Background
Radiation therapy plays an increasingly important role in the treatment of pancreatic cancer (PC). Studies have shown that aggressive local treatment with radiation dose escalation can improve local control.1, 2 Stereotactic body radiation therapy (SBRT) uses advanced imaging technology to verify the target lesion setting before and during radiation therapy and allows for the accurate delivery of high-dose radiation to pancreatic tumors.3
Major challenges for SBRT include respiratory organ motion and accurate assessment of tumor size and location in real time. SBRT usually relies on fiducial markers to track the location of the tumor in real time. This ensures that the treatment is delivered to the tumor with high precision while decreasing toxicity to normal surrounding tissue.4
The aim of this video (Video 1, available online at www.VideoGIE.org) is to describe the technique for placement of EUS-guided fiducial markers in the treatment of locally advanced PC.
Fiducial Markers Overview
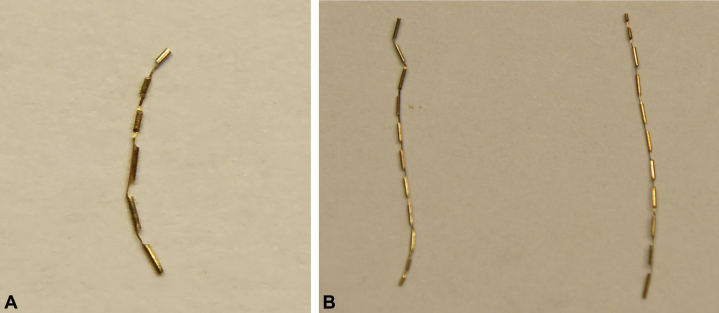
Fiducials are radiographically visible markers (spheres, coils, or seeds), usually made of gold, that are inserted into the target lesion in the pancreas (Fig. 1). Various types of fiducial markers and different delivery systems have been developed. Given the excellent visualization of the pancreas, EUS offers a viable approach for fiducial placement. The technique for fine-needle injection of fiducials is similar to that of FNA. Fiducials can be delivered with 19-gauge or 22-gauge needles, or by multifiducial delivery systems.5, 6 The 22-gauge needle has a greater flexibility and can be used in challenging anatomic locations or postsurgical anatomy. Conventional fiducials are cylindrical gold seeds, 3 to 5 mm long and 0.75 to 1.2 mm in diameter. These fiducials are deployed with a 19-gauge FNA needle. Smaller and longer fiducial markers have been developed and can be used with a 22-gauge needle, providing more flexibility.
Figure 1.
A, Gold fiducial marker, notched, 0.28 × 10 mm. B, Gold fiducial markers, notched, 0.28 × 20 mm.
The back-loading technique is the most common method used to load the fiducial marker into the EUS needle. The stylet is withdrawn approximately 3 cm. The fiducial marker, which is loaded on a needle carrier, is then inserted into an FNA needle tip. The fiducial is deployed into the needle tip by removing the needle carrier. Sterile bone wax is used to seal the tip of the FNA needle to secure the fiducial. The needle is then advanced down the operating channel of the echoendoscope. Once a safe insertion window has been identified, the needle is inserted into the target lesion under EUS guidance. Upon needle insertion into the target lesion, the fiducial is deployed by simultaneously retracting the needle while advancing the stylet. The needle is withdrawn from the echoendoscope and reloaded with a new fiducial, and the technique is repeated until the desired number of markers has been placed.
Fiducials are also available preloaded on a needle carrier delivery device for use with a 19-gauge or 22-gauge needle to be deployed under EUS guidance. There is not enough evidence that preloaded devices have better results than traditional hand-loaded devices, but they appear to be labor saving, given the reduced need for setup before the procedure.
Generally, at least 3 fiducial markers should be placed in different EUS viewing planes so that the pancreatic tumor borders and planes can be well defined during SBRT simulation and delivery.
Apart from the technical deployment, visualization during simulation for SBRT is of paramount importance.7 However, there are no firm recommendations regarding the optimal type of fiducial markers to be deployed considering visualization and level of artifacts on SBRT simulation and planning CT scans.
