Abstract
Parents of children with autism spectrum disorder (ASD) often report poor psychological well-being, including a high level of parenting stress and depressive symptoms. Little is known about the extent to which poor parent psychological well-being alters the emotional quality of the parent-child relationship in a context of child ASD. The current study examined the association between actor (one’s own) and partner (one’s partner’s) level of parenting stress and depressive symptoms and the emotional quality of the parent-child relationship using a Five Minute Speech Sample (FMSS) in 150 families of children with ASD, aged 5–12 years (85.7% male). Mothers and fathers were aged 38.69 (SD = 5.62) and 40.76 (SD = 6.19), respectively; 76% of mothers and 68% of fathers had a college degree. Structural equation modeling, using Analysis of Moment Structures software, was used to test Actor-Partner Interdependence Models. Results indicated that mother’s level of parenting stress and depressive symptoms were associated with her own FMSS Warmth and Criticism toward the child with ASD 12 months later in negative and positive directions. Mother’s level of parenting stress was also negatively associated with father’s FMSS Warmth toward the child with ASD 12 months later. Finally, father’s level of parenting stress was positively associated with his FMSS Criticism toward the child with ASD. Overall, findings indicate that the mother-child and father-child relationship are both impacted by parent psychological well-being in families of children with ASD; however, actor effects are stronger for mothers and partner effects were only found for fathers. Implications for interventions are discussed.
Keywords: Five Minute Speech Sample, Warmth, Criticism, Parent-child relationship quality, Autism, Expressed Emotion, Stress, Depression
Autism spectrum disorder (ASD) is a neurodevelopmental disability involving impairments in social communication, restricted and repetitive interests and behaviors, and sensory sensitivities (American Psychiatric Association, 2013). In the United States, ASD is currently estimated to impact 1 in 59 children, with a male to female ratio of 4:1 (Center for Disease Control and Prevention, 2018). Parents of children with ASD report a heightened level of parenting stress and depressive symptoms relative to other parents (Cohrs & Leslie, 2017; Hayes & Watson, 2013). In part, this heightened risk may be due to a genetic predisposition toward psychological distress; parents of children with ASD are more likely to have had psychiatric problems prior to having had children than other parents (Daniels et al., 2008; Piven et al., 1991). In addition, the heightened level of parenting stress and depressive symptoms may be driven by the unique child-related challenges faced by parents of children with ASD. These challenges stem from their son or daughter’s profile of ASD symptoms and co-occurring behavior problems (Maskey, Warnell, Parr, Le Coutuer, & McConachie, 2013; Valicenti-McDermott et al., 2015), navigating the special education (Whitaker, 2002) and healthcare (Nesbitt, 2000) systems, and dealing with the financial cost of ASD (Sharpe & Baker, 2007). Little is known about the extent to which a high level of parenting stress and depressive symptoms alter the parent-child relationship in a context of child ASD. The goal of the current study was to examine the association between actor and partner level of parenting stress and depressive symptoms and the quality of parent-child relationship 12 months later in sample of 150 families of children with ASD.
The elevated level of parenting stress and depressive symptoms reported by parents of children with ASD has been well-documented. As a group, parents of children with ASD report a higher level of parenting stress than parents of typically developing children (Estes et al., 2013; Pisula & Porębowicz-Dörsmann, 2017) and parents of children with other types of neurodevelopmental disabilities (Hayes & Watson, 2013; Valicenti-McDermott et al., 2015), with group differences of small to moderate effect size. Across studies, 20–56% of parents of children with ASD report a clinically significant level of depressive symptoms, relative to 7–29% of parents of children with other types of disabilities, and 8–19% of parents of typically developing children (Abbeduto et al., 2004; Cohrs & Leslie, 2017; Hartley, Seltzer, Head, & Abbeduto, 2012; Ingersoll & Hambrick, 2011). In the general population, a high level of parenting stress (e.g., Nelson, O’Brien, Blankson, Calkins, & Keane, 2009; Puff & Renk, 2014) and depressive symptoms (e.g., Kiernan & Huerta, 2008) has been shown to be associated with maladaptive parenting behaviors and/or a lower quality parent-child relationship. In a longitudinal study spanning 6 years, Mackler and colleagues (2015) found that having a higher level of parenting stress predicted increases in negative parenting responses, such as punishment and minimization (e.g., telling the child they were overreacting), in a general population sample of mothers of children aged 4–10 years. Similarly, in a meta-analysis of 28 studies, Wilson and Durbin (2010) found strong evidence that parent depression had significant, albeit small effect-sized, associations with reduced positive (e.g., affectionate, sensitive, and engaged) parenting behaviors (r2 = −0.19 – 0.20) and increased negative (e.g., hostile, intrusive, restrictive, and critical) parenting behaviors (r2 = 0.16 – 0.22). In reciprocal transactional fashion (Sameroff, 2000), maladaptive parenting behaviors may, in turn, inadvertently reinforce challenging child behaviors, escalating parents’ level of parenting stress and depressive symptoms. Indeed, bi-directional associations between child behavior problems and parents’ level of parenting stress have been observed in families of children with ASD (e.g., Zaidman-Zarit et al., 2014).
In addition to impacting one’s own parent-child relationship, in a family systems perspective, parenting stress and depressive symptoms in one parent would be expected to impact the other partner’s parent-child relationship (Belsky, 1981). Specifically, a high level of parenting stress or depressive symptoms experienced by one partner is theorized to alter the nature of the parent couple relationship and co-parenting relationship, which in turn, takes a toll on the other partner’s ability to engage in warm and positive parent-child interactions (e.g., Cummings, Keller, & Davies, 2005). There is evidence of such cross-partner effects of stress on parent-child relationship quality in the general population (Nelson et al., 2009; Ponnet, Wouters, Goedemé, & Mortelmans, 2016). In a sample of 101 couples who had a 7-year old child (Nelson et al., 2009), when mothers and fathers had higher work stress, their partner was less supportive of the child’s negative emotions. Similarly, cross-partner effects of depressive symptoms have been found for the parent-child relationship in non-ASD samples (Williams, 2018; Wymbs et al., 2017). In a study of parents of children exhibiting attention-deficit/hyperactivity disorder or oppositional defiant disorder behavior (Wymbs et al., 2017), parents with elevated depressive symptoms reported that their partner managed the child more negatively (29–79% higher on a rating of negativity, on average) than parents with low depressive symptoms.
