Abstract
Elderly patients who receive home dialysis (peritoneal dialysis or home hemodialysis) may have reduced survival compared to younger patients. Therefore, it is important to ascertain the goals of home dialysis in the elderly rather than simply fixate on standard metrics such as technique survival. As Canada’s population continues to age, the prevalence of end-stage kidney disease among the elderly population is increasing. Patients with multiple comorbidities are now surviving long enough to be started on dialysis. Although home dialysis has been associated with better survival and improved quality of life, its impact on the frail and elderly populations require further elucidation. Home dialysis patients can either independently perform tasks or have support in the home to safely conduct dialysis. Moreover, patients burdened with frailty and multiple comorbidities who lack support in the home may not be able to perform home dialysis safely. Innovative strategies to improve accessibility to home-based therapies need further exploration. In addition, the concept of goal-directed dialysis promotes more individualized treatment. Future continuous quality improvement initiatives must examine if goal-directed dialysis leads to better quality of life outcomes in the elderly.
Keywords: elderly, frailty, home dialysis, home hemodialysis, peritoneal dialysis
Abrégé
La survie des patients âgés recevant des traitements de dialyse à domicile (dialyse péritonéale ou dialyse à domicile) pourrait être réduite comparativement à celle des patients plus jeunes. Par conséquent, il est essentiel d’évaluer les objectifs de la dialyse à domicile chez les patients âgés plutôt que de simplement se fier à des paramètres standards tels que la survie d’un point de vue technique. Avec le vieillissement de la population canadienne, on note une augmentation de la prévalence de l’insuffisance rénale terminale chez les populations âgées. Des patients présentant de multiples comorbidités survivent désormais suffisamment longtemps pour être traités par dialyse. Bien que la dialyse à domicile soit associée à de meilleures chances de survie et à un rehaussement de la qualité de vie, ses conséquences sur les populations fragilisées et plus âgées doivent être éclairées. Les patients dialysés à domicile peuvent pratiquer la dialyse de façon autonome ou bénéficier de soutien pour procéder en toute sécurité. En outre, les patients fragilisés souffrant de multiples comorbidités et manquant de soutien à domicile pourraient ne pas être en mesure de procéder à la dialyse de façon sécuritaire. Des stratégies innovantes pour améliorer l’accessibilité à des traitements à domicile méritent d’être explorées. De plus, le concept de dialyse ciblée favorise un traitement plus individualisé. Les futures initiatives d’amélioration continue de la qualité doivent s’attarder à déterminer si la dialyse ciblée mène à une meilleure qualité de vie chez les patients âgés.
What was known before
Home dialysis has demonstrated better survival and improved quality of life in younger populations, but its impact on outcomes in frail and elderly populations remains unclear.
What this adds
This opinion piece highlights the importance of goal-directed home dialysis in caring for elderly patients. Goal-directed home dialysis allows practitioners to individualize treatment plans according to patient needs, allowing for more flexibility in social life and independence compared to in-center–based dialysis.
Introduction
The global prevalence of hypertension, diabetes, and cardiovascular diseases among elderly patients, as defined by persons aged 75 years and older, has steadily increased over the last several years, leading to a significant increase in the rates of end-stage renal disease (ESRD) within that population.1,2 As a result, the need for renal replacement therapy among elderly patients has increased. This has been further potentiated by better survival with chronic diseases, increases in dialysis accessibility along with more favorable patient and family perceptions of dialysis. According to most ESRD data registries, elderly patients account for about 25% to 30% of dialysis patients around the globe.3 The Dialysis Outcomes and Practice Patterns Study (DOPPS) revealed that between 2005 and 2007, elderly patients accounted for about 24% of prevalent dialysis patients in Canada.3
In light of the challenges posed by the management of ESRD and dialysis in the elderly population, the creation of the Geriatric Nephrology Advisory Group for the American Society of Nephrology (ASN) along with an online geriatric curriculum (https://www.asn-online.org/education/distancelearning/curricula/geriatrics/) has provided practitioners with better guidance.4 Despite these guidelines, differences in opinions within the nephrology community about the long-term benefits of dialysis, especially home dialysis, remain prevalent.
