Abstract
Background and Objectives:
Evaluation of health-related quality of life (HRQoL) among tuberculosis (TB) patients could improve understanding about the burden associated with the diseases. There is a paucity of research regarding evaluation of HRQoL among TB population in Indonesia. This study aimed to investigate HRQoL among TB patients in Ciamis, Indonesia.
Methods:
This was a cross-sectional study conducted at one primary health-care facility in Ciamis, Indonesia. HRQoL was measured using the World Health Organization (WHO) QoL-BREF instrument which covers assessment on physical, psychological, social relationship, and environmental health domains. Multiple regression analysis was used to investigate the association between domain scores with demographic factors of the participants such as age, sex, education years, and types of treatment. Statistical analysis was conducted using SPSS software version 21.
Results:
Eighty-one participants were recruited in the present study. The total mean score for all domains was 45.35 (±23.3). The mean scores for physical, physiological, social relationship, and environmental health domains were 20.5 (±9.9), 76.4 (±11.9), 36.9 (±9.2), and 46.9 (±10.4), respectively. Education years were significantly associated with improved HRQoL in environmental health domain (P < 0.05).
Conclusion:
TB had remarkable negative impacts on patients HRQoL, with physical domain was the most affected. This finding calls upon strategies addressing HRQoL problems in the management of TB patients.
Keywords: Health status, quality of life, tuberculosis, World Health Organization quality of life-BREF
INTRODUCTION
Tuberculosis (TB) remains a major public health problem. It is a leading cause of global morbidity from infectious diseases. In 2015, 10.4 million new TB cases were detected around the world. Indonesia shares 10% of this burden with more than a million TB incidence in that year, making it the second country with the highest TB burden worldwide, behind India.[1]
TB interferes with various aspects of patients’ health and well-being, including physical, psychological, financial, and social domains.[2] The disease itself is known to adversely affect patients’ ability to perform daily living activities. Besides, prolonged duration of therapy with multiple drugs can lead to concerns about adverse drug reaction and economic problem.[3,4] Moreover, the risk of resistance could hinder the treatment completion.[5] Social stigma about TB can also affect mental states of the patients. Individual perception regarding the impact of the diseases on their daily activities and functioning is known as health-related quality of life (HRQoL). It is important to evaluate HRQoL in patients, particularly in chronic disease like TB whose physical, mental, and social health is affected by the diseases and its treatment in the long term. Understanding HRQoL of patients will enable better design of a patient-oriented TB intervention that can improve health status and HRQoL of patients.[6]
A number of instruments are available to measure HRQoL.[7,8,9,10] Among them, the World Health Organization (WHO) QoL-BREF questionnaire captures broader domains, which includes physical capacity, psychological, social relationship, and environment and thus allows multidimensional understanding of HRQoL.[10] Besides, previous studies showed that WHO QoL-BREF questionnaire had fewer floor and ceiling effect than Short Form-36 Health Survey (SF-36 HS), which can result in more optimal assessment of participants’ responses.[11,12]
To date, the HRQoL among TB patients has not been studied adequately, particularly in developing countries.[5,6,13,14,15,16] Specifically, among TB populations in Indonesia, there is a paucity of research regarding HRQoL. Therefore, this study was conducted to assess the impact of TB and its treatment on HRQoL of TB patients in Ciamis, a city in TB endemic province in Indonesia.
METHODS
Study design and participants
This was a prospective cross-sectional study involving pulmonary TB patients who visited one primary health care facility in Ciamis, Indonesia. Using Slovin's formula, n = N/(1 + Ne2), the minimum sample size of 81 was required to obtain 95% confidence level.[17] Participants were recruited consecutively during April–June 2015. Eligible participants were those diagnosed with pulmonary TB, who were receiving TB treatment, aged between 18 and 59 years. We excluded patients who had physical or cognitive limitations that made them unable to answer the questions and those who were not willing to participate in the study. Informed consents were obtained from all participants. The study was approved by the Health Research Ethics Committee of the Faculty of Medicine, Universitas Padjadjaran, Indonesia, No. 410/UN6.C1.3.2/KEPK/PN/2015.
