Abstract
For patients with chronic, life-limiting illnesses, admission to the intensive care unit (ICU) near the end of life might not improve patient outcomes or be consistent with patient and family values, goals, and preferences. In this context, advance care planning and palliative care interventions designed to clarify patients’ values, goals, and preferences have the potential to reduce provision of high-intensity interventions that are unwanted or non-beneficial. In this Series paper, we have assessed interventions that are effective at helping patients with chronic, life-limiting illnesses to avoid an unwanted ICU admission. The evidence found was largely from observational studies, with considerable heterogeneity in populations, methods, and types of interventions. Results from randomised trials of interventions to improve communication about goals of care are scarce, of variable quality, and mixed. Although observational studies show that advance care planning and palliative care interventions are associated with a reduced number of ICU admissions at the end of life, causality has not been well established. Using the available evidence we suggest recommendations to help to avoid ICU admission when it does not align with patient and family values, goals, and preferences and conclude with future directions for research.
Introduction
High-intensity care in the intensive care unit (ICU), although beneficial for many, also has the potential to be burdensome and costly, especially for patients with chronic, life-limiting illnesses who are near the end of life. For example, nursing home residents in the USA with advanced dementia had a doubling in use of mechanical ventilation between 2000 and 2013, without any substantial improvement in survival, and the US national health insurance programme, Medicare, spent nearly US$100 million on this high-intensity, low-value care in 2013.1 Over the past decade, the number of ICU beds in the USA has increased, although the number of hospital beds has decreased.2 Most of the 4–6 million patients admitted to ICUs each year in the USA are older than 65 years and have multiple chronic conditions.3 Given the ageing American population, coupled with medical and surgical technological advancements, this population of chronically ill patients is growing, increasing the potential for non-beneficial ICU care at the end of life.1,4 These changes make it imperative to consider the appropriateness of using critical care services for patients who might not benefit from or would not choose critical care interventions.
Some studies suggest that more intensive care at the end of life for patients with chronic, life-limiting illness is associated with poorer quality of life for patients and higher levels of family distress.5–7 Among a national sample of patients older than 65 years, over 70% reported that they would prefer treatment focused on palliation rather than life extension,8 yet the American health-care system is oriented towards providing life-sustaining treatment by default, unless patients actively decline such treatment.7 Therefore, interventions that clarify patients’ values, goals, and treatment preferences with respect to ICU care have the potential to help patients to avoid high-intensity treatments that are unwanted or non-beneficial.9 However, which interventions are most effective at ensuring that ICU admission is consistent with patient and family goals is unclear.
In this Series paper, we discuss the role of advance care planning and palliative care in avoiding unwanted or non-beneficial ICU admission for patients with life-limiting illness, such as those with serious, chronic conditions, who are at high risk of death.10–12 We review both observational and randomised trial evidence13 for interventions that occur in prehospital and non-ICU hospital settings, before admission to the ICU, and propose directions for future research. This Series paper is based on a conceptual framework for interventions to ensure ICU admission is consistent with patient and family values, goals, and treatment preferences (figure 1). We define key terms used throughout this Series paper in panel 1.
Figure 1: Conceptual framework for interventions that might ensure ICU admission is consistent with patient and family values, goals, and treatment preferences.
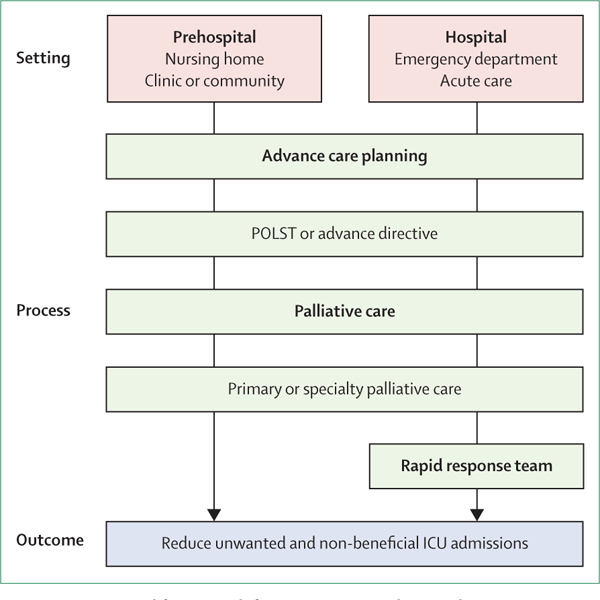
ICU=intensive care unit. POLST=Physician Orders for Life-Sustaining Treatment.
Key messages.
Advance care planning and specialty palliative care consultation have been associated with reductions in intensive care unit (ICU) admissions in both the prehospital and hospital setting; these associations are more robust in specific patient populations at high risk of death, including patients with cancer or dementia
Physician Orders for Life-Sustaining Treatment forms have been associated with reductions in ICU admissions, especially for patients in a nursing home setting
Early involvement of specialty palliative care in the outpatient setting might have an important role in preventing ICU admissions for patients with cancer, and this beneficial role might translate to other chronic, life-limiting conditions
Once admission to the ICU has occurred, the utility of pre-existing advance directives for reducing intensity of care is restricted, which highlights the importance of early intervention
Screening for palliative care needs coupled with triggered palliative care consultations in the emergency department and acute care settings might help to avoid ICU admissions
A causal relationship between the use of advance care planning and specialty palliative care consultations and reductions in ICU admissions has not been firmly established; additional research is necessary to identify the most effective ways to use these interventions to reduce non-beneficial health-care use at the end of life
Interventions in the prehospital setting
Advance care planning interventions
There is an extensive body of literature evaluating advance care planning interventions,14–19 with most studies examining either process outcomes (eg, documentation of preferences and satisfaction with care) or associations with health-care use. However, few studies have focused on ICU admission as an outcome. In this section, we review the following three components of advance care planning as it influences ICU admission: advance directives, advance care planning interventions in nursing homes, and the Physician Orders for Life-Sustaining Treatment (POLST) form.
Three retrospective studies have assessed the relationship between advance directives and ICU admission in the general adult population. A 2007 population-weighted analysis of decedents in the USA with non-traumatic death found that decedents with advance directives known to their family received less intensive care and mechanical ventilation, had fewer in-hospital deaths, and had greater use of hospice services during the last month of life than decedents with no known advance directive.20 In two retrospective cohort studies21,22 published in 2014, similar associations between advance directives and intensive care use were identified among decedents in the longitudinal Health and Retirement Study. In these studies, advance directives were associated with less use of mechanical ventilation and cardiopulmonary resuscitation (CPR) in all patients who were enrolled,21 and with less ICU use among those enrolled who were community dwelling with severe cognitive impairments.22 In each of these studies, both dementia and residence in a nursing home were associated with lower intensity of care near the end of life; however, examination of these factors as effect modifiers found that the beneficial effects of advance directives were observed principally among patients who were community dwelling with severe dementia who did not live in a nursing home. By contrast, no consistent association was observed between advance directives and study outcomes in individuals with normal cognition or mild cognitive impairment. Although participants who resided in nursing homes received less aggressive end-of-life care, this treatment appeared to be the case regardless of the presence of an advance directive.22
Cohort studies of populations with specific chronic, life-limiting diseases have also provided evidence to guide the optimal implementation of advance directives. Among nursing home residents with end-stage renal disease, results from a large Medicare-database retrospective cohort study23 showed that patients with advance directives received fewer ICU admissions and hospital admissions, and less mechanical ventilation and CPR, than those without advance directives. Among patients with heart failure, results from a smaller longitudinal cohort study24 found that advance directives were associated with less mechanical ventilation near the end of life and a trend toward fewer ICU admissions (appendix).
Although advance directives in the prehospital setting might prevent unwanted or non-beneficial ICU admissions, once a patient has been admitted to the ICU an existing advance directive might not influence intensity of care. Two matched cohort studies25,26 comparing care between patients admitted to the ICU with and without advance directives reported no difference in length of stay in the ICU, mechanical ventilation, vasoactive infusions, or dialysis; although one of these studies26 found that patients with advance directives received less CPR. Additionally, two retrospective cohort studies27,28 of patients admitted to oncological ICUs at cancer centres also found no differences between those patients with and without advance directives in the use of mechanical ventilation, vasoactive infusions, renal replacement therapy, invasive diagnostic procedures, or CPR.
Multifaceted, multidisciplinary advance care planning interventions in nursing homes are an attractive approach to improving care.15 Although we did not find any studies examining the effect of these interventions specifically on ICU admission, we did find studies showing the effects of these interventions on hospital admissions. Two large controlled trials, one randomised29 and one non-randomised,30 examined systematic implementation of a non-physician advance directive programme in nursing homes, and both identified reductions in hospital admissions for those patients receiving the intervention, compared with recipients of usual care (appendix). In a large systematic review,14 complex advance care planning interventions in nursing homes were associated with a lower frequency of hospital care, higher levels of compliance with patients’ preferences, and more satisfaction with care as assessed by family members when compared with usual care.