Although home dialysis (peritoneal dialysis [PD] and home hemodialysis [HHD]) has demonstrated better survival and improved quality of life (QoL) for younger patients, the overall benefits in elderly patients remain unclear. It is possible that elderly patients receiving home dialysis may have worse survival compared to younger patients. Some experts have also argued that renal replacement therapy, particularly in frail patients, may not improve any additional quantity of life.5,6 Elderly patients also experience significant reductions in their QoL and may be burdened with pain, sleep disturbances, and depression.5-8 However, goal-oriented dialysis offers a patient-centered approach, possibly leading to better QoL outcomes in elderly patients.
In this narrative review, we discuss the benefits and challenges of home dialysis treatment in elderly populations. We will also highlight the opportunities for future research to critically examine health outcomes in elderly populations on home dialysis.
Benefits of Home Dialysis
Both PD and HHD offer patients greater control of dialysis prescriptions in the home setting. In patients who have a reduced life expectancy, a major advantage of PD is that there is no need to establish vascular access with invasive vascular procedures. In addition, PD has better preservation of residual renal function compared to HD and can allow for patients to be gradually eased into therapy using an incremental approach.9
HHD provides better blood pressure control and improved middle molecular clearance.10 The removal of middle molecules such as phosphate allows for elderly patients to have a more liberal diet, reducing the risk of malnutrition by imposing strict protein and other dietary restrictions. The pill burden for elderly patients may also be reduced with better blood pressure and phosphate control. Elderly patients with short-term rehabilitation goals5 may also benefit from more intensive dialysis by reducing the uremic burden on their physical and cognitive function.
Drawbacks of Home Dialysis
Functional limitations in frail and elderly populations along with a lack of home support create a significant barrier for the implementation of home dialysis. This population may also suffer from other geriatric syndromes including falls, gait impairment, and malnutrition.6 Frailty in elderly dialysis patients is associated with cognitive impairment and increased mortality.5 In the absence of home support, the majority of elderly patients are placed on in-center hemodialysis primarily for safety concerns.5-7
The main drawbacks of hemodialysis involve intradialytic hypotension which can lead to falls after dialysis. In addition, myocardial stunning, cerebral hypoperfusion, and prolonged post-dialysis recovery times potentiate the risk of falls and other adverse events during and after hemodialysis.5 Although post-dialysis recovery time is shorter with more frequent hemodialysis,11 it remains an important consideration in the elderly population, as it may increase the risk of falls after treatment. Pain and discomfort during HHD treatment is sometimes underappreciated in the elderly. Prolonged stationary positioning in a chair or bed may be challenging for patients with arthritis and other musculoskeletal pain syndromes.5
In terms of vascular access, elderly patients have an increased likelihood of having central venous catheters (CVCs) which are associated with higher morbidity and mortality risk.3,12 Vascular access–related infections are more prevalent in patients with CVCs than those with arteriovenous grafts (AVGs) and arteriovenous fistulas (AVFs).13 Recent U.S. Renal Data System (USRDS) data showed a fourfold increase in risk of infectious complications in patients initiating dialysis with a CVC compared to either a fistula or graft.14,15 The risk is further increased to about sevenfold when a CVC is used as the prevalent access.14 The increase in CVC use is likely multifactorial but also driven by the reduced chance success of AVF or AVG creation in older compared to younger patients.12
Patients who are frail and incapable of self-care are still at risk for several PD complications despite assistance. These complications include infections, hernias, catheter leaks, and catheter dislodgement. Major drawbacks should be considered in terms of patient-related and PD-related factors. Patient-related factors include reduced physical function and manual dexterity to manipulate catheters and lift bags of PD solutions.5 Prior abdominal surgeries along with weak abdominal muscles also increase the risk for catheter leaks and hernias.6 Protein loss related to PD may also potentiate malnutrition in an elderly patient with reduced nutritional intake.5,6 Disruptions in sterility techniques or catheter dislodgement/migration may occur as a result of other geriatric syndromes, especially cognitive impairment and delirium. On the other hand, the storage of PD solutions can occupy significant space in the household; potentially increasing the burden of therapy-related intrusiveness for patients and family members.
Outcomes of Elderly Patients on Home Dialysis
Frailty is more common in the ESRD population compared to the general population, possibly due to uremia, malnutrition, and a hypercatabolic state.16 It is defined as a clinically recognizable state of a constellation of symptoms resulting in increased vulnerability from poor physical function, low physical activity, weight loss, cognitive impairment, and falls.17 Frailty can be assessed by examining the physical fitness of a patient coupled with the ability to perform tasks independently. A recent study has demonstrated that in elderly patients on dialysis, frailty was strongly associated with impaired QoL, regardless of the type of dialysis.18 In addition, frailty among elderly dialysis patients has also been associated with increased hospitalization and mortality rates.18 Despite the clear association between frailty and patient outcomes, several observational studies fail to report nor examine frailty as an outcome predictor in this vulnerable population.
