Abstract
Background:
In 2006, New Jersey was the first state to mandate prenatal education and screening at hospital delivery for postpartum depression. We sought to evaluate provision of prenatal education and screening at delivery, estimate the prevalence of postpartum depressive symptoms, and identify venues where additional screening and education could occur.
Methods:
For women who delivered live infants during 2009 and 2010 in New Jersey, data on Edinburgh Postnatal Depression Scale scores assessed at hospital delivery and recorded on birth records were linked to survey data from the Pregnancy Risk Assessment Monitoring System (PRAMS), a population-based survey of mothers completed 2–8 months postpartum (n = 2,391). The PRAMS survey assesses postpartum depressive symptoms and whether the woman’s prenatal care provider discussed the signs and symptoms of perinatal depression with her, used as a proxy for prenatal education on depression.
Results:
Two-thirds (67.0%) of women reported that a prenatal care provider discussed depression with them and 89.6% were screened for depression at hospital delivery. Among the 13% of women with depressive symptoms at hospital delivery or later in the postpartum period, over a third were Women, Infants, and Children program (WIC) participants, 13% to 32% had an infant in the neonatal intensive care unit (NICU), over 80% attended the maternal postpartum check-up, and over 88% of their infants attended ≥ 1 well baby visits.
Conclusions:
Prenatal education and screening for depression at hospital delivery is feasible and results in the majority of women being educated and screened. However, missed opportunities for education and screening exist. More information is needed on how to utilize WIC, NICU, and well baby and postpartum encounters to ensure effective education, accurate diagnosis, and treatment for depressed mothers.
Introduction
DEPRESSION AFTER THE BIRTH of a child can be debilitating and may have adverse consequences for maternal-infant bonding and infant development.1 A recently published study among 10,000 women at a Pittsburgh hospital who were screened for depression with the Edinburgh Postnatal Depression Scale (EPDS) at 4–6 weeks postpartum found that 14% had possible depression, 19% of whom experienced self-harm ideation.2 Although postpartum mood disorders, including major depression, are as or more common than mood disorders among nonpregnant women, postpartum women are half as likely to seek treatment for a mood disorder.3 This statistic is especially discouraging considering that approximately half of depressed nonpregnant women of reproductive age do not receive a diagnosis or treatment.4,5 Identifying pregnant and postpartum women with depression may be the first step toward treatment. However, a 2009 national survey of obstetrician-gynecologist fellows found that only 37% reported using a validated screening instrument to detect depression in their patients.6
In 2006, through the support of its Governor and in collaboration with the Health Department, New Jersey was the first state to enact a law mandating education and screening for depression among postpartum women (New Jersey Law N.J.S.A. 26: 2–175 et seq.). The law states that prenatal care providers shall provide education to women about postpartum depression to increase detection and treatment of the disorder. Additionally, the law specifies that “physicians, nurse midwives, and other licensed healthcare professionals providing postnatal care to women shall screen new mothers for postpartum depression symptoms prior to discharge from the birthing facility and at the first few postnatal check-up visits.” In 2007, a subcommittee of the NJ Postpartum Depression Task Force recommended using the EPDS; most hospitals in New Jersey continue to administer the EPDS during the delivery hospitalization. Since 2006, Illinois and West Virginia have implemented similar perinatal depression education and screening policies, and several other states have educational mandates and awareness campaigns.7
Evaluation of New Jersey’s law could inform decisions by other states in adopting and implementing similar comprehensive laws to promote screening and education for depression. However, no information has been published on the implementation of such laws and we found only one published study examining the effectiveness of New Jersey’s mandate8. Therefore, there were three aims of this study: (1) to evaluate provision of prenatal education and screening for depression at hospital delivery; (2) to assess the prevalence of depressive symptoms experienced postpartum; and (3) to identify possible venues where additional education and screening services could take place. This information may inform clinicians, public health practitioners, and policymakers in New Jersey and other states implementing or considering similar laws of the feasibility of providing prenatal education and screening at hospital delivery and the need for additional education and screening for perinatal depression at venues that serve the needs of postpartum women and their infants.
