Abstract
Purpose:
Hormonal variation throughout the menstrual cycle is posited to impact various physical and mental health symptoms; however, this is not observed in all women and mechanisms are not well understood. Difficulty in emotion regulation may elucidate differences women experience in physical and mental health functioning between menstrual phases. We examined the moderating role of difficulty in emotion regulation in the relation between menstrual phase and menstrual symptom severity and perceived control over anxiety-related events in healthy, regularly menstruating women.
Method:
The participants were 37 women (Mage = 26.5, SD = 9.6). A series of regression analyses were used to examine whether individual differences in emotion regulation difficulties moderate the relation between menstrual phase and our outcomes, severity of menstrual symptoms and perceived control over anxiety related events, using a within-subjects design.
Results:
The analyses revealed that difficulty in emotion regulation significantly moderated the relation between menstrual phase and perceived control over anxiety-related events (B = −0.42, p < .05), but not menstrual symptom severity.
Conclusion:
Women who reported higher emotion regulation difficulty experienced greater differences in perceived control over anxiety-related events between menstrual phases. Specifically, women lower in difficulty in emotion regulation report greater increase in control over anxiety during the late luteal phase compared to women with higher emotion regulation difficulty. Difficulty in emotion regulation may play an important role in understanding differences in menstrual phase-associated impairments, thereby informing the development of targeted interventions for vulnerable women.
Keywords: emotion regulation, menstrual symptoms, perceived control, menstrual cycle, anxiety
Introduction
Hormonal fluctuations during the menstrual cycle have been associated with an array of aversive mental and physical health symptoms (Backstrom et al., 2003; Freeman, 2003; Halbreich, 2003; Kowalczyk, Evans, Bisaga, Sullivan & Corner, 2006). The late luteal phase, occurring the week preceding menses, is characterized by decreases in progesterone and GABA receptor activity, which result in increased nervous system excitability, sleep disturbances, depressive and anxiety symptoms (Andreen et al., 2009; Ziomkiewicz et al., 2012), and physical symptoms, such as bloating, change in appetite, breast tenderness, and swelling (Milewicz & Jedrzejuk, 2006; Steiner, Dunn & Born, 2003). Conversely, the late follicular phase of the menstrual cycle, beginning immediately after the end of menses and ending at the onset of ovulation, is characterized by stable progesterone levels, fewer fluctuations in mood, and less intense physical symptoms (Gonda et al., 2008).
Notably, although 75% of women experience menstrual symptoms during the late luteal phase (i.e., premenstrual symptoms), just 3–8% meet criteria for premenstrual dysphoric disorder, a clinical diagnosis characterized by a combination of affective, cognitive, and physical symptoms that cause significant impairment in several areas of functioning (Halbreich, Borenstein, Pearlstein & Kahn, 2003). Thus, not all women experience menstrual cycle related changes in psychological (Romans, Clarkson, Einstein, Petrovic & Stewart, 2012) and physical health symptoms (Wolfram, Bellingrath & Kudielka, 2011), or significant impairment (Ziomkeiwicz, Wichary, Bochenek, Pawlowski & Jasienska, 2012). The extent to which hormonal shifts across the menstrual cycle differentially affect women may, in part, be explained by variability in underlying psychological factors that influence how women experience and respond to normal changes in symptoms due to menstrual cycle phase. For example, the ability to regulate one’s emotional states, (i.e., emotion regulation) may interplay with menstrual cycle phase to predict increases in negative affect and how individuals perceive their ability to control associated distress.
A leading clinically relevant conceptualization of emotion regulation suggests that it reflects individual differences in the ability to adaptively respond to distressing emotional states through awareness, understanding, and acceptance (Aldao, Nolen-Hoeksema & Schweizer, 2010; Gratz & Roemer, 2004; Mennin, Holaway, Fresco, Moore, & Heimberg, 2007), thereby promoting engagement in goal-directed behavior. In contrast to efforts to control emotion via suppression and avoidance, emotion regulation is associated with symptom improvement (e.g., Kumar, Feldman, & Hayes, 2008; Zanarini, Frankenburg, Hennen, & Silk, 2003). Given these relations, emotion regulation may inform differential psychological and physiological consequences of menstrual cycle-related changes and provide an inroad toward empirically driven interventions. For example, women who experience difficulty in emotion regulation may experience exacerbated symptoms in the context of typical hormonal fluctuations as a function of menstrual phase. Currently, the role of emotion regulation in terms of menstrual-cycle related symptoms has not been examined. However, difficulty in emotion regulation is associated with many psychological consequences, including worry, tension, and mood swings, as well as depression and anxiety (Aldao et al., 2010; Bargh & Williams, 2007).
The current investigation sought to examine the moderating role of emotion regulation difficulties in the relation between two menstrual cycle phase outcomes of interest: (1) menstrual symptom severity and (2) perceived control over anxiety-related events. Perceived control over anxiety-related events was identified as a relevant outcome; previous work in this domain has found that perceived control over anxiety is related to menstrual symptoms (Mahon, Nillni, Rohan & Zvolensky, 2015), and that specifically during the late luteal phase, women who are sensitive to anxiety report less control following a laboratory stressor (e.g., cognitive panic symptoms; Nillni, Rohan, & Zvolensky, 2012). Because efforts to control anxiety maligned with emotion regulation (e.g., avoidance and suppression) paradoxically exacerbate anxiety (Feldner, Zvolensky, Eifert & Spira, 2003; Feldner, Zvolensky, Stickle, Bonn-Miller & Leen-Feldner, 2006; Salters-Pedneault, Tull, & Roemer, 2004), it is possible that menstrual cycle-related changes in perceived control over anxiety-related events are moderated by one’s inherent difficulty in regulating emotions. Thus, we hypothesized that women in their late luteal phase, characterized as having relatively high difficulty in emotion regulation, would report more severe menstrual symptoms and perceive that they have less control over anxiety-related events, as compared to themselves during their late follicular phase and compared to women who have lower difficulty in emotion regulation, regardless of phase.
