Abstract
Background
Cardiac rehabilitation (CR) is a clinically-effective but complex model of care. The purpose of this study was to characterize the nature of CR programs around the world, in relation to guideline recommendations, and compare this by World Health Organization (WHO) region.
Methods
In this cross-sectional study, a piloted survey was administered online to CR programs globally. Cardiac associations and local champions facilitated program identification. Quality (benchmark of ≥ 75% of programs in a given country meeting each of 20 indicators) was ranked. Results were compared by WHO region using generalized linear mixed models.
Findings
111/203 (54.7%) countries in the world offer CR; data were collected in 93 (83.8%; N = 1082 surveys, 32.1% program response rate). The most commonly-accepted indications were: myocardial infarction (n = 832, 97.4%), percutaneous coronary intervention (n = 820, 96.1%; 0.10), and coronary artery bypass surgery (n = 817, 95.8%). Most programs were led by physicians (n = 680; 69.1%). The most common CR providers (mean = 5.9 ± 2.8/program) were: nurses (n = 816, 88.1%; low in Africa, p < 0.001), dietitians (n = 739, 80.2%), and physiotherapists (n = 733, 79.3%). The most commonly-offered core components (mean = 8.7 ± 1.9 program) were: initial assessment (n = 939, 98.8%; most commonly for hypertension, tobacco, and physical inactivity), risk factor management (n = 928, 98.2%), patient education (n = 895, 96.9%), and exercise (n = 898, 94.3%; lower in Western Pacific, p < 0.01). All regions met ≥ 16/20 quality indicators, but quality was < 75% for tobacco cessation and return-to-work counseling (lower in Americas, p = < 0.05).
Interpretation
This first-ever survey of CR around the globe suggests CR quality is high. However, there is significant regional variation, which could impact patient outcomes.
Keywords: Cardiac rehabilitation, Nature, Preventive cardiology, Global health, Health services, Survey
Research in context
Evidence before this study
The burden of cardiovascular disease is increasing globally, and cardiac rehabilitation (CR) is recognized as one of the most beneficial and cost-effective strategies to manage it. However, CR is a multi-component, and hence complex intervention, so the nature and quality of CR services may vary widely, impacting degree of patient benefit. Unfortunately, the nature of CR delivery has only been characterized in much less than half of the countries where it is offered around the world.
Added value of this study
For the first time, the nature of CR services in every country of the globe where it is offered has been established, and compared. This has been juxtaposed against international CR guidelines. Results showed that, where available, the quality of CR is high, but it does vary significantly by region.
Implications of all the available evidence
While the association between the quality indicators and patient outcomes requires establishment, advocacy for greater delivery of smoking cessation, stress management/psychosocial as well as counseling on return-to-work in the CR setting is needed, potentially through greater inclusion of nurses on the CR team. A global program accreditation mechanism could promote high-quality, consistent CR around the world.
Alt-text: Unlabelled Box
1. Introduction
Cardiac rehabilitation (CR) is an established model of care designed to mitigate the great burden of cardiovascular diseases (CVD) globally [1]. CR is a multi-component and hence complex intervention, so the nature and quality of CR services may vary widely, impacting degree of patient benefit. CR quality indicators or performance measures are established by American [2], Australian [3], Canadian [4], and European [5] CR societies. There are 20 CR components indicators that are generally common employed, yet whether CR is delivered up to these standards has been scantly characterized [6], [7]. Indeed, the nature of CR delivery has only been characterized in much less than half of countries where it is believed to be offered, and it has not been characterized in a comparable way [8].
For instance, CR referral is recommended in clinical practice guidelines for CVD patients [9], those with heart failure (HF) [10], [11], undergoing revascularization [12], [13], and with stable coronary artery disease [14], based on robust meta-analytic evidence of approximately 20% reductions in CVD mortality and re-hospitalization attributed to CR participation [1]. Benefits of CR in valve [15], transplant [16], and atrial fibrillation [17] patients are also established [18]. Despite this, CR guidelines vary in terms of accepted indications for CR [8], [19], and funding policies differ from country to country in terms of indications covered [20]. This may lead to variability in care received by patients around the world.