EUS-guided fiducial placement for GI malignancies is feasible, with a high technical success rate of 98%, according to a recent meta-analysis that included more than 1000 patients.8 The same study showed that EUS-guided fiducial placement is safe, with a pooled adverse events rate of 4%. Reported adverse events included mild acute pancreatitis, minor bleeding, fever, vomiting, abdominal pain, rectal pain, or elevated liver enzymes.8
Role of Fiducial Markers in SBRT
Studies have shown that fiducial markers improve the accuracy of target delineation during SBRT when compared with localization by the use of adjacent bony anatomy.9, 10, 11 Fiducial tracking is typically preferred when available.
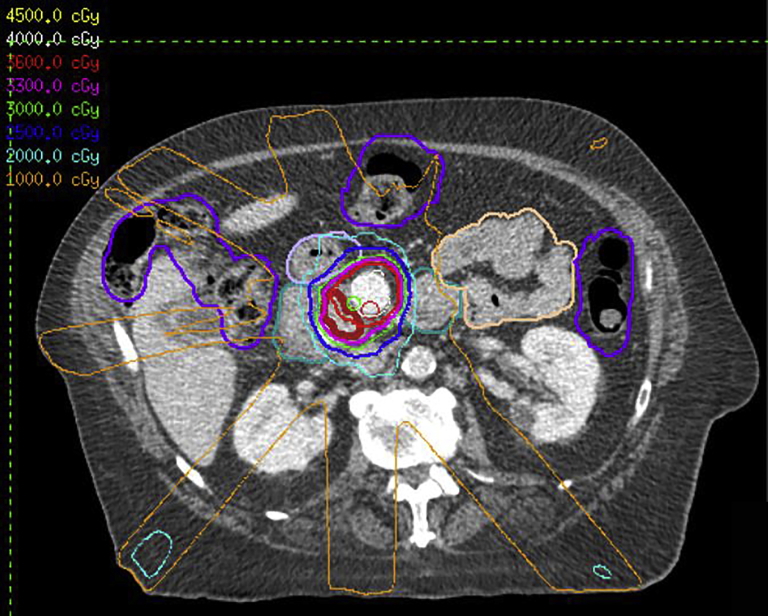
After the placement of fiducials, patients undergo SBRT simulation in order to map out the radiation treatment site and determine the appropriate dosage of radiation for the target tumor while reducing the dosage to nearby tissues. During simulation, the patient is placed in the desired treatment position for CT imaging to guarantee reproducibility during treatment delivery. During SBRT treatment planning, the goal is to identify the tumor volume, the normal tissue structures, and the total radiation dose and coverage to the desired volume while avoiding healthy surrounding tissues (Fig. 2). SBRT treatment involves a total radiation dose ranging from 25 to 55 Gy delivered over 1 to 5 fractions. SBRT delivery for pancreatic tumors has been shown to be safe and successful at achieving high local control rates.3
Figure 2.
Example of dose distribution on a stereotactic body radiation therapy-planning CT scan.
Illustrative Case with Technical Description
A 73-year-old man presented at our tertiary cancer center with a newly diagnosed borderline resectable pancreatic head adenocarcinoma. The mass measured 39 mm × 26.7 mm on the abdominal CT scan (Fig. 3). The plan of treatment included neoadjuvant chemotherapy and subsequent SBRT delivery. After completion of chemotherapy and many multidisciplinary consultations, the patient was referred for EUS-guided placement of fiducial markers within the pancreatic head tumor for SBRT.
Figure 3.
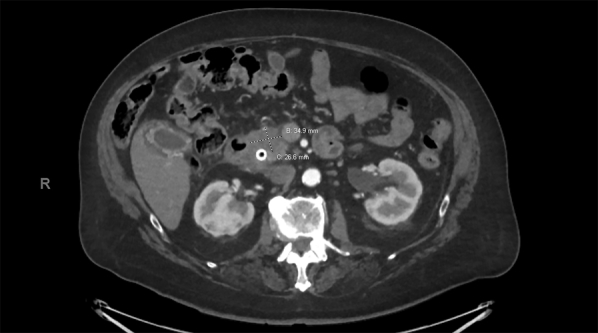
Abdominal CT scan with pancreatic protocol showing a poorly defined mass in the pancreatic head, measuring 30 × 41 mm.