Materials and Methods
Women were recruited from a suburban university community in the northeast United States. The present study was approved by the institutional review board and is a secondary analysis of data from a larger study that examined panic responses across the menstrual cycle (Nillni et al., 2012). All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Subjects
A total of 65 healthy, normally menstruating women were enrolled in the original study. For the current investigation, inclusion criteria were (1) normal menstrual cycle length between 25 and 35 days, (2) variability in month-to-month cycle length by no more than 7 days, and (3) verification of both late luteal and late follicular phases (see the “Measures” section). The exclusion criteria included (1) use of hormonal birth control methods; (2) experiencing perimenopause symptoms or being postmenopausal; (3) currently pregnant or trying to become pregnant; (4) a current or past DSM-IV Axis I diagnosis of panic disorder with or without agoraphobia; (5) a current DSM-IV Axis I diagnosis of generalized anxiety disorder, specific phobia, posttraumatic stress disorder, social anxiety disorder, obsessive compulsive disorder, alcohol or substance dependence, or psychosis; (6) current serious suicidal intent; (7) contraindicated medical conditions (e.g., cardiovascular or seizure disorder, severe asthma); and (8) current use of anxiety medication (e.g. beta blockers, benzodiazepines, anxiolytics; for additional details, please see Nillni et al., 2012).
Measures
The Structured Clinical Interview for DSM-IV Axis I Disorders--non patient version (SCID-IV-NP; First, Spitzer, Gibbon & Williams, 1994) was used to assess for the presence of current and lifetime Axis I diagnoses and current suicidal ideation. The SCID-IV-NP was used in the present study to assess exclusionary criteria relating to current and past psychological disorders and suicidal intent. A doctoral student in clinical psychology with extensive training in DSM-IV criterion and SCID-IV-NP administration, who served as an independent rater, coded 10% of the interviews for diagnostic reliability. There were no disagreements between raters.
The Positive and Negative Affect Schedule (PANAS) was used to assess general positive affect and negative affect (e.g., past two weeks). The PANAS is composed of 10 emotion items (Watson, Clark & Tellegen, 1988), reflecting positive (PANAS-PA α = 0.91; e.g., attentive, interested, alert) and negative affect (PANAS-NA α = 0.90; e.g., distressed, hostile, irritable), which are rated on a 5-point Likert scale (1 = slightly or not at all to 5 = very much). General positive and negative affect, measured at baseline, were examined as theoretically relevant covariates.
The Difficulties in Emotional Regulation Scale is a validated 36-item self-report index that was developed by Gratz and Roemer (2004) to comprehensively assess deficits in emotion regulation. Items (e.g. I have difficulty making sense out of my feelings) are rated on a five-point Likert scale (1 = almost never to 5 = almost always) and assess six dimensions of emotion regulation. In the current investigation, the Difficulties in Emotional Regulation Scale was completed during the screening interview and the total score was used as a self-report index of difficulty in emotion regulation, such that a higher score indicates lower emotion regulation (Cronbach’s α = 0.93).
The Daily Record of Severity of Problems (DRSP) is a validated 14-item daily self-report questionnaire that measures severity of physical and psychological symptoms across the menstrual cycle (e.g., felt angry, irritable), including three impairment items scored on a 6-point Likert Scale (1 = Not at all to 6=Extreme). The DRSP was developed to aid in the assessment of DSM-IV criteria for premenstrual dysphoric disorder and to assess the severity of symptoms and impairment at various phases of the menstrual cycle (Endicott & Harrison, 2006). In this study, the DRSP was completed daily throughout the study duration (1–3 full menstrual cycles), to assess self-reported menstrual symptom severity. All the items were summed and averaged across phases to create separate late luteal and late follicular phase scores for each participant.
The Anxiety Control Questionnaire is a validated self-report measure of perceived control over anxiety-related events: control over one’s emotions, escape from frightening events, and coping in stressful situations. It is comprised of 15 statements (e.g., Most events that make me anxious are outside my control) that participants rate on a 6-point Likert-type scale based on their level of agreement (0 = strongly disagree to 5 = strongly agree; Rapee, Craske, Brown & Barlow, 1996). In the present study, the Anxiety Control Questionnaire total score was completed at both late luteal and late follicular phase laboratory visits to measure perceived control for anxiety related events; higher scores were indicative of greater perceived control over anxiety-related events. This measure also demonstrated high internal reliability (luteal phase Cronbach’s α = 0.87; follicular phase Cronbach’s α= 0.84).