Moreover, CR guidelines recommend a “multidisciplinary team” [21], [22], [23], to ensure competent delivery of all the evidence-based elements of secondary prevention/core components (e.g., tobacco cessation interventions, dietary counseling, and stress management) [22], and medical leadership for safety [24]. Yet, little is known about the number and nature of healthcare professionals providing CR care around the globe [8], and how this may impact delivery of all the core components [3], [20], [24], [25], [26], including which CV risk factors are assessed during the initial assessment component [5].
In this first-ever survey of CR programs worldwide, the nature of CR services was assessed, specifically with regard to: (1) the type of patients served; (2) the number and types of healthcare professionals providing service, and (3) the core components delivered, in relation to international guideline recommendations [26], [27]. The nature of programs were compared by World Health Organization (WHO) region; while it was hypothesized there would be statistically significant variation, given this the first time the nature of CR services has been established globally, this study is exploratory.
2. Methods
2.1. Design & Procedure
This research was cross-sectional in design. The study was approved by York University's Office of Research Ethics (Toronto, Canada; e2014-078) and Mayo Clinic's Institutional Review Board (Rochester, United States; 16-001110). Countries where CR services were available were identified first through previous reviews [28], [29], and communication with CR and cardiology societies (see further detail elsewhere [30]). For each country identified to offer CR, first, available society leadership was contacted to solicit collaboration. If there was no society available or response, “champions” were identified from the peer-reviewed, or secondarily, gray literature/the web. Identified leaders were sent an email requesting their assistance administering the survey to each program in their country.
The lead clinician at each program identified was emailed requesting their completion of the survey. Informed consent was secured through an online form. Data were collected through REDCap from June 2016–July 2017. Contacts were sent two email reminders, at two week intervals. The national contact was provided the response rate four weeks following initial administration. Where it was < 40%, they were invited to suggest other approaches to increase response rate.
2.2. Sample
The sample consisted of all CR programs identified in the world, that offered services to patients following an acute cardiac event or hospitalization (i.e., Phase II). This included residential programs [8]. The inclusion criteria were CR programs that offered: (1) initial assessment, (2) structured exercise (supervised or not), and (3) at least one other strategy to control CV risk factors. All programs were contacted in countries known to have ≤ 250 CR programs. Where more existed, a random sub-sample of 250 was contacted. Random subsamples were generated electronically using the simple random sample module SAS institute, Cary, NC.
2.3. Measures
Development of the survey is described in detail elsewhere [30]. In short, items were based on previous national/regional CR program surveys [31], [32], [33]. Most items had forced-choice response options, and skip-logic was used to get more detail where applicable. This was pilot-tested in the Arab world and Canada [30]. It was then revised based on responses and recent literature (see online supplement; please note some questions have been slightly revised to improve clarity). The survey was translated to Portuguese, Spanish, and Mandarin (available upon request). The translations were reviewed by a national champion with the corresponding first language.
Overall, 20 structure and process quality indicators from CR societies [2], [3], [4], [5], [34] were assessed through the survey. Delivery of the 11 following core components was assessed: initial assessment, risk assessment/stratification, exercise training, patient education, management of CV risk factors, nutrition counseling, stress management, tobacco cessation interventions, vocational counseling/return-to-work, communication with primary care and end of program re-assessment (structure indicators). Assessment of the following 8 risk factors was also assessed: blood pressure, lipids, physical inactivity, poor diet, adiposity (e.g., body mass index, waist circumference, or body composition), tobacco use, glucose/HbA1c, and depression (process indicators). CR wait times were also assessed (benchmark < 30 days; process indicator) [4].
2.4. Data Analysis
SPSS version 24 and SAS version 11 were used. All initiated surveys were included. The number of responses for each question varied due to missing data (e.g., respondent did not answer a question due to inapplicability, use of skip logic); for descriptive analyses, percentages were computed using the number of responses for the specific item as the denominator.
Descriptive statistics (e.g., frequency with percentage or median with quartiles, as appropriate) were applied for all closed-ended items in the survey. All open-ended responses were coded; only those with greater than 10% responses are reported herein.
