Abstract
Objective
This paper aims to describe the medical service of two polyclinics of the PyeongChang Winter Olympic Games and to analyse the injury and illness of athletes who visited the polyclinics during the oilympic period in order to provide some insight with respect to the future construction and operation of polyclinics in mass gathering events such as the Olympic Games.
Methods
The PyeongChang Olympic Village was located near the Olympic Stadium for snow sports athletes and the Gangneung Olympic Village was located near the ice venues for ice sports athletes. During the Olympic Games, polyclinics were consisted of emergency service and outpatient clinics. We retrospectively analysed the electronic medical record data of athletes who visiting polyclinics between 9 February 2018 and 25 February 2018.
Results
During the Olympics, there were 1639 athlete encounters in both polyclinics. Among those, injuries of athletes were 237 (14% of all athlete encounters) in total, and the most common injured site was knee joint. Upper respiratory infection was the most frequent case in diseases of athlete encounters. Total 223 cases of image study were done, MRI was 44 cases.
Conclusion
The PyeongChang Winter Olympic Games had the highest number of participants in the history of Winter Olympic Games. Overall 48% of athletes encountered polyclinics due to disease during the Games period. Upper respiratory infection and other seasonal diseases were more frequent this Olympic Games than before. Polyclinics were managed healthcare of athletes as well as injury and illness of athletes. In winter sports, a polyclinic and similar medical facilities should be prepare for diseases considering geography, weather as well as injuries and endemic diseases when planning future mass gathering events.
Keywords: # polyclinic, # pyeongchang winter olympic games, # retrospective study
What are the new findings?
1639 (1020 in PyeongChang Polyclinic and 619 in Gangneung Polyclinic) athletes encountered polyclinics during the Olympic Games, 1402 encounters for illness and 237 encounters for injury.
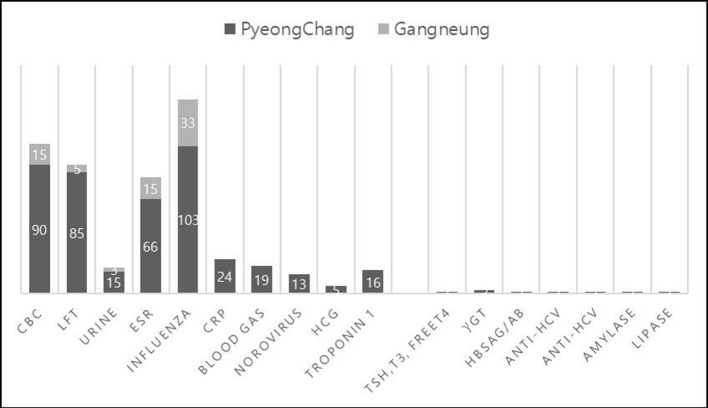
The polyclinic encounters increased on days 8–14 of the game period, when most of aerial manoeuvres and high-speed sport such as alpine ski, freestyle ski, snowboard, biathlon and ski jumping tournaments and final matches were held.
Encounters of orthopaedic surgery and emergency service were high in polyclinics at the early period of the games, and encounters of the internal medicine, rehabilitation medicine and physical therapy were high in the late period of games.
MRI was installed in the Gangneung Medical Center, where is outside the Olympic Village, considering the post-Game use. Medical Department of the PyeongChang Organizing Committee for the 2018 Olympic & Paralympic Games minimised the inconvenience of patients by using dedicated vehicles and the picture archiving and communication system connexion to both polyclinics.
How might it impact on clinical practice in the near future?
These data can help planning and construction of the polyclinic for competitive mass gathering event such as the Olympics Games, Asian Games, European Games and Pan American Games.
It is necessary to operate the polyclinic resiliently according to the game schedule, sport entries and the geographical factors such as the climate.
Operation of MRI equipment in the PyeongChang Winter Olympic Games suggests that the equipment of the polyclinic should be considered for the games and after the games.
Introduction
There were 2920 athletes from 92 countries’ National Olympic Committee (NOC) participating in the PyeongChang 2018 Winter Olympic Games. This was the first winter mega sports event held in Korea,1 and the third Olympic Winter Games held in Asia after the Sapporo 1972 Games (1006 athletes from 35 countries) and the Nagano 1998 Games (2176 participants from 72 countries). The PyeongChang 2018 Games was the largest Winter Olympic Games in the number of participating countries and athletes.2
In competitive mass gathering events such as the Olympic and Paralympic Games, athletes have a relatively high risk of injury during the games.3 Recent studies have also reported that the risk of disease-related illnesses is as high as the risk of injury.4–7 The PyeongChang Organizing Committee for the 2018 Olympic & Paralympic Games (POCOG) appointed the Medical Department of the POCOG to support the Olympic Games, based on the International Olympic Committees (IOC’s) agenda of keeping the athletes’ health at their best during the olympics.8–10
The goal of the POCOG medical service was to provide medical service of the highest quality to all participants to ensure that the games would be a healthy and joyful festival. Another goal of the POCOG medical was to contribute to the health and development of the host region following the competition. In addition, considering the distance from two Olympic Hospitals (about 30–100 km away from each venue) and risk of overloading local medical centres, two polyclinics were established in two Olympic villages in PyeongChang (mountain cluster) and Gangneung (coastal cluster) to provide continuous healthcare and satisfactory medical services for elite athletes.11–13
This paper aims to describe the medical service of the two Polyclinics of the PyeongChang 2018 Winter Olympic Games and to analyse the injury and illness of athletes who visited polyclinics during the olympic period in order to provide insight with respect to the future construction and operation of the polyclinic in mass gathering events such as the Olympic Games.
