Abstract
Neurogenic bowel dysfunction (NBD) and gut dysbiosis frequently occur in patients with traumatic cervical spinal cord injury (TCSCI). We evaluated neurogenic bowel management and changes in the gut microbiota in patients with TCSCI as well as associations between these changes and serum biomarkers. Fresh fecal and clinical data were collected from 20 male patients with TCSCI and 23 healthy males. Microbial diversity and composition were analyzed by sequencing the V3-V4 region of the 16S rRNA gene. Moderate NBD was observed in patients with TCSCI. The diversity of the gut microbiota was lower in patients with TCSCI than in healthy adults. Furthermore, patients with TCSCI showed altered levels of serum biomarkers related to lipid metabolism, indicating unfavorable lipid profiles. Interestingly, Firmicutes had a positive effect and Verrucomicrobia had a negative effect on lipid metabolism (P < 0.05). At the genus level, Bacteroides and Blautia were significantly more abundant in patients than in healthy subjects and could be associated with lipid metabolism (P < 0.05). Faecalibacterium, Megamonas, and Prevotella, which were correlated with lipid metabolism markers, may be suitable targets for the treatment of TCSCI. Lactobacillus was positively correlated with glucose levels. The dysbiosis of several key gut bacteria was associated with serum biomarkers of lipid metabolism in patients with TCSCI. The observed interdependency of the microbiota and lipid metabolism provides a basis for understanding the mechanisms underlying lipid disorders after cervical SCI.
Keywords: Gut microbiota dysbiosis, lipid metabolism, chronic traumatic cervical SCI, neurogenic bowel dysfunction, firmicutes, serum lipid biomarkers
Introduction
Traumatic cervical spinal cord injury (TCSCI) is a life-threatening condition that not only leads to a loss of motor and sensory function but also to dysfunctions of multiple organs and pathways, including the respiratory, gastrointestinal, urinary, metabolism, and autonomic nervous system [1-3]. Despite a recent increase in survival rates, the quality of life remains poor for patients with TCSCI, as cervical injuries often result in paralysis and bowel dysfunction. Neurogenic bowel dysfunction (NBD) is a major physical and psychological problem in patients with SCI. The two main manifestations of NBD are constipation (in 40-58% of patients) and fecal incontinence (in 2-61% of patients) [3-5]. Patients with chronic cervical SCI tend to spend more time evacuating their bowels than healthy individuals. An effective bowel program should address issues of fecal incontinence, constipation, and effective evacuation. In the current study, we documented neurogenic bowel management in male patients with chronic TCSCI at our center.
The human intestinal tract is colonized by thousands of bacteria species whose number and genetic content exceed those of the host by factors of 10- and 150-fold, respectively [6]. These taxa are critical for normal digestion, nutrient absorption, metabolism, and cell function [7,8]. Common causes of gut dysbiosis include antibiotic use, prolonged stress, and gastrointestinal dysfunction [7-10]. Most patients with acute complete SCI have substantial changes in physiological processes after injury, such as the excessive growth of bacteria and the displacement of the intestinal flora, making the intestines the largest “endotoxin pool” in the human body. In addition, cervical SCI often requires antibiotic treatment due to compounding factors, such as pulmonary infection. The use of antibiotics also affects healthy intestinal micro-ecological systems [11-14]. Gut dysbiosis is highly likely in TCSCI. Few clinical studies have evaluated the intestinal microecology after cervical SCI. In a clinical study of intestinal microbes in 30 patients with SCI and 10 healthy controls using 16S rRNA technology, Gungor et al. detected significantly fewer butyrate-producing members in patients with SCI than in healthy individuals [14].
Lipoprotein metabolism is influenced by a wide range of factors, including anthropometric factors, peripheral insulin resistance, catecholamines, physical activity, performance capacity, and sex [15-18]. Patients with SCI have a high incidence of dyslipidemia and cardiovascular disease [15]. The adverse lipid profile in men with SCI compared with control subjects results from physical inactivity with low maximum oxygen uptake levels depending on the injury level [16,17]. In previous studies, differences were found between the lipoprotein profiles of men with SCI and those of male controls. Among men with SCI, tetraplegia was associated with higher levels of very low-density lipoprotein (VLDL) and triglycerides (TG) and lower levels of high-density lipoproteins (HDL). Similarly, paraplegia was associated with high total cholesterol (TCHO) and LDL [18]. In the current study, we report the lipid profiles of patients with chronic TCSCI at our center.
Therapies to improve quality of life and restore function, even partially, would have a huge impact on patients with TCSCI and their caretakers [19]. Analyses of the gut microbiota in patients with TCSCI might provide insight into the interactions between gut microbes and lipid metabolism and provide a basis for diagnosis and therapy. The aim of this study was to investigate the association between the intestinal microbiota and serum biomarkers by a comparative analysis of male patients with chronic TCSCI and healthy subjects.
Materials and methods
Ethics statement
Approval from the hospital ethics committee was obtained before commencing the study (No. CRRC-IEC-RP-SQ-006-01).
Patients and controls
A total of 20 male patients with cervical chronic TCSCI were enrolled at our center between June 2017 and November 2017. We carried out a face-to-face clinical questionnaire survey and obtained signed informed consent before assessment. In addition, we used the “International Spinal Cord Injury Core Data Set”, “International bowel function basic spinal cord injury data set”, and “International bowel function extended spinal cord injury data set” to obtain the neurogenic bowel dysfunction (NBD) symptoms data [20,21]. Patients were included if they met the following criteria: 1) neurologically complete SCI (ASIA grade A) occurring 6 or more months prior to the study, 2) 18-60 years of age, 3) traumatic cervical SCI, and 4) male. The diagnostic criteria for patients with chronic traumatic complete SCI included 1 and 3 of the above criteria. The exclusion criteria were as follows: 1) inability to complete a questionnaire survey; 2) a history of antibiotic or probiotic use in the first month before enrolment; and 3) diabetes, gastrointestinal system diseases, multiple sclerosis, and immune metabolic diseases.
The clinical dates and fresh stool specimens of the subjects were collected. After extracting fecal genomic DNA, the V3-V4 region of 16S rDNA was amplified, and an Illumina MiSeq platform was used to analyze and compare the gut microbiota of healthy males with that of male patients with SCI.
The criteria for the healthy control group were as follows: 1) 18-60 years of age; 2) no history of antibiotics or probiotics use 1 month prior to study; and 3) no history of diabetes, gastrointestinal system diseases, multiple sclerosis, and immune metabolic diseases. All subjects were selected before sampling and signed informed consent with a full understanding of the sampling process and research options. All patients and healthy subjects were fed standard hospital food 2 weeks before stool collection to exclude the potential effects of diet on the gut microbiota.
Microbial diversity analysis
Stool sampling
A total of 43 fresh specimens were collected, including 23 healthy males and 20 patients with cervical SCI. Fresh fecal samples were collected and transferred to the laboratory. Samples were placed in a new 2-mL sterile centrifuge tube, quickly placed on ice, and transferred to a freezer maintained at -80°C for cryopreservation. The entire sampling process was completed in 30 minutes.
DNA extraction and PCR amplification
Microbial DNA was extracted from stool samples using an E.Z.N.A.® Stool DNA Kit (Omega Bio-tek, Norcross, GA, U.S.) according to the manufacturer’s protocols. The V3-V4 region of the bacterial 16S rRNA gene was amplified by PCR (95°C for 2 minutes, followed by 25 cycles at 95°C for 30 s, 55°C for 30 s, and 72°C for 30 s and a final extension at 72°C for 5 minutes) using primers 338F 5’-ACTCCTACGGGAGGCAGCA-3’ and 806R 5’-GGACTACHVGGGTWTCTAAT-3’. PCRs were performed in triplicate in a 20 μL mixture containing 4 μL 5 × FastPfu Buffer, 2 μL 2.5 mM dNTPs, 0.8 μL of each primer (5 μM), 0.4 μL FastPfu Polymerase, and 10 ng template DNA.
