Abstract
Acalculous cholecystitis etiologies while numerous, some of them are less-known such as brucellosis. In this report, we elaborate the clinical findings, investigations and management of two female patients presenting acalculous cholecystitis in whom diagnosis of acute brucellosis was retained. Both patients had fever, asthenia and abdominal tenderness. Laboratory results showed evidence of inflammation as well as hepatic cytolysis while cholestasis was noted in one patient. In both cases, ultrasound study and CT confirmed the presence of acalculous cholecystitis. Serology (tube agglutination test) led to the diagnosis of brucellosis. Diagnosis of brucellosis-related acute cholecystitis was established in both cases based on imaging findings as well as serology without resorting to cholecystectomy. Favourable clinical response to specific antibiotic therapy further supported our diagnosis as well as our decision to avoid surgery. Although few cases have been reported, brucellosis must be considered as a cause of acalculous cholecystitis, especially in endemic countries.
Keywords: infectious diseases, surgery, pancreas and biliary tract
Background
Owing to disease control in cattle, brucellosis has become rare in developed countries. However, it still remains endemic in some countries due to the lack of vaccination of livestock.1 2
Brucellosis symptoms are polymorphous and lack specificity. It can lead to various complications affecting several organs.2 Occurrence of acute acalculous cholecystitis is rare in acute brucellosis and has been seldom reported as the presenting symptom of this disease. In this regard, we report two new cases of acute acalculous cholecystitis revealing acute brucellosis with a review of similar cases reported in the literature.
Case presentation
Case A
A 23-year-old female patient with a history of allergic asthma was admitted in our internal medicine department for a 10-day history of fever, asthenia, diffuse myalgia and night sweats. She reported consumption of unpasteurised dairy products. On examination, she had fever at 39°C and generalised abdominal tenderness, especially in the right hypochondrium. Otherwise, generalised examination showed no other abnormalities.
Case B
A 62-year-old female patient, with no medical history, was admitted in our internal medicine department for diarrhoea and vomiting lasting for 2 weeks associated with fever and night sweats. The patient reported regular consumption of unpasteurised dairy products. Clinical examination found an asthenic patient with persistent fever. Abdominal examination showed tenderness of the right hypochondrium. The rest of the clinical examination was normal.
Investigations
Case A
Routine laboratory tests revealed evidence of inflammation: C reactive protein at 33 mg/L and erythrocyte sedimentation rate at 48 mm/hour. Cytolysis was also noted with both aspartate transaminase and alanine transaminase elevated, respectively, at 160 UI/L (normal range: 5–34 UI/L) and 230 UI/L (normal range: <55 UI/L). Bilirubin was within normal range with no cholestasis. Serum lipase test was also normal. Complete blood count (CBC) showed leucopenia with white blood cell count of 1860/mm3 (4000–10 000/mm3) and lymphopenia at 370/mm3. Haemoglobin and platelet count were normal. Renal function tests were within normal range. Given this presentation, infectious causes were suspected. Blood cultures and urinalysis were negative. Serologies of hepatitis B, hepatitis C, Epstein-Barr virus and cytomegalovirus were negative. Abdominal ultrasound revealed a non-distended, acalculous, thick-walled gallbladder with 12 mm thick and heterogeneous wall (figure 1). Intrahepatic and extrahepatic bile ducts were non-dilated and latent peritoneal effusion was noted. CT of the abdomen highlighted a distended thick-walled gallbladder and homogeneous hepatomegaly (figure 2). No acid-fast bacilli were found on sputum examination and chest X-ray was normal. Immunological screening did not detect antinuclear antibodies. As the patient reported consumption of dairy products and given the recrudescence of brucellosis cases in our country, serology of brucellosis was performed (tube agglutination test) and was positive (1/180). Thus, the diagnosis of acute brucellosis revealed by acute acalculous cholecystitis was retained.
Figure 1.
Abdominal ultrasound showing non-distended, acalculous, thick-walled gallbladder.