Materials and Methods
Data sources
For women who delivered live infants during 2009 and 2010 in New Jersey, data on EPDS scores assessed at hospital delivery and recorded on confidential birth certificate records were linked to survey data from the Pregnancy Risk Assessment Monitoring System (PRAMS). PRAMS is an annual population-based, self-reported survey of postpartum women that assesses maternal behaviors and experiences before, during, and after pregnancy (www.cdc.gov/PRAMS). Each year, a stratified sample of mothers who delivered live infants in New Jersey was selected from birth certificate records. Women were mailed a questionnaire typically 2–3 months after delivery. New Jersey PRAMS staff attempt to contact nonresponders through two additional mailed questionnaires and up to 15 phone calls up to 9 months after delivery. The overall PRAMS response rate in New Jersey for 2009 and 2010 was 72.6% and 73.2%, respectively.
Depression data and screening instruments
As stated previously, New Jersey hospitals use the EPDS to screen for depressive symptoms at delivery. Both ≥ 10 and ≥ 12 are cutoff scores recommended to providers by the NJ Department of Health. For analytic purposes, we used a cutoff score of ≥ 10 on the EPDS to indicate a positive screen for depression. For a cutoff score of ≥ 10 on the EPDS, the sensitivity ranges from 59% to 81% and specificity ranges from 77% to 88% depending upon the sample.9
The New Jersey PRAMS survey assessed women’s self-report of whether the healthcare provider discussed prenatal and postpartum depression with the woman during her pregnancy with the question, “During your pregnancy, did your healthcare provider discuss with you what to do if you feel depressed during pregnancy or after your baby is born?” In addition, the PRAMS survey used a three-item screener to assess maternal depressive symptoms since the birth of the baby. The three items included: “I have felt down, depressed or sad,” “I have felt hopeless,” and “I have felt slowed down physically.” Categorical responses were based on the frequency of experiencing these feelings since the woman’s new baby was born. Responses and their associated numerical values included “never” (1), “rarely” (2), “sometimes” (3), “often” (4), or “always” (5). When the sum of the responses totaled ≥ 10, the woman was considered to have postpartum depressive symptoms, which is the recommended cutoff for surveillance purposes based on findings from a validation study of the screening instrument.10 The sensitivity and specificity of this algorithm for postpartum depression has been reported as 57% and 87%, respectively.10
Additional analytic variables
Maternal demographic and infant characteristics examined in this analysis were derived from both the birth certificate and the PRAMS survey. Items from the birth certificate included maternal age, education, race/ethnicity, and gestational age. Items from the PRAMS survey included insurance status, participation in the Women, Infants, and Children (WIC) program, infant admission to the neonatal intensive care unit (NICU), and attendance at well-baby visits and the mother’s postpartum check-up.
Statistical analyses
To evaluate our first aim—implementation of the state mandate—we examined both the percent of women who reported discussing with their provider what to do if they feel depressed during pregnancy or after their baby is born, as a proxy for prenatal education on depression, and prevalence of receipt of screening for depression at hospital delivery. For the analysis on prenatal education on depression, we limited the analysis to women who attended one or more prenatal care visits. For both analyses, we used chi-squared tests to examine whether prevalence differed by maternal demographic and infant characteristics.
To assess the second aim—prevalence of postpartum depressive symptoms—we calculated prevalence estimates for screening positive for depression at delivery hospitalization and for screening positive for depressive symptoms at 2–9 months postpartum. We also examined the extent of overlap between the two.
To fulfill our third aim, identifying additional venues where maternal education and screening for depression could take place, we examined participation in the WIC program, infant admission to the NICU, and attendance at well-baby visits and the mother’s postpartum check-up. All data were weighted for sample design, nonresponse, and noncoverage to produce estimates representative of the New Jersey population. The Centers for Disease Control and Prevention institutional review board (IRB) approved the PRAMS protocol and the New Jersey Department of Health’s IRB approved the use of the EPDS birth certificate data for use in this analysis.