According to the 2018 USRDS, all dialysis patients over the age of 75 years have a mortality rate that is 4 times higher than the general population.19 Registry data from around the globe have shown poor survival outcomes in elderly patients with a median life of 2 years after the initiation of dialysis.5 Furthermore, observational data have not revealed a clear survival advantage with any type of dialysis among elderly patients with poor physical function or multiple medical comorbidities.20
Patients selected for home-based therapies tend to be more physically active and are not burdened by frailty. However, frailty is not a barrier for home dialysis adoption.5 For example, more than 60% of PD patients over the age of 80 years require some sort of assistance with exit site care, medications, and dialysis exchanges.21 Assisted PD and HHD are viable options for patients who cannot perform self-care. Several studies have not demonstrated any differences in technique failure rates nor mortality when comparing self-care to assisted home dialysis therapies.22,23 Despite similar outcomes between self-care and assisted-care, assisted home dialysis is only offered in a few countries primarily due to cost.6
In addition, self-efficacy and functionality are important factors for all individuals, particularly in the elderly population. If functionality declines, then patient satisfaction and overall QoL is negatively impacted. Therefore, care plans which include dialysis strategies that preserve functionality are important. Preliminary observational data demonstrate that patients who are transitioned from home-based therapy to in-center dialysis had worsening in physical functioning.24 Although this may reflect indication bias, this data may also suggest that home dialysis plays an important role in preserving physical function in elderly patients and may lead to better QoL. Maintaining physical function is important both at the patient and at the societal level, as it preserves patient independence and reduces cost to the health-care system.
Patient Perspectives on Home Dialysis
Literature on the perspectives of elderly patients, family members, and caregivers toward home dialysis is lacking. The perception of patients and their burden of disease has been described as one of the most important health outcomes for dialysis patients.6 A dialysis patient with poor QoL is more likely be non-adherent to therapy and in turn has an increased mortality risk.5,18 The impact of illness intrusiveness from ESRD and dialysis on a patient’s QoL must be considered by practitioners. Although a small observational study showed no differences in the degree of illness intrusiveness between PD and nocturnal HHD patients, this study was done in a much younger population and may not be representative of the perspective of elderly patients.25
Physical and psychosocial burdens associated with dialysis can outweigh potential benefits of uremia correction in the perspective of patients. However, there may be a lack of understanding of the burden of disease when conservative approaches are adopted. This highlights the importance of considering the patient’s perspective and utilization of shared–decision making processes, particularly among older patients with ESRD. Shared–decision making promotes patient-centered care by allowing the opinions and perspectives of patients to be factored in treatment decisions.26,27 Older patients and family members who are well-informed and have an awareness that overall life expectancy is reduced tend to place an emphasis on “quality” over “quantity.”
On the other hand, the concept of goal-directed dialysis can individualize treatment according to patient needs. Practitioners must focus on an individual’s priorities through active dialogue in an effort to understand what matters to the patient. Goal-directed dialysis obviates the need to rely on laboratory and clearance data to guide treatment decisions. It allows for practitioners to get to know their patients better. Patients may also perceive that care is more personalized, particularly if their opinions are valued in the decision making process.
In addition, elderly patients may deliberately delay dialysis initiation until they feel that it is absolutely necessary to prolong life. Elderly patients will also prioritize factors that preserve their independence in doing things that are not related to dialysis, differing from younger patients who have better longevity.28 Qualitative data have revealed that the decision to delay the start dialysis is mainly driven by patient fears that dialysis will negatively impact their social life and ability to travel.28 As a result, elderly patients may be more accepting of home dialysis as it would afford for more flexibility in preserving their social life compared to in-center–based dialysis.
Practitioners must work closely with patients and their caregivers in providing dialysis care plans that offer the ideal balance in reducing ESRD-related symptoms while attempting to respect and preserve lifestyle priorities. For instance, some patients enjoy the social interactions with other patients and health-care professionals with each in-center HD session. Whereas other patients are happier with independence and being at home. Therefore, identifying the needs and priorities of patients on an individual basis is an important first step in dialysis modality selection.29 Once a modality has been chosen, an incremental approach to dialysis should be considered for patients as attempt to preserve their independence with minimal disruptions.
