Abstract
Background
Little is known about the patterns of development assistance (DA) for each component of reproductive, maternal, newborn, child and adolescent health (RMNCAH) in conflict-affected countries nor about the DA allocation in relation to the burden of disease.
Methods
We tracked DA to RMNCAH in general and to each of its four components: reproductive health (RH), maternal and newborn health (MNH), child health (CH) and adolescent health (AH), in 25 conflict-affected countries between 2003 and 2017. We compared DA and disability-adjusted life years (DALYs) for each component. Using keyword searching and funding allocation methods, we produced two sets of estimates: DA primarily targeting RMNCAH (lower bound) and DA both primarily and partially for RMNCAH or DA not explicitly targeting RMNCAH but benefiting it (upper bound).
Findings
Between 2003 and 2017, we identified 46 833 projects among the 25 countries that targeted RMNCAH. During the study period, DA to RMNCAH increased by seven-fold from $0.5 billion to $3.6 billion, with a slowdown since 2013. Cumulatively, RH received the largest proportion of DA to RMNCAH (50%) with 84% of its funding earmarked for HIV/AIDS, which contributed to less than 6% of the total RMNCAH-related DALYs. AH received 3% of the DA-RMNCAH but contributed 15% to the RMNCAH-related DALYs. Non-communicable diseases caused more than one-third of the DALYs among adolescents, but received only 3% of DA to AH. RMNCAH-inclusive estimates showed consistent results.
Conclusion
While there was a substantial increase in funding to RMNCAH in conflict-affected countries over the period of study, some health issues with high disease burden (eg, AH and non-communicable diseases) received a disproportionately small portion of aid for RMNCAH. We recommend that donors increase investment to RMNCAH in conflict-affected countries, particularly in areas where the burden of disease or the potential benefit of investment is likely to be high.
Keywords: development assistance; reproductive, maternal, newborn, child, and adolescent health; conflict-affected countries; burden of disease
Key questions.
What is already known?
Conflict-affected countries frequently lack well-functioning local health system and are heavily dependent on foreign development assistance (DA) for health service provision.
Studies with special focus on health aid in conflict-affected countries found an increasing amount of DA in these countries, mainly due to increase in HIV/AIDS.
What are the new findings?
DA to reproductive, maternal, newborn, child and adolescent health (RMNCAH) increased substantially by seven-fold from $0.5 billion to $3.6 billion between 2003 and 2017, with a slower growth since 2013.
Reproductive health received the largest proportion of DA to RMNCAH (50%), followed by child health (30%), maternal and newborn heath (18%) and adolescent health (2%).
HIV/AIDs remained to be the focus of donors, accounting for two-fifths of DA to RMNCAH in 2017 while contributing to less than 6% of the total RMNCAH-related DALYs. Adolescent health received 3% of the DA-RMNCAH but contributed 15% to the RMNCAH-related DALYs.
Non-communicable diseases (NCDs) caused the large amount of DALYs (36%) among adolescents in 2017, but received the lowest proportion of DA.
What do the new findings imply?
More funds are needed in health areas with high disease burden (eg, adolescent health and NCDs) but little attention from donors in the conflicted countries.
Introduction
Reproductive, maternal, newborn, child and adolescent health (RMNCAH) are essential dimensions of survive and thrive, covering the largest proportion of the most vulnerable stages of life.1 2 Achieving progress in RMNCAH in conflict-affected areas is particularly challenging due to fragile political, economic and health systems.3 Conflict-affected countries account for a disproportionate morbidity burden. The 25 in-conflict and post-conflict countries (in-conflict and post-conflict countries include Afghanistan, Angola, Burundi, Chad, Central African Republic, Colombia, Democratic Republic of the Congo, Eritrea, Iraq, Liberia, Libya, Myanmar, Nepal, Nigeria, Pakistan, Sierra Leone, Somalia, Sri Lanka, South Sudan, Sudan, Syria, Timor-Leste, Uganda, Ukraine and Yemen) identified in this study accounted for less than one-tenth of the population in low-income and middle-income countries (LMICs), but contributed to 21.2% of disability-adjusted life years (DALYs) in LMICs. In 2017, RMNCAH comprised 34.2% of the total DALYs in these 25 conflict-affected countries, but only 20.1% at the global level and 25.8% in LMICs.4
Conflict-affected countries are known to often lack well-functioning health system with limited capacity to deal with common diseases, respond to infectious outbreaks and cope with the particularly high burden of mental illness.5 6 Women, children and adolescents are the ones most profoundly affected by conflicts because they constitute the major internally displaced population.7 8 RMNCAH in conflict-affected countries are heavily dependent on foreign development assistance (DA) for health service provision.9–11 Therefore, it is essential to assess the amount of DA donated to these countries, as well as to various health areas or specific diseases that contribute large proportion to the DALYs.
Previous studies by the Countdown and other groups have regularly tracked DA to reproductive, maternal, newborn and child health (RMNCH).12–22 Our previous study produced lower and upper bounds of the aid disbursed to RMNCH in fragile states (mostly conflict-affected countries) between 2000 and 2014.14 Two other studies also estimated DA to reproductive health (RH) in 18 conflict-affected countries between 2003 and 2011.9 10 This research extends the previous studies by tracking aid to the components of RMNCAH in conflict-affected countries, including RH, maternal and newborn health (MNH), child health (CH) and adolescent health (AH). Following previous studies,14 15 23 we produced lower and upper bound of estimates for RMNCAH and each of the four components. We also investigate the amount and share of DA in various health areas or diseases and compared that with their burden of disease.
Methods
Defining conflict-affected countries
Our focus was on countries that were either in conflicts or in postconflict stages between 2003 and 2017. Following previous practice,9 10 we defined conflict-affected countries as having been at ‘war’ at some point in the period 2000 to 2017 based on the Uppsala University Conflict Database.24 War is defined as major armed conflict in which there are over 1000 battle-related deaths in 1 year. As the conflicts could have ended by the studied period (2003 to 2017), the conflict-affected countries in the study include those that were either at war or in a postwar phase (the war occurred between 2000 and 2002 and ended before 2003). We identified 25 conflict-affected countries, including Afghanistan, Angola, Burundi, Chad, Central African Republic, Colombia, Democratic Republic of the Congo, Eritrea, Iraq, Liberia, Libya, Myanmar, Nepal, Nigeria, Pakistan, Sierra Leone, Somalia, Sri Lanka, South Sudan, Sudan, Syria, Timor-Leste, Uganda, Ukraine and Yemen (see appendix table 1).
