Abstract
A 53-year-old man with dysphagia underwent uneventful placement of a percutaneous endoscopic gastrostomy (PEG) tube for long-term enteral feeding access. 11 hours after the procedure, it was discovered that he had accidentally dislodged the feeding tube. On physical examination, he was found to have a benign abdomen without evidence of peritonitis or sepsis. He was observed overnight with serial abdominal examinations and nasogastric decompression. In the morning, he was taken back to the endoscopy suite where endoscopic clips were employed to close the gastric wall defect and a PEG tube was replaced at an adjacent site. The patient was fed 24 hours thereafter and discharged from the hospital 48 hours after the procedure. Early accidental removal of a PEG tube in patients without sepsis or peritonitis can be safely treated with simultaneous endoscopic closure of the gastrotomy and PEG tube replacement, resulting in earlier enteral feeding and shorter hospital stay.
Keywords: parenteral/enteral feeding, stomach and duodenum, gastrointestinal surgery
Background
Percutaneous endoscopic gastrostomy (PEG) has been the widely preferred invasive method of enteral feeding access for more than 30 years. Based on Medicare data, it is estimated that over 125 000 PEG tubes are placed annually in the USA alone.1 The procedure is safe with success rates of over 95% and morbidity ranging from 9% to 17%.2 3 One of the most dreaded PEG tube complications is early accidental dislodgement before the gastrocutaneous tract has matured. This complication has been reported in 1%–4% of cases with neurologically impaired patients at highest risk.4 In severe cases, early dislodgement can lead to intraperitoneal spillage of gastric contents with associated peritonitis and sepsis, necessitating emergent operative exploration.5 6 In the majority of cases, however, peritoneal contamination is minimal and more conservative approach is adopted. The mainstay of therapy has involved nasogastric decompression for a minimum of 5–7 days, at times necessitating parenteral nutrition to allow the gastric wall defect to close spontaneously.3 4 More recently, endoscopic clips and sutures have been employed to close the gastrotomy resulting in expedited recovery.7–9 In spite of this, in-hospital length of stay has remained upwards of a week and hospital costs associated with this complication have remained high in part because of a need for additional endoscopic procedure to replace the PEG tube before hospital discharge. This case illustrates that the subset of patients without peritonitis and sepsis after early accidental PEG tube dislodgement can be safely treated with simultaneous endoscopic closure of the gastric wall defect and PEG tube replacement resulting in earlier enteral feeding and shorter in-hospital length of stay.
Case presentation
A 53-year-old man with medical history of hypertension, peripheral arterial disease and diabetes was brought to the hospital by his family suffering from a large left middle cerebral artery infarct. A formal modified barium swallow study revealed severe oropharyngeal dysphagia with aspiration of liquids and solids. The neurology team, anticipating the need for long-term enteral nutritional support, consulted general surgery for placement of a PEG tube. The patient had no previous surgeries and no abdominal pathology.
The patient was taken to the endoscopy suite, and an esophagogastroduodenoscopy was performed under conscious sedation. The oesophagus, stomach and duodenum were found to be within normal limits. A 20-French PEG tube was then inserted into the stomach in the left upper quadrant of the abdomen using the standard push method. The position of the internal bumper was confirmed by direct visualisation. The PEG tube was placed to dependent drainage for the first 24 hours according to our institutional protocols. An abdominal binder was placed on the patient’s abdomen, covering the PEG tube.
Around 10 o’clock at night the day of the procedure, approximately 11 hours after the PEG tube placement, the nurse entered the patient’s room planning to administer his medications. She found the patient disoriented and agitated. His abdominal binder was found undone on the ground next to his bed. The feeding tube was completely dislodged and intertwined in the patient’s bedsheets. It is unknown how much time passed between the actual removal of the feeding tube and its detection. The general surgery team was immediately called to the bedside to examine the patient.
