GAPDH). Briefly, total RNA was used as templates for biotinylated probe synthesis. Each total RNA sample (8 μg) was combined with 2 μl of GEA primer mix and preheated at 70°C for 2 min. Twenty microliters of master labeling mix (containing 8 μl of 5× GEA-labeling buffer, 4 μl of 1 mm biotin-16-dUTP, 1 μl of RNase inhibitor, 100 U of Moloney murine leukemia virus reverse transcriptase, and 5 μl of RNase-free H2O) was added to each sample, and the labeling reaction was conducted at 42°C for 2 hr. The labeled cDNA probe was then hybridized with the inflammatory cytokine GEArray membrane containing prespotted cDNA fragments at 68°C overnight with continuous agitation. The size of the cDNAs spotted on the array varies from gene to gene but is usually between 250 and 600 base pairs. The membrane was then washed at 68°C twice with prewarmed solution 1 (2× SSC, 1% SDS) and twice with prewarmed wash solution 2 (0.1× SSC, 0.5% SDS) for 20 min each. The membrane was blocked with 10 ml of GEA-blocking solution for 40 min and incubated with 1:5000 to 1:10,000 diluted alkaline phosphatase-streptavidin for 40 min. After extensive washes, the membrane was incubated with disodium 2-chloro-5-(4-methoxyspiro{1,2-dioxetane-3,2′-(5′-chloro) tricyclo[3.3.1.1.3,7]decan}-4-yl)-1-phenyl phosphate-Star for 2-5 min and exposed to x-ray film. The relative expression level of each gene was determined by comparing the signal intensity of each gene in the array after normalization to the signal of housekeeping genes β-actin and GAPDH. Densitometric quantification of the array was performed with Un-Scan-It gel image software (Silk Scientific, Orem, UT). The limitation of this method is that the arrays are prespotted with mouse cytokine cDNAs. Although the arrays are developed using homology sequences between rats and mice and the sequences of the mouse genes on this array have a CLUSTAL W score of at least 80 when compared with the sequence of the corresponding rat gene, it is possible that some biotinylated cDNAs do not hybridize with sequences on the arrays and, therefore, we might not be able to detect all of the genes.
RT-PCR. Cortical astrocytes grown on poly-d-lysine-coated culture dishes for 2-5 d were serum deprived overnight and treated with V1 agonist and various pharmacological agents for appropriate periods. After treatment, total RNA was extracted from astrocytes using TRIzol (Invitrogen) according to the instructions of the manufacturer and resuspended in 10 μl of DEPC-treated water. RNA concentration was determined using a BioPhotometer (Eppendorf Scientific). Four micrograms of RNA was reverse-transcribed to generate cDNA using random hexamer primers and SuperScript II (Invitrogen). PCR was conducted using a RoboCycler (400864; Stratagene, La Jolla, CA). Primer sequences and annealing temperatures for IL-1β and TNF-α PCR are listed in Table 2. PCR products and a 1 kb DNA molecular weight marker were then electrophoresed on a 1% agarose gel, and the gel was visualized and photographed under UV light. Un-Scan-It gel image software (Silk Scientific) was used for the quantitative analyses.
Table 2.
Oligonucleotide primers used for cDNA amplification
|
|
Sense primer |
Antisense primer |
|
|
|
||||
|---|---|---|---|---|---|---|---|---|---|
| mRNA |
5′ |
3′ |
5′ |
3′ |
Anneal temperature |
PCR target |
Cycles |
||
| IL-1β | GCACCTTCTTTTCCTTCATC | CTGATGTACCAGTTGGGGAA | 55°C | 448 bp | 40 | ||||
| TNF-α |
GGCAGGTCTACTTTGGAGTCATTGC |
|
ACATTCGGGGATCCAGTGAGTTCCG |
56°C |
319 bp |
40 |
|||
Western immunoblotting. Protein concentration was determined by the BCA method. An appropriate volume of 4× sample buffer was added to the protein samples, and samples were boiled at 95°C for 5 min. Samples (25 μg of proteins per well) were loaded on a 10% SDS-PAGE gel and resolved by standard electrophoresis at 90 V. Proteins were then electrophoretically transferred to Immobilon-P polyvinylidene difluoride membranes overnight at 32 V at 4°C. Membranes were blocked for 1 hr at room temperature in 10% nonfat dried milk in PBS containing 0.05% Tween 20 (PBS-T), incubated with appropriate primary antibodies against phospho-CREB (pSer133; mouse monoclonal, 1:2000; Cell Signaling Technology, Beverly, MA), CREB (rabbit polyclonal, 1:1000; Cell Signaling Technology), or β-actin (mouse monoclonal, 1:200; Santa Cruz Biotechnology, Santa Cruz, CA) at temperatures and times specified by the antibody providers. All primary antibodies were dissolved in PBS-T with 1% horse serum for mouse monoclonal antibodies or 1% goat serum for rabbit polyclonal antibodies. After washing in PBS-T, the membranes were incubated with horseradish peroxidase-conjugated anti-mouse IgG (1:5000; Vector Laboratories, Burlingame, CA) in PBS-T with 1% horse serum or anti-rabbit IgG (1:5000; Vector Laboratories) in PBS-T with 1% goat serum for 1 hr. Immunoreactive bands were visualized by TMB detection kit (Vector Laboratories) and quantified using Un-Scan-It gel image software (Silk Scientific). After transfer, gels were stained with Coomassie blue (Bio-Rad, Hercules, CA) to double-check equal protein loading.
CREB antisense treatment. The contribution of CREB on the V1 agonist-induced suppression of IL-1β and TNF-α was determined by examining the influence of 200 nm CREB antisense, sense, and random oligonucleotides. The sequences of the oligonucleotides were 5′TGGTCATCTAGTCACCGGTG3′ for CREB antisense, 5′CACCGGTGACTAGATGACCA3′ for CREB sense, and 5′TGCTGAACTTGTCGCCAGTG3′ for the random oligonucleotide. The CREB antisense oligonucleotide (AS) has been used in several previous studies and has been shown to attenuate CREB expression (Konradi et al., 1994; Konradi and Heckers, 1995; Guzowski and McGaugh, 1997; Murphy and Segal, 1997; White et al., 2000). The phosphorothioate-modified HPLC-purified oligonucleotides were transfected into cortical astrocytes in the presence of a transfection reagent oligofectamine (Invitrogen) in Opti-MEM I reduced serum medium (Opti-MEM; Invitrogen). Briefly, astrocytes were washed with Opti-MEM once before addition of oligonucleotides and oligofectamine. The volume ratio of oligofectamine/oligonucleotide (20 μm stock) used for transfection studies was 3:10. After an overnight incubation, astrocytes were treated with V1 agonist or lipopolysaccharide (LPS) for 24 hr in fresh Opti-MEM with fresh oligonucleotides and oligofectamine added before RNA or medium collection for RT-PCR or ELISA analyses.
ELISA. Cortical astrocytes grown on poly-d-lysine-coated dishes for 2-5 d were serum-deprived overnight and treated with V1 agonist and various pharmacological agents for appropriate periods. After treatment, the medium was collected from cortical astrocytes. ELISA was conducted using Quantikine IL-1β or TNF-α ELISA system (R & D Systems, Minneapolis, MN). Briefly, a monoclonal antibody specific for rat IL-1β or TNF-α was precoated onto a microplate. Fifty microliters of assay diluent were added to each well of the microplate. Fifty microliters of standards, controls, or samples were pipetted into the wells and incubated for 2 hr at room temperature. After extensive washing to remove any unbound substances, an enzyme-linked polyclonal antibody specific for rat IL-1β or TNF-α (100 μl) was added to each well and incubated for 2 hr at room temperature. The wells were extensively washed to remove any unbound antibody-enzyme reagent, and 100 μl of substrate solution was added to each well to incubate for 30 min at room temperature in the dark. One hundres microliters of stop solution was then added to each well, and the optical density of each well was read at 450 nm using a microplate reader (Molecular Devices, Sunnyvale, CA).
Efflux assay of LDH. Cortical neuronal cultures grown in 24-well plates in NBM were treated with astrocyte-conditioned medium (ACM) and various cytokines for 24 hr followed by medium change to NBM. LDH release into the NBM culture media was measured 24 hr later using a cytotoxicity detection kit from Boehringer Mannheim (Indianapolis, IN), and absorption was read at 490 nm.
