Abstract
Introduction:
Financial concerns are frequently cited by providers as a barrier to adult vaccination. This study assessed insurance reimbursements to providers for administering vaccines to adults in the private sector.
Methods:
This study, conducted in 2018, used the 2016 MarketScan Commercial Claims and Encounters Database and included vaccination visits made by adults aged 19–64 years. Four routinely recommended vaccines targeted at adults were included: tetanus toxoid, reduced diphtheria toxoid, and acellular pertussis vaccine (Tdap); tetanus and diphtheria toxoids (Td); zoster; and influenza. The mean reimbursements for vaccine purchase and administration were reported and examined by state, metropolitan statistical area, provider type, and insurance plan type. Using the private vaccine purchase price published by the Centers for Disease Control and Prevention (CDC), the study reported the proportion of vaccination visits receiving reimbursements above the CDC-published price.
Results:
The mean vaccine administration reimbursement was $25.80 for the first dose and $14.71 for additional doses in the same visit. The mean vaccine purchase reimbursement was $44.15 for Tdap, $25.78 for Td, and $216.05 for the zoster vaccine; the unweighted mean for the four examined influenza vaccines was $17.25. Reimbursements varied widely by state. Vaccine reimbursements exceeded the CDC-published price for most visits where Tdap (71.4%), zoster (87.8%), and three of four influenza (61.5%–88.5%) vaccines were administered but only for 25.8% of visits where Td was given.
Conclusions:
On average, reimbursements for administering vaccines to privately insured adults were adequate for most private practices. However, providers’ financial concerns may vary across geographic locations.
INTRODUCTION
Receiving recommended vaccines reduces the risk of developing vaccine-preventable diseases and their complications and lowers the likelihood of disease transmission because of herd immunity benefits.1 In the 2000s, several vaccines targeted at adults aged 19–64 years have been recommended by the Advisory Committee on Immunization Practices (ACIP). In 2005, ACIP recommended one dose of tetanus toxoid, reduced diphtheria toxoid, and acellular pertussis vaccine (Tdap), followed by a dose of tetanus and diphtheria toxoids (Td) booster every 10 years2; in 2008, one dose of zoster vaccine was recommended for adults aged ≥60 years,3 and in 2010, universal annual influenza vaccination was recommended.4 Although vaccines have been found to substantially reduce deaths and disabilities, uptake of the recommended vaccines among adults is not optimal.5 According to the 2016 National Health Interview Survey, the coverage rate for Tdap vaccine among adults aged 19–64 years in the past 10 years was 28%, the coverage rate for zoster vaccine among adults aged 60–64 years was 23.9%, and the coverage rate for influenza vaccine in the 2015–2016 season among adults aged ≥19 years was 43.5%.6
Provider recommendation is a leading factor affecting patients’ decision to receive vaccines.7–9 Patients often report not receiving recommendations at provider visits.8,9 One common barrier to adult vaccination reported by providers is the financial burden associated with vaccination.10–14 A survey among general internists and family physicians indicated notable proportions were dissatisfied with insurance reimbursements for vaccine purchase and administration from both private and public payers.10 Few studies have attempted to assess providers’ financial concerns about providing routinely recommended vaccines to adults. Lindley et al.15 surveyed 104 general internal medicine and family medicine practices in 2014 and reported that payment levels and perceived profit on adult vaccination services varied by payer type: A larger proportion of providers serving patients covered by preferred provider organizations reported making profits on adult vaccination, whereas most providers serving Medicaid patients reported losing money. Although focusing on vaccines administered to children and adolescents, Freed and colleagues16 reported that the mean purchase price per vaccine dose for Tdap was $34.52 (range, $29.20–$38.61), and the mean insurance reimbursements for a dose of Tdap was $39.80 (range, $29.74–$50.84); the mean vaccine administration reimbursement for the first dose was $16.62 (range, $3.87–$26.55) and amounted to $11.63 (range, $3.36–$37.20) for subsequent doses in the same visit. Though survey studies provide valuable insights into providers’ financial concerns, these studies are limited in the number of included practices and geographic locations, and a substantial proportion of providers reported limited knowledge about payments received for vaccination services.10,13,14 To better characterize vaccine-financing issues among providers, it is important to examine provider payment for adult vaccination on a broader scope.
This study used an insurance claims database to examine reimbursements for vaccine purchase and administration in the private sector. Although physician dissatisfaction on reimbursements differs by payer type,10,15 this study focused on the private insurance market as it is the most common insurance type among adults,17 and information on reimbursements to private providers for adult vaccination is very limited.
METHODS
Study Sample
This study used the 2016 MarketScan Commercial Claims and Encounters (CCAE) Database. The CCAE contains individual-level enrollment information and medical claims for individuals aged ≤64 years and covered by large self-insured employers and health plans for all U.S. states and DC. The CCAE represents a large proportion of the U.S. privately insured population—about 28 million individuals (~13% of the privately insured population) were included in 2016.
Measures
The analysis included insurance claims for vaccination visits made by privately insured adults aged 19–64 years. A vaccination visit was defined as an outpatient visit with the Current Procedural Terminology (CPT) codes related to a vaccine/vaccines and vaccine administration (i.e., 90471, administration of the first vaccine dose in the visit). Visits at which multiple vaccines were administered may have included CPT code 90472, indicating administering an additional vaccine dose during the same visit; a visit was required for the CPT code 90471 to be included in the analysis. The outcome variables included insurance reimbursements for vaccine purchase and vaccine administration. Four ACIP routinely recommended vaccines for adults aged 19–64 years were the focus of this study: Tdap (90715), Td (90714), zoster live vaccine (90736), and influenza vaccine (90656, 90658, 90686, and 90688). Although there were other CPT codes associated with influenza vaccines, this study focused on the four most common CPT codes, accounting for >95% of the insurance claims for influenza vaccine in the CCAE. Vaccination visits with vaccine or vaccine administration reimbursements <$2 were excluded (~4%) as the CCAE frequently sets the reimbursement amount to $0 or $1 for services covered by capitated insurance plans in which payments are made on a per-enrollee per-month basis. Administrative data are subject to coding and data entry errors. Although MarketScan data processors adjust the payment information to reflect the correct payment amount, some erroneous records may remain unresolved. To exclude insurance claims with unusual reimbursement amounts, the analysis dropped ~5% of the vaccination visits for which reimbursements for the first administered vaccine dose were >$87.59 (2 SDs from the mean vaccine administration reimbursement before this exclusion condition of $27.28—a method generally adopted by researchers and the Centers for Medicare & Medicaid Services to identify outliers; this approach eliminates values substantially inconsistent with most observations, while retaining a large majority of observations)18–20 or for which vaccine reimbursements were more than double the 2016 Centers for Disease Control and Prevention (CDC)–published private vaccine purchase price.21 If a vaccine CPT code was associated with more than one purchase price because of more than one manufacturer producing that type of vaccine, the average purchase price of all vaccines billed with that CPT code was used as the CDC-published price. Finally, four states were excluded (Alaska, Hawaii, Rhode Island, and Vermont) because these states purchase all or selected routinely recommended vaccines for adults and distributed them free of cost to participating providers (providers in these states would not necessarily submit insurance claims to receive vaccine reimbursements).