Measurement
HRQoL measurement was performed by trained investigators using WHO QoL-BREF questionnaire that was adapted to Indonesian language. The validity and reliability of this translation were assessed in previous studies. The translation was found to be valid and reliable.[18,19,20] This instrument consists of 26 items, 2 items for evaluating general HRQoL and general health and 24 items for evaluating HRQoL in four domains, namely physical (7 items), psychological (6 items), social relationship (3 items), and environmental factors (8 items) [Table 1]. The response for each item is based upon a self-report using a scale from 0 to 5. Higher scores indicate better HRQoL.[6]
Table 1.
Questionnaire items in World Health Organization quality of life-BREF instrument
| Domain | Item |
|---|---|
| Global items | General QoL |
| General health | |
| Physical health | Pain and discomfort |
| Energy and fatigue | |
| Sleep and rest | |
| Dependence on medication | |
| Mobility | |
| Activities on daily living | |
| Working capacity | |
| Psychological | Positive feeling |
| Negative feeling | |
| Self-esteem | |
| Learning, memory, and concentration | |
| Body image | |
| Spirituality and personal beliefs | |
| Social relationship | Personal relations |
| Sex | |
| Practical social support | |
| Environment | Financial resources |
| Information and skills | |
| Recreation and leisure | |
| Home environment | |
| Access to health care | |
| Physical safety and security | |
| Physical environment | |
| Transport |
QOL: Quality of Life
Data analysis
Descriptive analysis was used to report demographic characteristics of the participants. The score for each domain was calculated using equations for computing domain outlined in WHO QoL-BREF scoring guideline.[9] These scores were then converted into a 4–20 scale, comparable with WHO QoL-100 instrument. The second conversion transformed these scores to a 0–100 scale. Reliability was measured by calculating the Cronbach's alpha (internal consistency index). Cronbach's alpha coefficient ≥0.60 was considered acceptable.[21] Multiple regression analysis was used to investigate the association between domain scores with demographic factors of the participants. The level of significance was set at P < 0.05. Statistical analysis was conducted using SPSS software version 21, SPSS Inc, Chicago, Illinois, USA.
RESULTS
Demographic characteristics of the study population are reported in Table 2. Participants of this study were in the age group of 18 to 59 years with the mean age of 39.4 ± 13.2 years. The majority were male (58%). More than a third of participants (34.6%) experienced only primary school-level education [Table 2].
Table 2.
Demographic characteristics of the participants
| Demographic variable | n (%) |
|---|---|
| Age | |
| 18-27 | 21 (26) |
| 28-37 | 17 (21) |
| 38-47 | 16 (20) |
| 48-59 | 27 (33) |
| Sex | |
| Male | 47 (58) |
| Female | 34 (42) |
| Level of education | |
| Illiterate | 1 (1.2) |
| Primary | 28 (34.6) |
| Middle | 19 (23.4) |
| High school | 25 (31) |
| Bachelor degree | 8 (9.8) |
| Type of drug dosage form | |
| Oral | 77 (95) |
| Oral and parenteral | 4 (5) |
Result of health-related quality of life
Cronbach's alpha coefficient for all questions was 0.625, showing that the responses of the questionnaire were reliable. Almost half of participants perceived bad or very bad general HRQoL. Only 14% were satisfied with their general HRQoL [Figure 1]. This finding was comparable with the result of patients’ perception on their general health. Fifty-one percent of participants were dissatisfied or very dissatisfied with their general health. A large number of participants (38%) felt average about their general health [Figure 2].
Figure 1.
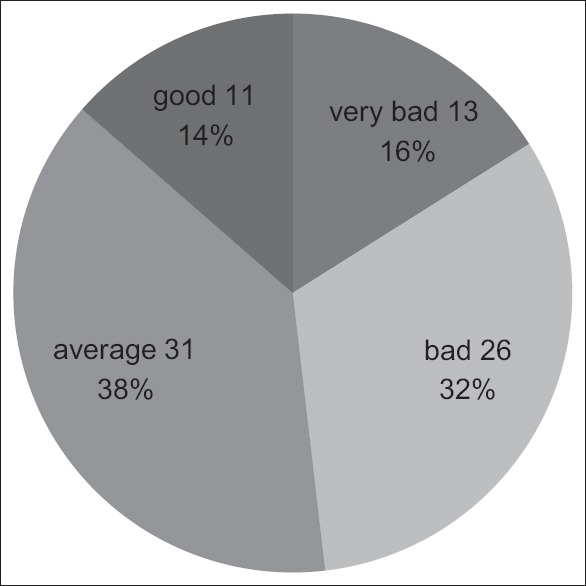
Patients perception of their quality of life
Figure 2.