Future Directions and Conclusions
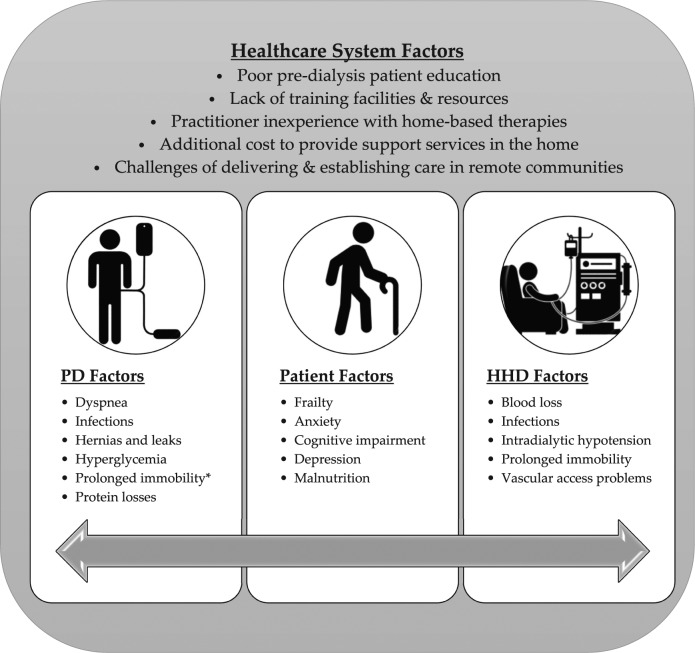
Despite the highlighted benefits of assisted home therapy, more novel ways to support the elderly on home-based therapy are required. Transporting frail elderly patients to hemodialysis centers 3 times per week poses challenges in the community. Mobile dialysis units on buses have been an emerging strategy to increase the access to dialysis to remote areas and reducing travel time for patients. These units have been popular in Australia and New Zealand with some limited experiences in Canada.30,31 The principles of increased access and convenience can be applied to frail populations, bringing dialysis to patients without having to burden them with protracted home dialysis training and long travel times. Mobile dialysis units are innovative yet viable alternatives in providing convenient and cost-effective quality care to our frail populations. Further research must therefore consider an economic analysis and outcomes in this population, focusing specifically on cost comparisons to other modalities and QoL measures specifically. The intention of the mobile units is not to prolong life expectancy but rather improve QoL in our elderly patients on dialysis. Practitioners must also be aware of the various factors that can present challenges to adoption of home-based therapies for patients (Figure 1). A thorough examination of these factors in future research will allow for more innovative and cost-effective strategies to promote home dialysis in elderly patients.
Figure 1.
Schematic diagram of various factors that pose challenges to home dialysis adoption and maintenance in elderly populations.
Note. PD = peritoneal dialysis; HHD = home hemodialysis.
aProlonged immobility may be an issue if patient is on automated PD.
Adopting practices that focus on incremental dialysis offers various benefits to elderly patients while ensuring that care remains individualized. The initiation of dialysis can be a major psychological and physical burden for the frail population. An incremental approach both for HHD and PD may reduce these burdens, allowing patients to become more comfortable with the therapy with a focus on symptom management rather than arbitrary clearance targets.
For example, starting patients on an HHD schedule of 3 to 4 times per week with 5 to 6 hours per session may be a reasonable initial approach for someone who is planning to eventually adopt an even more intensive HHD prescription such as frequent nocturnal hemodialysis. Alternatively, PD patients can be started with 2 exchanges during the day if there is a preference to have a dry abdomen overnight. Otherwise, 2 to 3 exchanges overnight on a cycler with a day dry abdomen is another option. These approaches minimize the initial burden of dialysis and focus on symptom management, allowing treatment to remain patient-centered.
As the population continues to age, more patients will develop ESRD and eventually need dialysis. Current data on clinical outcomes in elderly patients, especially the frail, are limited. Goal-directed dialysis and its impact on QoL in the elderly should be examined as part of future continuous quality improvement research initiatives. More evidence on comparative clinical outcomes for elderly patients on home dialysis to better inform practice is also needed. Future research with elderly patients on home dialysis should also focus on the following areas: (1) survival, (2) adverse events, (3) QoL, and (4) cost. If patients have marginal improvement in survival outcomes but the overall QoL and illness intrusiveness remain high, then future research priorities in home dialysis must reexamine the threshold of what may be considered as “beneficial” in this vulnerable population.
