Abstract
BACKGROUND:
Current point-of-care ultrasound protocols in the evaluation of lower extremity deep vein thrombosis (DVT) can miss isolated femoral vein clots. Extended compression ultrasound (ECUS) includes evaluation of the femoral vein from the femoral vein/deep femoral vein bifurcation to the adductor canal. Our objective is to determine if emergency physicians (EPs) can learn ECUS for lower extremity DVT evaluation after a focused training session.
METHODS:
Prospective study at an urban academic center. Participants with varied ultrasound experience received instruction in ECUS prior to evaluation. Two live models with varied levels of difficult sonographic anatomy were intentionally chosen for the evaluation. Each participant scanned both models. Pre- and post-study surveys were completed.
RESULTS:
A total of 96 ultrasound examinations were performed by 48 participants (11 attendings and 37 residents). Participants’ assessment scores averaged 95.8% (95% CI 93.3%–98.3%) on the easier anatomy live model and averaged 92.3% (95% CI 88.4%–96.2%) on the difficult anatomy model. There were no statistically significant differences between attendings and residents. On the model with easier anatomy, all but 1 participant identified and compressed the proximal femoral vein successfully, and all participants identified and compressed the mid and distal femoral vein. With the difficult anatomy, 97.9% (95% CI 93.8%–102%) identified and compressed the proximal femoral vein, whereas 93.8% (95% CI 86.9%–100.6%) identified and compressed the mid femoral vein, and 91.7% (95% CI 83.9%–99.5%) identified and compressed the distal femoral vein.
CONCLUSION:
EPs at our institution were able to perform ECUS with good reproducibility after a focused training session.
Keywords: Emergency medicine, Point-of-care ultrasound, Deep vein thrombosis
INTRODUCTION
Patients with suspected lower extremity deep vein thrombosis (DVT) are often evaluated in the emergency department (ED). DVT is a major life-threatening condition resulting in morbidity, mortality, and an expenditure of resources.[1] Approximately 2 million patients are diagnosed with DVT annually in the United States, with approximately 600,000 hospitalizations and another 200,000 deaths resulting from pulmonary embolism, its most feared complication.[2]
With the sharp increase in point-of-care ultrasound (POCUS) use over the past 15 years,[3] multiple protocols to evaluate for DVTs have been developed. Of those protocols, two have gained popularity: two-point and two-region compression ultrasound for DVT evaluation. Two-point technique includes external compression of only two locations of the lower extremity veins, specifically common femoral vein and popliteal vein. The two-region compression technique includes additional veins: common femoral vein, saphenofemoral junction, femoral/deep femoral vein, and popliteal vein. Despite Bernardi et al[4] showing two-point compression ultrasound (common femoral and popliteal veins) being equivalent to whole-leg, colored-coded, duplex lower extremity ultrasound when used for the management of symptomatic patients with suspected DVT, the two-point or two-region compression technique as a standalone test has limitations in detecting isolated thrombi in the femoral vein since these protocols do not interrogate the entire femoral vein. Adding D-dimer to the evaluation results in false positives, leading to unnecessary revisits and repeat ultrasound examinations, ultimately increasing resource utilization. Adhikari et al[5] found that 6% of emergency department (ED) patients with suspected DVT had isolated thrombi in the femoral vein, which is not evaluated in the above techniques. Extended compression ultrasound (ECUS) evaluates the entire femoral vein from the femoral/deep femoral vein bifurcation to the adductor canal. ECUS is favored over two-point compression because isolated femoral vein DVTs may be missed with two-point compression technique.[6]
Prior studies have demonstrated that emergency physicians (EPs) can learn two-point compression ultrasound technique after a short training session. To our knowledge, there are no studies that have evaluated whether or not we can train EPs how to perform ECUS.
The primary objective of this study is to determine if EPs can learn ECUS for lower extremity DVT evaluation after a focused training session. The secondary objective is to evaluate the confidence levels of EPs with varying ultrasound skills to accurately perform ECUS on the lower extremity after a focused training session.
METHODS
Study design and study setting
This prospective study was conducted at two academic medical centers with two categorical Emergency Medicine (EM) residencies and one combined EM/Pediatrics residency program. There is an Emergency Ultrasound fellowship program and robust training program for residents and faculty. EM faculty members receive hospital privileges in point-of-care ultrasound, which is based on the American College of Emergency Physicians ultrasound guidelines.[7] This study received institutional review board approval from the Institutional Review Board and Human Subjects Protection Program.