Methods
The PyeongChang Winter Olympic Games consisted of 13 competition venues and 10 non-competition venues. PyeongChang Olympic Village, located near the olympic stadium, was used by snow sports athletes (mountain cluster), while Gangneung Olympic Village, located near the ice venues, was used by ice sports athletes (coastal cluster). As a result, the PyeongChang Polyclinic (PC) and the Gangneung Polyclinic (GC) were constructed in each Olympic village. The PC consisted of one ground floor and one basement floor. On the first floor of the PC, there were clinics for orthopaedics, rehabilitation medicine, internal medicine, family medicine, otorhinolaryngology, psychiatry, obstetrics outpatient clinics, emergency room, radiology, laboratory and pharmacy. On the basement floor of the PC, there were clinics for physical therapy, dentistry, ophthalmology, acupuncture, orthosis, medical record, POCOG medical office, IOC medical office and IOC medical research office. The physical therapy room was moved to the ground floor from the basement a few days after the opening of the olympic games because the heating capacity of the basement floor proved inadequate against extremely cold weather. GC consisted of one ground floor that included clinics for orthopaedics, rehabilitation medicine, internal medicine, otorhinolaryngology, psychiatry, obstetrics, urology, family medicine, physical therapy, dentistry, ophthalmology, acupuncture, orthosis, as well as an emergency room, a medical records room, a laboratory and a pharmacy. Medical staffs at each clinic, including doctors, dentists, nurses, physiotherapists, radiological technologists, medical laboratory technologists, opticians, health information managers and translators, were most of volunteers who were interested in sports medicine in Korea and some staff were recruited from two university hospitals that were later selected as olympic hospitals. Emergency medicine specialists and traumatology specialists worked together in the emergency room so that it was possible to cope with emergencies as well as injuries caused during training and games period. In addition, at least one ambulance and one paramedic were on standby in the emergency room of each clinic. Polyclinics were able to share 24 hours contact with two olympic hospitals and immediately transfer patients who needed treatment in hospital such as surgery.
Polyclinics were operated from 26 January to 28 February 2018. Services were limited during the Olympic Village preopening period, 26–31 January and after the closing ceremony, 27–28 February 2018. During this period, only emergency medical service was provided for 24 hours. From 1 to 26 February 2018, polyclinics were operated on a full scale, providing emergency medical care and offering other essential clinical services. The details of service and schedule was in table 1.
Table 1.
Service scope of polyclinics
| Emergency service (24 hours operation) | Outpatient clinic 1 (16 hours operation) | Outpatient clinic II (on-call/scheduled) |
| Emergency services | Medicine/family medicine | Gastro intestinal |
| Trauma/orthopaedics | General surgery orthopaedics |
Pulmonary |
| First-aid services | Rehabilitation/physical therapy | Cardiology |
| Radiology | Ophthalmology | Endocrinology |
| Laboratory | Dental | Gynaecology |
| Eye, ear/nose/throat | Neurology | |
| Pharmacy | ||
| Acupuncture |
Both polyclinics had digital plain X-ray (Optima XR220amx; GE Healthcare, Chicago, Illinois, USA) and ultrasonogram (Logiq E Premium R7; GE Healthcare). MRI (Multiva 1.5T, PHILPS) was installed at the Gangneung Medical Center (located 35 km (25 min) from the PC and about 3 km (5 min) from the GC) for the exclusive use of athletes and other accredited individuals who require further imaging study. Diagnostic CT scans were performed at the designated olympic hospitals in Gangneung and Wonju, because patients who needed diagnostic CT scans were immediately transferred to the olympic hospitals. MRI images were sent to the picture archiving and communication system at polyclinics or stored in a portable disc. Radiologists were present at both polyclinics to provide imaging consultations or readings.
Pharmacy service was provided in both polyclinics from 07:00 to 23:00 hours for regular pharmacy operations during the games period. After this time, prescriptions for patient who visited emergency rooms of polyclinics were available. There were four pharmacists working in each polyclinic, two for daytime and two for evening. NOC physicians who have preregistered were able to request medication using a specific prescription request form. The request form was reviewed by Korean physicians in polyclinics and medication was ready for pick-up at the Polyclinic pharmacy.