Illumina MiSeq sequencing
Amplicons were extracted from 2% agarose gels, purified by using an AxyPrep DNA Gel Extraction Kit (Axygen Biosciences, Union City, CA, U.S.) and quantified by using QuantiFluor™-ST (Promega, U.S.). Purified amplicons were pooled in equimolar concentrations and paired-end sequenced (2 × 300 bp) on an Illumina MiSeq platform according to the standard protocols. The raw reads were deposited into the NCBI Sequence Read Archive database (Accession Number: SRP158549).
Processing of sequencing data
Raw fastq files were quality-filtered by Trimmomatic and merged by FLASH with the following criteria: (i) the reads were truncated at any site receiving an average quality score < 20 over a 50 bp sliding window. (ii) Sequences whose overlap was longer than 10 bp were merged according to their overlap with no more than 2 mismatched bp. (iii) The sequences of each sample were separated according to barcodes (exactly matching) and primers (allowing 2 mismatching nucleotides), and reads containing ambiguous bases were removed.
Operational taxonomic units (OTUs) were clustered with 97% similarity cutoff using UPARSE (version 7.1), and chimeric sequences were identified and removed using UCHIME. The taxonomy of each 16S rRNA gene sequence was analyzed by the RDP Classifier algorithm against the Silva (SSU123) 16S rRNA database using a confidence threshold of 70% Roche 454 (Roche, Switzerland). High-throughput sequencing of the PCR products was performed by Shanghai Majorbio Biological Technology Co. Ltd., Shanghai, China.
Bioinformatics and statistical analysis
Sequencing reads were processed using QIIME (version 1.9.0), with additional quality trimming, demultiplexing, and taxonomic assignments. Profiling of the predictive urine microbiota was performed using PiCRUSt based on the Greengenes database, accessed August 13, 2013 [22]. The KW rank sum test and pairwise Wilcoxon test were used for the identification of the different markers, and LDA was used to score each feature in LEfSe analysis. The index of alpha diversity was calculated with QIIME based on sequence similarity of 97%. Beta diversity was measured by unweighted UniFrac distance, which was also calculated by QIIME. Hierarchical clustering was performed, and a heatmap was generated using Spearman’s rank correlation coefficient as a distance measure and a customized script developed in the R statistical package. The output file was further analyzed using the Statistical Analysis of Metagenomic Profiles software package (version 2.1.3) [23].
Statistical analysis was performed using the SPSS data analysis program (version 21.0) and Statistical Analysis of Metagenomic Profiles software. For continuous variables, independent t-tests, Welch’s t-tests, White’s nonparametric t-tests, and Mann-Whitney U-tests were applied. For categorical variables between groups, we used either the Pearson chi-square or Fisher’s exact test, depending on validity of assumption. For taxa among subgroups, ANOVA was applied (Tukey-Kramer post hoc test was used, and the effect size was Eta-squared) with Benjamini-Hochberg FDP false discovery rate correction [23,24]. All tests of significance were two-sided and P < 0.05.
Results
Characteristics and neurogenic bowel management of male patients with chronic TCSCI
In total, 20 patients with chronic cervical SCI fulfilling the enrolment criteria were interviewed and asked to complete a survey (Tables 1, 2). The causes of injury in descending order of frequency were traffic accidents (50%), bruised by heavy object (20%), and falls from heights (15%). The mean NBD score was 11.17 ± 5.16. The mean defecation time was 41.789 ± 19.29 min. Most patients (75%) engaged in bowel care more than twice every week, and the remaining patients (25%) engaged in bowel care once daily. The main techniques used for fecal evacuation in descending order of frequency were suppository (100%), digital stimulation (40%), and manual evacuation (30%). Supplementary interventions for fecal evacuation included abdominal massage (50%), digital anus-rectal stimulation (35%), digital evacuation (10%), and cathartic drug use (5%).
Table 1.
Descriptive data of the NBD management in chronic cervical traumatic complete SCI participants
| TCSCI n (%) | |
|---|---|
| Course | 69.4 ± 52.72 (months) |
| Segment | C3-C4 12 (60%) |
| C5-C8 8 (40%) | |
| NBD Scores | 11.17 ± 5.16 |
| Defecation time | 41.789 ± 19.29 (minutes) |
| Pathogenesis | Traffic accident 10 (50%) |
| Bruised by heavy object 4 (20%) | |
| Falling down 3 (15%) | |
| Other causes 3 (15%) | |
| Frequency of bowel care | Once daily: 5 (25%) |
| Not daily but more than twice every week 15 (75%) | |
| Main techniques for fecal evacuation | Suppository 20 (100%) |
| Manual evacuation 8 (40%) | |
| Digital stimulation 6 (30%) | |
| Supplementary interventions | Abdominal massage 10 (50%) |
| Digital anus-rectal stimulation 7 (35%) | |
| Digital evacuation 2 (10%) | |
| Taking cathartic drug 1 (5%) | |
| Timing of bowel care | Morning 1 (5%) |
| Afternoon 14 (70%) | |
| Evening 5 (25%) | |
| Location during evacuation | Bed 12 (60%) |
| Potty chair 6 (30%) | |
| Toilet seat 2 (10%) | |
| Degree of assistance needed | Need all help 19 (95%) |
| Need special help 1 (5%) | |
| Abdominal symptoms | Abdominal discomfort 12 (60%) |
| Constipation 14 (70%) | |
| Bloating symptom 16 (80%)Flatus incontinence 18 (90%) |
Table 2.
Demographics and serum biomarkers between male healthy and patients with chronic cervical traumatic complete SCI
| Health Male | TCSCI-Male | P | |
|---|---|---|---|
| N | 23 | 20 | |
| AGE | 40 ± 9.03 | 39.9 ± 10.57 | 0.998 |
| BMI | 24.8 ± 2.677 | 23.11 ± 2.876 | 0.022 |
| ALT | 26.791 ± 16.367 | 26.2 ± 19.303 | 0.903 |
| AST | 23.848 ± 17.097 | 21 ± 9.8 | 0.429 |
| UREA | 4.416 ± 1.224 | 4.403 ± 1.14 | 0.966 |
| CR | 64.3 ± 12.701 | 60.7 ± 11.8 | 0.265 |
| UA | 309 ± 69.81 | 378.1 ± 64.93 | 0.001 |
| GLU | 4.343 ± 0.528 | 5.266 ± 1.964 | 0.033 |
| TG | 1.436 ± 1.319 | 1.928 ± 1.207 | 0.137 |
| TCHO | 3.695 ± 0.794 | 4.217 ± 1.005 | 0.038 |
| HDL | 0.9152 ± 0.2091 | 0.917 ± 0.163 | 0.974 |
| LDL | 2.177 ± 0.596 | 2.617 ± 0.701 | 0.005 |
| APOA1 | 1.417 ± 0.11 | 1.03 ± 0.129 | 0.001 |
| APOB | 0.833 ± 0.11 | 0.927 ± 0.183 | 0.045 |
| LP-A | 40.465 ± 25.32 | 94.16 ± 72.16 | 0.002 |
| NEFA | 0.251 ± 0.09 | 0.353 ± 0.207 | 0.038 |
More than half of the bowel care time occurred in the afternoon (70%), and the remaining bowel care time occurred in the evening (25%) and morning (5%). The location of bowel care was a bed (60%), a potty chair (30%) or a toilet seat (10%). Of the patients, 95% needed full assistance during defecation time, while the remaining 5% needed partial help. Further, 60% had abdominal discomfort, 70% had constipation, 80% had bloating, and 90% had flatus incontinence.
There was no significant difference (independent t-test, P = 0.998) between the mean age of healthy adult males (40 ± 9.03 years) and patients with cervical SCI (39.9 ± 10.57 years). The body mass index (BMI) of healthy males was significantly higher (24.8 ± 2.677 kg/m2) than that of SCI patients (23.11 ± 2.876 kg/m2) (independent t-test, P = 0.022). The serum levels of TG, TC, LDL, apolipoprotein B (APOB), lipoprotein A (LPA), and non-esterified fatty acids (NEFA) in the SCI group were higher than those in the healthy group, while levels of HDL and apolipoprotein A1 (APOA1) were lower than those in the healthy group. The serum biomarkers uric acid (UA), TCHO, LDL, APOA1, APOB, LPA, and NEFA showed a significant difference between the two groups (independent t-tests, P < 0.05; Table 2).