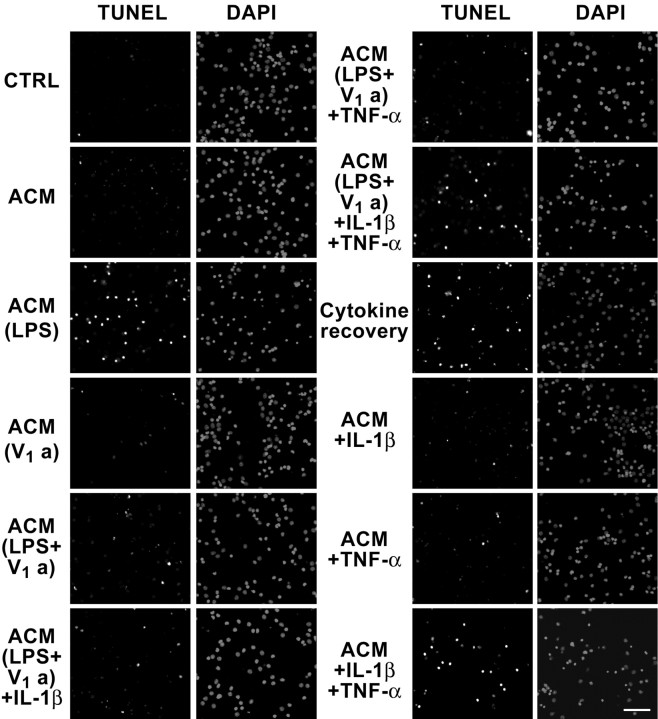
TUNEL analysis. Apoptosis was determined using TUNEL. Cortical neuronal cultures grown on 4-well chamber slides were treated with astrocyte-conditioned medium and various cytokines for 24 hr. The treated cells were rinsed with PBS and fixed with 95% methanol for 5 min at 4C°. Subsequently, neurons were incubated with the TUNEL reaction mixture (In Situ Cell Death Detection kit; fluorescein; Boehringer Mannheim) for 60 min at 37°C. After washing with PBS for three times, neurons were mounted with mounting medium containing 4′,6′-diamidino-2-phenylindole (DAPI; Vector Laboratories) to stain the nucleus. Apoptosis was qualified by fluorescence microscopy.
Chemicals. V1 agonist ([Phe2, Orn8]-oxytocin) was purchased from Bachem Bioscience (King of Prussia, PA). LPS was obtained from Sigma (St. Louis, MO). CREB antisense, sense, and random oligonucleotides were purchased from Integrated DNA Technologies (Coralville, IA).
Data analysis. Data were presented as group means ± SEM. RT-PCR, ELISA, and LDH data were expressed as the percentage relative to unstimulated controls run in the same experiment. Statistical analysis was performed by Student's t test or by one-way ANOVA followed by Newman-Keuls post hoc analysis.
Results
To selectively activate the V1a vasopressin receptor in cortical astrocytes, a specific V1 vasopressin receptor agonist, [Phe2, Orn8]-oxytocin, was used in the present study. Our previous studies showed that both the endogenous arginine vasopressin and the V1 agonist exerted comparable effects in raising intracellular Ca2+ level and kinase activation at 100 nm (Zhao and Brinton, 2002, 2003). V1 agonist used throughout the study was based on our previous dose-response analyses that determined 100 nm as the optimal concentration for V1 agonist-induced intracellular Ca2+ signaling (Zhao and Brinton, 2002).
Suppression of inflammatory cytokines gene expression in response to V1 agonist in cortical astrocytes
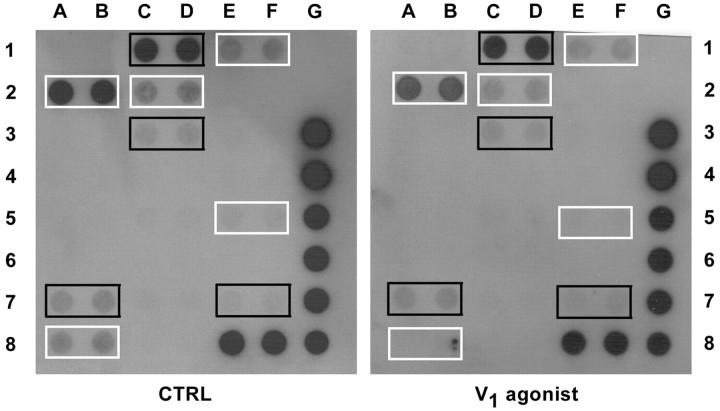
Astrocytes, which can function as immune cells in the brain, produce a variety of cytokines and chemokines. To investigate the impact of V1 agonist on the immune function of astrocytes, the expression profile of inflammatory cytokines was investigated using an inflammatory response cytokine GEArray system, which determines gene expression of 23 inflammatory cytokines. Each cytokine is represented by two consecutive spots on the control and the V1 agonist membranes containing prespotted cDNA fragments. The array set shown in Figure 1 is a representative of two independent experiments. Expression of five cytokines was decreased in response to 100 nm V1 agonist, including IL-1α (Fig. 1, 1E, 1F), IL-1β (2A, 2B), IL-2 (2C, 2D), lymphotoxin-B (5E, 5F), and TNF-α (8A, 8B) shown in white boxes. The percentage of cytokine expression relative to control is shown in Table 1. Expression of cytokines shown in the black boxes, including GRO1 oncogene (Fig. 1, 1C, 1D), IL-6 (3C, 3D), TGFβ1 (7A, 7B), and TGFβ3 (7E, 7F), was unchanged. Expression of the housekeeping genes β-actin (Fig. 1, 3G, 4G) and GAPDH (5G, 6G, 7G, 8E, 8F, 8G) were consistent across both conditions.
Figure 1.
Profile of inflammatory cytokine gene expression in response to V1 agonist in cortical astrocytes. Astrocytes were treated in the absence or presence of 100 nm V1 agonist for 24 hr followed by inflammatory cytokine GEArray analysis. Each cytokine is represented by two consecutive spots on both membranes. This array is representative of two independent analyses. Expression of a number of cytokines was decreased, including IL-1α (1E, 1F), IL-1β (2A, 2B), IL-2 (2C, 2D), lymphotoxin-B (5E, 5F), and TNF-α (8A, 8B), which are shown in white boxes. Expression of cytokines shown in the black boxes, including GRO1 oncogene (1C, 1D), IL-6 (3C, 3D), TGFβ1 (7A, 7B), and TGFβ3 (7E, 7F), were unchanged. Housekeeping genes, including β-actin (3G, 4G) and GAPDH (5G, 6G, 7G, 8E, 8F, 8G), were consistent between two membranes.
Table 1.
Densitometric quantification of V1 agonist-induced cytokine gene suppression
|
Cytokines |
IL-1α |
IL-1β |
IL-2 |
Lymphotoxin-B |
TNF-α |
|---|---|---|---|---|---|
| Percentage of control |
80.78% |
85.21% |
86.86% |
88.20% |
75.23% |
Astrocytes were treated in the absence or presence of 100nm V1 agonist for 24 hr followed by inflammatory cytokine GEArray analysis. Densitometric quantification of V1 agonist-induced cytokine gene expression was analyzed with Un-Scan-It gel image software and expressed as percentage of control gene expression.
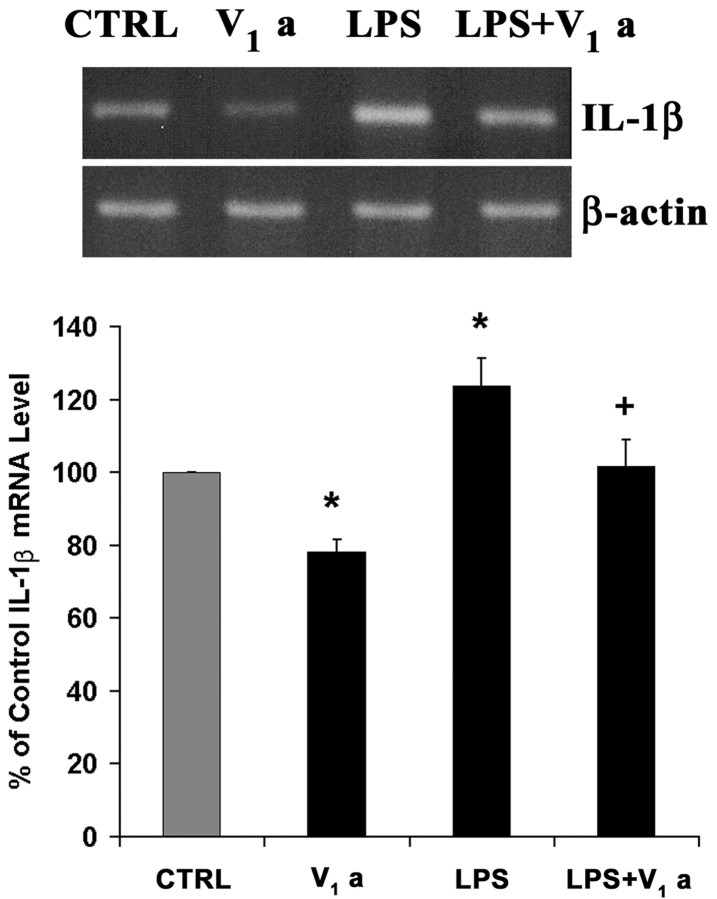
To confirm the gene array data on suppression of IL-1β by V1 agonist, semiquantitative RT-PCR was conducted. Furthermore, to determine whether V1 agonist also prevents toxin-stimulated inflammatory response, astrocytes were treated with LPS (50 ng/ml), a bacterial endotoxin known to induce cytokine upregulation in a number of immune cells (Raetz and Whitfield, 2002), and the impact of V1 agonist on LPS-upregulated IL-1β expression was investigated (Fig. 2). Primer sequences and annealing temperatures for IL-1β PCR are listed in Table 2. RT-PCR statistical data from three independent experiments indicate that V1a significantly decreased IL-1β mRNA level (78.29 ± 3.36% relative to control; *p < 0.05 compared with control), consistent with the gene array data. When astrocytes were stimulated with LPS, IL-1β mRNA increased significantly (123.68 ± 7.61% relative to control; *p < 0.05 compared with control). V1 agonist treatment significantly reduced IL-1β mRNA induction compared with the LPS alone-treated cultures (101.59 ± 7.51% relative to control; +p < 0.05 compared with LPS alone).