bmjgh-2019-001614supp001.pdf (949KB, pdf)
Data sources
Aid data in this study were mostly extracted in January 2019 from the publicly accessible Creditor Reporting System (CRS) database for 2003–2017. Since CRS did not include disbursement data for 2003–2006 for the Global Alliance for Vaccines and Immunization (GAVI), we obtained it directly from the GAVI website.12 Following the CRS recommendation and previous studies,12 14 15 25 we did not use CRS data before 2003 due to the large proportion of missing data in disbursements. We included all 85 donors donating to RMNCAH in the 25 conflict-affected countries, comprising: (1) 30 members of the Development Assistance Committee (DAC), (2) 39 multilateral organisations (eg, United Nations and the WHO), (3) 15 non-DAC countries (eg, United Arab Emirates) and (4) one private donor (Bill & Melinda Gates Foundation (BMGF)).25 We listed the donors included in the CRS report in appendix table 2. All disbursement data were converted to constant 2015 US$.26
We obtained data on the burden of disease from the Institute for Health Metrics and Evaluation (IHME) Global Health Data Exchange database. Population data were drawn from United Nations Development Programme.4 27
Defining and identifying projects for RMNCAH and its components
Previous studies on DA for RMNCH have defined children as 1–59 months old.28 As the WHO and UNICEF point out, the period between ages 5 and 9 years is a critical phase for children’s anthropometric and intellectual development, but has been neglected for decades.29 Our study therefore extended the definition of children to those aged 5 to 9 years old. We defined the target population of RH as those aged 15–49 years old, with both men and women included; MNH referred to the health of women and their newborn babies during pregnancy, childbirth and the first month of life; adolescents were defined as those between 10 and 24 years old.
Following previous practices,14 15 23 we produced two sets of estimates for aid disbursed to RMNCAH: RMNCAH-targeted projects (lower bound) and RMNCAH-inclusive projects (upper bound).
RMNCAH-targeted projects (lower bound)
We followed the previous studies9 10 12–22 and defined RMNCAH-targeted DA as the aid disbursed to projects with the primary objective to prevent diseases and restore, improve and maintain RH, CH, MNH and AH. Projects in these four components were set to be mutually exclusive. If a project included activities targeting multiple health areas, such as for both MNH and CH, we followed previous studies and divided the funding equally into the two areas. Following previous research practice,9 10 12 13 we defined RH as expenditures on family planning, sexual health and sexually transmitted diseases (STDs), including HIV. Projects addressing adolescents’ RH were classified as RH, not AH to avoid revising the age definition (15–49 years old) of RH projects. Projects on HIV/AIDS for children were classified as CH. Projects on mother-to-child transmission or other HIV/AIDS interventions targeting pregnant women and newborn were classified as MNH. We excluded projects that were allocated at the regional level, which accounted for 6.3% of all CRS disbursements between 2003 and 2017.
The CRS data have no variable indicating projects targeting RMNCAH. To identify relevant projects, we adopted a combination of keyword searching and manual review for 600 483 projects from both health and non-health sectors (eg, education, water and sanitation, humanitarian aid, as described in table 1). We followed three steps: (1) Keywords searching for each of the four components (RH, MNH, CH and AH) based on the practice used in previous studies.12–20 30 31 The keywords for RH and MNH are listed in appendix table 3 and 4. To identify projects on CH and AH, we first generated keywords for the related age groups (eg, CH: ‘child’, ‘orphan’, ‘infant’; AH: ‘adolescent’, ‘teen’, ‘youth’ (appendix table 5 and 6)) and then combined them with the health-related keywords (eg, ‘pneumonia’, ‘malaria’, ‘diarrhoea’ (appendix table 7)). A CH or AH project included both the age identification and the health keywords. We translated all keywords into eight major languages: Spanish, French, Portuguese, Italian, Dutch, German, Norwegian and Swedish. (2) To determine how many projects were falsely coded as RMNCAH-targeted projects using the keyword search, we manually reviewed the selected projects and excluded those that did not include components on RMNCAH (49.1% out of 91 994 projects). The final sample included 46 833 RMNCAH-targeted projects for the 25 conflict-affected countries. (3) Previous studies have observed that a keyword search strategy could lead to some projects for RMNCAH being missed due to the imperfect sensitivity of the strategy.14 15 20 21 23 32 33 We investigated this by randomly selecting 5% projects (1846) in 2017 and applied separately both the keyword search and manually coding to the selected projects separately. Comparing the results from the two methods, we found that the keyword searches missed about 0.22% of RMNCAH projects.
Table 1.
RMNCAH projects (totally 46 833) by sectors in the 25 conflict-affected countries: frequency and the most common themes, lower bound
| Sector name* | Sector code | Frequency and percentage of total project | Examples |
| Education | |||
| Basic Education | 112 | 1109 (2.37%) | Multisectoral HIV/AIDS Control and Orphans Project. Teaching theories and practical applications to enhance teenagers’ mental and physical health. |
| Secondary Education | 113 | 238 (0.51%) | Psychological counselling for abused girls and women. Medical education and care of young people. |
| Post-secondary Education | 114 | 118 (0.25%) | Physical therapy and prosthetics to disabled people. Innovative approaches for health development in postconflict areas. |
| Education, Level Unspecified | 111 | 518 (1.11%) | Child friendly schools with water, sanitation and hygiene programme. HIV/AIDS prevention in schools. |
| Health | |||
| Health, General | 121 | 1850 (3.95%) | HIV/AIDS Project. Safe motherhood. |
| Basic Health | 122 | 7429 (15.86%) | Quality improvement of maternal and child health service. Vaccine introduction grants. |
| Population and Reproductive Health | |||
| Population and Reproductive Health | 130 | 23 574 (50.34%) | Young people’s sexually and reproductive health and sexuality education. HIV/AIDS control programme. |
| Water and Sanitation | |||
| Water and Sanitation | 140 | 684 (1.46%) | Water, sanitation and hygiene (WASH) for maternal, newborn and child health. Maternal and under-5 nutrition and child health. |
| Government and Civil Society | |||
| Government and Civil Society, General | 151 | 3607 (7.70%) | Peace and health awareness for school children. Support for victims of sexual and gender-based violence. |
| Conflict, Peace and Security | 152 | 692 (1.48%) | Facilitate healthy psychosocial development for children affected by armed conflicts. Action to prevent gender-based violence. |
| Social Infrastructure and Services | |||
| Social Infrastructure and Services | 160 | 2733 (5.84%) | Increase national capacity to deliver comprehensive maternal health services. Increase demand for and supply of modern contraceptives and improve quality family planning services. |
| Economic Infrastructure and Services | |||
| Transport and Storage | 210 | 39 (0.08%) | Investment in health and nutrition targeting young children and mothers. Reduce the proportion of wasting and stunting in children and reduce the incidence of low birth weight. |
| Communications | 220 | 37 (0.08%) | Improve maternal, newborn and child health care. Health education for excluded children and women. |
| Multi-Sector/Cross-Cutting | |||
| Multi-Sector/Cross-Cutting† | 430 | 737 (1.57%) | Comprehensive care for children affected by HIV/AIDS. Integrated Prevention of Mother-to-Child Transmission of HIV |
| Commodity Aid/General Programme Assistance | |||
| Development Food Aid/Food Security Assistance | 520 | 530 (1.06%) | Food aid for maternal and child health. Prevention of malnutrition targeting children under-5 years old. |
| Humanitarian Aid | |||
| Emergency Response | 720 | 2694 (5.75%) | Infant, young child maternal feeding in emergencies. Emergency nutritional response. |
| Reconstruction Relief and Rehabilitation | 730 | 145 (0.31%) | Basic health assistance for mother and child. Care of traumatised children and youth by child-protecting and psychosocial measures in refugee camps. |
| Disaster Prevention and Preparedness | 740 | 66 (0.14%) | HIV/AIDS preparedness plan in humanitarian action. Sexual and reproductive health in emergencies. |
| Unallocated/Unspecified‡ | |||
| Unallocated/Unspecified | 998 | 141 (0.30%) | Buy and procure pentavalent and pneumococcal vaccines. Traumatic experiences, mental disorders and barriers to care among young men and women |
*See http://formin.finland.fi/public/download.aspx?ID=155821&GUID=%7B787221EE-A481-4AD4-81C5-E00FBAB924C0%7D for the definition of each sector category.
