Abstract
Barriers to genetic counseling services (GCS) utilization for Spanish-speaking patients (SSP) may include language barriers and limited availability of bilingual genetic counselors (GCs). The sample included GCs who: (1) practice cancer genetic counseling, (2) report a cancer practice setting, and (3) have a US mailing address. We assessed: (1) number of Spanish-speaking GCs, (2) estimated proportion of Hispanic patients, and (3) approaches used to counsel SSP. Of respondents (n = 229), 10% (n = 23) spoke Spanish. A higher proportion of GCs practicing in states with ≥ 25% Hispanics reported speaking Spanish compared to those in states with lower Hispanic populations (p = 0.02). While there was a significantly higher percentage of Spanish-speaking GCs in states with larger Hispanic populations, the absolute number was low and unlikely to meet the needs of patients. There is need to increase availability of GCS for SSPs and to understand the impact of services on patient health outcomes.
Keywords: BRCA, Breast cancer, Genetic counseling, Hereditary cancer, Spanish-speaking patients
Introduction
Despite the higher BC prevalence in non-Hispanic whites [1], Hispanics tend to be diagnosed at later stages and have worse prognoses [2].
Hispanics at increased hereditary cancer risk participate in genetic counseling/testing at low rates compared to nonHispanic whites [3, 4].
Risk appropriate utilization of cancer genetic services may be hindered by language barriers and the limited bilingual genetic counselor (GC) availability [5]. Few studies have specifically examined the availability of genetic counseling services (GCS) available to Spanish-speaking patients (SSP).
Methods
Participants
Mailing lists of GCs were obtained from the National Society of Genetic Counselors (NSGC) and the American Board of Genetic Counseling (ABGC). The study population included those who: (1) self-identified as a practicing cancer GC, (2) reported a cancer practice setting, and (3) had a US mailing address.
ABGC provided a pre-sorted mailing list by cancer practice setting (n = 1071). GCs outside of the US were excluded, yielding 964 GCs. NSGC provided a database of all members (n = 2102) including specialization and company name. The mailing list was sorted to include members reporting their specialization as ‘cancer’ or ‘PGM’ (personalized genomic medicine), and/or a company name that included ‘cancer’ and/or ‘oncology,’ and/or an address that listed ‘cancer,’ yielding 856 GCs. Additionally, we were contacted via email by a GC informed about our study through a colleague and was interested in participating (n = 1). After excluding duplicates, participants from pilot testing the survey (to verify face and content validity), and any undeliverables, we had a total of 1257 GCs.
Data Collection
Upon institutional review board approval from Mayo Clinic and the University of South Florida, a multiphase recruitment approach was utilized. Participants were first mailed a pre-notice postcard to inform them of the upcoming survey and to verify mailing address accuracy. Two weeks later, GCs were mailed a packet including a cover letter, survey, three previously mailed educational materials developed and distributed by our team [6], prepaid return envelope, and prepaid response card. The prepaid response card provided GCs the opportunity to indicate survey completion and enter a drawing for one of four $50 bills. Participants were asked to complete the survey via mail, fax, or online. Two weeks later, GCs who did not respond were mailed a reminder postcard. Two weeks later, a final packet containing all the materials were mailed to the remaining GCs. Surveys were collected May–October 2016.
Measures
As part of a larger study using two serial cross-sectional surveys to understand GC current practices and preferences for information regarding genetic testing for inherited BC risk [7], our team sought information specifically about practices related to GCs’ SSP in the second survey. Most relevant to the current study, GCs were asked the following three questions: (1) Do you speak Spanish (yes/no); (2) What percent of your patients are Spanish-speaking (0, 1–10, 11–20, 21–50, > 50%); and (3) How do you provide genetic counseling to your Spanish-speaking patients [I counsel in Spanish, I use a medical interpreter in-person, I use a telephone-based medical interpreter service, I use a telephone-based genetic counseling service, I refer to a local Spanish-speaking counselor, Other (participants could select more than 1 response)].
Analysis
Frequencies and percentages were obtained for: (1) participant demographic characteristics, (2) number of GCs who were Spanish-speaking, (3) proportion of Hispanic patients, and (4) approaches used to counsel SSP. We then used data from the Pew Research Center (http://www.pewhispanic.org/2016/09/08/4-ranking-the-latino-population-in-the-states/) to group respondents as being from states with ≥ 25% Hispanic population and those with < 25%. Chi square or Fisher’s Exact Test was used to compare response on items related to GCS for SSP. All data were analyzed using SPSS V.24.