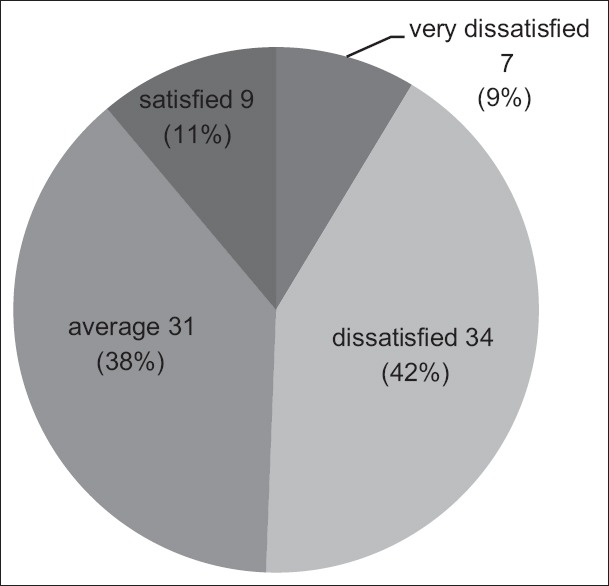
Patients perception of their general health
The mean scores (standard deviation) for physical, physiological, social relationship, and environmental health domains were 20.5 (±9.9), 76.4 (±11.9), 36.9 (±9.2), and 46.9 (±10.4), respectively. The total mean score for all domains was 45.35 (±23.3). Cutoff point ≥60% was used to distinguish satisfied and dissatisfied criteria.[17] Our study found that participants felt satisfied only on their psychological health domain. The lowest satisfaction score was in the physical health domain [Table 3].
Table 3.
Total health-related quality of life mean scores in each domain
| Domain | Mean±SD | Interpretation |
|---|---|---|
| Physical health | 20.8±8.8 | Dissatisfied |
| Psychological health | 76.4±11.9 | Satisfied |
| Social relationship health | 36.9±9.2 | Dissatisfied |
| Environmental health | 46.9±10.4 | Dissatisfied |
| Total domains | 45.25±23.3 | Dissatisfied |
SD: Standard deviation
Table 4 shows the differences of domain scores between different states of some variables. Age, sex, and types of drug dosage form were not significantly associated with improved HRQoL in any domain. Education years beneficially influenced HRQoL in environmental health domain (P < 0.05).
Table 4.
Association between health-related quality of life domain scores and demographic factors
| Variables | n (%) | Mean±SD | |||
|---|---|---|---|---|---|
| Physical health | Psychological health | Social relationship | Environmental health | ||
| Age | |||||
| ≤35 | 36 (44) | 21±8.0 | 72±11.6 | 38±9.5 | 45±10.2 |
| >35 | 45 (56) | 21±9.5 | 80±11.3 | 36±9.0 | 49±10.2 |
| P | 0.74 | 0.34 | 0.48 | 0.61 | |
| Sex | |||||
| Male | 47 (58) | 19±9.0 | 74±11.2 | 38±9.0 | 46±10.3 |
| Female | 34 (42) | 22±8.9 | 80±11.8 | 36±9.5 | 48±10.5 |
| P | 0.13 | 0.05 | 0.84 | 0.83 | |
| Education years | |||||
| 0-11 | 48 (59) | 20±9 | 79±12 | 38±9 | 46±10 |
| ≥12 | 33 (41) | 21±11 | 73±11 | 36±10 | 48±11 |
| P | 0.15 | 0.12 | 0.54 | 0.01 | |
| Dosage form | |||||
| Nonparenteral | 77 (95) | 20±10 | 76±12 | 37±9 | 47±10 |
| Parenteral | 4 (5) | 23±9 | 75±14 | 36±9 | 47±15 |
| P | 0.38 | 0.28 | 0.11 | 0.54 | |
SD: Standard deviation
DISCUSSION
This study indicated that TB had significant and encompassing impacts on patients HRQoL, relatively similar with the previous study.[3] Our study population had a low HRQoL rate, which was shown by the mean score for all domains was 45.25 (±23.3). Besides, a large number of participants felt dissatisfied with their general health and HRQoL.