†Multi-Sector/Cross-Cutting project refers to environment activities not allocable to any specific sectors.
‡Unallocated/Unspecified projects include those without specified sectors and aiming to promote development awareness.
RMNCAH, reproductive, maternal, newborn, child and adolescent health.
RMNCAH-inclusive projects (upper bound)
The RMNCAH-inclusive projects included three parts: (1) RMNHCAH-targeted projects identified above, (2) projects partially targeting RMNCAH and (3) projects that did not include the keywords for RMNCAH, but benefited RMNCAH, such as medical staff training, health education or health system strengthening.
Projects partially targeting RMNCAH were identified using the same method as for RMNCAH-targeted projects: combined keywords searching and manual review to identify projects that partially targeted RMNCAH, such as those to promote youth health and generate employment opportunities.
For the third part, we allocated some of the funds for projects beneficial for RMNCAH but that did not include the keywords to the RMNCAH. The categories of these projects are listed in appendix table 8. We allocated the funds following previous studies.12 16 17 19 20 34 For example, for general budget support, we first obtained the percentage of government spending on health for each country from the WHO Global Health Expenditure database.35 We then allocated government spending on health to RH/MNH/CH/AH based on the relative proportion of population involved in the component (reproductive population aged 15–49 years old/pregnant women and newborn/children aged 1 month to 9 years/adolescents aged 10–24 years old). The allocation factor of general budget support differed by country and year. We also applied the relative proportion of the related populations to allocate health system funds for each country (appendix table 8). Following previous studies,12 16 17 19 20 34 we allocated disease-specific or nutrition-specific funds, such as those for basic nutrition, tuberculosis and other infectious diseases based on the relative proportion of the related population and the proportion of the population living with the specific disease (appendix table 8). Funds that targeted STDs including HIV/AIDS (CRS purpose code 13040), family planning (code 13030), RH care (code 13020) and personnel development for population and RH (code 13081) were allocated 100% to RH.12 16 17 19 20 34 In total, we identified 86 317 RMNCAH-inclusive projects for the 25 conflict-affected countries.
Analysis of RMNCAH projects
Using both the lower-bound and upper-bound estimates, we tracked the aggregate level and trends of DA to RH/MNH/CH/AH among the 25 conflict-affected countries between 2003 and 2017 and identified the top donors during the study period. To understand regional differences, we divided the 25 countries into two groups: sub-Saharan Africa (SSA, 13 countries) and non-sub-Saharan Africa (non-SSA, 12 countries). We investigated DA per capita for RH/MNH/CH/AH in each country. DA per capita for SSA or non-SSA category was calculated as the total aid for RH/MNH/CH/AH received by all countries in that category divided by the total number of related population of those countries for a year. For example, DA to RH (DA-RH) per capita in SSA category is calculated as the total aid for RH received by all conflict-affected SSA countries divided by the total number of the population of reproductive age (15–49 years old) in these countries.
Moreover, we compared DA to RH/MNH/CH/AH with the corresponding DALYs. We provided the definition of DALYs on RH/MNH/CH/AH in appendix table 9. We paid specific attention to six leading causes of DALYs that accounted for 90% of total DALYs for children and adolescents.4 15 These six causes of DALYs were derived from the IHME, including (1) water, sanitation and hygiene (WASH)-related diseases, (2) communicable diseases, (3) mental disorders, (4) nutrition-related diseases, (5) other non-communicable diseases and (6) injuries. The definition of the six causes is provided in appendix table 10. To identify related projects for each cause of DALYs, we adopted the same combination of keyword search and manual review as aforementioned. We first used age-related keywords (appendix table 5 and 6) and cause-specific keywords (appendix tables 11-16) based on previous studies and reports to identify related projects. Then, we manually reviewed all identified projects to correct for any misclassifications. For a project with multiple purposes (eg, WASH-related diseases and nutritional status), we divided the funding of the project equally to each purpose.
Patient and public involvement statement
Patients were not involved in this study.
Results
Number of RMNCAH-targeted projects in each sector in the 25 conflict-affected countries
There were 46 833 projects targeting reproductive, maternal, newborn, child or AH. Table 1 shows that 32 853 projects (70.1%) were allocated to the health sector (including ‘General Health’, ‘Basic Health’ and ‘Population and Reproductive Health’) and the remaining 13 980 (29.9%) to non-health sectors. The ‘Population and Reproductive Health’ sector comprised more than half of the projects (23 574 (50.3%)), with the most common themes being sexual and RH, as well as HIV prevention and treatment. The ‘Basic Health’ and ‘Health, General’ sectors comprised 9279 (19.8%) projects, with maternal safety, HIV/AIDS control and vaccine introduction being the most common themes. The ‘Government and Civil Society’ sector comprised 3607 (7.7%) projects and ranked the highest in all non-health sectors, with promoting health awareness for school children and supporting victims of sexual and gender-based violence being the most common themes. This was followed by ‘Social Infrastructure and Services’ sector and ‘Emergency Response’ sector, which comprised 2733 (5.8%) and 2694 (5.8%) projects, respectively.
Estimates of total aid disbursed to RH/MNH/CH/AH and the top donors and targeted projects in the 25 conflict-affected countries
Between 2003 and 2017, DA to RMNCAH-targeted projects increased by seven-fold from $530.0 million to $3644.0 million, cumulatively $34 268.8 million, accounting for 61.3% of total DA in the 25 conflicted-affected countries (see figure 1). There were three relatively big leaps in DA-RMNCAH during the study period: the first was between 2004 and 2005 when DA-RMNCAH increased by 70.9% from $603.0 to $1030.6 million, the second was between 2008 and 2009 with DA-RMNCAH increased by 43.1% from $1725.2 to $2469.4 million and the third was between 2011 and 2013 when DA-RMNCAH further increased by 50.3% from $2327.8 to $3498.4 million. DA-RMNCAH remained around $3500 million since 2013. DA to RMNCAH-inclusive projects showed a similar trend (appendix figure 1).
Figure 1.