Results
Sample
The EPDS scores assessed at hospital delivery were entered into the electronic birth certificate record by 42 of 53 (79.2%) New Jersey maternity hospitals, allowing coverage of 81.3% of PRAMS interviews in 2009–2010 (n = 2,391; Fig. 1). Of the 2,391 women, 272 (11.4%) were missing an individual EPDS score. Of women with an EPDS score at delivery, 107 (5.1%) were missing values for the three-item PRAMS depression screener. Therefore, a total of 2,012 women (84.1%) were included in analyses using both the delivery and postpartum depressive symptom scores, which represents 145,595 New Jersey women. Compared with the 2,391 PRAMS participants who delivered their infant in hospitals reporting EPDS scores to the NJ Health Department, the 550 PRAMS participants who delivered in hospitals not reporting an EPDS score to the NJ Health Department were more likely to be less than 25 years of age, have less than a high school education, be African American, have Medicaid insurance, and report 6–13 prenatal stressful life events (chi square p-value < 0.05 for all); there was no difference in postpartum depressive symptoms. Women in our analytic sample completed the PRAMS questionnaire at a median of 3.8 months after the birth of their child (range: 2.5 to 8 months).
FIG. 1.
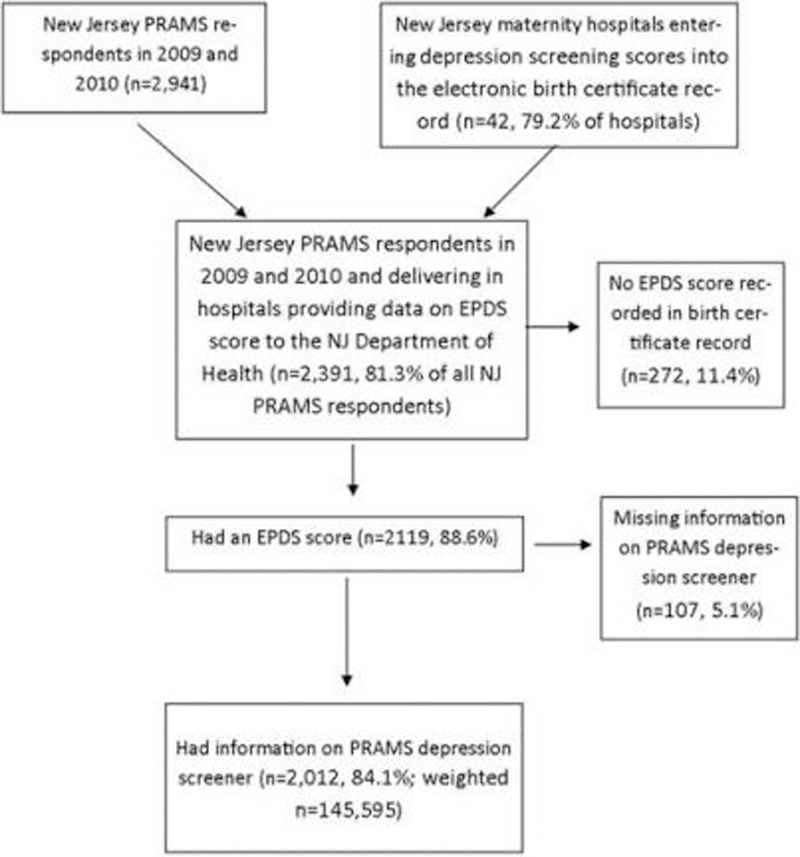
Linked data, sample sizes, and unweighted percentages from the Pregnancy Risk Assessment Monitoring System (PRAMS) and birth certificate records. EPDS, Edinburgh Postnatal Depression Scale.