Statistical Analysis
The mean insurance reimbursement for the vaccine and vaccine administration was compared by state, metropolitan statistical area (MSA; MSA versus non-MSA), insurance plan type, and provider type. Insurance plans were categorized into four types: fee-for-service plans, managed care plans (preferred provider organizations and point of service), capitated plans (HMO and capitated or partially capitated point of service), and high deductible plans (consumer-driven and high deductible health plans). The analysis considered seven types of healthcare providers: family physicians, internists, obstetricians and gynecologists, emergency physicians, nurse practitioners and physician assistants (NPs/PAs), pharmacists, and others (e.g., pediatricians and providers in public health agencies). The study reported the proportion of vaccination visits at which multiple vaccines were administered and examined the distribution of the reimbursement amount for vaccine purchase and vaccine administration. The proportion of vaccination visits with vaccine reimbursements above the CDC-published price was reported. SAS version 9.3 was used to clean the data and report the results.
As a secondary analysis of data without identifiers, the study did not require IRB review.
RESULTS
This study included 2,887,132 outpatient visits with insurance claims for vaccine administration. Table 1 presents the mean vaccine administration reimbursement and proportion of vaccination visits at which multiple vaccines were administered by the state. The mean reimbursement amounts for the first dose and for vaccines administered after the first dose were $25.80 and $14.71, respectively; most vaccination visits had vaccine administration reimbursements around the mean (results not shown). There were large variations in insurance reimbursements across states, ranging from <$14.99 (South Carolina; Truven Analytics, which publishes MarketScan data, prohibits publication of estimates generated from MarketScan databases for South Carolina) to $40.40 (Oregon); South Carolina (<$11.22) and Oregon ($24.26) also had the lowest and highest reimbursement for the CPT code 90472. Overall, 8.9% (n=256,955) of the vaccination visits had multiple vaccines administered during the visit; at these visits, influenza (59.5%) was the most prevalent vaccine administered. The proportion of visits with multiple vaccines administered was highest in Oklahoma (13.5%) and lowest in Mississippi (5.4%). The findings did not show noticeable differences in vaccine administration reimbursements by MSA and insurance plan type (results not shown). Vaccine administration reimbursements to pharmacists ($17.50) and NPs/PAs ($23.51) were lower than the reimbursements to physicians (i.e., $27.87 for obstetricians and gynecologists, $27 for internists, $26.48 for emergency physicians, and $25.84 for family physicians).
Table 1.
Mean Reimbursements for Vaccine Administration by State
| State | First vaccine dose,a n ($) | Vaccine administered after the first dose,b n ($) |
≥2 vaccines administered in the same visit, % |
|---|---|---|---|
| Overall | 2,887,132 (25.80) | 264,284 (14.71) | 8.9 |
| Oregon | 38,985 (40.40c) | 4,124 (24.26c) | 10.3 |
| Massachusetts | 55,583 (39.39) | 5,045 (22.83) | 9.0 |
| Washington | 73,218 (39.06) | 8,161 (21.01) | 10.7 |
| Iowa | 22,139 (36.94) | 2,328 (20.96) | 10.2 |
| North Dakota | 2,391 (34.54) | 219 (19.22) | 8.8 |
| Wisconsin | 50,258 (33.39) | 4,613 (20.79) | 8.9 |
| South Dakota | 4,957 (33.07) | 458 (19.83) | 9.3 |
| Idaho | 43,406 (33.07) | 4,203 (19.36) | 9.7 |
| Nebraska | 11,061 (32.65) | 1,111 (18.93) | 9.7 |
| New Hampshire | 11,126 (32.28) | 983 (17.07) | 8.9 |
| California | 155,248 (31.68) | 17,123 (17.05) | 11.3 |
| North Carolina | 100,838 (31.13) | 8,526 (17.16) | 8.4 |
| Montana | 3,275 (31.13) | 389 (20.50) | 11.6 |
| Minnesota | 50,534 (30.01) | 5,406 (20.32) | 10.4 |
| Oklahoma | 49,545 (28.56) | 7,858 (15.04) | 13.5c |
| New Mexico | 4,599 (28.44) | 375 (15.68) | 8.0 |
| Colorado | 51,876 (28.35) | 5,322 (15.62) | 10.0 |
| Arkansas | 12,253 (26.40) | 1,097 (14.25) | 8.8 |
| Michigan | 145,493 (26.33) | 12,873 (14.01) | 8.8 |
| Alabama | 29,927 (25.63) | 2,024 (15.01) | 6.6 |
| Florida | 132,310 (25.42) | 11,508 (13.13) | 8.3 |
| New York | 236,491 (25.29) | 20,556 (15.04) | 8.5 |
| Virginia | 62,847 (25.17) | 5,571 (13.74) | 8.7 |
| Connecticut | 36,062 (25.14) | 3,021 (15.04) | 8.2 |
| District of Columbia | 2,264 (25.11) | 214 (14.55) | 9.3 |
| Maine | 8,439 (25.03) | 597 (14.83) | 7.1 |
| Texas | 219,187 (24.97) | 21,241 (13.94) | 9.1 |
| Georgia | 154,885 (24.68) | 13,720 (13.17) | 8.6 |
| Wyoming | 1,668 (24.38) | 142 (17.94) | 8.5 |
| Ohio | 130,257 (24.21) | 12,281 (13.10) | 9.1 |
| Utah | 34,470 (24.14) | 3,490 (13.86) | 10.0 |
| West Virginia | 5,309 (23.72) | 415 (13.40) | 7.5 |
| Indiana | 61,206 (23.37) | 5,390 (12.67) | 8.4 |
| Mississippi | 32,810 (23.36) | 1,889 (12.83) | 5.4d |
| Arizona | 43,369 (23.28) | 4,579 (13.11) | 10.1 |
| Missouri | 59,285 (23.04) | 5,323 (12.51) | 8.7 |
| New Jersey | 84,287 (22.83) | 7,532 (13.96) | 8.4 |
| Maryland | 37,340 (22.63) | 3,305 (13.38) | 8.6 |
| Pennsylvania | 94,534 (22.46) | 7,187 (13.25) | 7.5 |
| Nevada | 6,212 (22.28) | 749 (12.14) | 10.3 |
| Louisiana | 119,163 (22.11) | 10,722 (11.24) | 8.9 |
| Kansas | 22,716 (21.94) | 2,152 (13.65) | 8.9 |
| Tennessee | 85,514 (21.86) | 6,405 (11.80) | 6.9 |
| Kentucky | 67,371 (20.78) | 5,166 (11.33) | 7.4 |
| Illinois | 92,677 (19.51) | 9,187 (11.22) | 9.5 |
| Delaware | 18,739 (14.99) | 1,314 (13.78) | 6.7 |
| South Carolinae | 121,008 (<14.99d) | 8,390 (<11.22d) | — |
Source: 2016 MarketScan Commercial Claims and Encounters Database.
