Abstract
Background
Little is known about the patient-reported and economic burdens of postherpetic neuralgia (PHN) among China’s urban population.
Methods
This noninterventional study was conducted among adults ≥40 years with PHN who were seeking medical care at eight urban hospitals in China. At one study site, patients completed a questionnaire evaluating the patient-reported disease burden (N=185). The questionnaire consisted of validated patient-reported outcomes including the Brief Pain Inventory (BPI), 5-dimension, 3-level EuroQol (EQ-5D-3L), Medical Outcomes Study Sleep Scale, and Work Productivity and Activity Impairment Questionnaire for Specific Health Problems. Questions on non-pharmacologic therapy and out-of-pocket (OOP) expenses were also included. At all study sites, physicians (N=100) completed a structured review of patient charts (N=828), which was used to derive health care resource utilization and associated costs from the societal perspective. Annual costs in Chinese Yuan Renminbi (RMB) for the year 2016 were converted to US dollars (US$).
Results
Patients (N=185, mean age 63.0 years, 53.5% female) reported pain of moderate severity (mean BPI score 4.6); poor sleep quantity (average of 5.3 hrs per night) and quality; and poorer health status on the EQ-5D-3L relative to the general Chinese population. Respondents also reported average annual OOP costs of RMB 16,873 (US$2541) per patient, mainly for prescription PHN medications (RMB 8990 [US$1354]). Substantial work impairment among employed individuals resulted in annual indirect costs of RMB 28,025 (US$4221). In the chart review, physicians reported that patients (N=828) had substantial health resource utilization, especially office visits; 98% had all-cause and 95% had PHN-related office visits. Total annual direct medical costs were RMB 10,002 (US$1507), mostly driven by hospitalizations (RMB 8781 [US$1323]).
Conclusion
In urban China, PHN is associated with a patient-reported burden, affecting sleep, quality-of-life, and daily activities including work impairment, and an economic burden resulting from direct medical costs and indirect costs due to lost productivity. These burdens suggest the need for appropriate prevention and management of PHN.
Keywords: postherpetic neuralgia, disease burden, health-related quality-of-life, EQ-5D, China, health care costs, productivity
Introduction
The varicella zoster virus is a highly infectious virus that has a worldwide distribution. In individuals who have previously been exposed to this virus, its reactivation results in a painful dermatomal rash that is known as herpes zoster (HZ), which is commonly referred to as shingles. Because of its widespread prevalence, HZ represents a global healthcare burden, with epidemiological data from North America, Europe, and the Asia-Pacific region suggesting a lifetime incidence of HZ of 3.0–5.0/1000 person-years.1 Since the risk of HZ increases with age, particularly among those >50 years old,1,2 the prevalence and burden of HZ will likely increase with the aging of the population. The most common complication of HZ is postherpetic neuralgia (PHN), defined as pain persisting for at least 1 month, 3 months, or 6 months after healing of the HZ rash.1,3 Depending on study methodology, population, and definition of the disease, it has been estimated that 5–30% of patients with HZ develop PHN.1
The pain associated with PHN is neuropathic in origin, defined as pain resulting from a lesion or disease of the peripheral or central somatosensory nervous systems.4 Neuropathic pain (NeP) does not respond to traditional pharmacologic interventions generally considered effective for nociceptive pain. Consequently, management of PHN is challenging and generally relies on pharmacologic agents from several drug classes (eg, anticonvulsants and antidepressants) that are approved for NeP but may have variable efficacy.5–8
The incidence rates of HZ and PHN in China are similar to those reported globally.9,10 A survey in Guangdong Province, using patient data from 2011 to 2013, estimated the regional lifetime prevalence of HZ infection at 3.5%, and following a diagnosis of HZ the rate of PHN was as high as 40% in these patients.9 A more recent epidemiologic study, based on chart review among 24 hospitals in 7 cities in China with large populations and high economic development, reported an overall population point prevalence of 7.7% for HZ and 2.3% for PHN; 29.8% of patients with HZ developed PHN.11
The presence of PHN further adds to the burden associated with HZ. From the patient’s perspective, PHN results in functional impairment, reductions in health-related quality-of-life (HRQoL), and lost productivity.12–14 In particular, reductions in HRQoL are both statistically significant and clinically relevant.13 PHN also results in excess health care resource utilization (HRU), increasing the economic burden to the health care systems and society in general.13,15–18 For example, a study based on real-world health care costs in the US reported that adjusted incremental annual health care costs among individuals >50 years of age with PHN were $7291 compared with matched controls without HZ.15 In contrast, adjusted incremental annual health care costs among non-PHN individuals with HZ were $1425 relative to matched non-HZ controls, indicating that the presence of PHN substantially increases resource utilization and costs relative to HZ. Similar trends in higher HRU and costs of PHN relative to HZ have also been observed in other countries.16–18
To prospectively reduce the potential burden of HZ and PHN, research over the past 15 years resulted in the development of two vaccines for the prevention of HZ, one for adults ≥50 years old (Zostavax®)19 and one for adults >60 years old (Shingrix®)20 both of which have received approval in the US. In the US, the current Centers for Disease Control and Prevention guidelines for immunization of adults recommend that adults >50 years old receive vaccination for the prevention of HZ.21 Unfortunately, neither of these vaccines is currently available in China, suggesting that PHN remains a substantial burden to Chinese patients and the health care system.
Few studies have investigated PHN among China’s urban population. Data on the epidemiology, HRU, and overall impact of PHN on patients’ HRQoL are sparse.9,10 To bridge this gap, the present study, which was a follow-up to a recent epidemiologic study on the prevalence of HZ and PHN in China,11 examined the patient-reported burden of PHN among adults ≥40 years old who sought medical care for their PHN. Additionally, the economic burden of PHN was evaluated from the societal perspective.
Materials and methods
Study design and participants
This noninterventional, cross-sectional study was conducted between August and December 2016 at 8 hospitals in Tier 1 and Tier 2 cities in China (Tier 1 cities have the largest populations, highest economic development/output, and greatest political influence, and Tier 2 cities have lesser degrees of the same characteristics); hospitals were located in Guangzhou, Shenzhen, Beijing, Shanghai, Nanjing, Xi’an, and Chengdu. All protocols were in accordance with accepted research practices described in Good Practices for Outcomes Research issued by the International Society for Pharmacoeconomics and Outcomes Research.22 Patients provided written informed consent before entering the study. The final protocol and documentation of informed consent were reviewed and approved by the Ethics Committee at Chinese PLA General Hospital, Hai Dian District, Beijing.