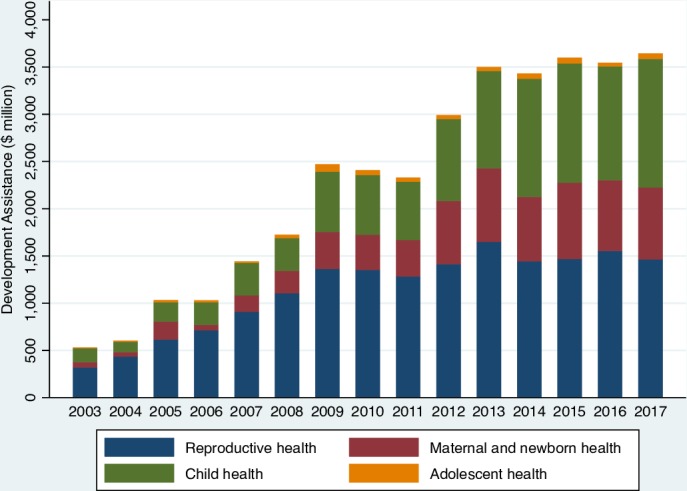
Annual trend of development assistance for reproductive, maternal, newborn, child and adolescent health in 25 conflict countries ($ million) by health component, lower-bound estimates.
Figure 1 presents aid disbursed (lower bound) to RH/MNH/CH/AH in total and by each component. DA-RH accounted for the largest proportion in all years, ranging from 40.2% in 2017 to 72.4% in 2004. Cumulatively, RH received $17 093.5 million between 2003 and 2017, 49.9% of total DA to RMNCAH-targeted projects. Most of the increase in DA-RH occurred between 2003 and 2009 when the annual growth rate was 27.2%; after 2009, DA-RH has been fluctuating around $1500 million. HIV/AIDS accounted for the largest proportion (74.9%–90.9%) of DA-RH in all years, tending to decrease over time since 2013 (appendix figure 2). CH received the second largest DA, cumulatively $10 247.5 million (29.9% of total DA to RMNCAH-targeted projects). DA to CH (DA-CH) increased rapidly throughout the study period, with an annual growth rate of 17.3%. Although DA-CH was only half as much as that of DA-RH in 2003, it reached DA-RH in 2017. DA to MNH (DA-MNH) increased dramatically with an annual growth rate of 30.3% between 2003 and 2013 ($55.1 million in 2003 and $778.9 million in 2013); yet, after year 2013, DA-MNH has been vacillating around $700 million. AH received the smallest amount of DA in all years and accounted for only 1.6% of total DA to RMNCAH-targeted projects ($562.3 million). For all three leaps in DA-RMNCAH (2004–2005, 2009–2009, 2011–2013), all components appeared to benefit substantially.
The upper-bound estimates showed that RH received the largest cumulative DA to RMNCAH-inclusive projects; yet, in several of the more recent years (2014–2017), DA-CH exceeded DA-RH. In 2017, DA-CH was $2289.2 million compared with $1623.2 million for DA-RH (appendix figure 3).
The top five donors for RMNCAH-targeted projects in the conflict-affected countries included the USA ($12 178.0 million), the Global Fund to Fight AIDS, Tuberculosis and Malaria (GFATM, $4601.7 million), the GAVI, ($3555.5 million), the United Kingdom (UK, $3445.1 million) and Canada ($1627.7 million). Together, they provided 74.1% of total aid for RMNCAH-targeted projects (appendix figure 4). All three leaps in DA-RMNCAH (2004–2005, 2009–2009, 2011–2013) were driven by multiple donors. For example, the USA, GFATM, GAVI and the UK were all contributed substantially to the leap in 2011–2013. In terms of RMNCAH-inclusive estimates, the top five donors were the USA, the GFATM, the UK, the GAVI and the IDA, which together provided 67.0% of total DA to RMNCAH-inclusive projects (appendix figure 5).
The lower-bound estimates showed that the USA was the largest donor of DA-RH, with cumulative disbursements of $9089.9 million between 2003 and 2017, followed by the GFATM ($3206.7 million), the UK ($981.9 million), IDA ($977.9 million) and the United Nations Population Fund (UNFPA, $640.5 million). These five donors accounted for 87.1% of the total DA-RH in the conflict-affected countries with a major focus on HIV/AIDS activities. The top donors for CH were the USA ($1817.8 million), the UK ($1746.4 million), the GAVI ($1443.3 million), Canada ($984.3 million) and the GFATM ($856.3 million). They together provided 66.8% of the total DA-CH, with improving CH services and vaccine coverage as the major themes. The top donors for MNH were the GAVI ($2102.9 million), the USA ($997.2 million), the UK ($688.1 million), the GFATM ($511.5 million) and the IDA ($302.3 million). Together they contributed to 72.3% of the total DA-MNH, mainly focusing on increasing maternal health services and vaccine coverage among newborns. In terms of AH, the top five donors were the USA ($273.1 million), Canada ($68.8 million), Germany ($30.5 million), the UK ($28.7 million) and the IDA ($28.4 million). These five donors together contributed to 76.3% of the total DA to AH (DA-AH), with health education, nutrition improvements and psychosocial care among the top donated projects. The top donors remained the same for all four components when applied to upper-bound estimates.
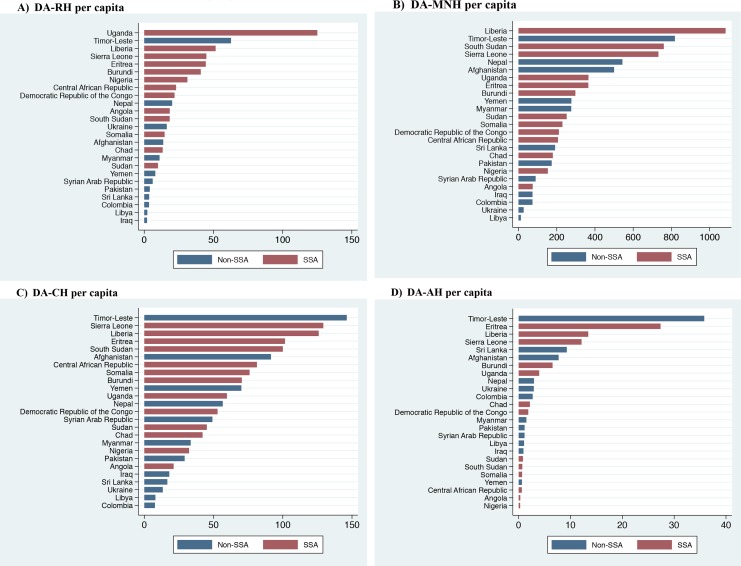
Estimates of per capita aid disbursed to RH/MNH/CH/AH-targeted projects between 2003 and 2017 in the 25 conflict-affected countries
Table 2 presents trends of per capita DA to RH, MNH, CH and AH between 2003 and 2017. Overall, DA-MNH per birth received the highest amount of aid in all studied years, which was cumulatively $222.3 between 2003 and 2017. DA-MNH per birth also had the fastest annual growth rate among the four RMNCAH components, at 18.5%. DA-CH per child received the second highest DA in all years (cumulatively $42.5 between 2003 and 2017) and increased at an annual rate of 14.8%. DA-RH received a total $19.9 per person of reproductive age during the studied period. The relatively small amount of DA-RH per capita was mainly due to the large population of reproductive age. DA-AH per adolescent ranged between $0.04 and $0.30 during the study period, cumulatively $2.1 per person over 14 years.
Table 2.