Study Procedure
Participants first completed a screening visit consisting of a diagnostic interview (SCID-IV-NP) and a medical questionnaire to assess eligibility, which included confirmation of inclusion and exclusion criteria. In addition, they completed a battery of self-report measures. Participants were then sent home with instructions to complete the DRSP each day, and to conduct an at-home ovulation test. Menstrual phase was first estimated via self-report and then further assessed with at-home ovulation tests to determine the day of the luteinizing hormone peak. On the day of the luteinizing hormone peak, as determined by an in-home urine test, the participants contacted the lab and scheduled two follow-up visits. The first follow-up visit was randomized to occur either during their late luteal or late follicular phase, and the second follow-up visit was during the other phase, respectively. The late luteal phase visit was scheduled within 12–14 days after this peak, and the late follicular phase visit was scheduled between 6 and 12 days following the onset of menses. At each follow-up visit, participants were administered a battery of self-report questionnaires and were led through a laboratory stress challenge (for details, please see Nillni et al., 2012). Menstrual phase for lab visits was additionally verified via hormonal (progesterone) assay of saliva sample.
Analytic Strategy
First, Pearson’s and Spearman’s zero order correlations for continuous and categorical variables, respectively, were examined to inform selection of theoretically-relevant covariates as well as relations between the proposed moderator, difficulty in emotion regulation, and ratings of severity of menstrual symptoms and perceived control over anxiety-related events during the late follicular and luteal phases. To assess the moderating role of emotion regulation in the relation between menstrual phase and (1) severity of menstrual symptoms and (2) perceived control over anxiety-related events, in the context of our within-subjects design, we ran a series of regression analyses using ordinary least squares estimation (Judd, Kenny, & McClelland, 2001; Judd, McClelland, & Smith, 1996). Mean-centered scores were calculated to allow for direct interpretation of the intercept as the observed effect on our outcomes of interest for individuals with average difficulty in emotion regulation. To calculate difference scores for both outcomes of interest, we subtracted late follicular values from luteal values. As outlined by Judd et al. (1996; 2001), we first examined the overall effect of phase on our outcomes, using paired sample t tests. Next, we estimated the effect of phase, considering emotion regulation as a stable continuous moderator that affects the strength of the effect of phase on our outcomes. In two separate regression equations, we regressed the outcomes of interest as measured during the (1) late follicular phase and (2) late luteal phase on emotion regulation. As a test of the moderating effect of emotion regulation, we regressed the difference score between menstrual phases for each outcome on emotion regulation. Here, the slope represents the difference in the two initial regression slopes for the late follicular and late luteal phase, respectively, where a significant slope signifies a significant interaction (i.e., moderation) (Judd et al., 1996; 2001). All analyses were conducted in PASW 23.0 (IBM Corp, SPSS Statistics, Version 23.0, 2015)
Results
Participants
Of the 65 participants who enrolled in the parent investigation, 37 women (Mage = 26.4, SD = 9.5) were eligible for the current study. They primarily identified as non-Hispanic (94.6%), single (70.3%), and had completed some college education (54.1%). In terms of psychopathology, 10.8% met criteria for one or more current Axis I diagnosis based on the DSM-IV and 37.8% for past Axis 1 diagnosis. For additional demographic information, please see Table 1. On average, they scored a 69.4 on the DERS (SD = 17.2), suggesting relatively low difficulties with emotion regulation as compared to clinical samples (Gratz & Roemer, 2004).
Table 1.
Demographics (n=37)
| Characteristic | N | % or M (SD) |
|---|---|---|
| DER1 | 37 | 69.405 (17.20) |
| Ethnicity | ||
| Non-Hispanic | 35 | 94.6 |
| Hispanic or Latino | 2 | 5.4 |
| Race | ||
| American Indian | 2 | 5.4 |
| Asian | 2 | 5.4 |
| African American | 1 | 2.7 |
| White | 32 | 86.5 |
| Highest Level of Education | ||
| High School Degree | 1 | 2.7 |
| Some College | 20 | 54.1 |
| Graduated from a 2-year College | 1 | 2.7 |
| Graduated from a 4-year College | 11 | 29.7 |
| Graduated with a Masters Degree | 3 | 8.1 |
| Other | 1 | 2.7 |
| Marital Status | ||
| Single | 26 | 70.3 |
| Married | 9 | 24.3 |
| Living Together | 1 | 2.7 |
| Divorced | 1 | 2.7 |
| Any Axis 1 diagnosis2 | ||
| Current | 4 | 10.8 |
| Past | 14 | 37.8 |
Difficulty in Emotion (Difficulties in Emotion Regulation Scale, Gratz & Roemer, 2004);
Structured Clinical Interview for the DSM-IV-NP (First et al., 2002).
Pearson’s and Spearman’s Correlations
Based on significant relations with outcomes of interest, we included both positive and negative affect and current DSM-IV diagnosis (yes/no) as covariates in all regression models. In addition, we included past DSM-IV diagnosis (yes/no) as covariate models examining menstrual symptoms severity (please see Table 2).
Table 2.
