Short abstract
Men who have sex with men (MSM) are at greater risk for sexually transmitted infections (STIs). Data on MSM chlamydia and gonorrhea prevalence estimates and associated risk factors are scarce. To our knowledge, this is the first study to describe the prevalence and the determinants of both chlamydia and gonorrhea infections in MSM in Portugal. We conducted a cross-sectional study using data from 1832 visits to CheckpointLX, a community-based center for screening blood-borne viruses and other STIs in MSM. Overall prevalence of chlamydia or gonorrhea in our sample was 16.05%, with 14.23% coinfection and 40.73% asymptomatic presentation among those testing positive. Anorectal infection was most common for chlamydia (67.26%), followed by urethral (24.78%) and oral (19.47%) infection. Oral infection was most common for gonorrhea (55.63%), followed by anal (51.25%) and urethral (17.50%) infection. In multivariate analyses, young age (U = 94684, p = 0.014), being foreign-born (χ2 = 11.724, p = 0.003), reporting STI symptoms (χ2 = 5.316, p = 0.021), inhaled drug use (χ2 = 4.278, p = 0.039) and having a higher number of concurrent (χ2 = 18.769, p < 0.001) or total (χ2 = 5.988, p = 0.050) sexual partners were each associated with higher rates of chlamydia or gonorrhea infection. Young and migrant MSM are a vulnerable population to STIs, as are those who use inhaled drugs and those with a higher number of concurrent or total sexual partners. Although Portugal has no guidelines on chlamydia and gonorrhea screening, our results point toward a need for greater awareness about the importance of high-frequency screening for those at increased risk (i.e., every three to six months).
Keywords: Sexually transmitted infections, men who have sex with men, chlamydia, gonorrhea
Introduction
Men who have sex with men (MSM) are at greater risk for sexually transmitted infections (STIs),1–3 which in turn cause mucosal inflammation or ulcers in the oral and anogenital areas, and increase the risk of transmission of human immunodeficiency virus (HIV).4–7
The United States of America Centers for Disease Control and Prevention recommend screening for gonorrhea, chlamydia, and syphilis at least annually for sexually active MSM at sites of contact (e.g., urethra, rectum) regardless of condom use, and every three to six months if at increased risk.8 The European AIDS Clinical Society recommends screening people living with HIV for STIs annually.9 The Portuguese General Directorate for Health recommends screening users of pre-exposure prophylaxis for HIV (PrEP) for gonorrhea, chlamydia, and syphilis at treatment onset and quarterly thereafter.10 No such recommendations exist in Portugal for screening of asymptomatic MSM otherwise not on PrEP.
In Portugal, STIs are part of a list of compulsory notifiable communicable diseases. In 2016 alone, there were 1040 notified cases of HIV (370, 35.6% in MSM), 181 cases of hepatitis B (112, 61.9% in men), 281 cases of hepatitis C (220, 78.3% in men), 773 cases of syphilis (564, 73.0% in men), 474 cases of gonorrhea (419, 88.4% in men), and 195 cases of infection by Chlamydia trachomatis excluding lymphogranuloma venereum (LGV) (117, 60.0% cases in men).11
Gonorrhea is caused by the infection with Neisseria gonorrhoeae and transmission can occur by direct inoculation of infected mucosal secretions.12 Extragenital gonorrhea may be missed, as anorectal and oropharyngeal infections are usually asymptomatic.12–15 Chlamydia is a similarly behaving and equally concerning infection, with frequently asymptomatic clinical presentation that renders chains of infection transmission harder to break. Undiagnosed gonorrhea or chlamydia infections are public health threats as they contribute to increased transmission of HIV, and increased incidence of the diseases.14,16,17
Few studies exist on the determinants of STIs other than HIV in MSM in Portugal. The Lisbon cohort of MSM is an open prospective cohort started in April 2011, and the first to characterize HIV infection and its determinants in this group.18 At entry to the cohort, 2.5% MSM had a diagnosis of gonorrhea during the previous 12 months, and 0.9% had a diagnosis of chlamydia in the same period. A different Lisbon walk-in STI clinic targeted at the general population recorded 157 diagnosed cases of gonorrhea in MSM between 2014 and 2016, though the data were not analyzed to include factors, which could be associated with the infection. Of the overall reported diagnoses of gonorrhea, exclusively extragenital disease accounted for the majority of cases (82%), with the highest proportion isolated in the anorectal site (57%).15 A third STI clinic reported 902 cases of anogenital condyloma between 2008 and 2014, of which 18.4% were diagnosed in MSM.19 Another study conducted in a community clinic in Lisbon between 2008 and 2013 found 238 cases (9.8%) of gonorrhea and 158 (6.5%) of chlamydia.20 Considering the ones who were infected, anorectal infection occurred in 38 (16%) of the ones infected by gonorrhea and 23 (14.6%) of the ones infected by chlamydia. Anorectal infection was more common in MSM with prior history of STIs, multiple partners, and immigrants.20 Community-based studies conducted in STI clinics targeted at MSM present an opportunity to better understand and cater to the needs of this population.