Investigations
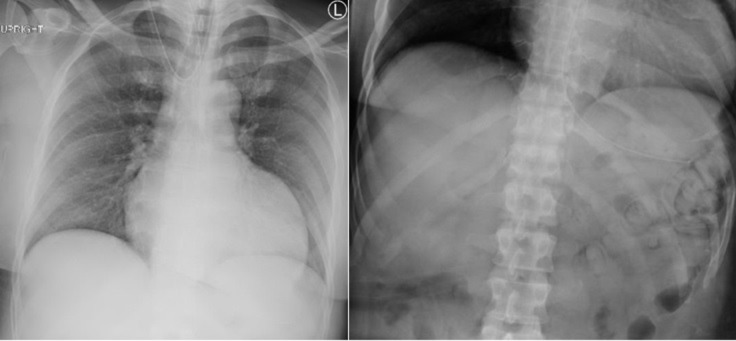
Once at the bedside, a thorough physical examination was performed. The patient was afebrile, non-tachycardic and normotensive. His abdomen was non-distended, and the PEG tube entry site in the left upper quadrant did not exhibit any signs of bleeding or infection. The patient’s abdomen was soft and non-tender, without any rigidity, rebound tenderness or other signs of peritonitis. Basic laboratory evaluation including a complete blood count revealed a normal haemoglobin level and an absence of leukocytosis. Chest and abdominal radiographs were found to be unremarkable with no evidence of pneumoperitoneum (figure 1). Unlike other clinical situations involving hollow viscus perforation, in this scenario, the absence of pneumoperitoneum on a plain radiograph was more telling and clinically useful compared with its presence. The radiographic absence of pneumoperitoneum suggests that the gastrotomy was likely not substantially enlarged by the act of the patient pulling the PEG tube out of the stomach and that the gastric wall defect was in the process of closing. The presence of pneumoperitoneum, on the other hand, would be less clinically significant because the air could have been displaced from the gastric lumen into the peritoneal cavity either during the PEG tube placement or during its dislodgment.
Figure 1.
Upright plain chest and abdominal radiographs showing the absence of pneumoperitoneum after early percutaneous endoscopic gastrostomy dislodgement.
Treatment
The patient’s abdominal examination was benign, and there was no evidence of significant intraperitoneal spillage of gastric contents or resultant systemic inflammatory reaction. Consequently, we decided to proceed with a conservative treatment course consisting of placement of a nasogastric tube for gastric decompression and intravenous antibiotics (β-lactam, metronidazole and fluconazole) followed by clinical observation with frequent serial abdominal examinations. Throughout the night, the patient’s vitals remained within normal limits and his abdominal examination was unchanged.
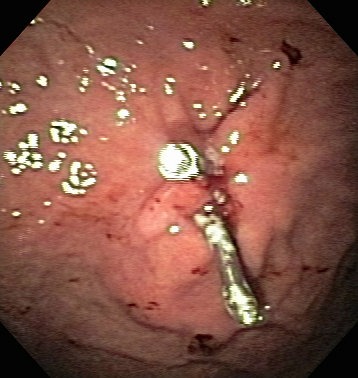
The next morning, approximately 10 hours following the accidental removal of the PEG tube, a decision was made to take the patient back to the endoscopy suite for definitive management. Under conscious sedation, an esophagogastroduodenoscopy was performed using a therapeutic gastroscope. There were no problems insufflating the stomach with air suggestive of at least partial spontaneous closure of the gastrotomy. Careful inspection of the anterior gastric mucosa led to identification of the previous PEG tube site. No appreciable full-thickness gastric wall defect was identified again suggesting at minimum partial closure. Only a small mucosal defect was seen with superficial rim of ulceration surrounding the site (figure 2). The mucosal defect was closed by deployment of two Boston Scientific endoscopic Resolution Clips (figure 3). A new 20-French PEG tube was subsequently inserted in much the same way as in the original procedure at an adjacent site. At the end of the case, the internal bumper was again visualised endoscopically. It was flush against the gastric mucosa and far enough away that even when the stomach was decompressed, the bumper did not interfere with the clips on the previous PEG site (figure 4). We elected not to perform a gastropexy during the repeat endoscopic procedure because after talking to the nursing staff and the patient, we determined the incident of dislodgement to be a truly accidental event that was unlikely to repeat itself with the patient having no other risk factors.
Figure 2.

Gastric mucosal defect at dislodged percutaneous endoscopic gastrostomy tube site.
Figure 3.
Closure of gastric wall defect with two endoscopic metallic clips.
Figure 4.
