Abstract
BACKGROUND:
Recently updated American College of Cardiology/ American Heart Association (ACC/AHA) guidelines redefine blood pressure categories as Stage 1 hypertension (systolic 130–139mmHg or diastolic 80–89mmHg), Elevated (systolic 120–129mmHg and diastolic <80mm) and Normal (<120/<80 mmHg), but their relevance to an obstetric population is uncertain.
OBJECTIVE:
We sought to evaluate the risk of gestational hypertension or preeclampsia based on early pregnancy blood pressure category and trajectory.
STUDY DESIGN:
We utilized data from the Nulliparous Pregnancy Outcomes Study: Monitoring Mothers-to-Be (nuMoM2b) cohort, a prospective observational study of nulliparous women with singleton pregnancies conducted at eight clinical sites between 2010–2014. Women included in this analysis had no known history of pre-pregnancy hypertension (blood pressure ≥140/90 mmHg) or diabetes. We compared the frequency of hypertensive disorders of pregnancy, including preeclampsia and gestational hypertension among women based on ACC/AHA blood pressure category at a first trimester study visit and blood pressure trajectory between study visits in the first and second trimesters. Blood pressure trajectories were categorized based on blood pressure difference between visit 1 and 2 as stable (<5mmHg difference), upward (≥5mmHg) or downward (≤−5mmHg). Associations of blood pressure category and trajectory with preeclampsia and gestational hypertension were assessed via univariate analysis and multinomial logistic regression analysis with co-variates identified a priori.
RESULTS:
8,899 women were included in the analysis. Study visit 1 occurred at a mean gestational age of 11.6 ± 1.5 weeks and study visit 2 at a mean GA of 19.0 ± 1.6 weeks. First trimester blood pressure category was significantly associated with both preeclampsia and gestational hypertension, with increasing blood pressure category associated with a higher risk of all hypertensive disorders of pregnancy. Elevated blood pressure was associated with an aRR 1.54 (95%CI 1.18–2.02) and Stage 1 hypertension was associated with aRR 2.16 (95%CI 1.31–3.57) of any hypertensive disorder of pregnancy. Stage 1 hypertension was associated with the highest risk of preeclampsia with severe features with an aRR 2.48 (95%CI 1.38–8.74). Both systolic and diastolic blood pressure trajectories were also significantly associated with the risk of hypertensive disorders of pregnancy independent of blood pressure category (p<0.001). Woman with a blood pressure categorized as Normal and with an upward systolic trajectory had a 41% increased risk of any hypertensive disorder of pregnancy (aRR 1.41; 95%CI 1.20–1.65) compared to women with a downward systolic trajectory.
CONCLUSIONS:
In nulliparous women, blood pressure category and trajectory in early pregnancy are independently associated with risk of preeclampsia and gestational hypertension. Our study demonstrates that blood pressure categories with lower thresholds than those traditionally used to identify individuals as hypertensive may identify more women at risk for preeclampsia and gestational hypertension.
Keywords: Stage 1 hypertension, mild hypertension, preeclampsia, gestational hypertension, BP trajectory, chronic hypertension, hypertensive disorder, pregnancy, American College of Cardiology, American Heart Association, guideline
CONDENSATION:
In non-hypertensive, non-diabetic nulliparous women, increasing blood pressure in early pregnancy is associated with an increased risk of gestational hypertension and preeclampsia.
INTRODUCTION
The American Heart Association (AHA) and the American College of Cardiology (ACC) Task Force on Clinical Practice Guidelines revised their recommendations for diagnosis of hypertension in adults recently.1 Citing the evidence that incremental increases in blood pressure impact the risk of cardiovascular disease (CVD) and death, blood pressure (BP) categories have been redefined as Stage 1 hypertension (systolic 130–139mmHg or diastolic 80–89mmHg), Elevated BP (systolic 120–129mmHg and diastolic <80mm) and Normal BP (<120/<80 mmHg). The changes to the guidelines were made based on prior observational studies that have demonstrated graded associations between both higher systolic and diastolic blood pressure and cardiovascular disease risk. In one large meta-analysis including over 60 prospective studies, the risk of cardiovascular disease increased in a log-linear fashion with a 20 mmHg higher systolic blood pressure and 10 mm Hg higher diastolic blood pressure each associated with a doubling in the risk of death from stroke, heart disease, or other vascular disease.2 While the guidelines outline the association of graded blood pressure increases with health outcomes in non-pregnant adults, their relevance to an obstetric population is uncertain.
