Abstract
Background:
Health literacy reflects a person's reading and numeracy abilities applied to understanding health-related information. These skills may influence how patients report symptoms, leading to underestimates or overestimates of symptom severity. No prior studies have examined health literacy measurement bias.
Objective:
The purpose of the current study was to determine whether PROMIS (Patient-Reported Outcomes Measurement Information System) anxiety and depression short forms, administered by interview, capture symptoms equally across health literacy groups. We examined the psychometric properties of PROMIS anxiety and depression short forms using differential item functioning (DIF) analysis by level of health literacy.
Methods:
The sample analyzed included 888 adults, age 55 to 74 years, in Chicago, IL. Health literacy was measured using the Test of Functional Health Literacy in Adults. PROMIS short forms assessed anxiety and depression.
Key Results:
DIF was present in 3 of 8 depression items, and 3 of 7 anxiety items. All items flagged for DIF had lower item-slopes for people with limited health literacy.
Conclusions:
Items with DIF were less strongly related to anxiety and depression, and thus less precise. Overall, impact of DIF on PROMIS scores was negligible, likely mitigated by interview administration. Although overall test impact of health literacy was minimal, DIF analyses flagged items that were potentially too complex for people with limited health literacy. Design and validation of patient-reported surveys should incorporate respondents with a range of health literacy and methods to identify and reduce measurement bias. [HLRP: Health Literacy Research and Practice. 2019;3(3):e196–e204.]
Plain Language Summary:
This study suggests that people with limited health literacy may respond differently to questions about depression and anxiety than people with adequate health literacy. Therefore, it is important to be aware of differences in literacy ability when creating and using questionnaires.
Health care considers self-report measures a vital sign (Dahl, Saeger, Stein, & Huss, 2000; Glasgow, Kaplan, Ockene, Fisher, & Emmons, 2012). Patients may not accurately comprehend questions about their health if limited health literacy interferes with understanding. Moreover, patients with low health literacy may feel uncomfortable answering questions about their health. Interview administration may mitigate the effects of limited health literacy on self-report. Some research has used a method where trained interviewers read self-report questions to patients and record patient responses, but whether this method is effective is unknown. Therefore, we analyzed this method of interview administration.
This study examined how health literacy influences interview assessment of anxiety and depression. Mood and anxiety disorders are a public health concern (Kessler et al., 2003; Kessler, Petukhova, Sampson, Zaslavsky, & Wittchen, 2012). The World Health Organization predicts that depression will be the second highest cause of disability by 2020 (Kessler & Bromet, 2013). The lifetime prevalence of unipolar depression and anxiety disorders have been reported at 17% and 29%, respectively (Kessler et al., 2005). Accurate assessment of depression and anxiety is necessary. As such, the Patient-Reported Outcomes Measurement Information System (PROMIS) includes depression and anxiety measures (Pilkonis et al., 2011), but it is unknown whether these items are precise across levels of health literacy. The current study examines how health literacy affects the psychometric properties of PROMIS depression and anxiety items (Cella et al., 2007, 2010, 2015; Pilkonis et al., 2011).
Health literacy is the “degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions” (Kindig, Panzer, Nielsen-Bohlman, 2004; Ratzan & Parker, 2000). People with limited health literacy are, on average, less knowledgeable about their disease and treatment, less able to successfully perform self-care tasks, and have poorer self-efficacy. This translates to worse health outcomes including greater hospitalization, mortality risk, use of emergency services, and decreased use of preventive care (e.g., Baker, 2006; Baker, Parker, Williams, & Clark, 1998; Berkman, Sheridan, Donahue, Halpern, & Crotty, 2011; Kindig, Panzer, Nielsen-Bohlman, 2004; Paasche-Orlow & Wolf, 2007; Vandenbosch et al., 2016).
People with limited health literacy have difficulty with information that is needed to care for oneself and navigate the health care system (Wolf et al., 2012). Thus, providers must find ways of communicating clearly with patients across levels of health literacy. Health literacy is distinct from literacy or educational attainment alone; it is specific to communication within the health care context (Nutbeam, 2008). Research has yet to explore differential item functioning (DIF) by health literacy. DIF is a way to statistically quantify whether group membership, in the current study having limited versus adequate health literacy, affects the relationship that a questionnaire item has to the concept it measures (depression or anxiety in this case). Jones and Gallo (2002) found DIF by educational attainment on the Mini-Mental State Examination; cognitive errors were overestimated in participants with lower education. Teresi et al. (2009), found DIF by education in 1 of 32 PROMIS depression items. Health literacy is determined by many sociodemographic variables, including education, but health literacy is a stronger predictor of health outcomes than education alone (Paasche-Orlow & Wolf, 2007). Therefore, health literacy has implications for health care utilization. Research is needed on improved means of assessment for people with limited health literacy.