Annual trend of development assistance for reproductive health (DA-RH) per person aged 15–49 years old, development assistance for maternal and newborn health (DA-MNH) per birth, development assistance for child health (DA-CH) per child aged 1 month to 9 years old and development assistance for adolescent health (DA-AH) per adolescent aged 10–24 years old in the 25 conflict-affected countries, lower bound, 2003–2017 (US$)
| 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | Total | Annual growth rate | |
| DA-RH per capita | |||||||||||||||||
| Overall | 0.48 | 0.64 | 0.82 | 0.93 | 1.16 | 1.39 | 1.67 | 1.63 | 1.49 | 1.61 | 1.84 | 1.58 | 1.57 | 1.62 | 1.50 | 19.93 | 8.4% |
| SSA | 0.78 | 1.16 | 1.47 | 1.70 | 2.03 | 2.69 | 3.07 | 2.97 | 2.65 | 2.90 | 3.23 | 2.71 | 2.49 | 2.71 | 2.51 | 35.07 | 8.7% |
| Non-SSA | 0.24 | 0.21 | 0.35 | 0.36 | 0.51 | 0.39 | 0.59 | 0.57 | 0.55 | 0.54 | 0.67 | 0.61 | 0.77 | 0.67 | 0.60 | 7.64 | 6.7% |
| DA-MNH per capita | |||||||||||||||||
| Overall | 2.31 | 1.87 | 7.51 | 2.32 | 6.67 | 8.90 | 14.50 | 13.57 | 13.69 | 23.39 | 26.90 | 23.27 | 27.38 | 25.09 | 24.88 | 222.26 | 18.5% |
| SSA | 2.06 | 2.41 | 12.22 | 2.60 | 8.45 | 6.67 | 17.99 | 12.37 | 15.19 | 23.67 | 25.18 | 21.54 | 28.11 | 26.42 | 25.36 | 230.27 | 19.6% |
| Non-SSA | 2.61 | 1.20 | 1.85 | 1.98 | 4.47 | 11.67 | 10.10 | 15.11 | 11.70 | 23.01 | 29.27 | 25.69 | 26.33 | 23.17 | 24.17 | 212.32 | 17.2% |
| DA-CH per capita | |||||||||||||||||
| Overall | 0.75 | 0.56 | 0.99 | 1.12 | 1.59 | 1.58 | 2.85 | 2.77 | 2.61 | 3.61 | 4.20 | 5.02 | 4.98 | 4.68 | 5.19 | 42.51 | 14.8% |
| SSA | 0.72 | 0.84 | 1.31 | 1.21 | 1.90 | 1.96 | 3.63 | 3.12 | 3.20 | 4.07 | 4.48 | 5.67 | 5.24 | 4.90 | 5.28 | 47.52 | 15.3% |
| Non-SSA | 0.78 | 0.26 | 0.66 | 1.03 | 1.27 | 1.18 | 2.00 | 2.39 | 1.91 | 3.06 | 3.87 | 4.22 | 4.66 | 4.39 | 5.08 | 36.76 | 14.3% |
| DA-AH per capita | |||||||||||||||||
| Overall | 0.04 | 0.05 | 0.09 | 0.08 | 0.07 | 0.14 | 0.30 | 0.19 | 0.16 | 0.15 | 0.14 | 0.19 | 0.20 | 0.13 | 0.19 | 2.12 | 12.6% |
| SSA | 0.06 | 0.08 | 0.14 | 0.11 | 0.06 | 0.11 | 0.20 | 0.17 | 0.11 | 0.11 | 0.12 | 0.15 | 0.17 | 0.10 | 0.18 | 1.88 | 8.0% |
| Non-SSA | 0.01 | 0.02 | 0.05 | 0.07 | 0.07 | 0.17 | 0.39 | 0.21 | 0.20 | 0.17 | 0.16 | 0.23 | 0.24 | 0.16 | 0.20 | 2.34 | 20.5% |
We estimate the number of births using the total population multiplied by crude birth rate. See http://adph.org/healthstats/assets/Formulas.pdf
SSA represents the category ‘Sub-Saharan Africa’; Non-SSA represents the category ‘Non Sub-Saharan Africa’.
Annual growth rate=((end value/start value)ˆ(1/periods) −1.
SSA and non-SSA countries differed greatly in the amounts of DA-RH per capita they received for all years. Cumulatively, SSA countries received $35.1 per person during 2003 and 2017, around five times that of non-SSA countries ($7.6 per person). SSA countries received slightly higher cumulative per capita aid for MNH and CH than non-SSA countries for most years. Countries in both groups received small cumulative per capita aid for AH ($1.9 in SSA vs $2.3 in non-SSA). Upper-bound estimates showed similar results (appendix table 17).
In figure 2, we rank the 25 conflict-affected countries according to the cumulative aid per capita of RH/MNH/CH/AH. Timor-Leste, Liberia and Sierra Leone received the highest aid per capita in all four health components. Libya, Iraq and Colombia received the lowest aid per capita in RH/MNH/CH. Nigeria received the lowest cumulative DA-AH per adolescent ($0.3), followed by Angola ($0.3) and Central African Republic ($0.6). Upper-bound estimates showed similar results (appendix figure 6).
Figure 2.
The rank of (A) development assistance for reproductive health (DA-RH) per person aged 15–49 years old, (B) development assistance for maternal and newborn health (DA-MNH) per birth, (C) development assistance for child health (DA-CH) per child aged 1 month to 9 years old and (D) development assistance for adolescent health (DA-AH) per adolescent aged 10–24 years old in the 25 conflict-affected countries, cumulatively received between 2003 and 2017, lower bound (US$).
We present country-level lower and upper bounds of annual aid per capita for RH/MNH/CH/AH in appendix table 18-25. For the majority of the countries, aid per capita generally increased over years, but with obvious fluctuations. For example, although DA-RH per capita in Uganda increased from $2.7 in 2003 to $9.3 in 2017, it varied from $5.2 to $14.1 in the years in between. There were several countries with a decreasing trend of aid per capita. For example, DA-MNH per capita in Eritrea decreased from $39.8 in 2003 to $12.6 in 2017.
Estimates of aid for RH/MNH/CH/AH-targeted projects versus DALYs attributed to RH/MNH/CH/AH during 2003 and 2017 in the 25 conflict-affected countries
Figure 3 presents the DALYs attributed to RMNCAH by RH, MNH, CH and AH, respectively, over time. CH caused the highest DALYs in all years, cumulatively 2.1 billion between 2003 and 2017, two times that of MNH (1.0 billion DALYs), three times that of AH (0.6 billion) and five times that of RH (0.4 billion). HIV/AIDS accounted for half of the RH-related DALYs (cumulatively 0.2 billion) and 5.4% of total RMNCAH-related DALYs, while it received 84.0% of DA-RH and 41.9% of all DA to RMNCAH-targeted projects (see appendix figures 2 and 7 for annual proportion). On the contrary, AH caused more DALYs than RH, but only received 3.3% as much DA as that of RH. At the country level (appendix table 26), the findings suggested a general lack of consistency between the proportion of aid for RH/MNH/CH/AH in total DA-RMNCAH to the proportion of DALYs of RH/MNH/CH/AH. For example, AH caused more DALYs than RH in all 25 countries; yet, in most countries, AH received less than one-tenth of the DA to RH.