Figure 2.
Suppression of IL-1β gene expression by V1 agonist is confirmed by RT-PCR. Astrocytes were treated in the absence or presence of V1 agonist (100 nm) or LPS (50 ng/ml) for 24 hr followed by RNA extraction and RT-PCR for IL-1β. PCR products were then run on an agarose gel to determine the expression level of IL-1β. The percentage change of IL-1β gene expression relative to control (CTRL) is presented in the bar graph. Each bar represents the mean ± SEM (n = 3 for each condition). *p < 0.05 versus control; +p < 0.05 versus LPS-treated culture.
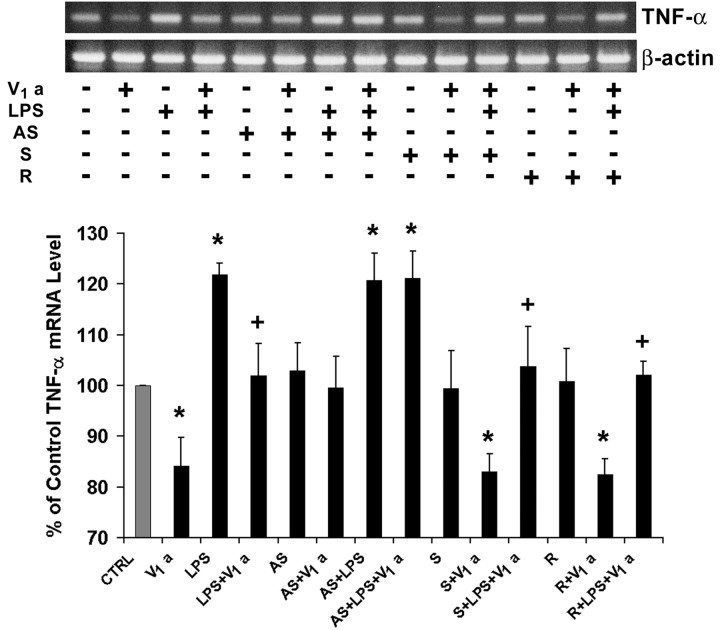
Confirmation of TNF-α suppression by V1 agonist was also investigated using RT-PCR (Fig. 3). Cortical astrocytes were treated the same as for the IL-1β mRNA analysis. Primer sequences and annealing temperatures for TNF-α PCR are also listed in Table 2. Statistical analysis of three independent experiments indicated that V1 agonist significantly decreased TNF-α mRNA level (80.87 ± 5.15% relative to control; *p < 0.05 compared with control), which is consistent with the gene array data. As expected, LPS significantly upregulated TNF-α gene expression (122.82 ± 1.86% relative to control; *p < 0.05 compared with control), which was reversed to control level by 100 nm V1 agonist treatment (103.79 ± 4.77% relative to control; +p < 0.05 compared with LPS alone).
Figure 3.
Suppression of TNF-α gene expression by V1 agonist is confirmed by RT-PCR. Astrocytes were treated in the absence or presence of V1 agonist (100 nm) or LPS (50 ng/ml) for 24 hr followed by RNA extraction and RT-PCR for TNF-α. PCR products were then run on an agarose gel to determine the expression level of TNF-α. The percentage change of TNF-α gene expression relative to control (CTRL) is presented in the bar graph. Each bar represents the mean ± SEM (n = 3 for each condition). *p < 0.05 versus control; +p < 0.05 versus LPS-treated culture.
Suppression of IL-1β and TNF-α gene expression in response to V1 agonist is dependent on transcription factor CREB activation
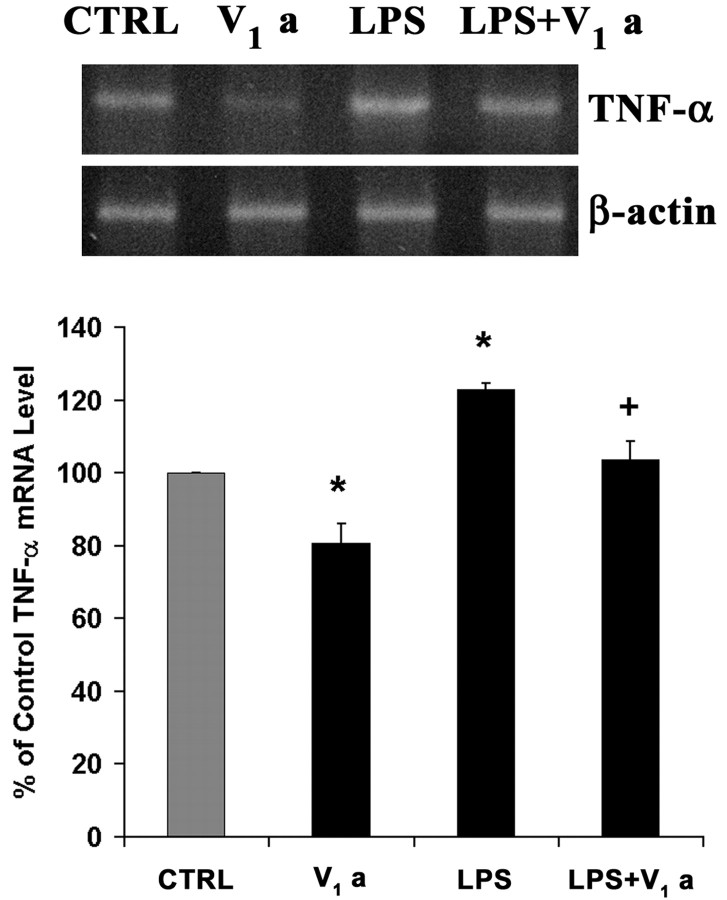
CREB is a multifunctional leucine zipper-containing transcription factor involved in the regulation of a variety of genes. Furthermore, it has been suggested that CREB is involved in suppression of cytokine gene expression in other systems (Delgado et al., 1998; Perez et al., 1999; Cho et al., 2001). Our previous studies on V1 agonist-induced nuclear-signaling cascade demonstrated that CREB is significantly activated in cortical astrocytes in response to V1 agonist in a time-dependent manner (Zhao and Brinton, 2003), which is confirmed in the current study and shown in Figure 4A.
Figure 4.
V1 agonist-induced suppression of IL-1β is dependent on CREB activation. A, Western blot data on V1 agonist-induced CREB activation in cortical astrocytes. Each bar represents the mean ± SEM (n = 3 for each condition). *p < 0.05 versus control (CTRL). B, Western blot data on CREB level after CREB antisense, sense, and random oligonucleotide treatment for overnight. CREB AS was used to knock down CREB in the cortical astrocytes. S and R were used as control conditions to rule out nonspecific effects of CREB antisense. Each bar represents the mean ± SEM (n = 3 for each condition). *p < 0.05 versus control. C, Astrocytes were treated according to the indicated conditions for 24 hr followed by RNA extraction and RT-PCR on IL-1β. Each bar represents the mean ± SEM (n = 3 for each condition). *p < 0.05 versus control; +p < 0.05 versus LPS-treated culture.
To determine whether CREB is required for V1 agonist-induced suppression of IL-1β and TNF-α gene expression in astrocytes, CREB AS was used to knock down CREB in astrocytes. CREB sense oligonucleotide (S) and a random oligonucleotide (R) were also used to rule out nonspecific effects of CREB antisense. First, to ensure the efficiency of CREB antisense to knock down CREB, CREB protein level was determined after the CREB antisense, sense, or random oligonucleotides treatment overnight. Western blot analysis revealed that CREB protein level was significantly decreased after CREB antisense treatment, although it was not affected by CREB sense or random oligonucleotides. Protein levels were normalized against β-actin protein content. Statistical analysis of optical density from three independent experiments indicated that CREB antisense induced ∼50% suppression in CREB protein level (Fig. 4B) (percentage ± relative to control; *p < 0.05). Impact of the CREB antisense on IL-1β and TNF-α mRNA level was investigated using RT-PCR. Cortical astrocytes were transfected overnight with various oligonucleotides followed by treatment with V1 agonist and LPS for 24 hr. Statistical analysis of RT-PCR data on IL-1β from three independent experiments indicated that CREB antisense completely blocked V1 agonist-induced suppression of IL-1β gene expression (Fig. 4C) (AS+V1a, 104.06 ± 3.60% relative to control, compared with V1a), whereas CREB sense and random oligonucleotides had no effect (Fig. 4C, compare V1a with S+V1a or R+V1a). Similarly, CREB antisense completely reversed V1 agonist inhibition of LPS induction of IL-1β (Fig. 4C) (AS+LPS+V1 a, 129.91 ± 4.00% relative to control, compared with LPS+V1a), whereas CREB sense and random oligonucleotides had no effect (Fig. 4C, compare LPS+V1a with S+LPS+V1a or R+LPS+V1a).
