Abstract
BACKGROUND:
It is not clear whether Emergency Severity Index (ESI) is valid to triage heart failure (HF) patients and if HF patients benefit more from a customized triage scale or not. The aim of study is to compare the effect of Heart Failure Triage Scale (HFTS) and ESI on mistriage among patients with HF who present to the emergency department (ED).
METHODS:
A randomized clinical trial was conducted from April to June 2017. HF patients with dyspnea were randomly assigned to HFTS or ESI groups. Triage level, used resources and time to electrocardiogram (ECG) were compared between both groups among HF patients who were admitted to coronary care unit (CCU), cardiac unit (CU) and discharged patients from the ED. Content validity was examined using Kappa designating agreement on relevance (K*). Reliability of both scale was evaluated using inter-observer agreement (Kappa).
RESULTS:
Seventy-three and 74 HF patients were assigned to HFTS and ESI groups respectively. Time to ECG in HFTS group was significantly shorter than that of ESI group (2.05 vs. 16.82 minutes). Triage level between HFTS and ESI groups was significantly different among patients admitted to CCU (1.0 vs. 2.8), cardiac unit (2.26 vs. 3.06) and discharged patients from the ED (3.53 vs. 2.86). Used resources in HFTS group was significantly different among triage levels (H=25.89; df=3; P<0.001).
CONCLUSION:
HFTS is associated with less mistriage than ESI for triaging HF patients. It is recommended to make use of HFTS to triage HF patients in the ED.
Keywords: Dyspnea, Heart failure, Triage, Emergency severity index
INTRODUCTION
Heart failure (HF) is a chronic and debilitating disease that is associated with significant morbidity and mortality.[1-4] Also, delay in providing care to patients with HF is significantly associated with increased morbidity and mortality.[5-7] Mistriage is one of the most important reasons of delay in providing care in the ED.[8] Therefore, it is essential that clinicians be well oriented about HF.[9] Fazel-Asgharpour et al[10] and Sanders et al[11] showed that 1.4% of HF patients was undertriaged. They showed that 1-day and 7-day mortality rate is 1.4% and 6.3% of patients who had been assigned to triage level 3 to 5, respectively. Also, it is argued that the Emergency Severity Index (ESI) may not be able to properly identify patients who present with chest pain. It may be due to a significant limitation that imposed by general criteria for triage of all types of patients in ESI.[12] General criteria may not be helpful to correctly identify subgroups of patients such as HF. HF patients take beta blockers and antihypertensive drugs that complicates interpretation of ESI vital signs criteria for HF patients. In addition, “high-risk situation” criteria mentioned in the second decision point of ESI is strictly dependent on the triage nurse’s ability to find a connection between the patient’s condition and heart failure trajectory. Sanders et al[11] reported emergency nurses take care of patients with various probabilities of disease, so they may not be highly knowledgeable about HF risk factors particularly. It seems that there is a need for well oriented scales for HF patients in the ED. Hence, it is very important to know whether triage scales stratify HF patients valid and reliable or not. Considering the above-mentioned points, there is a significant gap in the quick identification of HF patients in the ED, so HF patients suffer from significant mistriage. As such, it seems that developing a well oriented triage scale for patients with HF is one of the strategies to reduce undertriage rate. Therefore, the aims of study were to develop HF triage scale (HFTS) including validity and reliability assessment, and to compare the effect of HFTS and ESI on mistriage among patients with HF who present to the ED.
METHODS
The study has been conducted from April to June 2017. It was designed as a randomized clinical trial with a 6-hour follow-up to obtain short-term outcomes. The effect of HFTS and ESI on mistriage of HF patients in the ED was compared. The intervention group was composed of patients on whom the HFTS was conducted. The control group was composed of patients on whom the ESI (version 4) was conducted.