Figure 3.
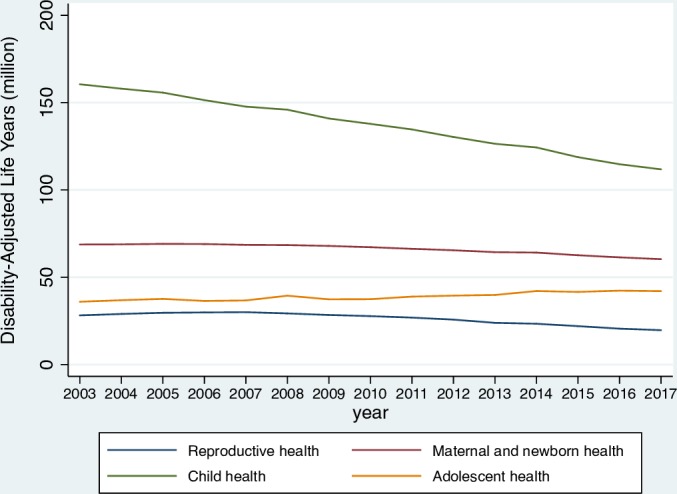
Annual trend of disability-adjusted life years (million) by health component in the 25 conflict-affected countries. See online appendix table 9 for the definition of disability-adjusted life years for each of the four health component.
We further compared DALYs of the six leading causes among children and adolescents with their DA in 2017. We included HIV/AIDS and other STDs in communicable diseases. The six causes of DALYs represented 90.3% and 88.0% of the total DALYs caused by CH and AH, respectively (table 3). In terms of CH, communicable diseases (excluding WASH diseases) contributed to the largest volume and proportion of DALYs (33.1%) in 2017 and received the largest share (43.8%) of DA-CH. Non-communicable (excluding nutrition and mental diseases) and WASH diseases (eg, diarrhoea) ranked second and third in terms of DALYs (19.1% and 18.8%, respectively), but received only 3.7% and 5.9% of DA-CH. Injury and physical rehabilitation caused 9.8% of total DALYs caused by CH and received 3.3% of DA-CH. In contrast, nutrition deficiency diseases contributed to 8.8% of the total DALYs among children but received 29.9% of aid for CH. In terms of adolescents, non-communicable diseases contributed to the largest DALYs (36.2%) in 2017, but received the lowest proportion of DA-AH (3.0%); communicable diseases caused 11.5% of total DALYs of AH, but received half of the total funding for AH, and nutritional deficiency caused 4.8% of total DALYs of AH, but received 12.5% of the DA-AH.
Table 3.
Causes of disability-adjusted life years (DALYs) for the 25 conflict-affected countries and the corresponding lower bound of development assistance (DA), child health (CH) and adolescent health (AH) in 2017
| Cause | Child health | Adolescent health | ||||||
| DALYs | DA | DALYs | DA | |||||
| Value (million) | Proportion in total DALYs caused by CH (%) | Value (million) | Proportion in total DA for CH (%) | Value (million) | Proportion in total DALYs caused by AH (%) | Value (million) | Proportion in total DA for AH (%) | |
| Communicable diseases, excluding WASH diseases | 39.2 | 33.1 | 596.1 | 43.8 | 6.0 | 11.5 | 39.5 | 49.5 |
| Injury and physical rehabilitation | 11.6 | 9.8 | 45.3 | 3.3 | 12.2 | 23.3 | 11.7 | 14.6 |
| Mental disorders | 0.8 | 0.7 | 5.6 | 0.4 | 5.0 | 9.5 | 3.2 | 4.0 |
| Non-communicable diseases, excluding nutrition and mental diseases | 22.7 | 19.1 | 50.1 | 3.7 | 19.0 | 36.2 | 2.4 | 3.0 |
| Nutritional deficiency diseases | 10.4 | 8.8 | 407.0 | 29.9 | 2.5 | 4.8 | 10.0 | 12.5 |
| WASH diseases | 22.3 | 18.8 | 80.9 | 5.9 | 1.4 | 2.6 | 4.5 | 5.6 |
| Other causes | 11.5 | 9.7 | 175.8 | 12.9 | 6.3 | 12.0 | 8.6 | 10.8 |
| Total | 118.5 | 100.0 | 1360.8 | 100.0 | 52.4 | 100.0 | 79.8 | 100.0 |
See ‘appendix table 10’ for definitions of the causes of DALYs.
WASH, water, sanitation and hygiene.
Discussion
Using data from the CRS, we tracked DA to RMNCAH in general and to RH/MNH/CH/AH separately in the 25 conflict-affected countries between 2003 and 2017. DA to RMNCAH-targeted projects rose substantially by seven-fold from 0.5 billion to 3.6 billion during the study period, with the fastest increase occurred before 2013 mainly driven by the USA, the GFATM, the GAVI and the UK. This trend reflects the continuing efforts made by the donor community to reducing child and maternal mortality rates during the era of the Millennium Development Goals. Meanwhile, the drastic increase driven by investments from a small number of donors is worrying—any changes made by those donors could substantially impact the financing of RMNCAH in the conflicted-affected countries.
Among the four components, at both aggregate and country level, RH received the largest portion of aid for RMNCAH in the 25 countries, mainly due to the large amount of aid earmarked for HIV/AIDS, accounting for 42% of total DA-RMNCAH during the study period. A decreasing trend of funding for HIV/AIDS occurred since 2013; there was, however, a surge in aid for family planning, likely a result of the 2012 London Family Planning summit and the launch of the FP2020.13 In 2017, HIV/AIDS accounted for only 5% of the RMNCAH-related DALYs, suggesting that large amounts of DA to prevention and treatment of HIV/AIDS during the Millennium Development Goals period contributed to the low level of DALYs in 2017, a topic that deserves future study.
Consistent with previous findings, AH received the smallest portion of aid for RMNCAH among the four components.15 This is despite the fact that adolescence is a phase of rapid physical, cognitive and emotional growth in which future patterns of adulthood health and development are established.36 37 AH may also impact the early childhood development of the next generation.37 In 2017, AH resulted in approximately 15% of the total DALYs attributed to RMNCAH in the 25 countries in 2017, but received only 3% of aid for RMNCAH to these countries in the same year. This suggests that AH in the conflict-affected countries has continuously been neglected by donors, just as it was at the global level. With further investigation, we found that within the small amount of AH investment, conditions that contributed to a large portion of DALYs of adolescents, including non-communicable diseases, mental disorders and road injury, received a negligible amount of aid in 2017. Mental disorders and NCDs received little attention from donors, probably due to stigmatisation, or lack of information about cost-effectiveness interventions, or misconceptions that these diseases do not kill.32 38 As AH has been included in the Every Woman Every Child agenda through the Global Strategy for Women’s, Children’s and Adolescents’ Health (2016–2030),2 our findings suggest that the levels of DA to AH should increase during the era of the Sustainable Development Goals (SDGs).