We also determined the role of CREB on V1 agonist-induced suppression of TNF-α (Fig. 5). Cortical astrocytes were treated the same as for IL-1β analyses. Statistical analysis of RT-PCR data on TNF-α from three independent experiments indicated that V1 agonist-induced suppression of TNF-α gene expression was completely abolished by CREB antisense (Fig. 5) (AS+V1a, 99.52 ± 6.21% relative to control, compared with V1a), whereas it was not affected by CREB sense and random oligonucleotides (Fig. 5, compare V1a with S+V1a or R+V1a). Similarly, CREB antisense completely abolished V1 agonist repression of LPS-upregulated TNF-α (Fig. 5) (AS+LPS+V1a, 121.16 ± 5.26% relative to control, compared with LPS+V1a), whereas CREB sense and random oligonucleotides had no effect (Fig. 5, compare LPS+V1a with S+LPS+V1a or R+LPS+V1a).
Figure 5.
V1 agonist-induced suppression of TNF-α is dependent on CREB activation. Astrocytes were treated according to the indicated conditions for 24 hr followed by RNA extraction and RT-PCR on TNF-α. CREB AS was used to knock down CREB in the cortical astrocytes. S and R were used as control (CTRL) conditions to rule out nonspecific effects of CREB antisense. Each bar represents the mean ± SEM (n = 3 for each condition). *p < 0.05 versus control; +p < 0.05 versus LPS-treated culture.
V1 agonist-induced decrease of IL-1β and TNF-α detected in the medium of cortical astrocytes and its dependence on CREB activation
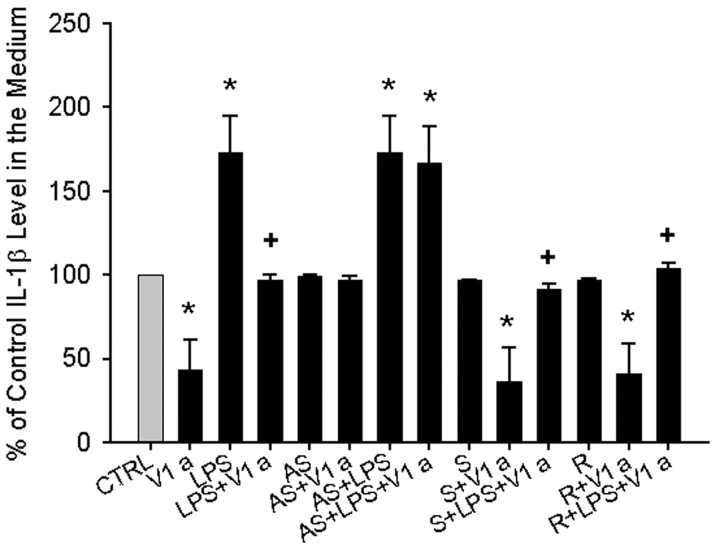
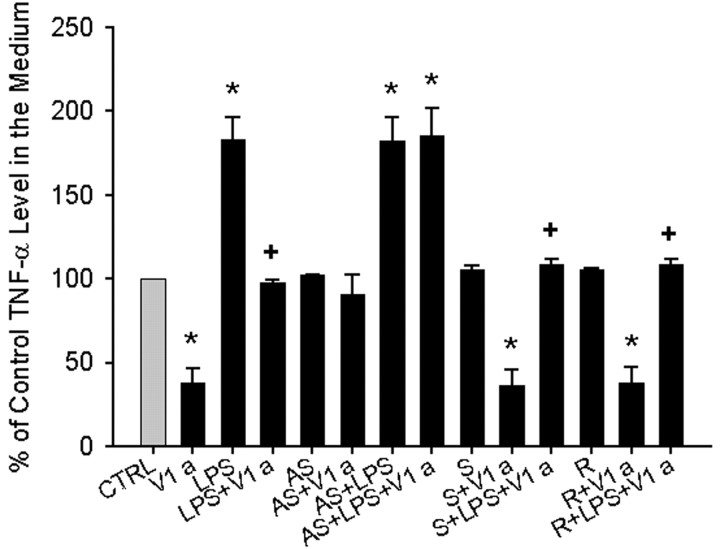
As shown above, V1 agonist decreased the mRNA level of IL-1β and TNF-α in astrocytes. We next pursued whether the products of IL-1β and TNF-α gene expression were altered in response to V1 agonist. IL-1β and TNF-α are released into the extracellular medium after synthesis and cleavage of their precursors to generate mature active peptides by IL-1β-converting enzyme and TNF-α-converting enzyme, respectively (Dinarello, 1994; Black et al., 1997; Moss et al., 1997). We conducted cytokine-specific ELISA to determine the level of IL-1β and TNF-α in the astrocyte medium. Statistical analysis of IL-1β relative to control is shown in Figure 6 and is representative of three independent experiments. V1 agonist treatment of astrocytes significantly decreased IL-1β peptide level in the medium (43.69 ± 17.51% relative to control; *p < 0.05 compared with control). LPS-stimulated IL-1β peptide upregulation (∼250 pg/ml) was completely blocked by treatment with V1 agonist (∼125 pg/ml; 97.16 ± 2.95% relative to control; +p < 0.05 compared with LPS alone).
Figure 6.
V1 agonist-induced decrease of IL-1β detected in the medium of cortical astrocytes and its dependence on CREB activation. Astrocytes were treated according to the indicated conditions for 24 hr followed by medium collection and ELISA analysis on IL-1β. Results are expressed as mean ± SEM percentage change of IL-1β level in the medium relative to control (CTRL) and are representative of three separate experiments. n = 3 for each condition; *p < 0.05 versus control; +p < 0.05 versus LPS-treated culture. The measured value for the control IL-1β level in the medium was 131.43 ± 9.09 pg/ml.
The contribution of CREB to V1 agonist regulation of IL-1β peptide release was investigated using CREB antisense, sense, and random oligonucleotides. CREB antisense completely blocked V1 agonist-induced decrease of IL-1β peptide in the medium derived from treated astrocytes (AS+V1a, 97.35 ± 2.07% relative to control, compared with V1a), whereas CREB sense and random oligonucleotides had no effect (compare V1a with S+V1a or R+V1a). Similarly, V1 agonist inhibition of LPS induction of IL-1β peptide in the astrocytes medium was completely reversed by CREB antisense (AS+LPS+V1a, 166.95 ± 21.68% relative to control, compared with LPS+V1a), whereas CREB sense and random oligonucleotides had no effect (Fig. 6, compare LPS+V1a with S+LPS+V1a or R+LPS+V1a).
TNF-α level in astrocyte medium after V1 agonist treatment was also investigated using ELISA (Fig. 7). Statistical analysis of TNF-α relative to control is shown in Figure 7 and is representative of three independent experiments. V1 agonist significantly decreased TNF-α peptide level in the medium (37.94 ± 8.71% relative to control, *p < 0.05 compared with control) and significantly reversed LPS induction of TNF-α from ∼100 to 50 pg/ml (98.19 ± 0.82% relative to control; +p < 0.05 compared with LPS alone). CREB antisense completely abolished V1 agonist-induced TNF-α peptide level decrease (AS+V1a, 90.80 ± 11.57% relative to control, compared with V1a), whereas CREB sense and random oligonucleotide had no effect (compare V1a with S+V1a or R+V1a). Similarly, CREB antisense completely abolished V1 agonist inhibition of LPS induction of TNF-α peptide (AS+LPS+V1a, 185.43 ± 16.10% relative to control, compared with LPS+V1a), whereas CREB sense and random oligonucleotides had no impact on the V1 agonist effect (Fig. 7, compare LPS+V1a with S+LPS+V1a or R+LPS+V1a).
Figure 7.
V1 agonist-induced decrease of TNF-α detected in the medium of cortical astrocytes and its dependence on CREB activation. Astrocytes were treated according to the indicated conditions for 24 hr followed by medium collection and ELISA analysis on TNF-α. Results are expressed as mean ± SEM percentage change of TNF-α level in the medium relative to control (CTRL) and are representative of three separate experiments. n = 3 for each condition; *p < 0.05 versus control; +p < 0.05 versus LPS-treated culture. The measured value for the control TNF-α level in the medium was 48.58 ± 2.95 pg/ml.