Ethics
This study was conducted with the permission of the Ethics Committee of Mashhad University of Medical Sciences (IR.MUMS.REC.1395.323). Furthermore, the informed consent was obtained from patients in the ED. The study was registered at Iranian Registry of Clinical Trials (IRCT2017050433807N1).
Setting
The study has been conducted in the Farabi Hospital (Mashhad, Razavi Khorasan). Four registered nurses were allocated to triage room during weekdays.
Design
The patients with chief complaint of dyspnea who presented to the ED were included if they had either history of hypertension or hospitalization due to cardiac problems. Included patients were randomly assigned to intervention (HFTS) and control (ESI) groups by pre-prepared randomized cards. Sampling was conducted over weekdays except night shift. A reduction in number of physicians and nurses takes place in the night shift, so we excluded the night shift. Triage nurses were unaware of each other’s decisions in both groups. The age, gender, vital signs (blood pressure [BP], pulse rate [PR], respiration rate [RR], oxygen saturation [SpO2]), triage level and clinical outcomes (number of used resources, ED admission, cardiac unit [CU] admission, coronary care unit [CCU] admission and ED discharge) were recorded during the first 6 hours of hospitalization in the ED. The time to first electrocardiogram (ECG), oxygen therapy and physician visit were recorded. The patients were excluded if (i) they were not diagnosed with HF by the cardiologist; (ii) they were transferred to the other hospital; and (iii) patients with incomplete documents.
Development of HFTS
Literature was searched in order to retrieve significant clinical manifestations of short-term mortality among HF patients in the emergent care. Twelve studies were identified.[13-22] Extracted clinical manifestations were organized into 4 triage levels based on risk or odd ratio. The preliminary HFTS was examined by expert panel including emergency medicine, cardiologist and cardiac nursing. Content validity (relevance) was examined based on Polit et al.[23] The scale to assess item content-relevance was labeled as 1 = not relevant, 2 = somewhat relevant, 3 = quite relevant and 4 = highly relevant. The item content validity index (I-CVI) was calculated as the number of individuals in the expert panel giving a score of either 3 or 4, divided by the number of experts. Probability of a chance occurrence (Pc) was calculated using:
Pc=[N!/A! (N - A)!] × 0.5N; N=number of experts; A=number agreeing on relevance.
Kappa designating agreement on relevance (K*) was computed using:
K*=(I-CVI - Pc)/(1 - Pc)
A minimum K* of 0.74 must be met to keep item in the HFTS.[24] The reliability of the triage scale was investigated using the Kappa Statistic.[25] The reliability of the ESI has been studied in literature. A meta-analysis showed that the kappa coefficient of reliability was substantial 0.791 (95% confidence interval: 0.787–0.795) for ESI.[26] Two triage nurses simultaneously triaged 10 patients to examine reliability of triage scales (ESI and HFTS).
Triage scales
HFTS is composed of 4 decision points. Basic criteria, high-risk criteria, ECG criteria and low-risk criteria help triage nurses to categorize HF patients into level 1, 2, 3 and 4 respectively (Figure 1). ESI triage scale is based on the patient’s acuity and used resources in the ED.[27] It is 5-point Likert scale to stratify patient’s risk in triage room. ESI level 4 and 5 were merged into one category (level 4) in the current study. Level 4 is defined as in need of 1 resource or less.
Figure 1.
