Abstract
Objective:
South Africa has the highest prevalence of HIV among women, the highest prevalence of gender-based violence (GBV), and the highest rates of per capita alcohol consumption in the world. Therefore, it is imperative to explore the nuanced associations between GBV, alcohol misuse, and HIV and identify protective factors. This study examines the associations between physical and sexual GBV and incident HIV infection and explores how alcohol misuse and sexual agency may act as mediators of the GBV-HIV association.
Method:
Participants were 361 Black African women (Mean age = 28.39, SD = 7.92) who reported using alcohol and/or drugs weekly for the past 3 months, engaging in condomless sex, and having a boyfriend. Women were recruited from disadvantaged communities in Pretoria, South Africa. Individuals who met the eligibility criteria and enrolled in the study provided consent and completed a computer-assisted personal interview assessing GBV, alcohol misuse, and sexual agency and underwent HIV testing (i.e., blood test).
Results:
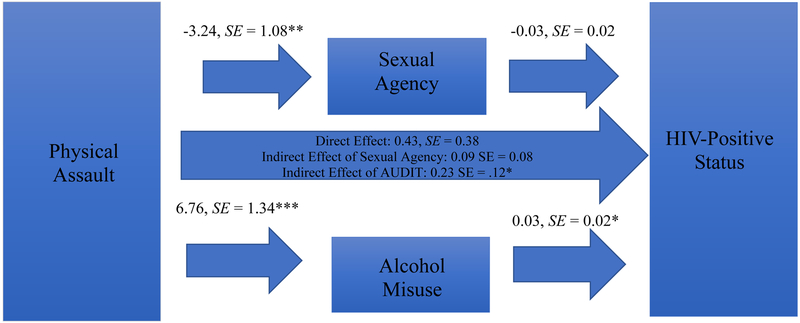
Analyses indicated that the indirect effect of physical assault on HIV status at enrollment through alcohol misuse was significant (log odds = 0.23, SE = 0.12, [95% CI: 0.0151, 0.4998]).
Conclusions:
By focusing on reducing alcohol misuse, HIV prevention efforts may be more effective; which, in turn, may reduce the HIV burden among this group of vulnerable women in South Africa.
Keywords: alcohol abuse, sexual negotiation, empowerment, protective factors, women, HIV, South Africa
Approximately 20% of women of reproductive age (15–49 years) are living with HIV in South Africa (Statistics South Africa, 2018) – with Black African women representing the highest proportion of those living with HIV (Human Sciences Research Council (HSRC), 2018). Furthermore, South Africa has one of the highest prevalences of gender-based violence (GBV) and rates of per capita alcohol consumption in the world (Johnson, Coetzee, & Dorrington, 2005; Parry, Rehm, & Morojele, 2010). In some provinces, 51% of women report experiencing GBV (Machisa, 2011). Among South African women who drink alcohol, 17% report hazardous drinking (Peltzer, Davids, & Njuho, 2011). Both GBV and alcohol misuse (e.g., being unable to stop drinking once one has started) are contributors to HIV risk in South Africa. For example, in Gauteng province, 11% of women who were experienced physical or sexual intimate partner violence (IPV) tested positive for HIV (Machisa, 2011). Approximately 7,000 incident HIV cases among women can be attributable to alcohol use in South Africa (Rehm, Probst, Shield, & Shuper, 2017). Alcohol misuse and GBV often co-occur, exacerbating the risk of HIV – especially for women (Pitpitan et al., 2013). Therefore, research is needed to understand the nuanced associations between GBV, alcohol misuse, and HIV.
Gender-based violence, especially IPV, has been linked to an increased likelihood of HIV among women (Dunkle et al., 2004; Dunkle and Decker, 2013; Jewkes, Dunkle, Nduna, & Shai, 2010). Researchers have also developed a framework to understand the association between GBV and HIV (Dunkle and Decker, 2013). This framework posits that GBV and HIV can be either (1) directly related through sexual violence or (2) indirectly through the psychosocial factors that are impacted by GBV. The framework provides a foundation to examine the impact of how different forms of GBV may impact HIV and to identify how factors such as alcohol misuse may impact this association.