Since 2004, much attention has been devoted to the POLST form, a portable order form that specifies treatment limitations for emergency care. Compared with traditional advance directives, which often do not provide definitive guidance in medical emergencies,31 the POLST is designed to map treatment preferences onto portable medical orders by use of standardised language acceptable to health-care providers across the continuum of care.32,33 These features have enabled systematic implementation of the POLST paradigm across multiple care settings. As of May, 2019, 24 states have implemented POLST programmes endorsed by the National POLST Paradigm, and all of the remaining 26 states and Washington DC have POLST programmes under development.34
Although the POLST has been promoted across the USA, to our knowledge, no randomised trials have examined the efficacy of the POLST in reducing care intensity near the end of life. The seminal 1998 description of the efficacy of the POLST was an uncontrolled, prospective study33 of care received by 180 nursing home residents with POLST orders for do not resuscitate (DNR) and comfort measures only. Over a 1-year follow-up period, most residents did not receive any inpatient care, and none of the participants received intensive care, mechanical ventilation, or CPR. Of the 38 deaths that occurred during the follow-up period, 36 occurred without a preceding hospital admission.33 Despite the absence of a comparison group, this study suggested that POLST forms might influence intensity of care at the end of life.
Subsequent retrospective cohort studies35–37 have also identified associations between treatment-limiting POLST forms and intensity of care near the end of life. A large, multistate retrospective cohort study35 of nursing home residents, both living and decedents, examined a composite outcome of hospital admissions, emergency department visits, invasive diagnostics and therapies, and mechanical ventilation. In this study, treatment-limiting POLSTs were independently associated with a lower incidence of the composite outcome35 and, within this same cohort, those with POLST forms precluding intensive care were rarely admitted to the ICU.36 However, nursing home residents who died during a terminal hospital admission were excluded from this cohort, raising concerns about possible systematic exclusion of recipients of POLST-discordant intensive care. A retrospective cohort study37 of decedents residing in a single community with integrated health-care systems and a community wide multidisciplinary advance care planning programme, also reported that fewer than 5% of the patients received POLST-discordant intensive care within their last 30 days of life.
Descriptive studies examining the effectiveness of POLST have yielded additional insights. An analysis of treatments received by nursing home residents found that those with POLSTs usually received treatments that were consistent with their POLST orders.36 In prehospital care, an unadjusted analysis of an out-of-hospital cardiac arrest cohort found that POLST-DNR orders were associated with less in-field CPR;38 however, 11 (22%) of 50 patients with POLST-DNR orders still received some in-field CPR, with 6 (12%) of 50 patients receiving continued CPR for the duration of prehospital care. In contrast to studies that enrolled living nursing home residents, which report a very low rate of POLST-discordant care,33,36 a descriptive study of care received by decedents from a care facility for older people found that approximately one in five patients with treatment-limiting POLSTs received more aggressive care than ordered by the POLST.39 These findings suggest room for improvement in the implementation of POLST (appendix).
Advance care planning has been widely promoted as a process that allows patients to specify treatment preferences for the future. However, most contemporary studies examining the effectiveness of advance directives in reducing ICU care are observational in nature and do not establish a causal relationship between advance directives and reductions in ICU admissions. Although this study design limits the ability to draw firm conclusions about the effects of advance care planning on intensity of care at the end of life, the literature does show findings that are likely to be relevant to the implementation of advance care planning interventions. Most positive findings were reported in specific populations with a high burden of morbidity, including nursing home residents, patients with severe cognitive impairment, and patients with specific chronic diseases (eg, heart failure and end-stage renal disease). This trend suggests that advance directives and POLST forms might have the highest potential to reduce both unwanted and non-beneficial ICU use for populations at high risk of death, and in specific patient groups with high medical input (eg, renal failure and heart failure), compared with the general population. For these patients, the presence of an advance directive or POLST might serve as an indicator of exposure to high-quality end-of-life counselling, or the occurrence of explicit conversations about values, goals, and preferences with family members. However, the observation that many patients still receive intensive care despite treatment-limiting advance care documents serves as an important reminder that there are many factors apart from patients’ values, goals, and preferences that influence ICU use. Additional studies of the implementation of advance care planning and palliative care in the outpatient setting are needed to better understand how to more effectively avoid unwanted or non-beneficial high-intensity therapies.
Palliative care interventions
Because many patients prefer to discuss goals-of-care when they feel well enough to participate,40,41 and to have these discussions with the physicians who care for them,42,43 the outpatient clinic represents an important setting to engage in early conversations about goals and preferences for future treatment. Few studies have specifically investigated the association between primary or specialty palliative care interventions, or both, in outpatient clinic settings and subsequent ICU use.
Two randomised trials44,45 investigating multicomponent palliative care interventions in patients with advanced cancer in outpatient settings, including early versus delayed palliative care consultation, found no difference in days spent in the ICU, which was a secondary and underpowered outcome (appendix). By contrast, a large retrospective study examined the association between specialty palliative care and aggressiveness of end-of-life care in the last 30 days of life in a cohort of patients with advanced pancreatic cancer. This study found that patients who received an outpatient palliative care consult were much less likely to be admitted to the ICU near death than patients who did not receive an outpatient palliative care consult, and more frequent palliative care follow-up was associated with fewer instances of intensive care near death.46 Another retrospective cohort study included patients with advanced cancer who were enrolled in a multidisciplinary outpatient palliative care programme that used early end-of-life care planning and weekly interdisciplinary meetings. In this study,47 patients in the control group had a higher likelihood of ICU admission at the end of life than patients who were enrolled in the multidisciplinary outpatient palliative care programme. Although early palliative care was associated with fewer ICU admissions, there was no association with ICU length of stay, code status, or ICU procedures once admitted to the ICU (appendix).
The identified studies44–47 assessing palliative care in the outpatient setting primarily involved specialty palliative care for patients with advanced cancer near the end of life, which limits the ability to generalise findings to other patient populations. In addition, the results were mixed, with no significant reduction in ICU use in randomised trials compared with evidence of fewer ICU admissions in the larger observational studies. Inconsistent results might be attributable to issues of power and variation in the quality and dose of palliative care interventions.48,49 Selection bias is also an important consideration in observational studies of palliative care. Patients who agree to engage in specialty palliative care might represent individuals who had preferences for less aggressive treatment that pre-dated palliative care involvement. Overall, the evidence suggests that early involvement of palliative care (primary or specialty), coupled with frequent follow-up throughout the course of disease, might give reductions in ICU admissions. An enhanced understanding of the relationship between palliative care in the outpatient setting and subsequent ICU admission will require additional investigation, including studies of diverse patient populations and studies that include outcomes such as measures of goal-concordant care.
Interventions in the hospital setting
For patients with chronic, life-limiting illness, exploration of goals of care and treatment preferences should begin in the prehospital setting. However, in many cases these conversations do not begin until an acute condition arises. For others, previously expressed goals and preferences change,50,51 requiring clinicians to revisit these topics in the acute care setting. In both scenarios, acute care clinicians must navigate conversations about goals of care and treatment preferences during an acute illness. In this section, we examine interventions aimed at clarifying goals and preferences in the hospital setting and assess the relationship between enhanced communication and ICU admission in three settings: the emergency department; acute care; and in the context of a rapid response or medical emergency team activation.
Emergency department
For most patients, admission to the acute care floor or ICU is preceded by a stay in the emergency department, a place in which exploration of goals of care and treatment preferences can be extremely challenging.52–57 Rapidly changing physiology, scarcity of information about the patient’s premorbid function, and time constraints all affect the ability to align care with goals and preferences in the emergency department. Moreover, patients might be unable to communicate, requiring clinicians to rely on family members to participate in the decision-making.58,59 Although the barriers to engaging patients and family members in discussions about goals and preferences in the emergency department are clear, the emergency department is also a natural transition point when clinicians have an opportunity to prevent unwanted or non-beneficial ICU admissions. Decisions to withdraw or withhold life-sustaining treatments are common in the emergency department,58–61 but the frequency and characteristics of accompanying conversations about goals of care and treatment preferences underpinning these decisions are not well described. Existing studies about decision-making related to life-sustaining therapies in the emergency department suggest that these decisions rely heavily on the perspective of the emergency department physician,55 with little input from nursing staff 58 or family members.58–61 These observations provide little insight into the quality of conversations occurring with patients and family members in the emergency department, and suggest deficiencies in the current approach to aligning care with goals and preferences.