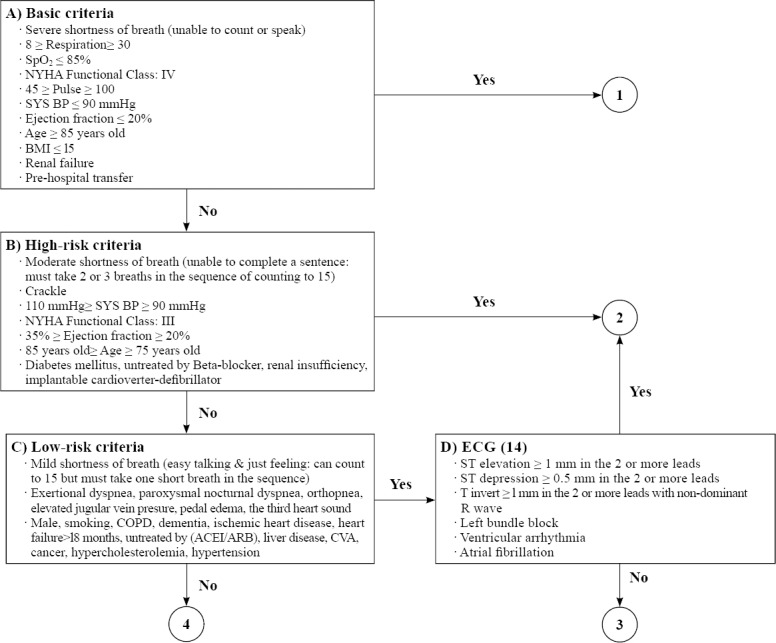
Heart failure triage scale.
Statistical analysis
The descriptive data were expressed as mean, standard deviation (SD) and percentage. The independent t-test, Man-Whitney U and Kruskal-Wallis statistics compared variables between the two groups. The SPSS 16.0 statistical software package (SPSS Inc., Chicago, IL, USA) was used. Mistriage was defined by expert panel. It does consist of undertriage and overtriage rate. Undertriage was defined as a percentage of CCU patients who had received triage level 3 or 4 plus a percentage of CU patients who had received triage level 5. Overtriage was defined as a percentage of discharged patients who had received triage level 1 or 2 plus CU patients who had received triage level 1 in the current study. Post hoc power analysis based on mean difference of triage levels showed that power is greater than 0.80 in CCU, CU and discharged patients.
RESULTS
Two patients in the HFTS group died. Six patients left ED against medical advice. Of the remaining 151 patients, 4 patients were excluded from the study (3 in HFTS, 1 in ESI) because of final diagnosis other than HF. Therefore, analysis was performed on 147 patients, 73 in HFTS and 74 in ESI. Baseline characteristics of the study population are shown in Tables 1 and 2.
Table 1.
Comparison of baseline characteristics between HFTS and ESI groups
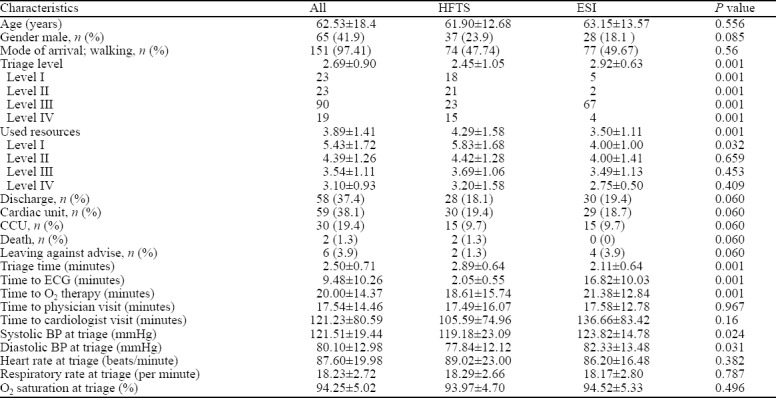
Table 2.
Comparison of patients’ characteristics between HFTS and ESI groups in regard to status of admission
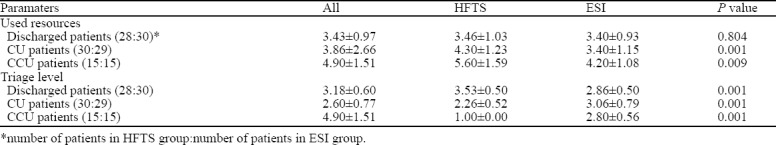
Triage level that was assigned to CCU, CU and discharged patients from the ED was presented in Figure 2. Overalls, undertriage rate was 0.0% and 20.5%; overtriage was 1.4% and 5.5% and correct triage was 98.6% and 74% for HFTS and ESI, respectively. Chi-square showed a significant difference of mistriage between groups (Z=19.371; df=2; P=0.001). In details, overtriage and undertriage among CCU, CU and discharged patients were 0.0%, 3.3%, 0.0% and 0.0%, 0.0%, 0.0% in HFTS group, respectively. Overtriage and undertriage among CCU, CU and discharged patients were 0.0%, 6.9%, 6.9% and 86.6%, 6.9%, 0.0% in ESI group, respectively
Figure 2.