There is some evidence from studies on the general population that cross-partner effects of poor psychological well-being on parent-child relationship quality differ for mothers versus fathers. In a study involving 203 families of typically developing children aged 8 to 16 years, Kouros, Papp, Goeke-Morey, and Cummings (2014) found that mother’s daily depressive symptoms were associated with lower father-child relationship quality, yet father’s daily depressive symptoms were associated with higher mother-child relationship quality. Research that has found a similar pattern has interpreted this to mean that mothers may be better at compartmentalizing family relationships than fathers, and/or may try to compensate for poor father psychological well-being by upping the quality of mother-child interactions over time (e.g., Elam, Chassin, Eisenberg, & Spinrad, 2017; Stevenson et al., 2014). To date, research assessing cross-partner effects of poor psychological well-being on the parent-child relationship have been limited to self-report measures of global parent-child relationship quality and have largely been cross-sectional. The current study adds to the broader literature by examining actor and partner effects of level of parenting stress and depressive symptoms on a direct measure of the emotional quality of the parent-child relationship (via a speech sample) 12 months later. Moreover, the current study provides the first examination of these associations in a context of child ASD. Cross-partner effects of poor psychological well-being may be pronounced in a context of high parenting stress such as child ASD. Individuals undergoing chronic stressors have been found to exhibit elevated stress reactions when faced with additional stressors (Caputo & Simon, 2013). Thus, the high level of child-related challenges faced by parents of children with ASD may mean that they have fewer resources to manage and/or compensate for a highly stressed or depressed partner. As a result, partner parenting stress and depressive symptoms may have marked effects on the parent-child relationship for both mothers and fathers of families of children with ASD.
The Current Study
The current study assessed the emotional quality of the parent-child relationship through the Five Minute Speech Sample (FMSS; Magaña et al., 1986). In the FMSS, parents talk about their child and their relationship with him/her for five minutes. Parent responses are transcribed and coded to capture indicators of parent-child relationship quality, including the parents’ level of Warmth (e.g., caring tone of voice, empathy, and interest) and Criticism (e.g., negativity, disapproval, and dissatisfaction) toward the child. The FMSS has the advantage of reducing response biases by eliciting open-ended responses based on a general prompt, rather than asking value-laden questions that can trigger socially desirable responses. FMSS ratings have been found to correlate with the observed emotions and behaviors of parents within actual parent-child interactions (Weston, Hawes, & Pasalich, 2017), and have high reliability and validity in diverse populations (Magaña et al., 1986; Van Humbeeck, Van Audenhove, De Hert, Pieters, & Storms, 2002), including in parents of children with neurodevelopmental disabilities (Hastings, Daley, Burns, & Beck, 2006) and ASD specifically (Greenberg, Seltzer, Hong, & Orsmond, 2006).
The study draws from a sample of 166 families of children with ASD (aged 5–12 years) who participated in two waves of data collection spaced approximately 12 months apart. The research questions were: (1) Does parents’ own (actor effect) level of parenting stress and depressive symptoms predict their Warmth and Criticism toward the child with ASD 12 months later? (2) Does partner’s (partner effect) level of parenting stress and depressive symptoms predict the other parent’s Warmth and Criticism toward the child with ASD 12 months later? Based on previous research, we hypothesized that one’s own level of parenting stress and depressive symptoms (actor effect) would be negatively associated with Warmth toward the child with ASD and positively associated with Criticism toward the child with ASD. Based on cross-partner findings in the general population, mother level of parenting stress and depressive symptoms was predicted to be negatively related to father Warmth and positively related to father Criticism toward the child with ASD. In contrast, we hypothesized that mothers would attempt to compensate for poor partner psychological well-being; thus, higher father level of parenting stress and depressive symptoms was predicted to be related to increased mother Warmth and decreased Criticism toward the child with ASD 12 months later.
Method
Participants
Analyses are based on the first and second waves of data collection (spaced approximately 12 months apart) in a larger longitudinal study originally including 188 couples who had a child with ASD aged 5–12 years. Measures of parenting stress and depressive symptoms were based at the first data collection time point (corresponding to 2013 – 2014) and FMSS ratings of Warmth and Criticism were obtained at the second data collection time point (FMSS was not collected at the first data collection time point).
Recruitment occurred through mailings to schools and childcare programs, fliers posted at ASD clinics and in community settings (e.g., libraries), and research registries. In order to participate, parents were required to be in a longstanding couple relationship (≥ 3 years), and have a child aged 5–12 years with a documented ASD diagnosis. Twelve families had more than one child with ASD. In these families, the oldest was selected as the child of focus, as this was when parenting in the context of ASD began. Parents were required to provide medical/educational records of the child’s ASD diagnosis, and these records had to indicate that the diagnostic evaluation included the Autism Diagnosis Observation Schedule (Lord et al., 2000). Parents completed the Social Responsiveness Scale – Second Edition (SRS-2; Constantino & Gruber, 2012) to assess the child’s current ASD symptoms. Five children had a SRS-2 Total t-score < 60, and were excluded, resulting in 183 families at the first time point. At the second time point, data was available for 166 families. The other 24 families did not participate for the following reasons: 3 separated/divorced, 3 moved out of the state, 3 could not be reached, 5 could not be reached, and 10 were too busy to participate at that time but remained in the study. There were no significant differences between the 183 families at Time 1 and the 166 families at Time 2 in: parent education level, household income, family size, couple relationship length, child age, and child SRS-2 and Child Behavior Checklist (CBCL; Achenbach & Rescorla, 2001) Total t-score. Sixteen families completed questionnaire packets via mail but did not complete the FMSS (which is administered in person). These 16 families significantly differed from the 150 families with FMSS data in father education (χ2 = 2.12, p = .04), but not in maternal education level, household income, family size, relationship length, child age, and child SRS-2 Total t-score or child CBCL Total t-score.
Procedure and Measures
At each data collection time point, parents were interviewed and independently completed questionnaires about family socio-demographics, the child with ASD, and the parent-child relationship during a 2.5-hour home or lab visit. Native Spanish speakers (n = 6) were given standardized questionnaires in both English and Spanish and a Spanish-speaking graduate student was present for these visits. Parents were each paid $50 at each wave of data collection.
Socio-demographic information.
The following variables were reported on by parents and included in analyses, as relevant, to control for their association with key variables of interest. Parent race/ethnicity was coded as White, non-Hispanic (0) versus ‘other’ (1). Parent educational level was coded: less than high school degree (0), high school diploma or General Equivalency Diploma (1), some college (2), college degree (3), some graduate school (4), and graduate/professional degree (5). Family size was operationalized as the number of children in the family. Duration of the parent couple relationship was defined as number of years in a committed relationship (in years). The date of birth of the child with ASD was used to calculate child age (in years). Child gender was coded as female (1) or male (2). Children with ASD were considered to have intellectual disability (ID) if they had a medical diagnosis of ID and/or met criteria for ID based on review of medical and/or educational records reporting IQ and adaptive behavior testing. Household income was coded from 1–14, starting at ≤$9,999 (1) and increasing by $10,000 to $20,000 intervals to ≥$160,000 (14).
Child ASD symptoms and co-occurring behavior problems.