Implementation of the mandate
Prenatal education on depression (reporting that a healthcare provider discussed with the woman what to do if she feels depressed during pregnancy or after her baby is born) was reported by 67.0% of the 2,280 women who attended one or more prenatal care visits (Table 1). However, report of prenatal education on depression ranged from 56.0% among women of races/ethnicities other than white, black or Hispanic, to 76.2% among women under 25 years of age. Women who were under 25 years of age, those with less education, women with Medicaid insurance, those with more prenatal stressful life events, women who wanted their child later, and those who had a preterm birth were significantly more likely than their counterparts to report that their prenatal care provider discussed perinatal depression with them (chi square p-value < 0.05 for all; Table 1). Report of prenatal education on depression did not vary by year of infant birth (Table 1) and women’s depression screening scores at delivery or postpartum (data not shown).
TABLE 1.
Prenatal Education on Depression and Depression Screening at Hospital Delivery by Maternal Demographic and Infant Characteristics
| Reported prenatal education on depressiona Weighted % (95% CI) |
Received screening for depression at hospital deliveryb Weighted % (95% CI) |
|
|---|---|---|
| Total | 66.9 (64.8, 69.0) | 89.6 (88.2, 90.8) |
| Year of infant birthd | ||
| 2009 | 66.8 (63.8, 69.7) | 87.8 (85.6, 89.6) |
| 2010 | 67.8 (64.7, 70.7) | 91.3 (89.5, 92.9) |
| Age (years)c | ||
| < 25 | 76.2 (71.9, 80.1) | 91.0 (88.1, 93.2) |
| 25–34 | 64.8 (61.9, 67.5) | 89.3 (87.5, 90.9) |
| ≥ 35 | 63.0 (58.1, 67.6) | 88.9 (85.5, 91.6) |
| Educationc | ||
| < High school | 79.2 (73.8, 83.8) | 89.9 (86.1, 92.8) |
| High school | 73.0 (69.0, 76.7) | 89.0 (86.2, 91.4) |
| > High school | 61.6 (58.7, 64.4) | 89.9 (88.1, 91.5) |
| Race/ethnicityc,d | ||
| Non-Hispanic white | 65.2 (61.7, 68.5) | 90.1 (87.9, 92.0) |
| Non-Hispanic black | 72.9 (68.3, 77.2) | 85.2 (81.4, 88.3) |
| Hispanic | 70.6 (66.3, 74.4) | 92.1 (89.5, 94.1) |
| Other | 56.0 (51.1, 60.8) | 88.3 (84.9, 91.1) |
| Medicaidc | ||
| Yes | 75.2 (71.9, 78.2) | 89.6 (87.4, 91.4) |
| No | 61.7 (58.9, 64.5) | 89.6 (87.8, 91.2) |
| Pregnancy intentionc | ||
| Did not want | 68.3 (61.1, 74.7) | 89.1 (84.2, 92.6) |
| Wanted later | 71.5 (67.6, 75.2) | 90.6 (88.0, 92.7) |
| Wanted now or sooner | 64.7 (61.9, 67.4) | 89.1 (87.2, 90.7) |
| Prenatal stressful life eventsc | ||
| 0 | 63.8 (59.7, 67.7) | 89.8 (87.1, 91.9) |
| 1–2 | 66.2 (63.0, 69.3) | 89.3 (87.2, 91.1) |
| 3–5 | 71.3 (66.5, 75.6) | 89.9 (86.7, 92.4) |
| 6–13 | 75.3 (66.0, 82.7) | 89.2 (82.0, 93.7) |
| Gestational age at birthc,d | ||
| < 37 weeks | 70.5 (62.8, 77.2) | 83.7 (77.1, 88.6) |
| ≥ 37 weeks | 66.6 (64.4, 68.8) | 90.1 (88.7, 91.3) |
n = 2,280 Women with ≥1 prenatal care visit.
Based on depressive screening score documentation in birth record; n = 2,391.
Chi-squared p-value < 0.05 for association with receipt of prenatal education on depression.
Chi-squared p-value < 0.05 for association with receipt of screening for depression at hospital delivery.