Distribution of triage levels according to triage groups and status of admission.
Mean triage level was compared between HFTS and ESI groups among CCU, CU and discharged patients from the ED. Triage level was significantly different between HFTS and ESI groups (U=2227.5; P<0.002) in regard to patients admitted to CCU (U=7.5; P<0.001), cardiac unit (U=162.5; P<0.001), discharged patients from the ED (U=182; P<0.001) (Table 2).
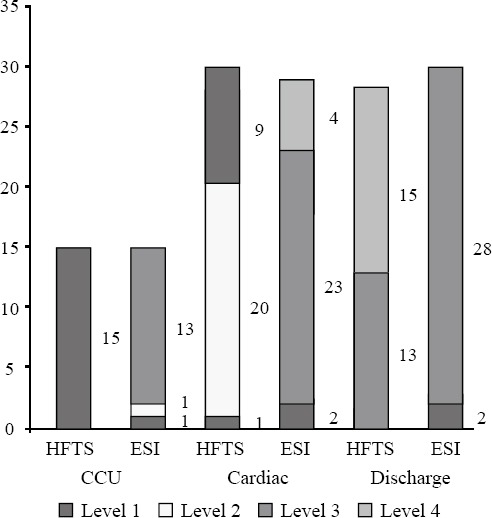
In HFTS group, used resources was significantly different among triage levels (H=25.89; df=3; P<0.001) (Figure 3). On contrary, there was no significant difference among triage levels in ESI group (H=3.415; df=3; P=0.332). Except for discharged patients (U=404; P<0.001), used resources between HFTS and ESI patients was significantly different among patients admitted to CCU (U=47; P<0.006) and CU (U=162.5; P<0.001) (Table 2).
Figure 3.
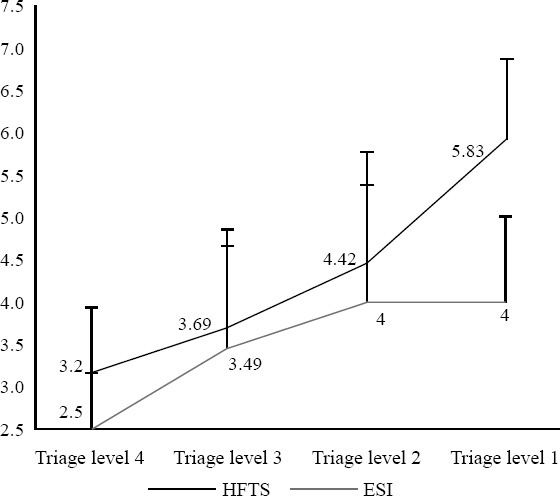
Mean used resources according to triage groups and triage levels.
Four triage nurses in ESI group and two triage nurses in HF group triaged patients. Mean nurses’ experience in the ED was 6 years for the ESI group and 7 years for the HFTS group. The kappa coefficient of reliability between nurses in HFTS group and ESI group was almost perfect, 0.82 and 0.80 respectively. Kappa (K*) ranged from 0.80 to 1. Therefore, no item was removed from preliminary HFTS. Finally, 42 items were retained in the HFTS (Figure 1).