Objective
The purpose of the present study was to analyze the psychometric properties of PROMIS Short Form v1.0 Depression - 8b and PROMIS Short Form v1.0 - Anxiety - 7a by level of health literacy. We hypothesized that DIF across level of health literacy would be observed for items on both short forms. If DIF was present, we examined whether it was uniform or non-uniform. We calculated correlations between depression, anxiety, and health literacy. We expected our sample to reflect the well-known association between depression and anxiety. To our knowledge, this is the first study to examine the impact of health literacy on DIF.
Methods
The present study is a secondary analysis of “LitCog,” a National Institute on Aging study (for further details, see Serper et al., 2014; Smith, Curtis, Wardle, Wagner, & Wolf, 2013; Wolf et al., 2012). LitCog assessed health literacy and cognition in older adults. The sample included 888 English-speaking patients, age 55 to 74 years, recruited from an academic general internal medicine clinic and four federally qualified health centers in Chicago, IL.
Procedure
Participants completed two structured interviews 7 to 10 days apart. A trained research assistant guided patients through a series of assessments that, on Day 1, included basic demographic information, socioeconomic status, comorbidity, health literacy, PROMIS measures, and an assessment of performance on everyday health tasks. On Day 2, the same patients completed a cognitive battery to measure processing speed, working memory, inductive reasoning, long-term memory, prospective memory, and verbal ability. Northwestern University's Institutional Review Board approved the study. All measures used in the present analyses were administered on Day 1.
Measures
Depression and Anxiety
The National Institutes of Health conducted an initiative to design standardized questionnaires to evaluate patient-reported outcomes with reliable scores and valid interpretations (Cella et al., 2007, 2010; Fries, Bruce, & Cella, 2005; Hays, Bjorner, Revicki, Spritzer, & Cella, 2009; Liu et al., 2010). We examined the psychometric properties of PROMIS anxiety and depression short forms, administered by interview, across levels of health literacy. PROMIS Short Form v1.0 Depression - 8b comprises eight items rated on 5-point frequency scales (never to always). All items begin with “In the past seven days…” Example depression items included “I felt hopeless” and “I felt I had nothing to look forward to” (Pilkonis et al., 2011). PROMIS Short Form v1.0 - Anxiety - 7a includes seven items rated on 5-point frequency scales. Example anxiety items included “I felt nervous” and “I found it hard to focus on anything other than my anxiety.” Raw total scores for both scales were transformed into T scores. The United States population mean T score is, by definition, 50 with standard deviation of 10. Both surveys show excellent internal consistency as demonstrated by the mean adjusted item–total correlations (depression: r = .83; anxiety: r = .79) and alpha coefficients (depression: α = .95; anxiety: α = .93; Pilkonis et al., 2011). In LitCog, an interviewer verbally administered the depression and anxiety short forms.
Health Literacy
Health literacy was measured using the Test of Functional Health Literacy in Adults (TOFHLA; Parker, Baker, Williams, & Nurss, 1995), one of the most common health literacy assessments (Baker, 2006). The numeracy section is interview based; participants receive prompts, and the interviewer poses a set of questions and records responses. Numeracy items test comprehension of directions for health tasks (e.g., taking medication as prescribed and keeping medical appointments). The literacy portion is paper based; participants work independently to answer multiple choice questions assessing comprehension. Literacy content includes health care documents (e.g., sections of an informed consent form and a Medicaid application; Parker et al., 1995). Total scores range from 0 to 100, with numeracy and literacy subscales each ranging from 0 to 50. A total score greater than or equal to 75 indicates adequate health literacy, whereas less than 75 reflects limited health literacy. The TOFHLA has high internal consistency (Cronbach's alpha = 0.98) and test-retest reliability (Spearman-Brown coefficient = 0.92). Moreover, it demonstrates excellent construct validity as it is highly correlated with measures of literacy—the Rapid Estimate of Adult Literacy in Medicine (Spearman's rho = 0.84) and the Wide Range Achievement Test-Revised (Spearman's rho = 0.74; Parker et al., 1995).
Differential Item Functioning
DIF can be used as a method to identify whether level of health literacy impacts the relationship between a questionnaire and the concept it measures (i.e., depression or anxiety in this study). DIF exists when “an item favor[s] matched examinees from one group over another” (Shealy & Stout, 1993). Thus, respondents from different groups consistently answer items differently (Reeve & Fayers, 2005). DIF exists when there is a difference in the strength of the relationship between a questionnaire item and a concept across groups. DIF is derived from Item Response Theory (IRT; for review see Cho, Suh, & Lee, 2016). If an item displays DIF, the level of depression or anxiety may be under- or overestimated in people with limited health literacy. DIF can be uniform or non-uniform (Swaminathan & Rogers, 1990). Uniform DIF could exist if the effect of health literacy is constant across levels of depression and anxiety. Non-uniform DIF could be present if, as depression and anxiety change, the effect of health literacy also changes. Even if the level of DIF for individual items is small, if several test items display DIF then the discrepancy between groups may exist for the test as a whole (Shealy & Stout, 1993). This introduces a problem for the construct validity of item score interpretations across groups. Therefore, examining DIF across groups with distinct health literacy capabilities for PROMIS anxiety and depression scales is crucial for accurate assessment. DIF analysis may flag items that may be difficult for people with limited health literacy and may be a useful adjunct to qualitative reviews of items and cognitive interviewing (Collins, 2014; Miller, Chepp, Willson, & Padilla, 2014) during test development.