One way to enhance conversations about goals and preferences in the emergency department includes involving clinicians trained to have these conversations, such as palliative care clinicians. A single-blind, randomised trial of palliative care consultation initiated in the emergency department enrolled adults with advanced cancer at an urban, academic emergency department.62 Research staff screened the emergency department track board for patients with advanced cancer and approached 311 patients for participation; of these, 136 participants were enrolled and randomised. Those patients randomly assigned to the intervention received a comprehensive palliative care consultation by the inpatient team on the same or following day. The primary outcome was quality of life measured by the change in Functional Assessment of Cancer Therapy-General Measure score at 12 weeks, and secondary outcomes included symptoms of depression measured by the Patient Health Questionnaire-9, health-care use at 180 days, and survival at 1 year. Quality of life was higher in patients randomised to the intervention, with no significant differences in symptoms of depression, hospital days, ICU admission, or discharge to hospice (appendix).62 Of note, the study was underpowered to detect differences in ICU admission because of few ICU admissions from the emergency department.
Observational studies and quality improvement approaches have also been used to assess the role of screening for palliative care needs and palliative care consultation in the emergency department,63–69 with consistently positive results regarding reduced health-care use.63,66,68 An observational evaluation63 of palliative care and case management for chronically ill older patients in the emergency department showed a reduction in hospital length of stay (7–9 days to 7 days) compared with baseline preproject chart review. They also observed a higher number of admissions to the palliative care unit from the emergency department during the intervention.63 Development of a palliative care pathway in the emergency department, including education about palliative care for clinicians in the emergency department and palliative care consultation occurring in the emergency department, was associated with a reduction in hospital length of stay for patients seen by the palliative care team in the emergency department, compared with patients seen after admission.66 Another observational study examined enhanced training in palliative care for clinicians in the emergency department at a large, specialised care centre.68 As a part of this intervention, nurse practitioners in the emergency department identified older patients (≥65 years) who might benefit from advance care planning or referral to palliative or hospice care, on the basis of the risk for future hospitalisation and life expectancy of 6 months or less, and then expedited referrals to social work, palliative care, or hospice. Following implementation, geriatric emergency department admissions to the ICU were lower68 (appendix).
Acute care floor
Although some obstacles to communication are removed after the patient leaves the emergency department, data suggest that conversations about goals of care and treatment preferences are still unlikely to occur on the acute care floor, and patients’ goals and preferences are infrequently recorded in the medical record.13,70–73 An observational study70 of communication between attending hospitalist physicians and their patients at the time of hospital admission found that 66% of seriously ill patients had no discussion of code status. In a prospective study71 of older patients (mean age of 80 years) at high risk of dying in the next 6 months, agreement between the patients’ expressed preferences for end-of-life care and documentation in the medical record was only 30%. In the acute care setting, clinician-perceived barriers to communication about goals and preferences shift from external factors cited in the emergency department (eg, time constraints and inadequate access to medical records) to factors related to the patient and family (eg, the inability of patients or family members to appreciate prognosis or understand the limitations of life-sustaining therapies).74,75 However, whether these barriers are accurately perceived by clinicians, or are attributable to clinician-patient communication that fails to effectively elucidate patient’s goals and preferences and place those goals and preferences in the context of the patient’s condition, is unclear.
Interventions to improve communication about goals of care and treatment preferences in the inpatient setting have produced mixed results (appendix).13,76,77 One of the most notable studies, the SUPPORT trial13 published in 1995, did not identify improvements in physician-patient communication or decreased use of intensive care after implementation of an intervention that included provision of prognostic estimates to physicians as well as patient and family engagement with a specifically trained nurse dedicated to eliciting preferences and enhancing patient-physician communication. However, other inter-ventions76,77 to help patients to express treatment preferences in the inpatient setting have been successful in promoting the completion of advance directives and care plans. A single-centre randomised trial77 of an intervention to facilitate advance care planning in the inpatient setting enrolled 309 medical inpatients aged 80 years or more, and then followed participants for 6 months or until death. Advance care planning was done by a trained facilitator, with family members present for 72% of the discussions. Among patients who died by 6 months, end-of-life preferences were more likely to be followed in the intervention group compared with the control group, and family members in the intervention group had fewer symptoms of psychological distress. In addition, patient and family satisfaction were higher in the intervention group, and patients in the intervention group were less likely to be admitted to and die in the ICU.77
Other attempts to engage inpatients in conversations about goals and preferences have focused on specialty palliative care. In a multi-centre randomised trial,78 inpatients receiving palliative care consultation had fewer ICU admissions on subsequent hospital admissions (appendix). Similarly, two retrospective observational studies79,80 suggest less use of intensive care for inpatients seen by palliative care clinicians. Both studies were done in Veterans Affairs medical centres; one study included veterans with advanced cancer or multiple chronic conditions,80 and the other study included veterans who died after an inpatient hospital stay greater than 3 days.79 There are also studies of palliative care consults triggered by specific patient characteristics. A prospective, sequential, three-cohort study81 implementing triggered palliative care consultations as part of standard care for patients with advanced cancer resulted in improved understanding of disease process for patients but found no difference in advance care planning or hospice use; resource use was also similar between cohorts, with no significant difference in proportion of patients transferred or admitted to the ICU. A quality improvement intervention82 with a combination of communication skills training for oncologists and triggered palliative care consultations for patients with advanced cancer resulted in more goals-of-care conversations when comparing the first 3 months of the study with the final 3 months, but did not change rates of ICU transfer (appendix).82
Rapid response and medical emergency teams
For inpatients whose hospital stay is complicated by a clinical deterioration on the acute care floor, the rapid response team (RRT), also known as a medical emergency team, might provide the last opportunity to clarify goals and preferences before ICU admission. Although the appropriateness of having these conversations during urgent or emergent situations is unclear, decisions to forgo life-sustaining interventions or defer admission to the ICU are often made during or immediately after a rapid response call.83–94 Observational studies suggest that rapid response teams play a role in prompting decision-making about life-sustaining interventions85,88,93,94 and can also affect changes in code status for patients, in some cases leading to DNR orders (appendix).83,86,87,89,91 One study84 comparing deaths on acute care before and after implementation of an RRT found a higher likelihood of patients receiving formal end-of-life medical orders after the RRT period than before the RTT period. However, an evaluation of the introduction of an RRT on end-of-life care at three academic hospitals did not identify differences in the proportion of patients with patient and family conferences or orders to forgo life-sustaining interventions on the acute care floor, when comparing time periods before and after RRT implementation.95 In addition, decedents seen by the RRT were less likely to receive palliative care consultation (30–2% vs 55–9%), spiritual care (25–4% vs 41–3%), or an order for sedatives as needed (44–4% vs 65–0%), compared with those not seen by the RRT (appendix). 95
Although mostly observational in nature, the evidence suggests that promoting advance care planning and both primary and specialty palliative care in the hospital setting might improve patient-centred outcomes, including better quality of life, reductions in hospital length of stay, and receipt of goal-concordant care. The absence of a clear trend related to ICU admissions from the emergency department or acute care is not surprising, because not all patients with chronic, life-limiting illness want to avoid the ICU. These interventions aim to improve communication about goals and preferences; whether that leads to a reduction in ICU admissions will be on the basis of the types of patients in the study and their specific goals and preferences. However, a failure to have these conversations in any meaningful way ensures that some patients will experience an unwanted ICU admission.
There is substantial room for improvement in the approach to engaging inpatients in conversations about goals of care and treatment preferences. Multiple factors contribute to the deficiencies in communication, including inadequate preparation on the part of clinicians to have goals-of-care conversations with patients and their families.96 The availability of palliative care clinicians is not sufficient to meet the needs of all patients who might benefit from a goals-of-care conversation.97 The ability to provide primary palliative care should be an essential skill for all clinicians providing care in the emergency department or acute care setting. Each hospital setting will require a unique approach to enhancing communication about goals and preferences. In the emergency department, a multi-faceted approach might include education of emergency medicine clinicians in the provision of primary palliative care, use of screening tools to identify patients with palliative care needs, and consultation of specialty palliative care clinicians in specific cases. Ideally, such interventions would be informed by a better understanding of patient and family perspectives about discussing goals of care and treatment preferences in the emergency department. On the acute care floor, efforts might include engaging patients in advance care planning and consideration of palliative care consultation for patients at high risk of death. One subset of inpatients who might benefit most from palliative care involvement includes individuals experiencing acute decompensation, in which conversations during rapid response events seem to focus primarily on preferences for life-sustaining treatments and perhaps less on patient values and overall goals of care.