DISCUSSION
The HFTS had significantly less mistriage than the ESI. The mean triage level of CCU patients was significantly different between the two groups (1 vs. 2.8). Also, 86.66% of the patients who were triaged by ESI and were hospitalized in CCU were assigned to triage level of 3 or higher. On contrary, no CCU patients who was triaged by HFTS received triage level 3 or higher. These findings indicated that undertriage in the ESI group is remarkable (86.66%). This may be due to the fact that the high risk criteria have been briefly mentioned in the second decision point of HFTS and so the nurses can easily refer to them in order to recognize high-risk patients. On the other hand, high risk criteria cited on the ESI are dependent on nurses’ knowledge of HF, resulting in a significant discrepancy in triage decisions. In this regard, Bergs et al[28] showed that the majority of the mistriage occurred on the ESI level 2 was undertriage. Mirhaghi et al[29] showed that high risk criteria in the ESI may be misinterpreted by triage nurses. This can lead to an increased rate of undertriage in ESI triage system.
In this line, the mean triage level of CU patients was significantly different between the two groups (2.26 vs. 3.06). Almost seven percent of the CU patients in ESI group had been undertriaged comparing to no one in HFTS group. Undertriage rate is inconsistent due to the substantial heterogeneity in patient case mix and triage scales among studies. Kamrani et al[30] reported undertrage rate of 23.7% and also Storm-Versloot et al[31] reported the undertriage rate of 14%. Both studies used general case mix of patients in ESI triage system and calculated undertriage rate based on expert panel opinion. van der Wulp et al[25] used Canadian Triage and Acuity Scale (CTAS) to triage HF patients and calculated undertriage rate based on 1-day and 7-day mortality in the ED. They showed that 1.4% to 6.3% of HF patients were undertriaged. Therefore, it is expected that undertriage rate rises dramatically when expert panel opinion was used to compute because inter-observer heterogeneity between expert panel and triage nurses may increase the undertriage rate. In the current study, final disposition was used to calculate undertriage rate, so it may overestimate the undertriage rate among HF patients.
The mean triage level of patients who were discharged from the ED (up to 6 hours) was significantly different in the two groups (3.53 vs. 2.86). About 53.5% of patients in HFTS group received triage level 4, while no discharged patient in ESI group was assigned triage level 4. In fact, it can be said that the ESI does not allow HF patients to be assigned to triage level 4 or 5 even if they are not severely ill because these patients usually need more than one resource during their admission to the ED. These results also indicate that the rate of overtriage is higher in the ESI than the HFTS. This was due to the fact that it was expected that part of discharged patients might be placed on the triage level 4. It should also be noted that 6.6% of discharged patients in ESI received triage level 2 (overtriaged). It indicates that high risk criteria decision point in ESI is not reliable and valid to triage HF patients.
The mean used resources must be associated with triage level in the ED. A valid triage scale predicts higher number of used resources for most seriously ill patients.[31] The used resources were significantly different among triage level in HFTS. On the other hand, there was no significant difference in the used resources among triage levels in patients who have been triaged by the ESI. It is worth mention that the mean used resources of level 2 was 4.5, which was lower than the other triage levels in the ESI group. This indicates that high-risk criteria in the ESI level 2 do not give sufficient understanding to correctly identify high risk patients in the ED. It is worth mentioning that CCU patients used more resources rather than CU and discharged patients, indicating that cardiologists’ decisions on patients’ final disposition is valid and associated strongly with HFTS triage levels under blinded conditions. These findings suggest that HFTS may be enable to increase agreement between nurses and cardiologist.
A large number of HF patients who presents to the ED are unlikely to develop acute changes in their vital signs and, as a result, nurses may place them on the ESI triage level 3. However only BP was significantly different between ESI and HFTS groups, and mean vital signs was in normal range in overall (Table 1). On the other hand, the high-risk criteria of the HF on the ESI are unclear. In addition, there is no possibility to put the HF into ESI triage level 4 and, thus, the patients accumulate on ESI triage level 3. Therefore, it is very important to note that the HF patients may have more different fate in relation to the triage scales than other diseases.