Results
A total of 229 GCs completed surveys (response rate: 18%). The sample was predominately female (95.6%), White/Caucasian (90.4%), non-Hispanic/Latino (98.2%), with an average age of 37 years (range 25–68 years). Most indicated cancer as their primary specialty area (87.7%), were board certified in genetic counseling (95.2%), had an average of 7.15 years of genetic counseling experience (range 1–28 years), and represented 46 of 50 states.
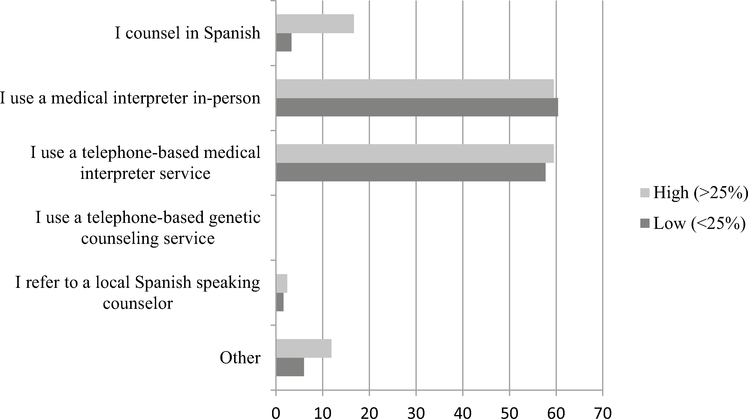
Table 1 illustrates the majority (94.3%) of GCs indicated 0–20% of their patients were SSP. Only 10.1% (n = 23) of counselors spoke Spanish, and even fewer (6%; n = 13) actually counseled in Spanish. Over half of GCs indicated they provided GCS to their SSP via a medical interpreter in-person (63.1%) and/or via a telephone-based medical interpreter service (59.9%). (Fig. 1).
Table 1.
Genetic counselor responses regarding genetic counseling comparing counselors from states with low (< 25%) and high (≥ 25%) Hispanic populations
| Question | Response options | Total N (%) | Low N (%) (n = 182) | High N (%) (n = 42) | Chi squared test or Fisher’s exact test |
|---|---|---|---|---|---|
| Do you speak Spanish? (n = 228) | Yes | 23 (10.1) | 14 (7.7) | 9 (21.4) | p = 0.02* |
| No | 205 (89.9) | 168 (92.3) | 33 (78.6) | ||
| What percent of your patients are Spanish-speaking? (n = 228) | 0–20% | 215 (94.3) | 176 (96.7) | 35 (83.3) | p = 0.01* |
| > 20% | 13 (5.7) | 6 (3.3) | 7 (16.7) | ||
| How do you provide genetic counseling to your Spanish-speaking patients?a (n = 217) | I counsel in Spanish | 13 (6.0) | 6 (3.3) | 7 (16.7) | p = 0.01* |
| I use a medical interpreter in-person | 137 (63.1) | 110 (60.4) | 25 (59.5) | X2 = 0.01, p = 0.94 | |
| I use a telephone-based medical interpreter service | 130 (59.9) | 105 (57.7) | 25 (59.5) | X2 = 0.07, p = 0.79 | |
| I use a telephone-based genetic counseling service | 0 | 0 | 0 | ||
| I refer to a local Spanish-speaking counselor | 5 (2.3) | 3 (1.6) | 1 (2.4) | p = 0.57 | |
| Other | 16 (7.4) | 11 (6.0) | 5 (11.9) | p = 0.19 |
Significant
Responses were not mutually exclusive
Fig. 1.
How GCs provide genetic counseling to Spanish-speaking patients (%)
Compared to GCs in states with smaller Hispanic populations, those practicing in states with ≥ 25% Hispanics, a higher proportion of GCs reported speaking Spanish (p = 0.02) and had > 20% of SSP (p = 0.01). GCs from states with a larger proportion of Hispanics were more likely to report counseling SSPs in Spanish (p = 0.01). However, there were no differences in providing services via a medical interpreter in-person, via telephone-based interpreter service, or referring locally to a Spanish-speaking GC (Table 1).
Discussion
Our findings demonstrate limited availability of GCS for SSP. While there were significantly higher percentages of Spanish-speaking GCs in states with larger Hispanic populations, the absolute number was low and unlikely to meet the needs of these patients. Previous studies have found barriers for Latino access to genetic counseling and testing may be due to language and the limited availability of bilingual genetics professionals [5]. Therefore it is important to consider strategies that may facilitate these preferences including telephone counseling in Spanish, group education sessions, or education by a well-trained member of the healthcare team.