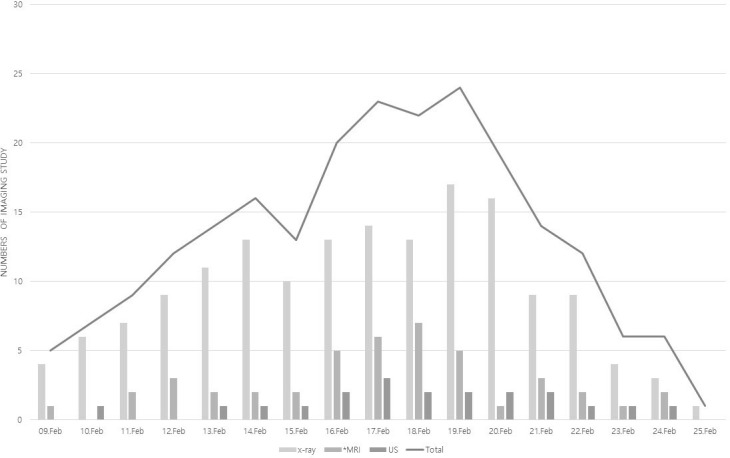
On the first floor of each polyclinic, there was a diagnostic laboratory room with technologists. Laboratory test panels available at polyclinics included the following: complete blood count (CBC), comprehensive metabolic profile (electrolytes, hepatic and renal panels) and arterial blood gas analysis, erythrocyte sedimentation rate (ESR), C reactive protein, human chorionic gonadotropin, rapid diagnostic tests for influenza and norovirus. Other essential tests were outsourced, and the results were available within 2 days.
Physical therapy was provided daily from 8:00 to 22:00 hours at polyclinics. Eight physiotherapist per roster provided electrotherapy, manual therapy, massage, exercise therapy and localised cryotherapy. Physiotherapy after injury was provided by referral from in-house physiatrist, and those for recovery, prevention, maintenance or advice contacted physiotherapy team directly.
Entrance of polyclinics was separated into two parts: an emergency room and outpatient clinics. At entrance of each part, there was a triage operated by a nurse or a paramedic. A 24 hours emergency contact system between polyclinics and venue medical managers, olympic hospitals and the POCOG medical department were operated during the games. Emergency medicine specialists and traumatologists resided in the emergency room together, and it took approximately 43 min for the decision-making and the average transfer to the hospital after the visit. Two radiologists reside from 7:00 to 21:00 hours and read the finding immediately after image study.
During the olympic games, PC and GC used Athlete Management Solution (AMS) electronic medical record (EMR) systems (GE Healthcare). The EMR form was composed of demographic information such as nationality, age, and sex, as well as participating sports, medical history and physical examination, severity of injury. All data were encrypted and protected. It was discarded 5 days after the olympics to ensure that confidentiality was maintained. Each polyclinic had a dedicated team of health information managers who were able to receive feedback on the missing records every evening. We retrospectively analysed EMR records of athletes from PC and GC during the olympic games period, from 9 to 25 February 2018.
Confidentiality
We used the athlete accreditation number to query the IOC athlete database for their age, gender and nationality and sport. We treated all information with strict confidence and anonymised our medical database at the end of the games.
Data analysis
Data analysis and correction for duplicate data were performed using Excel, V.2016 (Microsoft, Redmond, Washington, USA). Countries have been grouped into their respective continent based on the United Nations Statistics Division classification.14 Frequency of the cases was reported along with clinical incidence (CI= # of cases/# of total athletes encountered polyclinics) and the percentage of each injury was calculated as the same method as CI.
Results
In general, there were a total of 5405 (2885 in PC and 2520 in GC) clinical consultations in both polyclinics during the olympic games, of which 1639 (1020 in PC: 62.2% and 619 in GC: 37.8%) encounters were athletes. These encounters included cases related to primary care, illnesses, injuries, physical therapy, ophthalmology and dentistry. Total number of encounters and injury encounters of athletes by date is shown in figure 1. The usage of polyclinics varied over the period of the games, and more than 100 athletes were registered for treatment in polyclinics between days 8–14 of the competition period with a peak on day 11. More than 20 athletes were encountered in polyclinics on day 9 and 10 of competitions due to injuries.
Figure 1.
Total numbers of clinical consultation of athletes in both polyclinics.
Illness
Of the 2920 athletes who participated in the PyeongChang Winter Olympic Games, 1402 athletes encountered polyclinic because of illness. This is 47.9% CI. Upper respiratory infection (URI), including sinusitis, rhinitis and acute pharyngitis, tonsillitis, was the most frequent item in respiratory system (table 2). In the illness encounters, 107 cases of otorhinolaryngology, including three cases of influenza, were followed by ophthalmology, gastrointestinal diseases, dermatology, urology, neurology and cardiovascular diseases. Gastrointestinal disease, including norovirus (four cases) in athletes, was 20 cases.
Table 2.