Limitations
There were several limitations in this study. Although the reliability of nurses’ decisions was almost perfect in both groups, triage nurses may be regarded as a part of the difference in outcome. The triage nurses had more than 5 years of experience in the ED and they were unaware of nurses’ decisions in the comparison group. Chi-square analysis showed a significant difference between triage level (1 and 2 vs. 3 and 4) and HR (>100 vs. <100) in ESI group, meaning that patients with HR>100 was regularly assigned to triage level 1 or 2 and vice versa (P<0.001). This shows that the probability of bias in triage decisions is not significant because decisions were strictly made based on ESI protocol. To be comparable, ESI level 4 and 5 were merged into one category (level 4) in the current study, because HF patients usually need more than two resources when they come to the ED and besides they are rarely assigned to the level 4 or 5. We did not have any patients who must be assigned to the level 5. Therefore, it cannot be a source of bias in the current study.
CONCLUSION
HFTS is associated with less mistriage than ESI for triaging HF patients because it helps clinicians to correctly identify high risk patients with HF. The ESI was unable to distribute HF patients across triage levels, resulting in accumulation of HF patients in ESI triage level 3 because high risk criteria in the second decision points is ambiguous and triage level 4 and 5 do not work for the majority of HF patients. The HFTS can provide more information for triage nurses to know HF patients better in the ED. Conclusively, it is recommended to make use of HFTS to triage HF patients in the ED.
ACKNOWLEDGMENT
The authors thank Dr. Majid Yaghobian for technical assistance in the field.
Footnotes
Funding: This study was granted by the Vice Chancellor of Research in Mashhad University of Medical Sciences (Grant No. 950170).
Ethics approval: This study was conducted with the permission of the Ethics Committee of Mashhad University of Medical Sciences (IR.MUMS.REC.1395.323).
Conflict of interest: There is no conflict of interest.
Contributors: AM developed the concept of study and heart failure triage scale; all authors contributed to the collection of the data; AP and AM performed data analysis and wrote the draft; AE and SH critically reviewed manuscript; AE and SH provide administrative support. All authors approved the final manuscript.
REFERENCES
- 1.Ponikowski P, Anker SD, AlHabib KF, Cowie MR, Force TL, Hu S, et al. Heart failure:preventing disease and death worldwide. ESC Heart Fail. 2014;1(1):4–25. doi: 10.1002/ehf2.12005. [DOI] [PubMed] [Google Scholar]
- 2.Johansson P, van der Wal M, van Veldhuisen DJ, Jaarsma T. Association between prehospital delay and subsequent clinical course in patients with/hospitalized for heart failure. J Card Fail. 2012;18(3):202–7. doi: 10.1016/j.cardfail.2011.12.007. [DOI] [PubMed] [Google Scholar]
- 3.Jaarsma T, Strömberg A, Ben Gal T, Cameron J, Driscoll A, Duengen HD, et al. Comparison of self-care behaviors of heart failure patients in 15 countries worldwide. Patient Educ Couns. 2013;92(1):114–20. doi: 10.1016/j.pec.2013.02.017. [DOI] [PubMed] [Google Scholar]
- 4.Gheorghiade M, Zannad F, Sopko G, Klein L, Piña IL, Konstam MA, et al. Acute heart failure syndromes current state and framework for future research. Circulation. 2005;112(25):3958–68. doi: 10.1161/CIRCULATIONAHA.105.590091. [DOI] [PubMed] [Google Scholar]