Multiple aspects of health were affected by TB. In this study, physical health domain, mean 20.8 (±8.8), was the most affected one, implying low activity level in performing daily living activities, lack of sufficient rest and sleep, greater dependence on medicinal products, more pain and discomfort, not enough energy and mobility, and poor capacity for work. This finding confirmed the results of other studies assessing HRQoL of TB patients conducted at the USA, China, and India.[22,23,24,25] Several symptoms such as cough, fever, weight loss, and fatigue were often reported as the causes of limited physical functioning.[26] However, Chamla et al. found that although physical domain appeared to be worst affected by TB, it improved more quickly after the treatment while impairment on other domains tended to persist for a longer time.[27]
We found that age, sex, education years, and drug dosage forms were not associated with improved physical health. This contradicted previous studies which found that differences in age, sex, and education level significantly influenced physical functioning.[26,28,29,30] This may be due to differences in pathology of TB, comorbidities, and study environment.
The highest HRQoL score was observed in the psychological health domain 76.4 (±11.9). Majority (64.2%) of our participants experienced middle, high school, or undergraduate level of education. It was possible that education provides them the opportunity to have better conditions of life, so it can reduce psychological distress.[30] Besides, this finding was expected in religious population like in Indonesia.[31] Several studies have shown that there were positive associations between spirituality and mental health.[32,33]
Interestingly, we found that longer education years were associated with improved HRQoL in environmental health domain. Environmental health domain relates to the sense of security, financial resources, access to health care, recreation and leisure, home environment, and transport. This finding was in coherence with previous studies, showing that education was among the decisive factors on patients’ HRQoL status.[28,33]
In social relationship domain, we found no differences between different states of demographic factors. This domain was the second most affected after physical domain, mean 36.9 (±9.2). Social stigma attached to TB disease may lead to the isolation of TB patients from other members of community.[34] Previous studies suggested several interventions to reduce TB stigma, including TB club program in Africa by health-care workers which provide social support and compliance/side effect monitoring to TB patients,[35] education aiming to at-risk community members to change inaccurate perceptions with regard to the disease,[36] and patients’ counseling.[37]
In this study, prognostic features such as comorbidities data were not collected. Besides, this study was a single-center study which may affect its generalizability for Indonesian population. A strength of our study is the availability of information on the determinant of improved HRQoL among TB patients.
CONCLUSION
Our study showed that TB had a remarkable impact on patients’ HRQoL. Diminished HRQoL scores were observed particularly in physical health domain. Education year was determinant of improved HRQoL status in environmental health domain. This finding calls upon strategies addressing HRQoL problems in the management of TB patients.
Financial support and sponsorship
The authors received no specific funding for this work.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Raviglione M, Sulis G. Tuberculosis 2015: Burden, challenges and strategy for control and elimination. Infect Dis Rep. 2016;8:6570. doi: 10.4081/idr.2016.6570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. Global Tuberculosis Report 2015. Geneva: World Health Organization; 2015. [Last acessed 21 July 2018]. Available from: http://www.apps.who.int/iris/bitstream/1665/191102/1/9789241565059_eng.pdf . [Google Scholar]
