Abstract
Running is one of the most popular sports worldwide. Studies suggest that 11%–85% of recreational runners have at least one running-related injury (RRI) each year, resulting in a reduction or interruption in training. A high risk for running-related injuries (RRIs) represents an important inconvenience counterbalancing the beneficial effects of running. RRIs primarily affect the joints of the lower limb and lumbar spine. Noteworthy, in some cases, the clinical presentation of signs and symptoms is confusing and may hide serious conditions; thus, clinicians have to pay special attention when potential factors arise, such as the presence of red flags. As reported in this case report, patients can present with low back pain (LBP) as a primary problem, mimicking a red flag such as a fracture of the spine. The aim of this case report was to describe a case of a recreational runner presenting with LBP as the sole symptom of an underlying thoracolumbar fracture.
Keywords: orthopaedic and trauma surgery, physiotherapy (sports medicine), physiotherapy (rehabilitation), back pain
Background
Running is one of the most popular sports worldwide due to the low demand for expensive technical materials and to its beneficial impact on health.1 2 The benefits of running include prevention of cardiovascular disease, obesity and other chronic health disorders, and reduction in the risk of mortality.1–4 Media coverage of health and fitness issues has increased in the last decade, leading to a growing interest in running both at the competitive and recreational levels.3–6 Although running is one of the most effective ways to achieve a general healthy status,7 recent studies highlight a relatively high risk of associated injuries.8 9 Previous studies have reported that 11%–85% of recreational runners have at least one running-related injury (RRI) each year,8 resulting in a reduction or interruption in training in a large percentage of runners.9 10 Acute running-related injuries (RRIs) are described as rare; approximately 80% of RRIs are due to overuse, resulting from an imbalance between the resistance capacity of the connective tissue and the biomechanical load of running.11 12 The prevalence of RRIs among middle-distance and long-distance runners has been reported to range between 19% and 92%.2 13–16 However, comparisons between studies are difficult due to the discrepancies in the type of runners studied, follow-up provided, study design, aetiology and definition of RRI.1 2 11–22 In 2015, an international consensus was reached, and RRI was defined as a musculoskeletal pain or physical complaint of the lower limbs or of the back/trunk due to running activities, causing a total restriction or suspension of running for at least seven or more days and requiring medical assistance.17
RRIs primarily affect the joints of the lower limb and lumbar spine, including the pelvis,15 22 23 resulting in painful muscles, tendons and joints.11–23 Patients normally contact physical therapists for a clinical evaluation aimed at resolving RRIs, with low back pain (LBP) being a common complaint.24–30 Noteworthy, in some cases, the clinical presentation of signs and symptoms is confusing and may mimic more serious conditions; thus, clinicians have to pay special attention when factors arise, such as the presence of red flags (RFs). For these reasons it is necessary to adopt a careful process of clinical reasoning and of decision-making to screen for potential RFs, and eventually direct these patients towards an appropriate diagnostic-therapeutic pathway.25 31 As reported in this case report, patients can present with LBP as a primary problem, mimicking an RF such as a fracture of the spine. Vertebral fractures24 27 are among the most common serious pathologies of the spine, but despite this more than two-thirds of vertebral fractures remain undiagnosed on initial examination.32 Stress fractures are common in running, accounting for 15% of the overall injuries,33–37 and one of the most common sites of stress fractures is the pelvis.33–37 LBP may be the sole complaint in the initial stage of a vertebral fracture. Thus, clinicians involved in caring for patients with sport injuries, and especially RRIs, have to pay special attention to such cases in order to screen for RF. Indeed, less than 5% of primary care physicians routinely examine for RF during an initial screen.38
The primary aim of this case report was to describe a case of a recreational runner presenting with LBP as the sole and most important symptom of an underlying post-traumatic thoracolumbar fracture. Moreover, this case report highlights the diagnostic value of further imaging besides the traditional scan (ie, radiography), thus offering the opportunity to reflect on the risk to miss serious complications. Relying on the original diagnosis of the patient could have been dangerous for the patient and for the physical therapist.
Case presentation
A 37-year-old man, working as a dentist, self-referred to an outpatient physical therapist with a chief complaint of a stabbing LBP. He described the pain as a continuous and deep pain in the central thoracolumbar junction area, rated as an 8 out of 10 on the Numeric Pain Rating Scale (NPRS).39 He also reported a concomitant, more superficial pain in his lower posterior back (3 out of 10 on the NPRS) that began after he fell backwards to the ground during a middle-distance uphill running training session (10 km), a day before the physical therapy consultation. He presented on initial examination with difficulty walking, and he was accompanied by his wife who supported him during ambulation. In the history, he described aggravating activities such as walking, sitting for a short time (10 min) and breathing. Moreover, he reported lying in bed as the most aggravating activity, which limited his sleep. In his medical history, he reported sporadic episodes of LBP that resolved spontaneously after a few days. However, this episode of LBP was much worse than previous episodes of pain. The patient complained of sporadic numbness and tingling in his bilateral feet throughout the day. He reported his pain as continuous during the day, gradually worsening throughout the night. The patient denied serious symptoms such as unexplained recent weight loss or gain, and any bowel or bladder symptoms.