Figure 2.
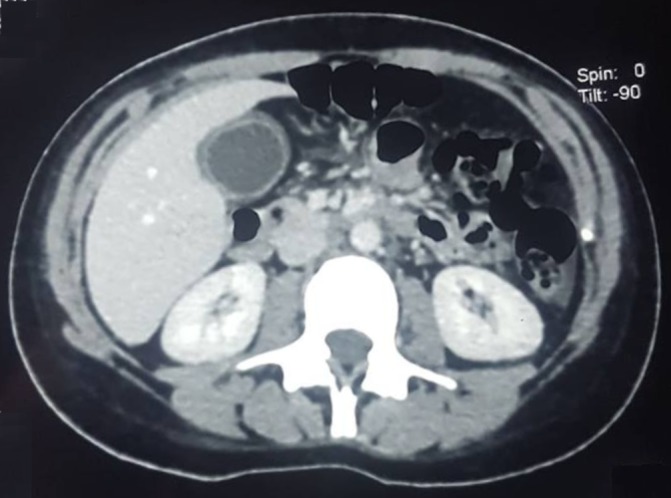
Abdominal CT showing dilated thick-walled gallbladder.
Case B
Routine laboratory tests revealed evidence of inflammation: C reactive protein at 114 mg/L and erythrocyte sedimentation rate at 80 mm/hour. CBC showed leucopenia with white blood cell count of 2700/mm3 (4000–10 000/mm3). Normocytic anaemia was also noted with haemoglobin of 108 g/L and mean corpuscular volume of 92 fL (80–100 fL). Platelet count was normal. Liver tests revealed cytolysis with aspartate transaminase at 88 UI/L (normal range: 5–34 UI/L) and alanine transaminase at 122 UI/L (normal range: <55 UI/L). It also showed an increased gamma-glutamyl transferase serum level at 94 UI/L (normal range: <64 UI/L) while bilirubin and alkaline phosphatase serum level were within normal range. Sepsis secondary to gastrointestinal tract infection was suspected. Both blood and stool cultures were negative. Abdominal ultrasound revealed an acalculous, thick-walled gallbladder with laminated aspect of the gallbladder wall and homogeneous splenomegaly. Abdominal CT showed acalculous, non-distended gallbladder with wall thickening and non-dilated intrahepatic and extrahepatic bile ducts. Since the patient had reported consumption of unpasteurised dairy products, brucellosis serology was requested (tube agglutination test) and was positive (1/200). Diagnosis of acute brucellosis associated with acute acalculous cholecystitis was retained.
Treatment
Case A
The patient was treated with doxycycline 200 mg per day and rifampicin (15 mg/kg/day) for 6 weeks. Cholecystectomy was not indicated.
Case B
The patient received antibiotic therapy with rifampicin (15 mg/kg/day) and doxycycline 200 mg per day for 6 weeks. Cholecystectomy was not indicated.
Outcome and follow-up
Case A
Clinical course was favourable with sustained apyrexia, disappearance of abdominal pain and the normalisation of liver function. An abdominal ultrasound after 2 weeks of antibiotic therapy showed a thin-walled, normal sized gallbladder with disappearance of peritoneal effusion.
Case B
Progressive improvement of the initial symptomatology was noted with lasting apyrexia as well as a regression of laboratory signs of inflammation. Abdominal ultrasound at 1 month of treatment was without abnormalities with a thin-walled gallbladder.
Discussion
We herein report two cases of acute acalculous cholecystitis secondary to acute brucellosis. Although our two patients did not undergo surgery and we did not acquire histological or bacteriological proof, positive serology and favourable clinical outcome on specific antibiotic therapy led us to consider brucellosis as the cause of acalculous cholecystitis.