- 3.Aggarwal AN. Health-related quality of life: A neglected aspect of pulmonary tuberculosis. Lung India. 2010;27:1–3. doi: 10.4103/0970-2113.59259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wardhana MF, Milanda T, Sumiwi SA. Assessment of risk factors of hepatotoxicity among tuberculosis patients. Pharmacol Clin Pharm Res. 2018;3:10–5. [Google Scholar]
- 5.Pradipta IS, Sodik DC, Lestari K, Parwati I, Halimah E, Diantini A, et al. Antibiotic resistance in sepsis patients: Evaluation and recommendation of antibiotic use. N Am J Med Sci. 2013;5:344–52. doi: 10.4103/1947-2714.114165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rajeswari R, Muniyandi M, Balasubramanian R, Narayanan PR. Perceptions of tuberculosis patients about their physical, mental and social well-being: A field report from South India. Soc Sci Med. 2005;60:1845–53. doi: 10.1016/j.socscimed.2004.08.024. [DOI] [PubMed] [Google Scholar]
- 7.Balestroni G, Bertolotti G. EuroQol-5D (EQ-5D): An instrument for measuring quality of life. Monaldi Arch Chest Dis. 2012;78:155–9. doi: 10.4081/monaldi.2012.121. [DOI] [PubMed] [Google Scholar]
- 8.Ware JE, Jr, Gandek B. Overview of the SF-36 health survey and the international quality of life assessment (IQOLA) project. J Clin Epidemiol. 1998;51:903–12. doi: 10.1016/s0895-4356(98)00081-x. [DOI] [PubMed] [Google Scholar]
- 9.Horsman J, Furlong W, Feeny D, Torrance G. The health utilities index (HUI): Concepts, measurement properties and applications. Health Qual Life Outcomes. 2003;1:54. doi: 10.1186/1477-7525-1-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Skevington SM, Lotfy M, O’Connell KA WHOQOL Group. The World Health Organization's WHOQOL-BREF quality of life assessment: Psychometric properties and results of the international field trial. A report from the WHOQOL group. Qual Life Res. 2004;13:299–310. doi: 10.1023/B:QURE.0000018486.91360.00. [DOI] [PubMed] [Google Scholar]
- 11.Hsiung PC, Fang CT, Chang YY, Chen MY, Wang JD. Comparison of WHOQOL-bREF and SF-36 in patients with HIV infection. Qual Life Res. 2005;14:141–50. doi: 10.1007/s11136-004-6252-z. [DOI] [PubMed] [Google Scholar]
- 12.Thakar S, Christopher S, Rajshekhar V. Quality of life assessment after central corpectomy for cervical spondylotic myelopathy: Comparative evaluation of the 36-item short form health survey and the World Health Organization quality of life-bref. J Neurosurg Spine. 2009;11:402–12. doi: 10.3171/2009.4.SPINE08749. [DOI] [PubMed] [Google Scholar]
- 13.Aggarwal AN, Gupta D, Janmeja AK, Jindal SK. Assessment of health-related quality of life in patients with pulmonary tuberculosis under programme conditions. Int J Tuberc Lung Dis. 2013;17:947–53. doi: 10.5588/ijtld.12.0299. [DOI] [PubMed] [Google Scholar]
- 14.Bauer M, Leavens A, Schwartzman K. A systematic review and meta-analysis of the impact of tuberculosis on health-related quality of life. Qual Life Res. 2013;22:2213–35. doi: 10.1007/s11136-012-0329-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Deribew A, Deribe K, Reda AA, Tesfaye M, Hailmichael Y, Maja T, et al. Change in quality of life: A follow up study among patients with HIV infection with and without TB in Ethiopia. BMC Public Health. 2013;13:408. doi: 10.1186/1471-2458-13-408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Masumoto S, Yamamoto T, Ohkado A, Yoshimatsu S, Querri AG, Kamiya Y, et al. Factors associated with health-related quality of life among pulmonary tuberculosis patients in Manila, the Philippines. Qual Life Res. 2014;23:1523–33. doi: 10.1007/s11136-013-0571-x. [DOI] [PubMed] [Google Scholar]
- 17.Nurhidayati A, Ivone J, Winata T. Thesis. Bandung: Maranatha Christian University; 2015. A Survey on Lung Tuberculosis Patients in Pamarican Primary Health Care, Ciamis, Indonesia. [Google Scholar]
- 18.Purba FD, Hunfeld JA, Iskandarsyah A, Fitriana TS, Sadarjoen SS, Passchier J, et al. Quality of life of the indonesian general population: Test-retest reliability and population norms of the EQ-5D-5L and WHOQOL-BREF. PLoS One. 2018;13:e0197098. doi: 10.1371/journal.pone.0197098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ch Salim O, Sudharma NI, Kusumaratna RK, Hidayat A. Validity and reliability of World Health Organization quality of life-bref to assess the quality of life in the elderly. Univ Med. 2007;26:27–38. [Google Scholar]