Investigations
First examination
On observation, no deformity was noted during the visual analysis of posture, but the assessment of active movements revealed a decrease in active range of motion (aROM) of the thoracolumbar junction (T12–L2) during flexion and less decreased aROM in combined movement with extension on the right. The assessment of bilateral side bending and rotation was not possible secondary to pain. All active spinal movements were accompanied by an intense pain (9 out of 10 on the NPRS) while standing, which resulted in pain (8 out of 10 on the NPRS) in the central thoracolumbar junction of the spine and more superficial pain in the lower posterior back (3 out of 10 on the NPRS). The hypothesised diagnosis was fracture as a result of trauma that occurred a day before physical therapy consultation, as LBP presents as the sole symptom during the initial presentation.24–26 To confirm this diagnosis, different additional provocative tests were performed, such as tuning fork test,40 41 percussion test (bone vibration test)42 and percussion to the affected vertebrae.43 All of these tests were positive; thus, no other overpressure testing was performed to avoid exacerbation of pain. No loss of function was detected during the neurological examination; thus, on the basis of the anamnestic report (trauma, night pain, unable to lie supine sign,43 pain over 9 out of 10 on the NPRS) and the results of the clinical examination, a clinical diagnosis of specific LBP was made considering a possible vertebral fracture in the thoracolumbar junction. In accordance with the literature and clinical best practice,3 24–27 29 31 44 45 the patient was referred to the emergency unit for consultation. The patient was asked to inform the physical therapist about the outcome of the emergency unit visit or any change in their symptoms of LBP.
Differential diagnosis
Spinal fracture is reported in 1%–4% of all patients presenting with LBP to a primary care clinic.26 A potential cause of spinal fracture is malignancy, and the incidence of malignancy causing a spinal fracture is less than 1% of those patients presenting to a primary care clinic.46 There has been debate among scholars on the importance of RF for patients who present with LBP, discussing its value during the decision-making process. Koes et al 47 reported there were 26 RFs that suggest spinal fracture. Downie et al 48 suggested that for patients who present to primary care clinics, the following RFs should be used: older age, prolonged steroid use, severe trauma, and contusion or abrasion.48 Downie et al 48 reported that when one of these RFs is present, there is a 10%–33% increased probability of a spinal fracture.48 They also suggested that when the patient presents with several of these RFs, the probability of fracture increases from 42% to 90%.48 Downie et al 48 noted that the European guidelines for non-specific LBP endorse 10 RFs for fracture: patients aged <20 or >55, non-mechanical pain, thoracic pain, history of cancer, steroid use, structural changes, general unwellness, loss of weight and diffuse neurological deficit.48 Moreover, Downie et al’s48 results suggested that age >55, thoracic pain, non-mechanical pain, structural change and loss of weight were uninformative as RFs.
Differentiating the presentation using RF did not clarify the patient’s diagnosis in this case report. The patient is middle-aged, which does not fit Downie et al’s suggestions,48 and the patient (1) did not have a history of prolonged steroid use; (2) did present trauma as he did fall during an uphill training session; and (3) did not have a contusion or abrasion at the thoracolumbar junction where he was complaining of an 8 out of 10 pain on the NPRS. Therefore, the patient only presented with LBP as the sole symptom during the initial presentation.
Treatment
Diagnostic imaging and first intervention
In the emergency department (ED), a physician, after carefully considering the patient’s medical history and observation, performed plain film radiographs of the lumbar and thoracic spine, which showed a closed fracture of the first lumbar vertebrae without involvement of the spinal cord (figure 1). Then the patient was referred to an orthopaedic surgeon; the surgeon prescribed absolute rest and use of a corset (Camp C35) for 45 days. Non-steroidal anti-inflammatory drugs (ibuprofen) and pain killer (tramadol) were prescribed for 2 weeks to assist in controlling the amount of pain the patient was experiencing. However, approximately 12 hours after the ED consultation, the patient presented to our clinic reporting an aggravation of pain during rest and sitting on the bed while wearing the corset. Furthermore, he noted numbness and tingling in the feet bilaterally which were now much more aggravated than during the initial evaluation with the physical therapist. For this reason, the physical therapist went to the patient’s home to analyse the change in clinical presentation and to consider if the corset was appropriately donned and worn by the patient.
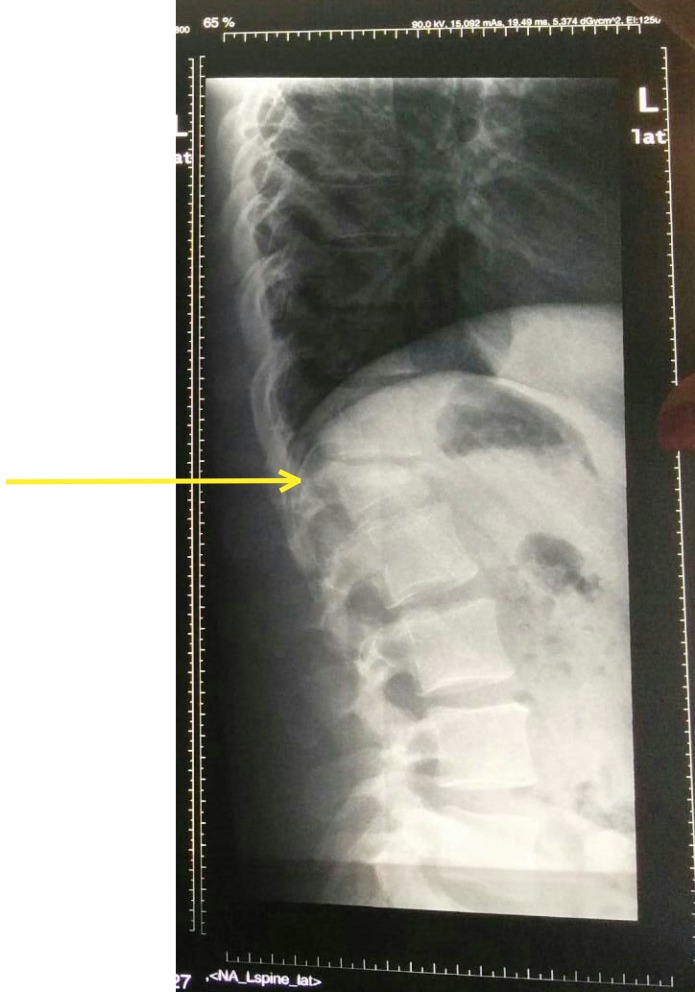
Figure 1.
