Abstract
Erysipelothrix rhusiopathiae is a major causative organism of swine erysipelas, but the infection has rarely occurred in humans. A soft-tissue infection with this organism is described as “erysipeloid.” Most reported cases in human are related to occupational exposure. Endocarditis is a common complication of E. rhusiopathiae bacteremia in human.
We report the case of a previously healthy 52-year-old Japanese female who presented with fever and an inflamed hand after being bitten by a stray cat. Blood culture was positive for E. rhusiopathiae, but no sign of infective endocarditis was observed. It may be prudent to consider E. rhusiopathiae infection in patients with animal bites.
Keywords: Erysipelothrix rhusiopathiae, Animal bites, Bacteremia
Introduction
Erysipelothrix rhusiopathiae is a rod-shaped, non-sporulating, aerobic or facultative aerobic, gram-positive bacillary organism. The organism has been identified as either a commensal or pathogen in a wide variety of animals, from swine and sheep to turkeys, ducks, fish, dogs, cats, and chickens. Among the animals that host it, domestic swine are considered the major reservoir. E. rhusiopathiae infection is communicable from animals to humans by direct cutaneous contact. The infection in human is generally linked to occupational exposure, generally among fishermen, fish handlers, butchers, farmers, slaughterhouse workers, veterinarians, and homemakers [1]. E. rhusiopathiae infection has also been reported in patients following marine exposure [2]. Animal bites have rarely been known to cause E. rhusiopathiae infection: two wound infections have been reported after cat bites and one case of bacteremia has been reported after a dog bite [3,4]. Three clinical varieties of E. rhusiopathiae human infection are known: a localized cutaneous form called “erysipeloid”, a generalized (diffuse) cutaneous form and bacteremia, often in association with endocarditis [1]. Although systemic infection with E. rhusiopathiae bacteremia is uncommon, a high incidence of endocarditis is reported among the patients who do develop bacteremia, and more than half of the endocarditis cases reported appeared in previously normal native valves [5]. Chronic liver disease and diabetes mellitus have been reported as important predisposing factors for E. rhusiopathiae bacteremia [6,7].
We describe a case of E. rhusiopathiae bacteremia without endocarditis in a previously healthy female who had recently been bitten by a cat.
Case report
A 52-year-old Japanese female presented to our hospital with a chief complaint of fever and swelling with tenderness in the thenar area of her right hand. She reported that three days before her visit, a stray cat had bitten her right thenar area as she was walking along a river terrace nearby her house in Wakayama City, Japan. She had no medical history and had not traveled in the last several years. She had one dog, but the dog had not bitten her in the last several months. Likewise, she had not cut any raw fish in recent memory. She began experiencing swelling and sensations of heat around the site of the bite from the day after the cat bit her.
Her triage vital signs were a blood pressure 153/77 mmHg, pulse 103 beats/min, respiratory rate 24 breath/min, SPO2 99% (room air), and body temperature 39.3 degrees C. She generally appeared unwell but was fully conscious and able to report her history. Her cardiovascular and respiratory examinations were normal. Redness and warmth were found around the bite site on the right thenar area. Neither pain nor swelling of the wrist joint was observed. Linear erythema extended from the bite site to the right forearm.
Laboratory results revealed the following: white blood cell count, 9900 /μL; platelet count, 23.1 × 104/μL; creatinine, 0.59 mg/dL; total bilirubin, 0.7 mg/dL; aspartate aminotransferase, 19 U/L; alanine aminotransferase, 19 U/L; lactate dehydrogenase, 238 U/L; CRP, 1.01 mg/dL.