Patients identified with PHN during an office visit to a participating physician at the primary data collection site, the Chinese PLA General Hospital, Hai Dian District, Beijing, completed a survey questionnaire that included questions and measures to quantify the patient-reported burden of PHN. For participation in the survey, patients >40 years old were required to be literate in Chinese (reading and writing), have a cognitive ability to participate in a research study, and be willing to provide informed consent. Patients were excluded if they had a serious or unstable medical or psychological condition that might compromise participation.
For evaluation of HRU utilization and costs, physician participants from 8 hospitals were eligible to participate if they had a specialty in dermatology, neurology, and/or pain management and saw at least 200 patients over a 2-month period that met the eligibility requirement. Patient eligibility included being at least 40 years old and diagnosed with PHN; age >40 years was used as a cutoff to capture more PHN patients given its low prevalence. Each participating physician reviewed charts for 200–350 consecutive eligible patients who had office visits over a 30–60-day period to document the presence or absence of PHN, defined as pain persisting for ≥1 month following healing of HZ.
Survey assessments and outcomes
The patient survey was a de-identified, self-administered 20-min questionnaire that was created in English and translated into Chinese, with subsequent review by multiple independent linguists for accuracy of the translation. The questionnaire consisted of validated patient-reported outcomes (PROs) that captured pain (Brief Pain Inventory [BPI]),23 sleep (Medical Outcomes StudySleep Scale [MOS-SS]),24 and HRQoL or health status (5-dimension 3-level EuroQol [EQ-5D-3L]).25 Inclusion of the Work Productivity and Activity Impairment Questionnaire for Specific Health Problems V2.0, Clinical Practice Version (WPAI-SHP),26,27 evaluated the impact of PHN on impairment of work among employed patient participants, and on impairment of daily activities among all patient participants.
The BPI includes 4 items measuring pain severity (worst, least, average, and pain right now) and 7 items on pain interference that assess the impact of pain on daily function including general activity, mood, walking ability, work inside and outside the home, relations with people, sleep, and enjoyment of life. The BPI items are scored on a 0–10 scale where higher scores indicate worse pain and greater pain interference with activities, with a Pain Severity Index and a Pain Interference Index that can be calculated by taking the average of the 4 pain ratings and the 7 interference ratings, respectively.23 The BPI has been recommended by the Initiative on Methods, Measurement, and Pain Assessment in Clinical Trials (IMMPACT) as a core outcome measure for chronic pain clinical trials.28
The MOS-SS is a 12-item PRO consisting of 12 items that evaluate key constructs of sleep, with derived subscales for the domains of sleep disturbance (4 items), quantity of sleep (1 item), snoring (1 item), awakening due to short of breath or with headache (1 item), sleep adequacy (2 items), and somnolence (3 items). The Sleep Quantity item indicates the number of hours slept each night, and nine of the other items are used to generate the Sleep Problems Index, which assesses overall sleep problems; higher scores indicate greater sleep impairment, and this index is often used as an indication of sleep quality. Normative values of the MOS-SS subscales have been estimated for the US general population29 and were used as a reference to provide the context in the absence of such values for the Chinese population. Additionally, based on the reported number of hours of sleep per night, the proportion of patients with optimal sleep, defined as 7 or 8 hrs daily, was determined.
The EQ-5D-3L is a generic, preference-based PRO for assessing HRQoL and includes two components. The first component consists of 5 domains (Mobility, Self-Care, Usual Activities, Pain/Discomfort, Anxiety/Depression) with 3 response levels (“No problem,” “Some problems,” or “Extreme problems/unable to do”).25 Reported responses on the domains can be used to generate a utility score that represents a health state anchored at perfect health (=1) and death (=0), although utility scores less than 0 (ie, health state worse than death) are attainable. The current analysis used the United Kingdom value set for calculating utility scores,30 which enables comparisons across different countries using a common value set. The second component is a visual analog scale (VAS; 0= worst imaginable health to 100= best imaginable health) that assesses the current health status as reported by the patient.
The WPAI:SPH is a 6-item questionnaire that evaluates the effects of a specific health problem on self-reported productivity and activity during the past week. For the current analysis, the WPAI:SHP was adapted for PHN by including “your post herpetic neuralgia” in the questionnaire text. The WPAI:SHP includes subscales for absenteeism (absence from work), presenteeism (lost productivity while at work), overall work impairment (based on absenteeism and presenteeism), as well as the effects on non-work-related activities. The subscales are scored from 0% to 100%, where higher scores indicate greater work or activity impairment.26,27 The three work productivity subscales were evaluated only among participants who were employed for pay, while the regular activities subscale was evaluated in all participants.
For each eligible patient, physicians completed a 7–10 min, structured data collection form that included demographic and clinical characteristics, health history, pain experience, household income, medical insurance information, and treatment practices, including use of prescription and non-prescription therapies for treating PHN. In addition, all-cause and PHN-related HRU over the past 6 months were evaluated based on the use of office visits, emergency department (ED), and hospital visits included in the patient records. The PHN-related resource use was determined based on physician report of the number of the overall HRU events that were due to the patient’s PHN.
The economic burden of PHN from a societal perspective was estimated based on costs derived from the physician chart reviews and patient surveys. All-cause direct medical costs were estimated from physician-reported HRU. These estimates assumed care in a tertiary hospital and were based on best available cost data including information from the Chinese Ministry of Health for outpatient and inpatient costs;31 clinician consensus was used for direct costs for ED, since an official source for these costs was unavailable. For patient participants who were employed and completed the survey, indirect costs related to lost productivity were calculated from the WPAI:SHP using the method of Lofland et al32 by obtaining the average wage rate for employees in China33 and multiplying this value by the percentage of overall work impairment. Allowing for holidays and paid leave, these calculations assumed 47 work weeks per year. Monthly out-of-pocket (OOP) costs for prescription and nonprescription PHN therapies were also captured in the patient questionnaire.
Data analysis
Both HRU and costs were annualized by dividing the event or costs by the time period observation, in years, eg, 3 visits over 4 months would equate to 9 visits over 1 year (3/0.333=9). Costs are presented in Chinese Yuan Renminbi (RMB) and US dollars (US$) for the year 2016; conversion to US$ was based on 1 RMB = US$0.15062, which was the average value over 2016.34 Unit costs were RMB 301 (US$45) for office visits, RMB 200 (US$30) for ED visits, and RMB 12,716 (US$1915) for hospitalizations.