Radiograph showing a closed compression fracture. Thick yellow arrow indicates a closed fracture of the first lumbar vertebrae without involvement of the spinal cord.
Diagnostic imaging and second intervention
During the home consultation, the patient informed the physical therapist that the pain has become more and more unbearable and the feeling of numbness in the lower limbs had become much worse. It was impossible to maintain a sitting position, even while wearing the corset. While the patient was lying on bed, the physical therapist performed a neurological examination, which displayed a reduction in osteotendinous reflexes (the patellar reflex was non-evocable bilaterally, and the Achilles’ tendon reflex was slightly evocable, especially on the left leg) and sensitivity; muscle strength was not evaluated to avoid intense efforts that may potentially aggravate the patient’s lumbar pain. Taking into account the radiographic results, the physical therapist hypothesised an aggravation of symptoms due to potential medullar compression, and for this reason the patient was advised to call an ambulance and return to the emergency unit. At the emergency hospital, the physician decided to perform a CT scan, which revealed a burst fracture of the first lumbar vertebrae with a spinal cord compression (figure 2). The patient was immediately taken for surgery, and an arthrodesis surgery with percutaneous stabilisation was performed with pedicle bars and screws at T12–L2 (figure 3).
Figure 2.
CT images showing a comminuted, burst fracture of the vertebral body of L1. Thick yellow arrow indicates, in axial plane (Left side), fracture of the vertebral body of L1 with displaced fragments of of the anterior vertebral wall and also shown are fractures of the right pedicle and left lamina next to the spinous process. Thick yellow arrow indicates, in sagittal plane (right side), fracture of the vertebral body of L1 with displaced fragments of the right and posterior walls, with loose fragments in the vertebral canal, impinging on the dural sac.
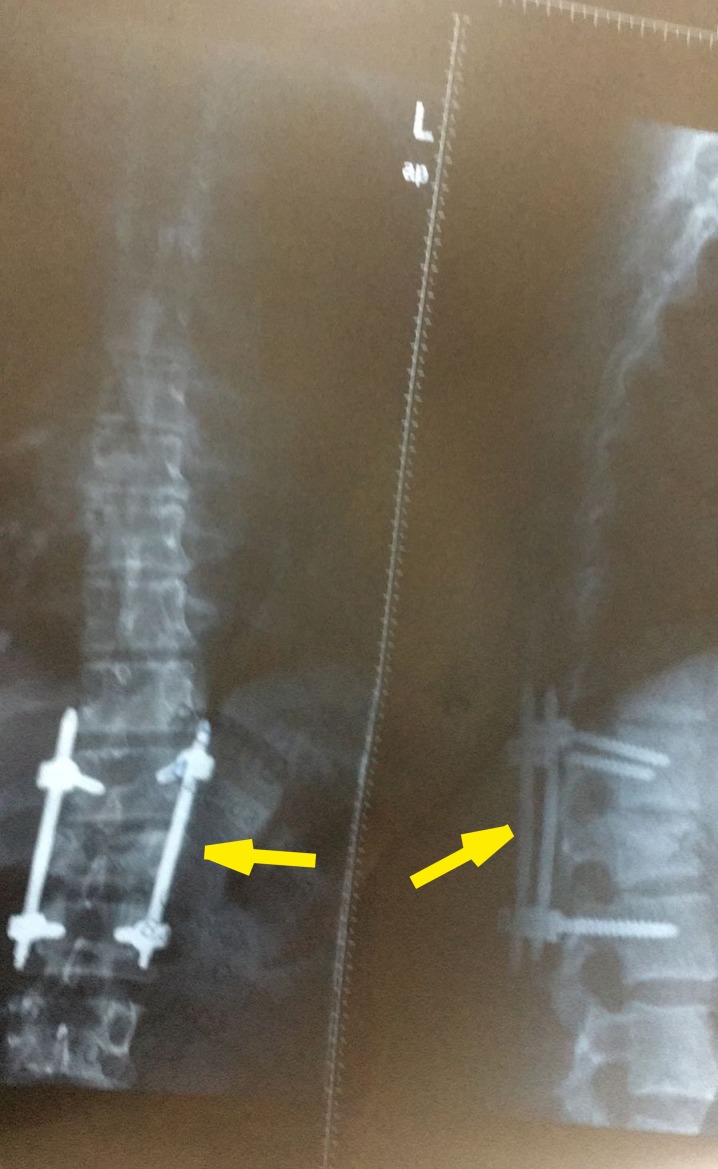
Figure 3.
Radiograph, showing open reduction and internal fixation of the L1 vertebral fracture; thick yellow arrow indicates stabilising pedicle bars and screws at T12–L2. Left side: posterior view; right side: sagittal view.
Outcome and follow-up
Two days after spinal surgery, the patient started to walk with a front-wheeled walker and began an active and active-assisted mobilisation of the lower limbs.49 Five days after spinal surgery, the patient was discharged with pharmacological therapies (heparin, ceftriaxone, ibuprofen and tramadol) and was referred for physical therapy in order to fully regain function so he could return to work activities and running. After spinal surgery, the patient’s symptoms decreased gradually (1 week), especially LBP and numbness in the lower limbs. From the second week after surgery, the patient started physical therapy, completing a total of 30 visits over the course of 48 weeks. A large number of visits over an extended period of time were agreed with the patient, who decided to pay individually for the treatment with the aim of returning to running. The details of physical therapy programmes are reported below. Patient follow-up was performed up to 1 year after surgery.
