Dear Editor,
Infertility affects about 48.5 million couples worldwide, and a male disorder is estimated to be a causative or contributing factor in 20%–50% of cases.1 Notably, increasing data support the view that obese men are at higher risk of fertility disorders.2 As is known, obesity is defined by an excess of white adipose tissue, currently recognized as being able to secrete many endocrinologically active molecules called adipokines.3 Their involvement in animal and human reproduction is recognized.4 Indeed, in rodents, the removal of epididymal adipose tissue decreases spermatogenesis and males lacking adipokines or their receptors have reduced fertility.3 Concerning humans, mature spermatozoa present leptin receptors on their surface,5 and recently, adiponectin, resistin, chemerin, visfatin, and vaspin have been identified in seminal fluid (SF).2
From these findings, we hypothesize that adipokines represent a pathophysiological link between energy metabolism and male reproductive function. Hence, our aim was to determine the expression profiles of adipokines in blood plasma (BP) and SF of healthy normal weight men (n = 44, 20–45 years old). Included cases were enrolled during a medical consultation for couple infertility exploration into two different Assisted Reproductive Centers (Tours, FERTIPROTECT protocol, and Paris, METASPERME protocol). They had normal body mass index (18–25 kg m−2) and overall normal semen quality according to the WHO (2010) guidelines.
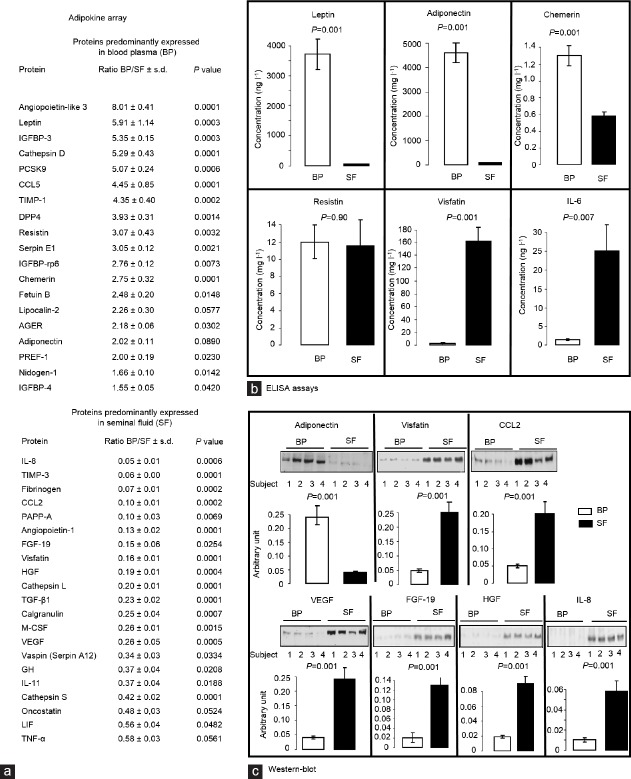
First, a human adipokine array, simultaneously testing 58 adipokines, was performed on SF and BP samples from seven cases, showing that BP concentrations of leptin, chemokine ligand-5 (CCL5), resistin, and chemerin were significantly higher than the seminal ones. On the contrary, interleukin-8 (IL-8), fibrinogen, chemokine ligand-2 (CCL2), fibroblast growth factor-19 (FGF-19), visfatin, hepatocyte growth factor (HGF), transforming growth factor β1 (TGF-β1), vascular endothelial growth factor (VEGF), and vaspin (serpin A12) were more highly expressed in SF (Figure 1a). Some adipokines of interest previously identified were then quantified by enzyme-linked immunosorbent assay (ELISA) (n = 25) or Western blotting (n = 19). ELISA confirmed significantly higher leptin, adiponectin, and chemerin concentrations in BP and high visfatin expression in SF (Figure 1b). Western blot analysis displayed similar results (Figure 1c): adiponectin was predominantly expressed in BP, while visfatin, FGF-19, VEGF, HGF, IL-8, and CCL2 concentrations were significantly higher in SF. By ELISA, but not with the adipokine array, we showed a higher IL-6 concentration in BP than in SF (Figure 1b).
Figure 1.