Parents independently reported on the child’s ASD symptoms and behavior problems, and these variables were controlled for in models. The severity of child ASD symptoms during the past 6 months was obtained using the SRS-2, a 65-item parent-report questionnaire. Items are summed to create a Total t-score, which was used in analyses. The SRS-2 has high internal consistency in samples of children with ASD (Bruni, 2014). Cronbach’s alphas for the SRS-2 Total t-score in the current sample were α = 0.88 for mothers and α = 0.86 for fathers. The frequency and severity of the child with ASD’s behavior problems was assessed through the CBCL Total t-score. Items are rated on a 3-point scale. The CBCL has been shown to have good internal consistency and construct validity in ASD samples (Sikora, Hall, Hartley, Gerrard-Morris, & Cagle, 2008). In the current sample, the Cronbach’s alpha for the CBCL Total t-score was α = 0.91 for mothers and α = 0.90 for fathers.
Parenting stress.
Mothers and fathers independently completed the Burden Interview (Zarit, Reever, & Bach-Peterson, 1980), a measure of subjective perception of the personal difficulty and distress associated with caregiving, at Time 1 and Time 2. The Burden Interview consists of 29 items rated on a 3-point scale from 0 (‘not at all’) to 2 (‘extremely’) and has been shown to have strong reliability and concurrent validity in the general population (Hébert, Bravo, & Préville, 2000) and in mothers of individuals with ASD (Hartley, Barker, Seltzer, Greenberg, & Floyd, 2011). The Total score was used in analyses; higher scores indicate a higher level of parenting stress. In the current sample, the Cronbach’s alpha for the Burden Interview was α = 0.91 and α = 0.88, respectively, for mothers and fathers.
Parental depressive symptoms.
Parent level of depressive symptoms were measured at both time points using the Center for Epidemiologic Studies Depression Scale (CES-D; Radloff, 1977), a 20 item self-report scale of depressive symptoms. Parents individually rated the frequency of each depressive symptom in the past week on a 4-point scale from ‘Rarely’ (0) to ‘Most of the Time’ (3). The Total score was used in analyses. Cronbach’s alphas for CES-D were α = 0.92 for mothers and α = 0.89 for fathers. In the current sample, 36.3% of mothers and 29.3% of fathers scored above the cutoff (≥ 16) for clinically significant depressive symptoms.
Parent-child relationship quality.
The FMSS (Magaña et al., 1986) was used to assess Warmth and Criticism in the parent-child relationship. Parents were individually asked to speak about their thoughts and feelings about their child for five minutes, including “what kind of a person (child’s name) is and how the two of you get along together.” The response was recorded, transcribed, and coded (according to Magaña et al., 1986 and Vaughn & Leff, 1976) by a trained FMSS rater who was blind to study questions.
Warmth.
An overall Warmth rating was based on (a) tone of voice; (b) spontaneity of expression of sympathy, concern, and empathy; and (c) expression of interest in the child with ASD, and globally considered across the entire speech sample as ‘low’ (0), ‘medium’ (3), or ‘high’ (5) (Magaña et al., 1986). The following excerpt is from a sample rated as ‘high Warmth’:
“He’s, like I said, very creative, creates his own super heroes… Likes to be helpful, really working on sharing, and offering people things. I think he’s got a very kind heart.”
Criticism.
An overall Criticism rating was globally considered across the entire speech sample on a 3-point scale: ‘no Criticism’ (0), ‘borderline’ (1), or ‘high Criticism’ (2) (Magaña et al., 1986). Parents were rated as ‘high Criticism’ if they (a) made a negative opening remark, (b) negatively described their relationship with their child, or (c) made one or more critical comments about their child during the FMSS. Parents were rated as ‘borderline’ if they made one or more statements of dissatisfaction but did not satisfy the requirements of a ‘high Criticism’ score and were rated as ‘no Criticism’ if they did not make any critical comments throughout the entire FMSS. The following is from a speech sample rated as ‘high Criticism’:
“I get frustrated often, every day with him. He’s not able to do basic routines. He can’t stay on task for things. He still has a lot of bathroom accidents, and just hygiene stuff, that’s pretty frustrating. I get pretty frustrated and I do sometimes yell at him…”
Past research has found a significant relation between FMSS Warmth and Criticism and observed behaviors in parent-child interactions (Weston et al., 2017). All FMSSs were coded by the same trained FMSS rater. Inter-rater reliability of this trained rater with twelve other trained raters was high (mean inter-rater agreement was 93.3% [range 80–100%]).
Data Analysis Plan
SPSS version 24 (SPSS; Arbuckle, 2016) was used to examine descriptive statistics and the normality of data. Fifty-three of the 150 families had missing items on the measures. In all cases, less than 20% of items on the measure were missing (M = 1.38, SD = 0.92). Item-mean imputation was used to fill-in missing values to allow for the calculation of total scores (Eekhout et al., 2014). Pearson correlations were used to identify socio-demographics associated with variables of interest. Paired sample t-tests were used to compare mother and father level of FMSS Warmth and Criticism. Structural equation modeling within Analysis of Moment Structures (AMOS, version 24.0; Arbuckle, 2016) was used to test Actor-Partner Interdependence Models (APIM; Cook & Kenny, 2005; Kashy & Kenny, 1999). APIM simultaneously estimates the associations between a respondent’s independent variable and their own dependent variable (i.e., actor effect), as well as another respondent’s dependent variable (i.e., partner effect) (Campbell, Simpson, Kashy, & Rholes, 2001), and accounts for the non-independence of data from partners in a couple. The first APIM examined the link between actor and partner level of parenting stress at Time 1 and FMSS Warmth and Criticism at Time 2 (12 months later). This APIM controlled for child ASD symptoms (SRS-2) and behavior problems (CBCL), as well as child gender and father race/ethnicity, which were correlated with level of parenting stress. The second APIM examined the link between actor and partner level of depressive symptoms at Time 1 and FMSS Warmth and Criticism at Time 2 (12 months later). This APIM also controlled for child ASD symptoms (SRS-2) and behavior problems (CBCL), as well as household income, which were all correlated with level of depressive symptoms.
Results
Preliminary Analyses
Of the 150 families, 34.4% of the children with ASD had ID, 85.7% were male, and their average age was 7.97 years (SD = 2.25). Children with ASD had a mean SRS-2 Total t-score of 77.84 (SD = 10.60) as reported by mothers and 76.23 (SD = 9.93) as reported by fathers. The average CBCL Total t-score for children with ASD was 65.35 (SD = 9.88) as reported by mothers and 64.25 (SD = 9.38) as reported by fathers. On average, mothers were aged 38.69 years (SD = 5.62) and 23.9% did not have a college degree. Fathers average age was 40.76 (SD = 6.19) and 32.4% did not have a college degree. The majority of parents identified as White, non-Hispanic (n = 255, 85%). The remaining families comprised of parents who identified as African American (n = 2, 0.7%), Hispanic (n = 25, 8.3%), American Indian (n = 2, 0.7%), Asian or Pacific Islander (n = 10, 33%), or multiple ethnicities (n = 5 1.2%), and were combined due to the relatively low numbers of any minority group. The average household income was $80–89K (SD = 30K). The child had been adopted in four families (occurred at least 5 years prior). Four couples were not married but had lived together for at least 5 years. In 8 families, one parent was a stepparent who had been married to the biological parent for at least 3 years.