Women entering pregnancy with pre-existing hypertension have increased pregnancy-related morbidity, including an increased risk of preeclampsia, preterm delivery, small for gestational age (SGA) infants, placental abruption and stillbirth.3,4 However, the relationship between the new hypertension categories and risk of hypertensive disorders of pregnancy (HDP), including gestational hypertension and preeclampsia, is not well characterized. While there have been promising results demonstrated by the use of biomarkers, mean arterial blood pressure and uterine artery Dopplers in screening for risk of preterm preeclampsia, these modalities are more expensive and have not been well-integrated into clinical practice in the United States.5 We sought to evaluate whether blood pressure trajectories in early pregnancy are associated with hypertensive disorders of pregnancy given that prior studies have had inconsistent results.6,7
We have previously demonstrated an increased risk of hypertensive disorders of pregnancy associated with Stage 1 hypertension in analyses of the Maternal Fetal Medicine Unit Network high and low-risk aspirin trials.8,9 However, the demographic characteristics of pregnant women and pregnancy management have changed since the 1990s, such as an increasing maternal age and an increasing prevalence of obesity, and generalizability of these results to contemporary practice remain uncertain. The objective of this study was to evaluate the risk of hypertensive disorders of pregnancy based on early pregnancy blood pressure category and trajectory in a contemporary and diverse cohort.
MATERIALS AND METHODS
This is an analysis of data from the Nulliparous Pregnancy Outcomes Study: Monitoring Mothers-to-Be (nuMoM2b), a prospective cohort study designed to identify factors that contribute to preterm birth and other adverse pregnancy outcomes.10 This study enrolled 10,038 nulliparous women with singleton pregnancies from 8 clinical centers in the United States (Case Western Reserve University; Columbia University; Indiana University; University of Pittsburgh; Northwestern University; University of California at Irvine; University of Pennsylvania; and University of Utah). IRB approval was obtained from each clinical center. In brief, women were eligible for enrollment if they had a viable singleton gestation, had no previous pregnancy that lasted more than 20 weeks of gestation, and were between 6 0/7 weeks of gestation and 13 6/7 weeks of gestation at enrollment (first study visit). Gestational dating was based on a documented ultrasound crown-rump length measurement by a certified nuMoM2b sonographer at the first study visit. Participants were evaluated at 3 study visits during pregnancy and again at delivery. Exclusion criteria were maternal age younger than 13 years, history of three or more spontaneous abortions, current pregnancy complicated by a suspected fatal fetal malformation, known fetal aneuploidy, assisted reproduction with a donor oocyte, multifetal reduction, or plans to terminate the pregnancy. All local institutional review boards approved the study protocol, and participants provided written informed consent prior to enrollment.
Blood pressures were taken by trained study staff at each visit in a standardized fashion using an aneroid sphygmomanometer.10,11 A common protocol and manual of operations were utilized for all aspects of the study at all sites with trained and credentialed study personnel performing all study procedures. Responsibility for training study staff on blood pressure measurement rested with the site Principal Investigator and Study Coordinator. Multiple cuff sizes were available to ensure appropriate cuff size based on arm circumference. Briefly, patients were allowed to rest for at least 10 minutes while seated comfortably in a quiet location before the BP measurement. The circumference of the right arm was measured in the following fashion: the participant stands with the right arm hanging and bending the elbow such that the forearm is parallel to the floor, the arm length is measured from the acromion to the olecranon using a standard tape measure to identify the midpoint on the dorsal surface of the arm. The arm circumference was then measured at this midpoint and the appropriate cuff size was selected. Participants were then seated in a chair with arm support or a chair and table providing for a comfortable resting posture of the arm with the cubital fossa at the level of the 4th intercostal space at heart level. Blood pressure was then measured three times at each visit with the participant seated with legs uncrossed. For the current analysis, participants were classified according to blood pressure measurement at enrollment (first study visit). Women with a systolic blood pressure <120 mmHg and a diastolic blood pressure <80mmHg were classified as Normal, women with a systolic blood pressure of 120 to 129 mmHg and diastolic blood pressure <80mmHg were classified as Elevated and women with a systolic blood pressure 130 to 139 mmHg or diastolic blood pressure of 80 to 89 mmHg were classified as Stage 1 hypertension.1 BP trajectories were categorized based on differences in systolic, diastolic or mean arterial pressure between visit 1 and 2 as stable (<5mmHg difference), upward (≥5mmHg) or downward (≤−5mmHg). Mean arterial pressure was defined as the sum of the diastolic blood pressure and one third of the pulse pressure (systolic blood pressure – diastolic blood pressure).