Analytical Strategy
We performed DIF analyses on each item of the PROMIS short forms for anxiety and depression, using the lordif package in R (Choi, Gibbons, & Crane, 2011). A graded response model is an appropriate IRT model because item responses were polytomous and ordered (Reeve & Fayers, 2005; Samejima, 2016). Note, lordif flags items with DIF based on effect-size measures rather than statistical significance. After conducting DIF analyses, we inspected individual items to determine whether item attributes (e.g., item length) were related to DIF across health literacy levels.
Monte Carlo simulations were used to determine the appropriate cutoff for detecting DIF. The Monte Carlo procedure creates simulated datasets under the null hypothesis of no DIF, creating an empirical distribution of effect sizes (Choi et al., 2011). We selected 500 iterations as sufficient to consistently detect the same items flagged for DIF. An effect size is selected at the tail of the distribution based on a chosen alpha level (Choi et al., 2011). We chose α = .01 to indicate possible DIF and used the McFadden pseudo R2 as the effect size.
Results
Descriptive Statistics
Descriptive statistics are presented in Table 1. Unsurprisingly based on prior work (e.g., Berkman et al., 2011; Paasche-Orlow & Wolf, 2007), level of education differed by health literacy group, such that 14% of people with adequate health literacy had a high school degree or less, compared to 63% of people with limited health literacy. Furthermore, 39% of participants with adequate health literacy completed a graduate degree, compared to only 6% of participants with limited health literacy. Race also differed by health literacy group. Seventy-six percent of people with limited health literacy were Black/African American and 11% were White. Conversely, 61% of people with adequate health literacy were White and 30% were Black/African American.
Table 1.
Sample Characteristics
| Characteristic | Overall SampleaN = 900 (%) | Adequate Literacy n = 604 (%) | Limited Literacy n = 284 (%) |
|---|---|---|---|
|
| |||
| Mean age, years (SD) | 63.1 (5.5) | 62.8 (5.3) | 63.8 (5.8) |
|
| |||
| Sex | |||
| Male | 618 (69) | 416 (69) | 194 (68) |
| Female | 282 (31) | 188 (31) | 90 (32) |
|
| |||
| Education | |||
| High school or less | 264 (29) | 83 (14) | 179 (63) |
| Some college or technical school | 206 (23) | 131 (22) | 70 (25) |
| College graduate | 174 (19) | 153 (25) | 18 (6) |
| Graduate degree | 256 (28) | 237 (39) | 17(6) |
|
| |||
| Ethnicity/race | |||
| White | 404 (45) | 368 (61) | 30 (11) |
| Black/African American | 401 (45) | 179 (30) | 216 (76) |
| Hispanic/Latinx | 21 (2) | 10 (2) | 11 (4) |
| Asian | 17 (2) | 10 (2) | 7 (2) |
| Other | 52 (6) | 33 (5) | 19 (7) |
| Missing | 5 (<1) | 4 (<1) | 1 (<1) |
Note.
Health literacy groups include 888 participants total; 12 did not complete the Test of Functional Health Literacy in Adults.
The sample (N = 888) had a mean TOFHLA score of 76.26 ± 16.29. The numeracy and reading subscale mean scores were 32.78 ± 8.65 and 43.45 ± 9.59, respectively. Approximately one-third (32%) of the sample had limited health literacy. The average PROMIS depression and anxiety T scores were 47.8 ± 9.1 and 53.2 ± 8.9, respectively. Mean levels of depression and anxiety of the sample were near the US population mean (T = 50). Bivariate correlations are presented in Table 2. As expected, depression and anxiety were strongly and positively associated (r = .73, p < .001). Although the relationship between depression and anxiety significantly differed by health literacy group, z = 2.19, p < .05, the effect sizes were similar (r = .78 for limited health literacy, r = .71 for adequate health literacy).
Table 2.