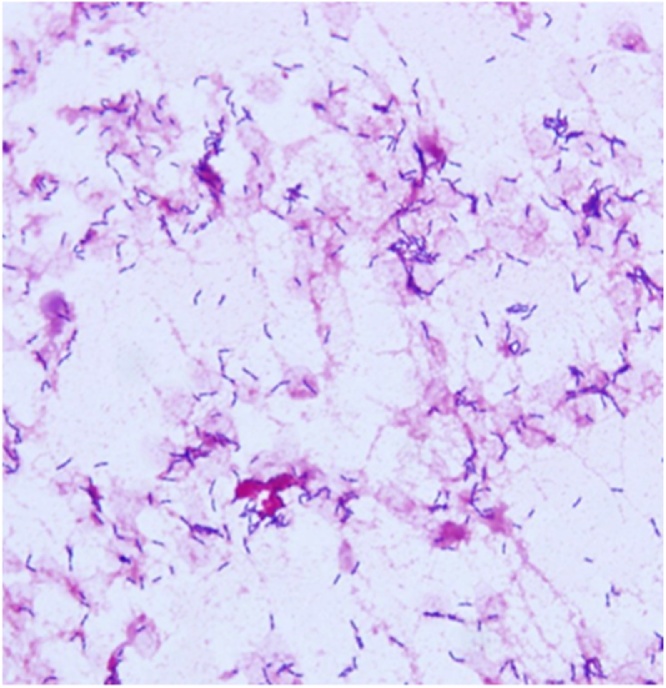
She was diagnosed with a soft tissue infection of the right hand, lymphangitis, and sepsis associated with a cat bite. Ampicillin/sulbactam was administered and amoxicillin/clavulanate was prescribed. A blood culture was positive for gram-positive rod on the day after her first hospital visit (Fig. 1). Although E. rhusiopathiae was detected by rapid bacterial identification and susceptibility testing (VITEK 2 ®, BioMérieux), further investigation was required because the cultured strain produced no hydrogen sulfate. The nucleotide sequences of the 16S rRNA genes of E. rhusiopathiae and E. tonsillarum were determined to have similarities of 99.9% and 99.7%, respectively. Tests revealed that the strain did not ferment sucrose, which enabled its identification as E. rhusiopathiae. The strain showed low minimum inhibitory concentrations (MICs) for penicillin (≦0.03) and ceftriaxone (≦0.03), and an elevated MIC for vancomycin (>4). Physical examination and echocardiography showed no signs of endocarditis. The patient’s fever abated and her other vital signs stabilized 2 days after the antibacterials were commenced. The symptom of lymphangitis in her right forearm disappeared and the swelling of her right hand improved. A follow-up blood culture after 5 days of antibacterial treatment was negative.
Fig. 1.
Gram stain of the blood culture.
The patient was treated with oral amoxicillin/clavulanate for 12 days after a single intravenous administration of ampicillin/sulbactam and recovered fully.
Discussion
We successfully treated an E. rhusiopathiae infection with bacteremia in an individual who had recently been bitten by a cat. The patient’s clinical course with antibacterial treatment was good and free of complications.
The route of infection in this case was considered the cat bite, based on the patient’s medical history. E. rhusiopathiae infections in humans usually occur as a consequence of occupational exposure. To our knowledge, this is the first known case of E. rhusiopathiae bacteremia to develop from a cat bite. While only a few cases of E. rhusiopathiae infection associated with animal bites have been reported so far, animal bites are still considered an important risk factor for the infection. First, this organism has been widely detected in animals. Second, clinicians usually forgo culture examinations for patients with mild soft tissue infections. Finally, E. rhusiopathiae is sensitive to oral antibacterials widely used for soft-tissue infections, such as amoxicillin. It seems conceivable, therefore, that many patients with E. rhusiopathiae infection have been cured without a bacteriological diagnosis.