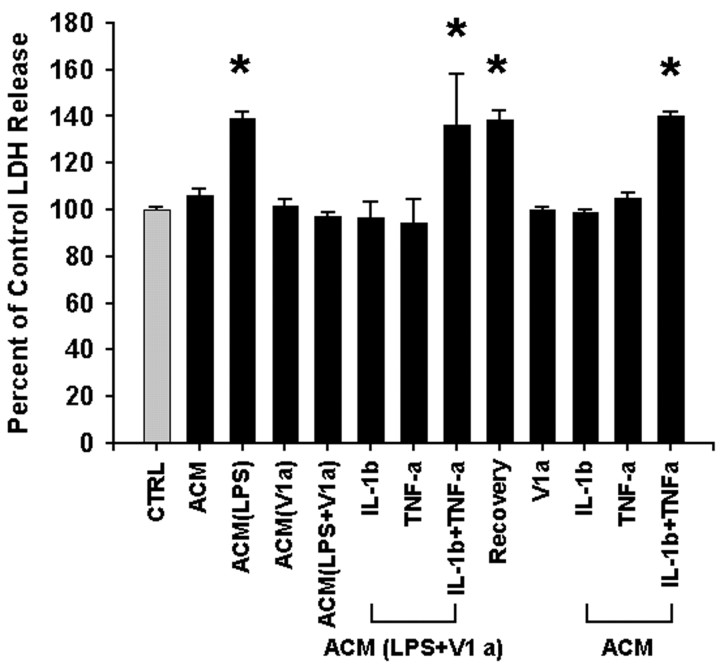
Impact of decreased cytokine release from astrocytes on cortical neuronal survival
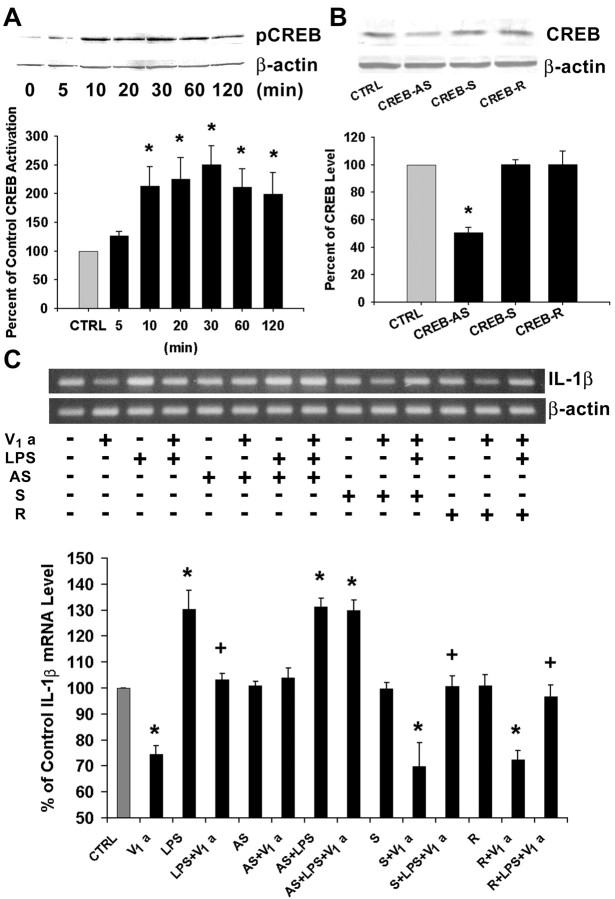
To determine the impact of reduced astrocyte cytokine release on neuronal survival, ACM was harvested and applied to cortical neurons followed by assessment of LDH release to determine the plasma membrane integrity of neurons. LDH is a stable cytoplasmic enzyme present in all cells, including neurons, and is rapidly released into media after plasma membrane damage. Cortical astrocytes were treated with LPS and V1 agonist for 24 hr. ACM was then harvested and applied to cortical neurons for 24 hr (Fig. 8). After treatment with LPS-treated ACM, LDH release in neuronal medium was significantly increased compared with control (139.29 ± 2.50%; *p < 0.05 compared with control), which was reversed by treatment with medium collected from LPS+V1 agonist-treated astrocytes (101.44 ± 3.02% relative to control). To determine whether this neuroprotection exerted by V1 agonist was attributable to reduced cytokine release from astrocytes, IL-1β (125 pg/ml) and TNF-α (50 pg/ml) were added to cortical neurons together with LPS+V1 agonist-treated ACM. The doses of IL-1β and TNF-α were chosen on the basis of the ELISA data showing V1 agonist-reduced IL-1β release by 125 pg/ml and TNF-α release by 50 pg/ml. IL-1β or TNF-α alone had no impact on the neuroprotective effect of V1 agonist, whereas the combination of these two proinflammatory cytokines was able to reverse the V1 agonist-induced neuroprotection (136.53 ± 21.41% relative to control; *p < 0.05 compared with control), indicating a synergistic effect of IL-1β and TNF-α. To investigate whether neurons can recover from IL-1β plus TNF-α-caused toxicity, cortical neurons were treated with LPS+V1a-treated astrocyte-conditioned medium supplemented with IL-1β plus TNF-α for 24 hr, and then the medium was changed to ACM without cytokines, and neurons were incubated for an additional 24 hr. Figure 8 indicates that removing cytokines after 24 hr of cytokine presence does not rescue the neurons from neurotoxicity (138.46 ± 4.23% relative to control; *p < 0.05 compared with control). Furthermore, astrocytes were also treated with V1 agonist alone, ACM+IL-1β, ACM+TNF-α, and ACM+IL-1β+TNF-α as controls. Results from these control experiments show that V1 agonist alone, ACM+IL-1β, or ACM+TNF-α did not have any significant impact on LDH release compared with control-treated neurons, although the combination of the two cytokines, ACM+IL-1β+TNF-α, caused significant increase in cell membrane damaged evidenced by increased LDH release (140.43 ± 1.37% relative to control; *p < 0.05 compared with control). These results confirm our conclusion that IL-1β or TNF-α alone is not neurotoxic, although the combination of IL-1β and TNF-α exert significant toxicity to primary cortical neurons. These results also serve as controls to validate our conclusion that the V1 agonist-induced decrease of cytokine release from cortical astrocytes was shown to be neuroprotective in cortical neurons.
Figure 8.
LDH analysis demonstrating neuroprotective effect of V1 agonist-induced suppression of IL-1β and TNF-α against LPS-treated ACM. Cortical neurons grown in 24-well plates were treated with ACM collected from LPS and V1 agonist-treated cortical astrocytes followed by LDH release analysis to determine the plasma integrity of neurons. Results are expressed as mean ± SEM percentage of control (CTRL) LDH release and are representative of three separate experiments. LPS-treated ACM induced significantly higher LDH release than control, which was reversed by medium collected from LPS+V1 agonist-treated astrocytes. Addition of IL-1β (125 pg/ml) or TNF-α (50 pg/ml) alone to neuronal cultures, together with LPS+V1 agonist-treated ACM, had no effect on V1 agonist-induced neuroprotection, whereas the combination of IL-1β and TNF-α reversed it. Neurons did not recover from IL-1β+TNF-α-induced cytotoxicity after cytokine removal. n = 12 per condition; *p < 0.05 compared with control cultures.
Besides LDH release, apoptotic cell death in response to ACM was determined. TUNEL staining was used to detect DNA damage in neurons undergoing apoptotic cell death. In addition, DAPI was used to label neuronal nuclei to quantitate the total number of neurons in the field (Fig. 9). Fluorescent images of TUNEL staining show that LPS-treated ACM induced a marked increase in the number of neurons undergoing apoptosis. The increase in apoptotic cell death was blocked by V1 agonist in that LPS+V1 agonist-treated ACM completely reversed the apoptotic effect of LPS-treated ACM. To determine whether V1 agonist-induced prevention of apoptosis is attributable to reduced cytokine release from astrocytes, IL-1β (125 pg/ml) and TNF-α (50 pg/ml) were added to cortical neurons together with LPS+V1 agonist-treated ACM followed by TUNEL analysis of apoptotic cell death. IL-1β or TNF-α alone had no impact on V1 agonist-induced neuroprotection, whereas the combination of these two proinflammatory cytokines synergistically reversed V1 agonist-induced prevention of neuronal apoptosis. Removing cytokines after 24 hr of cytokine presence does not rescue the neurons from neurotoxicity.
Figure 9.
TUNEL analysis demonstrating neuroprotective effect of V1 agonist-induced suppression of IL-1β and TNF-α against LPS-treated astrocyte-conditioned medium. Cortical neurons grown on 4-well chamber slides were treated with LPS and V1 agonist-treated ACM, and then neuronal apoptotic cell death was determined using fluorescent TUNEL analysis. Neuronal nuclei were labeled with DAPI to quantitate total number of neurons. Medium collected from LPS-treated astrocytes induced massive apoptotic cell death, which was reversed by medium collected from LPS+V1 agonist-treated astrocytes. When the proinflammatory cytokines IL-1β (125 pg/ml) and TNF-α (50 pg/ml) were added to neuronal cultures, together with LPS+V1 agonist-treated ACM, they alone had no impact on V1 agonist-induced prevention of apoptotic cell death, whereas the combination of IL-1β and TNF-α reversed the neuroprotective effect of V1 agonist. Removing cytokines after 24 hr did not recover the cells from cytotoxicity. CTRL, Control. Scale bar, 50 μm.