Brucellosis is the most widespread anthropozoonosis in the world, accounting for 500 000 new human cases per year.3 Digestive contamination predominates in Tunisia (62%), mostly due to Tunisian habits of ingesting unpasteurised raw cheese and milk.2 It is considered a public health problem because of its recurrence in recent years in relation to larger contamination of livestock.2
Clinical manifestations of the acute phase of brucellosis are classically vague and not very specific. Visceral involvement may reveal the disease. However, if isolated, it can make the diagnosis challenging. Digestive manifestations are frequent during acute brucellosis such as nausea, vomiting, constipation and diarrhoea. Hepatomegaly and splenomegaly are found in 15%–20% of patients,1 more rarely granulomatous hepatitis or splenic abscess.1
Acalculous cholecystitis could be related to a large variety of causes. Mainly to be considered are anatomical abnormalities of the gallbladder and cystic duct such as stenosis and obstructive or compressive causes; thrombosis of the cystic artery resulting in ischaemia and vesicular gangrene; spasm or fibrous inflammation of the hepatopancreatic sphincter with or without associated pancreatitis; diabetes mellitus; certain systemic diseases such as systemic lupus erythematosus; specific infections such as typhoid fever; systemic bacterial infections (salmonellosis) and parasitic infections such as distomatosis hepatica and also viral infections such as HIV and viral hepatitis, infections and systemic diseases. To sum it up, it seems that acalculous cholecystitis is either due to obstruction of cystic duct with secondary bacterial overgrowth as in calculous cholecystitis, or formation of an abscess and/or gallbladder necrosis.4 5
Mechanisms of acute cholecystitis in brucellosis are yet to be understood. Gallbladder wall-thickening may be related to biliary cell invasion by the Brucella since the bacterium was isolated in bile culture after cholecystectomy.6–8 Brucella dissemination can be either lymphatic or haematogenous during bacteremia.6
While hepatic involvement is classic during brucellosis, occurrence of acute acalculous cholecystitis is rare and has been described, since 1934, to our knowledge, only in 17 cases (table 1). It affected 12 men and 5 women with a mean age of 45 years. Thirteen patients had cholecystectomy and the Brucella germ was isolated in 11 bile cultures. Blood cultures were positive in 10 cases. Brucella melitensis was the most frequently isolated species. Pathological examination of the gallbladders after cholecystectomy generally showed non-specific inflammatory signs. Almost all cases had favourable clinical course on antibiotic therapy.6–8
Table 1.
Acalculous cholecystitis related to brucellosis reported cases
| Author | Year | Age/ gender |
Blood culture | Bile culture | Gallbladder calculus | Cholecyst ectomy |
Antibiotic therapy |
| White10 | 1934 | 58/F | – | Brucella abortus | Absent | – | – |
| Mettier11 | 1934 | 57/M | Brucella melitensis | B. melitensis | Absent | Yes | – |
| Hewlet12 | 1947 | 58/M | Negative | B. abortus | Present | No | Streptomycin |
| Valenzuela Cases13 | 1971 | 56/M | – | – | Absent | Yes | Tetracycline + streptomycin |
| Morris14 | 1979 | 34/M | Brucella suis | B. suis | Present | Yes | Tetracycline + streptomycin |
| Berbegal Serra15 | 1986 | 33/M | B. melitensis | Negative | Absent | Yes | Tetracycline + streptomycin |
| Shaheen16 | 1989 | 42/F | B. melitensis | B. melitensis | Absent | Yes | Tetracycline + streptomycin |
| Colmenero17 | 1996 | 58/M | B. melitensis | Negative | Present | Yes | Doxycycline + streptomycin |
| Fasquelle18 | 1999 | 72/F | B. melitensis | B. melitensis | Present | Yes | Doxycycline+ rifampicin |
| Serrano Guerra19 | 1999 | 59/M | B. melitensis | Negative | Present | Yes | Doxycycline + streptomycin |
| Ashley20 | 2000 | 6/M | B. abortus | – | Absent | No | TMP/SMX + rifampicin |
| Miranda8 | 2001 | 34/M | Negative | B. melitensis | Present | Yes | Doxycycline + rifampicin |
| Andriopoulos21 | 2003 | 72/M | B. melitensis | B. melitensis | Absent | Yes | Doxycycline + streptomycin |
| López-Prieto22 | 2003 | 56/F | Negative | B. melitensis | Present | Yes | Doxycycline + streptomycin |
| Kanafani7 | 2005 | 55/M | Brucella spp | Brucella spp | Present | Yes | Doxycycline + rifampicin |
| Kanafani7 | 2005 | 29/F | Negative | Brucella spp | Present | Yes | Doxycycline + rifampicin |
| Al-Otaibi6 | 2010 | 42/M | – | B. melitensis | Absent | No | Doxycycline + streptomycin |
F, female; M, male; TMP/SMX, trimethoprim/sulfametoxazole.