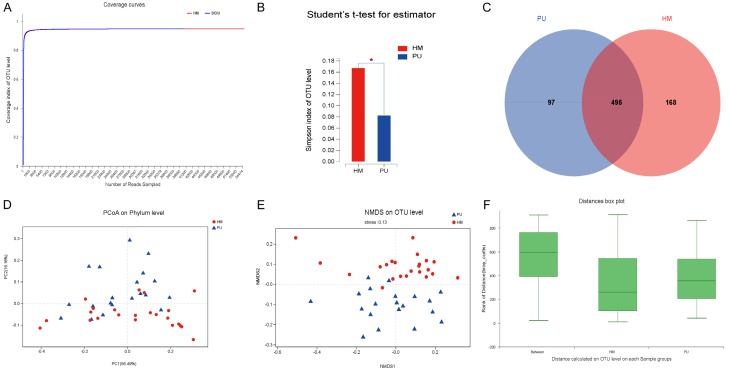
Sequencing data
16S rRNA gene sequences were generated using the Illumina MiSeq platform. Reads were clustered into OTUs at an identity threshold of 97%. Rarefaction curves showed clear asymptotes, and the Good’s coverage for the observed OTUs was 99.8% (Figure 1A). These findings indicated a near-complete sampling of the community. A total of 746 OTUs were recognized. No significant differences in OTU abundance (ACE or Chao1 index; Student’s t-test, P = 0.78 and 0.76, respectively) were observed between healthy males and patients with cervical SCI. At the genus level, the Simpson alpha-diversity index indicated lower diversity in patients with cervical SCI than in healthy subjects (Student’s t-test, P = 0.017; Figure 1B). In total, 495 of the 760 OTUs were shared between the two cohorts (Figure 1C). A principle coordinates analysis (PCoA) of phyla and a non-metric multidimensional scaling analysis (NIMDS) of OTUs revealed significant differences in bacterial community composition between the two groups (Figure 1D, 1E). ANOSIM/Adonis revealed significant differences in the structure of the gut microbiota between the two groups (ANOSIM, r 2 = 0.4532, P = 0.001; Figure 1F). Based on the dispersion of the sample point distribution in a partial least square-discriminant analysis (PLS-DA) at the OTU, phylum, and genus levels, we found differences in the bacterial community composition between the two groups (Supplementary File 1A-C).
Figure 1.
Diversity and taxonomic analysis in the health male and cervical SCI groups. A. The rarefaction curves showed clear asymptotes and the Good’s coverage for the observed OTUs was 99.8% in the health male and cervical SCI groups. B. OTU diversity index Simpson showed a significant difference between the health male and cervical SCI groups (Student’s t test, P = 0.017). C. A Venn diagram demonstrated 495 of the total 760 OTUs were shared between the health male and cervical SCI groups. D. The PCoA on phylum level of beta-diversity analysis showed there was significant difference in bacterial community composition between two groups (PCoA, PC1 = 56.49%; PC2 = 16.16%). E. The NIMDS on OTU level of beta-diversity analysis showed there was significant difference in bacterial community composition between two groups (NIMDS, stress = 0.13). F. ANOSIM/Adonis revealed significant differences in the structure of gut microbiota among the two groups (ANOSIM, r2 = 0.4532, P = 0.001).
Associations of the gut microbiota and cervical SCI
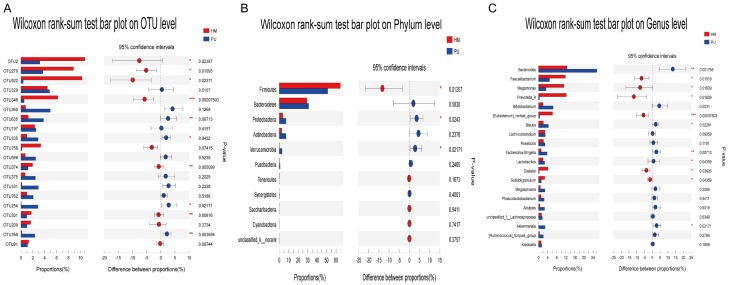
A STAMP analysis indicated that 10 of the top 20 OTUs showed a significant difference between the two groups (Wilcoxon rank-sum test, P < 0.05; Figure 2A). Additionally, 3 phyla and 11 of the top 20 genera showed a significant difference between the two groups (Wilcoxon rank-sum test, P < 0.05; Figure 2B, 2C). Firmicutes, Faecalibacterium, Megamonas, Prevotella_9, [Eubacterium]_rectale_group, Dialister, and Subdoligranulum were significantly more abundant in the healthy male group than in the cervical SCI group (Wilcoxon rank-sum test, P < 0.05); Proteobacteria, Verrucomicrobia, Bacteroides, Blautia, Escherichia-Shigella, Lactobacillus, and Akkermansia were significantly more abundant in the cervical SCI group than in the healthy male group (Wilcoxon rank-sum test, P < 0.05) (Figure 2B, 2C).
Figure 2.
STAMP analysis on significant difference test between health male and cervical SCI groups. A. STAMP analysis indicates there were 10 OTUs showed a significant difference (Wilcoxon rank-sum test, P < 0.05) among two groups in top 20 OTUs. B. There were 3 Phylum showed a significant difference (Wilcoxon rank-sum test, P < 0.05) among two groups. C. There were 11 of top 20 Genus showed a significant difference (Wilcoxon rank-sum test, P < 0.05) among two groups.
Cervical SCI associated biomarkers
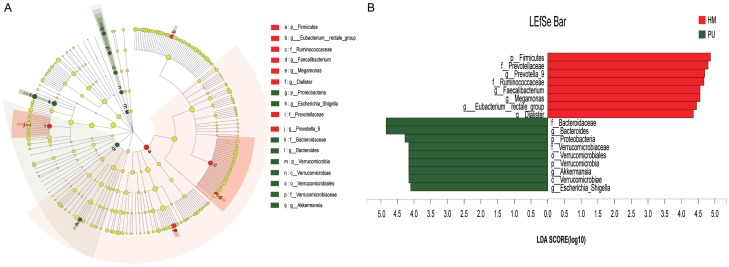
An LEfSe analysis (LDA threshold of 4) indicated that Bacteroidaceae and Bacteroides were significantly enriched in the SCI group compared with the healthy group, which was enriched for Firmicutes and Prevotellaceae. A cladogram representative of the structure of the gut microbiota, predominant bacteria, and the greatest taxonomic differences between the two cohorts are displayed in Figure 3A and 3B. These data suggested that dysbiosis was extensive in patients with cervical SCI. Further, Bacteroidaceae, Bacteroides, and Proteobacteria could be used as potential distinguishing biomarkers.
Figure 3.
Cladogram showing differentially abundant taxa of microbiota between health male and cervical SCI groups. A. LEfSe cladogram showed the most differentially abundant taxa of 16S sequences between the two groups. B. LEfSe analysis (LDA threshold of 4) indicated that Bacteroidaceae and Bacteroides were significantly enriched in the SCI group compared with the healthy group, which showed enrichment of Firmicutes and Prevotellaceae (Kruskal-Wallis (KW) sum-rank test).
Gut microbiota affected by participants’ conditions
We selected the following factors for redundancy analysis (RDA)/correspondence analysis (CCA): age, BMI, alanine aminotransferase (ALT), aspartate aminotransferase (AST), urea, UA, creatinine (CR), glucose (GLU), TG, TCHO, HDL, LDL, APOA1, APOB, LPA, and NEFA (Supplementary File 2). RDA/CCA showed that GLU (P = 0.047, r2 = 0.1475), HDL (P = 0.032, r2 = 0.1547), APOA1 (P = 0.001, r2 = 0.5067), and LPA (P = 0.001, r2 = 0.2143) significantly affected bacterial composition at the phylum level. In the top 20 genera, HDL (P = 0.035, r2 = 0.1508) and APOA1 (P = 0.002, r2 = 0.2785) significantly affected bacterial composition. Linear regression of the factors showed association between the serum levels of GLU, LPA on phylum level and HDL, APOA1 on genus level according to PCoA (Figure 4A-D). We found that serum biomarkers GLU, HDL, APOA1, and LPA had significant correlations with the microbial community structure (P < 0.05).