Study population and inclusion criteria
All subjects enrolled in the study were EM resident physicians and practicing attending physicians. An informed consent was obtained from all physicians who agreed to participate in this study.
Study protocol
Prior to the in-person hands-on training day, all EM faculty and residents received a video link to an educational video on the ECUS technique. On the day of the hands-on session, all subjects completed a pre-study survey collecting the following information: training level, total number of ultrasound studies performed, number of DVT examinations performed, familiarity and performance of ECUS in the past, and level of confidence of performing this technique. The participants then watched the video showing the technique of performing ECUS and the associated normal ultrasound anatomy. A short lecture about ECUS was given to them before they participated in a hands-on practice session. ECUS protocol consisted of B-mode scanning and external probe compression (ultrasound machines: Mindray M-9, Shen Zhen, China and Philips CX50, Amsterdam, The Netherlands) in transverse plane of the lower extremity deep veins (common femoral vein, every two centimeters or less of the entire femoral vein, deep femoral vein, popliteal veins, saphenofemoral junction, and femoral/deep femoral bifurcation).
Then each participant was asked to perform an ECUS exam on two live models, specifically chosen for their varied difficulty levels of lower extremity sonographic anatomy, one with easier anatomy and one with more technically challenging anatomy to acquire adequate images. The subjects were evaluated by an Emergency Ultrasound fellowship-trained physician during each examination. On each live model, in addition to performing the ECUS technique, each subject was also evaluated on appropriate positioning of the patient, correct probe choice, and making the appropriate depth/gain adjustments. A total of 10 points could be given with completion of each of these steps and acquisition and compression of the required views of ECUS for each live model by each participant. The evaluators assessed the operators’ difficulty with each required view. The time required for each participant to complete an examination on each live model was also collected. A post-study survey was given to the subjects. The following information was collected: confidence level with ECUS after the study, perception of how technically challenging this technique is, whether or not they think focused training in ECUS is adequate to assess the lower extremity venous anatomy, whether or not it is feasible to perform ECUS for DVT detection in the ED, and if they would like to continue to learn additional new techniques.
An expert sonologist who was blinded to the study hypothesis independently reviewed the images and assessed quality of each of the acquired images and clips using a scale of 1 (poor image quality) to 5 (good image quality).
Statistical analysis
The data were analyzed using descriptive statistics. Continuous data were presented as averages with standard deviations or 95% confidence intervals, and dichotomous data and nominal data were presented as a percentage of frequency of occurrences. Pearson’s correlation coefficients were calculated with statistical significance as P<0.05.
RESULTS
A total of 48 subjects (37 EM residents and 11 EM attending physicians) were enrolled. The EM residents’ levels of training ranged from first year residents to fifth year residents. Attending physicians who participated range from first year out of residency to those having practiced over 20 years. For the 11 faculty participants, the range for the number of completed DVT examinations prior to the study was 0 to 150. For the residents, the range for DVT scans was 0 to 30. In our general subject pool, 39.6% reported being familiar with ECUS before our study, which equates to 45% of attendings and 37.8% of residents. Only 27.1% of the subjects have used the ECUS technique for patient evaluation. Before the study’s hands-on session, majority (83.3%) of the subjects’ confidence level with performing ECUS technique was less than or equal to 5, on a 1 (low) to 10 (high) scale.
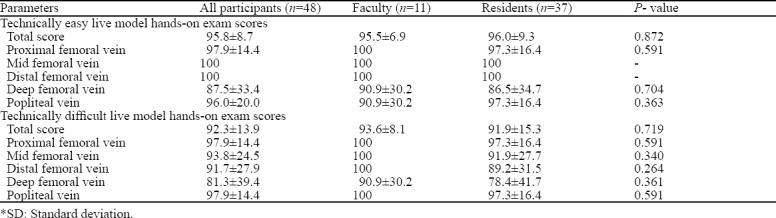
On the hands-on portion of the study, the subjects’ overall hands-on ECUS performance score was 95.8% on the live model with the easier lower extremity venous anatomy (LM1), as assessed by the Emergency Ultrasound fellowship-trained evaluating proctor. It appeared that the subjects had the most difficulty acquiring and identifying the deep femoral vein. Perceived difficulty as graded by the proctor was overall low; 83.3% of the subjects were given a 1 or 2 on a scale of 1 (easy) to 5 (difficult). As for the live model with more difficult anatomy (LM2), the overall hands-on score was 92.3%, and the most difficult views were the femoral/deep femoral vein bifurcation and the deep femoral vein. The perceived difficulty as graded by the evaluating proctor for LM2 had a wider range of 1 through 4. Table 1 summarizes faculty and resident hands-on assessment scores for evaluation of the lower extremity proximal veins for both technically easy and difficult live models.