Acute cholecystitis is an unusual presenting feature of brucellosis and may lead to an emergency cholecystectomy. However, although clinical presentation may be misleading, laboratory data, blood cultures and especially serology help to establish the diagnosis. Brucella is difficult to culture, as such, the microbiologist needs to be aware of the clinical suspicion and blood cultures must be continued for a prolonged period. Tube agglutination test offers a quick, sensitive way for the diagnosis of acute brucellosis and is recommended for epidemiological studies. Ultrasound aspect is generally that of a non-distended, acalculous, thick-walled gallbladder. Existence of concomitant biliary calculus raises a diagnosis problem and most likely leads to cholecystectomy. Diagnosis will be made later on by bile culture and histological examination.
Consensual treatment in acute or subacute brucellosis is the administration of doxycycline for a minimum of 6 weeks with either rifampicin for 6 weeks or an aminoglycoside: streptomycin or gentamicin for the first 2 weeks.1 9
In our two patients, favourable clinical course and disappearance of the thickening of the gallbladder wall on specific antibiotic therapy show that medical treatment may be sufficient for acute cholecystitis complicating brucellosis and surgery should be kept as a last resort once the diagnosis is established.
Learning points.
Etiologies of acute acalculous cholecystitis are numerous.
Considering infectious diseases such as brucellosis may prevent unnecessary cholecystectomy.
Blood culture, serology and in case of surgery bile culture are essential to diagnosis.
Antibiotic treatment may prove sufficient with no need to cholecystectomy.
Footnotes
Contributors: AH participated in the conception of the idea, in the redaction and literature review for this manuscript. MSH participated in the redaction and literature review of the manuscript. IB participated in the conception of the idea and in the redaction and literature review of the manuscript. EC participated in the revision and checking of the manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient consent for publication: Obtained.
References
- 1. Maurin M, Brian J-P. Brucellose. EMC (Elsevier Masson SAS, Paris), Maladies infectieuses, 8-038-A-10. 2009.