Summary of all athlete encounters by system
| Category (total) | Details | Percentage |
| Musculoskeletal (237) | See table 3 | 14 |
| Dental (408) | Dental calculus (81) sensitivity, request cleaning (140) Broken tooth/filling (20) Temporomandibular joint pain (1) Mouth guard (167) |
24.9 |
| Ophthalmic (50) | Ophthalmic examination (13) Blurred vision (1) Eye infection (1) Itching, Allergic conjunctivitis (13) Dry eye (10) Glasses making (13) |
3.1 |
| Ear, nose and throat (107) | Otitis media/externa (8) Sinusitis/rhinitis (12) Acute pharyngitis/tonsillitis (84) (influenza +: 3) Sensorineural hearing loss (1) Epistaxis (2) Acute laryngitis asthma (1) Nasal bone fracture (2) |
6.5 |
| Dermatological (11) | Skin rash (6) Dry skin (1) Cellulitis (1) Burn (1) Scar care (1) Herpes zoster (1) |
0.7 |
| Psychiatry (2) | Insomnia (2) | 0.1 |
| Gastrointestinal (20) | Nausea/vomiting (3) Abdominal pain/diarrhoea (16) (Norovirus: 4) Appendicitis (1) |
1.2 |
| Genitourinary (8) | Polycystic ovaries (1) dysuria (UTI) (5) STD (1) contraceptive pill (1) |
0.5 |
| Neurological (7) | Headache (4) Venous malformation (1) Scalp laceration (1) Dizziness (1) |
0.4 |
| Cardiovascular (6) | Chest pain (2) Hypokalaemia (1) Rib fracture (1) Left ventricular hypertrophy (1) Hypertension (1) |
0.4 |
| General (15) | Myalgia (11) For routine check (4) |
0.9 |
| Physical therapy (255)* | 15.6 | |
| Orthosis (513) | 31.3 |
*Physical therapy was started 3 days after the opening ceremony due to transfer of therapy room.
STD, sexually transmitted disease; UTI, urinary tract infection.
Injury
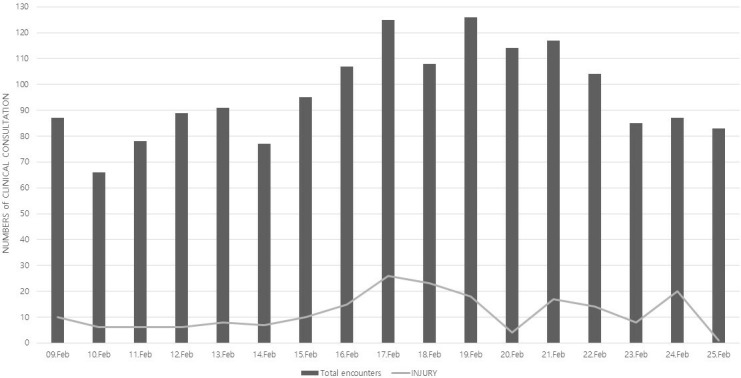
Of the athletes who visited polyclinics, 237 had injuries. This is 14.5% CI. Table 3 shows details. Of these, four cases of polytrauma were occurred. One of them is 22 years old male alpine ski player with lumbar spine injury and left hip muscle injury. Another one is 25 years old female luge player with cervical spine sprain, thoracic spine fracture and carpal bone fracture. Both cases had occurred during games and transferred from the polyclinics to the olympic hospital. Of the injury types, contact was the most common (62%) followed by non-contact trauma (22%) and overuse (16%). The most injured sport was alpine skiing, and the second was snowboarding. There were eight cases of fracture; one case of thoracic spine; one case of clavicle; three cases of radius and three cases of carpal bone. Of 29 cases of ligament injuries in total, there were 14 knees, 6 shoulders, 4 elbows, 4 ankles and 1 hand. Patients with severe injuries, such as polytrauma or thoracic spine fracture, were immediately transferred to the olympic hospital using the ambulance that was always on standby at polyclinics. MRI was used for diagnosis of minor fractures or ligament injuries that were uncertainly diagnosed by digital plain films or ultrasonograms. The most common site of injury was the knee (32%) followed by the spine, foot, hand and shoulder (figure 2). The knee was injured frequently in athletes from sports coming from snow sports, such as alpine skiing, snowboarding and freestyle skiing.
Table 3.
Summary of musculoskeletal encounters seen in polyclinics during the games period
| Description | Totals | Percentage of total injuries | Percentage of total encounters |
| Contusion | 64 | 27.0 | 3.9 |
| Sprain/strain | 108 | 45.6 | 6.6 |
| Ligament injury | 29 | 12.2 | 1.8 |
| Swelling | 7 | 3.0 | 0.4 |
| Fasciitis | 1 | 0.4 | 0.1 |
| Muscle injury | 7 | 3.0 | 0.4 |
| Tendinitis | 11 | 4.6 | 0.7 |
| Fracture | 8 | 3.4 | 0.5 |
| Laceration | 2 | 0.8 | 0.1 |
Figure 2.
Injury area of musculoskeletal encounters seen in the polyclinic during the games period.