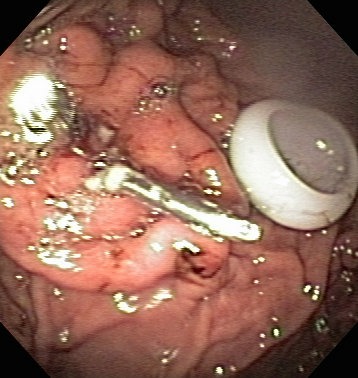
Placement of a new percutaneous endoscopic gastrostomy tube at an adjacent site to the closed gastrotomy.
Outcome and follow-up
Following the second endoscopy procedure, the feeding tube was kept to dependent drainage with only medications administered through it for 24 hours. The following day, patient was started on bolus Jevity 1.2 tube feeds, which he tolerated without any issues. 48 hours after the endoscopic closure of the gastric wall defect and replacement of the PEG tube, patient was discharged home to the care of his family. He was seen during a follow-up visit in the general surgery clinic 1 month after discharge from the hospital. He had no abdominal complaints and the PEG tube was functioning without problems.
Discussion
It is well established that early enteral feeding is superior to parenteral feeding, especially in septic and trauma patients.10–12 Since its introduction in the 1980s, the PEG tube has become the most common invasive method of obtaining long-term enteral feeding access. A PEG tube consists of silicone or polyurethane tubing ending in an inner bolster. The role of the inner bolster is to provide traction on the anterior gastric wall to aid in formation of a gastrocutaneous fistula.3 The inner bolster is soft and permits PEG tube removal with relatively minimal outward force. Additionally, PEG tubes have an external retention ring that has a dual purpose – prevention of antegrade tube migration and maintenance of the inner bolster at a constant distance from the surface of the abdomen. A mature gastrocutaneous tract typically takes 7–14 days to form.5 6 One of the most common PEG tube complications is accidental PEG tube dislodgement. The presence or absence of a mature gastrocutaneous tract helps classify PEG tube dislodgement into ‘early’ (<14 days, tract absent) and ‘late’ (>14 days, tract present).5 6 While late dislodgement is more than twice as common as early dislodgement, seen in 10%–15% of cases, it is far less morbid.3 13 When a tube is dislodged in the presence of a mature tract, a prompt replacement with a balloon-tipped feeding tube or a Foley catheter is necessary because the tract can narrow within hours of tube removal. If the tract closes completely, a repeat endoscopy is usually needed to replace the PEG tube.
Early dislodgement is reported to occur in up to 5% of cases and is equivalent to hollow viscus perforation with the potential for peritoneal contamination and associated sequelae. Endoscopists and surgeons should be cognizant of this potentially highly morbid complication and employ strategies to minimise the risk. Patient selection is an important element of risk management. Patients with impaired wound healing, immunocompromise and ascites are at risk for delayed gastrocutaneous fistula maturation.14–16 Patients with neurologic dysfunction are frequently in need of long-term enteral feeding access but are also more susceptible to confusion, delirium and agitation, which predisposes them to accidental removal of catheters and tubes.14 17 In a small percentage of patients with multiple high-risk features for early tube dislodgement, the risks may simply outweigh the benefits. In such patients, an alternative enteral feeding strategy or parenteral nutrition ought to be considered. Despite the presence of some high-risk features, the vast majority of patients are reasonable PEG candidates, assuming proper precautions are taken. Routine use of abdominal binders to keep the PEG tube up against the abdominal wall to minimise inadvertent pulling or tugging is encouraged.2 3 14 18 19 Use of restraints, both chemical and mechanical, in addition to periodic re-orientation especially in delirious and agitated patients is another worthwhile measure.14 18 19 Studies have not shown any difference between starting tube feeds early (<4 hours post-procedure) and late (>24 hours).20 21 In our experience, however, delaying tube feeds until the day after the procedure decreases the incidence and severity of peritoneal contamination and sepsis when a PEG tube becomes dislodged in the early post-operative period. In high-risk patients, endoscopic gastropexy using T-fasteners or the Carter-Thomason device should be strongly considered.22 23 In a more recent innovation, the SafetyBreak decoupling device is another step in the right direction in preventing accidental PEG tube dislodgement.24
In the early years, PEG tube dislodgement in the early post-operative period was treated with laparotomy, closure of the gastrotomy and open feeding tube placement regardless of clinical presentation.2–4 To this date, surgical exploration is the recommended treatment for patients presenting with peritonitis and sepsis. With the advent of minimally invasive surgery, laparoscopic approach to the management of gastric perforation has become the standard of care. Conversely, the management of patients without gross peritoneal spillage, benign clinical examination, no evidence of systemic inflammatory response, and favourable radiographic findings (ie, no pneumoperitoneum on plain film) has evolved considerably. At first, clinical observation, nasogastric decompression, intravenous antibiotics and hyperalimentation were employed to allow the gastrotomy defect to close spontaneously.5 6 In 2004, closure of the gastric wall defect using endoscopic clips was first described by Dr. Sugawa and associates.25 26 Since then, endoscopic suturing has been used for the same purpose.7 9 27 If performed in a timely fashion, these endoscopic interventions are effective at minimising peritoneal contamination and avoiding major surgery. However, even with these recent advancements, enteral feeding is delayed, and in-hospital stay is typically at least 5–7 days.