In the first phase (time: 2 weeks; total: 6 visits; scheduling: 3 visits each week), manual therapy (ie, passive joint mobilisation, stretching, myofascial release and mobilisation with movement) directed to the region of the thoracic and lumbar spine was performed to improve full aROM and to relieve pain. Relief of pain should be a priority to build the patient’s confidence and facilitate active engagement to optimise long-term outcomes.50–56
In the second phase (time: 3 weeks; total: 9 visits; scheduling: 3 visits each week), the patient was instructed to perform an exercise programme following the physical therapist’s instructions. Exercises were dosed and progressed according to pain levels and number of repetitions reached. Subsequently the treatment programme was progressively increased (3 times/week for 3 weeks) with functional exercises and load progressing from non-weightbearing to a weightbearing position following the patient’s tolerance.
In this phase, functional exercises for motor control have been included57–59: that is, bird dog (ie, four-point kneeling, pressing the hands and shins towards the floor with neutral lumbar spine); side bridge (ie, side-lying with bent knees, pressing and supporting the forearm on the floor; or side sitting with the upper knee upwards, pressing and supporting the hand down); single leg stretch; shoulder bridge; weight transfer, side lunge and one leg stand; and ‘cat – cow – downwards facing dog’.57 Weekly meetings were scheduled to ensure proper execution of exercises and gradual progression of loads (ie, side-lying hip abduction, supine two-leg bridge, plank and so on).54
Evidence59 60 suggests functional exercises ameliorate motor control strategies with short-term effects,58 redistributing the neuromuscular activities within and between muscles, decreasing aberrant movements, and improving the motor pattern variability of the thoracolumbar junction.60
However, recent motor control theories60–64 suggest the adoption of functional exercises for long-term effects aimed at60 (1) increasing the overall load capacity of the spine; (2) enhancing the ability to perform activities of daily living; and (3) improving patients’ self-efficacy.59 Therefore, functional exercises represent a new way for physical therapists to reduce the recurrence and to alleviate the persistence of pain after a spinal fracture.60
In the third phase (time: 12 weeks; scheduling: 5 sessions per week; details: alternating walking and running, with 2 rest days), a graded running retraining programme was initiated.54–56 Various strategies required considerations such as (1) increasing step rate, (2) reducing overstride, (3) altering the strike pattern, (4) reducing impact loading variables, (5) increasing step width and (6) altering proximal kinematics. The primary goal of these strategies was to optimise the dosage of loading stress to reduce the risk of RRIs even if it does not always lead to an improvement in the running biomechanics immediately on implementation (figure 4; video 1).21 54–56 65–68 The physical therapy programme was balanced with other interventions to include the management of psychosocial aspects of the pain experience, negative illness perceptions, education, maladaptive cognitions and coping strategy.50–53 60
Figure 4.
Photographs of the patient in a standing position and performing forward flexion movements.
Video 1.
The patient running on a treadmill (incline range of 1%–3%; speed range from 0.5 to 5.5 mph).
Discussion
In accordance with the clinical guideline,47 LBP is usually considered a musculoskeletal disorder with a positive prognosis commonly treated by a physical therapist using education, manual therapy and exercises. However, in a low percentage of cases, LBP could be secondary to a serious pathology, such as malignancy, infection, cauda equina syndrome or fracture.24–27 In the literature, the most common of serious spinal pathologies, which may initially manifest as LBP, is vertebral fracture.24–27
From a clinical perspective, the aim of this case report was to discuss the relevant aspects of the screening, the differential diagnosis and the therapeutic management concerning the severity of fracture of the thoracolumbar junction in a runner presenting with back pain in a direct-access physical therapy setting. The authors have observed, in this case report, that the most common of serious spinal pathologies among runners, which may initially manifest as LBP, is vertebral fracture.24–27
Among the athletes that the physical therapist regularly evaluates, runners, both recreational and competitive, enjoy running as it is one of the most popular sports activities practised all over the world.1 2 Physical therapists routinely assess patients and athletes whose primary complaint is back pain alone,24–30 but when the clinical presentation is not clear other clinical conditions must be considered, with attention to an accurate process of clinical reasoning and screening for referral.25 31
The ability to recognise a serious pathology is a key component of physical therapist practice.29 Differential diagnosis in physical therapy practice is the result of a complex process of clinical reasoning and decision-making encompassing the patient’s history, physical examination and the results of imaging when ordered.69 Clinical reasoning improves the rate of diagnosis of each system if a systematic approach is performed on each patient.69 The patient’s history is a milestone in the evaluation of physical therapy to obtain information on the clinical conditions of a patient with apparent musculoskeletal disorders,70 facilitating the therapist to improve or reduce the likelihood ratio of serious pathologies.71
In this case report, various elements of the patient’s history have been collected (ie, trauma, pain intensity, numbness of the lower limbs, supine positive sign) and included in the clinical reasoning process to guide the consequent physical examination.72 Physical therapists must ask themselves questions through self-reflection during assessment and treatment to identify the presence/absence of risk factors.73
In particular, in the presence of a change in a patient’s clinical situation (ie, aggravation of symptoms), the time until care rendered by the physical therapist can significantly change the patient’s medical prognosis. This occurred in this case and may have resulted in a life-changing clinical presentation such as cord compression due to fracture.74 75 It is important to remember that less than 5% of primary care physicians routinely examine for RFs during an initial screen.38
This case highlights the importance of a thorough physical assessment in the presence of an atypical clinical presentation. The patient’s history, clinical pattern of pain presentation and confirmation by imaging led the physical therapist to matching an effective intervention to the patient. This case report describes the history, assessment and treatment of a runner with a serious LBP caused by a vertebral fracture that was exacerbated by running.