Fiducial markers can be placed upfront at the time of EUS-guided FNA. However, given the controversies about the management of PC, the fiducial markers are not typically placed at the time of EUS-FNA.
Before placement of the fiducial marker, a full EUS assessment was completed to evaluate the tumor location, size, and surrounding vasculature. A hypoechoic lesion was identified in the pancreatic head, and a hyperechoic metal stent was seen next to it (Fig. 4). The FNA needle was inserted into the target lesion at an avascular angle. Tracking of the needle was performed to create a space for the fiducial marker to be placed. The first fiducial marker was deployed at the margin of the tumor, near the metal stent, and appeared as a bright chain on EUS (Fig. 5). For this patient, a total of 3 fiducials were placed into the pancreatic head tumor in different EUS viewing planes. The next 2 fiducial markers were deployed with the preloaded devices. All 3 fiducial markers were confirmed on EUS.
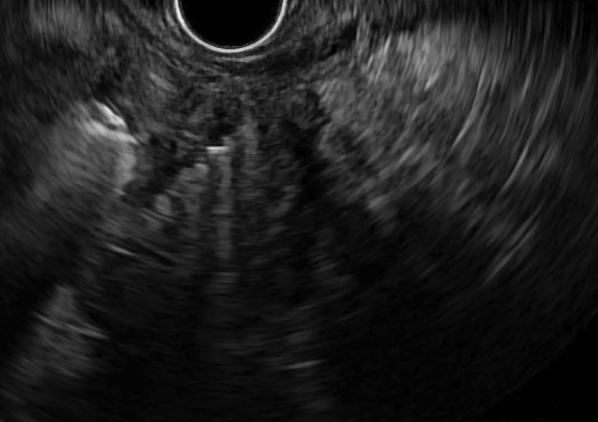
Figure 4.
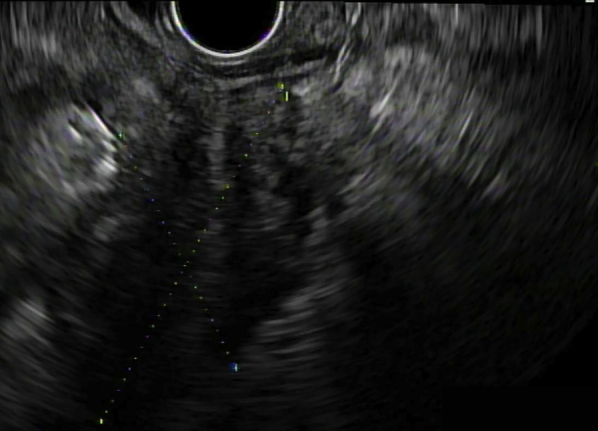
EUS view showing a heterogeneous hypoechoic mass in the pancreatic head, measuring 39 × 26.7 mm.
Figure 5.
Gold fiducial marker (0.28 × 20 mm) placed inside the target lesion, seen by EUS as a hyperechoic object.
Conclusion
The application of SBRT to locally advanced or metastatic PC usually requires the use of fiducial markers to track the precise location of the tumor in real time. This advancement in radiation therapy technique can contribute to tumor downstaging and improve the chances of secondary resection; furthermore, it can enhance local control for unresectable disease and facilitate palliation of obstructive symptoms. In clinical practice, the decision to use EUS-guided fiducial placement requires a multidisciplinary approach involving gastroenterologists, oncologists, surgeons, and radiation oncologists.
Disclosure
Dr Bhutani is the recipient of research support from Oncosil, Galera, and Augmenix. Dr Taniguchi is the recipient of research support from Galera and CyberKnife. Dr Herman is the recipient of research support from Oncosil, Galera, and Aduro and a consultant for Augmenix, BTG, AbbVie, Celgene, AstraZenica, BMS, Varian, and Boston Scientific. All other authors disclosed no financial relationships relevant to this publication.