- 5.National Clinical Guideline Centre. Chronic Heart Failure: National Clinical guideline for diagnosis and management in primary and secondary care. London: National Clinical Guideline Centre; 2010. [Google Scholar]
- 6.Mant J, Doust J, Roalfe A, Barton P, Cowie MR, Glasziou P, et al. Systematic review and individual patient data meta-analysis of diagnosis of heart failure, with modelling of implications of different diagnostic strategies in primary care. Health Technol Assess. 2009;13(32):1–207. doi: 10.3310/hta13320. iii. [DOI] [PubMed] [Google Scholar]
- 7.Ebrahimi M, Mirhaghi A, Mazlom R, Heydari A, Nassehi A, Jafari M. The role descriptions of triage nurse in emergency department:a Delphi study. Scientifica. 2016 Jun 13; doi: 10.1155/2016/5269815. 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.MiróÒ Tost J, Herrero P, Jacob J, Martín-Sánchez FJ, Gil V, et al. Short-term predictive capacity of two different triage systems in patients with acute heart failure:TRICA-EAHFE study. Eur J Emerg Med. 2016;23(6):435–41. doi: 10.1097/MEJ.0000000000000290. [DOI] [PubMed] [Google Scholar]
- 9.Van Spall HG, Atzema C, Schull MJ, Newton GE, Mak S, Chong A, et al. Prediction of emergent heart failure death by semi-quantitative triage risk stratification. PloS One. 2011;6(8):e23065. doi: 10.1371/journal.pone.0023065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fazel-Asgharpour A, Barfi-dokht A, Mirhaghi AH, Shakeri MT, Kianian T. Effect of the implementation of cardiac triage scale on the time indices of patients with chest pain. Medical-Surgical Nursing Journal. 2016;5(1):35–42. [Google Scholar]
- 11.Sanders SF, DeVon HA. Accuracy in ED triage for symptoms of acute myocardial infarction. J Emerg Nurs. 2016;42(4):331–7. doi: 10.1016/j.jen.2015.12.011. [DOI] [PubMed] [Google Scholar]
- 12.Mirhaghi A, Christ M. The culture of care interfacing internal validity of Emergency Severity Index. J Emerg Nurs. 2016;42(4):297–8. doi: 10.1016/j.jen.2016.03.026. [DOI] [PubMed] [Google Scholar]
- 13.Lee D, Austin P, Rouleau J, Liu P, Naimark D, Tu J. Predicting mortality among patients hospitalized for heart failure:derivation and validation of a clinical model. JAMA. 2003;290(19):2581–7. doi: 10.1001/jama.290.19.2581. [DOI] [PubMed] [Google Scholar]
- 14.Steg P, Dabbous O, Feldman L, Cohen-Solal A, Aumont M, López-Sendón J, et al. Determinants and prognostic impact of heart failure complicating acute coronary syndromes:observations from the Global Registry of Acute Coronary Events (GRACE) Circulation. 2004;109(4):494–9. doi: 10.1161/01.CIR.0000109691.16944.DA. [DOI] [PubMed] [Google Scholar]
- 15.Collins S, Lindsell C, Naftilan A, Peacock W, Diercks D, Hiestand B, et al. Low-risk acute heart failure patients:external validation of the Society of Chest Pain Center's recommendations. Crit Pathw Cardiol. 2009;8(3):99–103. doi: 10.1097/HPC.0b013e3181b5a534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lee D, Stitt A, Austin P, Stukel T, Schull M, Chong A, et al. Prediction of heart failure mortality in emergent care:a cohort study. Ann Intern Med. 2012;156(11):767–75. doi: 10.7326/0003-4819-156-11-201206050-00003. W-261, W-2. [DOI] [PubMed] [Google Scholar]
- 17.Pocock S, Ariti C, McMurray J, Maggioni A, Køber L, Squire I, et al. Predicting survival in heart failure:a risk score based on 39 372 patients from 30 studies. Eur Heart J. 2013;34(19):1404–13. doi: 10.1093/eurheartj/ehs337. [DOI] [PubMed] [Google Scholar]