Expression of adipokines in SF and BP of men of normal weight. (a) Adipokine array data. Proteome Profiler Human Adipokine Array Kit (ARY024 from R&D system, Paris, France) was used as described by the provider to analyze 58 adipokines in BP and SF of seven healthy patients with normal weight and normal semen quality. Data were reported as the ratio between protein expression in BP and in SF (mean ± s.d.). P values were also shown (Student's t-test). Nineteen proteins were higher expressed in BP whereas 21 proteins prevailed in SF. (b) ELISA assays. Plasma and seminal concentrations of leptin, adiponectin, chemerin, resistin, visfatin, and IL-6 were measured using ELISA kits from R&D System (Paris, France, mean ± s.d., n = 25, with serum intra-assay and inter-assay coefficients of variations <8, and for seminal plasma, intra-assay coefficients of variations ≤6% and inter-assay coefficients of variations ≤10%). Data were analyzed by Student's t-test (P values shown). (c) Western blotting. Plasma and seminal concentrations of adiponectin, visfatin, CCL2, VEGF, HGF, and IL-8 quantified by Western blots (mean ± s.d., n = 19). Eighty μg of seminal and BP as determined using bicinchoninic acid assay was denatured in ×5 Laemmli buffer. The samples were then heated at 95°C for 5 min, subjected to electrophoresis on 12% SDS-polyacrylamide gels, and transferred onto nitrocellulose membranes (Schleicher and Schuell, Ecquevilly, France). The membrane was blocked for 30 min in TBS-Tween-milk 5% (v/v) and incubated for 16 h with appropriate primary antibodies at a 1:1000 final dilution. These primary antibodies were obtained from Santa Cruz Biotechnology (Heidelberg, Germany) for VEGF (sc-53462), adiponectin (sc-17044-R), FGF-19 (sc-73984), HGF (sc-1358), CCL2 (sc-32771), and IL-8 (sc-376750) and from Sigma (St Quentin Fallavier, France) for visfatin (V9139). Finally, the blots were incubated for 1 h and 30 min at room temperature with HRP-conjugated anti-rabbit or anti-mouse IgG (dilution 1/5000). The oroteins were detected by enhanced chemiluminescence (Western Lightning Plus-ECL, Perkin Elmer) using a G:Box SynGene (Ozyme) with GeneSnap software (release 7.09.17; Chicago, IL, USA). The signals detected were quantified with the GeneTools software (release 4.01.02; Syngene, Fredrick, MD, USA). The results are expressed as intensity signal in arbitrary units after normalization, allowed by the use of reversible Ponceau staining, as an internal standard. Data were analyzed by Student's t-test (P values shown). s.d.: standard deviation; BP: blood plasma; SF: seminal fluid; HRP: horseradish-peroxidase; IgG: immunoglobulin G; IGFBP-3: insulin-like growth factor binding protein 3; PCSK9: proprotein convertase subtilisin/kexin type 9; CCL5: chemokine (C-C motif) ligand 5; TIMP-1: metallopeptidase inhibitor 1; DPP4: dipeptidyl peptidase-4; AGER: advanced glycosylation end-product specific receptor; PREF-1: preadipocyte factor 1; IL8: interleukin 8; TIMP-3: metallopeptidase inhibitor 3; CCL2: chemokine (C-C motif) ligand 2; PAPP-A: pregnancy-associated plasma protein-A; FGF 19: fibroblast growth factor 19; HGF: hepatocyte growth factor; TGF-β1: transforming growth factor beta 1; M-CSF: macrophage colony-stimulating factor; VEGF: vascular endothelial growth factor; GH: growth hormone; LIF: leukemia inhibitory factor; TNF-α: tumor necrosis factor alpha.
Remarkably, in SF, we found up to 100-fold higher concentrations of some well-known inflammatory markers and growth factors (GFs). The presence of a variety of cytokines, chemokines, and GFs in human semen has already been demonstrated, and their role in the regulation of spermatogenesis and other testicular cell functions was proven long ago.6 Implications of cytokines in male infertility are still controversial;7 however, a correlation between their seminal concentration and sperm quality parameters has been repeatedly shown.6 Interestingly, in our study, seminal IL-8 correlated positively with sperm vitality (r2 = 0.35, P < 0.01), encouraging further studies about the role of this cytokine in semen physiopathology. No significant correlation was found between seminal/plasma IL-6 and sperm parameter values, although data on sperm leukocyte count were not available for most of the patients. As for cytokines, GFs have long been implicated in intratesticular control, notably during fetal life.7 Expression of HGF and its receptor has been demonstrated in human germ cells and spermatozoa, and, in rats, HGF positively controls cell proliferation and seems to regulate Leydig cell steroidogenesis.7 In our study, we found a negative correlation between plasma HGF and inhibin B concentration (r2 = −0.32, P < 0.05). Inhibin B is considered as a marker of Sertoli cell function and spermatogenesis;8 thus, HGF could be involved in germ cell proliferation. We also observed a positive association between seminal HGF and testosterone levels (r2 = 0.26, P < 0.05), suggesting a potential role of HGF in the regulation of steroidogenesis. Although data implicating FGF-19 in human fertility is poor, its action as a regulator of the feeding response leading to an improvement of metabolic profile is increasingly being studied.9 To the best of our knowledge, we have shown, for the first time, FGF-19 is present in SF and its plasma concentration correlates negatively with inhibin B levels (r2 = 0.30, P < 0.05) and the percentage of spermatozoa with normal morphology (r2 = 0.44, P < 0.01). Further investigations on its potential role in the interplay between metabolic perturbations and infertility disorders could, thus, provide captivating results.