Bivariate Correlations Among the Study Variables
| Variable | N | 1 | 2 | 3 | 4 |
|---|---|---|---|---|---|
|
| |||||
| 1. Anxiety T Score | 897 | ||||
| 2. Depression T Score | 899 | .73*** | |||
| 3. TOFHLA Numeracy Score | 892 | −.11*** | −.20*** | ||
| 4. TOFHLA Reading Score | 895 | −.07* | −.17*** | .60*** | |
| 5. TOFHLA Total Score | 888 | −.10** | −.20*** | .88*** | .91*** |
Note. TOFHLA = Test of Functional Health Literacy in Adults.
p < .05;
p < .01;
p < .001
Differential Item Functioning
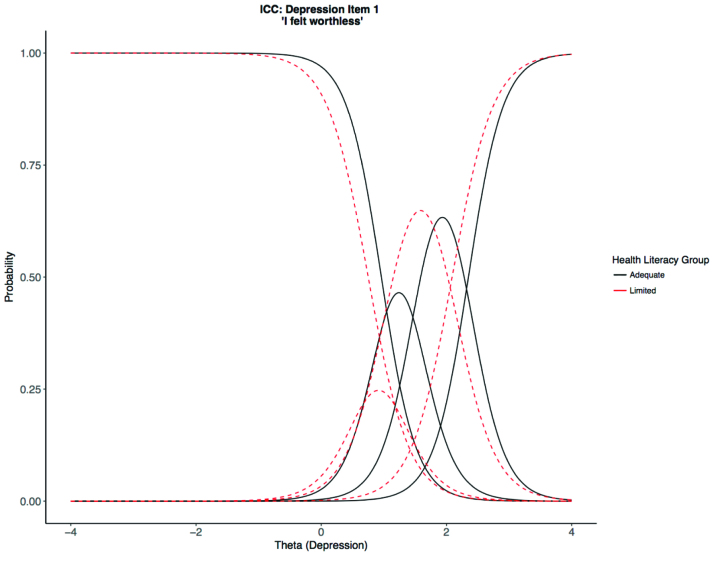
DIF analyses in lordif allow for one grouping variable in the model; we used health literacy as the grouping variable. Five hundred iterations of Monte Carlo simulation at α = .01 (i.e., the cutoff for the upper 1% of the Monte Carlo distribution) suggested effect sizes that exceeded McFadden pseudo R2 = .002 were indicative of possible DIF. Thus, we used R2 = .002 as the cutoff for flagging items for DIF in the observed data. A total effect of DIF was present in 3 of the 8 depression items. “I felt worthless” displayed uniform DIF, slope for limited health literacy, alimited = 3.06; slope for adequate health literacy, aadequate = 3.60; R2 = .018 (Figure 1). “I felt hopeless” displayed uniform DIF, alimited = 4.93; aadequate = 5.61; R2 = .007. “I felt depressed” showed non-uniform DIF, alimited = 2.88; aadequate = 4.22; R2 = .006.
Figure 1.
Example item characteristic curves (ICCs) exhibiting differential item functioning for the item “I felt worthless” on depression short form 8b. Theta is the depression metric on a standardized scale (M = 0, SD = 1 by definition). In this example, there are three rather than four thresholds (curve intersections); if fewer than five participants used a response category, categories were automatically collapsed by lordif. In this case, often and always were collapsed into one category.
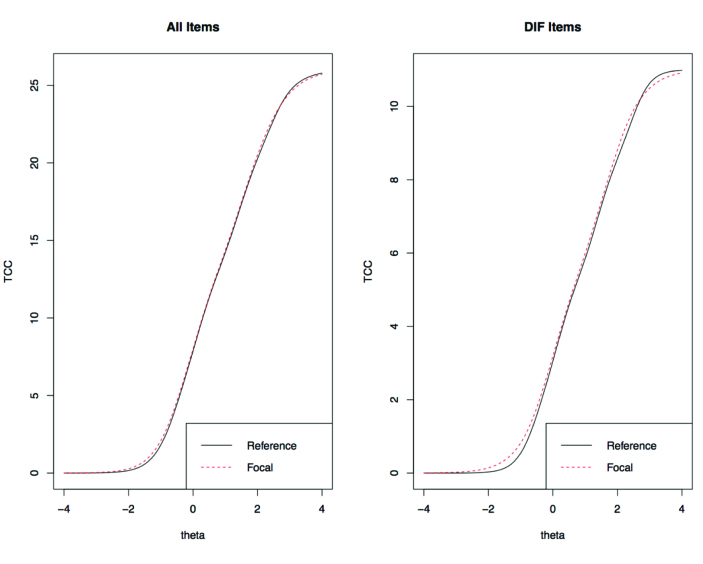
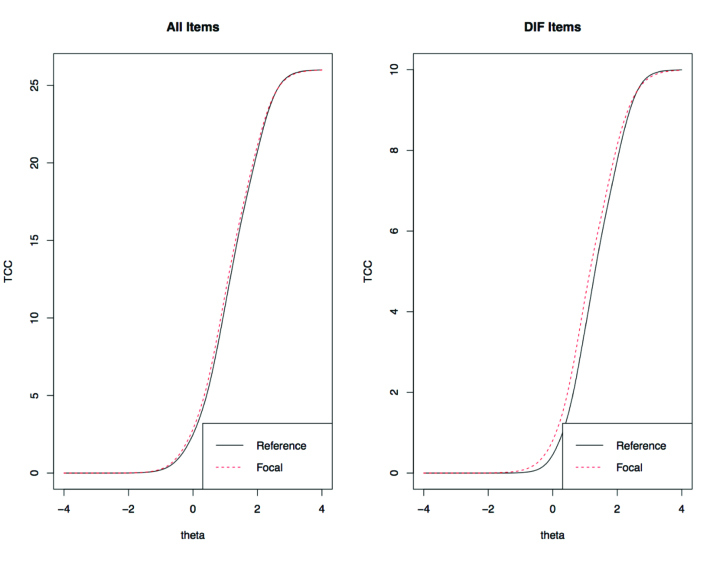
A small total effect of DIF was present for 3 of the 7 anxiety items. “I felt anxious” had uniform DIF, alimited = 1.91; aadequate = 3.15; R2 = .004. “I felt nervous” had uniform DIF, alimited = 3.52; aadequate = 3.92; R2 = .004. “I found it hard to focus on anything other than my anxiety” displayed non-uniform DIF, alimited = 1.95; aadequate = 2.78; R2 = .004. Figures 2A–2B show the test characteristic curves (TCCs) for anxiety and depression, respectively. The overlapping lines suggest that DIF negligibly impacted PROMIS T scores.
Figure 2.
