Abstract
There is evidence that the potential for high concentration oxygen therapy to increase PaCO2 is not limited to stable and acute exacerbations of COPD, but also to other acute respiratory disorders with abnormal gas exchange such as asthma and pneumonia, and chronic respiratory conditions with hypercapnia such as obesity hypoventilation syndrome. This evidence forms the basis of consensus guidelines which recommend that oxygen therapy is titrated in COPD and other respiratory conditions, to ensure the maximal benefits of oxygen therapy are achieved while reducing the potential for harm due to hyperoxia.
Electronic supplementary material
The online version of this article (doi:10.1186/2213-0802-1-8) contains supplementary material, which is available to authorized users.
Introduction
The risks associated with high concentration oxygen therapy in acute exacerbations of chronic obstructive pulmonary disease (COPD) were reported over 50 years ago [1]. Since then it has been demonstrated that high concentration oxygen therapy can cause an increase in PaCO2 in both stable COPD and exacerbations of COPD, and that in some patients the effect can be both rapid and marked with an increase in PaCO2 of >20 mmHg within 60 minutes [2]. The clinical significance of this effect is evident from the recent randomised controlled trial (RCT) which demonstrated that in acute exacerbations of COPD, high concentration oxygen therapy in the pre-hospital setting significantly increases mortality compared with a titrated regimen to achieve arterial oxygen saturations between 88% and 92% [3]. In patients with confirmed COPD who received oxygen therapy treatments as per protocol, the PaCO2 was 34 mmHg higher in the high concentration oxygen therapy group (Table 1).
Table 1.
High concentration versus titrated oxygen therapy in the pre-hospital setting in patients with confirmed COPD
| High concentration | Titrated | Relative risk (95% CI) | Difference | P Value | |
|---|---|---|---|---|---|
| Mortality | 9% | 2% | 0.22 (0.5 to 0.91) | 0.04 | |
| Ventilation | 14% | 10% | 0.67 (0.29 to 1.54) | 0.34 | |
| Arterial blood gases† | |||||
| Mean (SD) pH | 7.29 (0.15) | 7.41 (0.09) | 0.12 | 0.01 | |
| Mean (SD) PaCO2 (mmHg) | 76.5 (50.2) | 42.9 (14.2) | −33.6 | 0.02 | |
| Mean (SD) PaO2 (mmHg) | 98.4 (46.1) | 81.5 (30.9) | −16.9 | 0.46 |
† Treatment per protocol analysis.
Reproduced with modification from reference [3].
The main mechanisms responsible for the increase in PaCO2 with high concentration oxygen therapy are a reduction in respiratory drive and worsening ventilation/perfusion mismatch due to release of hypoxic pulmonary vasoconstriction [2, 4–7]. Ventilation-perfusion mismatch is also a predominant gas exchange abnormality in other acute respiratory disorders such as asthma and pneumonia, with the degree of mismatch worsening with the administration of oxygen [8–14]. As a result it would be expected that high concentration oxygen therapy would cause an increase in PaCO2 in severe asthma and pneumonia, similar to its administration in acute exacerbations of COPD.
Recently a series of RCTs has demonstrated that high concentration oxygen treatment results in a significant increase in PaCO2 or transcutaneous carbon dioxide tension (PtCO2) in patients presenting with severe exacerbations of asthma [15–17]. The clinical significance of this physiological effect is suggested by the observation that 10% of patients randomised to high concentration oxygen therapy had an increase in PtCO2 of ≥10 mmHg and a PtCO2 ≥45 mmHg after 60 minutes of treatment, whereas no patients receiving titrated oxygen therapy to maintain the arterial oxygen saturations between 93 and 95% had this response (Figure 1) [15]. In a similar RCT, high concentration oxygen therapy was also shown to increase the PtCO2 in patients presenting with community-acquired pneumonia when compared with the titrated oxygen regimen which avoided both hypoxia and hyperoxia [18]. The three- and six-fold relative risks of an increase in PtCO2 of at least 4 mmHg and at least 8 mmHg respectively, suggest that this effect may potentially be of both physiological and clinical significance (Table 2).
Figure 1.