After surgery, treatment focused on education and loading the tissues over many weeks through a graded programme of loaded functional exercises and running retraining. In running retraining there is a strong need to pay attention to the specific capacity of the structure during the progression of sessions; the cumulative load of the structure for the current session; the reduction of the specific capacity of the structure during a session in progress; and not exceeding the specific capacity of the structure and running at the regular pace.21 54–56 65–68 76 77 Indeed running speeds below 12 km/hour seem to be ideal and reduce the risk of injury to the joint.76 77
It is important to note that the patient was educated on his clinical condition, the neurophysiology of pain that influenced his behaviour and conception, and on lumbar anatomy, surgery and running retraining. This approach has enforced and improved his expectation for full recovery, which motivated him to strive towards a better outcome.50–53
Pain education and exercise positively influenced the patient in terms of pain modulation. This case report encourages physical therapists to use biopsychosocially oriented treatments to obtain good outcomes and facilitate return to running in a patient with a thoracolumbar fracture that was ultimately stabilised with surgery.50–53
In summary, this case report describes the clinical condition of a recreational runner presenting with post-traumatic thoracolumbar fracture, thus highlighting the importance of appropriate screening for physical therapists to facilitate the identification of potential pathologies that masquerade as a musculoskeletal condition by performing a thorough clinical examination.31
Patient’s perspective.
I greatly appreciated the help and work of my physical therapist. I realize that he has put a great deal of effort into therapeutic project for my healing and I want to praise his efforts. I did not believe that one day I would be back to running. Thanks so much to the surgeons and physical therapist that got me back to running again.
Learning points.
Consulting a physical therapist in this case was crucial for an appropriate evaluation and management of a patient with a serious pathology mimicking non-specific low back pain.
Differential diagnosis and screening for referral are critical steps for each healthcare provider.
Clinical reasoning and decision-making processes are important throughout all phases of a patient’s care pathway.
The diagnosis should not be limited to the results of a conventional radiograph; instead, the patient’s history and symptoms need to be considered, and the patient’s presentation needs to be continuously monitored for changes in the clinical presentation for appropriate management.
A tailored rehabilitation protocol, composed of loaded exercises and running retraining, assisted this patient to regain the optimal performance that he has set as his goal in therapy.
Acknowledgments
The authors would like to express their gratitude to Professor John Duane Heick, Pt BSc, DPT, PhD, Northern Arizona University Flagstaff, Arizona (USA), for his invaluable contribution in relation to the critical revision of the manuscript for important intellectual content.
Footnotes
Contributors: FM completed all examinations and decided on the final referral. FM, GR, AV and MT drafted the manuscript. FM performed the first clinical examination, and GR provided consultation on the interpretation of clinical examination findings, diagnosis and imaging method suggested. FM, GR and MT performed clinical revision of the paper’s content.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Correction notice: This article has been corrected since it was first published. The video has been replaced with the video in which the patient’s face is blurred.
Patient consent for publication: Obtained.
References
- 1. van Gent RN, Siem D, van Middelkoop M, et al. Incidence and determinants of lower extremity running injuries in long distance runners: a systematic review. Br J Sports Med 2007;41:469–80. 10.1136/bjsm.2006.033548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Van Middelkoop M, Kolkman J, Van Ochten J, et al. Prevalence and incidence of lower extremity injuries in male marathon runners. Scand J Med Sci Sports 2008;18:140–4. 10.1111/j.1600-0838.2007.00683.x [DOI] [PubMed] [Google Scholar]
- 3. Maselli F, Giovannico G, Cataldi F, et al. Case Report: Case Report: A different use of patellar pubic percussion test (PPPT) to identify an unrecognized hip stress fracture. Scienza Riabilitativa 2014;16:17–26. [Google Scholar]
- 4. Oja P, Titze S, Kokko S, et al. Health benefits of different sport disciplines for adults: systematic review of observational and intervention studies with meta-analysis. Br J Sports Med 2015;49:434–40. 10.1136/bjsports-2014-093885 [DOI] [PubMed] [Google Scholar]
- 5. Hulteen RM, Smith JJ, Morgan PJ, et al. Global participation in sport and leisure-time physical activities: a systematic review and meta-analysis. Prev Med 2017;95:14–25. 10.1016/j.ypmed.2016.11.027 [DOI] [PubMed] [Google Scholar]