(A) Test characteristic curves (TCCs) for anxiety short form 7a. The TCCs for limited versus adequate health literacy are overlapping, suggesting that measurement precision for the anxiety Patient-Reported Outcomes Measurement Information System (PROMIS) scale is similar across the two groups, across level of anxiety. Reference denotes adequate literacy; Focal denotes limited literacy. Theta is the anxiety metric on a standardized scale (M = 0, SD = 1 by definition). (B) TCCs for depression short form 8b. The TCCs for limited versus adequate health literacy are overlapping, suggesting that measurement precision for the depression PROMIS scale is similar across the two groups, across level of depression. Reference denotes adequate literacy; focal denotes limited literacy. Theta is the depression metric on a standardized scale (M = 0, SD = 1 by definition). DIF = differential item functioning.
Discussion
As predicted, we observed DIF by health literacy group. Six of 15 items on PROMIS anxiety and depression short forms displayed DIF with small effect sizes (negligible according to the R2 < .13 guideline suggested by Choi et al., 2011). TCCs for depression and anxiety scales showed little difference in total response between health literacy groups (Figures 2A–2B). Therefore, health literacy did not influence PROMIS T scores administered by interview. Interview administration was employed as a strategy to lessen the impact of health literacy on self-report, because the interviewer can verify participant comprehension (Doak, Doak, Friedell, & Meade, 1998). Even if health literacy did not impact overall test precision for PROMIS short forms, flagging individual items with DIF is valuable because it identifies items that are potentially problematic for people with limited health literacy. As Edelen and Reeve (2007) note—the advantage of IRT applications, including DIF, is “detailed item-level information” (p. 16). If the scales were completed as paper and pencil or on a computer, items may have shown ever greater DIF owing to the need for the participant to read the items.
Other studies have found negligible DIF of PROMIS items yet propose the value of examining DIF as a tool to implement assessments appropriately (e.g., Cook, Bamer, Amtmann, Molton, & Jensen, 2012; Coster et al., 2016; Hong et al., 2016). Moreover, similar effect sizes (pseudo R2 = .001 to .003) have been associated with impactful DIF in other studies (Crane et al., 2007). PROMIS was developed through evidence-based design. Hence, these analyses may be informative for questionnaires that have been designed less rigorously; that is, other questions with more complex questions might show even greater DIF. Researchers and clinicians should be cognizant of the effects of health literacy group on assessment. DIF analyses can elucidate issues within individual items. For example, “I felt depressed” may have shown DIF because “depressed” may be a low frequency word in everyday language, is often stigmatized, or it can have different meanings to different people (e.g., sadness vs. loss of interest). The item “I found it hard to focus on anything other than my anxiety” may have exhibited DIF because it requires some metacognition (i.e., thinking about anxiety); it is also longer than other items.