CI, confidence interval.
We found that 89.6% of women were screened for depression at hospital delivery (Table 1). Receipt of screening at delivery ranged from 85.2% among non-Hispanic black women to 92.1% among Hispanic women. Women giving birth in 2010, compared to 2009, those with full-term infants, and non-Hispanic white or Hispanic women were most likely to be screened compared to their counterparts (chi square p-value < 0.05 for all). Receipt of screening did not vary by maternal age, education, pregnancy intention, number of prenatal stressful life events, and infant admission to the NICU.
Prevalence of postpartum depressive symptoms
Of the 2,012 women in our analytic sample with depressive screening scores at hospital delivery and postpartum, 5.5% scored ≥ 10 on the EPDS at delivery hospitalization and 9.0% scored ≥ 10 on the PRAMS screener postpartum (Table 2). Overall, 87.1% of women screened negative at both delivery and postpartum, 3.9% screened positive at delivery and negative postpartum, 7.4% screened negative at delivery and positive postpartum, and 1.6% screened positive at both time points. Of the 94.5% (weighted n = 130,236) of women who screened negative on EPDS at delivery, 7.8% (weighted n = 10,209) reported depressive symptoms postpartum.
TABLE 2.
Depression Screening Results at Delivery Hospitalization and Between 2 and 8 Months Postpartum
| Postpartumb |
|||
|---|---|---|---|
| Deliverya | Positive | Negative | Total |
| % (95% CI) | % (95% CI) | % (95% CI) | |
| Positive | 1.6 (1.1, 2.3) | 3.9 (3.1, 4.9) | 5.5 (4.6, 6.7) |
| Negative | 7.4 (6.3, 8.8) | 87.1 (85.4, 88.6) | 94.5 (93.3, 95.4) |
| Total | 9.0 (7.8, 10.5) | 91.0 (88.5, 92.2) | 100 |
n = 2,012.
Depressive symptoms at delivery hospitalization based on Edinburgh Postnatal Depression Scale.
Depressive symptoms postpartum based on Pregnancy Risk Assessment Monitoring System questionnaire filled out by the mother between 2 to 8 months postpartum.
Venues for additional education and screening
Of the three groups of women with a positive screen at delivery and/or postpartum, 36.8% to 53.5% participated in the WIC program, 13.4% to 32.5% had an infant admitted to the NICU, 88.3% to 94.3% attended the first-week infant well-baby visit, 95.2% to 99.6% attended one or more well baby visits at 1, 2, 4, or 6 months, and 80.3% to 88.4% attended the maternal postpartum check-up (Table 3).
TABLE 3.
Attendance at Medical Visits and Venues Where Additional Education and Screening for Postpartum Depression Could Occur, by Depression Status at Delivery Hospitalization and at 2 to 8 Months Postpartum
| Total Weighted % (95% Cl) |
No depression at delivery or during postpartum period Weighted % (95% Cl) |
Depression at delivery only Weighted % (95% Cl) |
Depression during postpartum period only Weighted % (95% Cl) |
Depression at delivery and during postpartum period Weighted % (95% Cl) |
|
|---|---|---|---|---|---|
| WIC Participanta | 37.6 (35.5, 39.8) | 36.8 (34.5, 39.1) | 53.5 (41.8, 64.8) | 36.8 (29.0, 45.3) | 49.7 (32.5, 66.9) |
| NICU admissiona | 14.1 (12.5, 15.8) | 13.3 (11.7, 15.2) | 32.5 (22.4, 44.5) | 13.4 (8.6, 20.2) | 12.9 (5.3, 28.3) |
| Attended maternal postpartum visit | 86.7 (85.0, 88.2) | 87.2 (85.4, 88.8) | 88.4 (78.6, 94.1) | 80.3 (72.6, 86.2) | 82.6 (64.7, 92.5) |
| Attended infant visit (first week) | 94.0 (92.7, 95.1) | 94.1 (92.8, 95.3) | 92.8 (83.0, 97.2) | 94.3 (88.3, 97.3) | 88.3 (69.8, 96.1) |
| Attended at least one well-baby check-up (1, 2, 4, or 6 months) | 98.4 (97.6, 98.9) | 98.3 (97.5, 98.9) | 99.6 (97.5, 99.9) | 98.7 (95.2, 99.6) | 95.2 (72.9, 99.3) |
Depressive symptoms at delivery hospitalization based on Edinburgh Postnatal Depression Scale.