All data were reported as available, without any imputation strategy. Descriptive statistics, including numbers and percentages for dichotomous and polychotomous variables and means with their standard deviations for continuous variables, were used to characterize the patient-reported burden as well as HRU and their associated costs. Analyses were conducted using SAS version 9.3 (SAS Institute, Cary, NC) and R version 3.0.1.35
Results
Patient-reported burden
A total of 185 patients completed the survey questionnaire at the primary data collection site, and the demographic characteristics of this population (Table 1) show that the majority were female (53.5%) and were predominantly of Han ethnicity (94.1%) (Table 1); the mean age was 63 years, and 56.8% were retired.
Table 1.
Characteristics of patients diagnosed with postherpetic neuralgia who participated in the burden of illness survey (N=185)
| Variable | Value |
|---|---|
| Sex, n (%) | |
| Male | 86 (46.5) |
| Female | 99 (53.5) |
| Age, years, mean (SD); range | 63.0 (12.3); 40–86 |
| Age distribution, n (%) | |
| 40–54 years | 53 (28.6) |
| 55–64 years | 48 (25.9) |
| 65–99 years | 83 (44.9) |
| Ethnicity, n (%) | |
| Han | 174 (94.1) |
| Zhuang | 1 (0.5) |
| Man | 3 (1.6) |
| Hui | 1 (0.5) |
| Other | 3 (1.6) |
| Declined to answer | 3 (1.6) |
| Education, n (%) | |
| Less than high school | 47 (25.4) |
| High school | 62 (33.5) |
| Technical school/college (3 years) | 36 (19.5) |
| University (4 years) | 37 (20.0) |
| Postgraduate | 1 (0.5) |
| Employment status, n (%) | |
| Full-time | 39 (21.1) |
| Part-time | 2 (1.1) |
| Self-employed | 7 (3.8) |
| Not employed and not looking for work | 6 (3.2) |
| Retired | 105 (56.8) |
| Short-term disability | 6 (3.2) |
| Homemaker | 19 (10.3) |
| Monthly household income, n (%) | |
| RMB <4000 (<US$602) | 33 (17.8) |
| RMB 4000–9999 (US$602–US$1505) | 56 (30.2) |
| RMB ≥10,000 (≥ US$1506) | 44 (23.8) |
| Declined to answer | 33 (17.8) |
| Type of health coverage, n (%) | |
| Urban Employee Basic Medical Insurance (UEBMI)a | 101 (54.6) |
| Urban Resident Basic Medical Insurance (URBMI)b | 37 (20.0) |
| New Rural Cooperative Medical System (NRCMS)c | 14 (7.6) |
| Other types of insurance | 16 (8.6) |
| None of the above/no insurance | 14 (7.6) |
Notes: aObligatory insurance paid by the employer (generally 6% of salary) and employee (generally 2% of salary); self-employed individuals pay the entire contribution. bJointly paid by individuals and the state; unemployed individuals and those on social assistance are subsidized by the state. cContributions from individuals, rural collectives, and local governments, albeit reimbursement is low compared with urban enterprise employees and covers only serious disease but not wage loss.
Abbreviation: RMB, Chinese Yuan Renminbi; SD, standard deviation; US$, United States dollars.
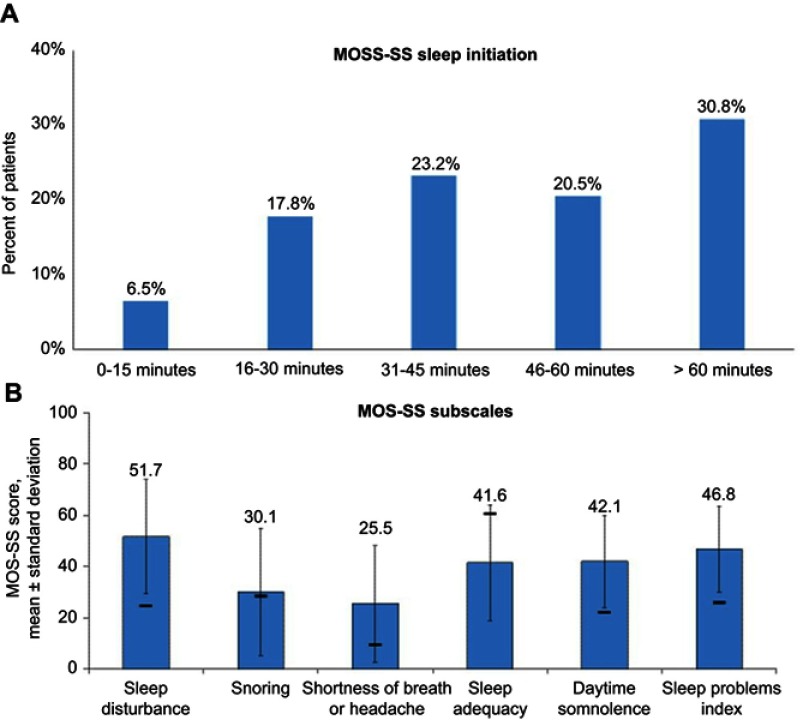
Patient participants reported pain of moderate severity and mild-to-moderate pain interference, with mean (SD) scores of 4.6 (2.0) and 3.8 (2.2) on the BPI Pain Severity Index and Pain Interference Index, respectively (Table 2). Generally, poor HRQoL was indicated by mean (SD) EQ-5D-3L scores of 60.1 (18.6) on the VAS and 0.65 (0.2) on the calculated health utility index (Table 2). The average hours of sleep each night was 5.3 (1.4), and few respondents (16.2%) reported optimal sleep (7–8 hrs daily). In almost one-third of respondents (30.8%), sleep initiation required 60 mins or longer (Figure 1A). The mean score of 46.8 (16.7) on the MOS-SS Sleep Problems Index indicated poor sleep quality, as did all other MOS-SS subscales, with mean scores that were consistently lower than available normative reference values for a US population (Figure 1B).
Table 2.
Patient-reported outcomes among patients diagnosed with postherpetic neuralgia who participated in the burden of illness survey (N=185)
| Patient-reported outcome measure | Value |
|---|---|
| BPI, mean (SD) | |
| Pain Severity Index | 4.6 (2.0) |
| Pain Interference Index | 3.8 (2.2) |
| EQ-5D-3L, mean (SD) | |
| VAS | 60.1 (18.6) |
| Health state utilities score | 0.65 (0.20) |
Abbreviations: BPI, Brief Pain Inventory; EQ-5D-3L, 5-dimension, 3-level EuroQol; VAS, visual analog scale; SD, standard deviation.
Figure 1.
Sleep problems as indicated by time to sleep initiation (A) and subscale scores (B) on the Medical Outcomes Study Sleep Scale (MOS-SS) among patients diagnosed with postherpetic neuralgia who participated in the survey. Higher scores indicate poorer sleep quality except on the Sleep adequacy subscale. For reference in (B), general population norms for the US population (data from reference Hays RD et al.29) are shown as black horizontal bars, since normative values have not been established for the Chinese population.