The link between alcohol misuse and GBV as well as HIV risk has been demonstrated among women (Pitpitan, et al., 2013). Furthermore, women who engage in alcohol misuse are about 79% more likely to be living with HIV than those who do not. This may be attributable to the fact that alcohol misuse, especially in the context of drinking establishments in South Africa called shebeens, is related to engaging in condomless sex and transactional sex as well as experiencing coercive sex (Bello et al., 2017; Fisher, Cook, & Kapiga, 2010; Fisher, Cook, Sam, & Kapiga, 2008; Scott-Sheldon et al., 2012; Watt et al., 2012; Watt et al., 2014). Thus, many women who experienced GBV are at risk of engaging in alcohol misuse, which may increase sexual risk and risk of HIV infection.
Given the association between GBV, alcohol misuse and HIV risk, it is imperative to identify potential protective factors that may mitigate the effects of this syndemic. One such factor may be sexual agency, or the ability to recognize, accept, and respond to one’s own sexual feelings, including the ability to refuse unwanted sex (Pearson, 2008). Sexual agency is tied to gender norms. Rigid gender norms that prescribe that women should be sexually submissive (Pearson, 2008; Strebel et al., 2006) may impair women’s ability to exercise sexual agency and increases their risk of HIV (Jewkes and Morrell, 2010). Furthermore, the impact of rigid gender norms may be exacerbated by GBV, whereby women may fear violence as a consequence of exercising their sexual agency (Onu et al., 2017; Peasant, Parra, & Okwumabua, 2015). Therefore, limited sexual agency can increase HIV risk (Jewkes and Morrell, 2012). Conversely, bolstered sexual agency may act as a protective factor to reduce HIV risk.
Research outlining the pathways from GBV to HIV is evidence-based (Dunkle and Decker, 2013). However, it is still unclear how the type of GBV women experience influences their likelihood of acquiring HIV and how these associations may be differentially impacted by alcohol misuse and sexual agency. This study examines the associations between physical and sexual GBV and incident HIV infection among women who use substances in Pretoria, South Africa. We also examine how alcohol misuse and sexual agency may mediate the GBV-HIV association. We hypothesize that physical and sexual GBV are directly related to HIV and that these mediated by sexual agency and alcohol misuse.
Method
Setting and Study Sample
Data for this secondary analysis were taken from a larger study that evaluated the efficacy of an HIV prevention intervention among women who used substances (Wechsberg et al., 2019; Wechsberg et al., 2014). Women from 14 disadvantaged communities in Pretoria, South Africa, were recruited through community-based outreach efforts. To be included in the study, participants had to be Black African women aged 15 or older (with no maximum age cutoff; if 15 to 17, with evidence of tacit emancipation, defined as living away from parents and earning their own income (Republic of South Africa, 2004); had to have used at least one substance (which could be alcohol) weekly for the past 3 months; had to have engaged in condomless sex with a male in the past 6 months; had to speak either English, Sesotho, isiZulu/Xhosa, or Setswana; had to provide informed consent to participate in the study; and had to plan to remain in Pretoria for at least a year. This study began before the National Health Act No 61, 2003 was fully implemented. Therefore, adolescents under the age of 18 could consent to research participation.
A total of 641 women were enrolled in the larger study. This baseline analysis focused on 361 women who reported they had a boyfriend (a man that they were in a relationship with, which could include their husband or spouse) at study enrollment, had complete data for the variables of interest, and either tested negative for HIV or were newly diagnosed as HIV positive at enrollment. While this study focuses on women who had a boyfriend, many women reported having other partners.
Procedure
Women were recruited and screened in communities that had been mapped based on socioeconomic conditions and estimates of alcohol and other drug use and sex work (Wechsberg et al., 2008; Wechsberg, Luseno, Kline, Browne, & Zule, 2010). Those who were eligible and interested in participating in the study were given an intake appointment. At the intake appointment, women were rescreened and asked to provide informed consent, complete a computer-assisted personal interview (CAPI), and underwent biological screening for drugs (panel drug urine screen), alcohol (alcohol breath scan), pregnancy (urine test), and HIV testing and pre-and post-test counseling (blood test). Women who were newly diagnosed with HIV at enrollment were informed of their status and referred for medical care. Additionally, women were offered referrals to substance abuse treatment and other social services.