- 6. van Dyck D, Cardon G, de Bourdeaudhuij I, et al. Who participates in running events? Socio-demographic characteristics, psychosocial factors and barriers as correlates of non-participation—a pilot study in Belgium. Int J Environ Res Public Health 2017;14:1315 10.3390/ijerph14111315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Fields KB, Sykes JC, Walker KM, et al. Prevention of running injuries. Curr Sports Med Rep 2010;9:176–82. 10.1249/JSR.0b013e3181de7ec5 [DOI] [PubMed] [Google Scholar]
- 8. Nielsen RO, Buist I, Sørensen H, et al. Training errors and running related injuries: a systematic review. Int J Sports Phys Ther 2012;7:58. [PMC free article] [PubMed] [Google Scholar]
- 9. van der Worp MP, ten Haaf DSM, van Cingel R, et al. Injuries in runners; a systematic review on risk factors and sex differences. PLoS One 2015;10:e0114937 10.1371/journal.pone.0114937 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kemler E, Blokland D, Backx F, et al. Differences in injury risk and characteristics of injuries between novice and experienced runners over a 4-year period. Phys Sportsmed 2018;46:485–91. 10.1080/00913847.2018.1507410 [DOI] [PubMed] [Google Scholar]
- 11. Walther M, Reuter I, Leonhard T, et al. Verletzungen und überlastungsreaktionen im laufsport. Der Orthopäde 2005;34:399–404. 10.1007/s00132-005-0790-0 [DOI] [PubMed] [Google Scholar]
- 12. Stanton TR, Latimer J, Maher CG, et al. A modified Delphi approach to standardize low back pain recurrence terminology. Eur Spine J 2011;20:744–52. 10.1007/s00586-010-1671-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. van der Worp MP, de Wijer A, van Cingel R, et al. The 5- or 10-km Marikenloop Run: A Prospective Study of the Etiology of Running-Related Injuries in Women. J Orthop Sports Phys Ther 2016;46:462–70. 10.2519/jospt.2016.6402 [DOI] [PubMed] [Google Scholar]
- 14. Hreljac A. Etiology, prevention, and early intervention of overuse injuries in runners: a biomechanical perspective. Phys Med Rehabil Clin N Am 2005;16:651–67. 10.1016/j.pmr.2005.02.002 [DOI] [PubMed] [Google Scholar]
- 15. Lopes AD, Hespanhol LC, Yeung SS, et al. What are the main running-related musculoskeletal injuries? A Systematic Review Sports Med 2012;42:891–905. 10.1007/BF03262301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Taunton JE, Ryan MB, Clement DB, et al. A retrospective case-control analysis of 2002 running injuries. Br J Sports Med 2002;36:95–101. 10.1136/bjsm.36.2.95 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Yamato TP, Saragiotto BT, Lopes AD. A consensus definition of running-related injury in recreational runners: a modified delphi approach. J Orthop Sports Phys Ther 2015;45:375–80. 10.2519/jospt.2015.5741 [DOI] [PubMed] [Google Scholar]
- 18. Hoeberigs JH. Factors related to the incidence of running injuries. A review. Sports Med 1992;13:408–22. 10.2165/00007256-199213060-00004 [DOI] [PubMed] [Google Scholar]
- 19. Satterthwaite P, Norton R, Larmer P, et al. Risk factors for injuries and other health problems sustained in a marathon. Br J Sports Med 1999;33:22–6. 10.1136/bjsm.33.1.22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Messier SP, Martin DF, Mihalko SL, et al. A 2-Year prospective cohort study of overuse running injuries: The Runners and Injury Longitudinal Study (TRAILS). Am J Sports Med 2018;46:2211–21. 10.1177/0363546518773755 [DOI] [PubMed] [Google Scholar]
- 21. Bertelsen ML, Hulme A, Petersen J, et al. A framework for the etiology of running-related injuries. Scand J Med Sci Sports 2017;27:1170–80. 10.1111/sms.12883 [DOI] [PubMed] [Google Scholar]
- 22. Hreljac A. Impact and overuse injuries in runners. Med Sci Sports Exerc 2004;36:845–9. 10.1249/01.MSS.0000126803.66636.DD [DOI] [PubMed] [Google Scholar]
- 23. Pinshaw R, Atlas V, Noakes TD. The nature and response to therapy of 196 consecutive injuries seen at a runners' clinic. S Afr Med J 1984;65:291–8. [PubMed] [Google Scholar]
- 24. Henschke N, Maher CG, Refshauge KM. Screening for malignancy in low back pain patients: a systematic review. Eur Spine J 2007;16:1673–9. 10.1007/s00586-007-0412-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Henschke N, Maher CG, Refshauge KM, et al. Prevalence of and screening for serious spinal pathology in patients presenting to primary care settings with acute low back pain. Arthritis Rheum 2009;60:3072–80. 10.1002/art.24853 [DOI] [PubMed] [Google Scholar]
- 26. Williams CM, Henschke N, Maher CG, et al. Red flags to screen for vertebral fracture in patients presenting with low-back pain. Cochrane Database Syst Rev 2013;1:CD008643 10.1002/14651858.CD008643.pub2 [DOI] [PubMed] [Google Scholar]
- 27. Premkumar A, Godfrey W, Gottschalk MB, et al. Red flags for low back pain are not always really red: a prospective evaluation of the clinical utility of commonly used screening questions for low back pain. J Bone Joint Surg Am 2018;100:368–74. 10.2106/JBJS.17.00134 [DOI] [PubMed] [Google Scholar]
- 28. Piano L, Maselli F, Viceconti A, et al. Direct access to physical therapy for the patient with musculoskeletal disorders, a literature review. J Phys Ther Sci 2017;29:1463–71. 10.1589/jpts.29.1463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Maselli F, Pennella D, Cataldi F, et al. Nonspecific low back pain (LBP) can occult a serious pathology: case report of Multiple Sclerosis (MS) in a young patient. Acta Medica International Jan 2016;3:202–6. [Google Scholar]