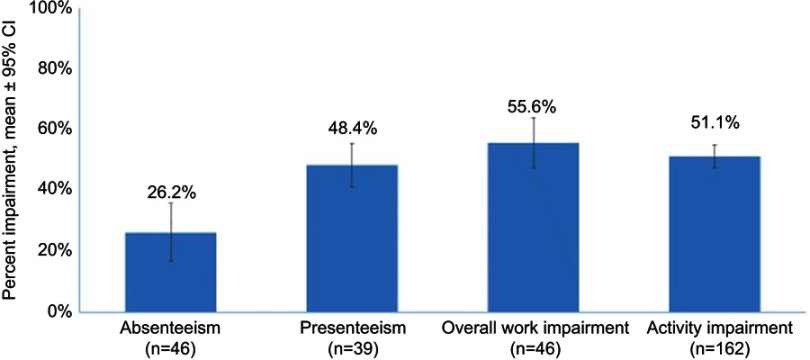
Participants who responded that they worked more than 1 hr in the past 7 days and answered the productivity and absenteeism questions on the WPAI:SHP reported losing 26.2% of productive time through lost days from work (absenteeism) and 48.4% of productive time while at work (presenteeism) due to their PHN (Figure 2). Overall work impairment due to PHN in these employed individuals was 55.6%. Among all respondents regardless of employment status, PHN resulted in overall activity impairment, other than work, of 51.1% (Figure 2).
Figure 2.
Self-reported work and activity impairment resulting from postherpetic neuralgia assessed using Work Productivity and Activity Impairment Questionnaire for Specific Health Problems (WPAI:SHP).
The mean (SD) annual indirect costs related to lost productivity were RMB 12,318 (16,619) for absenteeism-related costs, RMB 18,930 (10,227) costs related to presenteeism, and RMB 28,025 (19,039) for total indirect costs. These are equivalent to US$1855 ($2503), US$2851 ($1540), and US$4221 ($2868) for absenteeism, presenteeism, and total indirect costs, respectively.
Patient participants reported using a variety of nonpharmacologic therapies for treatment of their PHN (Table 3). While physical therapy was the most frequently cited type of nonpharmacologic treatment (33.5%), almost one-third of respondents also reported use of traditional Chinese medicine (31.9%) and acupuncture (30.3%; Table 3). The highest annual OOP costs were incurred for PHN prescription medications, RMB 8990 (US$1354), with additional OOP costs of RMB 3734 (US$562) for traditional Chinese medicines and RMB 4149 (US$625) for other PHN therapies (Table 4).
Table 3.
Self-reported use of nonpharmacologic therapies for postherpetic neuralgia among patients who participated in the burden of illness survey (N=185)
| Type of therapy | Number (%) of patients |
|---|---|
| Physical therapy | 62 (33.5) |
| Traditional Chinese medicine | 59 (31.9) |
| Acupuncture | 56 (30.3) |
| Massage | 29 (15.7) |
| Heat therapy | 22 (11.9) |
| Exercise | 19 (10.3) |
| Transcutaneous electrical nerve stimulation | 10 (5.4) |
| Chiropractor care | 9 (4.9) |
| Yoga | 3 (1.6) |
| Spinal decompression | 2 (1.1) |
| Attend support groups | 2 (1.1) |
| Other (nonspecified) nondrug treatments/programs | 12 (6.5) |
| No answer | 31 (16.8) |
Table 4.
Out-of-pocket costs among patients diagnosed with postherpetic neuralgia who participated in the burden of illness survey (N=185)
| Out-of-pocket cost category | Annual cost, mean (SD) | |
|---|---|---|
| RMB | US$ | |
| Prescription medication for PHN | 8990 (18,259) | 1354 (2750) |
| Traditional Chinese medicine for PHN | 3734 (10,687) | 562 (1610) |
| Other therapy for PHN | 4149 (10,056) | 625 (1515) |
Abbreviations: PHN, postherpetic neuralgia; RMB, Chinese Yuan Renminbi; SD, standard deviation; US$, United States dollars.
Clinician-reported HRU and associated costs
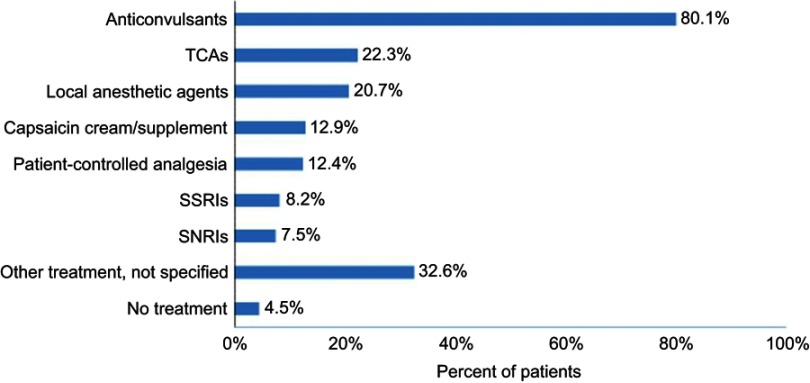
Overall, 100 physicians at the 8 hospitals identified 835 patients with PHN (51.3% female; 33.7% 40–59 years old and 66.3% ≥60 years old) and provided data on HRU and costs for 828 of these patients. While physicians reported use of prescription medications from a variety of pharmacologic classes for the treatment of PHN (Figure 3), anticonvulsants were the most frequently prescribed class (80.1%) followed by tricyclic antidepressants (22.3%). However, 32.6% of physicians reported use of other unspecified medications for PHN, and a low proportion of patients, 4.5%, had no recorded treatment.
Figure 3.
Medications used by patients to treat postherpetic neuralgia.
Abbreviations: SNRIs, serotonin-norepinephrine reuptake inhibitors; SSRI, selective serotonin reuptake inhibitors; TCAs, tricyclic antidepressants.
Among the HRU categories (Table 5), office visits had the highest reported use, both all-cause (98%) and PHN-related (95%). Among patients with available data on ED visits, the rates of ED use were 12.5% (81/647) and 9.9% (66/666) for all-cause and PHN-related visits, respectively, and similarly for patients with available data on hospitalizations, 19.1% (133/698) had at least 1 all-cause hospitalization and 13.3% (93/699) had at least 1 PHN-related hospitalization. Annualized units of use showed means (SD) of 9.4 (11.4) and 5.8 (7.8) for all-cause and PHN-related office visits per patient, respectively (Table 5). The mean (SD) number of ED visits, 0.4 (1.3) per year, appeared to be due to PHN (Table 5). The mean (SD) number of all-cause and PHN-related hospitalizations were 0.7 (2.4) and 0.4 (1.8) per year, respectively, with mean (SD) length-of-stay of 14.9 (13.5) days among all-cause hospitalized patients and 9.2 (9.3) days for those with PHN-related hospitalizations (Table 5).