Participants were provided with refreshments and 100 Rand (approximately 10 USD) for their time. Ethical approval for the study was granted by the South African Medical Association Research Ethics Committee (SAMAREC), Tshwane Research Committee (TRC), and the RTI International Committee for the Protection of Human Subjects. Additionally, this study established a Data and Safety Monitoring Board (DSMB).
Measures
Gender-based violence.
Participants’ experiences of physical GBV in the past year were assessed by using two items. First, participants were asked if anyone had ever physically hurt them (i.e., “struck or beat you to the point that you had bruises, cuts, or broken bones”). Those who reported that they had been physically hurt in their lifetime were asked: “When was the last time you were physically hurt?” Responses were coded as either 1 = Physical assault in the past 12 months or 0 = No physical assault in the past 12 months. Participants’ experiences of sexual assault in the past 12 months were assessed using an identical approach.
Alcohol misuse.
Participants reported the extent to which they experienced problems related to alcohol use in the past year using the 10-item Alcohol Use Disorders Identification Test (AUDIT; (Babor, Biddle-Higgins, Saunders, & Monteiro, 2001). Participants responded to items that were scored 0 to 4. Responses were summed, with higher scores indicating more alcohol misuse. Reliability for the AUDIT among this sample was 0.82.
Perceived sexual agency.
Participants’ sexual agency was measured by their perceived ability to refuse unwanted sex with their boyfriend. Six items were developed and validated by the research team. An example item was “Sometimes you have sex with your boyfriend even when you do not want to because it is expected of you”. Responses were given on a Likert scale, with 1= Strongly Agree to 5 = Strong Disagree. Responses were summed, with higher scores indicating greater perceived sexual agency. Reliability for this measure was 0.90.
HIV status.
A blood sample from a finger prick was collected to screen for HIV. Testing was done using two parallel rapid HIV tests: (1) First Response® HIV 1–2.0 or ABON®-Alere HIV 1/2/O Tri-line HIV Rapid Test and (2) iCARE One Step HIV [1&2] Whole Blood/Serum/Plasma Test. A third test (Alere Determine™ HIV-1/2) was performed if the two tests were discordant. A participant was classified as being HIV-positive if two tests were reactive. If participants reported that they did not know their status before being tested at enrollment and they tested positive at enrollment, then they were considered newly diagnosed with HIV. Only women who were HIV-negative (coded as 0) or newly diagnosed at intake (coded as 1) were included in this report to make stronger inferences about the temporality of the associations between variables.
Covariates
Age.
Participants’ age was explored as a possible covariate given the positive association between age and HIV status.
Condom use.
We assessed the number of acts of condomless vaginal sex with a boyfriend in the past month. We also measured the number of acts of condomless vaginal sex with other partners in the past month.
Number of partners.
We assessed the number of partners that participants had engaged in sex in the past month. Participants who reported that they only had sex with a boyfriend were coded as having 1 partner in the past month. Those who reported that they only had sex with other partners (not a boyfriend) were asked how many other partners they had sex within the past month. Those who reported having sex with a boyfriend and other partners were coded as having 1+ n (the number of other partners) in the past month.
Sex work.
Participants’ engagement in sex work in the past 6 months was assessed. Responses were either coded as 1 = Engaged in sex work in the past 6 months or 0 = Had not engaged in sex work in the past 6 months.
Analytic Approach
Analyses were conducted using SPSS 23 (IBM, 2017). Descriptive analyses were performed, assumptions were examined, and the association between covariates and variables of interests were explored. Next, bivariate analyses were conducted to assess the associations among physical assault in the past year, sexual assault in the past year, AUDIT scores, perceived sexual agency, and HIV status at enrollment. Based on bivariate analyses, mediation models were conducted to examine if there was an indirect effect of physical assault and/or sexual assault in the past year on HIV status through perceived sexual agency and alcohol misuse. The models were conducted based on the PROCESS procedures, which used the logit function and bootstrapping methods to estimate the direct and indirect effects of the hypothesized associations (Hayes, 2012). A bootstrapping sample of 5,000 was used to estimate the standard errors of parameter estimates and the bias-corrected 95% confidence intervals of the indirect effects. Confidence intervals that did not contain zero indicated a statistically significant effect.