Vaccination visit with CPT code 90471.
Vaccination visit with CPT code 90472.
Highest amount among states for which data are presented.
Lowest amount among states for which data are presented.
Truven Health Analytics prohibits publication of the estimates generated from MarketScan databases for the state of South Carolina. CPT, current procedural terminology.
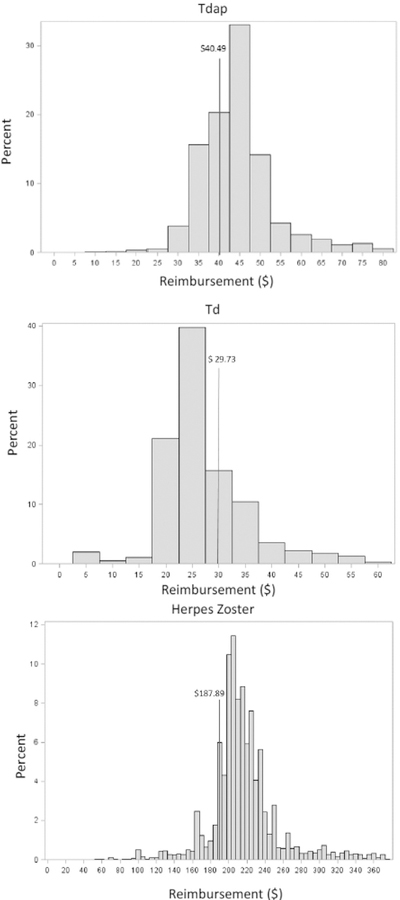
Tables 2 and 3 present the mean reimbursement amount per vaccine dose and the proportion of vaccination visits receiving insurance reimbursements above the CDC-published private sector vaccine purchase price for noninfluenza and influenza vaccines, respectively. For Tdap, the mean vaccine dose reimbursement was $44.15; the 2016 average CDC-published price was $40.49. For zoster, the mean vaccine dose reimbursement was $216.05, and the CDC-published price was $187.89; the corresponding numbers for Td were $27.20 and $29.73, respectively. Vaccine dose reimbursements higher than the CDC-published purchase price were received for 71.4% of Tdap vaccination visits and 87.7% of zoster vaccination visits; the corresponding proportion for Td was 25.8%. Figure 1 displays the distribution of the insurance reimbursements for the three vaccines. Although reimbursement amounts were clustered around the CDC-published price, the peak of the distribution was above the CDC price for Tdap and zoster. Reimbursement amounts varied by state, from $36.54 (Idaho) to $50.56 (Wisconsin) for Tdap, from $20.31 (Michigan) to $35.47 (Montana) for Td, and from $188.10 (Michigan) to $255.47 (Massachusetts) for zoster. The largest proportion of adult vaccine doses was administered by family physicians (42.4%), followed by internists (20.1%). For Tdap and Td, there was no significant difference in vaccine dose reimbursements by MSA, provider type, or insurance plan type (results not shown). For zoster, the mean vaccine dose reimbursement was lower for pharmacists ($206.26) and NPs/PAs ($209.77) compared with other types of provider; vaccine reimbursements were lower in non-MSAs ($213.56) than in MSAs ($216.30). By insurance plan type, fee-for-service plans ($210.98) received the lowest, whereas managed care plans ($217.85) received the highest vaccine dose reimbursements.
Table 2.