Discussion
In the present study, we pursued the functional significance of the complex signaling cascade activated by V1 agonist in astrocytes by investigating the impact of V1 agonist on the immune function of astrocytes, focusing on regulation of inflammatory cytokine production in astrocytes. Results of these analyses indicate that V1 agonist suppresses IL-1β and TNF-α expression at both mRNA and secreted peptide levels, which requires upstream activation of transcription factor CREB. Furthermore, reduced IL-1β and TNF-α release from astrocytes was shown to be neuroprotective against LPS inflammatory insults. This study provides a functional consequence of the V1 agonist-activated Ca2+ and kinase complex signaling cascade that leads to CREB activation in astrocytes (Zhao and Brinton, 2002, 2003). Specifically, results of this investigation indicate that V1 agonist acts as an immune modulator to repress proinflammatory cytokine expression in astrocytes and suggest that V1 agonist could exert an anti-inflammatory effect in vivo.
On the basis of our findings, vasopressin, a neuropeptide hormone, can be added to the growing list of neuropeptides and hormones that modulate the immune responses in the CNS. Thus far, that list of peptide immune regulators includes vasoactive intestinal peptide (VIP) and the pituitary adenylate cyclase-activating polypeptide (PACAP), the primary immunomodulatory function of which is also anti-inflammatory in nature. VIP and PACAP have been found to suppress LPS-induced production of proinflammatory cytokines TNF-α and IL-6 (Delgado et al., 1998). There are other hormones that also exert an immunomodulatory function in the CNS, such as estrogen. Estrogen exhibits anti-inflammatory effects on immune cells and prevents LPS-induced inflammatory response in the brain (Bruce-Keller et al., 2000; Vegeto et al., 2001).
Potential functional implications of V1 agonist-induced suppression of IL-1β and TNF-α in astrocytes
The finding of V1 agonist suppression of proinflammatory cytokine production suggests that V1 agonist is a potential direct immunosuppressive and anti-inflammatory molecule in the CNS. To understand the potential functional implications of cytokine suppression, a brief discussion of the role of IL-1β and TNF-α in the brain is provided.
IL-1β and TNF-α are intimately associated with elements of the acute phase immune responses, including fever, and are responsible for LPS (a potent bacteria-derived pyrogen)-induced fever (Saigusa, 1990; Luheshi et al., 1997; Luheshi, 1998). This is of particular interest because vasopressin functions as an antipyretic peptide (Naylor et al., 1988; Pittman and Wilkinson, 1992; Pittman et al., 1998). Pittman and colleagues found that injection or infusion of exogenous vasopressin into ventral septal area or central medial amygdala reduces fever in most mammals (Cooper et al., 1979a,b; Federico et al., 1992). Our demonstration of V1 agonist suppression of proinflammatory cytokines IL-1β and TNF-α therefore provides a potential mechanism underlying vasopressin-mediated antipyretic effect. Of equal interest, Pittman et al. (1998) also found that IL-1β is a potent stimulator for vasopressin release to activate an antipyretic pathway (Wilkinson et al., 1994), forming a negative feedback loop.
Expression of cytokine genes IL-1β and TNF-α has been linked to diverse forms of brain injury and neurodegeneration. Results from the current study showed that IL-1β and TNF-α synergistically induce neuronal cell death in vitro, consistent with other reports that exogenous addition of IL-1β and TNF-α causes neurotoxicity (Chao et al., 1995; Yamasaki et al., 1995; Barone et al., 1997; Hu et al., 1997; Zhao et al., 2001). Conversely, inhibition of IL-1β and TNF-α dramatically reduces the damages (Loddick and Rothwell, 1996; Barone et al., 1997; Nawashiro et al., 1997; Mayne et al., 2001). IL-1β and TNF-α are also associated with impairment of learning, memory, and cognition and are involved in the pathogenesis of a variety of neurodegenerative diseases including Alzheimer's disease (AD) and Parkinson's disease (PD). In AD patients, increased proinflammatory cytokines can cause increased amyloid precursor protein production and β-amyloid deposition (Griffin and Mrak, 2002). Immunocytochemical analyses have shown that these cytokines are closely associated with senile plaques (Mehlhorn et al., 2000). This is of particular interest given the increasing number of reports that show a beneficial effect of anti-inflammatory drugs on the progression of AD (McGeer and McGeer, 1995; Breitner, 1996). In PD, increased levels of IL-1β and TNF-α are also found in postmortem PD brains and in 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine or 6-OHDA-induced experimental PD animals (Boka et al., 1994; Mogi et al., 1994; Nagatsu et al., 2000). Together, these data suggest that reducing inflammatory cytokine production could be an effective therapeutic strategy for preventing or delaying the progression of these neurodegenerative disorders and diseases. However, despite consensus that cytokines themselves can be toxic, there has been controversy over whether or not LPS, via cytokine release, kills neurons in vivo. For example, studies published by Mouihate and Pittman (1998) indicated that it didn't, yet more recent studies have argued that it does (Shibata et al., 2003). These conflicting data are probably attributable to different animal species, or more importantly, different cytokine network environments. Cytokines interact with each other, and the spacial temporal expression patterns of different cytokines are pivotal in determining the impact of these cytokines in pathophysiology. Cytokines operate within a complex network and may act either synergistically or antagonistically and can influence the production of other cytokines. Therefore, more extensive studies on LPS neurotoxicity in vivo are needed, and therapeutic intervention against inflammatory cytokines should take into consideration the expression profile of other cytokines.
Autoimmune diseases such as multiple sclerosis (MS) are also associated with elevated levels of inflammatory cytokines. Examination of CSF and brain tissue from patients with MS has revealed dramatic elevation of IL-1β and TNF-α compared with controls (Merrill and Benveniste, 1996; Baranzini et al., 2000). Moreover, these cytokines can either directly cause oligodendrocyte injury and demyelination (Carrieri et al., 1992) or induce T cell activation, which leads to additional myelin sheath damage (Martino et al., 1998).
Stress is usually associated with activation of the hypothalamic-pituitary-adrenal (HPA) axis and suppressed immune function (Irwin, 1994; de Kloet, 2000). The long prevailing view proposes that activated HPA axis leads to increased secretion of corticotropin-releasing factor, which regulates ACTH secretion from pituitary. The endocrine action of ACTH, in turn, stimulates the release of adrenal stress hormone glucocorticoid, an immune suppressor. However, vasopressin secretion is also a typical constituent of the response to several types of stressors (Ebner et al., 1999; Altemus et al., 2001). The current finding of V1 agonist-suppressed cytokine production may be an alternative theory for suppressed immune function in stress situations.
Inflammatory cytokines are also implicated in a variety of psychiatric disorders such as schizophrenia, depressive disorders, and even autism. Increased production of inflammatory cytokines has been proposed to play a pivotal role in the pathogenesis of schizophrenia, possibly because of the activation of immune system in the CNS by these cytokines (Muller and Ackenheil, 1998). Both clinical and experimental studies indicate that depression is associated with increased concentrations of IL-1β and TNF-α in the CNS (Connor and Leonard, 1998). Interestingly, the plasma vasopressin level is increased in patients with major depression (van Londen et al., 1997), possibly acting via a negative-feedback mechanism by suppressing the production of proinflammatory cytokines. Autism (a pervasive developmental disorder characterized by the following: impairment of social interaction; language; restricted, repetitive, and stereotyped patterns of behavior; interests; and activities) has been hypothesized to be accompanied by activation of proinflammatory cytokines, which could contribute to the etiology of some autistic symptoms such as social withdrawal, suppression of exploratory behavior, sleep disturbances, and mood alterations (Croonenberghs et al., 2002).
CREB involvement in cytokine suppression
In the present study, CREB was found to be the pivotal transcription factor involved in V1 agonist suppression of IL-1β and TNF-α, which is consistent with findings from other laboratories. CRE-like promoter sequence is found in the promotor region of both IL-1β and TNF-α genes (Liu and Whisler, 1998; Perez et al., 1999). Suppression of LPS-induced IL-1β and TNF-α by N-acetyl-O-methyldopamine was found to be dependent on CREB activation (Cho et al., 2001). VIP- and PACAP-induced repression of TNF-α expression was also demonstrated to involve CREB (Delgado et al., 1998).