Objective
This study aims to characterize the prevalence and determinants of chlamydia and gonorrhea in a community clinic targeted at MSM.
Materials and methods
Data collection
Data for this cross-sectional study were collected at CheckpointLX, a community-based sexual health center managed by Grupo de Ativistas em Tratamentos (GAT) Portugal, a nongovernmental organization. CheckpointLX is the only STI clinic targeted exclusively at MSM in Portugal, working as a low threshold walk-in clinic offering rapid testing for blood-borne viruses and syphilis, and also as an outpatient clinic for screening of other STIs. During appointments, qualified peers (MSM nurses and physicians) conduct a health questionnaire, recording sociodemographic information (including gender), medical history, behavioral data (including sexual behavior), and risk factors for STIs. Appropriate samples are collected for point of care rapid testing for HIV, syphilis, hepatitis B and C, and for laboratory testing of other STIs, including gonorrhea, chlamydia, LGV, Mycoplasma genitalium, human papilloma virus (HPV) and anal intraepithelial neoplasia, many of which are not available elsewhere for men. Anal and urethral site testing began in 2012. Oral site tests were added in 2016. Culture detection methods were discontinued as first-line tests for gonorrhea from 2018 onwards, and only performed when nucleic acid amplification tests with real-time polymerase chain reaction (NAAT RT-PCR) yielded positive results.
Samples are sent to public external laboratories Instituto de Higiene e Medicina Tropical, Instituto Nacional de Saúde Doutor Ricardo Jorge and Instituto Português de Oncologia de Lisboa Francisco Gentil. Results are sent back to CheckpointLX and registered into a coded database. Service users are notified via email and offered free access to CheckOUT, a proprietary and standardized anonymous partner notification tool. Returning users are subject to repeat health questionnaires, and the data are linked to previous records upon consent, as authorized by the Portuguese Data Protection Commission (no. 3207/2017).
Participant selection
As depicted in Figure 1, we examined data from 1942 visits to CheckpointLX between May 2012 and May 2018, excluding 92 entries with incomplete data regarding STI diagnosis, and 18 entries tested for other STIs but not gonorrhea or chlamydia (e.g., syphilis alone). For comparison between infected and noninfected participants, the total sample consisted of 1832 fully completed records. The main outcome measures were gonorrhea or chlamydia infection. We also collected information on socio-demographics and detailed sexual practices and substance use habits.
Figure 1.
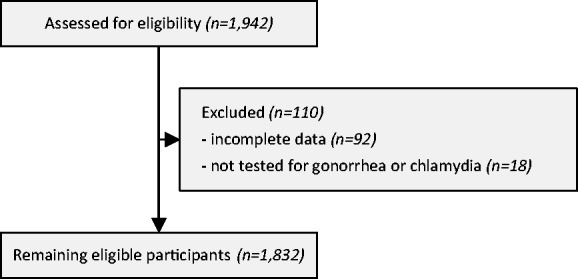
Flow diagram depicting participant selection.
Data analysis
Shapiro–Wilk normality test was used on continuous variables, and Mann–Whitney U or two-sided t-tests were performed accordingly. Pearson chi-square was used for comparison of categorical variables between groups. P values less than 0.05 (two-tailed) were considered statistically significant. Data were analyzed using R, version 3.5.1.
Results
Study population
Data from 1832 patient visits were considered for this study, of which 1263 were first-time appointments (68.94%) and 501 were follow-up visits (27.35%), with other types of visits (for communicating the results and/or for counseling only) accounting for the remainder 3.71%. The main reason for seeking an appointment was routine checkup (796, 43.45%), followed by presenting with signs or symptoms of an STI over the last 12 months (277, 15.12%), having a sexual partner with a recent STI diagnosis (205, 12.19%) or receiving an HIV reactive rapid test result (134, 7.31%). Users could indicate more than one reason, and data were missing in 377 (20.58%) entries of the sample.
The mean age of the sample was 33.26 years (9.51 standard deviation), and most were born in Portugal (N = 1264, 69.00%), followed by those born in Brazil (N = 213, 11.63%). Data were missing for age, country, and gender in 90 (4.91%), 94 (5.13%), and 89 (4.86%) entries, respectively. Table 1 summarizes high-level characteristics of the study population.
Table 1.
Sociodemographic characteristics of the study population.
| Age | M (SD) | Median (Interval) |
|---|---|---|
| Years of age | 33.26 (9.51) | 31 (16-69) |
| Gender | N | % |
| Men | 1,741 | 95.03 |
| Trans women (M to F) | 2 | 0.11 |
| Missing data | 89 | 4.86 |
| Country of origin | N | % |
| Portugal | 1,264 | 69.00 |
| Brazil | 213 | 11.63 |
| Other (54 countries)a | 261 | 14.25 |
| Missing data | 94 | 5.13 |
Other countries: South Africa, Germany, Angola, Argentina, Australia, Austria, Bangladesh, Belgium, Bolivia, Bulgaria, Cape Verde, Canada, Chile, China, Colombia, South Korea, Cuba, Denmark, Spain, USA, Estonia, Philippines, France, Ghana, Greece, Guinea Bissau, Netherlands, Ireland, Israel, Italy, Jamaica, Lebanon, Malaysia, Maldives, Mexico, Mozambique, Nepal, Norway, Pakistan, Poland, Kyrgyzstan, UK, Romania, Russia, Serbia, Syria, Sweden, Switzerland, Tanzania, Timor-Leste, Turkey, Ukraine, Uruguay, and Venezuela.
