Reann’s story
“When I first heard that I could share doing some of my own hemodialysis, I was scared and thought I could never do that! Despite my initial fear, I have learned how to needle. I found this rewarding and now I am in control. I have a lot less issues with my fistula now and I can get on with my dialysis without waiting for the nursing staff.”
Nicholas’ story
“Shared Care means a better way of life for me and my family. It has given me understanding so that I know what is happening during my dialysis helping me control my diet and fluids better. I have become much more confident and am less anxious than before.”
Introduction
Since hemodialysis (HD) has been available to treat ESKD, patients have had the choice to undertake it in their own home. Home HD has excellent outcomes providing considerable reassurance that it is safe for people to be trained to perform their own treatments. Despite this success, most dialysis patients receive it at centers where it is not standard procedure for people to train to manage their own care. Importantly, there is good evidence that people with long term conditions who are more involved in their own care, have better outcomes (1). In this article we explore a quality improvement program in the UK that has as its goal to increase the proportion of people who dialyze at centers who are consistently given the opportunity and choice to learn about and participate in their own treatment thereby aligning with the principles of person centered care (2). This program was coproduced with patients who coined the term “Shared Hemodialysis Care.”
Shared Hemodialysis Care
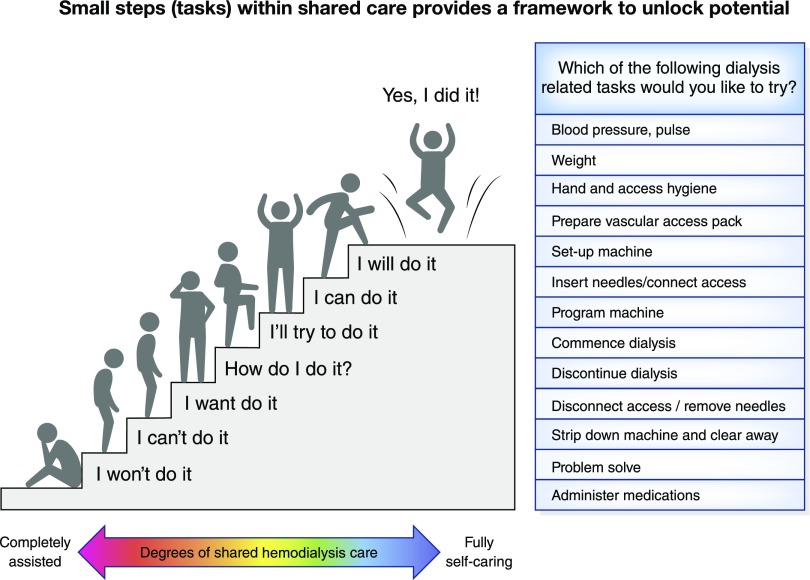
This is where the health care team offers the choice, support and training for patients to participate in the tasks related to their hemodialysis treatment to the extent that they wish. HD is broken down into approximately 14 component tasks, and the progress of training is documented from novice to expert using a competency record underpinned by specifically designed educational materials (3). Patients are able to participate and learn at different rates and individual preferences are acknowledged. Many start with the simpler tasks such as performing observations, building self-confidence to move onto the more complex, whereas others engage in those from the outset. At first, the thought of undertaking tasks normally carried out by the health care team may be overwhelming to the patient, and yet with support and by starting with small steps, people learn as much as they are comfortable with, gaining mastery over time (illustrated in Figure 1). In parallel, nurses receive training to develop their confidence and skills as facilitators.
Figure 1.
Small steps (tasks) within shared care provides a framework to unlock potential. Illustrates the stepwise approach that can be taken to Shared Hemodialysis Care. Patients can start with small tasks and do as much or as little as they feel able. As they learn, confidence is built.
Patient Activation
The Patient Activation Measure assesses a spectrum that ranges from the lowest level, where the individual is overwhelmed by their disease and disengaged, through to higher levels where they take a degree of control for their own health (1). Among kidney patients, those with lower activation levels tend to be older, more likely to be on HD and have higher levels of deprivation (4). Furthermore, levels of activation tend to be low among people who have a combination of diabetes and CKD (5). Patients with diabetes who have lower levels of activation attend more frequently at emergency departments and are more likely to be hospitalized (6). There is, therefore, interest in developing interventions that have the potential to increase patient activation among those attending center-based HD and to determine whether this approach improves outcomes.
Shared hemodialysis care aims to do this by supporting people with low levels of activation to engage with simple dialysis related tasks so that they begin to gain the confidence and move from being overwhelmed by their illness to greater independence (Figure 1). The stories presented here give the perspectives of two patients involved in Shared Hemodialysis Care. Reann describes how the program helped her to overcome her fears to undertake self-cannulation (needling) and that this gave her a greater sense of control. Nicholas highlights the benefits that learning has had on his ability to manage his diet and fluids, as well as leading to improved confidence and reduced anxiety. Nursing staff value shared care because they quickly see how they can improve their patients’ experience of HD through small changes.