Table 1 displays the correlations between variables of interest and socio-demographic variables. Mother level of parenting stress was significantly positively correlated with mother and father ratings of child ASD symptoms and behavior problems. Father level of parenting stress was significantly higher if the child with ASD was male (rather than female), and in White, non-Hispanic fathers than fathers of other race/ethnicities. Mother and father ratings of child ASD symptoms and behavior problems were significantly positively correlated with level of parenting stress. Parent level of depressive symptoms was significantly positively correlated with their rating of child ASD symptoms and child behavior problems. Father level of depressive symptoms was significantly negatively correlated with household income. Parent FMSS Warmth was significantly negatively correlated with parent ratings of child behavior problems and father FMSS Warmth was negatively correlated with mother rating of child ASD symptoms and behavior problems. Mother FMSS Criticism was significantly positively correlated with mother rating of child ASD symptoms and behavior problems.
Table 1.
Correlations with demographic variables
| Variable | Mother Parenting Stress | Father Parenting Stress | Mother Depressive Symptoms | Father Depressive Symptoms | Mother Warmth | Father Warmth | Mother Criticism | Father Criticism |
|---|---|---|---|---|---|---|---|---|
| Child Gender | 0.04 | 0.15* | −0.07 | 0.07 | 0.04 | 0.07 | −0.04 | −0.08 |
| Child Age | −0.13 | −0.12 | −0.05 | −0.02 | 0.01 | −0.02 | 0.01 | −0.04 |
| Child ID | 0.11 | 0.11 | 0.02 | 0.01 | 0.02 | −0.09 | −0.02 | −0.01 |
| Mother SRS-2 | 0.39*** | 0.31*** | 0.15* | 0.14 | −0.15 | −0.18* | 0.22** | 0.10 |
| Father SRS-2 | 0.18* | 0.34*** | 0.05 | 0.20** | −0.03 | −0.09 | −0.10 | −0.03 |
| Mother CBCL | 0.52*** | 0.36*** | 0.31*** | 0.16* | −0.25** | −0.21* | 0.28** | 0.12 |
| Father CBCL | 0.28*** | 0.53*** | 0.18* | 0.33*** | −0.12 | −0.26** | −0.03 | 0.12 |
| Mother Age | 0.09 | 0.13 | 0.06 | 0.12 | 0.01 | −0.07 | −0.00 | −0.03 |
| Mother Ethnicity | −0.01 | −0.10 | 0.05 | −0.02 | 0.01 | 0.03 | −0.02 | −0.01 |
| Mother Education | 0.03 | 0.03 | −0.13 | −0.06 | −0.04 | −0.03 | 0.07 | 0.05 |
| Father Age | 0.03 | 0.14 | −0.01 | 0.05 | 0.05 | −0.10 | −0.05 | −0.08 |
| Father Ethnicity | 0.01 | −0.19** | 0.06 | −0.08 | 0.06 | 0.08 | −0.03 | 0.01 |
| Father Education | 0.07 | 0.08 | 0.04 | −0.10 | −0.08 | 0.10 | −0.05 | −0.14 |
| Family Size | −0.12 | −0.01 | −0.02 | −0.02 | −0.11 | −0.04 | 0.08 | −0.06 |
| Household Income | −0.03 | 0.01 | −0.13 | −0.16* | −0.08 | 0.04 | 0.04 | 0.05 |
| Relationship Length | −0.03 | 0.12 | −0.08 | 0.04 | 0.06 | 0.01 | 0.01 | −0.07 |
| Mother Parenting Stress | -- | |||||||
| Father Parenting Stress | 0.41*** | -- | ||||||
| Mother Depressive Symptoms | 0.60*** | 0.31*** | -- | |||||
| Father Depressive Symptoms | 0.20** | 0.55*** | 0.18* | -- | ||||
| Mother Warmth | −0.29*** | −0.18* | −0.28** | −0.10 | -- | |||
| Father Warmth | −0.23** | −0.13 | −0.08 | −0.10 | 0.23** | -- | ||
| Mother Criticism | 0.33*** | 0.06 | 0.27** | 0.02 | −0.51*** | −0.19* | -- | |
| Father Criticism | 0.19* | 0.23** | 0.10 | 0.11 | −0.20* | −0.35*** | 0.16* | -- |
p-value = > 0.05; ** > 0.01; *** > 0.001. The race/ethnicity of each parent was coded as White, non-Hispanic (0) versus other (1). Parents reported on child’s gender, which was coded as either female (1) or male (2). Parents individually reported on their household income, coded from 1–14, starting at ≤$9,999 (1) and increasing by $10,000 to $20,000 intervals to ≥$160,000 (14).
> 0.01;
> 0.001.
Mother level of parenting stress was correlated with father level of parenting stress, mother and father level of depressive symptoms, and mother and father FMSS Warmth and Criticism, in the expected directions. Father level of parenting stress was significantly positively correlated with father level of depressive symptoms and father FMSS Criticism and negatively correlated with mother FMSS Warmth. Mother level of depressive symptoms was significantly positively correlated with father level of depressive symptoms and mother FMSS Criticism, and significantly negatively correlated with mother Warmth. Mother and father FMSS Warmth and Criticism were significantly correlated in expected directions. Paired samples t-tests revealed that mothers showed a significantly higher level of parenting stress than fathers at Time 1 (t (149) = 3.10, p = 0.002) and Time 2 (t (149) = 2.88, p = 0.005), a higher level of depressive symptoms at Time 1 (t (149) = 2.29, p = 0.023), and higher FMSS Criticism at Time 2 (t (147) = 2.26, p = 0.025).