Depressive symptoms postpartum based on Pregnancy Risk Assessment Monitoring System questionnaire filled out by the mother between 2 and 8 months postpartum.
Chi square p-value<0.05.
NICU, infant neonatal infant care unit; WIC, Women, Infants, and Children program.
Discussion
Based on our findings on implementation of the law, New Jersey’s mandate of universal prenatal education on depression and screening for depressive symptoms at hospital delivery is feasible and results in the majority of women being educated and screened. Overall, we found that in 2009 and 2010, two-thirds of women delivering live births in NJ hospitals that reported EPDS data to the NJ Health Department reported that their prenatal care provider discussed with them what to do if she feels depressed during pregnancy or after her baby is born and over 89% were screened for depressive symptoms at delivery hospitalization. Regarding prenatal education on depression, the percentage of women who reported discussing the signs and symptoms of depression with their prenatal healthcare provider differed by maternal and infant characteristics. Reported rates of prenatal education on depression were lowest among women of “other” racial/ ethnic groups, at 56%. A better understanding is needed as to whether language, cultural barriers, or other issues are responsible for the low percentage. Percentages of women reporting prenatal education were also significantly lower among older women, women with more education, those with private insurance, women with fewer reported stressful life events, and those delivering full-term infants. While these groups of women may have a lower risk of depression during and after pregnancy, up to 12% screened positive on one or both depression screeners (data not shown). In regard to depression screening at hospital delivery, rates improved from 2009 (87.8%) to 2010 (91.3%), and varied by race/ethnicity and infant gestational age at birth, with non-Hispanic black women and women with preterm infants having the lowest point prevalence of screening compared to their counterparts. Further research is needed as to why these disparities in screening exist.
Published reports from the Oregon Health Authority (http://public.health.oregon.gov/HealthyPeopleFamilies/DataReports/prams/2010/Pages/dodepr.aspx) and the Alabama Department of Health (www.adph.org/healthstats/assets/PRAMS2010.pdf) show that New Jersey’s estimate of prenatal education on depression is in line with other states (Oregon: 77%; Alabama: 66%). For women who reported no prenatal education on depression, their clinicians may not have educated them about depression due to lack of time, resources, or knowledge on the topic, or women may not recall the counseling they received. It is possible that some clinicians provide educational reading materials to all women, but only discuss depression with women at high risk or those who screen positive. However, discussing the signs and symptoms of depression before symptoms begin may help women identify their symptoms and seek care before symptoms become severe. Regardless, there are missed opportunities for effectively educating all women about the signs and symptoms of postpartum depression and how to seek help when needed. More information is needed on the prevalence, best practice approach, and effectiveness of clinicians educating their pregnant patients on depression, especially from states that mandate this type of education.