Results
Description of Sample
The mean age of participants was 28.39 (SD = 7.92; range = 16–58 years). Approximately 30% of the women were newly diagnosed with HIV at enrollment. Also, participants had a mean AUDIT score of 15.29 (SD = 7.92; range = 0 to 40), and a mean perceived sexual agency score of 20.93 (SD = 6.21; range = 6– 30; see Table 1).
Table 1.
Characteristics of study sample (N = 361)
| Variable | Total |
|---|---|
| Age | |
| 16 – 24 years of age | 131 (36.29%) |
| 25 – 58 years of age | 230 (63.71%) |
| Homeless | 90 (24.93%) |
| Unemployed | 322 (89.20%) |
| Highest level of education completed | |
| Standard 6 (Grade 8) or Less | 87 (24.10%) |
| Standard 7 to 10 (Grade 9 to 12) | 255 (70.64%) |
| Passed matric or higher (high school or higher) | 19 (5.26%) |
| Run out of money for necessities at least monthly | 150 (41.55%) |
| Engaged in sex work in the past 6 months | 110 (30.47%) |
| Newly diagnosed with HIV at enrollment | 108 (29.92%) |
| Perceived sexual agency score, mean (SD; range = 6 – 30) | 20.93 (6.21) |
| Number of condomless vaginal sex acts with boyfriend in the past month (SD; range = 0 – 60) | 9.21 (10.47) |
| Number of condomless vaginal sex acts with other partners in the past month (SD; range = 0 – 121) | 9.43 (12.64) |
| Number of sexual partners in the past month (SD; 0 – 21) | 1.57 (1.50) |
| Hazardous drinking as measured by the AUDIT (score ≥ 20) | 108 (29.92%) |
| Physical assault in the past year | 36 (9.97%) |
| Sexual assault in the past year | 23 (6.37%) |
Note. AUDIT = Alcohol Use Disorders Identification Test
Bivariate Analysis
Bivariate logistic regression revealed that physical assault in the past year (OR = 2.30, SE = 0. 82, p = 0.02, [95% CI: 1.1452, 4.6225], AUDIT scores (OR = 1.04, SE = 0.02, p = 0.01, [95% CI: 1.0111, 1.0723], and perceived sexual agency (OR = 0.96, SE = 0.18, p = 0.03, [95% CI: 0.9269, 0.9964] were significantly related to HIV status at enrollment. However, sexual assault in the past year was not significantly related to HIV status at enrollment (OR = 2.26, SE = 0.99, p = 0.06, [95% CI: 0.9721, 5.3361].
Primary Analysis
Based on bivariate analysis, only one mediation model was conducted to determine whether perceived sexual agency and alcohol misuse mediated the association between physical assault in the past year and HIV status at enrollment. Sex worker status and age were entered in the model as covariates. The direct effect of physical assault on a HIV status at enrollment was not significant (log odds = 0.43, SE = 0.38, p = 0.26, [95% CI: −0.3169, 1.1849]). The indirect effect of physical assault on HIV status at enrollment through perceived sexual agency was not significant (log odds = 0.09, SE = 0.08, [95% CI: −0.0293, 0.2809]). However, the indirect effect of physical assault on HIV status at enrollment through alcohol misuse was significant (log odds = 0.23, SE = 0.12, [95% CI: 0.0151, 0.4998]; see Figure 1). Consequently, there was an indirect effect of physical assault on HIV status at enrollment through alcohol misuse, but not perceived sexual agency.
Figure 1.