Our primary outcome was hypertensive disorders of pregnancy (HDP), including preeclampsia/eclampsia and gestational hypertension. Preeclampsia diagnoses were adjudicated from medical record abstraction, performed by certified research personnel. Definitions for preeclampsia and gestational hypertension in nuMom2b have been previously published.12 Briefly, hypertensive disorders of pregnancy (HDP) included both gestational hypertension and preeclampsia, and were diagnosed according to the American College of Obstetricians and Gynecologists guidelines; preeclampsia included preeclampsia without severe features, preeclampsia with severe features and eclampsia.13 Gestational hypertension was defined as new-onset hypertension ≥140 mmHg systolic or ≥90 mmHg diastolic on 2 occasions at least 4 hours apart above 20 weeks 0 days gestation. Preeclampsia was defined as new-onset hypertension ≥140 mmHg systolic or ≥90 mmHg diastolicon 2 occasions at least 4 hours apart above 20 weeks 0 days gestation and proteinuria (300mg or more per 24 hour urine collection or protein/creatinine ratio of 0.3 mg/dL or more). In the absence of proteinuria, new-onset hypertension with the new onset of any of the following: severe hypertension (≥160 mmHg systolic or ≥110 mmHg diastolic), thrombocytopenia (platelet count less than 100,000 ×109/ L), renal insufficiency (serum creatinine concentrations greater than 1.1 mg/dL or doubling of serum creatinine concentration), impaired liver function (elevated blood concentrations of liver transaminases to twice normal concentration), pulmonary edema or new-onset headache unresponsive to medication. Preeclampsia with severe features was defined as either new-onset severe hypertension or new-onset hypertension with evidence of end-organ dysfunction as outlined above or eclampsia. Spontaneous preterm birth was defined as a delivery between 20 weeks 0 days to 36 weeks 6 days secondary to preterm labor or preterm premature rupture of membranes. Quality control checks via re-abstraction were performed by the site principal investigator on a random selection of charts with and without complications and any discrepancies resolved. There were no discrepancies between the abstractions in terms of HDP diagnoses. Analysis was restricted to pregnancies carried 20 or more weeks of gestation. Women with pre-existing diabetes or chronic hypertension (either a pre-existing diagnosis or with intake BP ≥140/90mmHg), also identified via chart abstraction of the medical record (n = 423), were excluded from this analysis. Women with missing blood pressure values or pregnancy outcome data were also excluded (n=716).
Statistical analysis was conducted using STATA software, version 14 (StataCorp, College Station, TX). Continuous variables were compared using Student t-tests and Wilcoxon-Mann Whitney tests as appropriate. Categorical variables were analyzed using Chi-square or Fisher’s exact where appropriate. Multivariable analysis included multinomial logistic regression to evaluate the independent association between enrollment BP category or trajectory and hypertensive disorders of pregnancy (gestational hypertension, preeclampsia without severe features, preeclampsia with severe features). Adjustment covariates were chosen a priori based on prior studies and included age, pre-pregnancy body mass index (BMI), self-reported race and aspirin use. As the effect of blood pressure category depended on pre-pregnancy BMI, we included an interaction term in our multivariable model. We also present our results stratified by pre-pregnancy BMI (Table 4). Results are presented as adjusted risk ratios with corresponding 95% confidence intervals, and a p-value <0.05 was considered statistically significant. No adjustments were made for multiple comparisons as HDP was our a priori primary endpoint.
Table 4.
Risk of any hypertensive disorder of pregnancy (preeclampsia or gestational hypertension) by blood pressure category at study visit 1 stratified by pre-pregnancy body mass index (BMI).
| N=7,034 n(%) |
N=975 n(%) |
N=890 n(%) |
|
|---|---|---|---|
| (BMI <19.5 kg/m2) | |||
| (BMI 19.5–24.9 kg/m2) | |||
| (BMI 25–29.9 kg/m2) | |||
| (BMI ≥30 kg/m2) |
aRR: adjusted relative risk; adjusted for maternal age, race, aspirin use
RESULTS
The nuMoM2b cohort included 10,038 women. Women with pre-existing diabetes or a pre-pregnancy diagnosis of hypertension (n=423) and women with missing BP or clinical outcome data were excluded (n=716) and 8,899 women were included in our analysis. Of these women, 7,034 (79.0%) had Normal BP measured at the time of enrollment, 975 (11.0%) had Elevated BP and 890 (10.0%) had Stage 1 hypertension (HTN). Women with Stage 1 HTN were more likely to be older, non-Hispanic black, and have a higher BMI. Among our cohort, 794 (9.0%) of women reported using low-dose aspirin during pregnancy (Table 1).
Table 1.