There is limited published data on rates of screening for depression at hospital delivery. Although it is difficult to compare between studies due to different denominators and study designs, this figure is higher than reported rates of screening for depressive symptoms using a validated screening instrument at the maternal postpartum visit.6,11,12 In a 2009 national survey of obstetrician-gynecologist fellows agreeing to participate in surveys, only 37% reported routinely using a validated screening instrument to screen for postpartum depression.6 An earlier national survey, published in 2003, found that only 12% of new obstetrician- gynecologists and current residents identified their most recent patient with postpartum depression through routine questioning and screening results.12 At an academic hospital in North Carolina, postpartum care providers documented depression screening in only 39% of visits.11
A substantial percentage of New Jersey mothers experienced postpartum depressive symptoms, signifying a need for continued education and screening. In our sample of New Jersey women with recent live births, 13% screened positive for depressive symptoms at delivery and/or during the postpartum period, which is similar to a recent estimate of postpartum depressive symptoms.2 Of importance is the fact that over 7% of women who screened negative at hospital delivery screened positive for depressive symptoms between 2 and 8 months postpartum, which represents over 10,000 NJ mothers. The lack of agreement between the screening results at delivery and postpartum could be due to depressive symptoms beginning or resolving, with or without treatment, between hospital discharge and completion of the PRAMS survey due to changing demands on the mother across the first year postpartum; as well as differences in the questions asked, time periods covered, and binary cutoffs used between screeners; and the less than 100% sensitivity and specificity of the screeners.
Additional venues exist for education and depression screening during the postpartum period. The American College of Obstetricians and Gynecologists strongly encourages providers to screen for postpartum depression.13 The American Academy of Pediatrics recommends screening for maternal depression at the 1-, 2-, 4-, and 6-month well-child visits.14 New Jersey law mandates screening for postpartum depression at delivery prior to discharge and during postpartum maternal care. We did not have information on prevalence of screening for depression, or screening results, at the postpartum obstetric visit. As noted previously, other studies have reported low rates of using a validated screening instrument to detect postpartum depression.6,11,12 Additionally, up to 20% of women with depression at delivery and/or postpartum did not attend their maternal postpartum visit. In addition to obstetric visits, pediatric appointments, WIC visits, and NICU encounters are opportunities for education and subsequent screening. In this sample, over 95% of women’s infants attended at least one well-baby visit; a third to a half were WIC participants, and 13 to 32% had infants admitted to the NICU. Strengthening screening protocols may be needed to take advantage of women’s interactions with clinical and social services.
However, screening alone is insufficient to ensure depressed mothers receive appropriate care. The U.S. Preventive Services Task Force recommends that screening adults for depression must be coupled with procedures to ensure accurate diagnosis and treatment.15 Kozhimanill et al. found that among NJ mothers covered by Medicaid, there was no change in documented treatment after the enactment of the law.8 The authors concluded that additional efforts may be needed to ensure depressed women get treatment, such as ways to monitor and enforce the screening requirement, paying providers to screen and follow-up with women, and further research on effective interventions for depressed women. Connecting women to care is often difficult; barriers to treatment among pregnant women include cost and lack of insurance, opposition to treatment, stigma, and transportation and childcare issues5. Long wait times and lack of mental health providers also hinder receipt of treatment. Providing mental health services onsite has been shown to increase treatment utilization,16 but may not be feasible for all obstetric practices. Effective and efficient processes are needed to ensure that women who screen positive receive further assessment and treatment if needed.
This analysis has some limitations. The EPDS and PRAMS depression screeners detect depressive symptoms and have less than 100% sensitivity and specificity for identifying depression. Therefore, some women may have been inaccurately categorized. The data are not fully representative of all NJ mothers with live births, since 11 hospitals (18.7% of PRAMS-eligible births in 2009–2010) throughout the state did not provide data on EPDS score at delivery hospitalization to the NJ Department of Health. Differences were found between these groups of women, but it is difficult to evaluate whether the exclusions led to over- or underestimating the prevalence of screening or depressive symptoms at delivery. We did not have information on prevalence of depression screening at the maternal postpartum visit, nor did we have information on provision of educational materials on perinatal depression, limiting our ability to evaluate the mandate fully.
Conclusions
In summary, we found that the large majority of women delivering an infant in a New Jersey hospital included in our sample were screened for postpartum depression at hospital delivery and two-thirds reported receiving prenatal education on the signs and symptoms of depression. Additionally, a substantial percentage of women experienced depressive symptoms after delivery hospitalization, signaling a need for additional education and screening at other time points. Possible venues for education and screening for depression may include WIC and NICU encounters and well-baby visits. Additionally, more information is needed on how NJ hospitals and obstetric healthcare providers have implemented the education and screening mandates and what can be done to ensure accurate diagnosis and treatment for women who need it.