At the item level, health literacy influenced the item characteristic curves of six PROMIS depression and anxiety items, even with interview administration to potentially reduce impact of health literacy. All items flagged for DIF had lower item-slopes for people with limited health literacy (Figure 1), suggesting that these items were less strongly related to the constructs of anxiety and depression, and thus, less precise. The current analyses can guide the design of questionnaires to capture patients' symptomatology regardless of health literacy ability. Researchers can calculate an effect size and use the magnitude as a decision-making tool for how to handle each item where DIF is present (Cho et al., 2016). For example, if DIF exceeds the calculated effect size and if item length contributes to DIF, then the item could be revised. The design and validation of questionnaires should incorporate respondents with a range of health literacy and methods to identify and thus eliminate measurement bias. PROMIS measures were developed with reading level in mind, so other questionnaires may exhibit much more DIF if literacy is not considered in the questionnaire-development process.
Limitations and Future Directions
We acknowledge several limitations. First, the analyses were cross-sectional. Future studies may benefit from examining the longitudinal effect of health literacy on testing. Second, depression and anxiety in this sample were in the average range. Different results might be found in a clinical sample with higher levels of and/or more variability in depression and anxiety. Third, PROMIS was administered in a non-standard way (i.e., by interview). That said, it is possible that health literacy effects would have been greater had the participants been asked to read the questions on their own. Research has shown that people with limited literacy have poorer comprehension of health material, and that methods such as Teach-Back, whereby patients explain their understanding to an interviewer, are recommended (e.g., Kripalani, Bengtzen, Henderson, & Jacobson, 2008). Going forward, it is important to consider methods of improving comprehension, especially in the context of our digital world, where there are disparities in use of technology in people with limited literacy compared to those with adequate literacy (Bailey et al., 2014). Health literacy is a global concept that attempts to integrate various factors (e.g., education, socioeconomic status) that contribute to understanding of health-related information (Paasche-Orlow & Wolf, 2007). Future research may tease apart the individual contributions to health literacy as they relate to depression and anxiety assessment.
Conclusions
This study addressed the effects of health literacy on DIF of PROMIS anxiety and depression short forms. DIF analysis is important because if questions are not equally applicable (Reeve & Fayers, 2005) across health literacy groups, the validity of interpretations between groups on the measured construct is undermined. Examining individual item characteristics provides rich information about how group disparities impact assessment. Whether or not group differences affect the scale as a whole, placing assessment in the context of the patient informs research and clinical judgment. An item with DIF across health literacy may result in a different testing experience for participants; DIF analysis can identify these items.
References
- Bailey S. C. O'conor R. Bojarski E. A. Mullen R. Patzer R. E. Vicencio D. Wolf M. S. (2014). Literacy disparities in patient access and health-related use of Internet and mobile technologies. Health Expectations, 18(6), 3079–3087. 10.1111/hex.12294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker D. W. (2006). The meaning and the measure of health literacy. Journal of General Internal Medicine, 21(8), 878–883. 10.1111/j.1525-1497.2006.00540.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker D. W. Parker R. M. Williams M. V. Clark W. S. (1998). Health literacy and the risk of hospital admission. Journal of General Internal Medicine, 13(12), 791–798. 10.1046/j.1525-1497.1998.00242.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berkman N. D. Sheridan S. L. Donahue K. E. Halpern D. J. Crotty K. (2011). Low health literacy and health outcomes: An updated systematic review. Annals of Internal Medicine, 155(2), 97–107. 10.7326/0003-4819-155-2-201107190-00005 [DOI] [PubMed] [Google Scholar]
- Cella D. Hahn E. Jensen S. Butt Z. Nowinski C. Rothrock N. Lohr K. (2015). Patient-reported outcomes in performance measurement. Retrieved from RTI International website: http://www.rti.org/publication/patient-reported-outcomes-performance-measurement 10.3768/rtipress.2015.bk.0014.1509 [DOI] [PubMed]