Chlamydia and gonorrhea infection
To adequately control for a possible underestimation of prevalence or skewed anatomical site distribution due to the lack of oral site testing prior to 2016, we limited calculations of prevalence to data from patients tested from all three anatomical sites, from 2016 onwards (N = 1489, from the overall N = 1832 entries).
A total of 1250 (83.95%) participants had negative test results for both chlamydia and gonorrhea, and 239 (16.05%) tested positive for at least one of the infections, with 34 (14.23%) cases of coinfection with both bacteria. A total of 113 cases of chlamydia (including LGV strains) and 160 cases of gonorrhea were diagnosed in this sample, yielding an overall prevalence of chlamydia in our sample of 7.59% and prevalence of gonorrhea of 10.75%, accounting for all anatomical sites, alone or combined.
Table 4 details the number of infections by anatomical site. The most frequent site for chlamydia infection was anorectal infection (67.26%), followed by urethral infection (24.78%) and oral infection (19.47%). Anorectal coinfection with other sites was found in some cases (8.85%), half of which corresponded to simultaneous anal and oral coinfection.
As for gonorrhea, the most frequent site was oral infection (55.63%), followed by anal infection (51.25%) and urethral infection (17.50%). Here too, anal coinfection with other anatomical sites was found in several cases (20.63%), over half of which corresponded to anal and oral coinfection, as with chlamydia.
Gonorrhea diagnostic methods
Table 2 details the testing sensitivity of the diagnostic methods used for gonorrhea. Of entries testing positive for gonorrhea, 123 were subject to both NAAT RT-PCR and culture detection methods, while the remaining 62 were subject to NAAT RT-PCR alone.
Table 2.
Diagnostic methods sensitivity for gonorrhea.
| False negative at any site N (%) | True positive at any site N (%) | |
|---|---|---|
| NAAT RT-PCR | 3 (2.44) | 120 (97.56) |
| Culture | 93 (75.61) | 30 (24.39) |
|
|
False negative at same site N (%) |
True positive at same site N (%) |
| NAAT RT-PCR | 11 (8.94) | 112 (91.06) |
| Culture | 108 (87.80) | 15 (12.20) |
NAAT RT-PCR: nucleic acid amplification tests with real-time polymerase chain reaction.
We analyzed the 123 entries subject to both testing methods at the same laboratory to compare their real-world sensitivities. NAAT RT-PCR methods failed to detect gonorrhea infection in 3 (2.44%) samples with a positive culture at any site, while culture failed to detect gonorrhea infection in 93 (75.61%) samples with a positive NAAT RT-PCR result at any site.
Of the 30 positive cultures for gonorrhea, none demonstrated antibiotic resistance (0, 0.0%).
Correlates of infection
Table 3 details the correlates of chlamydia and gonorrhea positivity in our sample. We compared data entries with recorded negative results to entries testing positive for either chlamydia or gonorrhea. Service users testing positive for either infection registered a slightly younger average age of 31.99 years old (U = 94684, p = 0.014), compared to 33.48 years old for those testing negative. We also found statistically significant associations between infection with either chlamydia or gonorrhea and country of birth (χ2 = 11.724, p = 0.003), reporting STI symptoms (χ2 = 5.316, p = 0.021), inhaled drug use (χ2 = 4.278, p = 0.039), and having a higher number of concurrent (χ2 = 18.769, p < 0.001) or total (χ2 = 5.988, p = 0.050) sexual partners.
Table 3.
Correlates of chlamydia or gonorrhea infection.