Actor-Partner Interdependence Models
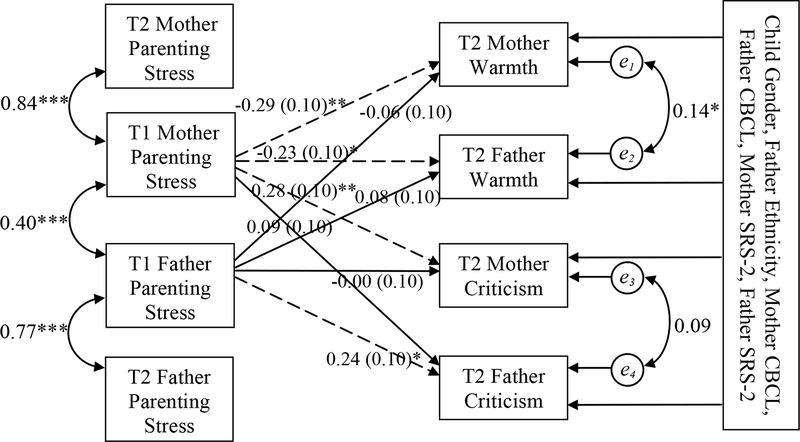
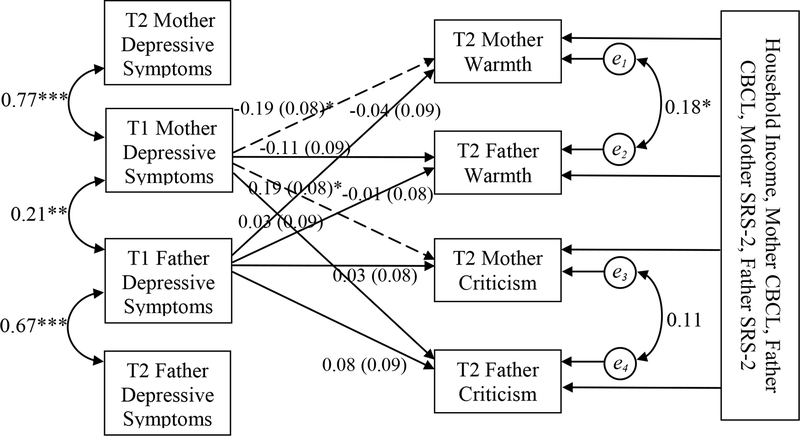
Figure 1 presents the calculated maximum likelihood estimates for the effect of mother and father level of parenting stress at Time 1 on FMSS Warmth and Criticism at Time 2, controlling for child gender, father ethnicity, and mother and father ratings of the child’s ASD symptoms and behavior problems. Figure 2 presents the calculated maximum likelihood estimates for the effect of mother and father level of depressive symptoms at Time 1 on FMSS Warmth and Criticism at Time 2, controlling for household income, and mother and father ratings of the child’s ASD symptoms and co-occurring behavior problems.
Figure 1.
Path diagram and estimates for the actor-partner interdependence model of parenting stress on mother and father Warmth and Criticism including child gender, father ethnicity, and mother and father SRS-2 (Social Responsiveness Scale – Second Edition) and CBCL (Child Behavior Checklist) ratings as covariates. Single-headed arrows indicate predictive paths; double-headed arrows indicate correlated variables. Dashed lines indicate significant predictive path. p-value = * > 0.05; ** > 0.01; *** > 0.001. Fit statistics: χ2 (df) = 85.41(14), RMSEA = .17, TLI = .60, CFI = .84.
Figure 2.
Path diagram and estimates for the actor-partner interdependence model of depressive symptoms on mother and father Warmth and Criticism including household income and mother and father SRS-2 (Social Responsiveness Scale – Second Edition) and CBCL (Child Behavior Checklist) ratings as covariates. Single-headed arrows indicate predictive paths; double-headed arrows indicate correlated variables. Dashed lines indicate significant predictive path. p-value = * > 0.05; ** > 0.01; *** > 0.001. Fit statistics: χ2 (df) = 100.18(20), RMSEA = .15, TLI = .42, CFI = .74.
In terms of the first study question, in support of our hypothesis, results indicated significant actor effects of one’s own level of parenting stress on FMSS Warmth (critical ratio = −2.95, p < .01) and Criticism (critical ratio = 2.91, p < .01) toward the child 12 months later for mothers. There was also a significant actor effect of one’s own level of parenting stress on FMSS Criticism (critical ratio = 2.29, p = .02) 12 months later for fathers. Further, there were significant actor effects of one’s own level of depressive symptoms on Time 2 FMSS Warmth (critical ratio = −2.32, p = .02) and Criticism (critical ratio = 2.39, p = .02) for mothers.
In terms of the second research question, in support of our hypothesis, results indicated a significant partner effect of level of parenting stress on fathers FMSS Warmth 12 months later (critical ratio = 2.29, p = .02). In other words, mother (actor) level of parenting stress at Time 1 predicted father (partner) Warmth toward the child with ASD. There was not a significant partner effect of mother’s depressive symptoms on father FMSS Warmth or Criticism toward the child 12 months later. Similarly, in contrast to our hypothesis, there were no significant parent effects for mothers. In other words, fathers’ level of parenting stress and depressive symptoms did not predict mother’s Warmth or Criticism toward the child 12 months later.
Discussion
Parents of children with ASD report facing numerous child-related challenges (e.g., Valicenti-McDermott et al., 2015) and have been shown to be at risk for experiencing a high level of parenting stress (e.g., Estes et al., 2013) and depressive symptoms (Cohrs & Leslie, 2017). Drawing on the family systems perspective (Belsky, 1981), the current study examined the association between actor and partner level of parenting stress and depressive symptoms and a direct measure of the emotional quality of the parent-child relationship in 150 families of children with ASD, using two time points of data spaced 12 months apart. Consistent with previous studies (e.g., Pisula & Porębowicz-Dörsmann, 2017), mothers of children with ASD experienced a higher level of parenting stress and depressive symptoms than fathers. Moreover, actor effects of psychological-being on the quality of the parent-child relationship were more prominent for mothers of children with ASD than fathers. In support of our hypothesis, mothers’ own level of parenting stress and depressive symptoms predicted her Warmth and Criticism toward the child with ASD 12 months later. In contrast, father level of parenting stress predicted his Criticism, but not Warmth, toward the child with ASD 12 months later. Further, fathers’ own level of depressive symptoms was not significantly related to his Criticism or Warmth toward the child with ASD 12 months later. Thus, mothers of children with ASD appear to be vulnerable to higher levels of parenting stress and depressive symptoms than fathers, and poor psychological well-being is more strongly linked to the parent-child relationship than it does for fathers.
Our findings of stronger actor effects of psychological well-being on the parent-child relationship in mothers than fathers is in contrast to evidence in the general population showing comparable effects for mothers and fathers (Wilson & Durbin, 2010). Families of children with ASD are more likely than their peers who have typically developing children to engage in role specialization in which one parent (most often mothers) take on the bulk of parenting activities and the other parent (most often fathers) focus on paid employment (e.g., Callander & Lindsay, 2017). The stronger association between level of parenting stress and depressive symptoms and parent-child relationship quality in mothers of children with ASD may be due to increased mother time spent in childcare. Indeed, in the present study, mothers were the primary parent (i.e., fathers spent approximately 24% less time in parenting activities than mothers). Thus, our results may reflect that the psychological well-being of the primary parent has stronger implications for the parent-child relationship than does the psychological well-being of the non-primary parent. Non-primary parents (generally fathers in our sample) may be better able to separate their own psychological well-being from their parent-child relationship given less time spent in parenting activities. That said, fathers’ level of parenting stress was associated with his Criticism toward the child with ASD 12 months later; thus, these pathways are still occurring.