Figure 4.
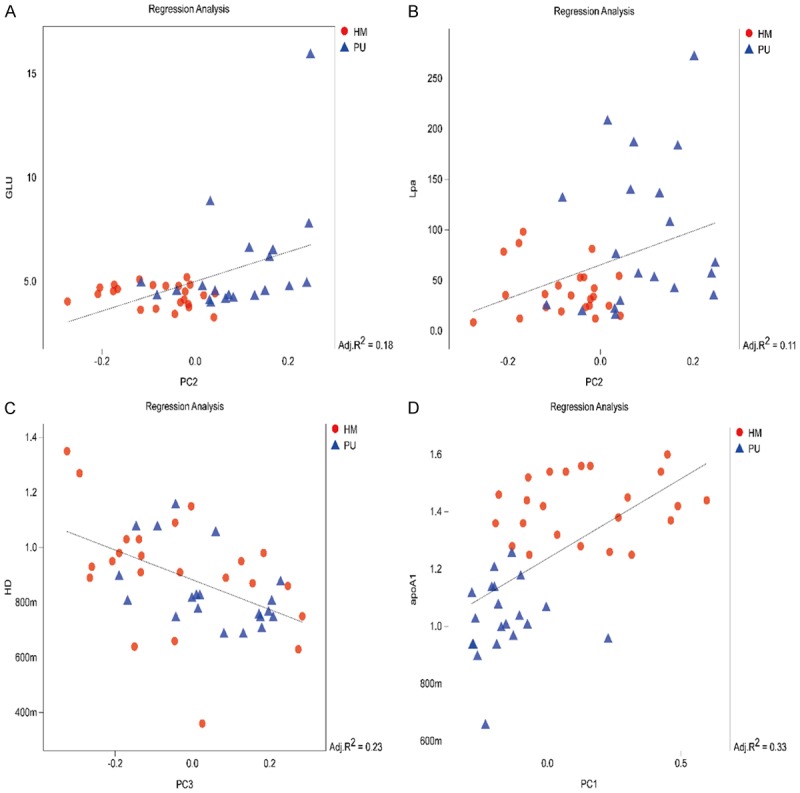
Linear regression of environmental factors between the serum lipid profiles and principal co-ordinates analysis in health male and cervical SCI groups. Linear Regression of the serum level of GLU on phylum (A), LPA on phylum (B), HDL on genus level (C), APOA1 on genus level (D) and principal co-ordinates analysis in health male and cervical SCI groups showed significant correlation with microbial community structure (A, R2 = 0.18, P < 0.05; B, R2 = 0.11, P < 0.05; C, R2 = 0.23, P < 0.05; D, R2 = 0.33, P < 0.05).
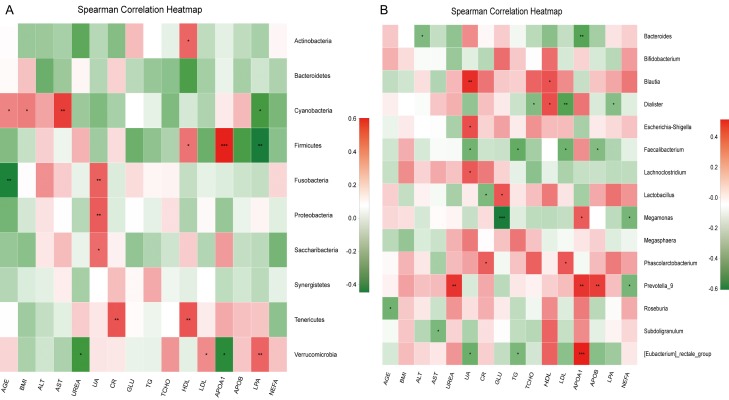
Correlation heatmap analysis of the relationship between different factors and the community composition of the two groups showed that Firmicutes was positively correlated with APOA1 (Pearson r = 0.604, P = 0.0001) and HDL (Pearson r = 0.358, P = 0.018), while it was negatively correlated with LPA (Pearson r = -0.447, P = 0.003). Proteobacteria was positively correlated with UA (Pearson r = 0.415, P = 0.006). Verrucomicrobia was positively correlated with LPA (Pearson r = 0.009, P = 0.003) and LDL (Pearson r = 0.31, P = 0.043), negatively correlated with APOA1 (Pearson r = -0.378, P = 0.012) and UREA (Pearson r = -0.322, P = 0.035) in phylum level ,other correlation analysis were showed in Figure 5A. In the top 15 genera, as significant difference genera between healthy and SCI groups, the Bacteroides was negative correlated with APOA1 (Pearson r = -0.414, P = 0.006) and ALT (Pearson r = -0.318, P = 0.038); Faecalibacterium was negative correlated with UA (Pearson r = -0.351, P = 0.021), TG (Pearson r = -0.381, P = 0.012), LDL (Pearson r = -0.357, P = 0.019) and APOB (Pearson r = -0.314, P = 0.04). Prevotella_9 was negatively correlated with NEFA (Pearson r = -0.336, P = 0.028) and positively correlated with APOA1 (Pearson r = 0.425, P = 0.005), APOB (Pearson r = 0.009, P = 0.045) and UREA (Pearson r = 0.426, P = 0.004); Dialister was negatively correlated with LDL (Pearson r = -0.422, P = 0.005), TCHO (Pearson r = -0.314, P = 0.04) and LPA (Pearson r = -0.303, P = 0.048), positively correlated with HDL (Pearson r = 0.349, P = 0.022). [Eubacterium]_rectale group was positively correlated with APOA1 (Pearson r = 0.515, P = 0.0001), negatively correlated with UA (Pearson r = -0.366, P = 0.016) and TG (Pearson r = -0.333, P = 0.029). Lactobacillus was positively correlated with GLU (Pearson r = 0.33, P = 0.031) and negatively correlated with CR (Pearson r = -0.322, P = 0.035). Escherichia-Shigella was positively correlated with UA (Pearson r = 0.35, P = 0.022). Lachnoclostridium was positively correlated with UA (Pearson r = 0.322, P = 0.036). Megamonas was negatively correlated with GLU (Pearson r = -0.605, P < 0.001), NEFA (Pearson r = -0.336, P = 0.028), and positively correlated with APOA1 (Pearson r = 0.314, P = 0.041) (Figure 5B and Supplementary Files 3, 4).
Figure 5.
Correlation heatmap analysis of different environmental factors on the community composition of the healthy male and cervical SCI groups in phylum level (A) and genus level (B).
Relationship between the gut microbiota and the condition of participants association between the gut microbiota and metabolism
According to a 16S rRNA functional predictive analysis, the abundances of taxa related to carbohydrate, amino acid, nucleotide, and lipid metabolism, transcription, and translation were decreased in patients with cervical SCI (Figure 6A). Of these, nucleotide (Wilcoxon rank-sum test, P = 0.027), lipid metabolism (Wilcoxon rank-sum test, P = 0.027), and translation (Wilcoxon rank-sum test, P = 0.019) were significantly decreased in the cervical SCI group. Lipid metabolism in level 2 of the of KEGG metabolic pathway hierarchy (Wilcoxon rank-sum test, P = 0.025) and fatty acid metabolism in level 3 (Wilcoxon rank-sum test, P = 0.014) were significantly decreased in the cervical SCI group (Figure 6B).
Figure 6.