| Characteristics/group | Infection | Non-Infection | χ2 p value | ||
|---|---|---|---|---|---|
| Socio-demographics | |||||
| Type of visit | |||||
| 1st visit | 191 | 15.1% | 1072 | 84.9% | χ2 = 0.688 p = 0.407 |
| Follow-up | 68 | 13.6% | 433 | 86.4% | |
| Country of birth | |||||
| Portugal | 168 | 13.3% | 1096 | 86.7% | χ2 = 11.724 p = 0.003 |
| Brazil | 44 | 20.7% | 169 | 79.3% | |
| Other* | 50 | 19.2% | 211 | 80.8% | |
| Gender identity | |||||
| Man | 261 | 15.0% | 1480 | 85.0% | χ2 = 1.917 p = 0.166 |
| Trans | 1 | 50.0% | 1 | 50.0% | |
| Sexual orientation | |||||
| Homosexual | 209 | 15.7% | 1123 | 84.3% | χ2 = 0.042 p = 0.838 |
| Bisexual | 14 | 14.9% | 80 | 85.1% | |
| STI history | |||||
| HIV coinfection | |||||
| Yes | 35 | 18.2% | 157 | 81.8% | χ2 = 2.102 p = 0.147 |
| No | 177 | 14.2% | 1066 | 85.8% | |
| History of STI of any kind | |||||
| Yes | 91 | 16.6% | 457 | 83.4% | χ2 = 0.677 p = 0.411 |
| No | 130 | 15.0% | 738 | 85.0% | |
| Symptoms of STI of any kind | |||||
| Yes | 147 | 16.7% | 734 | 83.3% | χ2 = 5.316 p = 0.021 |
| No | 112 | 12.8% | 764 | 87.2% | |
| Sexual practices | |||||
| Sexual partners during prior 12 months | |||||
| 0 | 0 | 0.0% | 4 | 100.0% | χ2 = 5.988 p = 0.050 |
| 1-10 | 122 | 13.2% | 805 | 86.8% | |
| 10+ | 135 | 17.1% | 653 | 82.9% | |
| Role in anal intercourse | |||||
| Receptive | 28 | 14.8% | 161 | 85.2% | χ2 = 1.509 p = 0.680 |
| Insertive | 41 | 13.6% | 261 | 86.4% | |
| Both | 183 | 15.2% | 1018 | 84.8% | |
| None | 4 | 23.5% | 13 | 76.5% | |
| Reported consistent condom use in all anal sexual practices | |||||
| Yes | 62 | 13.6% | 394 | 86.4% | χ2 = 0.939 p = 0.333 |
| No | 184 | 15.5% | 1003 | 84.5% | |
| Ejaculation in mouth | |||||
| Yes | 111 | 16.6% | 557 | 83.4% | χ2 = 0.813 p = 0.367 |
| No | 112 | 14.9% | 641 | 85.1% | |
| Oral-anal sex (i.e., oral stimulation of the anus) | |||||
| Yes | 165 | 16.2% | 853 | 83.8% | χ2 = 0.013 p = 0.909 |
| No | 55 | 15.9% | 290 | 84.1% | |
| Concurrent sexual intercourse with more than one partner | |||||
| Yes | 113 | 21.2% | 421 | 78.8% | χ2 = 18.769 p < 0.001 |
| No | 111 | 12.5% | 776 | 87.5% | |
| Fisting (i.e., introduction of the hand below the knuckles in the rectum) | |||||
| Yes | 26 | 19.4% | 108 | 80.6% | χ2 = 1.456 p = 0.228 |
| No | 198 | 15.4% | 1087 | 84.6% | |
| Anal douching (i.e., introduction of liquids in the rectum for cleaning purposes) | |||||
| Yes | 99 | 17.2% | 476 | 82.8% | χ2 = 1.561 p = 0.212 |
| No | 125 | 14.8% | 722 | 85.2% | |
| Substance use | |||||
| Tobacco smoking of any frequency | |||||
| Yes | 79 | 14.7% | 459 | 85.3% | χ2 = 0.600 p = 0.439 |
| No | 145 | 16.2% | 749 | 83.8% | |
| Alcohol use of any frequency | |||||
| Yes | 208 | 16.1% | 1084 | 83.9% | χ2 = 2.001 p = 0.157 |
| Injected drug use | |||||
| No | 16 | 11.5% | 123 | 88.5% | χ2 = 3.585 p = 0.058 |
| Yes | 8 | 28.6% | 20 | 71.4% | |
| No | 216 | 15.4% | 1184 | 84.6% | |
| Inhaled drug use (e.g., cocaine, alkyl nitrites) | |||||
| Yes | 79 | 18.8% | 342 | 81.2% | χ2 = 4.278 p = 0.039 |
| No | 145 | 14.4% | 862 | 85.6% | |
| Tattoos without asepsis | |||||
| Yes | 13 | 21.3% | 48 | 78.7% | χ2 = 1.518 p = 0.218 |
| No | 211 | 15.4% | 1155 | 84.6% | |
STI: sexually transmitted infections.
Other countries are the following: Angola, Argentina, Australia, Bangladesh, Belgium, Cape Verde, Colombia, Cuba, Estonia, France, Germany, Ireland, Israel, Italy, Jamaica, Kyrgyzstan, Mozambique, Nepal, Pakistan, Poland, Spain, Sweden, Switzerland, UK, USA, and Venezuela.
Table 4.
Positive test results by infection site, 2016–2018.
| Infection site | Chlamydia | Gonorrhea |
|---|---|---|
| N (%) | N (%) | |
| Urethral only | 23 (20.35) | 15 (9.38) |
| Anal only | 66 (58.41) | 49 (30.63) |
| Oral only | 13 (11.50) | 61 (38.13) |
| Urethral + anal | 2 (1.77) | 7 (4.38) |
| Urethral + oral | 1 (0.88) | 2 (1.25) |
| Anal + oral | 6 (5.31) | 22 (13.75) |
| Oral + anal + urethral | 2 (1.77) | 4 (2.50) |
| Total oral | 22 (19.47) | 89 (55.63) |
| Total urethral | 28 (24.78) | 28 (17.50) |
| Total anal | 76 (67.26) | 82 (51.25) |
| Total | 113 (100.00) | 160 (100.00) |
It was found that 20.7% Brazilian-born service users had at least one infection, as compared to 13.3% of Portuguese-born users or 19.2% for all other 54 countries combined. While 17.1% of service users reporting more than 10 total sexual partners during the previous 12-month period tested positive for chlamydia or gonorrhea, the proportion of positive test results dropped to 13.2% in those with fewer than 10 sexual partners in the same period. Similarly, 21.2% of those engaging in sexual intercourse with more than one concurrent partner had at least one of the infections, while only 12.5% of those not doing so had an infection. Finally, 18.8% of those reporting inhaled drug use in the past year had an infection, against 14.4% of those not doing so. Our study failed to demonstrate statistically significant associations between infection and all other correlates.