Cross-partner effects of psychological well-being only occurred for fathers. If mothers had a high initial level of parenting stress, fathers reported a lower level of Warmth toward their child with ASD 12 months later. Perhaps, as has been reported in the general population (e.g., Radcliffe & Cassell, 2015; Stevenson et al., 2014), mothers (or the primary parent) often serve as a “gatekeeper” for the child with ASD. In other words, the primary parent may demonstrate attitudes or behaviors that restrict, or conversely, promote the involvement of the other parent. For example, when mother level of parenting stress is low, mothers of children with ASD may be better able to facilitate father Warmth by planning fun family activities. Davies et al. (2009) also speculated that gatekeeping behaviors may be linked to marital conflict. For example, if mother level of parenting stress is high, this stress may spill into the parent couple relationship, and result in fathers being less involved and warm in their parent-child relationship.
There are several strengths of the current study. The study included mothers and fathers of children with ASD and investigated actor and partner effects in a relatively large sample and across two time points. The study also employed a direct measure (as opposed to self-report measure) of the emotional quality of the parent-child relationship. The study also had limitations. By utilizing two data collection time points of parent level of psychological stress and depressive symptoms, we are able to begin to understand time ordered associations. Still, causality cannot be determined, and FMSS from multiple time points should be included in future research. The current study focused on the impact of parent level of parenting stress and depressive symptoms on later parent-child relationship quality, given evidence of this direction of effects in the general population (Mackler et al, 2015; Puff & Renk, 2014; Wilson and Durbin, 2010). However, parent and child impacts are likely transactional such that the child with ASD’s symptoms and behavior problems also impact the emotional quality of the parent-child relationship and parents’ psychological well-being. Further studies are also needed to examine the role of parent couple relationship quality in mediating cross-partner effects of poor psychological well-being on the parent-child relationship, given theoretical links (Belsky, 1981).
Another limitation of the study is the homogeneous sample in terms of race/ethnicity and middle socioeconomic status. Our findings are largely reflective of White, non-Hispanic parents of middle socioeconomic. There is a need for research to explore how parenting experiences may differ by race/ethnicity and socioeconomic status. In the current study, level of parenting stress was higher in White, non-Hispanic fathers than in fathers from other race/ethnicities. Small numbers within any specific racial/ethnic minority group hindered exploration of which group(s) drove this difference. The prevalence of diagnosed ASD differs by racial/ethnic group (Durkin et al., 2010; Baio et al., 2018; Jo et al., 2015), and is likely reflective of racial/ethnic disparities in access to healthcare, language barriers, differences in cultural perspectives and preferences, and diagnostic biases (Baio et al., 2018). Barriers to the inclusion of minority families in research also occur, including an underrepresentation of minority families in research registers and lack of partnerships with universities (Hilton et al., 2010). Future research should establish and maintain community partnerships in order to broaden inclusion.
Interventions to reduce parenting stress and depressive symptoms may impact the parent-child relationship in a context of child ASD. Examples of such interventions include mindfulness stress reduction, cognitive behavioral therapy, and programs that educate parents on managing child behavior problems. Efforts to enhance parent support may also improve parent-child relationship quality, given evidence that these subsystems are interconnected (Hartley, Papp, & Bolt, 2016). Family-wide interventions may foster optimal outcomes for parents and children. Unequal parenting activities is not inherently maladaptive for couples (Goldberg & Perry-Jenkins, 2004); yet, education on how parent roles and responsibilities shape family processes and ways for parents to support each other may be beneficial.
Acknowledgments
This research was supported by a grant from the National Institute of Mental Health (Hartley; R01 MH099190) and National Institute of Child Health and Development (Messing; U54 HD090256 to A. Messing).
References
- Abbeduto L, Seltzer MM, Shattuck P, Krauss MW, Orsmond G, & Murphy MM (2004). Psychological well-being and coping in mothers of youths with autism, down syndrome, or fragile X syndrome. American Journal on Mental Retardation, 109, 237–254. doi: . [DOI] [PubMed] [Google Scholar]
- Achenbach TM, & Rescorla LA (2001). Manual for the ASEBA school-age forms & profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth, & Families. [Google Scholar]
- American Psychiatric Association. (2014). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: American Psychiatric Publishing. [Google Scholar]
- Arbuckle JL (2016). IBM SPSS Amos 24 user’s guide. Chicago, IL: IBM SPSS. [Google Scholar]
- Baio J, Wiggins L, Christensen DL, Maenner MJ, Daniels J, Warren Z, … & Durkin MS (2018). Prevalence of autism spectrum disorder among children aged 8 years—Autism and developmental disabilities monitoring network, 11 sites, United States, 2014. MMWR Surveillance Summaries, 67, 1–23. doi: 10.15585/mmwr.ss6706a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belsky J (1981). Early human experience: A family perspective. Developmental Psychology, 17, 3–23. doi: 10.1037/0012-1649.17.1.3. [DOI] [Google Scholar]
- Bruni TP (2014). Test review: Social responsiveness scale–Second edition (SRS-2). Journal of Psychoeducational Assessment, 32, 365–369. doi: 10.1177/0734282913517525. [DOI] [Google Scholar]
- Callander EJ, & Lindsay DB (2017). The impact of childhood autism spectrum disorder on parent’s labour force participation: Can parents be expected to be able to re-join the labour force? Autism. Prepublished April, 7, 2017. doi: 10.1177/1362361316688331. [DOI] [PubMed] [Google Scholar]
- Campbell L, Simpson JA, Kashy DA, & Rholes WS (2001). Attachment orientations, dependence, and behavior in a stressful situation: An application of the Actor-Partner Interdependence Model. Journal of Social and Personal Relationships, 18, 821–843. doi: 10.1177/0265407501186005. [DOI] [Google Scholar]
- Caputo J, & Simon RW (2013). Physical limitation and emotional well-being: Gender and marital status variations. Journal of Health and Social Behavior, 54, 241–257. doi: 10.1177/0022146513484766. [DOI] [PubMed] [Google Scholar]
- Center for Disease Control and Prevention (CDC). (2018, April 26). Autism Spectrum Disorder. Retrieved May 4, 2018, from https://www.cdc.gov/ncbddd/autism/addm.html.