Table 5.
Annualized health care resource utilization and costs derived from physician from chart reviews (N=828)
| Resource category | All-cause | PHN-related |
|---|---|---|
| Patients with resource use, % (patients with available data) | ||
| Office visits | 98 (828) | 95 (828) |
| ED visits | 12.5 (647) | 9.9 (666) |
| Hospitalizations | 19.1 (698) | 13.3 (699) |
| Annualized units of use, mean (SD) | ||
| Office visits | 9.4 (11.4) | 5.8 (7.8) |
| ED visits | 0.4 (1.3) | 0.4 (1.3) |
| Hospitalizations | 0.7 (2.4) | 0.4 (1.8) |
| Length of stay among hospitalized patients, days | 14.9 (13.5) | 9.2 (9.3) |
| Annualized costs, mean (SD)a | ||
| Office visits | RMB 2808 (3434);US$423 (US$517) | NC |
| ED visits | RMB 71 (267);US$11 (US$40) | NC |
| Hospitalizations | RMB 8781 (30,673); US$1323 (US$4620) | NC |
| Total costs | RMB 10,002 (30,114); US$1507 (US$4536) | NC |
Note: aUnit costs were RMB 301 (US$45) for office visits, RMB 200 (US$30) for ED visits, and RMB 12,716 (US$1915) for hospitalizations.
Abbreviations: ED, emergency department; NC, not calculated; PHN, postherpetic neuralgia; RMB, Chinese Yuan Renminbi; US$, United States dollars; SD, standard deviation.
As shown in Table 5, the mean (SD) total all-cause direct medical costs were estimated to be RMB 10,002 (30,114) per year (US$1507 [US$4536]) and were driven by hospitalization costs of RMB 8781 (30,673) per year (US$1323 [US$4620]). While ED visits had the lowest associated costs, RMB 71 (267), the annual cost of office visits was RMB 2808 (3434); these convert to US$11 (US$40) and US$423 (US$517), respectively.
Discussion
As a follow-up to the recent epidemiologic study that reported a 2.3% prevalence of PHN in China,11 the current analysis shows that PHN is associated with a substantial patient-reported burden and also results in frequent HRU that from the societal perspective has financial implications for patients and the overall health care system in China.
In the current analysis, survey respondents with PHN reported not only pain of moderate severity and mild-to-moderate pain interference with their daily activities, but also a substantial impact on sleep and HRQoL. In particular, respondents reported impairment of both sleep quantity and quality, with fewer hours of sleep per night than is considered optimal. Mean scores on all subscales of the MOS-SS, including the Sleep Problems Index, indicated substantial sleep problems relative to normative values, albeit the norms were for a US population29 in the absence of available normative values for China. These sleep problems are consistent with the impact of PHN on sleep that has been reported in other studies,36–39 including the presence of mild-to-severe insomnia symptoms,40 and reflect the well-recognized reciprocal relationship between pain and sleep.41–43
Pain and sleep are also important contributors to HRQoL, and pain, in particular, is one of the dimensions included in the EQ-5D-3L. Thus, it was not surprising that the mean EQ-5D-3L health utility score, 0.65, was lower than the norm of 0.951 that has been reported for the Chinese population and lower than the values for age groups that overlap with the age distribution in the current study.44 Similarly, the mean EQ-5D-3L VAS score of 60.1 is lower than the Chinese population norm of 80.4. The lower values on both the utility score and the VAS indicate a substantial reduction in HRQoL relative to the general population. This difference between PHN and normative utility values is within the range of 0.03–0.52 that has been estimated to indicate clinical significance45 and is similar to the weighted pooled score of 0.61 for PHN that was reported in a meta-analysis of NeP conditions.46 Although there is also no clear consensus as to what represents a clinically relevant difference on the EQ-5D-3L VAS, the difference between PHN and the general population exceeds the range of 4.3–12.1, which has been estimated to indicate clinical relevance in different populations.47–49
Inclusion of a demographic younger than generally evaluated in studies of PHN also enabled evaluation of the impact of PHN on work productivity, since in China, the mandatory age for retirement in women is 50–55 and for men is 60.50 Among those who were employed, there was higher work impairment due to lost productivity on the job (presenteeism) than resulting from absenteeism, consistent with what has been reported in a Canadian study of patients with HZ and PHN14 as well as in other common pain conditions.51,52 Overall, work was impaired by 55.6%, resulting in annual indirect costs of RMB 12,318 (US$4221), which has implications for not only lost individual wages but also for an economic impact on employers and society as a whole resulting from lost productivity.
Survey participants also reported annual OOP costs in excess of RMB 16,000 (US$2400), a substantial amount considering that almost 1 in 5 participants (17.8%) had an annual household income < RMB 48,000 (US$7230) and almost one-third (30.2%) had an annual income RMB 48,000–120,000 (US$7230–18074). These OOP costs exceeded mean total direct costs RMB 10,002 (US$1507). While just over half of the OOP costs (53.2%) were for prescription medications for PHN, the remainder of the OOP costs were traditional Chinese medicine, acupuncture, and other therapies, consistent with the use of a variety of nonpharmacologic therapies reported by the survey participants. While further research is needed to determine why OOP costs are higher relative to direct medical costs, this observation may represent issues of lack of access, where patients may self-pay for resources rather than receiving clinical (reimbursed) care.
Physicians reported substantial use of pharmacologic therapies among patients with PHN, and only 4.5% of patients reviewed had no treatment recorded. These pharmacologic treatments appeared to be consistent with guidelines for PHN management, with the predominant use of anticonvulsants followed by tricyclic antidepressants; both classes are considered first-line treatment.5,6,53
Office visits was the HRU category that received the most use in terms of annual number of visits per patient. However, total all-cause HRU costs were driven by hospitalizations, which accounted for 87.8% of the total direct medical costs. Although there were few hospitalizations, this resource category is the most costly, and length of stay among hospitalized patients was more than 2 weeks for all-cause and more than 1 week (9.2 days) for PHN-related hospitalizations. The length of stay of PHN-related hospitalizations is within the range of 8.7–14.8 days reported in other studies, but length of stay is likely to be dependent on standard of care and national health care setting.54–56
Total annual direct all-cause medical costs were estimated to be RMB 10,002 (US$1507) per year. Even considering that the prevalence of PHN is only 2.3%,11 this represents a substantial economic burden on the health care system given that the population of China is approximately 1.4 billion individuals. When also considering the indirect costs due to lost productivity and the humanistic burden resulting from reductions in HRQoL, PHN represents the source of a high socioeconomic burden in China and indicates the need for developing and initiating management strategies that can reduce this burden.