Scaling up Shared Hemodialysis Care
With support from the Health Foundation and UK kidney charities (Kidney Research UK and Kidney Care UK), a quality improvement collaborative of health care teams with their patients was developed to scale up shared hemodialysis care across 12 hospital trusts in England. This involved a series of learning events at which mechanisms of engagement were tested and shared between participants. Quality improvement focused on how choice was consistently given and examined the variation in tasks that were learned. Patients participated as equal partners in the design and delivery of the program.
A 2 year, randomized, stepped-wedge cohort study of the intervention involving 600 patients conducted at the 12 centers was completed and will report results during 2019 (A quality improvement collaborative to scale up Shared Hemodialysis Care for patients on centre based hemodialysis [SHAREHD]) (7). Baseline cross-sectional data from that study confirmed a positive association between the number of dialysis related tasks that patients undertook and individual levels of patient activation (8). During the program a number of patients who participated in shared hemodialysis care moved on to dialyze at home. For many, being able to engage more in the center enhanced their experience of care and enabled greater independence even if home dialysis was not a choice they wished to pursue. It became clear that certain treatment-related tasks provide the gateway to home or independent dialysis and one of these is self-cannulation. Evidence that there is the potential to increase the number of people who self-cannulate comes from a UK study of 189 center-based dialysis patients where 29% felt they could consider self-cannulation with a further 14% considering they could do so with help (9).
Shared hemodialysis care is a simple concept but a complex intervention. It requires a change in health care delivery that moves from a model of provision of treatment to one that is responsive and facilitates training in order to meet individual needs and preferences, enabling self-management. A qualitative evaluation of its implementation at Sheffield and York documented a spectrum of barriers and enablers that were context dependent. Organizational aspects of the dialysis unit interact with unit culture to provide opportunities or otherwise for individuals to develop skills and abilities in a supportive environment (10). No one method suits all units although there are common themes.
Conclusions
Consistently supporting people who dialyze at centers to learn and take on treatment-related tasks provides a practical method of engaging and educating patients in their own care. This has the potential to improve patient experience, benefit patient activation and outcomes. It provides a more equitable service, by giving all individuals the opportunity to learn about their condition irrespective of whether home dialysis is an option for them, increasing opportunities for self-management. Central to this model is patient engagement that is linked to confidence and choice driving motivation to learn. The SHAREHD study will provide evidence of how this works across a range of dialysis environments and for people with different personal characteristics (7).
Disclosures
Ms. Barnes and Dr. Wilkie have nothing to disclose.
Funding
Ms. Barnes reports receiving grants from Kidney Care UK during the conduct of the study. Dr. Wilkie received grants from the Health Foundation during the conduct of the study.
Acknowledgments
The authors would like to thank the researchers, health care teams and patients who participated in ShareHD.
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
References
- 1.Greene J, Hibbard JH, Sacks R, Overton V, Parrotta CD: When patient activation levels change, health outcomes and costs change, too. Health Aff (Millwood) 34: 431–437, 2015 [DOI] [PubMed] [Google Scholar]
- 2.Morton RL, Sellars M: From patient-centered to person-centered care for kidney diseases. Clin J Am Soc Nephrol 14: 623–625, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.NHS England and the UK Renal Registry. Available at: https://www.thinkkidneys.nhs.uk/kquip/hub/sharehd/. Accessed May 4, 2019
- 4.Gair R, Wong E, Stannard C, Van der Veer S, Farrington K, Fluck R: Associations between patient activation, characteristics and outcomes. Nephrol Dial Transplant 33[Suppl 1]: i153–i4, 2018 [Google Scholar]
- 5.Zimbudzi E, Lo C, Ranasinha S, Fulcher GR, Jan S, Kerr PG, Polkinghorne KR, Russell G, Walker RG, Zoungas S: Factors associated with patient activation in an Australian population with comorbid diabetes and chronic kidney disease: A cross-sectional study. BMJ Open 7: e017695, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Begum N, Donald M, Ozolins IZ, Dower J: Hospital admissions, emergency department utilisation and patient activation for self-management among people with diabetes. Diabetes Res Clin Pract 93: 260–267, 2011 [DOI] [PubMed] [Google Scholar]
- 7.Fotheringham J, Barnes T, Dunn L, Lee S, Ariss S, Young T, Walters SJ, Laboi P, Henwood A, Gair R, Wilkie M: Rationale and design for SHAREHD: A quality improvement collaborative to scale up shared haemodialysis care for patients on centre based haemodialysis. BMC Nephrol 18: 335, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Fotheringham J, Barnes T, Dunn L, Lee S, Ariss S, Young T, et al. The relationship between patient activation and self-performed treatment related tasks among patients receiving in-centre haemodialysis: The ShareHD cohort study. UK Kidney Week; Harrogate, UK, 2018.
- 9.Jayanti A, Foden P, Wearden A, Morris J, Brenchley P, Mitra S; BASIC-HHD Study Group: Self-cannulation for haemodialysis: Patient attributes, clinical correlates and self-cannulation predilection models. PLoS One 10: e0125606, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Glidewell L, Boocock S, Pine K, Campbell R, Hackett J, Gill S, Wilkie M; Yorkshire and Humber Shared Haemodialysis Care team: Using behavioural theories to optimise shared haemodialysis care: A qualitative intervention development study of patient and professional experience. Implement Sci 8: 118, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]