Infective endocarditis (IE) has been reported as a common comorbidity of E. rhusiopathiae infection. While 90 percent of the reported cases of E. rhusiopathiae bacteremia resulted in endocarditis and were associated with high mortality [5], many cases of E. rhusiopathiae bacteremia without endocarditis have been reported [8,9]. The high incidence of IE among patients with E. rhusiopathiae bacteremia may be due to reporting bias, given that more severe cases are likely to be reported more often [8]. Echocardiography to identify endocarditis is crucial step to take for patients with E. rhusiopathiae bacteremia. The procedure is important even for patients with normal heart valves, given that nearly 60% of cases with endocarditis developed in previously normal heart valves [5]. Furthermore, the duration of antibacterial treatment can be shortened in patients without endocarditis: our case received antibacterial treatment for a total of 12 days, whereas the recommended duration of treatment for patients with endocarditis is as long as 4–6 weeks [1]. Clinicians should note that this organism is resistant to vancomycin, an agent often administered empirically to treat gram positive rod infections of the bloodstream. Though E. rhusiopathiae is rare as causative organism of animal bite-related infections, clinicians should consider administering penicillin to patient with bacteremia after animal bites. In conclusion, we described a case of E. rhusiopathiae infection with bacteremia in a patient who had recently been bitten by a cat. By differentiating IE, the case could be cured with a 12-day course of antibacterial treatment.
It may be necessary to differentiate E. rhusiopathiae infection in patients presenting with bacteremia after animal bites.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request
Author contribution
Ken-ichiro Kobayashi: management of the case, create the manuscript
Tomoaki Kawano: conducted the culture test, identified the causative organism
Shinsuke Mizuno, Kenji Kubo, Nobuhiro Komiya, Satoko Otsu: Supervision on the case management
Sources of funding
None.
Declaration of Competing Interest
None.
Acknowledgement
We thank to Mr. Tomokazu Kuchibiro for his cooperation with the 16S rRNA genes sequencing.
References
- 1.Reboli A.C., Farrar W. 7th ed. Churchil Livingstone; Philadelphia, PA: 2010. Erysipelothrix rhusiopathiae. Principles and practice of infectious diseases; pp. 2226–2227. [Google Scholar]
- 2.Diaz J.H. Skin and soft tissue infections following marine injuries and exposures in travelers. J Travel Med. 2014;213:207–213. doi: 10.1111/jtm.12115. [DOI] [PubMed] [Google Scholar]
- 3.Abedini S., Lester A. Erysipelothrix rhusiopathiae bacteremia after dog bite. Ugeskr Laeg. 1997;15928:4400–4401. [PubMed] [Google Scholar]
- 4.Talan D.A., Citron D.M., Abrahamian F.M., Moran G.J., Goldstein E.J. Bacteriologic analysis of infected dog and cat bites. N Engl J Med. 1999;3402:85–92. doi: 10.1056/NEJM199901143400202. [DOI] [PubMed] [Google Scholar]
- 5.Gorby G.L., Peacock J.E., Jr Erysipelothrix rhusiopathiae endocarditis: microbiologic, epidemiologic, and clinical features of an occupational disease. Clin Infect Dis. 1998;102:317–325. doi: 10.1093/clinids/10.2.317. [DOI] [PubMed] [Google Scholar]
- 6.Schuster M.G., Brennan P.J., Edelstein P. Persistent bacteremia with Erysipelothrix rhusiopathiae in a hospitalized patient. Clin Infect Dis. 1993;174:783–784. doi: 10.1093/clinids/17.4.783. [DOI] [PubMed] [Google Scholar]
- 7.Upapan P., Chayakulkeeree M. Erysipelothrix rhusiopathiae bacteremia without endocarditis associated with psoas abscess: the first case report in Thailand. J Med Assoc Thai. 2014;97(March (Suppl. 3)):S232–S236. [PubMed] [Google Scholar]
- 8.Drekonja D.M. Erysipelothrix bacteremia without endocarditis: rare event or under-reported occurrence? Diagn Microbiol Infect Dis. 2013;773:280–281. doi: 10.1016/j.diagmicrobio.2013.07.002. [DOI] [PubMed] [Google Scholar]
- 9.Restoy E.G., Espejo E., Bella F., Llebot J. Bacteremia due to Erysipelothrix rhusiopathiae in immunocompromised hosts without endocarditis. Rev Infect Dis. 1991;136:1252–1253. doi: 10.1093/clinids/13.6.1252. [DOI] [PubMed] [Google Scholar]