Discussion
The Portuguese Directorate-General for Health publishes a summary yearly report with the number of notified cases of chlamydia and gonorrhea by age, sex and place of residence, but no further characterizing information is available on the cases. Access to further information, such as country of birth and sexual practices would be useful to understand the evolution of the diseases, and to offer targeted and efficient prevention and screening programs.
To our knowledge, this is one the first studies analyzing the prevalence of both chlamydia and gonorrhea in a community setting in Portugal, in MSM or otherwise. Previous studies identified STI diagnoses in MSM but did not further analyze data for this population.
Although other STI clinics exist in Portugal, they are targeted at the general population, which some regard as an access barrier to MSM sexual health services for fear of stigma and discrimination. CheckpointLX’s modus operandi and nearly decade-long existence represent an invaluable opportunity to study this population closely, as the clinic’s databases have accumulated a sizeable wealth of information to work on.
MSM attending CheckpointLX’s STI clinic in the 6-year period we analyzed had a mean age of 33.26 years, consistent with other studies.21 Most service users were born in Portugal (69.00%), followed by Brazil (11.63%), the second most represented country in our sample.
Almost half of the service’s users stated routine checkup as the main reason for seeking an appointment (43.45%). This is a positive finding, signaling MSM population awareness of the importance of routine STI screening, in line with international health authority recommendations.
Regarding diagnostic methods, CheckpointLX’s sample points toward a high performance of molecular methods for the diagnosis of gonorrhea infections, with 97.56% sensitivity, as opposed to poor performance of culture methods, with 24.39% sensitivity for the same purpose. While these results are in line with known literature,22 they ought to be interpreted with caution, as despite low sensitivity, culture still stands as the only easily accessible method to assess antibiotic resistance, which is an increasing concern surrounding gonorrhea infection,23 although it has yet to be identified in Portugal, including in this study.
The prevalence of chlamydia (7.59%) and gonorrhea (10.75%) in this sample was consistent with that found in studies conducted in similar settings. Of note, overall anorectal infection, either alone or in combination with other sites, remains an important finding in those testing positive for either gonorrhea (51.25%) or chlamydia (67.26%). This consideration is important in the provision of treatment of these infections, as literature points to potentially diminished antibiotic efficacy according to infection site.24,25 Coinfection with both bacteria among those testing positive was also relevant (14.23%), as was asymptomatic clinical presentation (40.73%), indicating the need for enhanced comprehensive prevention approaches.
When compared to the national chlamydia to gonorrhea infection ratio of 1:2.4, our study population registered a 1:1.4 chlamydia to gonorrhea infection ratio, signaling a proportionately higher number of cases of chlamydia than expected. Although these figures need to be interpreted with caution, this finding raises important questions regarding different relative risks of infection with Chlamydia trachomatis in the general population versus MSM. These differences might be due to multiple factors, such as different sexual practices or different number of sexual partners.
Our analysis found young age (U = 94684, p = 0.014) and being born outside of Portugal (χ2 = 11.724, p = 0.003) were significantly associated with testing positive for chlamydia or gonorrhea. It is a known fact that migrants represent a vulnerable subpopulation of MSM among new cases of HIV in Portugal.26 In our sample, we found that foreign-born service users (particularly those born in Brazil) were at increased risk for testing positive for chlamydia or gonorrhea when compared to Portuguese-born users. This is in line with another study conducted in a Lisbon STI walk-in clinic.15 Therefore, strategies for addressing outreach, prevention and early diagnosis of STIs in this particular population should be considered, while avoiding stigmatization and discrimination. Measuring and minimizing stigma is of high importance, as it can have an impact on health coverage on key populations.27
Although those with HIV coinfection or a history of a previous STI of any kind in the past 12-month period had higher rates of infection, our study failed to demonstrate a statistically significant association. Likewise, while those engaging in all purportedly high-risk sexual practices analyzed in this study had higher rates of infection, these associations were not statistically significant. However, while we were unable to establish a statistically significant association between infection and specific sexual practices, we found significant associations between infection and having a higher number of concurrent (χ2 = 18.769, p < 0.001) or total (χ2 = 5.988, p = 0.050) sexual partners.