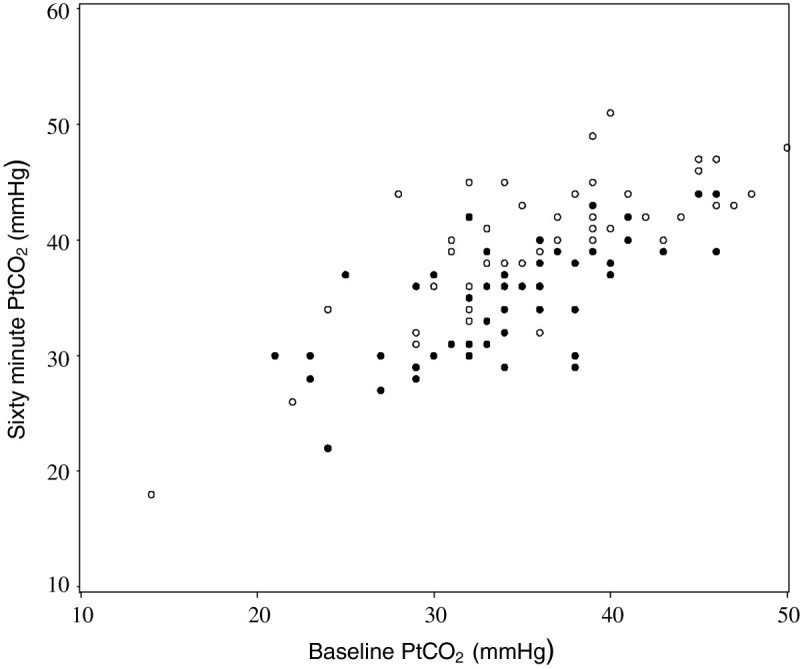
The transcutaneous partial pressure of carbon dioxide (PtCO 2 ) levels at baseline and after 60 min of high concentration (open circles) or titrated (filled circles) oxygen in patients presenting to the Emergency Department with a severe exacerbation of asthma. Reproduced from reference [15].
Table 2.
The proportion of patients with community-acquired pneumonia with a rise in PtCO 2 from baseline after 60 minutes of high concentration or titrated oxygen therapy
| High concentration | Titrated | Relative risk | P value | |
|---|---|---|---|---|
| n (%) | n (%) | (95% CI) | ||
| Change in PtCO2 ≥4 mmHg | 36 (50%) | 11 (14.7%) | 3.4 (1.9 to 6.2) | <0.001 |
| Change in PtCO2 ≥8 mmHg | 11 (15.3%) | 2 (2.7%) | 5.7 (1.3 to 25.0) | 0.007 |
Reproduced with modification from reference [18].
Chronic respiratory failure may also occur in other chronic respiratory disorders such as obesity hypoventilation syndrome [19], so it might be expected that high concentration oxygen therapy could cause CO2 retention in this condition, similar to stable COPD. This physiological effect has recently been demonstrated in a randomised placebo-controlled trial of 100% oxygen and room air in patients with obesity hypoventilation syndrome and baseline hypercapnia (Figure 2) [20]. The main mechanism responsible for the worsening hypercapnia when breathing 100% oxygen was a reduction in minute ventilation, leading to alveolar hypoventilation. The clinical significance of this physiological effect was suggested by the requirement to terminate the study in one in eight of the patients studied, due to an increase in PtCO2 ≥10 mmHg within 20 minutes of receiving 100% oxygen therapy.
Figure 2.