Pearson’s and Spearman’s Rank Order Correlations
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | M (%) | SD | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Age | - | 0.22 | −0.20 | 0.15 | 0.30 | −0.03 | 0.01 | −0.22 | −0.25 | −0.05 | 26.38 | 9.51 |
| 2. PANAS-NA1 | - | - | −0.15 | 0.75** | 0.30 | 0.37* | 0.36* | −0.45** | −0.37* | 0.15 | 20.54 | 7.16 |
| 3. PANAS-PA1 | - | - | - | −0.26 | −0.34* | −0.23 | −0.13 | 0.39* | 0.39* | −0.33* | 35.03 | 7.46 |
| 4. Current Axis 12 | - | - | - | - | 0.87 | 0.38* | 0.47** | −0.35* | −0.21 | 0.06 | 10.80% | - |
| 5. Past Axis 12 | - | - | - | - | - | 0.48** | 0.31 | −0.30 | −0.28 | 0.28 | 37.80% | - |
| 6. DRSP-F3 | - | - | - | - | - | - | 0.70** | −0.29 | −0.30 | 0.35* | 20.81 | 5.80 |
| 7. DRSP-L3 | - | - | - | - | - | - | - | −0.31 | −0.31 | 0.35* | 26.64 | 10.90 |
| 8. PCOARE-F4 | - | - | - | - | - | - | - | - | 0.91** | −0.51** | 95.46 | 17.15 |
| 9. PCOARE-L4 | - | - | - | - | - | - | - | - | - | −0.64** | 97.43 | 19.13 |
| 10. DER5 | - | - | - | - | - | - | - | - | - | - | 69.41 | 17.2 |
correlation is significant at the 0.05 level (2-tailed);
correlation is significant at the 0.01 level (2-tailed).
Note. Current and Past Axis 1 Diagnosis: 1 = present, 0 = absent.
PANAS (Positive and Negative Affect Scale; Watson, et al., 1988);
Structured Clinical Interview for the DSM-IV-NP (First et al., 1994);
DRSP (Daily Report of Severity of Problems; Endicott & Harrison, 2006);
Perceived Control Over Anxiety Related Events (Anxiety Control Questionnaire; Rapee et al. 1996);
Difficulty in Emotion (Difficulties in Emotion Regulation Scale, Gratz & Roemer, 2004)
Moderation of difficulty in emotion regulation in the relation between Emotion Regulation menstrual phase and severity of menstrual symptoms
Paired sample t tests revealed a significant difference in menstrual symptoms between the late follicular (M = 20.81, SD = 5.80) and late luteal (M = 26.64, SD = 10.90) phases; t(35) = 4.37, p < .001. Table 3 provides a summary of the series of hierarchical multiple regression analyses used to examine moderation. In terms of late follicular phase menstrual symptoms, the positive and negative affect, as well as current or past diagnosis, accounted for 34.1% of the variance (F(4, 31) = 4.02, p < .01) at step 1, with past diagnosis (β = .45, t(33) = 2.71, p = .01) significantly predicting menstrual symptom severity. The addition of emotion regulation difficulty at step 2 accounted for an additional 5.2% of the variance (F(5, 30) = 3.89, p < .01), but emotion regulation difficulty was not a significant predictor (β = 0.25, t(30) = 1.61, p = .12). In terms of late luteal phase menstrual symptoms, step 1 accounted for 30.3% of the variance (F(4, 31) = 3.37, p = .02) with past diagnosis being marginally related (β = 0.33, t(31) = 1.93, p = .06), and current diagnosis being significantly related (β = 0.59, t(31) = 2.36, p = .02) to severity of menstrual symptoms. The inclusion of emotion regulation difficulty at step 2 accounted for a 9.2% variance (F(5, 30) = 3.92, p < .01), with emotion regulation significantly predicting symptoms (β = 0.33; t(30) = 2.13, p=.04). In terms of change (e.g., difference) in severity of menstrual symptoms between phases, neither step 1 nor step 2 of the model was significant. Thus, we can conclude that emotion regulation does not significantly moderate phase differences in severity in menstrual symptoms.
Table 3.
Regression Analyses Predicting Severity of Menstrual Symptoms4
| Variable | DRSP_Follicular4 | DRSP_Luteal4 | DRSP_Difference4 | ||||||
|---|---|---|---|---|---|---|---|---|---|
| B | SE B | β | B | SE B | β | B | SE B | β | |
| Step 1 | |||||||||
| PANAS_NA1 | −..02 | 1.29 | −.03 | −.24 | .38 | −.16 | −.22 | .31 | −.20 |
| PANAS_PA1 | .01 | .13 | .01 | .16 | .24 | .11 | .15 | .20 | .14 |
| Past Diagnosis2 | 5.38 | 1.98 | .45* | 7.40 | 3.83 | .33+ | 2.02 | 3.11 | .12 |
| Current Diagnosis2 | 6.55 | 4.38 | .36 | 20.00 | 8.47 | .59* | 13.46 | 6.86 | .54+ |
| ΔR2 | 0.34 | 0.30 | .16 | ||||||
| F for change in R2 | 4.02** | 3.37* | 1.43 | ||||||
| Step 2 | |||||||||
| PANAS_NA1 | −.06 | .19 | −.08 | −.35 | .36 | −.23 | −.28 | .30 | −.26 |
| PANAS_PA1 | .07 | .19 | −.08 | .31 | .24 | .21 | .24 | .20 | .23 |
| Past Diagnosis2 | 4.97 | 1.95 | .42* | 6.40 | 3.66 | .29+ | 1.42 | 3.07 | .09 |
| Current Diagnosis2 | 7.45 | 4.31 | .41+ | 22.24 | 8.09 | .65* | 14.79 | 6.78 | .59* |
| DERS3 | .08 | .05 | .25 | .21 | .10 | .33* | .12 | .08 | .27 |
| ΔR2 | 0.05 | 0.09 | .06 | ||||||
| F for change in R2 | 3.89** | 3.92** | 1.66 | ||||||
p < .05.
p < .01.