CT with water soluble oral contrast, usually gastrografin, is an important adjunct in the management of early PEG tube dislodgement.2–4 16 28 29 While some surgeons perform this study routinely, it usually only alters clinical management in a specific subset of patients.2 3 28 29 In a patient with peritonitis and sepsis, CT imaging is superfluous and only leads to a delay in definitive therapy as operative intervention is indicated regardless of radiologic results. On the other hand, in a patient with normal clinical examination (ie, patient described in this case report), the likelihood that CT imaging will show a massive extravasation of contrast into the peritoneal cavity is minimal, making this study low yield in this subset of patients. One type of patient in whom CT imaging is highly recommended due to its ability to change management is someone with ambiguous clinical examination and equivocal laboratory studies and plain film imaging.2 3 28 29
The presence of pneumoperitoneum on CT or plain film imaging, regardless of its amount, after early PEG dislodgement is clinically meaningless because it is impossible to determine whether the intraluminal air escaped into the peritoneal cavity during the placement of the PEG tube or its dislodgment.30 On the other hand, the absence of peritoneal air is much more telling and clinically useful, signifying small-sized or closing gastric wall defect.30 The most important piece of information gleaned from CT imaging in this clinical setting is the distribution of the water-soluble oral contrast, with three distinct patterns identified.28 29 If the contrast is found only in the gastric lumen and does not extravasate, conservative management is indicated. Conversely, free intraperitoneal extravasation of oral contrast signifies a large gastric perforation with operative intervention warranted. The third pattern consists of small-volume contained contrast extravasation. In these cases, both conservative and operative management are acceptable and the entire clinical picture, not just imaging results, should be taken into consideration when making the final decision.
We present a case of an accidental removal of a PEG tube within 12 hours of placement. Our patient displayed benign clinical features obviating the need for emergent surgical intervention. After overnight observation with nasogastric decompression, the patient underwent simultaneous endoscopic closure of the gastrotomy and PEG replacement at an adjacent site. Enteral nutrition was resumed after 24 hours, and the patient was discharged within 48 hours.
Given the literature review and our experiences, we recommend careful patient selection, routine use of abdominal binders, delaying feeds for 24 hours and selective use of endoscopic gastropexy or a decoupling device to reduce the risk of early PEG dislodgement. In the event it does occur, a subset of patients with a favourable clinical presentation can be safely treated with endoscopic clip or suture gastrotomy closure and immediate PEG replacement. This approach results in earlier enteral feeding and shorter hospital stay.
Learning points.
Early dislodgement is a potentially highly morbid complication that occurs within 7–14 days of percutaneous endoscopic gastrostomy (PEG) tube placement before the gastrocutaneous fistula has matured.
Careful patient selection, routine use of abdominal binders and restraints, delaying tube feeding for 24 hours, and selective use of endoscopic gastropexy and/or a decoupling device can help lessen the risk and sequelae of early PEG dislodgement.
Treatment of early PEG dislodgement resulting in significant peritoneal contamination and sepsis is emergent open or laparoscopic surgical exploration.
Traditional treatment of patients without peritonitis and sepsis includes observation with nasogastric decompression and more recently endoscopic closure of the gastrotomy with clips or sutures followed by delayed PEG replacement.