Mean Reimbursements for Vaccine Purchase by State
| State | Tdap, $ (%)a | Td, $ (%)a | Zoster, $ (%)a |
|---|---|---|---|
| CDC-published priceb | $40.49c | $29.73 | $187.89 |
| N | 709,245 | 53,337 | 81,593 |
| Overall | 44.15 (71.43) | 27.2 (25.78) | 216.05 (87.74) |
| Alabama | 40.01 (22.76) | 27.35 (52.11) | 199.08 (96.15) |
| Arizona | 46.87 (87.20) | 30.72 (54.66) | 213.08 (85.15) |
| Arkansas | 42.31 (62.02) | 28.38 (21.33) | 202.77 (73.44) |
| California | 50.13 (91.34) | 30.91 (42.38) | 233.16 (84.58) |
| Colorado | 44.00 (86.59) | 28.73 (35.45) | 218.93 (91.56) |
| Connecticut | 40.23 (68.93) | 25.55 (8.62) | 208.42 (91.13) |
| Delaware | 48.24 (92.40) | 26.48 (18.52) | 208.06 (92.48) |
| District of Columbia | 43.70 (65.68) | 27.95 (23.33) | 201.98 (80.65) |
| Florida | 43.30 (80.96) | 29.72 (28.95) | 207.97 (87.60) |
| Georgia | 44.52 (95.88) | 27.96 (12.95) | 208.80 (95.65) |
| Idaho | 36.54d (12.32) | 26.13 (8.82) | 193.28 (74.61) |
| Illinois | 47.76 (92.67) | 33.20 (70.03) | 223.42 (89.72) |
| Indiana | 46.62 (93.30) | 28.12 (22.60) | 216.38 (94.70) |
| Iowa | 42.53 (50.73) | 25.78 (13.60) | 218.97 (94.54) |
| Kansas | 47.00 (88.63) | 27.51 (34.58) | 214.83 (80.02) |
| Kentucky | 43.52 (78.59) | 26.46 (9.37) | 209.50 (81.97) |
| Louisiana | 36.67 (10.13) | 23.25 (4.62) | 213.54 (98.66) |
| Maine | 42.42 (78.97) | 26.86 (19.51) | 201.55 (87.75) |
| Maryland | 39.57 (45.37) | 26.06 (11.92) | 202.33 (89.03) |
| Massachusetts | 44.85 (62.27) | 29.29 (44.26) | 255.47e (87.93) |
| Michigan | 40.93 (51.09) | 20.31d (30.79) | 188.10d (77.84) |
| Minnesota | 45.28 (51.04) | 27.77 (30.88) | 235.19 (96.45) |
| Mississippi | 41.75 (38.50) | 25.99 (17.69) | 189.65 (49.04) |
| Missouri | 45.92 (91.59) | 27.79 (31.20) | 225.74 (93.40) |
| Montana | 47.81 (88.33) | 35.47e (84.00) | 224.99 (90.77) |
| Nebraska | 39.87 (33.01) | 26.69 (14.14) | 194.74 (30.27) |
| Nevada | 44.83 (77.61) | 26.74 (13.79) | 214.15 (80.29) |
| New Hampshire | 44.20 (61.02) | 31.26 (46.42) | 221.75 (89.69) |
| New Jersey | 44.56 (89.39) | 27.25 (20.63) | 210.01 (80.44) |
| New Mexico | 42.43 (57.53) | 29.92 (35.59) | 205.02 (77.52) |
| New York | 42.24 (80.76) | 23.66 (6.45) | 206.31 (88.47) |
| North Carolina | 46.06 (89.57) | 30.97 (59.00) | 218.74 (88.89) |
| North Dakota | 42.17 (38.50) | 25.56 (6.25) | 215.50 (90.10) |
| Ohio | 48.75 (88.93) | 29.62 (34.88) | 229.60 (89.49) |
| Oklahoma | 42.45 (74.22) | 27.96 (33.47) | 230.26 (98.47) |
| Oregon | 41.81 (47.16) | 29.59 (52.31) | 222.19 (75.84) |
| Pennsylvania | 42.49 (60.25) | 27.57 (14.96) | 223.99 (87.80) |
| South Carolinaf | — | — | — |
| South Dakota | 44.55 (56.25) | 29.80 (36.36) | 211.47 (94.95) |
| Tennessee | 43.44 (91.67) | 27.00 (10.95) | 207.44 (89.53) |
| Texas | 45.04 (70.92) | 30.66 (38.28) | 214.47 (80.50) |
| Utah | 39.55 (37.01) | 25.54 (20.00) | 214.57 (92.41) |
| Virginia | 47.27 (91.30) | 29.40 (29.91) | 215.65 (91.42) |
| Washington | 40.60 (21.52) | 23.71 (11.86) | 216.51 (96.18) |
| West Virginia | 41.42 (44.39) | 26.57 (7.82) | 215.61 (83.95) |
| Wisconsin | 50.56e (78.41) | 35.45 (59.64) | 244.22 (84.79) |
| Wyoming | 45.36 (76.50) | 28.50 (25.00) | 216.32 (85.42) |
Source: 2016 MarketScan Commercial Claims and Encounters Database.
Note: CPT codes for Tdap, Td, and zoster are 90715, 90714, and 90736, respectively.
The proportion of vaccination visits with vaccine purchase reimbursements above the 2016 CDC published private sector purchase price.
The 2016 price per vaccine dose in the private sector can be accessed on the CDC vaccine price list website: www.cdc.gov/vaccines/programs/vfc/awardees/vaccine-management/price-list/2016/2016–12-01.html.
The average CDC private sector list price of Adacel ($43.42) and Boostrix ($37.55) in 2016.
The minimum reimbursement amount among states for which data are presented.
The maximum reimbursement amount among states for which data are presented.
Truven Health Analytics prohibits publication of estimates generated from MarketScan databases for the state of South Carolina.
CDC, Centers for Disease Control and Prevention; CPT, current procedural terminology; Td, tetanus and diphtheria toxoids; Tdap, tetanus toxoid, reduced diphtheria toxoid, and acellular pertussis vaccine; Zoster, herpes zoster live vaccine.
Table 3.