Limitations
This analysis should be interpreted in consideration of study limitations, some of which are inherent to the study design. Since the initial identification of patients with PHN was based on management by specialists (dermatologists, neurologists, and pain specialists), there may be systematic differences compared with those patients seen by general practitioners. This form of selection bias may have downstream effects that impact patient-reported burden and costs. Similarly, since study sites were in Tier 1/Tier 2 urban centers, external validity is a key limitation; such urban centers reflect only a small proportion of the population of China, and it is unclear to what extent the selected study sites represent all Tier 1/Tier 2 cities or generalize to Tier 3 cities and suburban/rural areas. Generalizability may have been further limited by the patient survey being conducted in a small sample at the primary data collection site. However, a post hoc analysis that compared survey completers with the rest of the population found only a small difference on one dimension of health care resource use (office visits), and therefore it remains unclear how different these groups may be. Another limitation is that the use of a survey questionnaire for collecting PROs may be susceptible to recall errors as well as social desirability bias. It is also possible that the burden on sleep may be overestimated, since available norms from the MOS-SS24 may not necessarily apply to the population of interest (ie, urban China) or, given the norms were generated several years ago, may have evolved. While costs were from tertiary hospitals, comprehensive cost data to enable comparisons with costs for other types of hospitals in China were not available. Similarly, ED costs in this analysis may not be generalizable, since they were based on physician consensus in the absence of an official source. In regard to costs, another potential limitation is that PHN-related direct medical costs were not estimated; only all-cause direct medical costs were estimated since these were considered relevant from a societal perspective. Last, since the definition of PHN used (ie pain persisting for ≥1 month following healing of the HZ rash) may be different from definitions used in other studies, comparisons with studies that defined PHN using other time periods for pain persisting after rash healing should be interpreted judiciously.
Conclusion
Adults aged ≥40 years who were living with PHN in a large urban center in China were characterized by a burden that was not limited to pain and pain interference with daily activities but also included poor sleep and low HRQoL. The presence and magnitude of this burden were generally consistent with other PHN populations. In addition, inclusion of a younger demographic, including individuals who were employed, showed that PHN results in work impairment, with broad economic implications. Frequent HRU with associated direct and OOP costs was indicative of the economic burden PHN has on patients and health care systems across China. Taken together, these results indicate that PHN is associated with a substantial patient and economic burden in China and suggests the need for more appropriate prevention and management.
Acknowledgments
This study was sponsored by Pfizer. The authors would also like to acknowledge Bruce Parsons, MD, and Yan-Qing Liu, MD, for their contributions during the conduct of this study. Medical writing support was provided by E. Jay Bienen, PhD, and was funded by Pfizer.
Abbreviation list
BPI, Brief Pain Inventory; ED, emergency department; EQ-5D-3L, 5-dimension 3-level EuroQol; HRU, healthcare resource utilization; HRQoL, health-related quality-of-life; HZ, herpes zoster; IMMPACT, Initiative on Methods, Measurement, and Pain Assessment in Clinical Trials; MOS-SS, Medical Outcomes Study Sleep Scale; NC, not calculated; NeP, neuropathic pain; OOP, out-of-pocket; PHN, postherpetic neuralgia; PRO, patient-reported outcomes; RMB, Chinese Yuan Renminbi; SNRIs, serotonin-norepinephrine reuptake inhibitors; SSRI, selective serotonin reuptake inhibitors; TCAs, tricyclic antidepressants; US$, US dollars; VAS, visual analogue scale; WPAI:SHP, Work Productivity and Activity Impairment Questionnaire for Specific Health Problems.
Data availability
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
Author contributions
Sheng-Yuan Yu, Bi-Fa Fan, Fei Yang, Yu-Xuan Chen, and Ruo-Yu Li were study investigators. All authors contributed to data analysis, drafting or revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
Marco DiBonaventura (an employee of Kantar Health at the time this study was conducted), Yu-Xuan Chen, Patrick Hlavacek, Markay Hopps, Margarita Udall, Alesia Sadosky, and Joseph C Cappelleri are employees of Pfizer and have stock options in Pfizer. Kristen Concialdi and Ian Kudel are employees of Kantar Health, who were paid consultants to Pfizer in relation to this study. The authors report no other conflicts of interest in this work.
References
- 1.Kawai K, Gebremeskel BG, Acosta CJ. Systematic review of incidence and complications of herpes zoster: towards a global perspective. BMJ Open. 2014;4(6):e004833. doi: 10.1136/bmjopen-2014-004833 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schmader K. Herpes zoster and postherpetic neuralgia in older adults. Clin Geriatr Med. 2007;23(3):615–632, vii-viii. doi: 10.1016/j.cger.2007.03.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dworkin RH, Gnann JW Jr., Oaklander AL, Raja SN, Schmader KE, Whitley RJ. Diagnosis and assessment of pain associated with herpes zoster and postherpetic neuralgia. J Pain. 2008;9(1 Suppl 1):S37–S44. doi: 10.1016/j.jpain.2007.10.008 [DOI] [PubMed] [Google Scholar]
- 4.International Association for the Study of Pain. IASP taxonomy. Available from: https://www.iasp-pain.org/Education/Content.aspx?ItemNumber=1698. Accessed September5, 2018.