Within substance use, those reporting all habits but smoking had higher rates of infection (i.e., alcohol or injected drug use), but only inhaled drug use (χ2 = 4.278, p = 0.039) was significantly associated with higher prevalence. For clarity, in CheckpointLX’s questionnaire, both use of cocaine and alkyl nitrites (i.e., “poppers”) elicit positive answers, and questions on substance use do not differentiate recreational use from use during sex, which is a limiting factor of this analysis. We ran additional chi-square goodness-of-fit analyses to learn there was a statistically significant association between inhaled drug use and multiple concurrent sexual partners (χ2 = 78.950, p < 0.001), with 55.26% of those using inhaled substances engaging in sexual intercourse with more than one concurrent partner in the prior 12-month period, while 30.21% of those not using inhaled substances did so. We hypothesize the use of these substances might be either facilitated during or facilitating of sexual intercourse with more than one concurrent partner.
These findings empirically demonstrate something those working in the field have long known to be true: within the MSM subgroup, the size of one’s sexual network and the number of connections within that network28 seem to pose a greater risk for infection with an STI than the particular sexual practices taking place, by sheer virtue of repeated exposure.
Finally, interestingly enough, those reporting consistent condom use during anal sex in our sample failed to demonstrate significantly lower rates of gonorrhea or chlamydia. Although condom use has been an invaluable tool in fighting HIV, its effectiveness in preventing other STIs has increasingly come into question. It does not adequately prevent HPV29 nor hepatitis A virus (HAV) infection,30 as both viruses can infect areas not covered by a condom. In our sample, although there was high reported condom use, gonorrhea and chlamydia transmission still occurred. We theorize this might be due to the role of sexual acts other than penetration in spreading these infections, such as oral–penile and oral–anal sex, where the use of condoms or dental dams is negligible.31 While promoting condom use should continue to be a staple of STI prevention programs, we conclude that comprehensive prevention strategies are needed, including a broader view of the sex acts taking place and further exploration of the roles of chemoprophylaxis, including PrEP for HIV prevention and doxycycline for gonorrhea, chlamydia and syphilis,32 as well as enhanced screening policies for STIs.
Our study has important limitations. The first one is selection bias. Men who use CheckpointLX are likely to have higher levels of health literacy and more access to healthcare services and could therefore be at less risk for STIs. Reporting bias should also be considered, as all information but test results are self-reported. Although the database is in Portuguese, some appointments are carried out in foreign languages, which represent an additional bias introduced by the interviewer. Our data have a considerable number of missing values on behavioral variables, which made the analysis of correlates of chlamydia and gonorrhea infection more difficult. Lastly, due to the rudimentary design and/or application of the health questionnaire data collection tool, it was not possible to adequately control for the effect of repeat visits from the same individuals, as there were instances of misidentification of repeat patients.
Conclusion
To the best of our knowledge, our study is one of the few to describe the prevalence and determinants of chlamydia and gonorrhea infection in MSM in Portugal. According to our analysis, young and migrant MSM are a vulnerable population to STIs, as are those with a higher number of concurrent or total sexual partners, and those who use inhaled drugs.
We analyzed purportedly high-risk sexual practices and substance use habits to better understand their roles in shaping personal risk for STIs. Rather than stigmatizing behaviors, we seek to produce information that empowers individuals to make good health decisions and ensure pleasurable and safer sexual experiences, as per the WHO’s definition of sexual health.33
MSM at increased risk for STIs ought to be aware of the importance of high-frequency screening (i.e., every three to six months). Portugal has no guidelines on chlamydia and gonorrhea screening, and screening practices are unequal across the country. More research is needed to inform public health policies for comprehensive prevention, diagnosis, and treatment of STIs.
Key messages
Prevalence of chlamydia or gonorrhea in our sample was 16.05%, with 14.23% coinfection and 40.73% asymptomatic presentation.
Higher prevalence was found in young and migrant MSM, those with higher number of concurrent or total sexual partners, and those who use inhaled drugs.
Our results point toward a need for greater awareness about the importance of high-frequency STI screening for MSM at increased risk.
Acknowledgements
The authors would like to thank the staff working at GAT, especially at CheckpointLX, and INSA and IHMT for the support given to this manuscript.
Authors’ note
Authors Sofia Ribeiro, Diogo de Sousa, and Diogo Medina contributed equally.