Acknowledgments
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Footnotes
Author Disclosure Statement
No competing financial interests exist.
References
- 1.O’Hara MW. Postpartum depression: What we know. J Clin Psychol 2009;65:1258–1269. [DOI] [PubMed] [Google Scholar]
- 2.Wisner KL, Sit DK, McShea MC, et al. Onset timing, thoughts of self-harm, and diagnoses in postpartum women with screen-positive depression findings. JAMA Psychiatry 2013;70(5):490–498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vesga-Lopez O, Blanco C, Keyes K, Olfson M, Grant BF, Hasin DS. Psychiatric disorders in pregnant and postpartum women in the United States. Arch Gen Psychiatry 2008;65: 805–815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Farr SL, Bitsko RH, Hayes DK, Dietz PM. Mental health and access to services among US women of reproductive age. Am J Obstet Gynecol 2010;203:542–549. [DOI] [PubMed] [Google Scholar]
- 5.Ko JY, Farr SL, Dietz PM, Robbins CL. Depression and treatment among U.S. pregnant and nonpregnant women of reproductive age, 2005–2009. J Womens Health (Larchmt) 2012;21:830–836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Leddy M, Haaga D, Gray J, Schulkin J. Postpartum mental health screening and diagnosis by obstetrician-gynecologists. J Psychosom Obstet Gynaecol 2011;32:27–34. [DOI] [PubMed] [Google Scholar]
- 7.Rhodes AM, Segre LS. Perinatal depression: a review of US legislation and law. Arch Womens Ment Health 2013;16:259–270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kozhimannil KB, Pereira MA, Harlow BL. Association between diabetes and perinatal depression among low-income mothers. JAMA 2009;301(8):842–847. [DOI] [PubMed] [Google Scholar]
- 9.Gaynes BN, Gavin N, Meltzer-Brody S, Lohr KN, Swinson T, Gartlehner G et al. Perinatal depression: Prevalence, screening accuracy, and screening outcomes. 05-E006–2. 2005. Washington, DC: U.S. Department of Health and Human Services, Agency for Healthcare Research and Quality, 2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.O’Hara MW, Stuart S, Watson D, Dietz PM, Farr SL, D’Angelo D. Brief Scales to detect postpartum depression and anxiety symptoms. J Womens Health (Larchmt) 2012;21: 1237–1243. [DOI] [PubMed] [Google Scholar]
- 11.Delatte R, Cao H, Meltzer-Brody S, Menard MK. Universal screening for postpartum depression: An inquiry into provider attitudes and practice. Am J Obstet Gynecol 2009; 200:e63–e64. [DOI] [PubMed] [Google Scholar]
- 12.Dietrich AJ, Williams JW Jr., Ciotti MC, Schulkin J, Stotland N, Rost K et al. Depression care attitudes and practices of newer obstetrician-gynecologists: a national survey. Am J Obstet Gynecol 2003;189:267–273. [DOI] [PubMed] [Google Scholar]
- 13.Committee opinion no. 453: Screening for depression during and after pregnancy. Obstet Gynecol 2010;115:394–395. [DOI] [PubMed] [Google Scholar]
- 14.Earls MF. Incorporating recognition and management of perinatal and postpartum depression into pediatric practice. Pediatrics 2010; 126(5):1032–1039. [DOI] [PubMed] [Google Scholar]
- 15.Screening for depression in adults: U.S. preventive services task force recommendation statement. Ann Intern Med 2009; 151:784–792. [DOI] [PubMed] [Google Scholar]
- 16.Yawn BP, Dietrich AJ, Wollan P, Bertram S, Graham D, Huff J et al. TRIPPD: A practice-based network effectiveness study of postpartum depression screening and management. Ann Fam Med 2012;10:320–329. [DOI] [PMC free article] [PubMed] [Google Scholar]