- 30. Farahbakhsh F, Rostami M, Noormohammadpour P, et al. Prevalence of low back pain among athletes: A systematic review. J Back Musculoskelet Rehabil 2018;31:901–16. 10.3233/BMR-170941 [DOI] [PubMed] [Google Scholar]
- 31. Mourad F, Giovannico G, Maselli F, et al. Basilar impression presenting as intermittent mechanical neck pain: a rare case report. BMC Musculoskelet Disord 2016;17:7 10.1186/s12891-015-0847-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Kendler DL, Bauer DC, Davison KS, et al. Vertebral fractures: clinical importance and management. Am J Med 2016;129:221.e1–10. 10.1016/j.amjmed.2015.09.020 [DOI] [PubMed] [Google Scholar]
- 33. Boden BP, Osbahr DC. High-risk stress fractures: evaluation and treatment. J Am Acad Orthop Surg 2000;8:344–53. 10.5435/00124635-200011000-00002 [DOI] [PubMed] [Google Scholar]
- 34. Brukner P, Bradshaw C, Khan KM, et al. Stress fractures: a review of 180 cases. Clin J Sport Med 1996;6:85–9. [PubMed] [Google Scholar]
- 35. Fredericson M, Bergman AG, Hoffman KL, et al. Tibial stress reaction in runners. Correlation of clinical symptoms and scintigraphy with a new magnetic resonance imaging grading system. Am J Sports Med 1995;23:472–81. 10.1177/036354659502300418 [DOI] [PubMed] [Google Scholar]
- 36. Hosey RG, Fernandez MMF, Johnson DL. Evaluation and management of stress fractures of the pelvis and sacrum. Orthopedics 2008;31:383–5. 10.3928/01477447-20080401-14 [DOI] [PubMed] [Google Scholar]
- 37. Henning PT. The running athlete: stress fractures, osteitis pubis, and snapping hips. Sports Health 2014;6:122–7. 10.1177/1941738114523381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Bishop PB, Wing PC. Knowledge transfer in family physicians managing patients with acute low back pain: a prospective randomized control trial. Spine J 2006;6:282–8. 10.1016/j.spinee.2005.10.008 [DOI] [PubMed] [Google Scholar]
- 39. Farrar JT, Young JP, LaMoreaux L, et al. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain 2001;94:149–58. 10.1016/S0304-3959(01)00349-9 [DOI] [PubMed] [Google Scholar]
- 40. Bache JB, Cross AB. The Barford test. A useful diagnostic sign in fractures of the femoral neck. Practitioner 1984;228:305–8. [PubMed] [Google Scholar]
- 41. Kazemi M. Tuning fork test utilization in detection of fractures: a review of the literature. J Can Chiropr Assoc 1999;43:120–4. [Google Scholar]
- 42. Hancock MJ, Maher CG, Latimer J, et al. Systematic review of tests to identify the disc, SIJ or facet joint as the source of low back pain. Eur Spine J 2007;16:1539–50. 10.1007/s00586-007-0391-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Langdon J, Way A, Heaton S, et al. Vertebral compression fractures – new clinical signs to aid diagnosis. Ann R Coll Surg Engl 2010;92:163–6. 10.1308/003588410X12518836440162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Mourad F, Maselli F, Cataldi F, et al. Hip bone marrow edema presenting as low back pain: a case report. Physiother Theory Pract 2018:1–9. 10.1080/09593985.2018.1481163 [DOI] [PubMed] [Google Scholar]
- 45. Sizer PS, Brismée J-M, Cook C. Medical screening for red flags in the diagnosis and management of musculoskeletal spine pain. Pain Pract 2007;7:53–71. 10.1111/j.1533-2500.2007.00112.x [DOI] [PubMed] [Google Scholar]
- 46. Henschke N, Maher CG, Ostelo RW, et al. Red flags to screen for malignancy in patients with low-back pain. Cochrane Database Syst Rev 2013;2:CD008686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Koes BW, van Tulder M, Lin CW, et al. An updated overview of clinical guidelines for the management of non-specific low back pain in primary care. Eur Spine J 2010;19:2075–94. 10.1007/s00586-010-1502-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Downie A, Williams CM, Henschke N, et al. Red flags to screen for malignancy and fracture in patients with low back pain: systematic review. BMJ 2013;347:f7095 10.1136/bmj.f7095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Wood KB, Li W, Lebl DS, et al. Management of thoracolumbar spine fractures. Spine J 2014;14:145–64. 10.1016/j.spinee.2012.10.041 [DOI] [PubMed] [Google Scholar]
- 50. Lederman E. A process approach in manual and physical therapies: beyond the structural model. CPDO Online Journal 2015:1–18. [Google Scholar]
- 51. Nijs J, Lluch Girbés E, Lundberg M, et al. Exercise therapy for chronic musculoskeletal pain: Innovation by altering pain memories. Man Ther 2015;20:216–20. 10.1016/j.math.2014.07.004 [DOI] [PubMed] [Google Scholar]
- 52. Nijs J, Roussel N, Paul van Wilgen C, et al. Thinking beyond muscles and joints: therapists' and patients' attitudes and beliefs regarding chronic musculoskeletal pain are key to applying effective treatment. Man Ther 2013;18:96–102. 10.1016/j.math.2012.11.001 [DOI] [PubMed] [Google Scholar]
- 53. Babatunde FO, MacDermid JC, MacIntyre N. A therapist-focused knowledge translation intervention for improving patient adherence in musculoskeletal physiotherapy practice. Arch Physiother 2017;7:1 10.1186/s40945-016-0029-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Passigli S, Capacci P, Volpi E. The effects of a multimodal rehabilitation program on pain, kinesiophobia and function in a runner with patellofemoral pain. Inter J Sports Phys Ther 2017;12:670–82. [PMC free article] [PubMed] [Google Scholar]