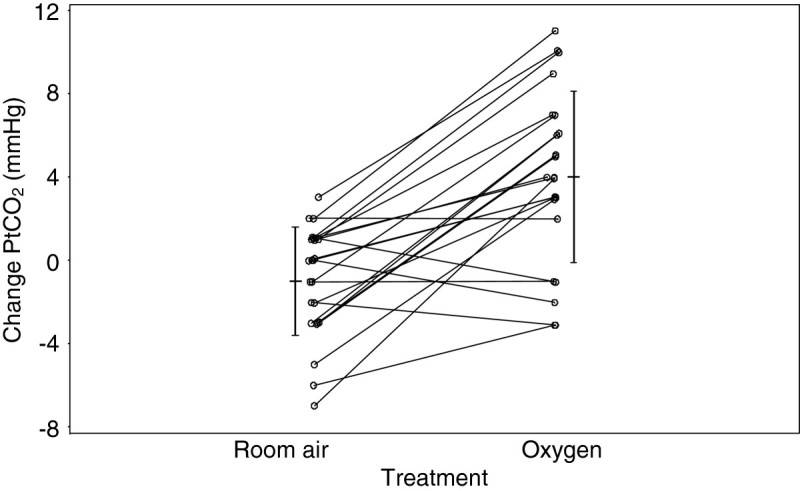
The change in PtCO 2 (mmHg) from baseline following breathing 100% oxygen or room air in subjects with obesity hypoventilation syndrome. The vertical lines are the mean (central horizontal line) ±1 SD for 20 min PtCO2 minus baseline. Reproduced from reference [20].
Thus there is evidence that the potential for high concentration oxygen therapy to increase PaCO2 is not limited to stable and acute exacerbations of COPD, but also to other acute respiratory disorders with abnormal gas exchange such as asthma and pneumonia, and chronic respiratory conditions with hypercapnia such as obesity hypoventilation syndrome. This evidence forms the basis of consensus guidelines [21] which recommend that oxygen therapy is titrated in COPD and other respiratory conditions, to ensure the maximal benefits of oxygen therapy are achieved while reducing the potential for harm due to hyperoxia.
Acknowledgements
JP is a Health Research Council of New Zealand Clinical Research Training Fellow.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Footnotes
Competing interests
The authors declare that they have no competing interests.
Authors’ contribution
JP, KP and RB all contributed to the drafting of this manuscript. All authors read and approved the final manuscript.
Contributor Information
Janine Pilcher, Email: Janine.pilcher@mrinz.ac.nz.
Kyle Perrin, Email: Kyle.Perrin@mrinz.ac.nz.
Richard Beasley, Email: Richard.Beasley@mrinz.ac.nz.
References
- 1.Campbell EJ. Respiratory failure: the relation between oxygen concentrations of inspired air and arterial blood. Lancet. 1960;2:10–11. doi: 10.1016/S0140-6736(60)92659-3. [DOI] [PubMed] [Google Scholar]
- 2.Murphy R, Driscoll P, O'Driscoll R. Emergency oxygen therapy for the COPD patient. Emerg Med J. 2001;18:333–339. doi: 10.1136/emj.18.5.333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Austin MA, Wills KE, Blizzard L, Walters EH, Wood-Baker R. Effect of high flow oxygen on mortality in chronic obstructive pulmonary disease patients in prehospital setting: randomised controlled trial. BMJ. 2010;341:c5462. doi: 10.1136/bmj.c5462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Aubier M, Murciano D, Milic-Emili J, Touaty E, Daghfous J, Pariente R, Derenne J-P. Effects of the administration of O2 on ventilation and blood gases in patients with chronic obstructive pulmonary disease during acute respiratory failure. Am Rev Respir Dis. 1980;122:747–754. doi: 10.1164/arrd.1980.122.5.747. [DOI] [PubMed] [Google Scholar]
- 5.Dick C, Liu Z, Sassoon C, Berry RB, Mahutte CK. O2-induced change in ventilation and ventilatory drive in COPD. Am J Respir Crit Care Med. 1997;155:609–614. doi: 10.1164/ajrccm.155.2.9032202. [DOI] [PubMed] [Google Scholar]
- 6.Robinson TD, Freiberg DB, Regnis JA, Young IH. The role of hypoventilation and ventilation-perfusion redistribution in oxygen-induced hypercapnia during acute exacerbations of chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2000;161:1524–1529. doi: 10.1164/ajrccm.161.5.9904119. [DOI] [PubMed] [Google Scholar]
- 7.Sassoon CS, Hassell KT, Mahutte CK. Hyperoxic-induced hypercapnia in stable chronic obstructive pulmonary disease. Am Rev Respir Dis. 1987;135:907–911. doi: 10.1164/arrd.1987.135.4.907. [DOI] [PubMed] [Google Scholar]