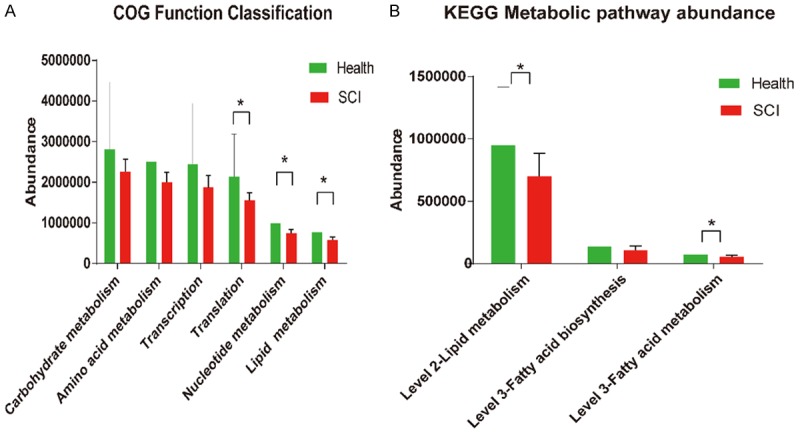
16S functional prediction of gut microbiota in healthy male and cervical SCI groups. A. The abundance of nucleotide (Wilcoxon rank-sum test, P = 0.027), lipid metabolism (Wilcoxon rank-sum test, P = 0.027) and translation (Wilcoxon rank-sum test, P = 0.019) had significant decreased in SCI group. B. The lipid metabolism in level 2 (Wilcoxon rank-sum test, P = 0.025) and fat acid metabolism in level 3 (Wilcoxon rank-sum test, P = 0.014) of KEGG metabolic pathway abundance had significant decreased in SCI group.
Discussion
In this study, we evaluated the bowel management of NBD in male patients with chronic TCSCI at our center. In a comparison of the gut microbiomes of healthy adult males and male patients with chronic TCSCI, the diversity of gut microbiota was lower in the TCSCI group than in healthy adult males and the structural composition was different. The dysbiosis of the gut microbiota involving several key bacteria was associated with serum biomarkers of lipid metabolism in participants with SCI. The lipid metabolism in the COG functional database and lipid metabolism (level 2) and fatty acid metabolism (level 3) in the KEGG metabolic pathways were significantly decreased in the cervical SCI group when compared with healthy males. To our knowledge, microbiome studies targeting lipid profiles in patients with cervical SCI are non-existent and the results of this study suggest that gut microbiome dysbiosis ha implications in cervical SCI.
TCSCI is most prevalent in adults and is often caused by falls from heights (49.7%) and traffic accidents (36.4%) [25]. In the current study, traffic accidents (50%), bruises by heavy objects (20%), and falls from heights (15%) were the main causes of injury. The average age of patients with cervical SCI in this study was 39.9 years old, which is considered the prime of life and the period when individuals also particularly susceptible to accidental injuries. Wu et al. reported that the male/female ratio for TCSCI is 5/1 [25]. Consistent with this, most of the patients with chronic traumatic complete cervical SCI admitted to our center were male; thus, we chose male patients as our research subjects.
The prevalence of NBD in patients with SCI is approximately 80-97.3% according to previous studies [3,26,27]; similarly, in our study, all patients with cervical SCI (100%) had at least one gastrointestinal problem. In previous studies, no significant correlation was detected between the prevalence of gastro-intestinal symptoms and injury level in SCI [28-30]. However, our study included only hospitalized patients with complete cervical SCI, and the prevalence of NBD was therefore higher owing to the limited physical activity. The average NBD score was 11.17, which is considered moderate [31]; the average defecation time was 41 min, which was similar to the 31-45 min reported in 72-80% patients in a previous study [26,27]. The main technique for fecal evacuation was suppository and supplementary interventions were abdominal massage and digital anus-rectal stimulation; 60% of patients were in bed during evacuation and 95% patients needed help to complete evacuation; constipation and bloating were common symptoms in those patients. Due to the absence of nervous control in patients with cervical SCI, NBD results in constipation, incontinence, and discoordination of defecation [3]. Patients with cervical SCI who participated in this study had serious symptoms of NBD, severely affecting the quality of life. Despite bowel management measures, but gastrointestinal problems were not completely addressed. The gut microbiota provides a potential target to address this problem.
Cardiovascular disease is among the leading causes of death among patients with SCI. The risk factors for cardiovascular disease include unfavorable lipid profiles, such as high concentrations of TC, LDL, and TG and low concentrations of HDL in individuals with tetraplegic SCI [18,32-36]. We found that differences in lipid profiles between groups; the serum biomarkers TG, TCHO, LDL, APOB, LPA, and NEFA were higher while HDL and APOA1 were lower in the SCI group than in healthy males. The serum biomarkers TCHO, LDL, APOA1, APOB, LPA, and NEFA showed a significant difference between SCI and healthy male groups, indicating that the patients with SCI in our study exhibited dyslipidemia. This may be explained by inactivity and dysfunction of the autonomic nervous system of patients with cervical SCI. Inactivity is associated with higher insulin resistance, increased occurrence of glucose intolerance and diabetes mellitus, and reduced activity of the lipoprotein lipase. This could be related to decreased body fat, increased cardiovascular fitness, and associated metabolic changes [37,38]. Different serum catecholamine levels resulting from the impairment of the sympathetic nervous system have been observed in patients with SCI. Schmid et al. found that the lower the noradrenaline values, the lower the HDL [18]. LDL is also correlated with levels of catecholamines and particularly with levels of adrenaline [18]. After SCI, sympathetic tone diminishes, reducing the resting metabolic rate, which could decrease lipid metabolism [39].
We found lower intestinal microbial diversity in patients with cervical SCI than in healthy males and differences in the bacterial community composition. Multiple linear regression and PCoA showed associations between the serum levels of GLU and LPA and taxa at the level of phyla and between HDL and APOA1 and taxa at the genus level. Additionally, the serum biomarkers GLU, HDL, APOA1, and LPA were significantly correlated with the microbial community structure. In the SCI group, the phylum Firmicutes decreased significantly, consistent with the results of Gungor et al. [14], who showed that butyrate-producing taxa are specifically reduced in patients with SCI when compared with healthy subjects. Short-chain fatty acids, particularly butyrate, have potent anti-inflammatory effects on macrophages [40], which contributes to secondary tissue damage and axonal retraction following SCI [41,42]. In our study, the abundance of fatty acid metabolism in level 3 of the KEGG metabolic pathway hierarchy in the 16S rRNA functional prediction was significantly decreased in the SCI group, suggesting that reduced levels of butyrate may contribute to macrophage-mediated neurotoxicity in these patients. The low butyrate levels may have an impact on long-term recovery after cervical SCI. Moreover, we found that the prevalence of [Eubacterium]_rectale, a butyrate-producing bacterial genus [43], in the SCI group was positively correlated with APOA1 and negatively correlated with TG. The decreased APOA1 and increased TG indicate that [Eubacterium]_rectale may affect lipid metabolism via these factors.
When the cervical spinal cord is injured, most or all brainstem circuitry that provides tonic executive control over sympathetic preganglionic neurons (SPNs) is lost. Injury to these pre-sympathetic axons unplugs SPNs from the brain and brainstem, eliminating the feedback regulation of autonomic reflexes that are initiated below the level of injury by, for example, visceral or somatic sensory nerves that relay information to the spinal cord from the bowel. After SCI, the loss of descending control over SPNs causes autonomic reflex circuitry to become dysfunctional, leading to dysfunctions, such as autonomic dysreflexia and SCI-immune depression syndrome.
SCI also causes an autonomic imbalance in the gastrointestinal tract, which leads to deficits in colonic motility, mucosal secretions, and vascular tone [44,45]. The autonomic nervous system and gastrointestinal dysfunction may be causes of gut microbiota dysbiosis in patients with cervical SCI at our center.
The changes in bacterial taxa were associated with changes in the lipid profiles of participants. At the phylum level, the decreased Firmicutes was positively correlated with APOA1 and HDL, and negatively correlated with LPA. The phyla Proteobacteria and Verrucomicrobia were significantly increased in the cervical SCI group, and the increase in Verrucomicrobia was positively correlated with LPA and LDL and negatively correlated with APOA1. Verrucomicrobia is increased in rats with non-alcoholic fatty liver disease [46]. Dramatic colonization of the human gut microbiota by Verrucomicrobia following a broad-spectrum antibiotic regimen occurred without significant gastrointestinal manifestations [47], suggesting that the phylum negatively regulates lipid metabolism.