Footnotes
Author’s Note: Bourne L. Auguste is now affiliated with Division of Nephrology, Sunnybrook Health Sciences Centre, Toronto, ON, Canada and Department of Medicine, Division of Nephrology, University of Toronto, ON, Canada. Christoper T. Chan is now affiliated with Department of Medicine, Division of Nephrology, University of Toronto, ON, Canada.
Author Contributions: Both authors contributed equally in terms of content in the drafting and revision of this manuscript. Both authors read and approved the final manuscript.
Ethics Approval and Consent to Participate: No ethics approval or consent to participate was required for this publication.
Consent for Publication: The authors have consented publication of this article.
Availability of Data and Materials: The data and materials are not available for this study.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Bourne L. Auguste  https://orcid.org/0000-0002-6741-2427
https://orcid.org/0000-0002-6741-2427
References
- 1. Collins AJ, Kasiske B, Herzog C, et al. Excerpts from the United States Renal Data System 2006 annual data report. Am J Kidney Dis. 2007;49(1) (suppl 1):A6-A7, S1–S296. [DOI] [PubMed] [Google Scholar]
- 2. Jager KJ, van Dijk PC, Dekker FW, Stengel B, Simpson K, Briggs JD. The epidemic of aging in renal replacement therapy: an update on elderly patients and their outcomes. Clin Nephrol. 2003;60(5):352-360. [DOI] [PubMed] [Google Scholar]
- 3. Canaud B, Tong L, Tentori F, et al. Clinical practices and outcomes in elderly hemodialysis patients: results from the Dialysis Outcomes and Practice Patterns Study (DOPPS). Clin J Am Soc Nephrol. 2011;6(7):1651-1662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Rosner M, Abdel-Rahman E, Williams ME. Geriatric nephrology: responding to a growing challenge. Clin J Am Soc Nephrol. 2010;5(5):936-942. [DOI] [PubMed] [Google Scholar]
- 5. Brown EA, Finkelstein FO, Iyasere OU, Kliger AS. Peritoneal or hemodialysis for the frail elderly patient, the choice of 2 evils? Kidney Int. 2017;91(2):294-303. [DOI] [PubMed] [Google Scholar]
- 6. Segall L, Nistor I, Van Biesen W, et al. Dialysis modality choice in elderly patients with end-stage renal disease: a narrative review of the available evidence. Nephrol Dial Transplant. 2017;32(1):41-49. [DOI] [PubMed] [Google Scholar]
- 7. Malavade T, Sokwala A, Jassal SV. Dialysis therapies in older patients with end-stage renal disease. Clin Geriatr Med. 2013;29(3):625-639. [DOI] [PubMed] [Google Scholar]
- 8. Brown EA, Johansson L. Dialysis options for end-stage renal disease in older people. Nephron Clin Pract. 2011;119(suppl 1):c10-c13. [DOI] [PubMed] [Google Scholar]
- 9. Auguste BL, Bargman JM. Incremental peritoneal dialysis: new ideas about an old approach. Semin Dial. 2018;31(5):445-448. [DOI] [PubMed] [Google Scholar]
- 10. Rocco MV, Lockridge RS, Jr, Beck GJ, et al. The effects of frequent nocturnal home hemodialysis: the frequent hemodialysis network nocturnal trial. Kidney Int. 2011;80(10):1080-1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Jaber BL, Schiller B, Burkart JM, et al. Impact of short daily hemodialysis on restless legs symptoms and sleep disturbances. Clin J Am Soc Nephrol. 2011;6(5):1049-1056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Lee T, Thamer M, Zhang Q, Zhang Y, Allon M. Vascular access type and clinical outcomes among elderly patients on hemodialysis. Clin J Am Soc Nephrol. 2017;12(11):1823-1830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Viecelli AK, O’Lone E, Sautenet B, et al. Vascular access outcomes reported in maintenance hemodialysis trials: a systematic review. Am J Kidney Dis. 2018;71(3):382-391. [DOI] [PubMed] [Google Scholar]
- 14. Methods USRDSA. USRDS 2012 Annual Data Report: Atlas of Chronic Kidney Disease and End-Stage Renal Disease in the United States. Bethesda, MD: National Institutes of Health; 2012. [Google Scholar]
- 15. Viecelli AK, Tong A, O’Lone E, et al. Report of the standardized outcomes in nephrology-hemodialysis (SONG-HD) consensus workshop on establishing a core outcome measure for hemodialysis vascular access. Am J Kidney Dis 2018;71(5):690-700. [DOI] [PubMed] [Google Scholar]
- 16. Roshanravan B, Khatri M, Robinson-Cohen C, et al. A prospective study of frailty in nephrology-referred patients with CKD. Am J Kidney Dis. 2012;60(6):912-921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Xue QL. The frailty syndrome: definition and natural history. Clin Geriatr Med. 2011;27(1):1-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Iyasere OU, Brown EA, Johansson L, et al. Quality of life and physical function in older patients on dialysis: a comparison of assisted peritoneal dialysis with hemodialysis. Clin J Am Soc Nephrol. 2016;11(3):423-430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. System USRD. 2018 USRDS annual data report: epidemiology of kidney disease in the United States. https://www.usrds.org/2018/view/Default.aspx. Published 2018.