Common challenges and potential solutions
In an ideal world, patients and their family members would engage in conversations about the patient’s values, goals of care, and treatment preferences before the development of life-threatening illness.98 However, in many cases these conversations do not occur before the development of a critical illness. Even when they have occurred, the dynamic nature of a patient’s illness might mean that previous conversations must be reevaluated, and previous decisions reframed in the context of a rapidly changing condition. Conflicts might arise when patients or their family members request interventions that clinicians view as futile or potentially inappropriate (panel 1).99 A recent multi-society statement provides recommendations to prevent and manage disagreements between surrogate decision-makers and clinicians. When potentially inappropriate treatments are requested, the guidelines recommend that clinicians communicate and advocate for the treatment plan they believe is most appropriate and if needed, implement a process of conflict-resolution.99
One approach that might minimise the provision of potentially inappropriate interventions in an ICU is to offer patients with decisional capacity, or family members if the patient does not have decisional capacity, the option of deferring decisions to clinicians.100,101 Patients and their family members vary in their desire for decisional control.102,103 Although patients and family members almost uniformly want to be informed and to know that decisions are made on the basis of the patients’ values and goals,104 they do not necessarily want to assume responsibility for decisions about initiating or continuing intensive medical care. When patients or family members would rather defer decision-making to clinicians, forcing these patients and family members to make decisions or be involved in decision-making might result in default decisions, which favour intensive treatments that might not be beneficial or might be inconsistent with patient values or preferences. When clinicians put patients and family members in the position of making complex medical decisions they would prefer not to make, we also risk worse patient-centred and family-centred outcomes, including increased symptoms of post-traumatic stress and complicated grief.104,105 Clinicians should strive to assess decision-making preferences of patients with serious illness and their family members and match the decision-making approach to those preferences.106,107
Clinicians are not obligated to implement treatment plans they feel are unethical or subject patients to harm without the potential for benefit. However, adopting an authoritarian approach to treatment decisions, without first ascertaining the decision-making preferences of patients and their family members, can escalate conflict and might generate additional distress for all involved parties. It has been our experience that in most conflicts, a compromise can be reached. This compromise often requires a multi-disciplinary approach, including specialty palliative care providers.
Although an important outcome of advance care planning and palliative care interventions is the receipt of goal-concordant care, measurement of this outcome is difficult. There are emerging efforts to measure goal-concordant care; however, this measure is a challenging area of research.108–110
Limitations
This Series paper has several limitations, most notably the paucity of high-quality studies on this topic. Although we have made recommendations on the basis of the available evidence, we recognise that the current evidence is mostly comprised of associations from observational studies, with considerable heterogeneity in populations, methods, and types of interventions. We also recognise that randomised trial data are scarce, of variable quality, and have shown mixed results. Therefore, causation cannot be determined. There are little data supporting valid measurement of goal-concordant care and thus it is difficult to assess intervention effects on receipt of goal-concordant care. Finally, our search strategy might not have captured all available evidence. Although our review was pragmatic, the systematic nature of our literature search and screening of articles, combined with vetting by experts in the field, make it improbable that key articles were missed.
Summary and recommendations
Despite limitations in the existing evidence, we believe that the existing data supports the following conclusions: first, advance care planning and specialty palliative care consultation in both pre-hospital and hospital settings might prevent ICU admissions in patients at high risk of death, including patients in nursing homes and those with chronic, life-limiting illness (eg, advanced cancer, heart failure or renal disease, and severe dementia); second, the POLST form might also prevent ICU admissions, especially when implemented in a nursing home setting; third, early involvement of specialty palliative care might prevent ICU admissions in the outpatient setting for patients with cancer; fourth, once admission to the ICU has occurred, the use of pre-existing advance directives for reducing intensity of care appears limited; and fifth, screening for palliative care needs, coupled with triggered palliative care consultations, might help to avoid ICU admissions for patients in the emergency department and acute care settings. A summary of strategies to avoid both unwanted and non-beneficial ICU admission is included in figure 2.
Figure 2: Summary of strategies to avoid unwanted and non-beneficial ICU admission.
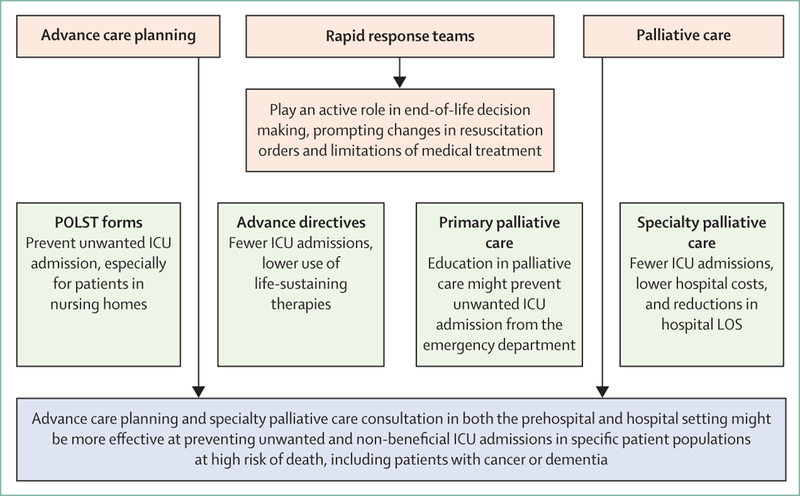
ICU=intensive care unit. LOS=length of stay. POLST=Physician Orders for Life-Sustaining Treatment.
On the basis of these findings, we make several recommendations designed to ensure that ICU admission is consistent with patient values, goals, and preferences. First, patients who are diagnosed with chronic, life-limiting conditions should have goals-of-care discussions shortly after the diagnosis is made. Studies in the past 3 years suggest that several interventions can increase the occurrence, documentation, and quality of goals-of-care discussions in the outpatient setting.109,111–114 This recommendation is further supported by our finding that advance directives do not appear to substantially influence intensity of care after ICU admission, suggesting that ICU admission dictates subsequent care for patients with chronic, life-limiting illness. This finding reinforces the importance of pre-hospital and acute care interventions to reduce ICU admissions near the end of life. Additionally, beginning discussions in the prehospital setting might not only help to prevent both unwanted and non-beneficial ICU admissions, but also prime patients and their family members if goals of care need to be readdressed in an acute care setting.
Second, the POLST form appears to be most effective in preventing unwanted or non-beneficial ICU admissions when completed by specific populations, such as patients residing in nursing homes and patients with advanced illness who prefer limitations to life-sustaining treatments. POLST initiatives should target these populations, given their high risk of death. Third, because the demand for specialty palliative care exceeds the resources both in the USA and globally,97,115,116 clinicians who deliver care in the emergency department and acute care settings need training in primary palliative care so that they are capable of engaging in meaningful conversations with patients and their family members about goals of care and treatment preferences.7 Additionally, clinicians need to develop screening systems that identify patients with palliative care needs and, if warranted, prompt specialty palliative care consultation.117,118
Collectively, our findings show the complexity of advance care planning and palliative care interventions, in both implementation and measurement of effect. The existing evidence does not strongly support a single type of intervention, in either the outpatient or inpatient setting, as the most effective way to help patients avoid unwanted and non-beneficial ICU admission. A multifaceted, complex set of interventions that span settings is probably needed.18 We therefore recommend that for patients with chronic, life-limiting illness, discussions about goals of care begin in the pre-hospital and outpatient setting and extend into the hospital setting, in advance of admission to the ICU. These discussions should be used to guidewhether admission to the ICU is consistent with a patient’s values and if the interventions available in an ICU setting will help them to achieve their goals of care.
Future directions
In panel 2, we list key research challenges and proposed approaches that we believe will improve the quality of advance care planning and palliative care interventions for patients with chronic, life-limiting illnesses. Several clinical trials are currently underway investigating how to deliver advance care planning and palliative care, which might address the deficits that we noted earlier. We highlight these trials that are available on ClinicalTrials.gov in the table. This list includes studies examining interventions with diverse populations and in diverse environments.
Panel 2: Research challenges and proposed approaches.