In selected patients with benign clinical features, endoscopic gastrotomy closure and immediate PEG replacement result in earlier initiation of tube feeds and shorter inpatient stay.
Footnotes
Contributors: All three of the primary authors: PC, MM and CS have contributed equally to the conception of the submitted work as well as acquisition and interpretation of data. All three were involved equally in drafting the work and critically revising it.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient consent for publication: Next of kin consent obtained.
References
- 1. Duszak R, Mabry MR. National trends in gastrointestinal access procedures: an analysis of Medicare services provided by radiologists and other specialists. J Vasc Interv Radiol 2003;14:1031–6. 10.1097/01.RVI.0000082983.48544.2C [DOI] [PubMed] [Google Scholar]
- 2. Schrag SP, Sharma R, Jaik NP, et al. Complications related to percutaneous endoscopic gastrostomy (PEG) tubes. A comprehensive clinical review. J Gastrointestin Liver Dis 2007;16:407–18. [PubMed] [Google Scholar]
- 3. Rahnemai-Azar AA, Rahnemaiazar AA, Naghshizadian R, et al. Percutaneous endoscopic gastrostomy: indications, technique, complications and management. World J Gastroenterol 2014;20:7739 10.3748/wjg.v20.i24.7739 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Potack JZ, Chokhavatia S. Complications of and controversies associated with percutaneous endoscopic gastrostomy: report of a case and literature review. Medscape J Med 2008;10:142. [PMC free article] [PubMed] [Google Scholar]
- 5. Marshall JB, Bodnarchuk G, Barthel JS. Early accidental dislodgement of PEG tubes. J Clin Gastroenterol 1994;18:210–2. 10.1097/00004836-199404000-00007 [DOI] [PubMed] [Google Scholar]
- 6. Mincheff TV. Early dislodgement of percutaneous and endoscopic gastrostomy tube. J S C Med Assoc 2007;103:13–15. [PubMed] [Google Scholar]
- 7. Kumar N, Thompson CC. Endoscopic therapy for postoperative leaks and fistulae. Gastrointest Endosc Clin N Am 2013;23:123–36. 10.1016/j.giec.2012.10.002 [DOI] [PubMed] [Google Scholar]
- 8. Baron TH, Song LM, Ross A, et al. Use of an over-the-scope clipping device: multicenter retrospective results of the first U.S. experience (with videos). Gastrointest Endosc 2012;76:202–8. 10.1016/j.gie.2012.03.250 [DOI] [PubMed] [Google Scholar]
- 9. Stavropoulos SN, Modayil R, Friedel D. Current applications of endoscopic suturing. World J Gastrointest Endosc 2015;7:777–89. 10.4253/wjge.v7.i8.777 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ono H, Azuma T, Miyaji H, et al. Effects of percutaneous endoscopic gastrostomy tube placement on gastric antral motility and gastric emptying. J Gastroenterol 2003;38:930–6. 10.1007/s00535-003-1174-z [DOI] [PubMed] [Google Scholar]
- 11. Moore FA, Feliciano DV, Andrassy RJ, et al. Early enteral feeding, compared with parenteral, reduces postoperative septic complications. The results of a meta-analysis. Ann Surg 1992;216:172–83. 10.1097/00000658-199208000-00008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Dwyer KM, Watts DD, Thurber JS, et al. Percutaneous endoscopic gastrostomy: the preferred method of elective feeding tube placement in trauma patients. J Trauma 2002;52:26–32. 10.1097/00005373-200201000-00007 [DOI] [PubMed] [Google Scholar]
- 13. Rosenberger LH, Newhook T, Schirmer B, et al. Late accidental dislodgement of a percutaneous endoscopic gastrostomy tube: an underestimated burden on patients and the health care system. Surg Endosc 2011;25:3307–11. 10.1007/s00464-011-1709-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Lin HS, Ibrahim HZ, Kheng JW, et al. Percutaneous endoscopic gastrostomy: strategies for prevention and management of complications. Laryngoscope 2001;111:1847–52. 10.1097/00005537-200110000-00033 [DOI] [PubMed] [Google Scholar]