- 2. Zribi M, Ammari L, Masmoudi A, et al. complications and treatment of brucellosis: 45-patient study. Pathol Biol 2009;57:349–52. [DOI] [PubMed] [Google Scholar]
- 3. Queipo-Ortuno MI, Moratap OP, Manchado P, et al. Rapid diagnosis of human brucellosis by peripheral-blood PCR assay. J clin Microbiol 1997;35:2927–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Trésallet C, Bastien L, Rabahi Y, et al. Cholécystite alithiasique révélatrice d’une hépatite aiguë secondaire au virus de l’hépatite C. J Radiol 2010;91(7-8):813–5. 10.1016/S0221-0363(10)70121-9 [DOI] [PubMed] [Google Scholar]
- 5. Boukinda F, Chakirou L, Wang PJ, et al. Les cholécystites aigues non lithiasiques. A propos de 3 observations. Médecine d’Afrique Noire 1993:3. [Google Scholar]
- 6. Al-Otaibi FE. Acute acalculus cholecystitis and hepatitis caused by Brucella melitensis. J Infect Dev Ctries 2010;4:464–7. 10.3855/jidc.618 [DOI] [PubMed] [Google Scholar]
- 7. Kanafani ZA, Sharara AI, Issa IA, et al. Acute calculous cholecystitis associated with brucellosis: A report of two cases and review of the literature. Scand J Infect Dis 2005;37(11-12):927–30. 10.1080/00365540500264035 [DOI] [PubMed] [Google Scholar]
- 8. Miranda RT, Gimeno AE, Rodriguez TF, et al. Acute cholecystitis caused by Brucella melitensis: case report and review. J Infect 2001;42:77–8. 10.1053/jinf.2000.0757 [DOI] [PubMed] [Google Scholar]
- 9. Ariza J, Bosilkovski M, Cascio A, et al. Perspectives for the treatment of Brucellosis in the 21st century: the ioannina recommendations. PLoS Med 2007;4:e317 10.1371/journal.pmed.0040317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. White CS. Cholecystitis as a complication of brucellosis: report of a case. Med Ann Distr 1934;12:60–2. [Google Scholar]
- 11. Mettier SR. Hepatitis and Cholecystitis in the course of Brucella Infection. Arch Intern Med 1934;54:702–9. 10.1001/archinte.1934.00160170045004 [DOI] [Google Scholar]
- 12. Hewlett JS, Ernstene AC. Brucella abortus infection of the gallbladder treated with streptomycin; report of a case. Cleve Clin Q 1947;14:258–63. 10.3949/ccjm.14.4.258 [DOI] [PubMed] [Google Scholar]
- 13. Valenzuela Casas E. [Melitococcic hemorrhage cholecystitis]. Rev Esp Enferm Apar Dig 1971;33:723–6. [PubMed] [Google Scholar]
- 14. Morris SJ, Greenwald RA, Turner RL, et al. Brucella-induced cholecystitis. Am J Gastroenterol 1979;71:481–4. [PubMed] [Google Scholar]
- 15. Berbegal Serra JM, Rodríguez Alfaro JJ, Royo García G. [Brucellosis complicated by acute alithiasic cholecystitis]. Rev Esp Enferm Apar Dig 1986;70:88. [PubMed] [Google Scholar]
- 16. Shaheen SE, el-Taweel AZ, al-Awadi NZ, et al. Acute calcular cholecystitis associated with Brucella melitensis. Am J Gastroenterol 1989;84:336–7. [PubMed] [Google Scholar]
- 17. Colmenero JD, Reguera JM, Martos F, et al. Complications associated with Brucella melitensis infection: a study of 530 cases. Medicine 1996;75:195–211. 10.1097/00005792-199607000-00003 [DOI] [PubMed] [Google Scholar]
- 18. Fasquelle D, Charignon G, Rami M. Acute calcular cholecystitis in a patient with brucellosis. Eur J Clin Microbiol Infect Dis 1999;18:599–600. 10.1007/s100960050355 [DOI] [PubMed] [Google Scholar]
- 19. Serrano Guerra FJ, Sánchez Chaparro MA, Valdivielso Felices P, et al. [Acute cholecystitis during systemic brucellosis]. Rev Clin Esp 1999;199:621–2. [PubMed] [Google Scholar]
- 20. Ashley D, Vade A, Challapalli M. Brucellosis with acute acalculous cholecystitis. Pediatr Infect Dis J 2000;19:1112–3. 10.1097/00006454-200011000-00024 [DOI] [PubMed] [Google Scholar]
- 21. Andriopoulos P, Tsironi M, Asimakopoulos G. Acute abdomen due to Brucella melitensis. Scand J Infect Dis 2003;35:204–5. 10.1080/0036554021000027025 [DOI] [PubMed] [Google Scholar]
- 22. López-Prieto MD, Aller AI, Alcaraz S, et al. [Acute calculous cholecystitis associated with Brucella melitensis]. Enferm Infecc Microbiol Clin 2003;21:464–5. [PubMed] [Google Scholar]