Mean Reimbursements for Influenza Vaccine Purchase by State
| State | CPT code 90656, $ (%)a |
CPT code 90658, $ (%)a |
CPT code 90686, $ (%)a |
CPT code 90688, $ (%)a |
Unweighted average |
|---|---|---|---|---|---|
| CDC-published priceb | $15.67 | $14.41c | $17.76d | $16.20e | — |
| N | 127,376 | 242,138 | 810,914 | 347,719 | — |
| Overall | 16.66 (61.47) | 14.08 (43.88) | 19.68 (85.64) | 18.57 (88.49) | 17.25 |
| Wisconsin | 18.93 (84.60) | 18.03g (75.67) | 22.10 (89.47) | 21.83 (97.29) | 20.23g |
| Massachusetts | 17.08 (54.27) | 15.70 (51.50) | 23.35g (91.23) | 22.41g (86.25) | 19.63 |
| Delaware | 19.23 (89.85) | 15.68 (87.49) | 23.26 (98.82) | 19.47 (97.73) | 19.41 |
| Virginia | 19.30 (81.26) | 15.76 (86.91) | 20.35 (89.82) | 19.33 (92.10) | 18.69 |
| Ohio | 17.93 (72.45) | 15.45 (55.85) | 21.37 (91.13) | 19.84 (89.56) | 18.65 |
| Colorado | 21.77 (82.43) | 15.13 (63.03) | 18.78 (81.79) | 18.53 (92.60) | 18.55 |
| California | 18.24 (77.76) | 15.41 (46.25) | 20.59 (81.62) | 19.67 (91.50) | 18.48 |
| Oregon | 22.56g (82.20) | 14.63 (65.44) | 18.77 (79.50) | 17.88 (81.77) | 18.46 |
| Oklahoma | 17.28 (69.16) | 13.16 (29.16) | 22.73 (97.95) | 20.33 (96.29) | 18.38 |
| Arizona | 18.21 (70.52) | 15.50 (72.32) | 20.06 (71.82) | 19.69 (88.76) | 18.37 |
| Kansas | 18.49 (82.00) | 15.31 (68.21) | 20.19 (90.54) | 19.13 (93.64) | 18.28 |
| New Hampshire | 16.35 (45.80) | 15.25 (48.57) | 21.31 (87.44) | 20.16 (95.74) | 18.27 |
| Nebraska | 17.83 (66.15) | 16.58 (75.00) | 19.29 (86.50) | 19.16 (92.34) | 18.21 |
| District of Columbia | 20.29 (72.53) | 14.95 (72.82) | 18.87 (71.68) | 18.65 (56.11) | 18.19 |
| South Dakota | 17.14 (48.00) | 15.43 (37.50) | 19.65 (81.31) | 20.21 (73.44) | 18.11 |
| South Carolinaf | — | — | — | — | — |
| Pennsylvania | 15.35 (39.54) | 15.04 (46.81) | 20.66 (88.76) | 20.30 (95.77) | 17.84 |
| Montana | 16.18 (37.93) | 16.57 (75.34) | 19.91 (85.96) | 18.60 (76.81) | 17.82 |
| New Mexico | 14.23 (48.32) | 15.18 (57.87) | 20.93 (85.30) | 20.77 (83.29) | 17.78 |
| Michigan | 16.76 (87.99) | 16.24 (85.89) | 19.07 (97.43) | 18.89 (97.93) | 17.74 |
| Alabama | 17.52 (86.69) | 15.82 (83.88) | 19.33 (98.16) | 18.19 (98.94) | 17.71 |
| North Carolina | 17.79 (70.64) | 15.19 (71.33) | 20.05 (90.60) | 17.81 (88.45) | 17.71 |
| Missouri | 16.99 (64.47) | 15.04 (58.02) | 20.14 (91.49) | 18.59 (95.49) | 17.69 |
| Illinois | 17.05 (75.93) | 14.84 (56.95) | 19.81 (91.01) | 18.98 (93.61) | 17.67 |
| Indiana | 16.93 (89.14) | 14.19 (25.11) | 19.77 (83.23) | 19.32 (91.63) | 17.55 |
| Kentucky | 17.38 (90.04) | 13.74 (16.58) | 20.48 (98.12) | 18.19 (95.50) | 17.44 |
| Georgia | 16.67 (92.76) | 14.36 (18.80) | 20.12 (95.70) | 18.41 (98.28) | 17.39 |
| Iowa | 17.21 (62.39) | 14.53 (67.56) | 19.61 (92.75) | 18.06 (87.36) | 17.35 |
| Nevada | 17.05 (66.99) | 14.94 (63.31) | 18.63 (64.95) | 18.35 (84.01) | 17.24 |
| West Virginia | 14.55 (37.91) | 14.13 (32.92) | 20.58 (94.55) | 19.13 (91.19) | 17.10 |
| North Dakota | 17.10 (72.73) | 12.86 (26.32) | 20.78 (92.02) | 17.61 (72.77) | 17.09 |
| Wyoming | 15.68 (43.33) | 16.49 (81.48) | 17.02 (60.56) | 18.69 (68.52) | 16.97 |
| Maryland | 16.79 (67.56) | 14.56 (74.80) | 18.70 (84.58) | 17.55 (46.60) | 16.90 |
| New Jersey | 15.43 (30.86) | 14.03 (27.65) | 19.56 (71.36) | 17.99 (87.01) | 16.75 |
| Florida | 15.84 (45.44) | 13.67 (34.69) | 19.36 (81.06) | 17.82 (91.53) | 16.67 |
| Arkansas | 15.31 (43.06) | 14.15 (64.84) | 18.71 (96.49) | 18.30 (94.46) | 16.62 |
| Connecticut | 15.77 (44.79) | 13.37 (35.05) | 18.77 (90.06) | 17.79 (92.78) | 16.43 |
| Washington | 16.03 (48.97) | 13.90 (50.20) | 18.68 (92.75) | 16.83 (77.91) | 16.36 |
| New York | 15.35 (39.71) | 13.38 (29.48) | 18.95 (81.92) | 17.43 (86.94) | 16.28 |
| Utah | 14.90 (45.62) | 11.34 (27.13) | 19.29 (86.87) | 18.60 (90.31) | 16.03 |
| Texas | 14.26 (41.48) | 13.17 (46.14) | 18.11 (54.41) | 18.30 (72.61) | 15.96 |
| Maine | 13.08 (10.04) | 14.24 (36.69) | 18.00 (52.63) | 18.13 (82.80) | 15.86 |
| Mississippi | 14.22 (21.11) | 12.53 (7.87) | 18.44 (98.74) | 17.84 (82.26) | 15.76 |
| Idaho | 18.36 (87.73) | 12.51 (46.68) | 16.80 (43.91) | 15.30h (47.20) | 15.74 |
| Minnesota | 14.11 (29.47) | 12.87 (18.64) | 16.67h (46.46) | 18.28 (77.03) | 15.48 |
| Tennessee | 13.14 (14.52) | 12.67 (15.07) | 18.66 (94.84) | 16.80 (86.56) | 15.32 |
| Louisiana | 9.34h (5.89) | 9.10h (5.62) | 18.40 (97.81) | 17.10 (95.84) | 13.48h |
Source: 2016 MarketScan Commercial Claims and Encounters Database.