p > .05 and ≤ .1
PANAS (Positive and Negative Affect Scale; Watson et al., 1988);
Structured Clinical Interview for the DSM-IV-NP (First et al., 1994);
DERS (Difficulties in Emotion Regulation Scale; Gratz & Roemer, 2004)
DRSP (Daily Report of Severity of [Menstrual] Problems; Endicott et al., 2006);
Perceived Control Over Anxiety Related Events (Anxiety Control Questionnaire; Rapee et al. 1996)
Moderation of difficulty in emotion regulation in the relation between menstrual phase and perceived control over anxiety-related events
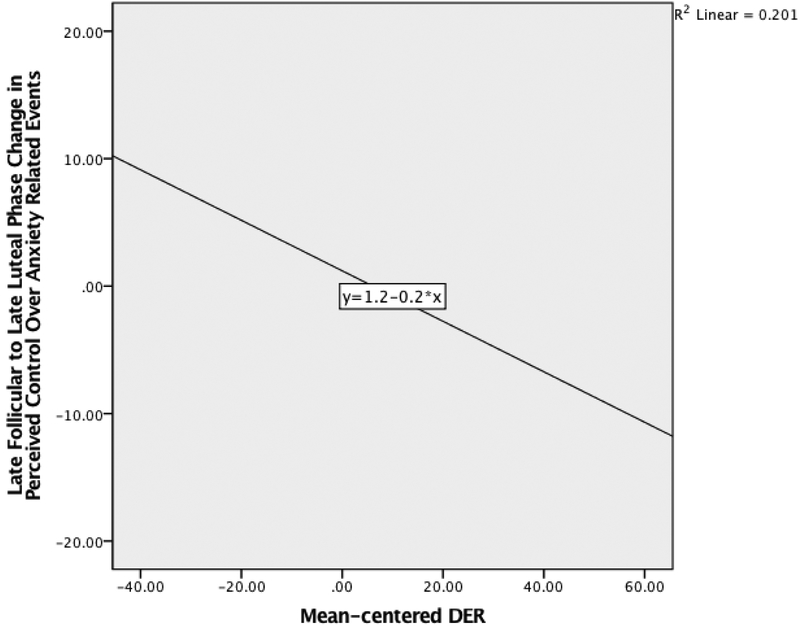
Paired sample t tests revealed there was no significant difference in perceived control over anxiety-related events between the late follicular (M = 95.46, SD = 17.15) and late luteal phases (M = 97.43, SD = 19.12) phases; t(36) = 1.48, p = .15). Table 4 provides a summary of the series of hierarchical multiple regression analyses used to examine moderation. In terms of perceived control over anxiety-related events in the late follicular phase, entering positive and negative affect and past diagnosis at step 1 accounted for 31.7% of the variance (F(3, 33) = 5.11, p < .01). Both negative (β = −0.47, t(33) = −2.17, p < .05) and positive affects (β = .5, t(33) = 2.32, p < .05) were significantly related to perceived control over anxiety-related events. The addition of emotion regulation difficulty at step 2 accounted for an additional 12.9% of the variance (F(4, 32) = 6.46; p = .001), and emotion regulation difficulty was significantly related to perceived control over anxiety-related events (β = −0.39, t(32) = −2.74, p = .01). A similar pattern was observed in relation to perceived control over anxiety-related events in the late luteal phase with step 1 accounting for 28.9% of the variance (F(3, 33)=4.47, p=.01). Again, negative (β=−.53 t(33)=−2.38, p<.05) and positive affect (β=0.39, t(33)= 2.5 p<.05) were significant predictors. The inclusion of emotion regulation difficulty at step 2 accounted for 23.8% additional variance (F(4, 32) = 8.91, p < .001), and emotion regulation was a significant predictor (β = −0.53, t(32) = −4.01, p < .001). In terms of change in perceived control over anxiety-related events between phases, step 1 of the model was non-significant. At step 2, the inclusion of emotion regulation difficulty accounted for a significant 15.3% of model variance (F(4, 32) = 2.87, p < .05), and emotion regulation was significantly related to change in perceived control over anxiety-related events between menstrual phases (β = −0.42, t(32) = −2.58, p < .05). Thus, we can conclude that emotion regulation significantly moderates phase differences in perceived control over anxiety-related events, with larger differences between phases observed for those with greater emotion regulation difficulties (please see Figure 1).
Table 4.
Regression Analyses Predicting Severity of Perceived Control over Anxiety Related Events5
| Variable | PCOARE_Follicular5 | PCOARE_Luteal5 | PCOARE_Difference5 | ||||||
|---|---|---|---|---|---|---|---|---|---|
| B | SE B | β | B | SE B | β | B | SE B | β | |
| Step 1 | |||||||||
| PANAS_NA1 | −1.13 | .52 | −.47* | −1.41 | .59 | −.53* | −.28 | .28 | −.25 |
| PANAS_PA1 | .80 | .34 | .35* | 1.00 | .39 | .39* | .20 | .19 | .18 |
| Current Diagnosis2 | 5.26 | 12.16 | .10 | 17.42 | 13.84 | .30 | 12.16 | 6.56 | .47+ |
| ΔR2 | 0.32 | 0.29 | .11 | ||||||
| F for change in R2 | 5.11* | 4.47** | 1.38 | ||||||
| Step 2 | |||||||||
| PANAS_NA1 | −.88 | .49 | −.37+ | −1.02 | .50 | −.38* | −.15 | .27 | −.13 |
| PANAS_PA1 | .48 | .34 | .21 | .51 | .35 | .20 | .04 | .18 | .03 |
| Current Diagnosis2 | .17 | 11.27 | .00 | 9.70 | 1.62 | .16 | .37 | 1.55 | .13 |
| DERS3 | −.39 | .14 | −.39** | −.59 | .15 | −.53** | −.20 | .07 | −.42* |
| ΔR2 | 0.13 | 0.24 | .15 | ||||||
| F for change in R2 | 6.46** | 8.91** | 2.87+ | ||||||
p < .05.