In conclusion, we demonstrated a novel anti-inflammatory role for V1 agonist in brain. We have shown that activation of the V1aR leads to suppression of five inflammatory cytokines. Detailed analysis of V1 agonist-induced suppression of two proinflammatory cytokines, IL-1β and TNF-α, demonstrated that the neuroprotective molecule V1 agonist suppresses IL-1β and TNF-α at both the mRNA and released peptide levels via a CREB-dependent mechanism, and that suppression of inflammatory cytokine suppression is neuroprotective. The potential therapeutic implications of V1 agonist as an anti-inflammatory agent are currently under investigation.
Footnotes
This work was supported by the Kenneth T. and Eileen L. Norris Foundation (R.D.B.).
Correspondence should be addressed to Dr. Roberta Diaz Brinton, Department of Molecular Pharmacology and Toxicology, Norris Foundation Laboratory for Neuroscience Research, Pharmaceutical Sciences Center, University of Southern California, 1985 Zonal Avenue, Los Angeles, CA 90089-9121. E-mail: rbrinton@hsc.usc.edu.
Copyright © 2004 Society for Neuroscience 0270-6474/04/242226-10$15.00/0
References
- Altemus M, Roca C, Galliven E, Romanos C, Deuster P (2001) Increased vasopressin and adrenocorticotropin responses to stress in the midluteal phase of the menstrual cycle. J Clin Endocrinol Metab 86: 2525-2530. [DOI] [PubMed] [Google Scholar]
- Baranzini SE, Elfstrom C, Chang SY, Butunoi C, Murray R, Higuchi R, Oksenberg JR (2000) Transcriptional analysis of multiple sclerosis brain lesions reveals a complex pattern of cytokine expression. J Immunol 165: 6576-6582. [DOI] [PubMed] [Google Scholar]
- Barone FC, Arvin B, White RF, Miller A, Webb CL, Willette RN, Lysko PG, Feuerstein GZ (1997) Tumor necrosis factor-alpha. A mediator of focal ischemic brain injury. Stroke 28: 1233-1244. [DOI] [PubMed] [Google Scholar]
- Black RA, Rauch CT, Kozlosky CJ, Peschon JJ, Slack JL, Wolfson MF, Castner BJ, Stocking KL, Reddy P, Srinivasan S, Nelson N, Boiani N, Schooley KA, Gerhart M, Davis R, Fitzner JN, Johnson RS, Paxton RJ, March CJ, Cerretti DP (1997) A metalloproteinase disintegrin that releases tumour-necrosis factor-alpha from cells. Nature 385: 729-733. [DOI] [PubMed] [Google Scholar]
- Boka G, Anglade P, Wallach D, Javoy-Agid F, Agid Y, Hirsch EC (1994) Immunocytochemical analysis of tumor necrosis factor and its receptors in Parkinson's disease. Neurosci Lett 172: 151-154. [DOI] [PubMed] [Google Scholar]
- Breitner JC (1996) The role of anti-inflammatory drugs in the prevention and treatment of Alzheimer's disease. Annu Rev Med 47: 401-411. [DOI] [PubMed] [Google Scholar]
- Bruce-Keller AJ, Keeling JL, Keller JN, Huang FF, Camondola S, Mattson MP (2000) Antiinflammatory effects of estrogen on microglial activation. Endocrinology 141: 3646-3656. [DOI] [PubMed] [Google Scholar]
- Carrieri PB, Maiorino A, Provitera V, Soscia E, Perrella O (1992) Cytokines in the pathogenesis of multiple sclerosis. Acta Neurol (Napoli) 14: 333-341. [PubMed] [Google Scholar]
- Cau P, Rougon-Rapuzzi G (1979) Autoimmune alterations in the neurohypophysis of rabbits immunized against vasopressin. Brain Res 177: 265-271. [DOI] [PubMed] [Google Scholar]
- Chao CC, Hu S, Ehrlich L, Peterson PK (1995) Interleukin-1 and tumor necrosis factor-alpha synergistically mediate neurotoxicity: involvement of nitric oxide and of N-methyl-d-aspartate receptors. Brain Behav Immun 9: 355-365. [DOI] [PubMed] [Google Scholar]
- Cho S, Kim Y, Cruz MO, Park EM, Chu CK, Song GY, Joh TH (2001) Repression of proinflammatory cytokine and inducible nitric oxide synthase (NOS2) gene expression in activated microglia by N-acetyl-O-methyldopamine: protein kinase A-dependent mechanism. Glia 33: 324-333. [DOI] [PubMed] [Google Scholar]
- Connor TJ, Leonard BE (1998) Depression, stress and immunological activation: the role of cytokines in depressive disorders. Life Sci 62: 583-606. [DOI] [PubMed] [Google Scholar]
- Cooper KE, Kasting NW, Lederis K, Veale WL (1979a) Evidence supporting a role for endogenous vasopressin in natural suppression of fever in the sheep. J Physiol (Lond) 295: 33-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper KE, Veale WL, Kasting N, Pittman QJ (1979b) Ontogeny of fever. Fed Proc 38: 35-38. [PubMed] [Google Scholar]
- Croonenberghs J, Bosmans E, Deboutte D, Kenis G, Maes M (2002) Activation of the inflammatory response system in autism. Neuropsychobiology 45: 1-6. [DOI] [PubMed] [Google Scholar]
- de Kloet ER (2000) Stress in the brain. Eur J Pharmacol 405: 187-198. [DOI] [PubMed] [Google Scholar]
- Delgado M, Munoz-Elias EJ, Kan Y, Gozes I, Fridkin M, Brenneman DE, Gomariz RP, Ganea D (1998) Vasoactive intestinal peptide and pituitary adenylate cyclase-activating polypeptide inhibit tumor necrosis factor alpha transcriptional activation by regulating nuclear factor-kB and cAMP response element-binding protein/c-Jun. J Biol Chem 273: 31427-31436. [DOI] [PubMed] [Google Scholar]
- Dinarello CA (1994) The interleukin-1 family: 10 years of discovery. FASEB J 8: 1314-1325. [PubMed] [Google Scholar]
- Dong Y (2001) Immune function of astrocytes. Glia 36: 180-190. [DOI] [PubMed] [Google Scholar]
- Ebner K, Wotjak CT, Holsboer F, Landgraf R, Engelmann M (1999) Vasopressin released within the septal brain area during swim stress modulates the behavioural stress response in rats. Eur J Neurosci 11: 997-1002. [DOI] [PubMed] [Google Scholar]
- Federico P, Veale WL, Pittman QJ (1992) Vasopressin-induced antipyresis in the medial amygdaloid nucleus of conscious rats. Am J Physiol 262: R901-R908. [DOI] [PubMed] [Google Scholar]
- Griffin WS, Mrak RE (2002) Interleukin-1 in the genesis and progression of and risk for development of neuronal degeneration in Alzheimer's disease. J Leukoc Biol 72: 233-238. [PMC free article] [PubMed] [Google Scholar]
- Guzowski JF, McGaugh JL (1997) Antisense oligodeoxynucleotide-mediated disruption of hippocampal cAMP response element binding protein levels impairs consolidation of memory for water maze training. Proc Natl Acad Sci USA 94: 2693-2698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu S, Peterson PK, Chao CC (1997) Cytokine-mediated neuronal apoptosis. Neurochem Int 30: 427-431. [DOI] [PubMed] [Google Scholar]
- Irwin M (1994) Stress-induced immune suppression: role of brain corticotropin releasing hormone and autonomic nervous system mechanisms. Adv Neuroimmunol 4: 29-47. [DOI] [PubMed] [Google Scholar]
- Konradi C, Heckers S (1995) Haloperidol-induced Fos expression in striatum is dependent upon transcription factor cyclic AMP response element binding protein. Neuroscience 65: 1051-1061. [DOI] [PubMed] [Google Scholar]
- Konradi C, Cole RL, Heckers S, Hyman SE (1994) Amphetamine regulates gene expression in rat striatum via transcription factor CREB. J Neurosci 14: 5623-5634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu B, Whisler RL (1998) Transcriptional activation and redox regulation of the tumor necrosis factor-alpha promoter in human T cells: role of the CRE/kappa3 promoter region. J Interferon Cytokine Res 18: 999-1007. [DOI] [PubMed] [Google Scholar]
- Loddick SA, Rothwell NJ (1996) Neuroprotective effects of human recombinant interleukin-1 receptor antagonist in focal cerebral ischaemia in the rat. J Cereb Blood Flow Metab 16: 932-940. [DOI] [PubMed] [Google Scholar]
- Luheshi GN (1998) Cytokines and fever. Mechanisms and sites of action. Ann NY Acad Sci 856: 83-89. [DOI] [PubMed] [Google Scholar]
- Luheshi GN, Stefferl A, Turnbull AV, Dascombe MJ, Brouwer S, Hopkins SJ, Rothwell NJ (1997) Febrile response to tissue inflammation involves both peripheral and brain IL-1 and TNF-alpha in the rat. Am J Physiol 272: R862-868. [DOI] [PubMed] [Google Scholar]