Log odds coefficients for the indirect effect of sexual agency and alcohol misuse on the relationship between physically assault and biologically confirmed HIV status, controlling for sex worker status and age (n = 361). *p < .05, **p < .01, ***p < .001
Discussion
Gender-based violence underlies the heavy burden of HIV among South African women. This study examined alcohol misuse and perceived sexual agency as key factors that may affect the association between GBV and HIV among women living in disadvantaged communities in South Africa. The percentage of women testing positive HIV at enrollment was higher than national estimates of HIV incidence among Black African women in South Africa (Human Sciences Research Council (HSRC), 2018), indicating that women who use substances are a key population for HIV prevention.
We found that the more alcohol problems women reported, the greater the likelihood that participants would be newly diagnosed with HIV. Our findings support previous research (Cook and Clark, 2005)and highlight the role of alcohol in maintaining the HIV epidemic among Black African women in South Africa (Parry, et al., 2010). This study also extends the existing literature by identifying alcohol misuse as a mechanism through which experiences of physical assault may contribute to HIV acquisition (Fisher, et al., 2010; Fisher, et al., 2008). Our findings suggest that alcohol misuse may be a part of negative sequela related to physical assault and increase women’s HIV risk. Consequently, strategies to reduce HIV risk may benefit from addressing alcohol misuse, especially as it relates to past trauma such as physical assault.
Our findings did not demonstrate that perceived sexual agency mediated to the association between physical assault and HIV status. Our findings were incongruent with our hypothesis and other research (Shefer, Strebel, & Foster, 2000; Strebel, et al., 2006), but may point to the importance of other factors that have more influence on HIV acquisition. For example, women in our sample were more likely to test positive for HIV if they reported engaging in sex work in the past 6 months. For many women, the choice to engage in sex work is driven by the lack of available economic opportunities (Mantsios et al., 2018). Economic empowerment is directly tied to agency and sexual health among women (Huis, Hansen, Otten, & Lensink, 2017). Therefore, improving structural factors such as economic empowerment may be more protective against HIV acquisition than individual perceived agency among women in South Africa.
There was not a significant association between sexual assault and HIV status at enrollment. This was contrary to our hypothesis and other research (Dunkle and Decker, 2013). However, this may highlight the extent to which HIV acquisition directly through sexual assault may be less prevalent than HIV acquisition through contextual and relational factors that include GBV.
This discussion is timely given the increased attention to the HIV epidemic among women and the current efforts to empower girls and women to reduce HIV in South Africa (DREAMS; (President’s Emergency Plan for AIDS Relief, 2017; Republic of South Africa Department of Health, 2016). These efforts aim to equip girls and women with the resources needed to reduce their sexual risk. These efforts should also include addressing the associations between GBV, alcohol misuse, and HIV as well as equipping girls and women with women-controlled strategies such as the female condom and pre-exposure prophylaxis, which may be especially important for women who engage in alcohol misuse or are unable to refuse sex because of the threat of violence.
Limitations
Although this study contributes to the literature on HIV prevention in South Africa, the findings should be interpreted considering their limitations. First, this is a cross-sectional study and causality cannot be inferred. Also, cross-sectional data limits the inferences of mediation analyses (Maxwell and Cole, 2007). We attempted to address this limitation by examining incident cases of HIV, therefore establishing temporality. Future research should explore these relationships prospectively. Second, participants in the current study were women who use alcohol and other drugs in Pretoria, South Africa. Consequently, the generalizability of these findings is limited. Third, data was collected using CAPI technology which requires an in-person interview with research participants. Research suggests that this method may introduce some social desirability in responses (Morrison-Beedy, Carey, & Tu, 2006). Therefore, future research should utilize audio-computer assisted self-interview software which allows participants to answer questions without the involvement of research staff – which may result in less social desirability.
Conclusions
Our findings highlight how alcohol misuse may contribute to HIV infection among South African women. Efforts seeking to reduce HIV incidence among women may consider emphasizing harm reduction strategies to limit the adverse effects of alcohol use on HIV risk. Key decision-makers may consider incorporating HIV prevention and trauma-informed care within substance use treatment centers. Consequently, HIV prevention efforts among women who engage in alcohol misuse may be more effective – reducing the HIV burden.