The proportion of vaccination visits with vaccine purchase reimbursements above the 2016 CDC published private sector purchase price.
The 2016 price per vaccine dose in the private sector can be accessed on the CDC vaccine price list website: www.cdc.gov/vaccines/programs/vfc/awardees/vaccine-management/price-list/2016/2016–12-01.html.
The average CDC private sector list price of Afluria ($14.41) and Fluvirin ($14.41) in 2016.
The average CDC private sector list price of Fluzone Quadrivalent No-Preservative ($18.487 and $17.97) and Fluarix Quadrivalent Preservative Free ($16.82) in 2016.
The average CDC private sector list price of Fluzone Quadrivalent ($16.622) and FluLaval Quadrivalent ($15.77) in 2016.
Truven Health Analytics prohibits publication of estimates generated from MarketScan databases for the state of South Carolina.
The maximum reimbursement amount among states for which data are presented.
The minimum reimbursement amount among states for which data are presented.
CDC, Centers for Disease Control and Prevention; CPT, current procedural terminology.
Figure 1.
Distribution of insurance reimbursements for selected routinely recommended adult vaccines.
Note: Data from the 2016 MarketScan Commercial Claims and Encounters Database. The y-AXIS presents the proportion of insurance claims with reimbursement amount in each price category. The line presents the 2016 CDC-published vaccine purchase price in the private sector; for Tdap, this price is the average of the two vaccines listed. CPT codes for Tdap, Td, and zoster live vaccine are 90715, 90714, and 90736, respectively.
CDC, Centers for Disease Control and Prevention; CPT, current procedural terminology; Td, tetanus and diphtheria toxoids; Tdap, tetanus toxoid, reduced diphtheria toxoid, and acellular pertussis vaccine.
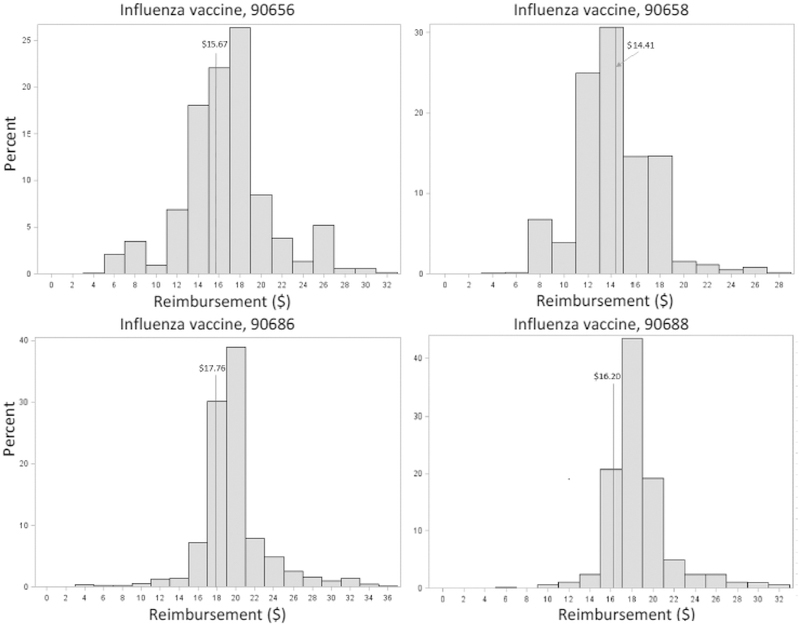
Table 3 presents the reimbursement amount for the four most commonly billed types of influenza vaccines. CPT codes 90686 (n=810,914) and 90688 (n=347,719) were the most prevalent influenza vaccine claim codes in the data, accounting for 75.8% of the adult influenza vaccines; the mean reimbursement for CPT codes 90686 and 90688 was higher ($19.68 for the CPT code 90686 and $18.57 for the CPT code 90688) than that for the CPT codes 90656 and 90658 ($16.66 for CPT code 90656 and $14.08 for CPT code 90658). The unweighted average reimbursement for these vaccines was $17.25. Mean reimbursement for three of the four influenza vaccines was above the CDC-published vaccine purchase price, and >85% of visits at which either of the two most commonly administered influenza vaccines were administered received vaccine reimbursements higher than the CDC-published price. Figure 2 displays the distribution of insurance reimbursements for the four influenza vaccines. Reimbursements for influenza vaccine purchase were clustered around the price published by CDC, and the peak of the distribution for all four occurred at or above the CDC price. Looking at the reimbursement amount by state, the unweighted mean reimbursement for the four influenza vaccines ranged from $13.48 (Louisiana) to $20.23 (Wisconsin). For the most commonly billed influenza vaccine (90686), the range of reimbursement was between $16.67 (Minnesota) and $23.35 (Massachusetts); Massachusetts was also the highest reimbursement ($22.41) state for the vaccine with the CPT code 90688. Reimbursement for CPT codes 90656 ($9.34) and 90658 ($9.10) was the lowest in Louisiana; <6% of claims in Louisiana were above the CDC-published price for those two influenza vaccines. The data did not show noticeable and consistent differences in influenza vaccine reimbursements by MSA and insurance plan type across the four vaccines. By provider type, reimbursements were lower for nonphysician providers: NPs/PAs received the lowest reimbursements for CPT code 90686 ($18.62), and pharmacists received the lowest reimbursements for CPT codes 90656 ($15.46), 90658 ($12.45), and 90688 ($17.82).
Figure 2.
Distribution of insurance reimbursements for adult influenza vaccines.
Note: Data from the 2016 MarketScan Commercial Claims and Encounters Database. The y-axis presents the proportion of insurance claims with reimbursement amount in each price category. The line presents the 2016 CDC-published vaccine purchase price in the private sector; for CPT codes covering more than one influenza vaccine product, this is the average price of the products listed.
CDC, Centers for Disease Control and Prevention; CPT, current procedural terminology.
DISCUSSION
This study used the 2016 MarketScan CCAE data to examine insurance reimbursements to private providers for administering routinely recommended adult vaccines in 46 states and DC. The mean reimbursement amount for five of seven vaccines included was above the private purchase price published by the CDC, although payments varied widely by state. When comparing vaccine dose and administration payments by provider type, reimbursement was lower for nonphysician vaccine providers than physician vaccine providers.