- 15. Vanis N, Saray A, Gornjakovic S, et al. Percutaneous endoscopic gastrostomy (PEG): retrospective analysis of a 7-year clinical experience. Acta Inform Med 2012;20:235–7. 10.5455/aim.2012.20.235-237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Lohsiriwat V. Percutaneous endoscopic gastrostomy tube replacement: a simple procedure? World J Gastrointest Endosc 2013;5:14–18. 10.4253/wjge.v5.i1.14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Lockett MA, Templeton ML, Byrne TK, et al. Percutaneous endoscopic gastrostomy complications in a tertiary-care center. Am Surg 2002;68:117–20. [PubMed] [Google Scholar]
- 18. Santos PM, McDonald J. Percutaneous endoscopic gastrostomy: avoiding complications. Otolaryngol Head Neck Surg 1999;120:195–9. 10.1016/S0194-5998(99)70406-7 [DOI] [PubMed] [Google Scholar]
- 19. Schurink CA, Tuynman H, Scholten P, et al. Percutaneous endoscopic gastrostomy: complications and suggestions to avoid them. Eur J Gastroenterol Hepatol 2001;13:819–23. 10.1097/00042737-200107000-00010 [DOI] [PubMed] [Google Scholar]
- 20. Choudhry U, Barde CJ, Markert R, et al. Percutaneous endoscopic gastrostomy: a randomized prospective comparison of early and delayed feeding. Gastrointest Endosc 1996;44:164–7. 10.1016/S0016-5107(96)70134-7 [DOI] [PubMed] [Google Scholar]
- 21. Bechtold ML, Matteson ML, Choudhary A, et al. Early versus delayed feeding after placement of a percutaneous endoscopic gastrostomy: a meta-analysis. Am J Gastroenterol 2008;103:2919–24. 10.1111/j.1572-0241.2008.02108.x [DOI] [PubMed] [Google Scholar]
- 22. Timratana P, El-Hayek K, Shimizu H, et al. Percutaneous endoscopic gastrostomy (PEG) with T-fasteners obviates the need for emergent replacement after early tube dislodgement. Surg Endosc 2012;26:3541–7. 10.1007/s00464-012-2348-7 [DOI] [PubMed] [Google Scholar]
- 23. Rosenberger LH, Hu Y, Yang Z, et al. Gastropexy using the Carter-Thomason device in lieu of T-fasteners in a critically ill, severely obese patient: an innovative technique. Surg Laparosc Endosc Percutan Tech 2012;22:e316–e318. 10.1097/SLE.0b013e318264cf88 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Rosenberger LH, Guidry CA, Davis JP, et al. Reducing accidental dislodgement of the percutaneous endoscopic gastrostomy: a prospective trial of the "SafetyBreak" device. Surg Innov 2016;23:62–9. 10.1177/1553350615587408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Blocksom JM, Sugawa C, Tokioka S, et al. Endoscopic repair of gastrostomy after inadvertent removal of percutaneous endoscopic gastrostomy tube. Surg Endosc 2004;18:868–70. 10.1007/s00464-003-4541-1 [DOI] [PubMed] [Google Scholar]
- 26. Singhal S, Changela K, Culliford A, et al. Endoscopic closure of persistent gastrocutaneous fistulae, after percutaneous endoscopic gastrostomy (PEG) tube placement, using the over-the-scope-clip system. Therap Adv Gastroenterol 2015;8:182–8. 10.1177/1756283X15578603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Eskaros S, Ghevariya V, Krishnaiah M, et al. Percutaneous endoscopic suturing: an effective treatment for gastrocutaneous fistula. Gastrointest Endosc 2009;70:768–71. 10.1016/j.gie.2009.05.002 [DOI] [PubMed] [Google Scholar]
- 28. Milanchi S, Wilson MT. Malposition of percutaneous endoscopic-guided gastrostomy: Guideline and management. J Minim Access Surg 2008;4:1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Pofahl WE, Ringold F. Management of early dislodgment of percutaneous endoscopic gastrostomy tubes. Surg Laparosc Endosc Percutan Tech 1999;9:253–6. 10.1097/00129689-199908000-00004 [DOI] [PubMed] [Google Scholar]
- 30. Blum CA, Selander C, Ruddy JM, et al. The incidence and clinical significance of pneumoperitoneum after percutaneous endoscopic gastrostomy: a review of 722 cases. Am Surg 2009;75:39. [PubMed] [Google Scholar]