Measuring palliative care needs among patients and families at high risk for poor outcomes
Identification of advance care planning and palliative care interventions that lead to goal-concordant care
Development, validation, and implementation of a measure for goal-concordance
Designing complex interventions that span settings and providers
Novel intervention designs and tools to ensure preferences are transmitted across settings and readdressed as needed
Designing and delivering high-value interventions
Detailed collection of costs associated with providing an intervention and both cost and use outcomes to do robust economic evaluations
Table:
Characteristics of planned, ongoing, or recently completed studies evaluating advance care planning in inpatient and outpatient settings
| Country | Setting | Study type | Estimated enrolment | Exposure | Primary outcome | Secondary outcome(s) | |
|---|---|---|---|---|---|---|---|
| Emergency Medicine Palliative Care Access, March, 2018-August, 2022 | USA | Seven hospitals | Randomised, parallel assignment clinical trial | 2025 adults over 50 years with advanced cancer, COPD, end stage organ failure, or heart failure and their caregivers who present to emergency department | Nurse-led telephonic palliative care vs outpatient specialty palliative care | Change in quality of life for patients, measured by FACT-G | Health-care use, loneliness, symptom burden, caregiver strain, and bereavement. |
| Advance Care Planning at London Health Sciences Centre (ACP@LHSC), January, 2017-December, 2018 | UK | Single academic medical centre | Randomised, parallel assignment clinical trial | 400 complex patients admitted to acute care floor | In-depth conversations about ACP for those referred to intervention vs random selection | Discordance between goals of care expressed and care received. | Risk factors for discordance |
| Integrated Multidisciplinary Patient and Family Advance Care Planning Trial (IMPACT), August, 2018-September, 2019 | USA | One accountable care organisation | Randomised, pragmatic comparative effectiveness trial | 600 multi-morbid older adults (≥65 years) in primary care | ACP with nurse navigator vs usual care | Number and quality of ACP discussion from perspective of patient and providers. | ACP billing code usage, ADs completed, and number of surrogate decision-makers |
| Engaging in Advance Care Planning Talks (ENACT), August, 2017-May, 2020 | USA | One primary care health system | Pilot randomised controlled trial | 120 medically complex older adults (>50 years) in primary care | Facilitated group ACP discussions vs mailed ACP materials | Change in documentation of the surrogate decision-maker | Readiness to participate in ACP, change in AD in medical record, and change in participant choice of surrogate decision-maker |
| Advance Care Planning in Nursing Homes in Flanders (ACP+), March, 2018-December, 2018 | Belgium | 14 nursing homes | Randomised controlled trial | 284 nursing home staff, to increase knowledge of and comfort with ACP | ACP training programme vs usual care | Change in knowledge and attitudes regarding ACP | .. |
| BABEL Advance Care Planning in Long-term Care, August, 2018-March, 2020 | Canada | Multiple nursing homes | Randomised, clustered, parallel assignment clinical trial | 1129 nursing home residents | BABEL ACP intervention vs usual care | ACP processes and Comfort in Dying of Nursing Home Residents measure | Rate of transfer from nursing home to emergency department or hospital, rate of antibiotic and feeding tubes in nursing homes, discordance in care received vs documented wishes, and staff efficacy in ACP |
| Aligning Patient Preferences a Role Offering Alzheimer’s Patients, Caregivers, and Healthcare Providers Education and Support (APPROACHES), September, 2019-September, 2022 | USA | Multiple nursing homes | Randomised, clustered, parallel assignment clinical trial | 22 650 nursing home residents with Alzheimer’s disease or related dementias | ACP specialist programme vs usual care | Hospital transfers | ACP preferences documentation, hospice enrolment, death in hospital, and family satisfaction |
| Palliative Care Communication with Alaska Native and American Indian People (PALL), December, 2017-June, 2019 | USA | Two primary care sites | Randomised, parallel assignment clinical trial | 60 outpatient American Indian or Alaska Native patients | Tailored ACP intervention vs usual care | ACP communication occurrence and ACP communication quality | Advance directives |
| Reducing Disparities in the Quality of Palliative Care for Older African Americans Through Improved Advance Care Planning (EQUAL-ACP), November, 2018-September, 2022 | USA | Ten primary care practices from five medical centres in Deep South* | Randomised, parallel, clustered clinical trial | 800 chronically ill older adults (≥65 years) | Structured ACP approach with trained facilitator vs ACP documents | Proportion of African American adults vs white adults completing ACP | Patient readiness to engage in ACP, patient quality of life |
| With Love: Using Promotoras† for a Hispanic Community Palliative Care Intervention, April, 2018-November, 2019 | USA | Two Texas medical centres | Randomised, parallel, clustered clinical trial | 150 Latinx patients with cancer | Three face to face meetings with community educator vs usual care | Pain scores, patient health questionnaire 9, physical wellbeing, social wellbeing, emotional wellbeing, and palliative care subscale | ICU admissions and emergency department visits |
COPD=chronic obstructive pulmonary disease. FACT-G=Functional Assessment of Cancer Therapy-General Measure. ACP=advanced care planning. AD=advance directive. ICU=intensive care unit.
Deep South refers to University of Alabama (Birmingham, AL), University of South Carolina (Columbia, SC), Emory University (Atlanta, GA), Duke University (Durham, NC), and University of Texas Southwestern (Dallas, TX).
Promotoras are community health workers in Latinx communities.
Ensuring that admission to the ICU aligns with patients’ values, goals, and treatment preferences begins with advance care planning. The goal is to help to ensure that people receive medical care that is consistent with their values, goals, and preferences in the context of serious and chronic illness.120 These preferences need to be documented so that information is transmitted across settings and readdressed in the inpatient setting through high quality primary and specialty palliative care. Future investigations would benefit from using novel approaches to patient care, specifically the use of technology including point-of-care interventions that allow patients to tailor communication to their specific needs, avoiding a one-size-fits all approach. This flexibility might allow patients and their family members to transform a static approach to advance care planning and palliative care (ie, isolated visits or single episodes of documenting preferences) into a dynamic process that changes as their needs change.
Supplementary Material
Panel 1: Definitions and descriptions of key terms.
Patient perspectives
Values-Pertains to judgements about what is most important in life; patients and family members might prioritise concepts such as life extension, independence, cognitive capacity, or comfort
Goals-Refers to specific results desired by patients and their family members; for example, returning home or living to see a child get married
Preferences-Refers to choices about specific treatments, particularly life-sustaining interventions such as mechanical ventilation or cardiopulmonary resuscitation
Interventions
Non-beneficial-Does not benefit the patient; is grounded in an understanding of the patient’s values and preferences, accompanied by clinician perspective regarding the potential of an intervention to achieve the patient’s goals
Unwanted-Undesired by an informed and supported patient; includes interventions that a clinician perceives as potentially beneficial but that the patient decides against, based on their values, goals or preferences
Futile-Cannot accomplish the intended physiological goal
Inappropriate-Has at least some chance of accomplishing a patient’s goals of care but the clinician believes competing considerations justify refusing to provide the treatment
Search strategy and selection criteria.
We searched the PubMed database for studies in English addressing advance care planning or palliative care, or both, in prehospital and non-ICU hospital settings, with a goal of identifying studies that included ICU admission as an outcome. We included studies from Jan 1, 1995 to Aug 31, 2018. We reviewed reference lists from published papers and used experts in the field for additional references to include in this Series paper. We focused on adults (≥18 years) because interventions and outcomes in the neonatal and paediatric ICU are likely to be very different.Our search strategy used terms grouped under three main subject headings that captured advance care planning and palliative care interventions, pre-hospital and hospital settings, and intensive care unit admission. A full list of search terms is included in the appendix. A research librarian assisted with development and execution of our search strategy. Two authors independently screened titles and abstracts to identify relevant studies for full-text review (NK, ACL). Discrepancies were resolved through discussion and consensus. Highlights of studies included in this Series paper are listed in the appendix.
Acknowledgments
We would like to recognise the contributions of Sarah Safranek, research librarian at the University of Washington Health Sciences library.
Footnotes
Declaration of interests
We declare no competing interests.
References
- 1.Teno JM, Gozalo P, Khandelwal N, et al. Association of increasing use of mechanical ventilation among nursing home residents with advanced dementia and intensive care unit beds. JAMA Intern Med 2016; 176: 1809–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wallace DJ, Angus DC, Seymour CW, Barnato AE, Kahn JM. Critical care bed growth in the United States. A comparison of regional and national trends. Am J Respir Crit Care Med 2015; 191: 410–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Halpern NA, Pastores SM, Oropello JM, Kvetan V. Critical care medicine in the United States: addressing the intensivist shortage and image of the specialty. Crit Care Med 2013; 41: 2754–61. [DOI] [PubMed] [Google Scholar]
- 4.Ward BW, Schiller JS. Prevalence of multiple chronic conditions among US adults: estimates from the National Health Interview Survey, 2010. Prev Chronic Dis 2013; 10: E65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wright AA, Zhang B, Ray A, et al. Associations between end-of-life discussions, patient mental health, medical care near death, and caregiver bereavement adjustment. JAMA 2008; 300: 1665–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhang B, Wright AA, Huskamp HA, et al. Health care costs in the last week of life: associations with end-of-life conversations. Arch Intern Med 2009; 169: 480–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bernacki RE, Block SD, and the American College of Physicians High Value Care Task Force. Communication about serious illness care goals: a review and synthesis of best practices. JAMA Intern Med 2014; 174: 199–2003. [DOI] [PubMed] [Google Scholar]
- 8.Barnato AE, Herndon MB, Anthony DL, et al. Are regional variations in end-of-life care intensity explained by patient preferences? A Study of the US Medicare population. Med Care 2007; 45: 386–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Khandelwal N, Kross EK, Engelberg RA, Coe NB, Long AC, Curtis JR. Estimating the effect of palliative care interventions and advance care planning on ICU utilization: a systematic review. Crit Care Med 2015; 43: 1102–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ward BW, Schiller JS, Goodman RA. Multiple chronic conditions among US adults: a 2012 update. Prev Chronic Dis 2014; 11: e62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dartmouth Atlas of Health Care. 2018. http://www.dartmouthatlas.org/keyissues/issue.aspx?con=2944 (accessed June 10, 2018).