Insurance companies set their reimbursement rates for private providers based on Medicare reimbursement rates, which are adjusted to account for geographic variations in medical costs.22 This may contribute to the finding of a large variation in insurance reimbursements by geographic location. Other factors, such as variations in population health, healthcare utilization pattern, and the competition among insurance carriers within a state, are likely to play a role in geographic differences in reimbursements for private providers.
The mean vaccine administration reimbursement ($25.80 for the first dose and $14.71 for subsequent doses) and the mean reimbursement for Tdap vaccine purchase ($44.15) were higher than the numbers reported by Freed et al.16 The differences are likely attributable to differences in study methods (e.g., surveying providers versus insurance claims data), study samples (e.g., 89% of the practices included by Freed and colleagues were pediatric offices), and geographic variations (i.e., their survey covered only five states). In the report of Freed et al., the mean purchase price per vaccine dose for Tdap was $34.52 ($39.96 in 2016 dollars based on the Consumer Price Index). This number was still lower than the CDC-published price, $40.49. Using $39.96 as the cut off, the proportion of Tdap vaccination visits receiving reimbursements above the cut off increased to 74.3%.
The CDC private vaccine purchase prices are reported by vaccine manufacturers. It is common for private providers to pay lower than the manufacturer-reported price as private providers often receive discounts through participating in group purchasing, bulk ordering, or prompt payment.15,16 Accordingly, the proportion of vaccination visits receiving reimbursements above the actual vaccine purchase price is likely to be higher than what this study reports. Moreover, the mean vaccine administration reimbursement ($25.80) was substantially greater than the average total variable cost per vaccine injection ($11.51; $13.32 in 2016 dollars) as reported in Glazner and colleagues.23 These findings suggest that many private providers are likely to receive adequate insurance reimbursements. Previous research on payments for adult vaccination mostly comes from surveying providers, and their results suggest that providers are generally dissatisfied with insurance reimbursements for vaccination services.10–14 Using insurance claims data, this study suggests that many providers may profit when administering vaccines to privately insured adults. The statement is consistent with Lindley et al.15 that a greater proportion of private providers reported profiting on adult vaccination services; this may also explain why many physician practices reported that they rarely/never negotiated insurance payments with private insurers. However, financial concerns among private providers are likely to vary by location, as the findings showed large variations in insurance reimbursements by state. It would also vary by individual practices as costs to vaccinate also include labor, vaccine storage, recovery costs attributable to wastage, and inventory shrinkage, among others.24
This study showed lower reimbursements for nonphysician providers, such as pharmacists and NPs/PAs. The adult immunization standards recommend that all types of providers recommend and administer vaccines to adult patients25; having lower reimbursements for nonphysician providers may be a disincentive to have vaccines recommended by every provider at every visit. Moreover, pharmacies are often present when other vaccine providers are scarce (i.e., rural or other provider shortage areas). Although low reimbursements do not necessarily result in low profits or financial losses for pharmacies (the overhead costs of administering vaccines in pharmacies are likely to be lower than the overhead costs in physician’s offices, and individuals receiving vaccines at pharmacies often make retail purchases that may offset the low vaccination reimbursements), increasing reimbursements for nonphysician providers could still improve access to adult vaccines.
The data show that influenza vaccines were the most common vaccine types administered to adults: About 1.5 million vaccination visits had influenza vaccine administered compared with about 710,000 visits for Tdap. The results were consistent with the adult vaccine coverage estimates generated from the 2016 National Health Interview Survey.6 Public campaign for influenza vaccines might increase adults’ awareness and demand for the vaccine. In addition, studies have shown that physicians are more likely to assess patient vaccination status for seasonal influenza and stock influenza vaccines.11 One reason may be that influenza vaccines are relatively less expensive than other vaccines recommended for adults, and a higher proportion of physicians report making profits on seasonal influenza vaccination.15
Limitations
This study is subject to some limitations. First, it considered four ACIP routinely recommended vaccines and was based on a convenience sample of patients aged 19–64 years residing in 46 states and DC covered by large self-insured employers or regional health plans in the private insurance market. The results may not generalize to all providers administering adult vaccines. However, more than 2.8 million vaccination claims were included, with variations in geographic locations and health insurance plans. Second, the authors used the CDC-published vaccine purchase prices as the basis to gain insights into the financial well-being of private providers. Studies have shown large variations in vaccine purchase prices among private pediatric practices,16,26 and vaccine purchase costs in individual practices likely differed from the CDC price. However, no published data on vaccine purchase costs are available. Accordingly, this study evaluated providers’ financial concerns on adult vaccination at an average level rather than assessed the financial gains or losses of individual practices on vaccinating adults. The financial well-being of an individual practice would depend on practice-specific vaccine purchase costs and other related costs to vaccinate,16,24 as well as the mix of payers billed by that practice.
CONCLUSIONS
Although some private practices may profit from administering vaccines to adults, providers’ financial well-being is likely to vary across states and individual practices. It is important to understand profitability of adult vaccination services at the state and local levels, as financial disincentives could reduce the number of providers offering adult vaccines and hinder the ability to improve vaccination coverage in underserved areas.
ACKNOWLEDGMENTS
The findings and conclusions of this paper are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Footnotes
No financial disclosures were reported by the authors of this paper.
REFERENCES
- 1.Centers for Disease Control and Prevention. Why vaccines are important for you www.cdc.gov/vaccines/adults/reasons-to-vaccinate.html Published 2016. Accessed August 15, 2018.