Demographics by blood pressure category at study visit 1.
| N=7,034 n(%) |
N=975 n(%) |
N=890 n(%) |
||
|---|---|---|---|---|
| Age (years)* | 27.0 ± 5.6 | 26.8 ± 5.5 | 27.4 ± 5.6 | 0.03 |
| Other | 342 (4.9%) | 61 (6.3%) | 42 (9.5%) | |
| Pre-pregnancy Body Mass Index (kg/m2)* | 25.0 + 5.1 | 28.7 ± 6.8 | 30.8 ± 7.5 | <0.001 |
| Gestational age at enrollment (weeks)* | 11.6 ± 1.5 | 11.5 ± 1.6 | 11.6 + 1.5 | 0.9 |
| Enrollment Systolic blood pressure (mmHg)* | 105 ± 8 | 122 ± 3 | 122 ± 9 | <0.001 |
| Enrollment Diastolic blood pressure (mmHg)* | 65 ± 7 | 70 ± 6 | 80 ± 5 | <0.001 |
| Gestational age at Study Visit 2 (weeks)* | 19.0 ± 1.6 | 19.1 ± 1.6 | 19.1 ± 1.5 | 0.9 |
| Aspirin Use | 642 (9.2%) | 74 (7.7%) | 78 (8.8%) | 0.3 |
mean ± standard deviation
Stage 1 HTN was associated with earlier gestational age at delivery (p=0.02) and lower birthweight (p<0.001) as well as an increased risk of indicated preterm birth. 5.3% of women with Stage 1 HTN had an indicated preterm birth, compared to 2.1% of women with BP categorized as Normal (p<0.001). Gestational diabetes was more prevalent among women with Stage 1 HTN (p<0.001), 6.2% of women compared to 3.5% of women in the Normal BP category (Table 2).
Table 2.
Pregnancy outcomes by blood pressure category at study visit 1
| N=7,034 n(%) |
N=975 n(%) |
N=890 n(%) |
||
|---|---|---|---|---|
| Gestational Diabetes | 248 (3.5%) | 53 (5.4%) | 55 (6.2%) | <0.001 |
| Gestational age at delivery (weeks)* | 38.9 ± 2.1 | 38.7 ± 2.5 | 38.6 ± 2.5 | 0.02 |
| Indicated preterm birth | 148 (2.1%) | 36 (3.7%) | 47 (5.3%) | <0.001 |
| Cesarean section | 1,784 (25.4%) | 295 (30.3%) | 309 (34.7%) | |
| Birthweight (grams)* | 3279 ± 548 | 3269 ± 598 | 3258 ± 611 | <0.001 |
mean ± standard deviation
As shown in Table 3, in our cohort 2,028 (22.8%) women developed any HDP, 1,292 (14.5%) women developed gestational hypertension, and 735 (8.3%) women developed preeclampsia, 365 (4.1%) of whom had severe features. First-trimester BP category was significantly associated with HDP. The prevalence of any HDP among women with Elevated BP was 30.3% (aRR 1.54; 95%CI 1.18–2.02) and among women with Stage 1 HTN was 37.8% (aRR 2.16; 95%CI 1.31–3.57).
Table 3.
Hypertensive disorders of pregnancy outcomes by blood pressure category at study visit 1.
| N=7,034 n(%) |
N=975 n(%) |
N=890 n(%) |
|
|---|---|---|---|
| Ref | aRR 1.54 (95% CI 1.18–2.02) | aRR 2.16 (95% CI 1.31–3.57) | |
| All Preeclampsia | 496 (7.1%) | 99 (10.2%) | 141 (15.8%) |
| Ref | aRR 1.43 (95% CI 0.83–2.47) | aRR 2.39 (95% CI 0.88–6.49) | |
| Ref | aRR 1.56 (95% CI 0.93–2.64) | aRR 3.48 (95% CI 1.38–8.74) | |
| Ref | aRR 1.56 (95% CI 1.14–2.14) | aRR 1.80 (95% CI 0.99–3.28) |
aRR: adjusted relative risk; adjusted for maternal age, pre-pregnancy body mass index, interaction of body mass index and blood pressure, race
The prevalence of both preeclampsia and gestational HTN was increased among women with increasing BP category and persisted after adjustment for age, pre-pregnancy BMI, the interaction of BMI and first-trimester blood pressure, race and aspirin use (Table 2). The prevalence of gestational hypertension among women with Elevated BP was 20.1% (aRR 1.56; 95%CI 1.14–2.14) and among women with Stage 1 HTN was 21.9% (aRR 1.80; 95%CI 0.99–3.28). The prevalence of preeclampsia among women with Elevated BP was 10.2% (aRR 1.50; 95%CI 1.01–2.22) and among women with Stage 1 HTN was 15.8% (aRR 2.92; 95%CI 1.44–5.95), compared to women with a BP in the Normal category in the first trimester, who had a preeclampsia prevalence of 7.1%. This increased risk was seen with both preeclampsia with and without severe features. Stage 1 hypertension was associated with the highest risk of preeclampsia with severe features, with a prevalence of 9.0% (aRR 3.48; 95%CI 1.38–8.74), compared to 3.4% among women in the Normal BP category. As the effect of blood pressure category depended on pre-pregnancy BMI, we also performed a stratified analysis examining the risk of hypertensive disorders of pregnancy based on blood pressure category by pre-pregnancy BMI. As shown in Table 4, within each BMI category, the risk of hypertensive disorders of pregnancy was increased among women with increasing BP category. In sensitivity analyses, we attempted to address the impact of low-dose aspirin prophylaxis on the risk of hypertensive disorders. There were 794 women (9.0%) on low-dose aspirin during pregnancy. The use of low-dose aspirin was not associated with a reduction in risk of hypertensive disorders in our cohort.