Funding for MNH increased at a drastic rate during 2003 and 2013, which reflected donors’ focus on maternal health and the growing recognition of the importance of newborn survival in reducing child mortality, 44% of under-5 child deaths being neonatal.1 13 However, it is alarming that funding for MNH stagnated or even slightly decreased since 2013, probably reflecting unpredictability in funding flows and/or a switch of donors’ focus to other health components (eg, CH). Reducing newborn mortality is a key target in the SDGs, and conflict-affected countries have some of the highest rates of neonatal mortality. For example, Afghanistan accounts for 2% of global neonatal mortality. Clearly, stable funding from donors is necessary for achieving the target in these countries.39
CH kept increasing during the study period due to sizeable growth in funding from global initiatives such as GFATM, GAVI and UNFPA in financing malaria, immunisation and HIV projects, benefiting CH. For example, after the Global Vaccine Summit in Abu Dhabi in 2013, we observed a jump in funding for immunisation projects. We observed a similar pattern for DA-AH; more than two-thirds of funding was allocated to communicable and nutritional deficiency diseases. NCDs and WASH diseases received disproportionally small amount of aid, while they contributed to a large portion of DALYs.
While producing valuable information, the study has some limitations. First, in terms of identification strategy, the keyword searching strategy could fail to capture some RMNCAH projects; however, as demonstrated in our study, 0.22% of RMNCAH projects were not captured. In addition, we followed previous practice and divided projects with multiple health components equally into each component, but the method is not supported by sufficient empirical evidence. Second, in terms of data used in the study, we excluded aid that was allocated at the regional level because we lacked the information necessary to distribute it to a specific country. Due to data unavailability, we could not include newly emerging economies (eg, China) and NGOs or private foundations (except for BMGF) in the analysis. For missing data in CRS between 2003 and 2006, we were able to obtain GAVI data and added them to the estimates, but this could not be done for other donors. These issues led to underestimation of aid for RMNCAH in the conflict-affected countries in those years. Further, the reliability of DALYs data provided by IHME has also been challenged by previous studies, particularly in low-income countries.40 Countries in conflicts may not have strong information systems for gathering quality data required for estimating DALYs. Third, in terms of estimation method, allocating aid to HIV/AIDS and other STDs for adolescents to DA-RH would lead to underestimation of aid for AH. Projects that partially target RMNCAH were not included in RMNCAH-targeted estimates, as a result of which DA-RMNCAH might be underestimated. At the same time, RMNCAH-inclusive estimates included projects with purpose unrelated to RMNCAH and might have overestimated DA-RMNCAH. In addition, as indicated in previous studies,9 10 we were uncertain about what percentage of a country’s population was affected by conflict.
This study was the first to systematically track DA to each component of RMNCAH in the 25 conflict-affected countries and also the first to compare DA with various health areas with their corresponding DALYs. The overall increase in DA to RMNCAH is encouraging, but additional investments in areas that have received low levels of aid but with high burden of disease are needed. In addition, it is important that aid is used effectively. Investing in cost-effective interventions may gain high potential benefits. For example, interventions targeting AH, such as mental healthcare and injury prevention, are found to have high benefit to cost ratios, even without considering the benefits on the early development of their offspring.16 36 37 Due to political and economic instability in conflict-affected countries, donors tend to provide short-term aid (eg, food, humanitarian aid) rather than investing in building up primary healthcare systems that would greatly benefit RMNCAH.41 Considering fragile health financing in the area, we call for more donors to contribute to neglected health areas or conditions such as AH and non-communicable diseases. In addition, it is important to note that external funding to RMNCAH is only one source for financing RMNCAH. Estimating domestic spending on RMNCAH is beyond the scope of this study, and we call for more research on tracking government spending on RMNCAH. This would help to hold governments accountable for providing sufficient and sustainable funds for RMNCAH in the long term. Future research is also needed to identify cost-effective interventions, instruments for improving information system and evaluating the impact of DA-RMNCAH on population health outcomes in conflict-affected countries.
Footnotes
Handling editor: Eduardo Gómez
Contributors: ZL and CL conceptualised the analysis and developed the analysis plan. ZL conducted the analysis under CL’s advice. ZL wrote the first draft of the report. All authors interpreted findings, critically reviewed the report for important intellectual content, participated in writings and approved the final version.
Funding: This study is funded by Faculty Resources Grant of Brigham & Women’s Hospital.
Competing interests: None declared.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data are available in a public, open access repository.
References
- 1. UNDP Millennium development goals, 2000. Available: http://www.undp.org/content/undp/en/home/sdgoverview/mdg_goals.html [Accessed 23 Aug 2016].
- 2. World Health Organization WHO | Global Strategy for Women’s, Children’s and Adolescent’s Health & Every Woman Every Child Initiative, 2017. Available: http://www.who.int/life-course/partners/global-strategy/en/ [Accessed 4 Oct 2017].
- 3. Guha-Sapir D, D’Aoust O. World development report 2011. Available: https://pdfs.semanticscholar.org/48c7/b14f4c8f0af731e729c229fa4c848564cf5a.pdf
- 4. Global Burden of Disease Collaborative Network Global burden of disease study 2017 (GBD 2017) results. Seattle, United States: Institute for Health Metrics and Evaluation (IHME), 2018. [Google Scholar]
- 5. National Academies Press (US) Global health risk framework: governance for global health: workshop summary, 2016. Available: https://www.ncbi.nlm.nih.gov/books/NBK362968/ [Accessed 13 Nov 2018]. [PubMed]
- 6. United States Institute of Peace Health in Postconflict and fragile states, 2012. Available: www.usip.org [Accessed 13 Nov 2018].
- 7. Boerma T, Requejo J, Victora CG, et al. . Countdown to 2030: tracking progress towards universal coverage for reproductive, maternal, newborn, and child health. Lancet 2018;391:1538–48. 10.1016/S0140-6736(18)30104-1 [DOI] [PubMed] [Google Scholar]
- 8. The Countdown group Countdown 2030 – countdown 2017 report. Available: http://countdown2030.org/reports-and-publications/countdown-2017-report [Accessed 31 Jan 2019].