Responses were then compared by WHO region (independent variable). Clustering of program-level data within countries was taken into consideration in these exploratory inferential tests. It was tested whether the nature of programs (e.g., personnel, accepted indications; i.e., dependent variables) differed by region using generalized linear mixed models, with country as a random effect. The models were fitted via the Poisson distribution log link function for continuous dependent variables and via a binomial distribution with logit link function for categorical dependent variables, because the dependent variables were often positively skewed. For each analysis, the distribution of the residuals was reviewed to consider the model performance. While practical importance could not be considered given the novelty of this study, p < .05 was considered statistically significant where regional differences were explored inferentially.
3. Results
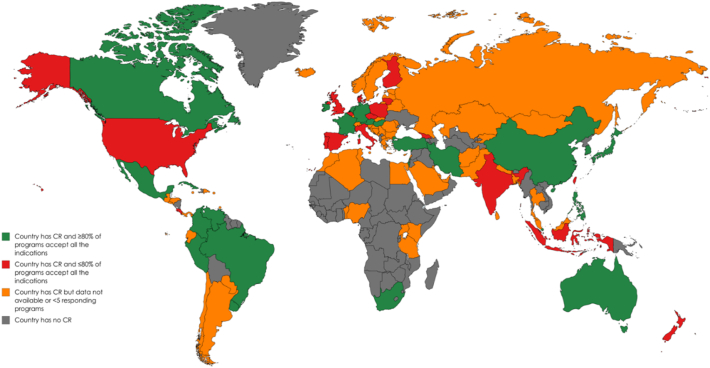
As shown in Table 1, there were 111/203 (54.7%) countries in the world with existent CR programs (Fig. 1 displays countries without), of which data were collected in 93 (83.8%; Fig. 1 also displays countries with CR where no programs responded). The number of responses per country, and response rates are shown by WHO region. More information on CR availability and capacity is reported elsewhere [35].
Table 1.
Number of participating cardiac rehabilitation programs by country and WHO region, N = 111.
| Region country | Number of programs | Number of responses | Response rate |
|---|---|---|---|
| African | |||
| Algeria | 1 | 1 | 100.0% |
| Benin | 1 | 0 | 0.0% |
| Kenya | 3 | 1 | 33.3% |
| Mauritius | 1 | 1 | 100.0% |
| Nigeria | 1 | 1 | 100.0% |
| South Africa | 23 | 14 | 60.8% |
| Tanzania | 1 | 0 | 0.0% |
| Uganda | 1 | 0 | 0.0% |
| Subtotal (across 5/8 countries with CR; 62.5%) | 32 | 18 | 56.3% |
| Americas | |||
| Argentina | 23 | 3 | 13.0% |
| Aruba | 1 | 0 | 0.0% |
| Barbados | 1 | 1 | 100.0% |
| Bermuda | 1 | 1 | 100.0% |
| Brazil | 75 | 30 | 40.0% |
| Canada | 170 | 57 | 33.5% |
| Chile | 10 | 1 | 10.0% |
| Colombia | 50 | 48 | 96.0% |
| Costa Rica | 6 | 6 | 100.0% |
| Cuba | 8 | 8 | 100.0% |
| Curacao | 2 | 1 | 50.0% |
| Dominican Republic | 2 | 1 | 50.0% |
| Ecuador | 5 | 2 | 40.0% |
| El Salvador | 2 | 0 | 0.0% |
| Grenada | 1 | 0 | 0.0% |
| Guam | 1 | 0 | 0.0% |
| Guatemala | 2 | 2 | 100.0% |
| Honduras | 2 | 1 | 50.0% |
| Jamaica | 3 | 1 | 33.3% |
| Mexico | 24 | 9 | 37.5% |
| Panama | 1 | 1 | 100.0% |
| Paraguay | 3 | 3 | 100.0% |
| Peru | 10 | 7 | 70.0% |
| Puerto Rico | 1 | 0 | 0.0% |