ApoA1, a major structural protein among HDLs, is mainly synthesized in the liver [48]. There is a very close correlation between ApoA1 and HDL cholesterol (HDLC), and ApoA1 is a protective factor for atherosclerosis [49]. ApoA1 activates key enzymes in cholesterol metabolism. Thus, the reduced serum levels of APOA1 and HDL might lead to a blood lipid metabolism disorder and have a negative effect on SCI recovery.
At the genus level, Bacteroides and Blautia were significantly more abundant, while Faecalibacterium, Megamonas, Prevotella_9, Lactobacillus, and Dialister were significantly less abundant in the cervical SCI group than in healthy males. These key bacteria were associated with serum biomarkers of lipid metabolism. Bacteroides is a gram-negative bacterium, accounting for more than 1/4 of the adult intestinal flora with important roles in the health of hosts. When immunity is low, bacterial proliferation and translocation can cause endogenous infections [50,51]. In our study, Bacteroides was negatively correlated with APOA1, indicating that increased Bacteroides may have adverse effects in immune-compromised patients with cervical SCI. Blautia produces short-chain fatty acids [50]. Blautia was positively correlated with UA and HDL, suggesting that increased Blautia in the SCI group may improve lipid metabolism in these patients.
The genus Faecalibacterium is an important component of a healthy human gut microbiome. Species in the genus can utilize acetate CoA-transferase to affect butyrate synthesis [52]. Butyrate has histone deacetylase activity and signals via GRP43 and GRP109a, thereby influencing brain function or structure [53]. In this study, Faecalibacterium was negatively correlated with UA, TG, LDL, and APOB. The protein APOB is synthesized in the liver and accounts for 97% of the total protein content of LDL. APOB can directly reflect the level of LDL [35]. Decreased Faecalibacterium was correlated with increased levels of TG, LDL, and APOB, which is harmful for lipid metabolism, suggesting that this genus is beneficial for lipid metabolism.
Liao et al. reported a positive association between bean consumption and the genus Megamonas, suggesting that Megamonas is a beneficial microbe [54]. The abundance of Megamonas was decreased in the cervical SCI group and was negatively correlated with GLU and positively correlated with APOA1, suggesting that the genus has a positive effect in terms of carbohydrate and lipid metabolism. This may be due to the fact that some carbohydrates in food cannot be digested and absorbed by intestinal digestive enzymes, but they can be metabolized by Megamonas.
Although Prevotella is considered a beneficial microbe, it is also linked to chronic inflammatory conditions [55,56]. In this study, decreased Prevotella in the cervical SCI group was negatively correlated with NEFA and positively correlated with APOA1, APOB, and UREA. This suggests that Prevotella has a positive effect on the body by regulating lipid metabolism.
Lactobacillus is a genus of probiotic bacteria capable of producing organic acids and hydrogen peroxide, creating an inhospitable environment for pathogenic bacteria. In addition, an increase in the proportion of Lactobacillus can increase insulin secretion [57]. Therefore, the increased Lactobacillus may have a protective effect in patients with cervical SCI by the regulation of carbohydrate and lipid metabolism. Vogt et al. reported that a high abundance of Dialister is associated with less Alzheimer’s disease (AD) pathology, suggesting that these bacterial taxa have protective effects against the development or progression of AD [58]. In the current study, Dialister was negatively correlated with LDL, TCHO, and LPA and positively correlated with HDL. Elevations of these serum markers indicate high blood lipids, which are harmful to health. Together, our observations revealed that carbohydrate, lipid, and fatty acid metabolism were damaged in patients with cervical SCI. This suggests that improvements in carbohydrate and lipid metabolism in patients can correspond with an improvement in the composition of the gut microbiota. Moreover, therapies targeting the gut microbiota can be used to evaluate and modulate patient metabolism.
To exclude the confounding effects of gender and thoracic splanchnic nerves on gut functions, we only included male patients with complete SCI in this study. However, individual differences in diet-associated flora could not be determined; this remains a major weakness of our study. We found that gut microbiota dysbiosis is associated with serum lipid profiles in male patients with cervical complete SCI and used 16S rRNA sequencing to predict the dysfunctional components of lipid metabolism in these patients. This is the first comprehensive investigation of the correlations between gut dysbiosis and serum biomarkers in patients with TCSCI. This study could contribute to the development of novel strategies for improving conditions of patients with TCSCI. However, further genomic and metagenomic analyses are required to determine the precise functional changes caused by the SCI-mediated dysbiosis of the gut microbiota and the effects of those changes on serum lipid profiles. Further work, including animal experiments and longitudinal human studies, are needed to determine the causal relationship between the gut microbiota and cervical SCI. Determining the role of the gut microbiota in the progression or maintenance of SCI may lead to novel interventional approaches that can alter or restore a healthy gut bacterial composition or to the identification of microbial metabolites that are protective against cervical SCI.
Overall, we demonstrated that microbiota dysbiosis might be related to cervical SCI. The relative abundances of some key bacteria in patients with cervical SCI were different compared with those in healthy males. Moreover, these relative abundances were correlated with serum lipid profiles. Further, there was an interdependency between the gut microbiota and carbohydrate and lipid metabolism. Our study provides a basis for future investigations of the dysbiosis of the gut microbiota and the functional implications of these changes.
Acknowledgements
This work was supported by the Beijing Municipal Science and Technology Commission (No. Z171100001017076); the Special Fund for Basic Scientific Research of Central Public Research Institutes (grant number: 2016CZ-1; 2018CZ-1; 2018CZ-8); the National Natural Science Foundation of China (No. 81870979); the Beijing Science and Technology Major Project (No. D161100002816004) and the Capital Health Research and Development of Special (No. 2018-1-6011). The National Key Research and Development Program of China (No. 2018YFF0301104).
Disclosure of conflict of interest
None.