Concerning adipokines, in agreement with previous data,2 we confirmed a predominant expression of leptin, adiponectin, resistin, and chemerin in BP compared with that of SF. No significant correlation was found between concentrations of seminal adipokines and semen parameter values, but we observed a positive association between plasma adiponectin and sperm total (r2 = 0.20, P < 0.05) and progressive motility (r2 = 0.17, P < 0.05) and a negative correlation between blood chemerin concentration and sperm normal morphological forms (r2 = 0.16, P < 0.05). Negative correlations were also observed between resistin plasma concentrations, sperm vitality (r2 = 0.31, P < 0.01), and normal morphology spermatozoa percentage (r2 = 0.25, P = 0.01), confirming literature data.3 Indeed, resistin is known to be involved in inflammation processes and its seminal concentration correlates positively with levels of proinflammatory markers, whose increase is associated with impaired male fertility.3 The presence of visfatin and vaspin (Serpin A12) in SF has already been reported,2 and visfatin has been previously detected in human spermatozoa, where it likely exerts an inhibitory effect on capacitation.10 We showed no significant correlation between these adipokines and sperm parameters. However, the expression of these adipokines in SF was considerably higher than in BP, encouraging further explorations on the role of these molecules in male reproduction. Interestingly, no significant correlation was found between blood and seminal adipokines levels, supporting the hypothesis of gonadal production or compartment-specific regulation of adipokines in the reproductive tract and peripheral blood.2,3
In conclusion, we confirmed that the adipokine expression profile in SF is different from that in plasma. However, the meaning of a predominant concentration of some adipokines, including well-known inflammatory markers, in SF remains to be clarified. Studies aimed to evaluate the direct effects of recombinant adipokines on spermatozoa are currently in progress in our laboratory and they could allow us to elucidate the role of adipokines in male reproduction.
AUTHOR CONTRIBUTIONS
JD and RL designed the study. JD, YE, JSB, CR, NM, JPB, SF, RL, and CV were involved in experimental procedures, data collection, and assembly. AB and JD analyzed data and wrote the manuscript. AB, JD, PF, and RL revised the paper and participated in critical discussion. All authors read and approved the final manuscript.
COMPETING INTERESTS
All authors declared no competing interests.
ACKNOWLEDGMENTS
This work was supported by the Agence de Biomédicine Project “Adipocytokines” (grant number 32000822).
REFERENCES
- 1.Morrison CD, Brannigan RE. Metabolic syndrome and infertility in men. Best Pract Res Clin Obstet Gynaecol. 2015;29:507–15. doi: 10.1016/j.bpobgyn.2014.10.006. [DOI] [PubMed] [Google Scholar]
- 2.Thomas S, Kratzsch D, Schaab M, Scholz M, Grunewald S, et al. Seminal plasma adipokine levels are correlated with functional characteristics of spermatozoa. Fertil Steril. 2013;99:1256–63. doi: 10.1016/j.fertnstert.2012.12.022. [DOI] [PubMed] [Google Scholar]
- 3.Elfassy Y, Bastard JP, McAvoy C, Fellahi S, Dupont J, et al. Adipokines in semen: Physiopathology and effects on spermatozoa. Int J Endocrinol. 2018:3906490. doi: 10.1155/2018/3906490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dupont J, Pollet-Villard X, Reverchon M, Mellouk N, Levy R. Adipokines in human reproduction. Horm Mol Biol Clin Investig. 2015;24:11–24. doi: 10.1515/hmbci-2015-0034. [DOI] [PubMed] [Google Scholar]
- 5.Jope T, Lammert A, Kratzsch J, Paasch U, Glander HJ. Leptin and leptin receptor in human seminal plasma and in human spermatozoa. Int J Androl. 2003;26:335–41. doi: 10.1111/j.1365-2605.2003.00434.x. [DOI] [PubMed] [Google Scholar]
- 6.Fraczek M, Kurpisz M. Cytokines in the male reproductive tract and their role in infertility disorders. J Reprod Immunol. 2015;108:98–104. doi: 10.1016/j.jri.2015.02.001. [DOI] [PubMed] [Google Scholar]
- 7.Zachow R, Uzumcu M. The hepatocyte growth factor system as a regulator of female and male gonadal function. J Endocrinol. 2007;195:359–71. doi: 10.1677/JOE-07-0466. [DOI] [PubMed] [Google Scholar]
- 8.Kumanov P, Nandipati K, Tomova A, Robeva R, Agarwal A. Significance of inhibin in reproductive pathophysiology and current clinical applications. Reprod Biomed Online. 2005;10:786–812. doi: 10.1016/s1472-6483(10)61124-8. [DOI] [PubMed] [Google Scholar]
- 9.Nies VJ, Sancar G, Liu W, van Zutphen T, Struik D, et al. Fibroblast growth factor signalling in metabolic regulation. Front Endocrinol (Lausanne) 2016;6:193. doi: 10.3389/fendo.2015.00193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Riammer S, Garten A, Schaab M, Grunewald S, Kiess W, et al. Nicotinamide phosphoribosyltransferase production in human spermatozoa is influenced by maturation stage. Andrology. 2016;4:1045–53. doi: 10.1111/andr.12252. [DOI] [PubMed] [Google Scholar]