Table 1.
Assessment scores for evaluation of lower extremity veins by Emergency Medicine faculty and residents on technically easy and technically difficult live models (%±SD
There was no statistically significant correlation between subjects’ prior ultrasound experience and the hands-on evaluation portion for either live model (LM1 P=0.93 and LM2 P=0.57). There was no statistically significant correlation (P=0.27) between the observer’s perceived level of difficulty for the subjects and the quality evaluations for the technically easy live model. However, there was a statistically significant correlation (P=0.01) for the more technically difficult model: the lower the perceived difficulty for LM2, the higher the quality of the images.
The average duration for LM1 ECUS examinations was 165.3 seconds (2.8 minutes) and for LM2 ECUS examinations was 218.2 seconds (3.6 minutes). Post-study survey showed large increase in overall confidence in performing the ECUS technique, with 83.3% of participants rating their confidence level equal or less than 5 on a 10-point Likert scale prior to the training session and subsequently 87.5% stating their confidence being greater than 5 after the training session. All participants felt this ECUS technique was not technically challenging, and they all agreed that focused training in ECUS is adequate for detecting DVTs. From the survey, all subjects stated that it was feasible to learn ECUS in a short educational session.
The image review data showed that for the LM1 examinations, the average score was 3.0, and 3.4 for the LM2 exams. Quality scores between faculty and residents were similar, and the lowest quality score of both live patients’ examinations was the deep femoral vein view. There was also no statistically significant correlation between prior ultrasound experience and quality of the images (LM1 P=0.07 and LM2 P=0.59) or time spent performing the examinations (LM1 P=0.9 and LM2 P=0.11).
DISCUSSION
In this study, our participants demonstrated the ability to learn ECUS after a short training session. Their confidence in performing ECUS increased after completion of educational session and hands-on evaluation. We believe the educational session serves as a good foundation, but participants have to perform the examination multiple times in the clinical environment to achieve competency. There are arguments that in a busy ED environment, the additional time needed to evaluate the entire femoral vein would deter physicians from performing ECUS. However, our data suggests that even in the more technically challenging live subject, physicians took fewer than 4 minutes to complete the ECUS examination. This shows that it is feasible, and certainly the time is worthwhile to evaluate for the 6% of isolated DVTs in the femoral vein. Additionally, it appears that prior experience with performing DVT ultrasounds does not factor into the subjects’ ability to learn and perform the ECUS. Among different lower extremity proximal veins, our subjects had difficulty with the deep femoral vein, as seen with the lowest hands-on scores for identifying that anatomy. However, the prevalence of isolated deep femoral vein DVTs is less than 1%,[5] so perhaps this skill may not be critical.
Our study included image quality assessments by a blinded emergency ultrasound-trained physician, mimicking the quality assurance review performed by our institution for every ultrasound examination performed. There are limitations in reviewing the images after their acquisition compared to live assessment. The hands-on assessment evaluators rated the subjects by the evaluators’ perceived level of difficulty the subject had with image acquisition. There was no statistically significant correlation between the evaluator’s perceived level of difficulty for the subjects and the quality evaluations for the technically easy live model. However, there was a statistically significant correlation for the more technically difficult model, which showed that the lower the perceived difficulty for LM2, the higher the quality of the images. Perhaps LM1’s technically easy anatomy simply yielded uniformly high-quality images, whereas for LM2, if the subject had difficulty acquiring images, the overall quality of the images decreased. Interestingly, despite having overall lower hands-on evaluation scores on the more technically difficult live model, the quality of the images acquired, as evaluated by the blinded POCUS expert, were given higher scores than the technically easy model. Perhaps the participants recognized the higher level of difficulty, so they were more careful with image acquisition.
Our physician subjects all had increased confidence with ECUS after the short training, and all thought that the limited training was adequate for them to use ECUS in the ED for DVT diagnosis. Based on our findings, we recommend training residents and clinicians to use bedside ultrasound to evaluate for lower extremity DVTs and to specifically include more thorough assessment of the femoral vein. Our data found that training emergency physicians to perform ECUS after a short educational session is feasible. However, it also demonstrates that certain aspects of the ECUS are more difficult and likely requires a certain amount of repetition in addition to an introductory training session. How much training needed remains to be defined.