Imaging study
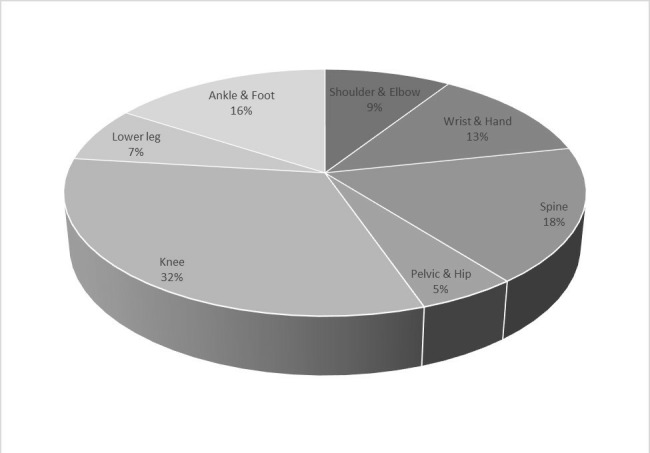
In polyclinics, 159 digital plain films, 20 ultrasonograms and 44 MRIs were performed to the athletes (table 4). Plain films peaked on day 11 of the competition. MRI peaked on day 10, and it showed a similar pattern to the daily injury encounters of the athlete (figure 3). Because diagnostic CT scans were taken at olympic hospitals as described above, we will not describe it in this paper.
Table 4.
Statistics of medical image service of athlete in polyclinics
| PC | GC | TOTAL | |
| X-ray | 81 | 78 | 159 |
| Ultrasonogram | 9 | 11 | 20 |
| MRI* | 44 | 44 | |
| TOTAL | 223 | ||
*MRIs were taken at Gangneung Medical Center, Olympic designated MRI laboratory.
GC, Gangneung Polyclinic; PC, PyeongChang Polyclinic.
Figure 3.
Daily number of imaging studies of athlete performed in polyclinics. (*MRIs were taken at Gangneung medical Center, Olympic designated MRI laboratory.). US, ultrasound.
Pharmacy
A total of 1965 (1094 in PC and 871 in GC) prescriptions were registered by both polyclinics during the games period, of which 300 (203 in PC and 97 in GC) prescriptions were for athlete encounters (figure 4). Of the prescriptions, analgesics and anti-inflammatory agents were the most common (25% of total prescriptions, such as tylenol and non-steroidal anti-inflammatory drugs), followed by gastrointestinal drugs and respiratory agents. None of the World Anti-Doping Agency-prohibited drugs were prescribed and there were 95 prescriptions for influenza.
Figure 4.
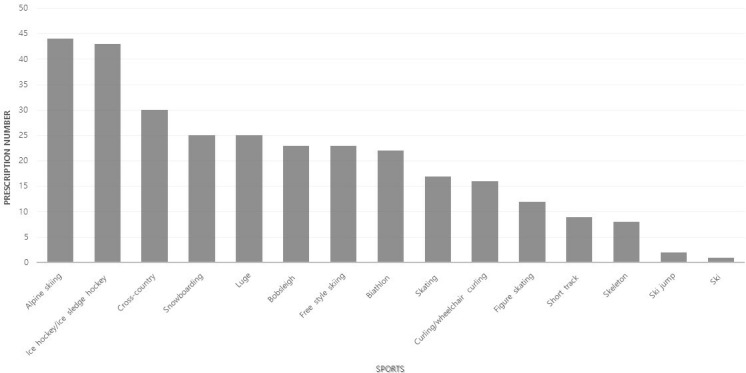
Number of pharmacy prescription of athletes by sports.
Laboratory tests
A total of 515 samples were analysed and 136 influenza tests were the most common, followed by CBC, liver function test and ESR (figure 5).
Figure 5.
Number of laboratory tests in polyclinics. CBC, complete blood count; CRP, C reactive protein; ESR, erythrocyte sedimentation rate; γGT, Gamma-glutamyltransferase; HCG, human chorionic gonadotropin; HCV, Hepatitis C virus.
Distribution of athlete encounters by continent
Over the 17 days period under scrutiny, there were a total of 1639 athlete encounters within polyclinics (table 5). This table combines usage of all services within the facility such as medical consultations, radiology/pathology investigations and prescriptions dispensed. Each encounter has been further analysed to establish the continent of origin of the athlete. The greatest proportion of total encounters was athletes from Europe nations (51%) followed by athletes from Asian nations (23%). Once corrected for multiple follow-up counters of the same case, Africa had the highest proportion of athletes seen at polyclinics (45%) and Oceania the least (17.8%).
Table 5.
Summary of elite athletes encounters by continent
| Continent no of individual athletes | Total competing athletes | Polyclinic encounters | Percentage of total encounters (%) | Correction for duplicates | ||
| Proportion of total encounters | Proportion of athletes seeking attention (%) | Proportion of athletes encounters in each continent (%) | ||||
| Africa | 11 | 9 | 0.5 | 5 | 0.7 | 45.4 |
| Asia | 437 | 382 | 23.3 | 182 | 26.7 | 41.6 |
| Europe | 1701 | 833 | 50.8 | 333 | 48.8 | 19.5 |
| America | 507 | 293 | 17.9 | 93 | 13.6 | 18.3 |
| Oceania | 73 | 43 | 2.6 | 13 | 1.9 | 17.8 |
| Independent olympic athlete | 196 | 79 | 4.8 | 55 | 8.0 | 28 |
| Total | 2925 | 1639 | 100 | 681 | 100.0 | |
Discussion
The aims of this paper are to appreciate the medical service of polyclinics, to analyse the composition of athlete encounters in polyclinics during the PyeongChang 2018 Winter Olympic Games and provide insight with respect to the future construction and operation of polyclinics in mass gathering events. PyeongChang is located 700 m above sea level and is a snowy mountain area. There are many Korean ski resorts before the PyeongChang 2018 Olympic Games. Also, the coldest January average temperature is −7.7°C, and the lowest temperature observed is −30°C. During the olympics, snow fell twice, with a minimum temperature of minus 11°C, a maximum temperature of minus 0.5°C and an average temperature of −5.6°C.