p < .01.
p > .05 and ≤ .1
PANAS (Positive and Negative Affect Scale; Watson et al., 1988);
Structured Clinical Interview for the DSM-IV-NP (First et al., 1994);
DERS (Difficulties in Emotion Regulation Scale; Gratz & Roemer, 2004);
DRSP (Daily Report of Severity of [Menstrual] Problems; Endicott et al., 2006);
Perceived Control Over Anxiety Related Events (Anxiety Control Questionnaire; Rapee et al. 1996
Figure 1. Change in Perceived Control Over Anxiety Related Events is Moderated by DER.
Note. Regression line fitted based on mean-centered DER and perceived control over anxiety related events difference scores, not including model
Discussion
The menstrual cycle and associated hormonal fluctuations that women experience have been empirically linked to aversive physical and mental health symptoms (Backstrom et al., 2003; Freeman, 2003; Halbreich, 2003; Kowalczyk et al., 2006). Women who report greater difficulty in emotion regulation may be at greater risk for menstrual symptoms and emotional interference as a function of their menstrual phase. The present investigation examined whether relative elevations in difficulty in emotion regulation moderate the relation between menstrual phase and severity of menstrual symptoms and perceived control over anxiety related events. Partially consistent with study hypotheses, difficulty in emotion regulation moderated the relation between menstrual phase and perceived control over anxiety-related events, such that the difference in perceived control over anxiety-related events between menstrual phases is greater among women low in difficulty in emotion regulation. However, difficulty in emotion regulation did not moderate changes in menstrual symptom severity between menstrual phases.
Consistent with previous research, we found that during the late luteal phase, women report significantly greater menstrual symptoms, as compared to during their late follicular phase (Andreen et al., 2009; Gonda et al., 2008; Milewicz & Jedrzejuk, 2006; Ziomkiewicz et al., 2012). Emotion regulation difficulties were not related to severity of menstrual symptoms in the late follicular phase but were related to severity of symptoms reported during the late luteal phase; we found no evidence of an interaction between emotion regulation difficulties and menstrual phase in the prediction of menstrual symptom severity. This finding suggests while individual differences in difficulty in emotion regulation may affect menstrual symptom ratings during the late luteal phase, they do not affect the extent to which symptoms change between the late follicular and late luteal phase.
A nearly opposite, and somewhat unexpected, relation was observed in the examination of changes in perceived control over anxiety-related events between menstrual phases. Here, no main effect of phase was observed, which suggests that on average, our sample did not report significant differences in perceived control over anxiety-related events between examined menstrual phases. This is consistent with trait-like conceptualizations of perceived control over anxiety-related events (Brown et al., 2004). Despite this, we observed a relation between difficulty in emotion regulation and perceived control over anxiety-related events during both menstrual phases. The direction of our findings suggests that women who report less difficulty in emotion regulation report greater perceived control over anxiety-related events throughout the menstrual cycle. Also, we found evidence that difficulty in emotion regulation moderates the strength of the difference in these ratings between phases. The interaction suggests that women with lower difficulty in emotion regulation reported an even greater increase in perceived control over anxiety during the late luteal phase, as compared to their late follicular phase. This suggests that having low difficulty in emotion regulation may be conceptualized as a resiliency factor and having high difficulty in emotion regulation as a risk factor. Although this finding warrants replication, women with lower difficulty in emotion regulation may be better poised to cope with and therefore feel in control of changes in anxiety that may occur, in part due to hormonal fluctuations, whereas women with higher difficulty in emotion regulation may be at greater risk for emotional vulnerability. Also, the late luteal phase may serve as an in vivo opportunity to utilize emotion regulation strategies, thereby bolstering one’s self-efficacy or sense of control in the context of stress. This is aligned with research suggesting that the use of emotion regulation strategies (e.g., mindfulness; (re)appraisal of a stressor as controllable; Erisman & Roemer, 2010) is associated with less affective distress (Erisman & Roemer, 2010) and physical distress (Kassam, Koslov, & Mendes, 2009). The interaction additionally underscores the important role that emotional vulnerability (e.g., emotion regulation) may play in cognitive-based processes across various contexts (e.g., menstrual phase changes). Perceived control over anxiety-related events remains an important cognitive vulnerability to consider in the context of menstrual distress given that past work indicates a relation between perceived control over anxiety-related events and menstrual symptom severity (Mahon et al., 2015).
Clinically, given the interaction between difficulty in emotion regulation and menstrual phase, it is possible that interventions to improve emotion regulation may diminish one’s self-efficacy in managing anxiety-relevant distress. Additionally, it is possible that pharmacological interventions (e.g., hormonal birth control; Benagiano, Bastianelli, & Farris, 2008) prescribed to reduce the fluctuations in hormones, such as progesterone, may provide an additional avenue by which to reduce potential negative outcomes for those with high difficulty in emotion regulation. Moreover, exposure-based therapies may consider the additional clinical utility of conducting exposures during the late luteal phase, which may maximize therapeutic outcomes and diminish treatment setbacks (Moscovitch, Antony, & Swinson, 2009; Powers, Smits, Leyro, & Otto, 2006).