Abbreviations
- SCI
spinal cord injury
- TCSCI
traumatic cervical spinal cord injury
- NBD
neurogenic bowel dysfunction
- GLU
glucose
- VLDL
very low density lipoprotein
- HDL
high density lipoprotein
- LDL
low density lipoprotein
- UA
uric acid
- CR
creatinine
- CPR
C-reactive protein
- OTUs
operational taxonomic units
- PLS-DA
partial least squares discrimination analysis
- BMI
body mass index
- APOA1
apolipoprotein A1
- APOB
apolipoprotein B
- ALT
alanine transaminase
- AST
aspartate transaminase
- TG
triglyceride
- TCHO
total cholesterol
- LPA
lipoprotein A
- NEFA
non-esterifed fatty acid
- HCY
homocysteine
- ASCI
acute spinal cord injury
- LPS
lipopolysaccharide
- PCoA
Principle coordinates analysis
- NMDS
non-metric multidimensional scaling analysis
- PLS-DA
partial least square-discriminant analysis
- AD
Alzheimer’s disease
- HM
healthy male
- PU
patient with quadriplegia and SCI
Supplementary File 1
Supplementary File 2
Supplementary File 3
Supplementary File 4
References
- 1.Pickelsimer E, Shiroma EJ, Wilson DA. Statewide investigation of medically attended adverse health conditions of persons with spinal cord injury. J Spinal Cord Med. 2010;33:221–231. doi: 10.1080/10790268.2010.11689699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tate DG, Chiodo A, Cameron AP, Meade M, Krassioukov A. Risk factors associated with neurogenic bowel complications and dysfunction in spinal cord injury. J Arch Phys Med Rehabil. 2016;97:1679–1686. doi: 10.1016/j.apmr.2016.03.019. [DOI] [PubMed] [Google Scholar]
- 3.Ozisler Z, Koklu K, Ozel S, Unsal-Delialioglu S. Outcomes of bowel program in spinal cord injury patients with neurogenic bowel dysfunction. J Neural Regen Res. 2015;10:1153–1158. doi: 10.4103/1673-5374.160112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Koo BI, Bang TS, Kim SY, Ko SH, Kim W, Ko HY. Anorectal manometric and urodynamic parameters according to the spinal cord injury lesion. J Ann Rehabil Med. 2016;40:528–533. doi: 10.5535/arm.2016.40.3.528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Longo WE, Ballantyne GH, Modlin IM. The colon, anorectum and spinal cord patient. A review of the functional alternations of the denervated hindgut. Dis Colon Rectum. 1989;32:261–267. doi: 10.1007/BF02554543. [DOI] [PubMed] [Google Scholar]
- 6.Dethlefsen L, McFall-Ngai M, Relman DA. An ecological and evolutionary perspective on human microbe mutualism and disease. Nature. 2007;449:811–818. doi: 10.1038/nature06245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hooper LV, Littman DR, Macpherson AJ. Interactions between the microbiota and the immune system. Science. 2012;336:1268–1273. doi: 10.1126/science.1223490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yano JM, Yu K, Donaldson GP, Shastri GG, Ann P, Ma L, Nagler CR, Ismagilov RF, Mazmanian SK, Hsiao EY. Indigenous bacteria from the gut microbiota regulate host serotonin biosynthesis. Cell. 2015;161:264–276. doi: 10.1016/j.cell.2015.02.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hill DA, Artis D. Intestinal bacteria and the regulation of immune cell homeostasis. Annu Rev Immunol. 2010;28:623–667. doi: 10.1146/annurev-immunol-030409-101330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.El Aidy S, Dinan TG, Cryan JF. Gut microbiota: the conductor in the orchestra of immune-neuroendocrine communication. Clin Ther. 2015;37:954–967. doi: 10.1016/j.clinthera.2015.03.002. [DOI] [PubMed] [Google Scholar]
- 11.Balzan S, de Almeida Quadros C, de Cleva R, Zilberstein B, Cecconello I. Bacterial translocation: overview of mechanisms and clinical impact. J Gastroenterol Hepatol. 2007;22:464–471. doi: 10.1111/j.1440-1746.2007.04933.x. [DOI] [PubMed] [Google Scholar]
- 12.Khosravi A, Yáñez A, Price JG, Chow A, Merad M, Goodridge HS, Mazmanian SK. Gut microbiota promote hematopoiesis to control bacterial infection. Cell Host Microbe. 2014;15:374–381. doi: 10.1016/j.chom.2014.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mazo IB, Massberg S, von Andrian UH. Hematopoietic stem and progenitor cell trafficking. Trends Immunol. 2011;32:493–503. doi: 10.1016/j.it.2011.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gungor B, Adiguzel E, Gursel I, Yilmaz B, Gursel M. Intestinal microbiota in patients with spinal cord injury. PLoS One. 2016;11:e0145878. doi: 10.1371/journal.pone.0145878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Myers J, Lee M, Kiratli J. Cardiovascular disease in spinal cord injury: an overview of prevalence, risk, evaluation, and management. Am J Phys Med Rehabil. 2007;86:142–152. doi: 10.1097/PHM.0b013e31802f0247. [DOI] [PubMed] [Google Scholar]
- 16.Hopman MT. Circulatory responses during arm exercise in individuals with paraplegia. Int J Sports Med. 1994;15:126–131. doi: 10.1055/s-2007-1021033. [DOI] [PubMed] [Google Scholar]
- 17.Vidal J, Javierre C, Curia FJ, Garrido E, Lizarraga MA, Segura R. Long-term evolution of blood lipid profiles and glycemic levels in patients after spinal cord injury. Spinal Cord. 2003;41:178–181. doi: 10.1038/sj.sc.3101390. [DOI] [PubMed] [Google Scholar]
- 18.Schmid A, Halle M, Stützle C, König D, Baumstark MW, Storch MJ, Schmidt-Trucksäss A, Lehmann M, Berg A, Keul J. Lipoproteins and free plasma catecholamines in spinal cord injured men with different injury levels. Clin Physiol. 2000;20:304–310. doi: 10.1046/j.1365-2281.2000.00263.x. [DOI] [PubMed] [Google Scholar]
- 19.Doulames VM, Plant GW. Induced pluripotent stem cell therapies for cervical spinal cord injury. Int J Mol Sci. 2016;17:530. doi: 10.3390/ijms17040530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.DeVivo M, Biering-Sørensen F, New P, Chen Y. International spinal cord injury data set. Standardization of data analysis and reporting of results from the international spinal cord injury core data set. Spinal Cord. 2006;44:535–540. [Google Scholar]
- 21.Krogh K, Perkash I, Stiens SA, Biering-Sørensen F. International bowel function extended spinal cord injury data set. J Spinal Cord. 2009;47:235–241. doi: 10.1038/sc.2008.103. [DOI] [PubMed] [Google Scholar]
- 22.Langille MG, Zaneveld J, Caporaso JG, McDonald D, Knights D, Reyes JA, Clemente JC, Burkepile DE, Vega Thurber RL, Knight R, Beiko RG, Huttenhower C. Predictive functional profiling of microbial communities using 16S rRNA marker gene sequences. Nat Biotechnol. 2013;31:814–821. doi: 10.1038/nbt.2676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Parks DH, Tyson GW, Hugenholtz P, Beiko RG. STAMP: statistical analysis of taxonomic and functional profiles. Bioinformatics. 2014;30:3123–3124. doi: 10.1093/bioinformatics/btu494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.White JR, Nagarajan N, Pop M. Statistical methods for detecting differentially abundant features in clinical metagenomic samples. PLoS Comput Biol. 2009;5:e1000352. doi: 10.1371/journal.pcbi.1000352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wu Q, Li YL, Ning GZ, Feng SQ, Chu TC, Li Y, Hao Y, Wu QL. Epidemiology of traumatic cervical spinal cord injury in Tianjin, China. Spinal Cord. 2012;50:740–744. doi: 10.1038/sc.2012.42. [DOI] [PubMed] [Google Scholar]
- 26.Engkasan JP, Sudin SS. Neurogenic bowel management after spinal cord injury: malaysian experience. J Rehabil Med. 2013;45:141–144. doi: 10.2340/16501977-1074. [DOI] [PubMed] [Google Scholar]
- 27.Yasmeen R, Rathore FA, Ashraf K, Butt AW. How do patients with chronic spinal injury in pakistan manage their bowels? A cross-sectional survey of 50 patients. Spinal Cord. 2010;48:872–875. doi: 10.1038/sc.2010.46. [DOI] [PubMed] [Google Scholar]
- 28.Han TR, Kim JH, Kwon BS. Chronic gastrointestinal problems and bowel dysfunction in patients with spinal cord injury. Spinal Cord. 1998;36:485–490. doi: 10.1038/sj.sc.3100616. [DOI] [PubMed] [Google Scholar]