In 17 days of game period, 8% of all athletes encountered polyclinics at least once with injury and 16% with illness. Encounters of orthopaedics and emergency service were high in the early period of the game period, but encounters of internal medicine and rehabilitation medicine were high in the late period of game. It was increased on days 8–14 of the competition, when the most tournaments and final matches were held,15 up to 120 cases a day. During game period, the number of encounters who visited polyclinics also increased for mouth guards, orthoses, glasses and scaling. It is due to the increased usage of these parts of elite athletes who was finished his own game. The busiest period of polyclinics was on days 9, 10 and 11 of the competitions. This time was many snow sports events that involved aerial manoeuvres and high speed such as alpine skiing, freestyle Skiing, snowboarding, biathlon and ski jumping were held. A similar trend could be observed in the previous Winter Olympic Games.2
Orthosis was the most common reason of encounters, followed by dentistry. Most of the orthosis were prescripted for leg orthosis, most cases required orthosis for chronic injuries before this Olympic Games. Since orthosis was provided free of charge at polyclinics, some athletes wanted to prescribe a new orthosis instead of an old one. The most common cause of the dentistry encounters was for mouthguard and teeth cleaning, which seems to be due to the visitation of athletes who were not easy to use the dentistry in their homeland.
The rate of illness in the PyeongChang Winter Olympic Games was higher than those reported in the Vancouver Games and Sochi Games (16% of all athletes affected in PyeongChang vs 7% in Vancouver and 8% in Sochi).2 The most common illness among athletes was acute pharyngitis and tonsillitis. The high incidence of URIs is similar to other elite sport events.2 4–7 It was suggested that cold and dry regional characteristics of the PyeongChang contributed to the development of these diseases. Of particular note was the occurrence of norovirus. A total of 172 cases of norovirus occurrence were observed in volunteers who stayed at hostels, but in the Olympic Villages only four cases with diarrhoea were confirmed. It is believed that establishing entrance to the athlete’s village, providing hand disinfectants for each room, spreading rapid news such as official letter from Korea Centers for Disease Control and Prevention, and promoting public information have played important roles in isolating patients from others.16 In the future, mass gathering event, vaccination of all participants including volunteers against local epidemic such as influenza will be helpful to reduce the incidence and spread of these diseases.14 17
The overall rate of injury in the PyeongChang Winter Olympic Games (8% of all athletes) was lower than those in Vancouver 2010 (11% of all athletes) and in Sochi 2014 (12% of all athletes).2 Injury encounters of PC were more than two times higher than GC, likely because athletes participating in snow events such as alpine skiing, freestyle skiing and snowboarding that have the higher risk of injury resided in the PyeongChang Athlete Village. Most of the injured athletes visiting polyclinics required treatment for musculoskeletal injuries. Patients with major traumas such as head injuries that occurred in games were immediately transferred by Venue medical officers to olympic hospitals where there was an intensive care unit or other facilities that could perform major trauma surgeries. The most common site of injuries was knee, and minor trauma such as contusion and sprain were the most common type of injury (72.6%). This was similar to other major winter sport events.2 18
The most frequently used imaging modality was digital plain film. MRI is essential for the diagnosis of musculoskeletal injuries.19–21 But the number of MRI examinations in the PyeongChang Winter Games (20% of all radiological examinations) was very lower than Rio de Janeiro 2016 (68% of all radiological examinations).19 Location of MRI equipment may have influenced these results. POCOG installed and operated an olympic-exclusive MRI service in Gangneung Medical Center, which is located 10 min and 30 min away from the Gangneung Athletes Village and the PyeongChang Athletes Village respectively. The initial plan was to instal the MRI equipment inside PC; however, after taking into consideration the distance from the GC as well as the cost of relocating the equipment following the games, it was decided that the equipment would be installed at the midway point of the two villages. Considering the important role that the MRI examination plays in diagnoses of injuries in the musculoskeletal system, as well as the high demand for it, it is ideal for MRI equipment to be installed in the polyclinics of each athletes village. Furthermore, as it is usual for summer olympics to only operate a single polyclinic even though the number of participating athletes is much larger than that of the Winter Games, it is foreseeable that two or more MRI in Polyclinic would be required for the Olympic Summer Games. However, as such equipments are expensive investments, their postgame usage must be taken into serious consideration.