References
- Babor TF, Biddle-Higgins JC, Saunders JB, & Monteiro MG (2001). AUDIT: The Alcohol Use Disorders Identification Test: Guidelines for use in primary health care Geneva, Switzerland: World Health Organization. [Google Scholar]
- Bello B, Moultrie H, Somji A, Chersich MF, Watts C, & Delany-Moretlwe S (2017). Alcohol use and sexual risk behaviour among men and women in inner-city Johannesburg, South Africa. BMC Public Health, 17(3), p 548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook RL, & Clark DB (2005). Is there an association between alcohol consumption and sexually transmitted diseases? A systematic review. Sexually transmitted diseases, 32(3), pp. 156–164. [DOI] [PubMed] [Google Scholar]
- Dunkle K, Jewkes R, Brown H, Gray G, McIntryre J, & Harlow S (2004). Gender-based violence, relationship power, and risk of HIV infection in women attending antenatal clinics in South Africa. The Lancet, 363(9419), pp. 1415–1421. Retrieved from http://www.sciencedirect.com/science/article/B6T1B-4CB06W1-6/2/aab9a0601374bc1b195e11290f490487 [DOI] [PubMed] [Google Scholar]
- Dunkle KL, & Decker MR (2013). Gender-based violence and HIV: reviewing the evidence for links and causal pathways in the general population and high-risk groups. American Journal of Reproductive Immunology, 69 Suppl 1, pp. 20–26. doi: 10.1111/aji.12039 [DOI] [PubMed] [Google Scholar]
- Fisher JC, Cook PA, & Kapiga SH (2010). Alcohol use before sex and HIV risk: situational characteristics of protected and unprotected encounters among high-risk African women. [Research Support, Non-U.S. Gov’t]. Sexually Transmitted Diseases, 37(9), pp. 571–578. doi:10.1097/OLQ.0b013e3181dbafad Retrieved from 10.1097/OLQ.0b013e3181dbafadhttp://www.ncbi.nlm.nih.gov/pubmed/20644501 Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/20644501 [DOI] [PubMed] [Google Scholar]
- Fisher JC, Cook PA, Sam NE, & Kapiga SH (2008). Patterns of alcohol use, problem drinking, and HIV infection among high-risk African women. Sexually Transmitted Diseases, 35(6), pp. 537–544. [DOI] [PubMed] [Google Scholar]
- Hayes AF (2012). PROCESS: A versatile computational tool for observed variable mediation, moderation, and conditional process modeling: University of Kansas, KS. [Google Scholar]
- Huis MA, Hansen N, Otten S, & Lensink R (2017). A Three-Dimensional Model of Women’s Empowerment: Implications in the Field of Microfinance and Future Directions. Frontiers in Psychology, 8, p 1678. doi: 10.3389/fpsyg.2017.01678 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Human Sciences Research Council (HSRC). (2018). South African National HIV Prevalence, Incidence, Behaviour and Communication Survey, 2017: Key Findings Presentation. Cape Town: HSRC Press. [Google Scholar]
- Jewkes R, & Morrell R (2010). Gender and sexuality: emerging perspectives from the heterosexual epidemic in South Africa and implications for HIV risk and prevention. J Int AIDS Soc, 13, p 6. doi: 10.1186/1758-2652-13-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jewkes R, & Morrell R (2012). Sexuality and the limits of agency among South African teenage women: Theorising femininities and their connections to HIV risk practises. Social Science and Medicine, 74, Retrieved from 10.1016/j.socscimed.2011.05.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jewkes RK, Dunkle K, Nduna M, & Shai N (2010). Intimate partner violence, relationship power inequity, and incidence of HIV infection in young women in South Africa: a cohort study. [Research Support, N.I.H., Extramural, Research Support, Non-U.S. Gov’t]. Lancet, 376(9734), pp. 41–48. doi:10.1016/S0140-6736(10)60548-X Retrieved from 10.1016/S0140-6736(10)60548-Xhttp://www.ncbi.nlm.nih.gov/pubmed/20557928 Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/20557928 [DOI] [PubMed] [Google Scholar]