- Cella D. Riley W. Stone A. Rothrock N. Reeve B. Yount S. Hays R. (2010). The Patient-Reported Outcomes Measurement Information System (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005–2008. Journal of Clinical Epidemiology, 63(11), 1179–1194. 10.1016/j.jclinepi.2010.04.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cella D. Yount S. Rothrock N. Gershon R. Cook K. Reeve B. Rose M. (2007). The Patient-Reported Outcomes Measurement Information System (PROMIS). Medical Care, 45(Suppl. 1), S3–S11. 10.1097/01.mlr.0000258615.42478.55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cho S. J. Suh Y. Lee W. Y. (2016). After differential item functioning is detected: IRT item calibration and scoring in the presence of DIF. Applied Psychological Measurement, 40(8), 573–591. 10.1177/0146621616664304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi S. W. Gibbons L. E. Crane P. K. (2011). Lordif: An R package for detecting differential item functioning using iterative hybrid ordinal logistic regression/item response theory and Monte Carlo simulations. Journal of Statistical Software, 39(8), 1–30. 10.18637/jss.v039.i08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins D. (2014). Cognitive Interviewing practice. Los Angeles, CA: SAGE. [Google Scholar]
- Cook K. F. Bamer A. M. Amtmann D. Molton I. R. Jensen M. P. (2012). Six patient-reported outcome measurement information system short form measures have negligible age- or diagnosis-related differential item functioning in individuals with disabilities. Archives of Physical Medicine and Rehabilitation, 93(7), 1289–1291. 10.1016/j.apmr.2011.11.022 [DOI] [PubMed] [Google Scholar]
- Coster W. J. Ni P. Slavin M. D. Kisala P. A. Nandakumar R. Mulcahey M. J. Jette A. M. (2016). Differential item functioning in the Patient Reported Outcomes Measurement Information System Pediatric Short Forms in a sample of children and adolescents with cerebral palsy. Developmental Medicine & Child Neurology, 58(11), 1132–1138. 10.1111/dmcn.13138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crane P. K. Gibbons L. E. Ocepek-Welikson K. Cook K. Cella D. Narasimhalu K. Teresi J. A. (2007). A comparison of three sets of criteria for determining the presence of differential item functioning using ordinal logistic regression. Quality of Life Research, 16(Suppl. 1), 69–84. 10.1007/s11136-007-9185-5 [DOI] [PubMed] [Google Scholar]
- Dahl J. L. Saeger L. Stein W. Huss R. D. (2000). The new JCAHO pain assessment standards: Implications for the medical director. Journal of the American Medical Directors Association, 1(Suppl. 6), S24–S31. [PubMed] [Google Scholar]
- Doak C. C. Doak L. G. Friedell G. H. Meade C. D. (1998). Improving comprehension for cancer patients with low literacy skills: Strategies for clinicians. CA: A Cancer Journal for Clinicians, 48(3), 151–162. 10.3322/canjclin.48.3.151 [DOI] [PubMed] [Google Scholar]
- Edelen M. O. Reeve B. B. (2007). Applying item response theory (IRT) modeling to questionnaire development, evaluation, and refinement. Quality of Life Research, 16(Suppl. 1), S5–S18. 10.1007/s11136-007-9198-0 [DOI] [PubMed] [Google Scholar]
- Fries J. F. Bruce B. Cella D. (2005). The promise of PROMIS: Using item response theory to improve assessment of patient-reported outcomes. Clinical and Experimental Rheumatology, 23(5), S53–S57. [PubMed] [Google Scholar]
- Glasgow R. E. Kaplan R. M. Ockene J. K. Fisher E. B. Emmons K. M. (2012). Patient-reported measures of psychosocial issues and health behavior should be added to electronic health records. Health Affairs, 31(3), 497–504. 10.1377/hlthaff.2010.1295 [DOI] [PubMed] [Google Scholar]
- Hays R. D. Bjorner J. B. Revicki D. A. Spritzer K. L. Cella D. (2009). Development of physical and mental health summary scores from the Patient-Reported Outcomes Measurement Information System (PROMIS) global items. Quality of Life Research, 18(7), 873–880. 10.1007/s11136-009-9496-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hong I. Velozo C. A. Li C.-Y. Romero S. Gruber-Baldini A. L. Shulman L. M. (2016). Assessment of the psychometrics of a PROMIS item bank: Self-efficacy for managing daily activities. Quality of Life Research, 25(9), 2221–2232. 10.1007/s11136-016-1270-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones R. N. Gallo J. J. (2002). Education and sex differences in the Mini-Mental State Examination: Effects of differential item functioning. The Journals of Gerontology: Series B, 57(6), P548–P558. 10.1093/geronb/57.6.P548 [DOI] [PubMed] [Google Scholar]
- Kessler R. C. Berglund P. Demler O. Jin R. Koretz D. Merikangas K. R. Wang P. S. (2003). The epidemiology of major depressive disorder: Results from the National Comorbidity Survey Replication (NCS-R). The Journal of the American Medical Association, 289(23), 3095–3105. 10.1001/jama.289.23.3095 [DOI] [PubMed] [Google Scholar]
- Kessler R. C. Berglund P. Demler O. Jin R. Merikangas K. R. Walters E. E. (2005). Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry, 62(6), 593–602. 10.1001/archpsyc.62.6.593 [DOI] [PubMed] [Google Scholar]