- Martino G, Grohovaz F, Brambilla E, Codazzi F, Consiglio A, Clementi E, Filippi M, Comi G, Grimaldi LM (1998) Proinflammatory cytokines regulate antigen-independent T-cell activation by two separate calcium-signaling pathways in multiple sclerosis patients. Ann Neurol 43: 340-349. [DOI] [PubMed] [Google Scholar]
- Mayne M, Ni W, Yan HJ, Xue M, Johnston JB, Del Bigio MR, Peeling J, Power C (2001) Antisense oligodeoxynucleotide inhibition of tumor necrosis factor-alpha expression is neuroprotective after intracerebral hemorrhage. Stroke 32: 240-248. [DOI] [PubMed] [Google Scholar]
- McGeer PL, McGeer EG (1995) The inflammatory response system of brain: implications for therapy of Alzheimer and other neurodegenerative diseases. Brain Res Brain Res Rev 21: 195-218. [DOI] [PubMed] [Google Scholar]
- Mehlhorn G, Hollborn M, Schliebs R (2000) Induction of cytokines in glial cells surrounding cortical beta-amyloid plaques in transgenic Tg2576 mice with Alzheimer pathology. Int J Dev Neurosci 18: 423-431. [DOI] [PubMed] [Google Scholar]
- Melis MR, Stancampiano R, Argiolas A (1993) Oxytocin- and vasopressin-like immunoreactivity in the rat thymus: characterization and possible involvement in the immune response. Regul Pept 45: 269-272. [DOI] [PubMed] [Google Scholar]
- Merrill JE, Benveniste EN (1996) Cytokines in inflammatory brain lesions: helpful and harmful. Trends Neurosci 19: 331-338. [DOI] [PubMed] [Google Scholar]
- Mogi M, Harada M, Riederer P, Narabayashi H, Fujita K, Nagatsu T (1994) Tumor necrosis factor-alpha (TNF-alpha) increases both in the brain and in the cerebrospinal fluid from parkinsonian patients. Neurosci Lett 165: 208-210. [DOI] [PubMed] [Google Scholar]
- Moss ML, Jin SL, Milla ME, Bickett DM, Burkhart W, Carter HL, Chen WJ, Clay WC, Didsbury JR, Hassler D, Hoffman CR, Kost TA, Lambert MH, Leesnitzer MA, McCauley P, McGeehan G, Mitchell J, Moyer M, Pahel G, Rocque W, et al. (1997) Cloning of a disintegrin metalloproteinase that processes precursor tumour-necrosis factor-alpha. Nature 385: 733-736. [DOI] [PubMed] [Google Scholar]
- Mouihate A, Pittman QJ (1998) Lipopolysaccharide-induced fever is dissociated from apoptotic cell death in the rat brain. Brain Res 805: 95-103. [DOI] [PubMed] [Google Scholar]
- Muller N, Ackenheil M (1998) Psychoneuroimmunology and the cytokine action in the CNS: implications for psychiatric disorders. Prog Neuropsychopharmacol Biol Psychiatry 22: 1-33. [DOI] [PubMed] [Google Scholar]
- Murphy DD, Segal M (1997) Morphological plasticity of dendritic spines in central neurons is mediated by activation of cAMP response element binding protein. Proc Natl Acad Sci USA 94: 1482-1487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagatsu T, Mogi M, Ichinose H, Togari A (2000) Changes in cytokines and neurotrophins in Parkinson's disease. J Neural Transm Suppl 60: 277-290. [DOI] [PubMed] [Google Scholar]
- Nawashiro H, Martin D, Hallenbeck JM (1997) Inhibition of tumor necrosis factor and amelioration of brain infarction in mice. J Cereb Blood Flow Metab 17: 229-232. [DOI] [PubMed] [Google Scholar]
- Naylor AM, Pittman QJ, Veale WL (1988) Stimulation of vasopressin release in the ventral septum of the rat brain suppresses prostaglandin E1 fever. J Physiol (Lond) 399: 177-189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nikcevich KM, Gordon KB, Tan L, Hurst SD, Kroepfl JF, Gardinier M, Barrett TA, Miller SD (1997) IFN-gamma-activated primary murine astrocytes express B7 costimulatory molecules and prime naive antigen-specific T cells. J Immunol 158: 614-621. [PubMed] [Google Scholar]
- Perez RL, Ritzenthaler JD, Roman J (1999) Transcriptional regulation of the interleukin-1beta promoter via fibrinogen engagement of the CD18 integrin receptor. Am J Respir Cell Mol Biol 20: 1059-1066. [DOI] [PubMed] [Google Scholar]
- Pittman QJ, Wilkinson MF (1992) Central arginine vasopressin and endogenous antipyresis. Can J Physiol Pharmacol 70: 786-790. [DOI] [PubMed] [Google Scholar]
- Pittman QJ, Chen X, Mouihate A, Hirasawa M, Martin S (1998) Arginine vasopressin, fever and temperature regulation. Prog Brain Res 119: 383-392. [DOI] [PubMed] [Google Scholar]
- Raetz CR, Whitfield C (2002) Lipopolysaccharide endotoxins. Annu Rev Biochem 71: 635-700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saigusa T (1990) Participation of interleukin-1 and tumor necrosis factor in the responses of the sympathetic nervous system during lipopolysaccharide-induced fever. Pflügers Arch 416: 225-229. [DOI] [PubMed] [Google Scholar]
- Shibasaki T, Hotta M, Sugihara H, Wakabayashi I (1998) Brain vasopressin is involved in stress-induced suppression of immune function in the rat. Brain Res 808: 84-92. [DOI] [PubMed] [Google Scholar]
- Shibata H, Katsuki H, Nishiwaki M, Kume T, Kaneko S, Akaike A (2003) Lipopolysaccharide-induced dopaminergic cell death in rat midbrain slice cultures: role of inducible nitric oxide synthase and protection by indomethacin. J Neurochem 86: 1201-1212. [DOI] [PubMed] [Google Scholar]
- Sternberg EM (1997) Neural-immune interactions in health and disease. J Clin Invest 100: 2641-2647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Londen L, Goekoop JG, van Kempen GM, Frankhuijzen-Sierevogel AC, Wiegant VM, van der Velde EA, De Wied D (1997) Plasma levels of arginine vasopressin elevated in patients with major depression. Neuropsychopharmacology 17: 284-292. [DOI] [PubMed] [Google Scholar]
- Vegeto E, Bonincontro C, Pollio G, Sala A, Viappiani S, Nardi F, Brusadelli A, Viviani B, Ciana P, Maggi A (2001) Estrogen prevents the lipopolysaccharide-induced inflammatory response in microglia. J Neurosci 21: 1809-1818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White DM, Walker S, Brenneman DE, Gozes I (2000) CREB contributes to the increased neurite outgrowth of sensory neurons induced by vasoactive intestinal polypeptide and activity-dependent neurotrophic factor. Brain Res 868: 31-38. [DOI] [PubMed] [Google Scholar]
- Wilkinson MF, Horn TF, Kasting NW, Pittman QJ (1994) Central interleukin-1 beta stimulation of vasopressin release into the rat brain: activation of an antipyretic pathway. J Physiol (Lond) 481: 641-646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong GH, Bartlett PF, Clark-Lewis I, Battye F, Schrader JW (1984) Inducible expression of H-2 and Ia antigens on brain cells. Nature 310: 688-691. [DOI] [PubMed] [Google Scholar]
- Yamasaki Y, Matsuura N, Shozuhara H, Onodera H, Itoyama Y, Kogure K (1995) Interleukin-1 as a pathogenetic mediator of ischemic brain damage in rats. Stroke 26: 676-680. [DOI] [PubMed] [Google Scholar]
- Yirmiya R, Shavit Y, Ben-Eliyahu S, Martin FC, Weiner H, Liebeskind JC (1989) Natural killer cell activity in vasopressin-deficient rats (Brattleboro strain). Brain Res 479: 16-22. [DOI] [PubMed] [Google Scholar]
- Zhao L, Brinton RD (2002) Vasopressin-induced cytoplasmic and nuclear calcium signaling in cultured cortical astrocytes. Brain Res 943: 117-131. [DOI] [PubMed] [Google Scholar]
- Zhao L, Brinton RD (2003) Vasopressin-induced cytoplasmic and nuclear calcium signaling in embryonic cortical astrocytes: dynamics of calcium and calcium-dependent kinase translocation. J Neurosci 23: 4228-4239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao L, Chen S, Brinton RD (2003) An estrogen replacement therapy containing nine synthetic plant-based conjugated estrogens promotes neuronal survival. Exp Biol Med (Maywood) 228: 823-835. [DOI] [PubMed] [Google Scholar]
- Zhao X, Bausano B, Pike BR, Newcomb-Fernandez JK, Wang KK, Shohami E, Ringger NC, DeFord SM, Anderson DK, Hayes RL (2001) TNF-alpha stimulates caspase-3 activation and apoptotic cell death in primary septo-hippocampal cultures. J Neurosci Res 64: 121-131. [DOI] [PubMed] [Google Scholar]