- Johnson LF, Coetzee DJ, & Dorrington RE (2005). Sentinel surveillance of sexually transmitted infections in South Africa: a review. Sexually Transmitted Infections, 81(4), pp. 287–293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Machisa MJ,R; Morna CL; Rama K (2011). The War at Home: Gender-based Violence Indicators Project. South Africa: https://www.saferspaces.org.za/uploads/files/GenderLinks-13452_begin_war_at_home.pdf [Google Scholar]
- Mantsios A, Shembilu C, Mbwambo J, Likindikoki S, Sherman S, Kennedy C, & Kerrigan D (2018). ‘That’s how we help each other’: Community savings groups, economic empowerment and HIV risk among female sex workers in Iringa, Tanzania. PloS One, 13(7), p e0199583. doi: 10.1371/journal.pone.0199583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maxwell SE, & Cole DA (2007). Bias in cross-sectional analyses of longitudinal mediation. Psychological Methods, 12(1), pp. 23–44. doi: 10.1037/1082-989X.12.1.23 [DOI] [PubMed] [Google Scholar]
- Morrison-Beedy D, Carey MP, & Tu X (2006). Accuracy of audio computer-assisted self-interviewing (ACASI) and self-administered questionnaires for the assessment of sexual behavior. AIDS and Behavior, 10(5), pp. 541–552. doi:10.1007/s10461-006-9081-y Retrieved from 10.1007/s10461-006-9081-yhttps://www.ncbi.nlm.nih.gov/pubmed/16721506 Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/16721506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- https://www.ncbi.nlm.nih.gov/pmc/PMC2430922/
- Onu CC, Dworkin SL, Ongeri LG, Oyaro P, Neylan TC, Cohen CR, … Meffert SM (2017). Brief Report: Sexual Violence Against HIV-Positive Women in the Nyanza Region of Kenya: Is Condom Negotiation an Instigator? Journal of Acquired Immune Deficiency Syndromes (1999), 74(1), pp. 52–55. doi: 10.1097/qai.0000000000001135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parry C, Rehm J, & Morojele N (2010). Is there a causal relationship between alcohol and HIV? Implications for policy, practice and future research. African Journal of Drug and Alcohol Studies, 9(2) [Google Scholar]
- Pearson JD (2008). Young women’s sexual agency in the transition to adulthood (Doctor of Philosophy. The University of Texas at Austin. [Google Scholar]
- Peasant C, Parra GR, & Okwumabua TM (2015). Condom negotiation: Findings and future directions. Journal of Sex Research, 52(4), pp. 470–483. [DOI] [PubMed] [Google Scholar]
- Peltzer K, Davids A, & Njuho P (2011). Alcohol use and problem drinking in South Africa: findings from a national population-based survey. African Journal of Psychiatry, 14(1), pp. 30–37. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/21509408 [DOI] [PubMed] [Google Scholar]
- Pitpitan EV, Kalichman SC, Eaton LA, Cain D, Sikkema KJ, Skinner D, … Pieterse D (2013). Gender-based violence, alcohol use, and sexual risk among female patrons of drinking venues in Cape Town, South Africa. Journal of Behavioral Medicine, 36(3), pp. 295–304. Retrieved from http://www.scopus.com/inward/record.url?eid=2-s2.0-84877837174&partnerID=40&md5=561c71c06e0b346d75de9f570f5d8d16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- President’s Emergency Plan for AIDS Relief. (2017). South Africa DREAMS Overview. Retrieved Date from http://www.pepfar.gov/documents/organization/253958.pdf.
- Rehm J, Probst C, Shield KD, & Shuper PA (2017). Does alcohol use have a causal effect on HIV incidence and disease progression? A review of the literature and a modeling strategy for quantifying the effect. Population Health Metrics, 15(1), p 4. doi:10.1186/s12963-017-0121-9 Retrieved from 10.1186/s12963-017-0121-9https://doi.org/10.1186/s12963-017-0121-9 Retrieved from https://doi.org/10.1186/s12963-017-0121-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Republic of South Africa. (2004). Ethics in Health Research: Principles, Structures, and Processes. Retrieved from http://www.mrc.ac.za/ethics/DOHEthics.pdf.
- Republic of South Africa Department of Health. (2016). The South African National Sex Worker HIV Plan.