- Kessler R. C. Bromet E. J. (2013). The epidemiology of depression across cultures. Annual Review of Public Health, 34(1), 119–138. 10.1146/annurev-publhealth-031912-114409 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler R. C. Petukhova M. Sampson N. A. Zaslavsky A. M. Wittchen H.-U. (2012). Twelve-month and lifetime prevalence and lifetime morbid risk of anxiety and mood disorders in the United States. International Journal of Methods in Psychiatric Research, 21(3), 169–184. 10.1002/mpr.1359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kindig D. A., Panzer A. M., Nielsen-Bohlman L. (Eds.). (2004). Health literacy: A prescription to end confusion . Retrieved from National Academies Press website: https://www.nap.edu/catalog/10883/health-literacy-a-prescription-to-end-confusion [PubMed]
- Kripalani S. Bengtzen R. Henderson L. E. Jacobson T. A. (2008). Clinical research in low-literacy populations: Using teach-back to assess comprehension of informed consent and privacy information. IRB: Ethics & Human Research, 30(2), 13–19. [PubMed] [Google Scholar]
- Liu H. Cella D. Gershon R. Shen J. Morales L. S. Riley W. Hays R. D. (2010). Representativeness of the PROMIS Internet Panel. Journal of Clinical Epidemiology, 63(11), 1169–1178. 10.1016/j.jclinepi.2009.11.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller K. Chepp V. Willson S. Padilla J. L. (2014). Cognitive interviewing methodology. Hoboken, NJ: John Wiley & Sons. [Google Scholar]
- Nutbeam D. (2008). The evolving concept of health literacy. Social Science & Medicine, 67(12), 2072–2078. 10.1016/j.socscimed.2008.09.050 [DOI] [PubMed] [Google Scholar]
- Paasche-Orlow M. K. Wolf M. S. (2007). The causal pathways linking health literacy to health outcomes. American Journal of Health Behavior, 31(Suppl. 1), S19–S26. 10.5993/AJHB.31.s1.4 [DOI] [PubMed] [Google Scholar]
- Parker R. M. Baker D. W. Williams M. V. Nurss J. R. (1995). The test of functional health literacy in adults. Journal of General Internal Medicine, 10(10), 537–541. 10.1007/BF02640361 [DOI] [PubMed] [Google Scholar]
- Pilkonis P. A. Choi S. W. Reise S. P. Stover A. M. Riley W. T. Cella D. PROMIS Cooperative Group. (2011). Item banks for measuring emotional distress from the Patient-Reported Outcomes Measurement Information System (PROMIS®): Depression, anxiety, and anger. Assessment, 18(3), 263–283. 10.1177/1073191111411667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ratzan S. C. Parker R. M. (2000). Health literacy. National Library of Medicine current bibliographies in medicine. Bethesda, MD: National Institutes of Health, US Department of Health and Human Services. [Google Scholar]
- Reeve B. B. Fayers P. (2005). Applying item response theory modeling for evaluating questionnaire item and scale properties. In Fayers P. M., Hays R. D. (Eds.), Assessing quality of life in clinical trials: Methods of practice (pp. 55–73). New York, NY: Oxford University Press. [Google Scholar]
- Samejima F. (2016). Graded response models. In van der Linden W. J. (Eds.), Handbook of item response theory (pp. 95–107). Boca Raton, FL: CRC Press. [Google Scholar]
- Serper M. Patzer R. E. Curtis L. M. Smith S. G. O'Conor R. Baker D. W. Wolf M. S. (2014). Health literacy, cognitive ability, and functional health status among older adults. Health Services Research, 49(4), 1249–1267. 10.1111/1475-6773.12154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shealy R. Stout W. (1993). A model-based standardization approach that separates true bias/DIF from group ability differences and detects test bias/DTF as well as item bias/DIF. Psychometrika, 58(2), 159–194. 10.1007/BF02294572 [DOI] [Google Scholar]
- Smith S. G. Curtis L. M. Wardle J. Wagner C. von Wolf M. S. (2013). Skill set or mind set? Associations between health literacy, patient activation and health. PLoS One, 8(9), e74373. 10.1371/journal.pone.0074373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swaminathan H. Rogers H. J. (1990). Detecting differential item functioning using logistic regression procedures. Journal of Educational Measurement, 27(4), 361–370. 10.1111/j.1745-3984.1990.tb00754.x [DOI] [Google Scholar]
- Teresi J. A. Ocepek-Welikson K. Kleinman M. Eimicke J. P. Crane P. K. Jones R. N. Cella D. (2009). Analysis of differential item functioning in the depression item bank from the Patient Reported Outcome Measurement Information System (PROMIS): An item response theory approach. Psychology Science Quarterly, 51(2), 148–180. [PMC free article] [PubMed] [Google Scholar]
- Vandenbosch J. Van den Broucke S. Vancorenland S. Avalosse H. Verniest R. Callens M. (2016). Health literacy and the use of healthcare services in Belgium. Journal of Epidemiology and Community Health, 70(10), 1032–1038. 10.1136/jech-2015-206910 [DOI] [PubMed] [Google Scholar]
- Wolf M. S. Curtis L. M. Wilson E. A. H. Revelle W. Waite K. R. Smith S. G. Baker D. W. (2012). Literacy, cognitive function, and health: Results of the LitCog study. Journal of General Internal Medicine, 27(10), 1300–1307. 10.1007/s11606-012-2079-4 [DOI] [PMC free article] [PubMed] [Google Scholar]