- 20.Djoerban Z. Validity and reability test of Indonesian version of world health the quality of life patients with HIV/AIDS. J Intern Med Indones. 2017;4:112–8. [Google Scholar]
- 21.Abdullah L. Validation of an instrument for measuring quality of life amongst Malaysian youth. Mod Appl Sci. 2014;8:22–35. [Google Scholar]
- 22.Silva PA, Soares SM, Santos JF, Silva LB. Cut-off point for WHOQOL-bref as a measure of quality of life of older adults. Rev Saude Publica. 2014;48:390–7. doi: 10.1590/S0034-8910.2014048004912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gholami A, Araghi MT, Shamsabadi F, Bayat M, Dabirkhani F, Moradpour F, et al. Application of the World Health Organization quality of life instrument, short form (WHOQOL-BREF) to patients with cataract. Epidemiol Health. 2016;38:e2016005. doi: 10.4178/epih.e2016005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hansel NN, Wu AW, Chang B, Diette GB. Quality of life in tuberculosis: Patient and provider perspectives. Qual Life Res. 2004;13:639–52. doi: 10.1023/B:QURE.0000021317.12945.f0. [DOI] [PubMed] [Google Scholar]
- 25.Dhuria M, Sharma N, Ingle G. Impact of tuberculosis on the quality of life. Indian J Community Med. 2008;33:58–9. doi: 10.4103/0970-0218.39249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Guo N, Marra F, Marra CA. Measuring health-related quality of life in tuberculosis: A systematic review. Health Qual Life Outcomes. 2009;7:14. doi: 10.1186/1477-7525-7-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chamla D. The assessment of patients’ health-related quality of life during tuberculosis treatment in Wuhan, China. Int J Tuberc Lung Dis. 2004;8:1100–6. [PubMed] [Google Scholar]
- 28.Duyan V, Kurt B, Aktas Z, Duyan GC, Kulkul DO. Relationship between quality of life and characteristics of patients hospitalised with tuberculosis. Int J Tuberc Lung Dis. 2005;9:1361–6. [PubMed] [Google Scholar]
- 29.Kittikraisak W, Kingkaew P, Teerawattananon Y, Yothasamut J, Natesuwan S, Manosuthi W, et al. Health related quality of life among patients with tuberculosis and HIV in Thailand. PLoS One. 2012;7:e29775. doi: 10.1371/journal.pone.0029775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Darvishpoor Kakhki A, Masjedi MR. Factors associated with health-related quality of life in tuberculosis patients referred to the National Research Institute of Tuberculosis and Lung Disease in Tehran. Tuberc Respir Dis (Seoul) 2015;78:309–14. doi: 10.4046/trd.2015.78.4.309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Adeyeye OO, Ogunleye OO, Coker A, Kuyinu Y, Bamisile RT, Ekrikpo U, et al. Factors influencing quality of life and predictors of low quality of life scores in patients on treatment for pulmonary tuberculosis: A cross sectional study. J Public Health Afr. 2014;5:366. doi: 10.4081/jphia.2014.366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Webster PC. Indonesia: Islam and health. Can Med Assoc J. 2013;185:E101–2. doi: 10.1503/cmaj.109-4364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Larson DB, Sherrill KA, Lyons JS, Craigie FC, Jr, Thielman SB, Greenwold MA, et al. Associations between dimensions of religious commitment and mental health reported in the American Journal of Psychiatry and Archives of General Psychiatry: 1978-1989. Am J Psychiatry. 1992;149:557–9. doi: 10.1176/ajp.149.4.557. [DOI] [PubMed] [Google Scholar]
- 34.Verghese A. Spirituality and mental health. Indian J Psychiatry. 2008;50:233–7. doi: 10.4103/0019-5545.44742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Courtwright A, Turner AN. Tuberculosis and stigmatization: Pathways and interventions. Public Health Rep. 2010;125(Suppl 4):34–42. doi: 10.1177/00333549101250S407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Demissie M, Getahun H, Lindtjørn B. Community tuberculosis care through “B clubs” in rural North Ethiopia. Soc Sci Med. 2003;56:2009–18. doi: 10.1016/s0277-9536(02)00182-x. [DOI] [PubMed] [Google Scholar]
- 37.Hadley M, Maher D. Community involvement in tuberculosis control: Lessons from other health care programmes. Int J Tuberc Lung Dis. 2000;4:401–8. [PubMed] [Google Scholar]