- 2.Kretsinger K, Broder KR, Cortese MM, et al. Preventing tetanus, diphtheria, and pertussis among adults: use of tetanus toxoid, reduced diphtheria toxoid and acellular pertussis vaccine recommendations of the Advisory Committee on Immunization Practices (ACIP) and recommendation of ACIP, supported by the Healthcare Infection Control Practices Advisory Committee (HICPAC), for use of Tdap among health-care personnel. MMWR Recomm Rep 2006;55(RR-17):1–37. [PubMed] [Google Scholar]
- 3.Harpaz R, Ortega-Sanchez IR, Seward JF, Advisory Committee on Immunization Practices (ACIP) Centers for Disease Control and Prevention (CDC). Prevention of herpes zoster: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep 2008;57(RR–5):1–30. [PubMed] [Google Scholar]
- 4.Fiore AE, Uyeki TM, Broder K, et al. Prevention and control of influenza with vaccines: recommendations of the Advisory Committee on Immunization Practices (ACIP), 2010. MMWR Recomm Rep 2010;59 (RR–8):1–62. [PubMed] [Google Scholar]
- 5.Office of Disease Prevention and Health Promotion. Healthy People 2020 topics and objectives www.healthypeople.gov/2020/topics-objectives/topic/immunization-and-infectious-diseases/objectives Accessed July 25, 2017.
- 6.Centers for Disease Control and Prevention. Vaccination coverage among adults in the United States. National Health Interview Survey; 2016. www.cdc.gov/vaccines/imz-managers/coverage/adultvaxview/pubs-resources/NHIS-2016.html Published 2016 Accessed February 6, 2019.
- 7.Armstrong K, Berlin M, Schwartz JS, Propert K, Ubel PA. Barriers to influenza immunization in a low-income urban population. Am J Prev Med 2001;20(1):21–25. 10.1016/S0749-3797(00)00263-4. [DOI] [PubMed] [Google Scholar]
- 8.Johnson DR, Nichol KL, Lipczynski K. Barriers to adult immunization. Am J Med 2008;121(7 suppl 2):S28–S35. 10.1016/j.amjmed.2008.05.005. [DOI] [PubMed] [Google Scholar]
- 9.Bridges CB, Hurley LP, Williams WW, Ramakrishnan A, Dean AK, Groom AV. Meeting the challenges of immunizing adults. Am J Prev Med 2015;49(6 suppl 4):S455–S464. 10.1016/j.amepre.2015.08.014. [DOI] [PubMed] [Google Scholar]
- 10.Hurley LP, Lindley MC, Allison MA, et al. Primary care physicians’ perspective on financial issues and adult immunization in the era of the Affordable Care Act. Vaccine 2017;35(4):647–654. 10.1016/j.vaccine.2016.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hurley LP, Bridges CB, Harpaz R, et al. U.S. physicians’ perspective of adult vaccine delivery. Ann Intern Med 2014;160(3):161–170. 10.7326/M13-2332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Freed GL, Clark SJ, Cowan AE, Coleman MS. Primary care physician perspectives on providing adult vaccines. Vaccine 2011;29(9):1850–1854. 10.1016/j.vaccine.2010.12.097. [DOI] [PubMed] [Google Scholar]
- 13.Hurley LP, Lindley MC, Harpaz R, et al. Barriers to the use of herpes zoster vaccine. Ann Intern Med 2010;152(9):555–560. 10.7326/0003-4819-152-9-201005040-00005. [DOI] [PubMed] [Google Scholar]
- 14.Daley MF, Hennessey KA, Weinbaum CM, et al. Physician practices regarding adult hepatitis B vaccination: a national survey. Am J Prev Med 2009;36(6):491–496. 10.1016/j.amepre.2009.01.037. [DOI] [PubMed] [Google Scholar]
- 15.Lindley MC, Hurley LP, Beaty BL, et al. Vaccine financing and billing in practices serving adult patients: a follow-up survey. Vaccine 2018;36(8):1093–1100. 10.1016/j.vaccine.2018.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Freed GL, Cowan AE, Gregory S, Clark SJ. Variation in provider vaccine purchase prices and payer reimbursement. Pediatrics 2009;124 (suppl 5):S459–S465. 10.1542/peds.2009-1542E. [DOI] [PubMed] [Google Scholar]
- 17.Henry J Kaiser Family Foundation. Health insurance coverage of adults 19–64 www.kff.org/other/state-indicator/adults-19-64/?currentTimeframe=0&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D Accessed August 21, 2018.
- 18.Centers for Medicare & Medicaid. Methodology for calculating the national average drug acquisition cost (NADAC) for Medicaid covered outpatient drugs www.medicaid.gov/medicaid-chip-program-information/by-topics/prescription-drugs/ful-nadac-downloads/nadacmethodology.pdf Published November 2013. Accessed February 12, 2019.
- 19.Ruttner L, Borck R, Nysenbaum J, Williams S. Guide to MAX data. Mathematica Policy Research 2015; Brief 21 www.cms.gov/Research-Statistics-Data-and-Systems/Computer-Data-and-Systems/Medicaid-DataSourcesGenInfo/Downloads/MAX_IB21_MAX_Data_Guide.pdf Accessed March 14, 2019.
- 20.Krishnan A, Xu T, Hutfless S, et al. Outlier practice patterns in Mohs micrographic surgery: defining the problem and a proposed solution. JAMA Dermatol 2017;153(6):565–570. 10.1001/jamadermatol.2017.1450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Centers for Disease Control and Prevention. Adult vaccine price list https://www.cdc.gov/vaccines/programs/vfc/awardees/vaccine-management/price-list/2016/2016-12-01.html#adult Published 2016. Accessed August 15, 2018.
- 22.Centers for Medicare & Medicaid Services. Medicare PFS locality configuration www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/PhysicianFeeSched/Locality.html Published 2017. Accessed February 12, 2019.
- 23.Glazner JE, Beaty B, Berman S. Cost of vaccine administration among pediatric practices. Pediatrics 2009;124(suppl 5):S492–S498. 10.1542/peds.2009-1542H. [DOI] [PubMed] [Google Scholar]
- 24.American Academy of Pediatrics. The business case for pricing vaccines www.aap.org/en-us/Documents/immunizations_thebusinesscase.pdf Revised March 2012. Accessed October 23, 2018.
- 25.National Vaccine Advisory Committee. Recommendations from the National Vaccine Advisory committee: standards for adult immunization practice. Public Health Rep 2014;129(2):115–123. 10.1177/003335491412900203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Coleman MS, Lindley MC, Ekong J, Rodewald L. Net financial gain or loss from vaccination in pediatric medical practices. Pediatrics 2009;124(suppl 5):S472–S491. 10.1542/peds.2009-1542G. [DOI] [PubMed] [Google Scholar]