Declaration of conflicting interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1.Remis RS, Liu J, Loutfy MR, et al. Prevalence of sexually transmitted viral and bacterial infections in HIV-positive and HIV-negative men who have sex with men in Toronto. Baral S, editor. PLoS One 2016; 11: e0158090, http://plos.org/10.1371/journal.pone.0158090 (2016, accessed 8 August 2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pathela P, Braunstein SL, Schillinger JA, et al. Men who have sex with men have a 140-fold higher risk for newly diagnosed HIV and syphilis compared with heterosexual men in New York City. JAIDS J Acquir Immune Defic Syndr 2011; 58: 408–416, http://www.ncbi.nlm.nih.gov/pubmed/21857351 (2011, accessed 8 August 2018) [DOI] [PubMed] [Google Scholar]
- 3.Wolitski RJ, Fenton KA. Sexual health, HIV, and sexually transmitted infections among gay, bisexual, and other men who have sex with men in the United States. AIDS Behav 2011; 15: 9, http://www.ncbi.nlm.nih.gov/pubmed/21331797 (2011, accessed 8 August 2018). [DOI] [PubMed] [Google Scholar]
- 4.Galvin SR, Cohen MS. The role of sexually transmitted diseases in HIV transmission. Nat Rev Microbiol 2004; 2: 33–42, http://www.ncbi.nlm.nih.gov/pubmed/15035007 (2014, accessed 8 August 2018). [DOI] [PubMed] [Google Scholar]
- 5.Peters RP, Verweij SP, Nijsten N, et al. Evaluation of sexual history-based screening of anatomic sites for chlamydia trachomatis and Neisseria gonorrhoeae infection in men having sex with men in routine practice. BMC Infect Dis 2011; 11: 203, http://www.ncbi.nlm.nih.gov/pubmed/21791061 (accessed 7 August 2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Benn PD, Rooney G, Carder C, et al. Chlamydia trachomatis and Neisseria gonorrhoeae infection and the sexual behaviour of men who have sex with men. Sex Transm Infect 2007; 83: 106, http://www.ncbi.nlm.nih.gov/pubmed/17020893 (2007, accessed 7 August 2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Morris SR, Klausner JD, Buchbinder SP, et al. Prevalence and incidence of pharyngeal gonorrhea in a longitudinal sample of men who have sex with men: the EXPLORE study. Clin Infect Dis 2006; 43: 1284–1289, http://www.ncbi.nlm.nih.gov/pubmed/17051493 (2006, accessed 7 August 2018). [DOI] [PubMed] [Google Scholar]
- 8.CDC. Sexually transmitted diseases treatment guidelines, 2015. MMWR 2015; 64: 1–37, https://www.cdc.gov/mmwr/preview/mmwrhtml/rr6403a1.htm (2015, accessed 7 August 2018). [Google Scholar]
- 9.EACS. European Guidelines for treatment of HIV-positive adults in Europe version 9.0. 2017. [Internet]. 2017, http://www.eacsociety.org/files/guidelines_9.0-english.pdf (2017, accessed 19 September 2018).
- 10.Direção-Geral da Saúde, Ministério da Saúde. Norma 025/2017 atualizada a 16/05/2018. Profilaxia de Pré-exposição da Infeção por VIH no Adulto [Internet]. 2018, https://www.dgs.pt/directrizes-da-dgs/normas-e-circulares-normativas/norma-n-0252017-de-28112017-pdf.aspx (2018, accessed 8 August 2018).
- 11.Gaspar C, Augusto G, Albuquerque M, et al. Doenças de Declaração Obrigatória 2013-2016, Volume I—Portugal. Direção-Geral da Saúde, 2017, https://comum.rcaap.pt/handle/10400.26/22529 (2017, accessed 27 May 2018).
- 12.Bignell C, Unemo M, Radcliffe K, et al. 2012 European guideline on the diagnosis and treatment of gonorrhoea in adults. Int J STD AIDS 2013; 24: 85–92, http://www.ncbi.nlm.nih.gov/pubmed/24400344 (2013, accessed 8 August 2018). [DOI] [PubMed] [Google Scholar]
- 13.Dudareva-Vizule S, Haar K, Sailer A, et al. Prevalence of pharyngeal and rectal Chlamydia trachomatis and Neisseria gonorrhoeae infections among men who have sex with men in Germany. Sex Transm Infect 2014; 90: 46–51, http://www.ncbi.nlm.nih.gov/pubmed/23920398 (2014, accessed 8 August 2018). [DOI] [PubMed] [Google Scholar]
- 14.Lutz AR. Screening for asymptomatic extragenital gonorrhea and chlamydia in men who have sex with men: significance, recommendations, and options for overcoming barriers to testing. LGBT Heal 2015; 2: 27–34, http://www.ncbi.nlm.nih.gov/pubmed/26790015 (2015, accessed 8 August 2018) [DOI] [PubMed] [Google Scholar]
- 15.Valejo Coelho MM, Matos-Pires E, Serrão V, et al. Extragenital gonorrhoea in men who have sex with men: a retrospective study in a STI clinic in Lisbon, Portugal. Acta Med Port 2018; 31: 247, https://www.actamedicaportuguesa.com/revista/index.php/amp/article/view/10146 (2018, accessed 14 June 2018). [DOI] [PubMed] [Google Scholar]
- 16.Hui B, Fairley CK, Chen M, et al. Oral and anal sex are key to sustaining gonorrhoea at endemic levels in MSM populations: a mathematical model. Sex Transm Infect 2015; 91: 365–369, http://www.ncbi.nlm.nih.gov/pubmed/25596192 (2015, accessed 7 August 2018). [DOI] [PubMed] [Google Scholar]