In the PyeongChang Winter Olympic games, athletes from European continent showed greatest proportion of attendances. European athletes were the most encountered by the gross number of overall attendances and also when corrected for multiple attendances by individual athletes. This might mean that the athletes from the European continent sought to continue the treatment of the chronic injury or illness that they had before participating in the PyeongChang Winter Olympic games, even during the games period. Attention should be paid to interpreting the results of encounter athletes from the Asian continent who showed second most attendance frequencies. The number of visitors from Korea has accounted for 80% of encounters from Asia. Korean athletes are familiar with the medical staffs of polyclinics because some athletes and staffs know each other before the olympic games and do not have the problem of the linguistic communication. As a result, they could access medical service relatively easily and the number of encounter was therefore high. Forty-five per cent of African athletes visited polyclinics, but as the number of participating athletes from Africa was small, many of them required the attention of interpreters. At the London Olympic Games, athletes from African continent had the highest frequency of visiting polyclinics.
When a mass gathering event such as the Olympic Games occurs, it is necessary to provide a larger scale medical service than the medical service usually needed in the region.22 23 In addition, the athletes need more delicate medical service and healthcare in order to maintain the best performance. In the PyeongChang Winter Olympic games, injury encounters increased during the period when the final competitions of snow sports were held. So it is necessary to prepare for operation of the winter mass gathering event Polyclinic by analysing the injury pattern of the winter sports athletes and the distribution by daily encounters of the polyclinic in other winter games. Of course, it should also be prepared for non-athlete patients, which will account for more of polyclinic encounters.
During the PyeongChang Winter Olympic Games, two Olympic Village Polyclinics (PC and GC) were commissioned and operated by two university hospitals in consideration of the efficiency of operation, the stability of securing professional medical personnel, and the expertise of supply and management of drugs and medical supplies. As a result, POCOG was able to provide stable and high-quality care services while overcoming the following unexpected difficulties.
Most of the medical personnel at each of the polyclinics were composed of medical staff of the hospital in charge of respective polyclinics (PC at Wonju Severance Christian Hospital, GC at Seoul National University Hospital). These hospitals had regional emergency medical centre and level I trauma centre from the initiative. This has been a great help for the close cooperation between the staff and the smooth operation of the clinic during the operation of the clinic. At each clinic, the nurses, who were in charge of triage in each hospital, were responsible for outpatient clinics. Emergency medicine specialists and traumatology specialists in the emergency service of polyclinics also staffed who worked or working in olympic hospitals and were able to consult on-call easily with olympic hospitals when necessary.
Limitations
Until day 3 of competitions, there was some technical difficulties in using AMS EMR system, so in some cases it was necessary to transporting the EMR from paper chart after outpatient clinics closed. Every evening, the medical records of the day were checked by certified medical record specialist, and the missing parts were feedback to the clinic staffed. Physical therapy was provided in earnest 3 days after the opening ceremony due to transfer of therapy room. Therefore, it had made implicate on the numbers of encounters of physical therapy and would have affected the number of total encounters in the first 3 days of the game period.
Conclusions
The PyeongChang Winter Olympic Games was the largest winter sporting event not only in Korea but in Asia as well, with the highest number of participants in the history of Winter Olympic Games. During the games period, two athletes villages were established after taking into account the nature of the Winter Olympics—one in the coastal region and the other in the mountain region. The polyclinics’ comprehensive medical service played a vital role during the games, particularly because the hosting region of the PyeongChang did not possess adequate local medical resources. The hosting city of future Winter Olympic Games must make an effort to consider variables such as geography, weather and sporting events when preparing for the games in order to promote the health of athletes, prevent injuries, and ensure their peak performance.
Patient and public involvement
There were no funds or time allocated for PPI so we were unable to involve patients. We have invited patients to help us develop our dissemination strategy.
Footnotes
Contributors: D-SK organied and wrote the paper. Y-HL was responsible for the communication between the authors and finalising and confirming the data. KSB took over the PyeongChang polyclinic data. GHB took over the Gangneung polyclinic data. SYL was responsible for statistical analysis. HS was responsible for emergency and trauma data. MGO was responsible for outpatient clinic and image study data. SJYR was responsible for pharmacy data.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: These authors, there immediate family and research foundation with which they are affiliated did not receive any financial payments or other benefits from any commercial entity related to the subject of this article.
Patient consent for publication: Not required.
Ethics approval: The study was approved by the research ethics committee of the Wonju College of Medicine, Yonsei University (approval no. CR318001).
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data are available in a public, open access repository. All data relevant to the study are included in the article or uploaded as online supplementary information.