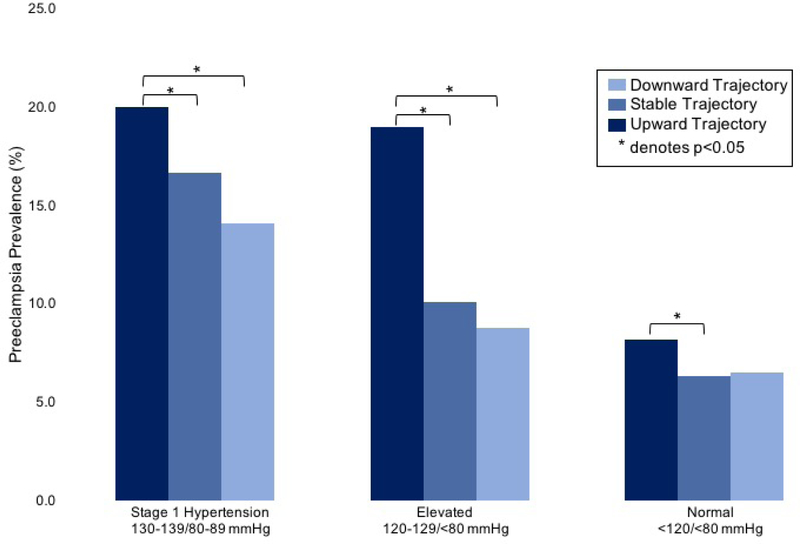
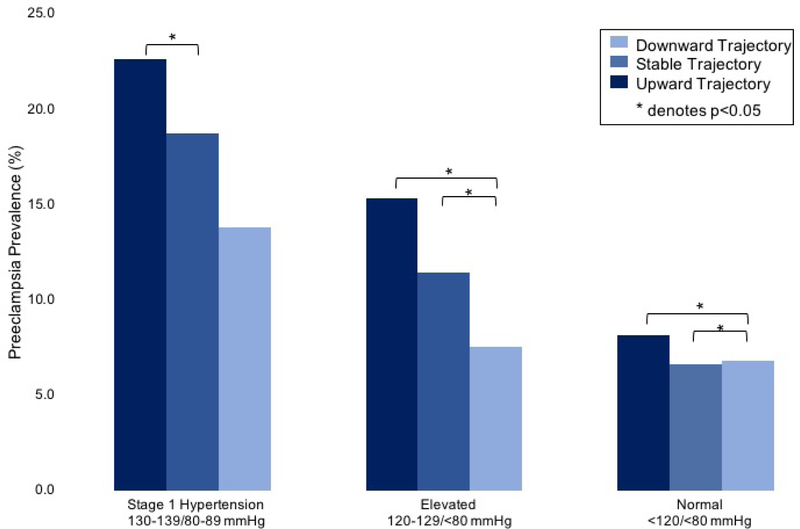
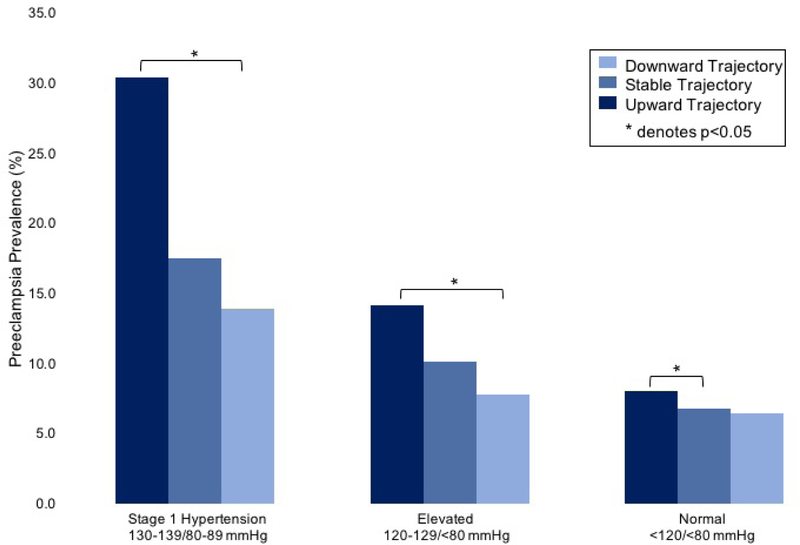
Both systolic and diastolic BP trajectories were significantly associated with HDP risk (p<0.001), with an increased prevalence associated with an upward trajectory and a decreased prevalence associated with a downward trajectory (Figures 1–3), which was independent of first trimester BP category. Among women with a first trimester BP categorized as Normal, an upward systolic trajectory was associated with a 41% increased risk of any HDP (aRR 1.41; 95%CI 1.21–1.65); with a 49% increased risk of gestational hypertension (aRR 1.49; 95% CI 1.23–1.80) and a 30% increased risk of preeclampsia (aRR 1.30; 95%CI 1.02–1.65) compared to women with a downward systolic trajectory. Similarly, an upward diastolic trajectory was associated with an adjusted RR 1.23 (95%CI 1.05–1.45) of any HDP compared to women with a downward diastolic trajectory.