- 5.Attal N, Cruccu G, Baron R, et al. EFNS guidelines on the pharmacological treatment of neuropathic pain: 2010 revision. Eur J Neurol. 2010;17(9):1113–1123. doi: 10.1111/j.1468-1331.2010.02999.x [DOI] [PubMed] [Google Scholar]
- 6.Dworkin RH, O’Connor AB, Audette J, et al. Recommendations for the pharmacological management of neuropathic pain: an overview and literature update. Mayo Clin Proc. 2010;85(3 Suppl):S3–S14. doi: 10.4065/mcp.2009.0649 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Argoff CE. Review of current guidelines on the care of postherpetic neuralgia. Postgrad Med. 2011;123(5):134–142. doi: 10.3810/pgm.2011.09.2469 [DOI] [PubMed] [Google Scholar]
- 8.Snedecor SJ, Sudharshan L, Cappelleri JC, et al. Systematic review and meta-analysis of pharmacological therapies for pain associated with postherpetic neuralgia and less common neuropathic conditions. Int J Clin Pract. 2014;68(7):900–918. doi: 10.1111/ijcp.12411 [DOI] [PubMed] [Google Scholar]
- 9.Zhu Q, Zheng H, Qu H, et al. Epidemiology of herpes zoster among adults aged 50 and above in Guangdong, China. Hum Vaccin Immunother. 2015;11(8):2113–2118. doi: 10.1080/21645515.2015.1016672 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Li Y, An Z, Yin D, et al. Disease burden due to herpes zoster among population aged >/=50 years old in China: a community based retrospective survey. PLoS One. 2016;11(4):e0152660. doi: 10.1371/journal.pone.0152660 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yang F, Yu S, Fan B, et al. The epidemiology of herpes zoster and postherpetic neuralgia in China: results from a non-interventional, cross-sectional study. Pain Ther. Epub 2019. Jun 19. doi: 10.1007/s40122-019-0127-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Johnson RW, Bouhassira D, Kassianos G, Leplege A, Schmader KE, Weinke T. The impact of herpes zoster and post-herpetic neuralgia on quality-of-life. BMC Med. 2010;8:37. doi: 10.1186/1741-7015-8-37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gater A, Uhart M, McCool R, Preaud E. The humanistic, economic and societal burden of herpes zoster in Europe: a critical review. BMC Public Health. 2015;15:193. doi: 10.1186/s12889-015-1514-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Drolet M, Levin MJ, Schmader KE, et al. Employment related productivity loss associated with herpes zoster and postherpetic neuralgia: a 6-month prospective study. Vaccine. 2012;30(12):2047–2050. doi: 10.1016/j.vaccine.2012.01.045 [DOI] [PubMed] [Google Scholar]
- 15.Meyers JL, Madhwani S, Rausch D, Candrilli SD, Krishnarajah G, Yan S. Analysis of real-world health care costs among immunocompetent patients aged 50 years or older with herpes zoster in the United States. Hum Vaccin Immunother. 2017;13(8):1861–1872. doi: 10.1080/21645515.2017.1324373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Matthews S, De Maria A, Passamonti M, et al. The economic burden and impact on quality of life of herpes zoster and postherpetic neuralgia in individuals aged 50 years or older in Italy. Open Forum Infect Dis. 2019;6(2):ofz007. doi: 10.1093/ofid/ofz125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schmidt-Ott R, Schutter U, Simon J, et al. Incidence and costs of herpes zoster and postherpetic neuralgia in German adults aged >/=50 years: A prospective study. J Infect. 2018;76(5):475–482. doi: 10.1016/j.jinf.2018.02.001 [DOI] [PubMed] [Google Scholar]
- 18.Rampakakis E, Pollock C, Vujacich C, et al. Economic burden of herpes zoster (“culebrilla”) in Latin America. Int J Infect Dis. 2017;58:22–26. doi: 10.1016/j.ijid.2017.02.021 [DOI] [PubMed] [Google Scholar]
- 19.Zostavax® (Zoster Vaccine Live) suspension for subcutaneous injection prescribing information. Merck & Co., Inc. Whitehouse Station, NJ; April, 2018. Available from: http://www.merck.com/product/usa/pi_circulars/z/zostavax/zostavax_pi2.pdf. Accessed June6, 2019.
- 20.Shingrix® (Zoster Vaccine Recombinant ASfIIpi). GlaxoSmithKline, Research Triangle Park, NC; October 2017. Available from: https://gsksource.com/pharma/content/dam/GlaxoSmithKline/US/en/Prescribing_Information/Shingrix/pdf/SHINGRIX.PDF. Accessed June6, 2019.
- 21.Centers for Disease Control and Prevention. Recommended immunization schedule for adults aged 19 years or older, United States; 2018. Available from: https://www.cdc.gov/vaccines/schedules/downloads/adult/adult-combined-schedule.pdf. Accessed June6, 2019.
- 22.Berger ML, Sox H, Willke RJ, et al. Good practices for real-world data studies of treatment and/or comparative effectiveness: recommendations from the joint ISPOR-ISPE special task force on real-world evidence in health care decision making. Value Health. 2017;20(8):1003–1008. doi: 10.1016/j.jval.2017.08.3019 [DOI] [PubMed] [Google Scholar]
- 23.Cleeland CS, Ryan KM. Pain assessment: global use of the Brief Pain Inventory. Ann Acad Med Singapore. 1994;23(2):129–138. [PubMed] [Google Scholar]
- 24.Hays R, Stewart A. Sleep measures In: Stewart A, Ware J, editors. Measuring Functioning and Well-Being: The Medical Outcomes Study Approach. Durham, NC: Duke University Press; 1992:235–259. [Google Scholar]
- 25.The EuroQol Group. EuroQol – a new facility for the measurement of health-related quality of life. The EuroQol Group. Health Policy. 1990;16(3):199–208. [DOI] [PubMed] [Google Scholar]
- 26.Reilly MC, Zbrozek AS, Dukes EM. The validity and reproducibility of a work productivity and activity impairment instrument. Pharmacoeconomics. 1993;4:353–365. doi: 10.2165/00019053-199304050-00006 [DOI] [PubMed] [Google Scholar]
- 27.Reilly MC. Work Productivity and Activity Impairment Questionnaire: Specific Health Problem V2.0 (WPAI:SHP). Available from: http://www.reillyassociates.net/WPAI_SHP.html. Accessed September5, 2018.
- 28.Dworkin RH, Turk DC, Farrar JT, et al. Core outcome measures for chronic pain clinical trials: IMMPACT recommendations. Pain. 2005;113:9–19. doi: 10.1016/j.pain.2004.09.012 [DOI] [PubMed] [Google Scholar]
- 29.Hays RD, Martin SA, Sesti AM, Spritzer KL. Psychometric properties of the Medical Outcomes Study Sleep. Sleep Med. 2005;6(1):41–44. doi: 10.1016/j.sleep.2004.07.006 [DOI] [PubMed] [Google Scholar]
- 30.Dolan P. Modeling valuations for EuroQol health states. Med Care. 1997;35(11):1095–1108. [DOI] [PubMed] [Google Scholar]
- 31.Chinese Ministry of Health. Available from: http://www.nhfpc.gov.cn/mohwsbwstjxxzx/s7967/201808/4f106ab85862461c8b0a3f24f86f7c37.shtml. Accessed September5, 2018.