- Scott-Sheldon LAJ, Carey MP, Carey KB, Cain D, Harel O, Mehlomakulu V, … Kalichman SC (2012). Patterns of alcohol use and sexual behaviors among current drinkers in Cape Town, South Africa. Addictive Behaviors, 37(4), pp. 492–497. doi:10.1016/j.addbeh.2012.01.002 Retrieved from 10.1016/j.addbeh.2012.01.002http://www.sciencedirect.com.prox.lib.ncsu.edu/science/article/pii/S0306460312000032 Retrieved from http://www.sciencedirect.com.prox.lib.ncsu.edu/science/article/pii/S0306460312000032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shefer T, Strebel A, & Foster D (2000). ‘So women have to submit to that...’ discourses of power and violence in student’s talk on heterosexual negotiation. South African Journal of Psychology, 30(2), pp. 28–36. [Google Scholar]
- Statistics South Africa. (2018). Mid-year population estimates 2018. (P0302). Retrieved from http://www.statssa.gov.za/publications/P0302/P03022018.pdf.
- Strebel A, Crawford M, Shefer T, Cloete A, Henda N, Kaufman M, … Kalichman S (2006). Social constructions of gender roles, gender-based violence and HIV/AIDS in two communities of the Western Cape, South Africa. Journal of Social Aspects of HIV/AIDS, 3(3), pp. 516–528. doi: 10.1080/17290376.2006.9724879 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watt MH, Aunon FM, Skinner D, Sikkema KJ, Kalichman SC, & Pieterse D (2012). “Because he has bought for her, he wants to sleep with her”: Alcohol as a currency for sexual exchange in South African drinking venues. Social Science and Medicine, 74(7), pp. 1005–1012. Retrieved from http://www.scopus.com/inward/record.url?eid=2-s2.0-84857917772&partnerID=40&md5=c9216f1cf138230aa3dc8e745fdcacd9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watt MH, Sikkema KJ, Abler L, Velloza J, Eaton LA, Kalichman SC, … Pieterse D (2014). Experiences of forced sex among female patrons of alcohol-serving venues in a South African Township. Journal Interpersonal Violence doi: 10.1177/0886260514540807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsberg WA, Luseno WK, Karg RS, Young S, Rodman N, Myers B, & Parry CDH (2008). Alcohol, cannabis, and methamphetamine use and other risk behaviours among Black and Coloured South African women: A small randomized trial in the Western Cape. International Journal of Drug Policy, 19(2), pp. 130–139. doi: 10.1016/j.drugpo.2007.11.018 R [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsberg WM, Bonner CP, Zule WA, van der Horst C, Ndirangu J, Browne FA, … Rodman NF (2019). Addressing the nexus of risk: biobehavioral outcomes from a cluster randomized trial of the Women’s Health CoOp Plus in Pretoria, South Africa. Drug and Alcohol Dependence., 195, pp. 16–26. doi:https://doi.org/10.1016/j.drugalcdep.2018.10.036 Retrieved from https://doi.org/10.1016/j.drugalcdep.2018.10.036http://www.sciencedirect.com/science/article/pii/S0376871618308196 Retrieved from http://www.sciencedirect.com/science/article/pii/S0376871618308196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsberg WM, Luseno WK, Kline TL, Browne FA, & Zule WA (2010). Preliminary findings of an adapted evidence-based woman-focused HIV intervention on condom use and negotiation among at-risk women in Pretoria, South Africa. Journal of Prevention & Intervention in the Community, 38(2), pp. 132–146. doi: 10.1080/10852351003640799 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsberg WM, Zule WA, Ndirangu J, Kline TL, Rodman NF, Doherty IA, … van der Horst CM (2014). The biobehavioral Women’s Health CoOp in Pretoria, South Africa: Study protocol for a cluster-randomized design. BMC Public Health, 14, p 1074. doi:10.1186/1471-2458-14-1074 Retrieved from 10.1186/1471-2458-14-1074http://www.ncbi.nlm.nih.gov/pubmed/25318563 Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/25318563 [DOI] [PMC free article] [PubMed] [Google Scholar]