- 12.Wennberg JE, Fisher ES, Goodman DC, Skinner JS. The Dartmouth Atlas of Health Care 2008. Lebanon, New Hampshire: Dartmouth Medical School, 2008. [Google Scholar]
- 13.The SUPPORT Principal Investigators. A controlled trial to improve care for seriously ill hospitalized patients. The study to understand prognoses and preferences for outcomes and risks of treatments (SUPPORT). JAMA 1995; 274: 1591–98. [PubMed] [Google Scholar]
- 14.Brinkman-Stoppelenburg A, Rietjens JA, van der Heide A. The effects of advance care planning on end-of-life care: a systematic review. Palliat Med 2014; 28: 1000–25. [DOI] [PubMed] [Google Scholar]
- 15.Martin RS, Hayes B, Gregorevic K, Lim WK. The effects of advance care planning interventions on nursing home residents: a systematic review. J Am Med Dir Assoc 2016; 17: 284–93. [DOI] [PubMed] [Google Scholar]
- 16.Hickman SE, Keevern E, Hammes BJ. Use of the physician orders for life-sustaining treatment program in the clinical setting: a systematic review of the literature. J Am Geriatr Soc 2015; 63: 341–50. [DOI] [PubMed] [Google Scholar]
- 17.Jimenez G, Tan WS, Virk AK, Low CK, Car J, Ho AHY. State of advance care planning research: a descriptive overview of systematic reviews. Palliat Support Care 2018; published online July 30. DOI: 10.1017/S1478951518000500. [DOI] [PubMed] [Google Scholar]
- 18.Jimenez G, Tan WS, Virk AK, Low CK, Car J, Ho AHY. Overview of systematic reviews of advance care planning: summary of evidence and global lessons. J Pain Symptom Manage 2018; 56: 436–459.e25. [DOI] [PubMed] [Google Scholar]
- 19.Robinson L, Dickinson C, Rousseau N, et al. A systematic review of the effectiveness of advance care planning interventions for people with cognitive impairment and dementia. Age Ageing 2012; 41: 263–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Teno JM, Gruneir A, Schwartz Z, Nanda A, Wetle T. Association between advance directives and quality of end-of-life care: a national study. J Am Geriatr Soc 2007; 55: 189–94. [DOI] [PubMed] [Google Scholar]
- 21.Tschirhart EC, Du Q, Kelley AS. Factors influencing the use of intensive procedures at the end of life. J Am Geriatr Soc 2014; 62: 2088–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nicholas LH, Bynum JP, Iwashyna TJ, Weir DR, Langa KM. Advance directives and nursing home stays associated with less aggressive end-of-life care for patients with severe dementia. Health Aff(Millwood) 2014; 33: 667–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kurella Tamura M, Montez-Rath ME, Hall YN, Katz R, O’Hare AM. Advance directives and end-of-life care among nursing home residents receiving maintenance dialysis. Clin J Am Soc Nephrol 2017; 12: 435–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dunlay SM, Swetz KM, Mueller PS, Roger VL. Advance directives in community patients with heart failure. Circ Cardiovasc Qual Outcomes 2012; 5: 283–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Goodman MD, Tarnoff M, Slotman GJ. Effect of advance directives on the management of elderly critically ill patients. Crit Care Med 1998; 26: 701–04. [DOI] [PubMed] [Google Scholar]
- 26.Hartog CS, Peschel I, Schwarzkopf D, et al. Are written advance directives helpful to guide end-of-life therapy in the intensive care unit? A retrospective matched-cohort study. J Crit Care 2014; 29: 128–33. [DOI] [PubMed] [Google Scholar]
- 27.Halpern NA, Pastores SM, Chou JF, Chawla S, Thaler HT Advance directives in an oncologic intensive care unit: a contemporary analysis of their frequency, type, and impact. J Palliat Med 2011; 14: 483–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kish Wallace S, Martin CG, Shaw AD, Price KJ. Influence of an advance directive on the initiation of life support technology in critically ill cancer patients. Crit Care Med 2001; 29: 2294–98. [DOI] [PubMed] [Google Scholar]
- 29.Molloy DW, Guyatt GH, Russo R, et al. Systematic implementation of an advance directive program in nursing homes: a randomized controlled trial. JAMA 2000; 283: 1437–44. [DOI] [PubMed] [Google Scholar]
- 30.Caplan GA, Meller A, Squires B, Chan S, Willett W. Advance care planning and hospital in the nursing home. Age Ageing 2006; 35: 581–85. [DOI] [PubMed] [Google Scholar]
- 31.Teno JM, Licks S, Lynn J, et al. Do advance directives provide instructions that direct care? SUPPORT Investigators. J Am Geriatr Soc 1997; 45: 508–12. [DOI] [PubMed] [Google Scholar]
- 32.Dunn PM, Schmidt TA, Carley MM, Donius M, Weinstein MA, Dull VT. A method to communicate patient preferences about medically indicated life-sustaining treatment in the out-of-hospital setting. J Am Geriatr Soc 1996; 44: 785–91. [DOI] [PubMed] [Google Scholar]
- 33.Tolle SW, Tilden VP, Nelson CA, Dunn PM. A prospective study of the efficacy of the physician order form for life-sustaining treatment. J Am Geriatr Soc 1998; 46: 1097–102. [DOI] [PubMed] [Google Scholar]
- 34.The National POLST Paradigm. POLST programs in your state. http://www.polst.org/programs-in-your-state (accessed May 1, 2019).
- 35.Hickman SE, Nelson CA, Perrin NA, Moss AH, Hammes BJ, Tolle SW. A comparison of methods to communicate treatment preferences in nursing facilities: traditional practices versus the physician orders for life-sustaining treatment program. J Am Geriatr Soc 2010; 58: 1241–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hickman SE, Nelson CA, Moss AH, Tolle SW, Perrin NA, Hammes BJ. The consistency between treatments provided to nursing facility residents and orders on the physician orders for life-sustaining treatment form. J Am Geriatr Soc 2011; 59: 2091–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hammes BJ, Rooney BL, Gundrum JD, Hickman SE, Hager N. The POLST program: a retrospective review of the demographics of use and outcomes in one community where advance directives are prevalent. J Palliat Med 2012; 15: 77–85. [DOI] [PubMed] [Google Scholar]
- 38.Richardson DK, Fromme E, Zive D, Fu R, Newgard CD. Concordance of out-of-hospital and emergency department cardiac arrest resuscitation with documented end-of-life choices in Oregon. Ann Emerg Med2014; 63: 375–83. [DOI] [PubMed] [Google Scholar]
- 39.Lee MA, Brummel-Smith K, Meyer J, Drew N, London MR. Physician orders for life-sustaining treatment (POLST): outcomes in a PACE program. Program of all-inclusive care for the elderly. J Am Geriatr Soc 2000; 48: 1219–25. [DOI] [PubMed] [Google Scholar]
- 40.Curtis JR, Wenrich MD, Carline JD, Shannon SE, Ambrozy DM, Ramsey PG. Understanding physicians’ skills at providing end-of-life care perspectives of patients, families, and health care workers. J Gen Intern Med 2001; 16: 41–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wenrich MD, Curtis JR, Shannon SE, Carline JD, Ambrozy DM, Ramsey PG. Communicating with dying patients within the spectrum of medical care from terminal diagnosis to death. Arch Intern Med 2001; 161: 868–74. [DOI] [PubMed] [Google Scholar]
- 42.Wenrich MD, Curtis JR, Ambrozy DA, Carline JD, Shannon SE, Ramsey PG. Dying patients’ need for emotional support and personalized care from physicians: perspectives of patients with terminal illness, families, and health care providers. J Pain Symptom Manage 2003; 25: 236–46. [DOI] [PubMed] [Google Scholar]
- 43.Dow LA, Matsuyama RK, Ramakrishnan V, et al. Paradoxes in advance care planning: the complex relationship of oncology patients, their physicians, and advance medical directives. J Clin Oncol 2010; 28: 299–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bakitas M, Lyons KD, Hegel MT, et al. Effects of a palliative care intervention on clinical outcomes in patients with advanced cancer: the Project ENABLE II randomized controlled trial. JAMA 2009; 302: 741–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bakitas MA, Tosteson TD, Li Z, et al. Early versus delayed initiation of concurrent palliative oncology care: patient outcomes in the ENABLE III randomized controlled trial. J Clin Oncol 2015; 33: 1438–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Jang RW, Krzyzanowska MK, Zimmermann C, Taback N, Alibhai SM. Palliative care and the aggressiveness of end-of-life care in patients with advanced pancreatic cancer. J Natl Cancer Inst 2015; 107: dju424 [DOI] [PubMed] [Google Scholar]