- 32.Lofland JH, Pizzi L, Frick KD. A review of health-related workplace productivity loss instruments. Pharmacoeconomics. 2004;22(3):165–184. doi: 10.2165/00019053-200422030-00003 [DOI] [PubMed] [Google Scholar]
- 33.National Bureau of Statistics of China. China statistical yearbook; 2016; Available from: http://www.stats.gov.cn/tjsj/ndsj/2016/indexeh.htm. Accessed September5, 2018.
- 34.OANDA. Historical exchange rates. Available from: https://www.oanda.com/currency/average. Accessed September5, 2018.
- 35.The R project for statistical computing. Available from: https://www.r-project.org/. Accessed September5, 2018.
- 36.van Seventer R, Sadosky A, Lucero M, Dukes E. A cross-sectional survey of health state impairment and treatment patterns in patients with postherpetic neuralgia (PHN). Age Ageing. 2006;35(2):132–137. doi: 10.1093/ageing/afj048 [DOI] [PubMed] [Google Scholar]
- 37.Drolet M, Brisson M, Schmader KE, et al. The impact of herpes zoster and postherpetic neuralgia on health-related quality of life: a prospective study. Can Med Assoc J. 2010;182(16):1731–1736. doi: 10.1503/cmaj.091711 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Serpell M, Gater A, Carroll S, Abetz-Webb L, Mannan A, Johnson R. Burden of post-herpetic neuralgia in a sample of UK residents aged 50 years or older: findings from the Zoster Quality of Life (ZQOL) study. Health Qual Life Outcomes. 2014;12:92. doi: 10.1186/1477-7525-12-92 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mizukami A, Sato K, Adachi K, et al. Impact of herpes zoster and post-herpetic neuralgia on health-related quality of life in Japanese adults aged 60 years or older: results from a prospective, observational cohort study. Clin Drug Investig. 2018;38(1):29–37. doi: 10.1007/s40261-017-0581-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lee DH, Park JE, Yoon DM, Yoon KB, Kim K, Kim SH. Factors associated with increased risk for clinical insomnia in patients with postherpetic neuralgia: a retrospective cross-sectional study. Pain Med. 2016;17(10):1917–1922. doi: 10.1093/pm/pnw066 [DOI] [PubMed] [Google Scholar]
- 41.Smith MT, Haythornthwaite JA. How do sleep disturbance and chronic pain inter-relate? Insights from the longitudinal and cognitive-behavioral clinical trials literature. Sleep Med Rev. 2004;8(2):119–132. doi: 10.1016/S1087-0792(03)00044-3 [DOI] [PubMed] [Google Scholar]
- 42.Edwards RR, Almeida DM, Klick B, Haythornthwaite JA, Smith MT. Duration of sleep contributes to next-day pain report in the general population. Pain. 2008;137(1):202–207. doi: 10.1016/j.pain.2008.01.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Finan PH, Goodin BR, Smith MT. The association of sleep and pain: an update and a path forward. J Pain. 2014;14(12):1539–1552. doi: 10.1016/j.jpain.2013.08.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Szende A, Janssen B. Population norms for the EQ-5D. In: Cabases JM, Szende A, Janssen B, editors. Self-reported population health: an international perspective based on EQ-5D Dordrecht: Springer; 2014:19–30. [PubMed] [Google Scholar]
- 45.Coretti S, Ruggeri M, McNamee P. The minimum clinically important difference for EQ-5D index: a critical review. Expert Rev Pharmacoecon Outcomes Res. 2014;14(2):221–233. doi: 10.1586/14737167.2014.894462 [DOI] [PubMed] [Google Scholar]
- 46.Doth AH, Hansson PT, Jensen MP, Taylor RS. The burden of neuropathic pain: a systematic review and meta-analysis of health utilities. Pain. 2010;149(2):338–344. doi: 10.1016/j.pain.2010.02.034 [DOI] [PubMed] [Google Scholar]
- 47.Pickard AS, Neary MP, Cella D. Estimation of minimally important differences in EQ-5D utility and VAS scores in cancer. Health Qual Life Outcomes. 2007;5:70. doi: 10.1186/1477-7525-5-70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Coteur G, Feagan B, Keininger DL, Kosinski M. Evaluation of the meaningfulness of health-related quality of life improvements as assessed by the SF-36 and the EQ-5D VAS in patients with active Crohn’s disease. Aliment Pharmacol Ther. 2009;29(9):1032–1041. doi: 10.1111/j.1365-2036.2009.03966.x [DOI] [PubMed] [Google Scholar]
- 49.Zanini A, Aiello M, Adamo D, et al. Estimation of minimal clinically important difference in EQ-5D visual analog scale score after pulmonary rehabilitation in subjects with COPD. Respir Care. 2015;60(1):88–95. doi: 10.4187/respcare.03272 [DOI] [PubMed] [Google Scholar]
- 50.Feng Q, Yeung W-J-J, Wang Z, Zeng Y. Age of retirement and human capital in an aging China, 2015–2050. Eur J Popul. 2018;35(1):29–62. doi: 10.1007/s10680-018-9467-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Stewart WF, Ricci JA, Chee E, Morganstein D, Lipton R. Lost productive time and cost due to common pain conditions in the US workforce. JAMA. 2003;290(18):2443–2454. doi: 10.1001/jama.290.18.2443 [DOI] [PubMed] [Google Scholar]
- 52.Langley PC, Van Litsenburg C, Cappelleri JC, Carroll D. The burden associated with neuropathic pain in Western Europe. J Med Econ. 2013;16(1):85–95. doi: 10.3111/13696998.2012.729548 [DOI] [PubMed] [Google Scholar]
- 53.Dubinsky RM, Kabbani H, El-Chami Z, Boutwell C, Ali H. Practice parameter: treatment of postherpetic neuralgia. An evidence-based report of the Quality Standards Subcommittee of the American Academy of Neurology . Neurology. 2004;63:959–965. doi: 10.1212/01.wnl.0000140708.62856.72 [DOI] [PubMed] [Google Scholar]
- 54.Gialloreti LE, Merito M, Pezzotti P, et al. Epidemiology and economic burden of herpes zoster and post-herpetic neuralgia in Italy: a retrospective, population-based study. BMC Infect Dis. 2010;10:230. doi: 10.1186/1471-2334-10-230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Nilsson J, Cassel T, Lindquist L. Burden of herpes zoster and post-herpetic neuralgia in Sweden. BMC Infect Dis. 2015;15:215. doi: 10.1186/s12879-015-0951-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Cheong C, Lee TJ. Prevalence and healthcare utilization of herpes zoster and postherpetic neuralgia in South Korea: disparity among patients with different immune statuses. Epidemiol Health. 2014;36:e2014012. doi: 10.4178/epih/e2014012 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.