- 29.Kirshblum SC, Gulati MO, Connor KC, Voorman SJ. Bowel care practices in chronic spinal cord injury patients. Arch Phys Med Rehabil. 1998;79:20–23. doi: 10.1016/s0003-9993(98)90201-5. [DOI] [PubMed] [Google Scholar]
- 30.Stone JM, Nino-Murcia M, Wolfe VA, Perkash I. Chronic gastrointestinal problems in spinal cord injury patients: a prospective analysis. Am J Gastroenterol. 1990;85:1114–1119. [PubMed] [Google Scholar]
- 31.Krogh K, Christensen P, Sabroe S, Laurberg S. Neurogenic bowel dysfunction score. Spinal Cord. 2006;44:625–631. doi: 10.1038/sj.sc.3101887. [DOI] [PubMed] [Google Scholar]
- 32.Wahman K, Nash MS, Lewis JE, Seiger A, Levi R. Increased cardiovascular disease risk in swedish persons with paraplegia: the stockholm spinal cord injury study. J Rehabil Med. 2010;42:489–492. doi: 10.2340/16501977-0541. [DOI] [PubMed] [Google Scholar]
- 33.Van den Berg ME, Castellote JM, de Pedro-Cuesta J, Mahillo-Fernandez I. Survival after spinal cord injury: a systematic review. J Neurotrauma. 2010;27:1517–1528. doi: 10.1089/neu.2009.1138. [DOI] [PubMed] [Google Scholar]
- 34.Wilmore J, Costill D. Physiology of sport and exercise. 3rd edition. Champaign: Human Kinetics; 2006. [Google Scholar]
- 35.Gilbert O, Croffoot JR, Taylor AJ, Nash M, Schomer K, Groah S. Serum lipid concentrations among persons with spinal cord injury-a systematic review and meta-analysis of the literature. Atherosclerosis. 2014;232:305–312. doi: 10.1016/j.atherosclerosis.2013.11.028. [DOI] [PubMed] [Google Scholar]
- 36.Wang YH, Chen SY, Wang TD, Hwang BS, Su TC. The relationships among serum glucose, albumin concentrations and carotid atherosclerosis in men with spinal cord injury. Atherosclerosis. 2009;206:528–534. doi: 10.1016/j.atherosclerosis.2009.02.035. [DOI] [PubMed] [Google Scholar]
- 37.Bauman WA, Adkins RH, Spungen AM, Herbert R, Schechter C, Smith D, Kemp BJ, Gambino R, Maloney P, Waters RL. Is immobilization associated with an abnormal lipoprotein profile? Observations from a diverse cohort. Spinal Cord. 1999;37:485–493. doi: 10.1038/sj.sc.3100862. [DOI] [PubMed] [Google Scholar]
- 38.Washburn RA, Figoni SF. High density lipoprotein cholesterol in individuals with spinal cord injury: the potential role of physical activity. Spinal Cord. 1999;37:685–695. doi: 10.1038/sj.sc.3100917. [DOI] [PubMed] [Google Scholar]
- 39.Jeon JY, Steadward RD, Wheeler GD, Bell G, McCargar L, Harber V. Intact sympathetic nervous system is required for leptin effects on resting metabolic rate in people with spinal cord injury. J Clin Endocrinol Metab. 2003;88:402–407. doi: 10.1210/jc.2002-020939. [DOI] [PubMed] [Google Scholar]
- 40.Chen PS, Wang CC, Bortner CD, Peng GS, Wu X, Pang H, Lu RB, Gean PW, Chuang DM, Hong JS. Valproic acid and other histone deacetylase inhibitors induce microglial apoptosis and attenuate lipopolysaccharide-induced dopaminergic neurotoxicity. Neuroscience. 2007;149:203–212. doi: 10.1016/j.neuroscience.2007.06.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kigerl KA, Gensel JC, Ankeny DP, Alexander JK, Donnelly DJ, Popovich PG. Identification of two distinct macrophage subsets with divergent effects causing either neurotoxicity or regeneration in the injured mouse spinal cord. J Neurosci. 2009;29:13435–13444. doi: 10.1523/JNEUROSCI.3257-09.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Busch SA, Horn KP, Silver DJ, Silver J. Overcoming macrophage-mediated axonal dieback following CNS injury. J Neurosci. 2009;29:9967–9976. doi: 10.1523/JNEUROSCI.1151-09.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Labus JS, Oezguen N, Hollister EB, Tillisch K, Savidge T, Versalovic J, Mayer EA. 752 regional brain morphology is associated with gut microbial metabolites in irritable bowel syndrome (IBS) Gastroenterology. 2015;148:S142. [Google Scholar]
- 44.Kigerl KA, Mostacada K, Popovich PG. Gut microbiota are disease-modifying factors after traumatic spinal cord injury. Neurotherapeutics. 2017;15:60–67. doi: 10.1007/s13311-017-0583-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Espinosa-Medina I, Saha O, Boismoreau F, Chettouh Z, Rossi F, Richardson WD, Brunet JF. The sacral autonomic outflow is sympathetic. Science. 2016;354:893–897. doi: 10.1126/science.aah5454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Huang HL, Zhou YJ, Zheng TY, Nie YQ, Du YL. Changes of intestinal flora in rats with non-alcoholic fatty liver disease and its significance. Guangdong Medical Journal. 2016;37:9. [Google Scholar]
- 47.Dubourg G, Lagier JC, Armougom F, Robert C, Audoly G, Papazian L, Raoult D. High-level colonisation of the human gut by Verrucomicrobia following bread-spectrum antibiotic treatment. Int J Antimicrob Agents. 2013;41:149–155. doi: 10.1016/j.ijantimicag.2012.10.012. [DOI] [PubMed] [Google Scholar]
- 48.Rye KA, Barter PJ. Formation and metabolism of prebeta-migrating, lipid-poor apolipoprotein A-I. Arterioscler Thromb Vasc Biol. 2004;24:421–428. doi: 10.1161/01.ATV.0000104029.74961.f5. [DOI] [PubMed] [Google Scholar]
- 49.Chen GL, Liu L, Xie S, Liu H, Liu YQ, Li YS. High-density lipoprotein associated factors apoA-I and serum amyloid a in Chinese non-diabetic patients with coronary heart disease. Chin Med J. 2010;123:658–663. [PubMed] [Google Scholar]
- 50.Floch MH. Intestinal microecology in health and wellness. J Clin Gastroenterol. 2011;45:S108–110. doi: 10.1097/MCG.0b013e3182309276. [DOI] [PubMed] [Google Scholar]
- 51.Wallace TC, Guarner F, Madsen K, Cabana MD, Gibson G, Hentges E, Sanders ME. Human gut microbiota and its relationship to health and disease. Nutr Rev. 2011;7:392–403. doi: 10.1111/j.1753-4887.2011.00402.x. [DOI] [PubMed] [Google Scholar]
- 52.Louis P, Flint HJ. Development of a semiquantitative degenerate real-time PCR-based assay for estimation of numbers of butyryl-coenzyme A (CoA) CoA transferase genes in complex bacterial samples. Appl Environ Microbiol. 2007;73:2009–2012. doi: 10.1128/AEM.02561-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Bourassa MW, Alim I, Bultman SJ, Ratan RR. Butyrate, neuroepigenetics and the gut microbiome: can a high fiber diet improve brain health? Neurosci Lett. 2016;625:56–63. doi: 10.1016/j.neulet.2016.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Liao M, Xie YL, Mao Y, Lu Z, Tan A, Wu C, Zhang Z, Chen Y, Li T, Ye Y, Yao Z, Jiang Y, Li H, Li X, Yang X, Wang Q, Mo Z. Comparative analyses of fecal microbiota in Chinese isolated Yao population, minority Zhuang and rural Han by 16sRNA sequencing. Sci Rep. 2018;8:1142. doi: 10.1038/s41598-017-17851-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kovatcheva-Datchary P, Nilsson A, Akrami R, Lee YS, De Vadder F, Arora T, Hallen A, Martens E, Björck I, Bäckhed F. Dietary fiber-induced improvement in glucose metabolism is associated with increased abundance of prevotella. Cell Metab. 2015;22:971–982. doi: 10.1016/j.cmet.2015.10.001. [DOI] [PubMed] [Google Scholar]
- 56.Hofer U. Microbiome: pro-inflammatory prevotella? Nat Rev Microbiol. 2014;12:5. doi: 10.1038/nrmicro3180. [DOI] [PubMed] [Google Scholar]
- 57.Simon MC, Strassburger K, Nowotny B, Kolb H, Nowotny P, Burkart V, Zivehe F, Hwang JH, Stehle P, Pacini G, Hartmann B, Holst JJ, MacKenzie C, Bindels LB, Martinez I, Walter J, Henrich B, Schloot NC, Roden M. Intake of lactobacillus reuteri improves incretin and insulin secretion in glucose-tolerant humans: a proof of concept. Diabetes Care. 2015;38:1827–1834. doi: 10.2337/dc14-2690. [DOI] [PubMed] [Google Scholar]
- 58.Vogt NM, Kerby RL, Dill-McFarland KA, Harding SJ, Merluzzi AP, Johnson SC, Carlsson CM, Asthana S, Zetterberg H, Blennow K, Bendlin BB, Rey FE. Gut microbiome alterations in Alzheimer’s disease. Sci Rep. 2017;7:13537. doi: 10.1038/s41598-017-13601-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.