- Cohrs AC, & Leslie DL (2017). Depression in parents of children diagnosed with autism spectrum disorder: A claims-based analysis. Journal of Autism and Developmental Disorders, 47, 1416–1422. doi: 10.1007/s10803-017-3063-y. [DOI] [PubMed] [Google Scholar]
- Constantino JN, Gruber CP (2012). Social Responsiveness Scale, Second Edition (SRS-2) Torrance, CA: Western Psychological Services. [Google Scholar]
- Cook WL, & Kenny DA (2005). The actor–partner interdependence model: A model of bidirectional effects in developmental studies. International Journal of Behavioral Development, 29, 101–109. doi: 10.1080/01650250444000405. [DOI] [Google Scholar]
- Cummings EM, Keller PS, & Davies PT (2005). Towards a family process model of maternal and paternal depressive symptoms: Exploring multiple relations with child and family functioning. Journal of Child Psychology and Psychiatry, 46, 479–489. doi: 10.1111/j.1469-7610.2004.00368.x. [DOI] [PubMed] [Google Scholar]
- Daniels JL, Forssen U, Hultman CM, Cnattingius S, Savitz DA, Feychting M, & Sparen P (2008). Parental psychiatric disorders associated with autism spectrum disorders in the offspring. Pediatrics, 121, e1357–e1362. doi: 10.1542/peds.2007-2296. [DOI] [PubMed] [Google Scholar]
- Durkin MS, Maenner MJ, Meaney FJ, Levy SE, DiGuiseppi C, Nicholas JS, … & Schieve LA (2010). Socioeconomic inequality in the prevalence of autism spectrum disorder: Evidence from a US cross-sectional study. PLOS One, 5, e11551. doi: 10.1371/journal.pone.0011551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eekhout I, de Vet HC, Twisk JW, Brand JP, de Boer MR, & Heymans MW (2014). Missing data in a multi-item instrument were best handled by multiple imputation at the item score level. Journal of Clinical Epidemiology, 67, 335–342. doi: 10.1016/j.jclinepi.2013.09.009. [DOI] [PubMed] [Google Scholar]
- Elam K, Chassin L, Eisenberg N, & Spinrad T (2017). Marital stress and children’s externalizing behavior as predictors of mothers’ and fathers’ parenting. Development and Psychopathology, 29, 1305–1318. doi: 10.1017/S0954579416001322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Estes A, Olson E, Sullivan K, Greenson J, Winter J, Dawson G, & Munson J (2013). Parenting-related stress and psychological distress in mothers of toddlers with autism spectrum disorders. Brain and Development, 35, 133–138. doi: 10.1016/j.braindev.2012.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldberg AE, & Perry-Jenkins M (2004). Division of labor and working-class women’s well-being across the transition to parenthood. Journal of Family Psychology, 18, 225. doi: 10.1037/0893-3200.18.1.225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenberg JS, Seltzer MM, Hong J, & Orsmond GI (2006). Bidirectional effects of emotion and behavior problems and symptoms in adolescents and adults with autism. American Journal on Mental Retardation, 111, 229–249. doi: 10.1352/0895-8017(2006)111[229:BEOEEA]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Hartley SL, Barker ET, Seltzer MM, Greenberg JS, & Floyd FJ (2011). Marital satisfaction and parenting experiences of mothers and fathers of adolescents and adults with autism. American Journal on Intellectual and Developmental Disabilities, 116, 81–95. doi: 10.1352/1944-7558-116.1.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartley SL, Papp LM, & Bolt D (2016). Spillover of marital interactions and parenting stress in families of children with autism spectrum disorder. Journal of Clinical Child & Adolescent Psychology, 1–12. doi: 10.1080/15374416.2016.1152552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartley SL, Seltzer MM, Head L, & Abbeduto L (2012). Psychological well‐being in fathers of adolescents and young adults with Down Syndrome, Fragile X syndrome, and autism. Family Relations, 61, 327–342. doi: 10.1111/j.1741-3729.2011.00693.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hastings RP, Daley D, Burns C, & Beck A (2006). Maternal distress and expressed emotion: Cross-sectional and longitudinal relationships with behavior problems of children with intellectual disabilities. American Journal on Mental Retardation, 111, 48–61. doi: 10.1352/0895-8017(2006)111[48:MDAEEC]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Hayes SA, & Watson SL (2013). The impact of parenting stress: A meta-analysis of studies comparing the experience of parenting stress in parents of children with and without autism spectrum disorder. Journal of Autism and Developmental Disorders, 43, 629–642. doi: 10.1007/s10803-012-1604-y. [DOI] [PubMed] [Google Scholar]
- Hébert R, Bravo G, & Préville M (2000). Reliability, validity and reference values of the Zarit Burden Interview for assessing informal caregivers of community-dwelling older persons with dementia. Canadian Journal on Aging/La Revue canadienne du vieillissement, 19, 494–507. doi: 10.1017/S0714980800012484. [DOI] [Google Scholar]
- Hilton CL, Fitzgerald RT, Jackson KM, Maxim RA, Bosworth CC, Shattuck PT, … & Constantino JN (2010). Brief report: Under-representation of African Americans in autism genetic research: A rationale for inclusion of subjects representing diverse family structures. Journal of Autism and Developmental Disorders, 40, 633–639. doi: 10.1007/s10803-009-0905-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ingersoll B, & Hambrick DZ (2011). The relationship between the broader autism phenotype, child severity, and stress and depression in parents of children with autism spectrum disorders. Research in Autism Spectrum Disorders, 5, 337–344. doi: 10.1016/j.rasd.2010.04.017. [DOI] [Google Scholar]
- Jo H, Schieve LA, Rice CE, Yeargin-Allsopp M, Tian LH, Blumberg SJ, … & Boyle CA (2015). Age at autism spectrum disorder (ASD) diagnosis by race, ethnicity, and primary household language among children with special health care needs, United States, 2009–2010. Maternal and Child Health Journal, 19, 1687–1697. doi: 10.1007/s10995-015-1683-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kashy DA, Kenny DA (1999). The analysis of data from dyads and groups In Reis HT, Judd CM (Eds.), Handbook of research methods in social psychology (pp. 451–477). New York, NY: Cambridge University Press. [Google Scholar]
- Kiernan KE, & Huerta MC (2008). Economic deprivation, maternal depression, parenting and children’s cognitive and emotional development in early childhood. The British Journal of Sociology, 59, 783–806. doi: 10.1111/j.1468-4446.2008.00219.x. [DOI] [PubMed] [Google Scholar]
- Kouros CD, Papp LM, Goeke-Morey MC, & Cummings EM (2014). Spillover between marital quality and parent–child relationship quality: Parental depressive symptoms as moderators. Journal of Family Psychology, 28, 315–325. doi: 10.1037/a0036804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuusikko-Gauffin S, Pollock-Wurman R, Mattila ML, Jussila K, Ebeling H, Pauls D, et al. (2013). Social anxiety in parents of high-functioning children with autism and Asperger syndrome. Journal of Autism and Developmental Disorders, 43, 521–529. doi: 10.1007/s10803-012-1581-1. [DOI] [PubMed] [Google Scholar]