- 18.Peterson P, Rumsfeld J, Liang L, Albert N, Hernandez A, Peterson E, et al. A validated risk score for in-hospital mortality in patients with heart failure from the American Heart Association get with the guidelines program. Circ Cardiovasc Qual Outcomes. 2010;3(1):25–32. doi: 10.1161/CIRCOUTCOMES.109.854877. [DOI] [PubMed] [Google Scholar]
- 19.O'Connor C, Abraham W, Albert N, Clare R, Gattis Stough W, Gheorghiade M, et al. Predictors of mortality after discharge in patients hospitalized with heart failure:an analysis from the Organized Program to Initiate Lifesaving Treatment in Hospitalized Patients with Heart Failure (OPTIMIZE-HF) Am Heart J. 2008;156(4):662–73. doi: 10.1016/j.ahj.2008.04.030. [DOI] [PubMed] [Google Scholar]
- 20.Xu Y, Shi Y, Zhu Z, Cui C, Li B, Chen F, et al. Prognosis of patients with heart failure and reduced ejection fraction in China. Exp Ther Med. 2013;6(6):1437–42. doi: 10.3892/etm.2013.1341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stolz L, Valenzuela J, Situ-LaCasse E, Stolz U, Hawbaker N, Thompson M, et al. Clinical and historical features of emergency department patients with pericardial effusions. World J Emerg Med. 2017;8(1):29–33. doi: 10.5847/wjem.j.1920-8642.2017.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fonarow G. Epidemiology and risk stratification in acute heart failure. Am Heart J. 2008;155(2):200–7. doi: 10.1016/j.ahj.2006.10.043. [DOI] [PubMed] [Google Scholar]
- 23.Polit DF, Beck CT, Owen SV. Is the CVI an acceptable indicator of content validity?Appraisal and recommendations. Research in Nursing &Health. 2007;30(4):459–67. doi: 10.1002/nur.20199. [DOI] [PubMed] [Google Scholar]
- 24.Cicchetti DV, Sparrow SA. Developing criteria for establishing interrater reliability of specific items:applications to assessment of adaptive behavior. Am J Ment Defic. 1981;86(2):127–37. [PubMed] [Google Scholar]
- 25.van der Wulp I, van Stel HF. Calculating kappas from adjusted data improved the comparability of the reliability of triage systems:a comparative study. J Clin Epidemiol. 2010;63(11):1256–63. doi: 10.1016/j.jclinepi.2010.01.012. [DOI] [PubMed] [Google Scholar]
- 26.Mirhaghi A, Heydari A, Mazlom R, Hasanzadeh F. Reliability of the Emergency Severity Index:Meta-analysis. Sultan Qaboos Univ Med J. 2015;15(1):e71–7. [PMC free article] [PubMed] [Google Scholar]
- 27.Aeimchanbanjong K, Pandee U. Validation of different pediatric triage systems in the emergency department. World J Emerg Med. 2017;8(3):223–7. doi: 10.5847/wjem.j.1920-8642.2017.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bergs J, Verelst S, Gillet JB, Vandijck D. Evaluating implementation of the emergency severity index in a Belgian hospital. J Emerg Nurs. 2014;40(6):592–7. doi: 10.1016/j.jen.2014.01.006. [DOI] [PubMed] [Google Scholar]
- 29.Mirhaghi A, Kooshiar H, Esmaeili H, Ebrahimi M. Outcomes for emergency severity index triage implementation in the emergency department. J Clin Diagn Res. 2015;9(4):OC04–7. doi: 10.7860/JCDR/2015/11791.5737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kamrani F, Ghaemipour F, Nikravan M, Alavi Majd H. Prevalence of miss triage and outcomes under triage of patients in emergency department. JHPM. 2013;2(3):17–23. persian. [Google Scholar]
- 31.Storm-Versloot MN, Ubbink DT, Kappelhof J, Luitse JS. Comparison of an informally structured triage system, the emergency severity index, and the manchester triage system to distinguish patient priority in the emergency department. Acad Emerg Med. 2011;18(8):822–9. doi: 10.1111/j.1553-2712.2011.01122.x. [DOI] [PubMed] [Google Scholar]