Limitations
There were several limitations in this study. This was a small sample size, at a single academic institution. We did not evaluate for the long-term retention of skills, and we did not evaluate the physicians in the clinical environment. A further prospective study is necessary to truly assess the physicians’ ability to accurately diagnose or rule out DVTs in the Emergency Department using ECUS technique.
While we found slight differences between novice and experienced sonographers for their ability to locate and compress the entire femoral vein adequately, the study was not powered for such an analysis, and this is a post-hoc stratification. This study represents findings from one institution and may not be generalizable across other institutions. We used checklists to assess participants to minimize evaluator variability. A video recording of each participant performing ECUS on each live model would have been ideal for an ultrasound expert to independently assess the subjects’ difficulty with psychomotor skills or identification of the anatomy after the fact.
Our study may have investigator bias since we assessed the participants in real time, but we attempted to minimize the bias through a blinded image reviewer and use of checklists. We attempted to simulate the complexity involved in the technique and in the clinical environment by using two models with varied difficulty levels of lower extremity sonographic anatomy.
CONCLUSIONS
EPs at our institution were able to learn ECUS with good reproducibility after a focused training session. This technique shows promise as a rapid, easy-to-use, EP-performed technique of assessing patients in ED presenting with complaints concerning for DVT.
Footnotes
Funding: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. There were also no sources of support for equipment or drugs.
Ethics approval: This study received institutional review board approval from the Institutional Review Board and Human Subjects Protection Program.
Conflicts of interest: The authors declare no financial or other conflicts of interest.
Contributors: ESL: concept, design, acquisition and interpretation of data, drafting and revising article, final approval of version; HG: data analysis, drafting article; LF: acquisition of data, drafting the article; AEP: interpretation of data; SEC: interpretation of data; SA: concept, design, acquisition and interpretation of data, drafting and revising article, final approval of version.
REFERENCES
- 1.Shiver SA, Lyon M, Blaivas M, Adhikari S. Prospective comparison of emergency physician–performed venous ultrasound and CT venography for deep venous thrombosis. Am J Emerg Med. 2010;28(3):354–8. doi: 10.1016/j.ajem.2009.01.009. [DOI] [PubMed] [Google Scholar]
- 2.Crisp JG, Lovato LM, Jang TB. Compression ultrasonography of the lower extremity with portable vascular ultrasonography can accurately detect deep venous thrombosis in the emergency department. Ann Emerg Med. 2010;56(6):601–10. doi: 10.1016/j.annemergmed.2010.07.010. [DOI] [PubMed] [Google Scholar]
- 3.Pedraza García J, Valle Alonso J, Ceballos García P, Rico Rodríguez F, Aguayo López MÁ, Muñoz-Villanueva MdC. Comparison of the accuracy of emergency department-performed point-of-care-ultrasound (POCUS) in the diagnosis of lower-extremity deep vein thrombosis. J Emerg Med. 2018;54(5):656–64. doi: 10.1016/j.jemermed.2017.12.020. [DOI] [PubMed] [Google Scholar]
- 4.Bernardi E, Camporese G, Büller HR, Siragusa S, Imberti D, Berchio A, et al. Serial 2-point ultrasonography plus d-dimer vs whole-leg color-coded doppler ultrasonography for diagnosing suspected symptomatic deep vein thrombosis. JAMA. 2008;300(14):1653–9. doi: 10.1001/jama.300.14.1653. [DOI] [PubMed] [Google Scholar]
- 5.Adhikari S, Zeger W, Thom C, Fields JM. Isolated deep venous thrombosis:implications for 2-point compression ultrasonography of the lower extremity. Ann Emerg Med. 2015;66(3):262–6. doi: 10.1016/j.annemergmed.2014.10.032. [DOI] [PubMed] [Google Scholar]
- 6.Needleman L, Cronan JJ, Lilly MP, Merli GJ, Adhikari S, Hertzberg BS, et al. Ultrasound for Lower Extremity Deep Venous Thrombosis:Multidisciplinary Recommendations From the Society of Radiologists in Ultrasound Consensus Conference. Circulation. 2018;137(14):1505–5. doi: 10.1161/CIRCULATIONAHA.117.030687. [DOI] [PubMed] [Google Scholar]
- 7.Policy Statement:Ultrasound Guidelines:Emergency, Point-of-care, and Clinical Ultrasound Guidelines in Medicine. American College of Emergency Physicians. [Accessed November 9, 2018]. at https://www.acep.org/globalassets/uploads/uploaded-files/acep/membership/sections-of-membership/ultra/ultrasound-policy-2016-complete_updatedlinks_2018.pdf .