- 9. Patel P, Roberts B, Guy S, et al. . Tracking official development assistance for reproductive health in Conflict-Affected countries. PLoS Med 2009;6:e1000090 10.1371/journal.pmed.1000090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Patel P, Dahab M, Tanabe M, et al. . Tracking official development assistance for reproductive health in conflict-affected countries: 2002-2011. BJOG: Int J Obstet Gy 2016;123:1693–704. 10.1111/1471-0528.13851 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Spiegel PB, Checchi F, Colombo S, et al. . Health-Care needs of people affected by conflict: future trends and changing frameworks. The Lancet 2010;375:341–5. 10.1016/S0140-6736(09)61873-0 [DOI] [PubMed] [Google Scholar]
- 12. Grollman C, Arregoces L, Martínez-Álvarez M, et al. . 11 years of tracking aid to reproductive, maternal, newborn, and child health: estimates and analysis for 2003-13 from the countdown to 2015. Lancet Glob Health 2017;5:e104–14. 10.1016/S2214-109X(16)30304-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Arregoces L, Daly F, Pitt C, et al. . Countdown to 2015: changes in official development assistance to reproductive, maternal, newborn, and child health, and assessment of progress between 2003 and 2012. Lancet Glob Health 2015;3:e410–21. 10.1016/S2214-109X(15)00057-1 [DOI] [PubMed] [Google Scholar]
- 14. Lu C, Chu A, Li Z, et al. . Assessing development assistance for child survival between 2000 and 2014: a multi-sectoral perspective. PLoS One 2017;12:e0178887 10.1371/journal.pone.0178887 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Li Z, Li M, Patton GC, et al. . Global development assistance for adolescent health from 2003 to 2015. JAMA Netw Open 2018;1:e181072 10.1001/jamanetworkopen.2018.1072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Grollman C, Arregoces L, Martinez-Alvarez M, et al. . Developing a dataset to track aid for reproductive, maternal, newborn and child health, 2003–2013. Sci Data 2017;4 10.1038/sdata.2017.38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Pitt C, Grollman C, Martinez-Alvarez M, et al. . Tracking aid for global health goals: a systematic comparison of four approaches applied to reproductive, maternal, newborn, and child health. Lancet Glob Heal 2018;6:e859–74. 10.1016/S2214-109X(18)30276-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Pitt C, Lawn JE, Ranganathan M, et al. . Donor funding for newborn survival: an analysis of Donor-Reported data, 2002–2010. PLoS Med 2012;9:e1001332 10.1371/journal.pmed.1001332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Pitt C, Greco G, Powell-Jackson T, et al. . Countdown to 2015: assessment of official development assistance to maternal, newborn, and child health, 2003–08. The Lancet 2010;376:1485–96. 10.1016/S0140-6736(10)61302-5 [DOI] [PubMed] [Google Scholar]
- 20. Hsu J, Pitt C, Greco G, et al. . Countdown to 2015: changes in official development assistance to maternal, newborn, and child health in 2009–10, and assessment of progress since 2003. Lancet 2012;380:1157–68. 10.1016/S0140-6736(12)61415-9 [DOI] [PubMed] [Google Scholar]
- 21. Hsu J, Berman P, Mills A. Reproductive health priorities: evidence from a resource tracking analysis of official development assistance in 2009 and 2010. Lancet 2013;381:1772–82. 10.1016/S0140-6736(13)60762-X [DOI] [PubMed] [Google Scholar]
- 22. Powell-Jackson T, Borghi J, Mueller DH, et al. . Countdown to 2015: tracking donor assistance to maternal, newborn, and child health. Lancet 2006;368:1077–87. 10.1016/S0140-6736(06)69338-0 [DOI] [PubMed] [Google Scholar]
- 23. Lu C, Li Z, Patel V. Global child and adolescent mental health: the orphan of development assistance for health. PLoS Med 2018;15:e1002524 10.1371/journal.pmed.1002524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Uppsala University UCDP - Uppsala Conflict Data Program. Available: http://ucdp.uu.se/#/exploratory [Accessed 19 Jul 2018].
- 25. OECD Technical guide to terms and data in the Creditor reporting system (CRS) aid activities database. Available: http://www.oecd.org/dac/stats/crsguide.htm [Accessed 2 Aug 2017].
- 26. OECD Information note on the DAC Deflators. Available: http://www.oecd.org/dac/stats/informationnoteonthedacdeflators.htm [Accessed 10 Aug 2017].
- 27. UNDP World population prospects. Available: https://esa.un.org/unpd/wpp/Download/Standard/Population/ [Accessed 2 Aug 2017].
- 28. Black RE, Walker N, Laxminarayan R, et al. . Maternal, newborn, and child health: key messages of this volume. reproductive, maternal, newborn, and child health: disease control priorities, third edition (volume 2). The International Bank for Reconstruction and Development / The World Bank, 2016. [PubMed] [Google Scholar]
- 29. World Health Organization Preconception care. Report of a regional expert group consultation. Available: http://www.searo.who.int/entity/child_adolescent/documents/2014/sea-cah-16.pdf [Accessed 29 Oct 2018].
- 30. Dieleman JL, Schneider MT, Haakenstad A, et al. . Development assistance for health: past trends, associations, and the future of international financial flows for health. Lancet 2016;387:2536–44. 10.1016/S0140-6736(16)30168-4 [DOI] [PubMed] [Google Scholar]
- 31. Dieleman JL, Graves CM, Templin T, et al. . Global Health Development Assistance Remained Steady In 2013 But Did Not Align With Recipients’ Disease Burden. Health Aff 2014;33:878–86. 10.1377/hlthaff.2013.1432 [DOI] [PubMed] [Google Scholar]
- 32. Gilbert BJ, Patel V, Farmer PE, et al. . Assessing development assistance for mental health in developing countries: 2007–2013. PLoS Med 2015;12:e1001834 10.1371/journal.pmed.1001834 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Schäferhoff M, Schrade C, Yamey G. Financing maternal and child Health—What are the limitations in estimating donor flows and resource needs? PLoS Med 2010;7:e1000305 10.1371/journal.pmed.1000305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. G8 Muskoka Methodology for calculating baselines and commitments: G8 member spending on maternal, newborn and child health [Internet], 2010. ]. Available from: Available: www.g8.utoronto.ca/summit/2010muskoka/methodology.html [Accessed cited 2019 Feb 10].
- 35. World Health Organization Global health expenditure database. Available: http://apps.who.int/nha/database/Select/Indicators/en [Accessed 11 Jun 2018].
- 36. Sawyer SM, Afifi RA, Bearinger LH, et al. . Adolescence: a foundation for future health. Lancet 2012;379:1630–40. 10.1016/S0140-6736(12)60072-5 [DOI] [PubMed] [Google Scholar]
- 37. Sheehan P, Sweeny K, Rasmussen B, et al. . Building the foundations for sustainable development: a case for global investment in the capabilities of adolescents. Lancet 2017;390:1792–806. 10.1016/S0140-6736(17)30872-3 [DOI] [PubMed] [Google Scholar]
- 38. Saraceno B, van Ommeren M, Batniji R, et al. . Barriers to improvement of mental health services in low-income and middle-income countries. Lancet 2007;370:1164–74. 10.1016/S0140-6736(07)61263-X [DOI] [PubMed] [Google Scholar]
- 39. Gopalan SS, Das A, Howard N. Maternal and neonatal service usage and determinants in fragile and conflict-affected situations: a systematic review of Asia and the Middle-East. BMC Womens Health 2017;17:20 10.1186/s12905-017-0379-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Yoon S-J, Kim Y-E, Kim E-J. Why they are different: based on the burden of disease research of who and Institute for health metrics and evaluation. Biomed Res Int 2018;2018:1–4. 2018 10.1155/2018/7236194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. World Health Organization Effective aid, 2008. Available: http://www.who.int/hdp/publications/effectiveaid_betterhealth_en.pdf [Accessed 12 Nov 2018].
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjgh-2019-001614supp001.pdf (949KB, pdf)