- 47.Romano AM, Gade KE, Nielsen G, et al. Early palliative care reduces end-of-life intensive care unit (ICU) use but not ICU course in patients with advanced cancer. Oncologist 2017; 22: 318–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Tulsky JA, Chesney MA, Lo B. See one, do one, teach one? House staff experience discussing do-not-resuscitate orders. Arch Intern Med 1996; 156: 1285–89. [DOI] [PubMed] [Google Scholar]
- 49.Dickson RP, Engelberg RA, Back AL, Ford DW, Curtis JR. Internal medicine trainee self-assessments of end-of-life communication skills do not predict assessments of patients, families, or clinician-evaluators. J Palliat Med 2012; 15: 418–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Houben CHM, Spruit MA, Schols JMGA, Wouters EFM, Janssen DJA. Instability of willingness to accept life-sustaining treatments in patients with advanced chronic organ failure during 1 year. Chest 2017; 151: 1081–87. [DOI] [PubMed] [Google Scholar]
- 51.Janssen DJA, Spruit MA, Schols JMGA, et al. Predicting changes in preferences for life-sustaining treatment among patients with advanced chronic organ failure. Chest 2012; 141: 1251–59. [DOI] [PubMed] [Google Scholar]
- 52.Smith AK, Fisher J, Schonberg MA, et al. Am I doing the right thing? Provider perspectives on improving palliative care in the emergency department. Ann Emerg Med 2009; 54: 86–93, 93.e1. [DOI] [PubMed] [Google Scholar]
- 53.Grudzen CR, Richardson LD, Major-Monfried H, Kandarian B, Ortiz JM, Morrison RS. Hospital administrators’ views on barriers and opportunities to delivering palliative care in the emergency department. Ann Emerg Med 2013; 61: 654–60. [DOI] [PubMed] [Google Scholar]
- 54.Lamba S, Nagurka R, Zielinski A, Scott SR. Palliative care provision in the emergency department: barriers reported by emergency physicians. J Palliat Med 2013; 16: 143–47. [DOI] [PubMed] [Google Scholar]
- 55.Fassier T, Valour E, Colin C, Danet F. Who am I to decide whether this person is to die today? Physicians’ life-or-death decisions for elderly critically ill patients at the emergency department-ICU interface: a qualitative study. Ann Emerg Med 2016; 68: 28–39.e3. [DOI] [PubMed] [Google Scholar]
- 56.Argintaru N, Quinn KL, Chartier LB, et al. Perceived barriers and facilitators to goals of care discussions in the emergency department: A descriptive analysis of the views of emergency medicine physicians and residents. CJEM 2019; 21: 211–18. [DOI] [PubMed] [Google Scholar]
- 57.Cooper E, Hutchinson A, Sheikh Z, Taylor P, Townend W, Johnson MJ. Palliative care in the emergency department: a systematic literature qualitative review and thematic synthesis. Palliat Med 2018; 32: 1443–54. [DOI] [PubMed] [Google Scholar]
- 58.Le Conte P, Baron D, Trewick D, et al. Withholding and withdrawing life-support therapy in an emergency department: prospective survey. Intensive Care Med 2004; 30: 2216–21. [DOI] [PubMed] [Google Scholar]
- 59.Sedillot N, Holzapfel L, Jacquet-Francillon T, et al. A five-step protocol for withholding and withdrawing of life support in an emergency department: an observational study. Eur J Emerg Med 2008; 15: 14–5-49. [DOI] [PubMed] [Google Scholar]
- 60.Damghi N, Belayachi J, Aggoug B, et al. Withholding and withdrawing life-sustaining therapy in a Moroccan Emergency Department: an observational study. BMC Emerg Med 2011; 11: 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Richardson PG, Greenslade J, Isoardi J, et al. End-of-life issues: Withdrawal and withholding of life-sustaining healthcare in the emergency department: a comparison between emergency physicians and emergency registrars: a sub-study. Emerg Med Australas 2016; 28: 684–90. [DOI] [PubMed] [Google Scholar]
- 62.Grudzen CR, Richardson LD, Johnson PN, et al. Emergency department-initiated palliative care in advanced cancer: a randomized clinical trial. JAMA Oncol 2016; 2: 591–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Mahony SO, Blank A, Simpson J, et al. Preliminary report of a palliative care and case management project in an emergency department for chronically ill elderly patients. J Urban Health 2008; 85: 443–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Glajchen M, Lawson R, Homel P, Desandre P, Todd KH. A rapid two-stage screening protocol for palliative care in the emergency department: a quality improvement initiative. J Pain Symptom Manage 2011; 42: 657–62. [DOI] [PubMed] [Google Scholar]
- 65.Quest T, Herr S, Lamba S, Weissman D, and the IPAL-EM Advisory Board. Demonstrations of clinical initiatives to improve palliative care in the emergency department: a report from the IPAL-EM Initiative. Ann Emerg Med 2013; 61: 661–67 [DOI] [PubMed] [Google Scholar]
- 66.Wu FM, Newman JM, Lasher A, Brody AA. Effects of initiating palliative care consultation in the emergency department on inpatient length of stay. J Palliat Med 2013; 16: 1362–67. [DOI] [PubMed] [Google Scholar]
- 67.Ouchi K, Wu M, Medairos R, et al. Initiating palliative care consults for advanced dementia patients in the emergency department. J Palliat Med 2014; 17: 346–50. [DOI] [PubMed] [Google Scholar]
- 68.Grudzen C, Richardson LD, Baumlin KM, et al. Redesigned geriatric emergency care may have helped reduce admissions of older adults to intensive care units. Health Aff(Millwood) 2015; 34: 788–95. [DOI] [PubMed] [Google Scholar]
- 69.George N, Phillips E, Zaurova M, Song C, Lamba S, Grudzen C. Palliative care screening and assessment in the emergency department: a systematic review. J Pain Symptom Manage 2016; 51: 108–19.e2. [DOI] [PubMed] [Google Scholar]
- 70.Anderson WG, Chase R, Pantilat SZ, Tulsky JA, Auerbach AD. Code status discussions between attending hospitalist physicians and medical patients at hospital admission. J Gen Intern Med 2011; 26: 359–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Heyland DK, Barwich D, Pichora D, et al. Failure to engage hospitalized elderly patients and their families in advance care planning. JAMA Intern Med 2013; 173: 778–87. [DOI] [PubMed] [Google Scholar]
- 72.Cohen RI, Eichorn A, Motschwiller C, et al. Medical intensive care unit consults occurring within 48 hours of admission: a prospective study. J Crit Care 2015; 30: 363–68. [DOI] [PubMed] [Google Scholar]
- 73.Wong HJ, Wang J, Grinman M, Wu RC. Goals of care discussions among hospitalized long-term care residents: predictors and associated outcomes of care. J Hosp Med 2016; 11: 824–31. [DOI] [PubMed] [Google Scholar]
- 74.You JJ, Downar J, Fowler RA, et al. Barriers to goals of care discussions with seriously ill hospitalized patients and their families: a multicenter survey of clinicians. JAMA Intern Med 2015; 175: 549–56. [DOI] [PubMed] [Google Scholar]
- 75.Aleksova N, Demers C, Strachan PH, et al. Barriers to goals of care discussions with hospitalized patients with advanced heart failure: feasibility and performance of a novel questionnaire. ESC Heart Fail 2016; 3: 245–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Reilly BM, Wagner M, Magnussen CR, Ross J, Papa L, Ash J. Promoting inpatient directives about life-sustaining treatments in a community hospital. Results of a 3-year time-series intervention trial. Arch Intern Med 1995; 155: 2317–23. [PubMed] [Google Scholar]
- 77.Detering KM, Hancock AD, Reade MC, Silvester W. The impact of advance care planning on end of life care in elderly patients: randomised controlled trial. BMJ 2010; 340: c1345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Gade G, Venohr I, Conner D, et al. Impact of an inpatient palliative care team: a randomized control trial. J Palliat Med 2008; 11: 180–90. [DOI] [PubMed] [Google Scholar]
- 79.Penrod JD, Deb P, Luhrs C, et al. Cost and utilization outcomes of patients receiving hospital-based palliative care consultation. J Palliat Med 2006; 9: 855–60. [DOI] [PubMed] [Google Scholar]
- 80.Penrod JD, Deb P, Dellenbaugh C, et al. Hospital-based palliative care consultation: effects on hospital cost. J Palliat Med 2010; 13: 973–79. [DOI] [PubMed] [Google Scholar]
- 81.Rocque GB, Campbell TC, Johnson SK, et al. A quantitative study of triggered palliative care consultation for hospitalized patients with advanced cancer. J Pain Symptom Manage 2015; 50: 462–69. [DOI] [PubMed] [Google Scholar]
- 82.Hanson LC, Collichio F, Bernard SA, et al. Integrating palliative and oncology care for patients with advanced cancer: a quality improvement intervention. J Palliat Med 2017; 20: 1366–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Jones DA, McIntyre T, Baldwin I, Mercer I, Kattula A, Bellomo R. The medical emergency team and end-of-life care: a pilot study. Crit Care Resusc 2007; 9: 151–56. [PubMed] [Google Scholar]