Figure 1.
Preeclampsia prevalence based on blood pressure category at study visit 1 and systolic trajectory.
Figure 3.
Preeclampsia prevalence based on blood pressure category at study visit 1 and mean arterial pressure trajectory.
COMMENT
Principal Findings
Elevated blood pressure and Stage 1 hypertension categories recently recommended by the American College of Cardiology and American Heart Association identify nulliparous women with significant increased risk for gestational hypertension or preeclampsia. In addition, we found that both systolic and diastolic upward blood pressure trajectory (≥ 5 mmHg difference between visit 1 and visit 2) were also significantly associated with gestational hypertension or preeclampsia independent of blood pressure category.
Results
These findings may identify otherwise “low-risk” women at increased risk for HDP. Considering that the prevalence of pre-gestational hypertension has been projected to double in women newly-designated as having hypertension based on the new ACC/AHA guidelines, understanding risk in this group is particularly relevant for clinicians.14,15 In our cohort, 10.0% of women were categorized as Stage 1 HTN at the first prenatal visit. Further, BP trajectory in the first and early second trimester may provide additional insight into HDP risk and allow for a low-cost office screening tool. While recent studies, such as the ASPRE trial have developed detailed methods for preeclampsia prediction and identification of high-risk women for aspirin prophylaxis utilizing methods such as uterine artery Dopplers and serum biomarkers, our results suggest that BP trajectory may be particularly useful for this purpose and might be beneficial in such a model.5 For example, a woman entering pregnancy with a BP of 120/70 mmHg would be classified as having “Elevated” BP by the ACC/AHA categories; however, most clinicians would not be overly concerned with such a measurement at an initial prenatal visit. Our findings suggest that at a subsequent prenatal visit, the patient’s preeclampsia risk is substantially changed beyond her initial category risk based on the trajectory of BP. Based on our data, an upward trajectory of systolic BP increases the risk of preeclampsia from 10.2% to 19.0%, whereas a downward trajectory decreases the risk to 8.8%. Prior studies have demonstrated a potential benefit of low-dose aspirin in women with Stage 1 HTN. However, these were secondary analyses performed in non-contemporary cohorts and such treatment warrants further investigation prior to consideration for implementation into clinical practice.8,9
Clinical and Research Implications
Importantly, the new ACC/AHA guidelines also suggest benefit from initiation of treatment in nonpregnant adults with Stage 1 hypertension and additional risk factors for cardiovascular disease.1 A foreseeable consequence of this change in guidelines will be an increasing number of young women entering pregnancy with a diagnosis of Stage 1 hypertension, many of whom may be on anti-hypertensive agents.14 While multiple trials, including the currently ongoing Chronic Hypertension and Pregnancy study (CHAP study; ) are evaluating the impact of “tight” versus less-tight control of chronic hypertension in pregnancy, few studies have addressed the clinical and pregnancy outcomes of women based on the new ACC/AHA BP guidelines. Recently published ACOG clinical practice guidelines recommend that women with Stage 1 hypertension should be managed similar to those with chronic hypertension in pregnancy in regards to antenatal surveillance, while recognizing the uncertainty regarding benefit.18 Further study is needed to describe pregnancy outcomes in women entering pregnancy with a known diagnosis of Stage 1 hypertension.