References
- 1. Piat SC, Minniti D, Traversi D, et al. . Torino 2006 winter Olympic games: highlight on health services organization. J Emerg Med 2010;39:454–61. 10.1016/j.jemermed.2009.08.028 [DOI] [PubMed] [Google Scholar]
- 2. Soligard T, Steffen K, Palmer-Green D, et al. . Sports injuries and illnesses in the Sochi 2014 Olympic winter games. Br J Sports Med 2015;49:441–7. 10.1136/bjsports-2014-094538 [DOI] [PubMed] [Google Scholar]
- 3. Drawer S, Fuller CW. Evaluating the level of injury in English professional football using a risk based assessment process. Br J Sports Med 2002;36:446–51. 10.1136/bjsm.36.6.446 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Schwellnus M, Derman W, Jordaan E, et al. . Factors associated with illness in athletes participating in the London 2012 Paralympic games: a prospective cohort study involving 49,910 athlete-days. Br J Sports Med 2013;47:433–40. 10.1136/bjsports-2013-092371 [DOI] [PubMed] [Google Scholar]
- 5. Derman W, Schwellnus M, Jordaan E, et al. . Illness and injury in athletes during the competition period at the London 2012 Paralympic games: development and implementation of a web-based surveillance system (WEB-IISS) for team medical staff. Br J Sports Med 2013;47:420–5. 10.1136/bjsports-2013-092375 [DOI] [PubMed] [Google Scholar]
- 6. Engebretsen L, Soligard T, Steffen K, et al. . Sports injuries and illnesses during the London summer Olympic Games 2012. Br J Sports Med 2013;47:407–14. 10.1136/bjsports-2013-092380 [DOI] [PubMed] [Google Scholar]
- 7. Engebretsen L, Steffen K, Alonso JM, et al. . Sports injuries and illnesses during the winter Olympic Games 2010. Br J Sports Med 2010;44:772–80. 10.1136/bjsm.2010.076992 [DOI] [PubMed] [Google Scholar]
- 8. Steffen K, Soligard T, Engebretsen L. Health protection of the Olympic athlete. Br J Sports Med 2012;46:466–70. 10.1136/bjsports-2012-091168 [DOI] [PubMed] [Google Scholar]
- 9. Ljungqvist A, Jenoure P, Engebretsen L, et al. . The International Olympic Committee (IOC) consensus statement on periodic health evaluation of elite athletes March 2009. Br J Sports Med 2009;43:631–43. 10.1136/bjsm.2009.064394 [DOI] [PubMed] [Google Scholar]
- 10. International Olympic Committee Olympic Charter—the organisation, action and operation of the Olympic movement. IOC. Available: https://stillmed.olympic.org/media/Document%20Library/OlympicOrg/General/EN-Olympic-Charter.pdf [Accessed 15 Sep 2017].
- 11. Athanasopoulos S, Kapreli E, Tsakoniti A, et al. . The 2004 Olympic games: physiotherapy services in the Olympic village polyclinic. Br J Sports Med 2007;41:603–9. 10.1136/bjsm.2007.035204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Vanhegan IS, Palmer-Green D, Soligard T, et al. . The London 2012 Summer Olympic Games: an analysis of usage of the Olympic Village 'Polyclinic' by competing athletes. Br J Sports Med 2013;47:415–9. 10.1136/bjsports-2013-092325 [DOI] [PubMed] [Google Scholar]
- 13. Eaton SB, Woodfin BA, Askew JL, et al. . The Polyclinic at the 1996 Atlanta Olympic village. Med J Aust 1997;167:599–602. 10.5694/j.1326-5377.1997.tb138909.x [DOI] [PubMed] [Google Scholar]
- 14. Gärtner BC, Meyer T. Vaccination in elite athletes. Sports Med 2014;44:1361–76. 10.1007/s40279-014-0217-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Available: https://en.wikipedia.org/wiki/2018_Winter_Olympics#Event_scheduling
- 16. Robilotti E, Deresinski S, Pinsky BA. Norovirus. Clin Microbiol Rev 2015;28:134–64. 10.1128/CMR.00075-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. McIntosh EDG. Healthcare-Associated infections: potential for prevention through vaccination. Ther Adv Vaccines Immunother 2018;6:19–27. 10.1177/2515135518763183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Edouard P, Depiesse F, Branco P, et al. . Analyses of Helsinki 2012 European athletics Championships injury and illness surveillance to discuss elite athletes risk factors. Clin J Sport Med 2014;24:409–15. 10.1097/JSM.0000000000000052 [DOI] [PubMed] [Google Scholar]
- 19. Guermazi A, Hayashi D, Jarraya M, et al. . Sports injuries at the Rio de Janeiro 2016 summer Olympics: use of diagnostic imaging services. Radiology 2018;287:922–32. 10.1148/radiol.2018171510 [DOI] [PubMed] [Google Scholar]
- 20. Farshad-Amacker NA, Potter HG. MRI of knee ligament injury and reconstruction. J Magn Reson Imaging 2013;38:757–73. 10.1002/jmri.24311 [DOI] [PubMed] [Google Scholar]
- 21. Guenoun D, Le Corroller T, Amous Z, et al. . The contribution of MRI to the diagnosis of traumatic tears of the anterior cruciate ligament. Diagn Interv Imaging 2012;93:331–41. 10.1016/j.diii.2012.02.003 [DOI] [PubMed] [Google Scholar]
- 22. De Lorenzo RA. Mass gathering medicine: a review. Prehosp Disaster Med 1997;12:68–72. 10.1017/S1049023X00037250 [DOI] [PubMed] [Google Scholar]
- 23. Arbon P. The development of conceptual models for mass-gathering health. Prehosp Disaster Med 2004;19:208–12. 10.1017/S1049023X00001795 [DOI] [PubMed] [Google Scholar]