- 84.Vazquez R, Gheorghe C, Grigoriyan A, Palvinskaya T, Amoateng-Adjepong Y, Manthous CA. Enhanced end-of-life care associated with deploying a rapid response team: a pilot study. J Hosp Med 2009; 4: 449–52. [DOI] [PubMed] [Google Scholar]
- 85.Jones DA, Bagshaw SM, Barrett J, et al. The role of the medical emergency team in end-of-life care: a multicenter, prospective, observational study. Crit Care Med 2012; 40: 98–103. [DOI] [PubMed] [Google Scholar]
- 86.Al-Qahtani S, Al-Dorzi HM, Tamim HM, et al. Impact of an intensivist-led multidisciplinary extended rapid response team on hospital-wide cardiopulmonary arrests and mortality. Crit Care Med 2013; 41: 506–17. [DOI] [PubMed] [Google Scholar]
- 87.Downar J, Rodin D, Barua R, et al. Rapid response teams, do not resuscitate orders, and potential opportunities to improve end-of-life care: a multicentre retrospective study. J Crit Care 2013; 28: 498–503. [DOI] [PubMed] [Google Scholar]
- 88.Jäderling G, Bell M, Martling CR, Ekbom A, Konrad D. Limitations of medical treatment among patients attended by the rapid response team. Acta Anaesthesiol Scand 2013; 57: 1268–74. [DOI] [PubMed] [Google Scholar]
- 89.Dargin JM, Mackey CG, Lei Y, Liesching TN. Resource utilization and end-of-life care in a US hospital following medical emergency team-implemented do not resuscitate orders. J Hosp Med 2014; 9: 372–78. [DOI] [PubMed] [Google Scholar]
- 90.Orosz J, Bailey M, Bohensky M, Gold M, Zalstein S, Pilcher D. Deteriorating patients managed with end-of-life care following Medical Emergency Team calls. Intern Med J 2014; 44: 246–54. [DOI] [PubMed] [Google Scholar]
- 91.Smith RL, Hayashi VN, Lee YI, Navarro-Mariazeta L, Felner K. The medical emergency team call: a sentinel event that triggers goals of care discussion. Crit Care Med 2014; 42: 322–27. [DOI] [PubMed] [Google Scholar]
- 92.Tan LH, Delaney A. Medical emergency teams and end-of-life care: a systematic review. Crit Care Resusc 2014; 16: 62–68. [PubMed] [Google Scholar]
- 93.Sulistio M, Franco M, Vo A, Poon P, William L. Hospital rapid response team and patients with life-limiting illness: a multicentre retrospective cohort study. Palliat Med 2015; 29: 302–09. [DOI] [PubMed] [Google Scholar]
- 94.Tirkkonen J, Olkkola KT, Tenhunen J, Hoppu S. Ethically justified treatment limitations in emergency situations. Eur J Emerg Med 2016; 23: 214–18. [DOI] [PubMed] [Google Scholar]
- 95.Downar J, Barua R, Rodin D, et al. Changes in end of life care 5 years after the introduction of a rapid response team: a multicentre retrospective study. Resuscitation 2013; 84: 1339–44. [DOI] [PubMed] [Google Scholar]
- 96.Childers JW, Arnold RM. expanding goals of care conversations across a health system: the mapping the future program. J Pain Symptom Manage 2018; 56: 637–44. [DOI] [PubMed] [Google Scholar]
- 97.Lupu D, and the American Academy of Hospice and Palliative Medicine Workforce Task Force. Estimate of current hospice and palliative medicine physician workforce shortage. J Pain Symptom Manage 2010; 40: 899–911. [DOI] [PubMed] [Google Scholar]
- 98.Angus DC, Truog RD. Toward better ICU use at the end of life. JAMA 2016; 315: 255–56. [DOI] [PubMed] [Google Scholar]
- 99.Bosslet GT, Pope TM, Rubenfeld GD, et al. An official ATS/AACN/ACCP/ESICM/SCCM policy statement: responding to requests for potentially inappropriate treatments in intensive care units. Am J Respir Crit Care Med 2015; 191: 1318–30. [DOI] [PubMed] [Google Scholar]
- 100.Curtis JR, Burt RA. Point: the ethics of unilateral “do not resuscitate” orders: the role of “informed assent”. Chest 2007; 132: 748–51, discussion 755–56. [DOI] [PubMed] [Google Scholar]
- 101.Kon AA, Davidson JE, Morrison W, Danis M, White DB, and the American College of Critical Care Medicine, and the American Thoracic Society. Shared decision making in ICUs: an American College of Critical Care Medicine and American Thoracic Society Policy Statement. Crit Care Med 2016; 44: 188–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Heyland DK, Cook DJ, Rocker GM, et al. Decision-making in the ICU: perspectives of the substitute decision-maker. Intensive Care Med 2003; 29: 75–82. [DOI] [PubMed] [Google Scholar]
- 103.Azoulay E, Pochard F, Chevret S, et al. Half the family members of intensive care unit patients do not want to share in the decision-making process: a study in 78 French intensive care units. Crit Care Med 2004; 32: 1832–38. [DOI] [PubMed] [Google Scholar]
- 104.Botti S, Orfali K, Iyengar SS. Tragic choices: autonomy and emotional responses to medical decisions. J Consum Res 2009; 36: 337–52. [Google Scholar]
- 105.Gries CJ, Curtis JR, Wall RJ, Engelberg RA. Family member satisfaction with end-of-life decision making in the ICU. Chest 2008; 133: 70–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Curtis JR, White DB. Practical guidance for evidence-based ICU family conferences. Chest 2008; 134: 835–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Curtis JR, Vincent JL. Ethics and end-of-life care for adults in the intensive care unit. Lancet 2010; 376: 1347–53. [DOI] [PubMed] [Google Scholar]
- 108.Sanders JJ, Curtis JR, Tulsky JA. Achieving goal-concordant care: a conceptual model and approach to measuring serious illness communication and its impact. J Palliat Med 2018; 21: S17–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Curtis JR, Downey L, Back AL, et al. Effect of a patient and clinician communication-priming intervention on patient-reported goals-of-care discussions between patients with serious illness and clinicians: a randomized clinical trial. JAMA Intern Med 2018; 178: 930–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Turnbull AE, Sahetya SK, Colantuoni E, Kweku J, Nikooie R, Curtis JR. Inter-rater agreement of intensivists evaluating the goal concordance of preference-sensitive ICU interventions. J Pain Symptom Manage 2018; 56: 406–413.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Sudore RL, Schillinger D, Katen MT, et al. Engaging diverse English-and Spanish-speaking older adults in advance care planning: the PREPARE randomized clinical trial. JAMA Intern Med 2018; 178: 1616–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Sudore RL, Boscardin J, Feuz MA, McMahan RD, Katen MT, Barnes DE. Effect of the PREPARE website vs an easy-to-read advance directive on advance care planning documentation and engagement among veterans: a randomized clinical trial. JAMA Intern Med 2017; 177: 1102–09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Mitchell SL, Shaffer ML, Cohen S, Hanson LC, Habtemariam D, Volandes AE. An advance care planning video decision support tool for nursing home residents with advanced dementia: a cluster randomized clinical trial. JAMA Intern Med 2018; 178: 961–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.El-Jawahri A, Paasche-Orlow MK, Matlock D, et al. Randomized, controlled trial of an advance care planning video decision support tool for patients with advanced heart failure. Circulation 2016; 134: 52–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Courtright KR, Cassel JB, Halpern SD. A research agenda for high-value palliative care. Ann Intern Med 2018; 168: 71–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Osman H, Shrestha S, Temin S, et al. Palliative care in the global setting: ASCO resource-stratified practice guideline. J Glob Oncol 2018; 4: 1–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Cox CE, Curtis JR. Using technology to create a more humanistic approach to integrating palliative care into the intensive care unit. Am J Respir Crit Care Med 2016; 193: 242–50. [DOI] [PubMed] [Google Scholar]
- 118.Emanuel LL, Alpert HR, Emanuel EE. Concise screening questions for clinical assessments of terminal care: the needs near the end-of-life care screening tool. J Palliat Med 2001; 4: 465–74. [DOI] [PubMed] [Google Scholar]
- 119.Richards CT, Gisondi MA, Chang CH, et al. Palliative care symptom assessment for patients with cancer in the emergency department: validation of the Screen for Palliative and End-of-life care needs in the Emergency Department instrument. J Palliat Med 2011; 14: 757–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Sudore RL, Lum HD, You JJ, et al. Defining advance care planning for adults: a consensus definition from a multidisciplinary delphi panel. J Pain Symptom Manage 2017; 53: 821–832. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