Several limitations to the current investigation warrant discussion. First, due to the small sample size, replication is necessary in a larger, more diverse group of women in order to increase confidence in these findings. Furthermore, our relatively clinically healthy and homogenous sample may reduce the generalizability of our findings to clinical populations. For example, there was a low prevalence of current (10.8%) and past (37.8%) psychopathology, and women evidenced relatively low scores on the index of difficulty in emotion regulation (M = 69.41) as compared with previously observed scores in clinical samples (M = 77.99; Gratz & Roemer, 2004). Second, the observed relations were examined between two menstrual phases. Future work would benefit from examining difficulty in emotion regulation as a moderator of day-to-day changes in menstrual symptoms and perceived control over anxiety-related events throughout the entire menstrual phase. Related, the Daily Record for Severity of Problems (DRSP) was collected for just one month in the majority of the sample (68%), with just 27% and 5% completing two and three months of ratings, respectively. Future studies should consider analyzing the severity of menstrual symptoms for multiple cycles to confirm consistency. Finally, although our sample was screened for the use of hormonal contraception, hormone levels vary considerably between women; therefore, future work should include direct measurement of female hormones that may help elucidate differences in women’s experiences throughout the menstrual phase, which may, in part, explain different outcomes (Backstrom et al., 2003; Halbreich, 2003).
Together, the current investigation extends work on emotion regulation as a construct relevant to various forms of psychopathology to menstrual phase interference in women. Specifically, the results suggest that individual differences in emotion regulation difficulty may not affect varying severity of menstrual symptoms between women. However, difficulty in emotion regulation may be related to perceived control over-anxiety related events, with women who report less difficulty in emotion regulation experiencing greater improvements in perceived control over anxiety during the late luteal phase as compared to their ratings during the late follicular phase.
Acknowledgments
This project was conducted as a part of a larger study funded under Yael I. Nillni by National Institute of Mental Health—1R36MH086170–01A1.
Footnotes
Conflict of Interest The authors declare that they have no conflict of interest.
References
- Aldao A, Nolen-Hoeksema S, & Schweizer S (2010). Emotion-regulation strategies across psychopathology: A meta-analytic review. Clinical Psychology Review, 30(2), 217–237. [DOI] [PubMed] [Google Scholar]
- Andreen L, Nyberg S, Turkmen S, van Wingen G, Fernandez G, & Backstrom T (2009). Sex steroid induced negative mood may be explained by the paradoxical effect mediated by GABAA modulators. Psychoneuroendocrinology, 34(8), 1121–1132. [DOI] [PubMed] [Google Scholar]
- Bäckström T, Andreen L, Birzniece V, Björn I, Johansson IM, Nordenstam- Haghjo M, Nyberg S, Sundström-Poromaa I, &Wahlström G, Wang M (2003). The role of hormones and hormonal treatments in premenstrual syndrome. CNS Drugs, 17(5), 325–342. [DOI] [PubMed] [Google Scholar]
- Bargh JA, & Williams LE (2007). On the nonconscious of emotion regulation In Gross J (Ed.), Handbook of Emotion Regulation (pp. 429–445). New York, NY: Guilford Press. [Google Scholar]
- Benagiano G, Bastianelli C, & Farris M (2008). Hormonal contraception: present and future. Drugs of Today, 44(12), 905. [DOI] [PubMed] [Google Scholar]
- Brown TA, White KS, Forsyth JP, & Barlow DH (2004). The structure of perceived emotional control: Psychometric properties of a revised anxiety control questionnaire. Behavior Therapy, 35(1), 75–99. [Google Scholar]
- Endicott J, & Harrison W (2006). Daily Record of Severity of Problems (DRSP): Reliability and validity. Archives of Women’s Mental Health, 9, 41–49. [DOI] [PubMed] [Google Scholar]
- Erisman SM, & Roemer L (2010). A preliminary investigation of the effects of experimentally induced mindfulness on emotional responding to film clips. Emotion, 10(1), 72–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feldner MT, Zvolensky MJ, Eifer GH, & Spira AP (2003). Emotional avoidance: an experimental test of individual differences and response suppression using biological challenge. Behavior Research and Therapy, 41(4), 403–411. [DOI] [PubMed] [Google Scholar]
- Feldner MT, Zvolensky MJ, Stickle TR, Bonn-Miller MO, & Leen-Feldner EW (2006). Anxiety sensitivity-physical concerns as a moderator of the emotional consequences of emotion suppression during biological challenge: An experimental test using individual growth curve analysis. Behavior Research and Therapy, 44(2), 249–272. [DOI] [PubMed] [Google Scholar]
- First M, Spitzer R, Gibbon M, Williams J (1994) Structured clinical interview for DSM-IV Axis I disorders-nonpatient edition Biometrics Research Department, New York [Google Scholar]
- Freeman EW (2003). Premenstrual syndrome and premenstrual dysphoric disorder: definitions and diagnosis. Psychoneuroendocrinology, 28(3), 25–37. [DOI] [PubMed] [Google Scholar]