- 8.Ballester E, Reyes A, Roca J, Guitart R, Wagner PD, Rodriguez-Roisin R. Ventilation-perfusion mismatching in acute severe asthma: effects of salbutamol and 100% oxygen. Thorax. 1989;44:258–267. doi: 10.1136/thx.44.4.258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Corte P, Young IH. Ventilation-perfusion relationships in symptomatic asthma. Response to oxygen and clemastine. Chest. 1985;88:167–175. doi: 10.1378/chest.88.2.167. [DOI] [PubMed] [Google Scholar]
- 10.Field GB. The effects of posture, oxygen, isoproterenol and atropine on ventilation-perfusion relationships in the lung in asthma. Clin Sci. 1967;32:279–288. [PubMed] [Google Scholar]
- 11.Rodriguez-Roisin R, Ballester E, Roca J, Torres A, Wagner PD. Mechanisms of hypoxemia in patients with status asthmaticus requiring mechanical ventilation. Am Rev Respir Dis. 1989;139:732–739. doi: 10.1164/ajrccm/139.3.732. [DOI] [PubMed] [Google Scholar]
- 12.Gea J, Roca J, Torres A, Agusti AG, Wagner PD, Rodriguez-Roisin R. Mechanisms of abnormal gas exchange in patients with pneumonia. Anesthesiology. 1991;75:782–789. doi: 10.1097/00000542-199111000-00009. [DOI] [PubMed] [Google Scholar]
- 13.Light RB. Pulmonary pathophysiology of pneumococcal pneumonia. Semin Respir Infect. 1999;14:218–226. [PubMed] [Google Scholar]
- 14.Rodriguez-Roisin R, Roca J. Update ’96 on pulmonary gas exchange pathophysiology in pneumonia. Semin Respir Infect. 1996;11:3–12. [PubMed] [Google Scholar]
- 15.Perrin K, Wijesinghe M, Healy B, Wadsworth K, Bowditch R, Bibby S, Baker T, Weatherall M, Beasley R. Randomised controlled trial of high concentration versus titrated oxygen therapy in severe exacerbations of asthma. Thorax. 2011;66:937–941. doi: 10.1136/thx.2010.155259. [DOI] [PubMed] [Google Scholar]
- 16.Chien JW, Ciufo R, Novak R, Skowronski M, Nelson J, Coreno A, McFadden ER., Jr Uncontrolled oxygen administration and respiratory failure in acute asthma. Chest. 2000;117:728e33. doi: 10.1378/chest.117.3.728. [DOI] [PubMed] [Google Scholar]
- 17.Rodrigo GJ, Rodriquez Verde M, Peregalli V, Rodrigo C. Effects of short-term 28% and 100% oxygen on PaCO2 and peak expiratory flow rate in acute asthma: a randomized trial. Chest. 2003;124:1312e17. doi: 10.1378/chest.124.4.1312. [DOI] [PubMed] [Google Scholar]
- 18.Wijesinghe M, Perrin K, Healy B, Weatherall M, Beasley R. Randomized controlled trial of high concentration oxygen in suspected community-acquired pneumonia. J R Soc Med. 2012;105:208–216. doi: 10.1258/jrsm.2012.110084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nowbar S, Burkart KM, Gonzales R, Fedorowicz A, Gozansky WS, Gaudio JC, Taylor MR, Zwillich CW. Obesity-associated hypoventilation in hospitalized patients: prevalence, effects, and outcome. Am J Med. 2004;116:1–7. doi: 10.1016/j.amjmed.2003.08.022. [DOI] [PubMed] [Google Scholar]
- 20.Wijesinghe M, Williams M, Perrin K, Weatherall M, Beasley R. The effect of supplemental oxygen on hypercapnia in subjects with obesity-associated hypoventilation: a randomized, crossover clinical study. Chest. 2011;139:1018–1024. doi: 10.1378/chest.10-1280. [DOI] [PubMed] [Google Scholar]
- 21.O’Driscoll BR, Howard LS, Davison AG. British Thoracic Society guideline for emergency oxygen use in adult patients. Thorax. 2008;63(Suppl 6):vi1–68. doi: 10.1136/thx.2008.102947. [DOI] [PubMed] [Google Scholar]