The ACOG guidelines note the lack of clarity on the management of women with previously undiagnosed chronic hypertension with BPs in the Stage 1 HTN range prior to 20 weeks gestation. However, the guidelines suggest that while BPs in this range would not require initiation of anti-hypertensive medication, a conservative approach with a higher degree of observation may be warranted. Indeed, prior studies have evaluated the impact of “prehypertension” on pregnancy outcomes and have found that it is associated with an increased risk of both maternal and neonatal complications.16,17 A small cohort study found that prehypertension in the first half of pregnancy was associated with earlier delivery, and more pregnancy-related hypertension as well as a composite maternal adverse outcomes and concluded that pre-hypertension in the first half of pregnancy increases the risk of adverse outcomes. Our findings similarly demonstrate that women with Stage 1 HTN are at increased risk of HDP. However, based on the nature of this study, we cannot delineate the effects of increased surveillance and preventative strategies in women with Stage 1 HTN. The most rigorous manner in which to establish the impact of such recommendations would be through randomized controlled trials.
Strengths and Limitations
This study is limited by our use of BP measurements during pregnancy for BP categorization. While pre-pregnancy BPs would be ideal, it is well established that women do not reliably seek care outside of pregnancy and often the only BP data available to obstetricians is that measured at the first prenatal visit, making our data clinically relevant. In the United States, pre-conception care visits occur in 18–45% of reproductive-age women. Thus, early pregnancy BPs may be all that is available for the obstetrician.19 This study is also limited by our use of a single BP within each study visit. While the standardized measurement of BP by study staff is a strength of our study, classification of BP should be based on more than one measure, per the ACC/AHA guidelines.1 Further, our study is based on research BPs and not those measured clinically. It is possible that clinical BPs may overestimate the number of women with Elevated or Stage 1 HTN, which may change our findings. Future study is needed to address this concern.
Conclusions
Given the recently revised ACC/AHA definitions, there is expected to be an increasing prevalence of women categorized as Stage 1 HTN.1,20 Our study demonstrates that BP categories with lower thresholds than those traditionally used to identify individuals as hypertensive, may identify more women at risk for HDP. Stage 1 hypertension in the first trimester is associated with a more than two-fold increased risk of hypertensive disorders of pregnancy. Further study to identify the efficacy of additional surveillance and potential risk-reducing interventions, such as low-dose aspirin, is needed in this population.
Figure 2.
Preeclampsia prevalence based on blood pressure category at study visit 1 and diastolic trajectory.
AJOG AT A GLANCE:
Why was this study conducted?
Recently updated American College of Cardiology/ American Heart Association guidelines redefine blood pressure categories and lower threshold for defining chronic hypertension.
Relevance of these new guidelines to an obstetric population is uncertain.
What are the key findings?
First trimester blood pressure category was associated with the development of a hypertensive disorder of pregnancy (gestational hypertension or preeclampsia).
Stage 1 hypertension was associated with the highest risk of preeclampsia with severe features with an aRR 2.48 (95%CI 1.38–8.74).
Blood pressure trajectory also was significantly associated with hypertensive disorders of pregnancy.
What does this study add to what is already known?
This study evaluates the risk of gestational hypertension and preeclampsia associated with first trimester blood pressure category and blood pressure trajectory.
This study provides evidence of an association between gestational hypertension and preeclampsia and the new ACC/AHA hypertension guidelines.
FUNDING SOURCE:
This work was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development: U10 HD063036, RTI International; U10 HD063072, Case Western Reserve University; U10 HD063047, Columbia University; U10 HD063037, Indiana University; U10 HD063041, University of Pittsburgh; U10 HD063020, Northwestern University; U10 HD063046, University of California, Irvine; U10 HD063048, University of Pennsylvania; and U10 HD063053, University of Utah.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The authors report no conflicts of interest.
This work will be presented in poster format at the Society for Maternal Fetal Medicine’s 39th Annual Pregnancy Meeting, February 13–16, 2019 in Las Vegas, NV.