- 17.Annan NT, Sullivan AK, Nori A, et al. Rectal chlamydia—a reservoir of undiagnosed infection in men who have sex with men. Sex Transm Infect 2009; 85: 176–179, http://www.ncbi.nlm.nih.gov/pubmed/19176570 (2009, accessed 7 August 2018). [DOI] [PubMed] [Google Scholar]
- 18.Meireles P, Lucas R, Martins A, et al. The Lisbon cohort of men who have sex with men. BMJ Open. British Medical Journal Publishing Group 2015; 5: e007220, http://www.ncbi.nlm.nih.gov/pubmed/25967995 (2015, accessed 27 December 2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gameiro A, Alves J, Santo I, et al. Condilomas Anogenitais numa Consulta de Doenças Sexualmente Transmissíveis: Centro de Saúde da Lapa - Lisboa, 2008 a 2014. Acta Med Port 2016; 29: 101, http://www.actamedicaportuguesa.com/revista/index.php/amp/article/view/6402 (2016, accessed 27 December 2017). [DOI] [PubMed] [Google Scholar]
- 20.Alves J, Azevedo J, Santo I, et al. Proctite e Infeção Anoretal por Chlamydia trachomatis e Neisseria gonorrhoeae em HSH—Estudo Retrospetivo. spdv 2016; 74: 59, https://revista.spdv.com.pt/index.php/spdv/article/view/516 (2016, accessed 22 December 2018). [Google Scholar]
- 21.Remis RS, Liu J, Loutfy MR, et al. Prevalence of sexually transmitted viral and bacterial infections in HIV-positive and HIV-negative men who have sex with men in Toronto. Baral S, editor. PLoS One 2016; 11: e0158090, http://plos.org/10.1371/journal.pone.0158090 (2016, accessed 31 May 2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.CDC. Recommendations for the laboratory-based detection of Chlamydia trachomatis and Neisseria gonorrhoeae. MMWR 2014; 63: 1–19, https://www.cdc.gov/mmwr/preview/mmwrhtml/rr6302a1.htm (2014, accessed 7 August 2018). [PMC free article] [PubMed] [Google Scholar]
- 23.Michaela D, Cole M, Unemo M, et al. Gonococcal antimicrobial susceptibility surveillance in Europe, 2016, https://www.ecdc.europa.eu/sites/portal/files/documents/EURO-GASP-report-2016.pdf (2016, accessed 19 September 2018).
- 24.Hathorn E, Opie C, Goold P. What is the appropriate treatment for the management of rectal Chlamydia trachomatis in men and women?. Sex Transm Infect 2012; 88: 352–354, http://www.ncbi.nlm.nih.gov/pubmed/22517887 (2012, accessed 7 August 2018). [DOI] [PubMed] [Google Scholar]
- 25.Steedman NM, McMillan A. Treatment of asymptomatic rectal Chlamydia trachomatis : is single-dose azithromycin effective?. Int J STD AIDS 2009; 20: 16–18, http://www.ncbi.nlm.nih.gov/pubmed/19103887 (2009, accessed 7 August 2018). [DOI] [PubMed] [Google Scholar]
- 26.Direção-Geral da Saúde, Ministério da Saúde. Infeção VIH e SIDA | Desafios e estratégias [Internet]. 2018, http://www.dgs.pt/documentos-e-publicacoes/infecao-vih-e-sida-desafios-e-estrategias-2018.aspx (2018, accessed 8 December 2018).
- 27.Stahlman S, Hargreaves JR, Sprague L, et al. Measuring sexual behavior stigma to inform effective HIV prevention and treatment programs for key populations. JMIR Public Heal Surveill 2017; 3: e23, http://www.ncbi.nlm.nih.gov/pubmed/28446420 (2017, accessed 23 December 2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Moody J, Adams J, Morris M. Epidemic potential by sexual activity distributions. Netw Sci 2017; 5: 461, http://www.ncbi.nlm.nih.gov/pubmed/29449942 (2017, accessed 19 September 2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Holmes KK, Levine R, Weaver M. Effectiveness of condoms in preventing sexually transmitted infections. Bull World Health Organ 2004; 82: 454–461, http://www.ncbi.nlm.nih.gov/pubmed/15356939 (2004, accessed 8 August 2018). [PMC free article] [PubMed] [Google Scholar]
- 30.Werber D, Michaelis K, Hausner M, et al. Ongoing outbreaks of hepatitis A among men who have sex with men (MSM), Berlin, November 2016 to January 2017—linked to other German cities and European countries. Eurosurveillance 2017; 22, http://www.ncbi.nlm.nih.gov/pubmed/28183391 (2017, accessed 8 August 2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Blanc Molina A, Rojas Tejada AJ. Uso del preservativo, número de parejas y debut sexual en jóvenes en coito vaginal, sexo oral y sexo anal. Rev Int Andrología 2018; 16: 8–14, http://www.ncbi.nlm.nih.gov/pubmed/30063024 (2018, accessed 8 August 2018). [DOI] [PubMed] [Google Scholar]
- 32.Bolan RK, Beymer MR, Weiss RE, et al. Doxycycline prophylaxis to reduce incident syphilis among HIV-infected men who have sex with men who continue to engage in high-risk sex: a randomized, controlled pilot study. Sex Transm Dis 2015; 42: 98–103, http://content.wkhealth.com/linkback/openurl?sid=WKPTLP:landingpage&an=00007435-201502000-00009 (2015, accessed 16 April 2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.WHO. Defining sexual health: report of a technical consultation on sexual health, 28–31 January 2002, Geneva. [Internet]. 2006, http://www.who.int/reproductivehealth/publications/sexual_health/defining_sexual_health.pdf (2002, accessed 19 September 2018).