Although access to GCS is a major barrier, access alone does not guarantee high quality services. Gaps in effective communication are a major contributor to health disparities [8], yet few studies have addressed communication between GCs and underserved patients [9]. Simply offering Spanish language services but failing to address these communication gaps will not improve existing health disparities.
The majority of GCs indicated they provided GCS to their SSP via a medical interpreter in-person and/or via telephone. Professional medical interpreters are more effective than family or other staff [10]. Technological advances have made medical interpreters more readily available via video or telephone, however, the quality of the services remains variable and further research should identify strategies to improve communication when utilizing an interpreter. For example, there are novel training programs to assist interpreters to work in cancer genetics and introduces specialized vocabulary as well as opportunities to discuss challenges faced by interpreters in this area (http://www.chiaonline.org/Interpreting-for-Cancer-Genetics).
Findings should be considered in light of study limitations. Responses may differ from those who chose not to participate, limiting generalizability. However, the demographics for this population are similar to that of our first survey which also surveyed GCs from the mailing lists of ABGC and NSGC [7]. Additionally, the term “medical interpreter” was not defined in the survey and it is unclear whether respondents were including family and staff as well as professional medical interpreters when answering.
There is an urgent need to increase availability of GCS for SSP and to understand the impact of currently used services on patient outcomes. In addition, because GCs rely greatly on the use of medical interpreters, understanding effective communication to SSP is a necessary area for future research.
Acknowledgements
This work was supported by the Breast Cancer Spore CA 116201 and in part by the Survey Methods Core Facility at the H. Lee Moffitt Cancer Center & Research Institute; a National Cancer Institute designated Comprehensive Cancer Center (P30-CA76292).
Footnotes
Conflict of interest Author Vadaparampil has a research grant from Myriad Genetics Laboratories. Authors Augusto, Lindor, and Couch declare no conflicts of interest.
Compliance with Ethical Standards
Ethical Approval All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent Informed consent was obtained from all individual participants included in this study.
References
- 1.DeSantis C, Ma J, Bryan L, Jemal A. Breast cancer statistics, 2013. CA Cancer J Clin. 2014;64(1):52–62. [DOI] [PubMed] [Google Scholar]
- 2.Parise CA, Caggiano V. The influence of socioeconomic status on racial/ethnic disparities among the ER/PR/HER2 breast cancer subtypes. J Cancer Epidemiol 2015 10.1155/2015/813456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wideroff L, Thomas Vadaparampil S, Breen N, Croyle RT, Freedman AN. Awareness of genetic testing for increased cancer risk in the year 2000 National Health Interview Survey. Public Health Genomics. 2003;6(3):147–56. [DOI] [PubMed] [Google Scholar]
- 4.Levy DE, Byfield SD, Comstock CB, Garber JE, Syngal S, Crown WH, SHields AE. Underutilization of BRCA1/2 testing to guide breast cancer treatment: black and Hispanic women particularly at risk. Genet Med. 2011;13(4):349–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kinney AY, Gammon A, Coxworth J, Simonsen SE, Arce-Laretta M. Exploring attitudes, beliefs, and communication preferences of Latino community members regarding BRCA1/2 mutation testing and preventive strategies. Genet Med. 2010;12(2):105–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Augusto BM, Lake P, Scherr CL, Couch FJ, Lindor NM, Vadaparampil ST. From the laboratory to the clinic: sharing BRCA VUS reclassification tools with practicing genetics professionals. J Community Genet 2017 10.1007/s12687-017-0343-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Scherr CL, Lindor NM, Malo TL, Couch FJ, Vadaparampil ST. Genetic counselors’ practices and confidence regarding variant of uncertain significance results and reclassification from BRCA testing. Clin Genet. 2015;88(6):523–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Andrus MR, Roth MT. Health literacy: a review. Pharmacotherapy. 2002;22(3):282–302. [DOI] [PubMed] [Google Scholar]
- 9.Lee E, Maxwel A, Baty BJ, Roter D, Dudley WN, Kinney AY. Genetic counseling communication with an African American BRCA1 kindred. Soc Sci Med. 2007;64(3):724–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Karliner LS, Jacobs EA, Chen AH, Mutha S. Do professional interpreters improve clinical care for patients with limited English proficiency? A systematic review of the literature. Health Serv Res. 2007;42(2):727–54. [DOI] [PMC free article] [PubMed] [Google Scholar]