- Gonda X, Telek T, Jusahz G, Lazary J, Vargha A, & Bagdy G (2008). Patterns of mood changes throughout the reproductive cycle in healthy women without premenstrual dysphoric disorder. Progress in Neuropsychopharmacology and Biological Psychiatry, 32, (1782–1788). [DOI] [PubMed] [Google Scholar]
- Gratz KL, & Roemer L (2004). Multidimensional assessment of emotional regulation and dysregulation: Development, factor structure, and initial validation of the Difficulties in Emotion Regulation Scale. Journal of Psychopathology and Behavioral Assessment, 26(1), 41–54. [Google Scholar]
- Halbreich U (2003). The etiology, biology and evolving pathology of premenstrual syndromes. Psychoneuroendocrinology, 28(3), 55–99. [DOI] [PubMed] [Google Scholar]
- Halbreich U, Borenstein J, Pearlstein T, & Kahn LS (2003). The prevalence impairment, impact, and burden of premenstrual dysphoric disorder (PMS/PMDD). Psychoneuroendocrinology. 28(3), 1–23. [DOI] [PubMed] [Google Scholar]
- IBM Corp. Released 2015. IBM SPSS Statistics for Windows, Version 23.0. Armonk, NY: IBM Corp. [Google Scholar]
- Judd CM, Kenny DA, & McClellan GH (2001). Estimating and testing mediation and moderation in within-subject designs. Psychological methods, 6(2), 115. [DOI] [PubMed] [Google Scholar]
- Judd CM, McClelland GH, & Smith ER (1996). Testing treatment by covariate interactions when treatment varies within subjects. Psychological Methods. 1(4), (366–378) [Google Scholar]
- Kassam KS, Koslov K, & Mendes WB (2009). Decisions under distress: stress profiles influence anchoring and adjustment. Psychological Science, 20(11), 1394–1399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kowalczyk WJ, Evans SM, Bisaga AM, Sullivan MA, & Corner SD (2006). Sex differences and hormonal influences on response to cold pressor pain. The Journal of Pain, 7(3), 151–160. [DOI] [PubMed] [Google Scholar]
- Kumar S, Feldman G & Hayes A (2008). Changes in mindfulness and emotion regulation in an exposure-based cognitive therapy for depression. Cognitive Therapy and Research, 32(6), 734–744. [Google Scholar]
- Mahon JN, Rohan KJ, Nillni YI, & Zvolensky MJ (2015). The role of perceived control over anxiety in prospective symptom reports across the menstrual cycle. Archives of Women’s Mental Health, 18(2), 239–246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mennin DS, Holaway RB, Fresco DM, Moore MT, & Heimberg RG (2007). Delineating components of emotion and its dysregulation in anxiety and mood psychopathology. Behavior Therapy, 38(3), 284–302. [DOI] [PubMed] [Google Scholar]
- Milewicz A, & Jedrzejuk D (2006). Premenstrual syndrome: From etiology to treatment. Maturitas, 55(1), S47–S54. [Google Scholar]
- Moscovitch DA, Antony MM, & Swinson RP (2009). Exposure-based treatments for anxiety disorders: Theory and process. Oxford Handbook for Anxiety and Related Disorders, 461–475. [Google Scholar]
- Nillni YI, Rohan KJ, & Zvolensky MJ (2012). The role of menstrual cycle phase and anxiety sensitivity in catastrophic misinterpretation of physical symptoms during a CO2 challenge. Archives of Women’s Mental Health, 15, 413–422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powers MB, Smits JAJ, Leyro TM, & Otto M (2006). Translational research perspectives on maximizing the effectiveness of exposure therapy In Richard DCSand Lauterbach D (Eds). Handbook of Exposure Therapies, Academic Press. [Google Scholar]
- Rapee RM, Craske MG, Brown TA, & Barlow DA (1996). Measurement of perceived control over anxiety-related events. Behavioral Therapy, 27, 279–293. [Google Scholar]
- Romans S, Clarkson R, Einstein G, Petrovic M, & Stewart D (2012). Mood and menstrual cycle: A review of prospective data studies. Gender Medicine, 9, 361–384. [DOI] [PubMed] [Google Scholar]
- Salters-Pedneault K, Tull MT, & Roemer L (2004). The role of avoidance of emotional material in the anxiety disorders. Applied and Preventative Psychology 11(2), 95–114. [Google Scholar]
- Steiner M, Dunn E, & Born L (2003). Hormones and mood: from menarche to menopause and beyond. Journal of Affective Disorders, 74(1), 67–83. [DOI] [PubMed] [Google Scholar]
- Watson D, Clark LA, & Tellegen A (1988). Development and validation of brief measure of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology, 54(6), 1063–1070. [DOI] [PubMed] [Google Scholar]
- Wolfram M, Bellingrath S, & Kudielka BM (2011). The cortisol awakening response (CAR) across the female menstrual cycle. Psychoneuroendocrinology, 36(6), 905–912. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Frankenburg FR, Hennen J, & Silk KR (2003). The longitudinal course of borderline psychopathology: 6-year prospective follow-up of the phenomenology of borderline personality disorder. American Journal of Psychiatry, 160(2), 274–283. [DOI] [PubMed] [Google Scholar]
- Ziomkiewicz A, Pawlowski B, Ellison PT, Lipson SF, Thune I, & Jasienska G (2012). Higher luteal progesterone is associated with low levels of premenstrual aggressive behavior and fatigue. Biological Psychology, 91(3), 376–382. [DOI] [PubMed] [Google Scholar]
- Ziomkeiwicz A, Wichary S, Bochenek D, Pawlowski B, & Jasienska G (2012). Temperament and ovarian reproductive hormones in women: Evidence from a study during the entire menstrual cycle. Biological Psychology, 61(4), 535–540. [DOI] [PubMed] [Google Scholar]