- Lord C, Risi S, Lambrecht L, Cook EJ, Leventhal BL, DiLavore PC, Pickles A, & Rutter M (2000). The Autism Diagnostic Observation Schedule—Generic: A standard measure of social and communication deficits associated with the spectrum of autism. Journal of Autism and Developmental Disorders, 30, 205–223. doi: 10.1023/A:1005592401947. [DOI] [PubMed] [Google Scholar]
- Mackler JS, Kelleher RT, Shanahan L, Calkins SD, Keane SP, & O’Brien M (2015). Parenting stress, parental reactions, and externalizing behavior from ages 4 to 10. Journal of Marriage and Family, 77, 388–406. doi: 10.1111/jomf.12163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magaña AB, Goldstein MJ, Karno M, Miklowitz DJ, Jenkins J, & Falloon IR (1986). A brief method for assessing expressed emotion in relatives of psychiatric patients. Psychiatry Research, 17, 203–212. doi: 10.1016/0165-1781(86)90049-1. [DOI] [PubMed] [Google Scholar]
- Maskey M, Warnell F, Parr JR, Le Couteur A, & McConachie H (2013). Emotional and behavioural problems in children with autism spectrum disorder. Journal of Autism and Developmental Disorders, 43, 851–859. doi: 10.1007/s10803-012-1622-9. [DOI] [PubMed] [Google Scholar]
- Nelson JA, O’Brien M, Blankson AN, Calkins SD, & Keane SP (2009). Family stress and parental responses to children’s negative emotions: Tests of the spillover, crossover, and compensatory hypotheses. Journal of Family Psychology, 23, 671–679. doi: 10.1037/a0015977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nesbitt S (2000). An evaluation of multi-agency service provision for children with autistic spectrum disorders. The British Journal of Development Disabilities, 46, 43–50. doi: 10.1179/096979500799155757 [DOI] [Google Scholar]
- Pisula E, & Porębowicz-Dörsmann A (2017). Family functioning, parenting stress and quality of life in mothers and fathers of Polish children with high functioning autism or Asperger syndrome. PLOS One, 12. doi: 10.1371/journal.pone.0186536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piven J, Chase GA, Landa R, Wzorek M, Gayle J, Cloud D, & Folstein S (1991). Psychiatric disorders in the parents of autistic individuals. Journal of the American Academy of Child & Adolescent Psychiatry, 30, 471–478. doi: 10.1097/00004583-199105000-00019. [DOI] [PubMed] [Google Scholar]
- Ponnet K, Wouters E, Goedemé T, & Mortelmans D (2016). Family financial stress, parenting and problem behavior in adolescents: An actor-partner interdependence approach. Journal of Family Issues, 37, 574–597. doi: 10.1177/0192513X13514409. [DOI] [Google Scholar]
- Puff J, & Renk K (2014). Relationships among parents’ economic stress, parenting, and young children’s behavior problems. Child Psychiatry and Human Development, 45, 712–727. doi: 10.1007/s10578-014-0440-z. [DOI] [PubMed] [Google Scholar]
- Radcliffe LS, & Cassell C (2015). Flexible working, work–family conflict, and maternal gatekeeping: The daily experiences of dual‐earner couples. Journal of Occupational and Organizational Psychology, 88, 835–855. doi: 10.1111/joop.12100. [DOI] [Google Scholar]
- Radloff LS (1977). The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1, 385–401. doi: 10.1177/014662167700100306. [DOI] [Google Scholar]
- Sameroff AJ (2000). Developmental systems and psychopathology. Development and Psychopathology, 12, 297–312. doi: 10.1017/s0954579400003035. [DOI] [PubMed] [Google Scholar]
- Sharpe DL, & Baker DL (2007). Financial issues associated with having a child with autism. Journal of Family and Economic Issues, 28, 247–264. doi: 10.1007/s10834-007-9059-6. [DOI] [Google Scholar]
- Sikora DM, Hall TA, Hartley SL, Gerrard-Morris AE, & Cagle S (2008). Does parent report of behavior differ across ADOS-G classifications: Analysis of scores from the CBCL and GARS. Journal of Autism and Developmental Disorders, 38, 440–448. doi: 10.1007/s10803-007-0407-z. [DOI] [PubMed] [Google Scholar]
- Stevenson MM, Fabricius WV, Cookston JT, Parke RD, Coltrane S, Braver SL, & Saenz DS (2014). Marital problems, maternal gatekeeping attitudes, and father–child relationships in adolescence. Developmental Psychology, 50, 1208–1218. doi: 10.1037/a0035327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valicenti-McDermott M, Lawson K, Hottinger K, Seijo R, Schechtman M, Shulman L, & Shinnar S (2015). Parental stress in families of children with autism and other developmental disabilities. Journal of Child Neurology, 30, 1728–1735. doi: 10.1177/0883073815579705. [DOI] [PubMed] [Google Scholar]
- Van Humbeeck G, Van Audenhove C, De Hert M, Pieters G, & Storms G (2002). Expressed emotion: A review of assessment instruments. Clinical Psychology Review, 22, 321–341. doi: 10.1016/S0272-7358(01)00098-8. [DOI] [PubMed] [Google Scholar]
- Vaughn CE, & Leff JP (1976). The influence of family and social factors on the course of psychiatric illness. A comparison of schizophrenic and depressed neurotic patients. The British Journal of Psychiatry, 129, 125–137. doi: 10.1192/bjp.129.2.125. [DOI] [PubMed] [Google Scholar]
- Weston S, Hawes DJ, & Pasalich DS (2017). The five minute speech sample as a measure of parent–child dynamics: Evidence from observational research. Journal of Child and Family Studies, 26, 118–136. doi: 10.1007/s10826-016-0549-8. [DOI] [Google Scholar]
- Whitaker P (2002). Supporting families of preschool children with autism: What parents want and what helps. Autism, 6, 411–426. doi: 10.1177/1362361302006004007. [DOI] [PubMed] [Google Scholar]
- Williams DT (2018). Parental depression and cooperative coparenting: A longitudinal and dyadic approach. Family Relations, 67, 253–269. doi: 10.1111/fare.12308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson S, & Durbin CE (2010). Effects of paternal depression on fathers’ parenting behaviors: A meta-analytic review. Clinical psychology review, 30, 167–180. doi: 10.1016/j.cpr.2009.10.007. [DOI] [PubMed] [Google Scholar]
- Wymbs BT, Dawson AE, Egan TE, Sacchetti GM, Tams ST, & Wymbs FA (2017). ADHD and depression symptoms in parent couples predict response to child ADHD and ODD behavior. Journal of Abnormal Child Psychology, 45, 471–484. doi: 10.1007/s10802-016-0220-2. [DOI] [PubMed] [Google Scholar]
- Zaidman-Zait A, Mirenda P, Duku E, Szatmari P, Georgiades S, Volden J, … & Fombonne E (2014). Examination of bidirectional relationships between parent stress and two types of problem behavior in children with autism spectrum disorder. Journal of Autism and Developmental Disorders, 44, 1908–1917. doi: 10.1007/s10803-014-2064-3. [DOI] [PubMed] [Google Scholar]
- Zarit SH, Reever KE, & Bach-Peterson J (1980). Relatives of the impaired elderly: Correlates of feelings of burden. Gerontologist, 20, 649–655. doi: 10.1093/geront/20.6.649. [DOI] [PubMed] [Google Scholar]