- 55. Barton CJ, Lack S, Hemmings S, et al. The ‘Best Practice Guide to Conservative Management of Patellofemoral Pain’: incorporating level 1 evidence with expert clinical reasoning. Br J Sports Med 2015;49:923–34. 10.1136/bjsports-2014-093637 [DOI] [PubMed] [Google Scholar]
- 56. Barton CJ, Bonanno DR, Carr J, et al. Running retraining to treat lower limb injuries: a mixed-methods study of current evidence synthesised with expert opinion. Br J Sports Med 2016;50:513–26. 10.1136/bjsports-2015-095278 [DOI] [PubMed] [Google Scholar]
- 57. Suni JH, Rinne M, Kankaanpää M, et al. Neuromuscular exercise and back counselling for female nursing personnel with recurrent non-specific low back pain: study protocol of a randomised controlled trial (NURSE-RCT). BMJ Open Sport Exerc Med 2016;2:e000098 10.1136/bmjsem-2015-000098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Suni JH, Kolu P, Tokola K, et al. Effectiveness and cost-effectiveness of neuromuscular exercise and back care counseling in female healthcare workers with recurrent non-specific low back pain: a blinded four-arm randomized controlled trial. BMC Public Health 2018;18:1376 10.1186/s12889-018-6293-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Bauer CM, Kankaanpää MJ, Meichtry A, et al. Efficacy of six months neuromuscular exercise on lumbar movement variability – A randomized controlled trial. J Electromyogr Kinesiol 2019;48:84–93. 10.1016/j.jelekin.2019.06.008 [DOI] [PubMed] [Google Scholar]
- 60. Hodges PW. Pain and motor control: From the laboratory to rehabilitation. J Electromyogr Kinesiol 2011;21:220–8. 10.1016/j.jelekin.2011.01.002 [DOI] [PubMed] [Google Scholar]
- 61. Falla D, Hodges PW. Individualized Exercise Interventions for Spinal Pain. Exerc Sport Sci Rev 2017;45:105–15. 10.1249/JES.0000000000000103 [DOI] [PubMed] [Google Scholar]
- 62. Hodges PW, Smeets RJ. Interaction between pain, movement, and physical activity: short-term benefits, long-term consequences, and targets for treatment. Clin J Pain 2015;31:97–107. 10.1097/AJP.0000000000000098 [DOI] [PubMed] [Google Scholar]
- 63. Hodges PW, Tucker K. Moving differently in pain: a new theory to explain the adaptation to pain. Pain 2011;152(3 Suppl):S90–8. 10.1016/j.pain.2010.10.020 [DOI] [PubMed] [Google Scholar]
- 64. Cote JN, Hoeger Bement MK. Update on the relation between pain and movement: consequences for clinical practice. Clin J Pain 2010;26:754–62. 10.1097/AJP.0b013e3181e0174f [DOI] [PubMed] [Google Scholar]
- 65. Cai C, Kong PW. Low back and lower-limb muscle performance in male and female recreational runners with chronic low back pain. J Orthop Sports Phys Ther 2015;45:436–43. 10.2519/jospt.2015.5460 [DOI] [PubMed] [Google Scholar]
- 66. Molloy JM. Factors influencing running-related musculoskeletal injury risk among U.S. military recruits. Mil Med 2016;181:512–23. 10.7205/MILMED-D-15-00143 [DOI] [PubMed] [Google Scholar]
- 67. Malisoux L, Nielsen RO, Urhausen A, et al. A step towards understanding the mechanisms of running-related injuries. J Sci Med Sport 2015;18:523–8. 10.1016/j.jsams.2014.07.014 [DOI] [PubMed] [Google Scholar]
- 68. Maselli F, Testa M. Superficial peroneal nerve schwannoma presenting as lumbar radicular syndrome in a non-competitive runner. J Back Musculoskelet Rehabil 2019;32:361–5. 10.3233/BMR-181164 [DOI] [PubMed] [Google Scholar]
- 69. Goodman CC, Heick J, Lazaro RT. Differential diagnosis for physical therapist, Screening for referral. 6th edn: Elsevier, 2018. [Google Scholar]
- 70. Jull G, Moore A, Falla D, et al. Grieve’s modern musculoskeletal physiotherapy. 4th edn: Elsevier, 2015. [Google Scholar]
- 71. Deyo RA, Rainville J, Kent DL. What can the history and physical examination tell us about low back pain? JAMA 1992;268:760–5. 10.1001/jama.1992.03490060092030 [DOI] [PubMed] [Google Scholar]
- 72. Ristori D, Miele S, Rossettini G, et al. Towards an integrated clinical framework for patient with shoulder pain. Arch Physiother 2018;8:7 10.1186/s40945-018-0050-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Ferguson FC, Morison S, Ryan CG. Physiotherapists' understanding of red flags for back pain. Musculoskeletal Care 2015;13:42–50. 10.1002/msc.1079 [DOI] [PubMed] [Google Scholar]
- 74. Obuchowski NA, Graham RJ, Baker ME, et al. Ten criteria for effective screening. Am J Roent 2001;176:1357–62. 10.2214/ajr.176.6.1761357 [DOI] [PubMed] [Google Scholar]
- 75. Levack P, Graham J, Collie D, et al. Don’t wait for a sensory level-listen to the symptoms: a prospective audit of the delays in diagnosis of malignant cord compression. Clin Oncol 2002;14:472–80. 10.1053/clon.2002.0098 [DOI] [PubMed] [Google Scholar]
- 76. Ramskov D, Rasmussen S, Sørensen H, et al. Progression in Running Intensity or Running Volume and the Development of Specific Injuries in Recreational Runners: Run Clever, a Randomized Trial Using Competing Risks. J Orthop Sports Phys Ther 2018;48:740–8. 10.2519/jospt.2018.8062 [DOI] [PubMed] [Google Scholar]
- 77. Thompson PD, Buchner D, Pina IL, et al. Exercise and physical activity in the prevention and treatment of atherosclerotic cardiovascular disease: a statement from the Council on Clinical Cardiology (Subcommittee on Exercise, Rehabilitation, and Prevention) and the Council on Nutrition, Physical Activity, and Metabolism (Subcommittee on Physical Activity). Circulation 2003;107:3109–16. 10.1161/01.CIR.0000075572.40158.77 [DOI] [PubMed] [Google Scholar]