Footnotes
E. Coronel and B. S. Singh are joint first authors.
Supplementary data
EUS-guided placement of gold fiducial markers in a pancreatic head adenocarcinoma to guide delivery of stereotactic body radiation therapy.
References
- 1.Milano M.T., Chmura S.J., Garofalo M.C. Intensity-modulated radiotherapy in treatment of pancreatic and bile duct malignancies: toxicity and clinical outcome. Int J Radiat Oncol Biol Phys. 2004;59:445–453. doi: 10.1016/j.ijrobp.2003.11.003. [DOI] [PubMed] [Google Scholar]
- 2.Chang D.T., Schellenberg D., Shen J. Stereotactic radiotherapy for unresectable adenocarcinoma of the pancreas. Cancer. 2009;115:665–672. doi: 10.1002/cncr.24059. [DOI] [PubMed] [Google Scholar]
- 3.de Geus S.W.L., Eskander M.F., Kasumova G.G. Stereotactic body radiotherapy for unresected pancreatic cancer: a nationwide review. Cancer. 2017;123:4158–4167. doi: 10.1002/cncr.30856. [DOI] [PubMed] [Google Scholar]
- 4.Cheesman A.R., DiMaio C.J. Role and technique of endoscopic ultrasound placement of fiducial markers in gastrointestinal malignancies. Tech Gastrointest Endosc. 2017;19:213–218. [Google Scholar]
- 5.DiMaio C.J., Nagula S., Goodman K.A. EUS-guided fiducial placement for image-guided radiation therapy in GI malignancies by using a 22-gauge needle (with videos) Gastrointest Endosc. 2010;71:1204–1210. doi: 10.1016/j.gie.2010.01.003. [DOI] [PubMed] [Google Scholar]
- 6.Park W.G., Yan B.M., Schellenberg D. EUS-guided gold fiducial insertion for image-guided radiation therapy of pancreatic cancer: 50 successful cases without fluoroscopy. Gastrointest Endosc. 2010;71:513–518. doi: 10.1016/j.gie.2009.10.030. [DOI] [PubMed] [Google Scholar]
- 7.Machiels M., van Hooft J., van Berge Henegouwen M.I. Endoscopy/EUS-guided fiducial marker placement in patients with esophageal cancer: a comparative analysis of 3 types of markers. Gastrointest Endosc. 2015;82:641–649. doi: 10.1016/j.gie.2015.03.1972. [DOI] [PubMed] [Google Scholar]
- 8.Coronel E., Cazacu I.M., Sakuraba A. EUS-guided fiducial placement for GI malignancies: a systematic review and meta-analysis. Gastrointest Endosc. 2019;89:659–670.e18. doi: 10.1016/j.gie.2018.10.047. [DOI] [PubMed] [Google Scholar]
- 9.Jayachandran P., Minn A.Y., Van Dam J. Interfractional uncertainty in the treatment of pancreatic cancer with radiation. Int J Radiat Oncol Biol Phys. 2010;76:603–607. doi: 10.1016/j.ijrobp.2009.06.029. [DOI] [PubMed] [Google Scholar]
- 10.van der Horst A., Wognum S., Dávila Fajardo R. Interfractional position variation of pancreatic tumors quantified using intratumoral fiducial markers and daily cone beam computed tomography. Int J Radiat Oncol Biol Phys. 2013;87:202–208. doi: 10.1016/j.ijrobp.2013.05.001. [DOI] [PubMed] [Google Scholar]
- 11.Packard M., Gayou O., Gurram K. Use of implanted gold fiducial markers with MV-CBCT image-guided IMRT for pancreatic tumours. J Med Imaging Radiat Oncol. 2015;59:499–506. doi: 10.1111/1754-9485.12294. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
EUS-guided placement of gold fiducial markers in a pancreatic head adenocarcinoma to guide delivery of stereotactic body radiation therapy.