REFERENCES
- 1.Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71(6):e13–e115. doi: 10.1161/HYP.0000000000000065. [DOI] [PubMed] [Google Scholar]
- 2.Lewington S, Clarke R, Qizilbash N, Peto R, Collins R, Prospective Studies Collaboration. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet (London, England). 2002;360(9349):1903–1913. http://www.ncbi.nlm.nih.gov/pubmed/12493255. Accessed June 4, 2019 [DOI] [PubMed] [Google Scholar]
- 3.Ankumah N-A, Cantu J, Jauk V, et al. Risk of adverse pregnancy outcomes in women with mild chronic hypertension before 20 weeks of gestation. Obstet Gynecol. 2014;123(5):966–972. doi: 10.1097/AOG.0000000000000205. [DOI] [PubMed] [Google Scholar]
- 4.Bramham K, Parnell B, Nelson-Piercy C, Seed PT, Poston L, Chappell LC. Chronic hypertension and pregnancy outcomes: systematic review and meta-analysis. BMJ. 2014;348(apr15 7):g2301–g2301. doi: 10.1136/bmj.g2301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rolnik DL, Wright D, Poon LC, et al. Aspirin versus Placebo in Pregnancies at High Risk for Preterm Preeclampsia. N Engl J Med. 2017;377(7):613–622. doi: 10.1056/NEJMoa1704559. [DOI] [PubMed] [Google Scholar]
- 6.Hermida RC, Ayala DE, Iglesias M. Predictable blood pressure variability in healthy and complicated pregnancies. Hypertens (Dallas, Tex 1979). 2001;38(3 Pt 2):736–741. http://www.ncbi.nlm.nih.gov/pubmed/11566967. Accessed January 2, 2019 [DOI] [PubMed] [Google Scholar]
- 7.Ayala DE, Hermida RC, Mojón A, et al. Blood pressure variability during gestation in healthy and complicated pregnancies. Hypertens (Dallas, Tex 1979). 1997;30(3 Pt 2):611–618. http://www.ncbi.nlm.nih.gov/pubmed/9322990. Accessed January 2, 2019 [DOI] [PubMed] [Google Scholar]
- 8.Hauspurg A, Sutton EF, Catov JM, Caritis SN. Aspirin Effect on Adverse Pregnancy Outcomes Associated With Stage 1 Hypertension in a High-Risk Cohort. Hypertens (Dallas, Tex 1979). 2018;72(1):202–207. doi: 10.1161/HYPERTENSIONAHA.118.11196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sutton EF, Hauspurg A, Caritis SN, Powers RW, Catov JM. Maternal Outcomes Associated With Lower Range Stage 1 Hypertension. Obstet Gynecol. 2018;132(4):843–849. doi: 10.1097/AOG.0000000000002870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Haas DM, Parker CB, Wing DA, et al. A description of the methods of the Nulliparous Pregnancy Outcomes Study: monitoring mothers-to-be (nuMoM2b). Am J Obstet Gynecol. 2015;212(4):539.e1–539.e24. doi: 10.1016/j.ajog.2015.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pickering TG, Hall JE, Appel LJ, et al. Recommendations for Blood Pressure Measurement in Humans and Experimental Animals. Circulation. 2005;111(5):697–716. doi: 10.1161/01.CIR.0000154900.76284.F6. [DOI] [PubMed] [Google Scholar]
- 12.Facco FL, Parker CB, Reddy UM, et al. Association Between Sleep-Disordered Breathing and Hypertensive Disorders of Pregnancy and Gestational Diabetes Mellitus. Obstet Gynecol. 2017;129(1):31–41. doi: 10.1097/AOG.0000000000001805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.ACOG Practice Bulletin No. 202: Gestational Hypertension and Preeclampsia. Obstet Gynecol.2019;133(1):e1–e25. doi: 10.1097/AOG.0000000000003018. [DOI] [PubMed] [Google Scholar]
- 14.Topel ML, Duncan EM, Krishna I, Badell ML, Vaccarino V, Quyyumi AA. Estimated Impact of the 2017 American College of Cardiology/American Heart Association Blood Pressure Guidelines on Reproductive-Aged Women. Hypertension. 2018;72(4). doi: 10.1161/HYPERTENSIONAHA.118.11660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Smith G, Pudwell J, Saade G. Impact of the New American Hypertension Guidelines on the Prevalence of Postpartum Hypertension. Am J Perinatol. 2019;36(4):440–442. doi: 10.1055/s-0038-1669441. [DOI] [PubMed] [Google Scholar]
- 16.Rosner JY, Gutierrez M, Dziadosz M, et al. Prehypertension in Early Pregnancy: What is the Significance? Am J Perinatol. 2017;34(2):117–122. doi: 10.1055/s-0036-1584542. [DOI] [PubMed] [Google Scholar]
- 17.Cao C, Cai W, Niu X, et al. Prehypertension during pregnancy and risk of small for gestational age: a systematic review and meta-analysis. J Matern Neonatal Med. September 2018:1–8. doi: 10.1080/14767058.2018.1519015. [DOI] [PubMed] [Google Scholar]
- 18.ACOG Practice Bulletin No. 203: Chronic Hypertension in Pregnancy. Obstet Gynecol. 2019;133(1):e26–e50. doi: 10.1097/AOG.0000000000003020. [DOI] [PubMed] [Google Scholar]
- 19.Steel A, Lucke J, Adams J. The prevalence and nature of the use of preconception services by women with chronic health conditions: an integrative review. BMC Womens Health. 2015;15:14. doi: 10.1186/s12905-015-0165-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Muntner P, Carey RM, Gidding S, et al. Potential US Population Impact of the 2017 ACC/AHA High Blood Pressure Guideline. Circulation. 2018;137(2):109–118. doi: 10.1161/CIRCULATIONAHA.117.032582. [DOI] [PMC free article] [PubMed] [Google Scholar]