- 20. Chandna SM, DaSilva-Gane M, Marshall C, Warwicker P, Greenwood RN, Farrington K. Survival of elderly patients with stage 5 CKD: comparison of conservative management and renal replacement therapy. Nephrol Dial Transplant. 2011;26(5):1608-1614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Jagose JT, Afthentopoulos IE, Shetty A, Oreopoulos DG. Successful use of continuous ambulatory peritoneal dialysis in octogenarians. Adv Perit Dial. 1996;12:126-131. [PubMed] [Google Scholar]
- 22. Brown EA, Davies SJ, Rutherford P, et al. Survival of functionally anuric patients on automated peritoneal dialysis: the European APD outcome study. J Am Soc Nephrol. 2003;14(11):2948-2957. [DOI] [PubMed] [Google Scholar]
- 23. Li PK, Law MC, Chow KM, et al. Good patient and technique survival in elderly patients on continuous ambulatory peritoneal dialysis. Perit Dial Int. 2007;27(suppl 2):S196-S201. [PubMed] [Google Scholar]
- 24. Eneanya ND, Maddux DW, Reviriego-Mendoza MM, et al. Longitudinal patterns of health-related quality of life and dialysis modality: a national cohort study. BMC Nephrol. 2019;20:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Fong E, Bargman JM, Chan CT. Cross-sectional comparison of quality of life and illness intrusiveness in patients who are treated with nocturnal home hemodialysis versus peritoneal dialysis. Clin J Am Soc Nephrol. 2007;2(6):1195-1200. [DOI] [PubMed] [Google Scholar]
- 26. Singh P, Germain MJ, Cohen L, Unruh M. The elderly patient on dialysis: geriatric considerations. Nephrol Dial Transplant. 2014;29(5):990-996. [DOI] [PubMed] [Google Scholar]
- 27. Walker RC, Howard K, Morton RL, Palmer SC, Marshall MR, Tong A. Patient and caregiver values, beliefs and experiences when considering home dialysis as a treatment option: a semi-structured interview study. Nephrol Dial Transplant. 2016;31(1):133-141. [DOI] [PubMed] [Google Scholar]
- 28. Lovell S, Walker RJ, Schollum JB, Marshall MR, McNoe BM, Derrett S. To dialyse or delay: a qualitative study of older New Zealanders’ perceptions and experiences of decision-making, with stage 5 chronic kidney disease. BMJ Open. 2017;7(3):e014781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Juergensen E, Wuerth D, Finkelstein SH, Juergensen PH, Bekui A, Finkelstein FO. Hemodialysis and peritoneal dialysis: patients’ assessment of their satisfaction with therapy and the impact of the therapy on their lives. Clin J Am Soc Nephrol. 2006;1(6):1191-1196. [DOI] [PubMed] [Google Scholar]
- 30. Kidney Health Australia. Home dialysis on the road. https://kidney.org.au/cms_uploads/docs/home-dialysis-on-the-road.pdf.
- 31. Central HD. Hop on the bus, get an HD treatment. https://homedialysis.org/news-and-research/news/living-well-with-home-treatments/articles/265-hop-on-the-bus-get-an-hd-treatment. Published 2016.