| Trinidad and Tobago | 2 | 0 | 0.0% |
| United States of America | 250a | 65 | 26.0% |
| Uruguay | 12 | 5 | 41.6% |
| Venezuela | 9 | 8 | 88.9% |
| Subtotal (across 22/28 countries with CR; 78.6%) | 677 | 261 | 38.6% |
| Eastern Mediterranean | |||
| Afghanistan | 1 | 1 | 100.0% |
| Bahrain | 1 | 1 | 100.0% |
| Egypt | 2 | 2 | 100.0% |
| Iran | 34 | 14 | 41.2% |
| Kuwait | 1 | 0 | 0.0% |
| Lebanon | 1 | 1 | 100.0% |
| Morocco | 1 | 1 | 100.0% |
| Pakistan | 4 | 2 | 50.0% |
| Qatar | 1 | 1 | 100.0% |
| Saudi Arabia | 1 | 0 | 0.0% |
| Tunisia | 1 | 1 | 100.0% |
| United Arab Emirates | 1 | 0 | 0.0% |
| Subtotal (across 9/12 countries with CR; 75.0%) | 49 | 24 | 49.0% |
| Europe | |||
| Austriab | 26 | 5 | 19.2% |
| Belarus | 5 | 1 | 20.0% |
| Belgium | 48 | 9 | 18.8% |
| Bosnia and Herzegovina | 1 | 1 | 100.0% |
| Bulgaria | 1 | 1 | 100.0% |
| Croatia | 3 | 3 | 100.0% |
| Cyprus | 1 | 0 | 0.0% |
| Czech Republic | 15 | 6 | 40.0% |
| Denmark | 35 | 8 | 22.9% |
| England | 266 | 57 | 21.4% |
| Estonia | 2 | 2 | 100.0% |
| Finland | 25 | 11 | 44.0% |
| France | 130 | 16 | 12.3% |
| Georgia | 17 | 13 | 76.5% |
| Germany | 120 | 34 | 28.3% |
| Greece | 4 | 4 | 100.0% |
| Hungary | 33 | 20 | 60.6% |
| Iceland | 4 | 4 | 100.0% |
| Ireland | 37 | 7 | 18.9% |
| Israel | 22 | 6 | 27.3% |
| Italy | 221 | 70 | 31.7% |
| Kazakhstan | 1 | 1 | 100.0% |
| Kyrgyzstan | 1 | 0 | 0.0% |
| Latvia | 2 | 1 | 50.0% |
| Lithuania | 25 | 9 | 36.0% |
| Luxembourg | 4 | 0 | 0.0% |
| Republic of Northern Macedonia | 1 | 1 | 100.0% |
| Malta | 1 | 1 | 100.0% |
| Montenegro | 1 | 0 | 0.0% |
| Netherlands | 90 | 29 | 32.2% |
| Northern Ireland | 13 | 10 | 76.9% |
| Norway | 35 | 0 | 0.0% |
| Poland | 56 | 21 | 37.5% |
| Portugal | 23 | 21 | 91.3% |
| Republic of Moldova | 1 | 1 | 100.0% |
| Romania | 3 | 2 | 66.7% |
| Russian Federation | 3 | 3 | 100.0% |
| Scotlandb | 69 | 24 | 34.8% |
| Serbia | 2 | 2 | 100.0% |
| Slovak Republic | 7 | 1 | 14.3% |
| Slovenia | 2 | 2 | 100.0% |
| Spain | 87 | 47 | 54.0% |
| Sweden | 69 | 1 | 1.4% |
| Switzerland | 51 | 4 | 7.8% |
| Turkey | 10 | 9 | 90.0% |
| Wales | 17 | 16 | 94.1% |
| Subtotal (across 41/46 countries with CR; 89.1%) | 1590 | 484 | 30.4% |
| South-East Asia | |||
| Bangladesh | 1 | 1 | 100.0% |
| India | 23 | 18 | 78.3% |
| Indonesia | 13 | 10 | 76.9% |
| Nepal | 1 | 1 | 100.0% |
| Sri Lanka | 4 | 2 | 50.0% |
| Thailand | 5 | 0 | 0.0% |
| Subtotal (across 5/6 countries with CR; 83.3%) | 47 | 32 | 68.1% |
| Western Pacific | |||
| Australia | 314 | 85 | 27.1% |
| Brunei Darussalam | 2 | 2 | 100.0% |
| China (including Macau) | 218 | 83 | 38.1% |
| Japanb | 325 | 9 | 2.8% |
| Malaysia | 6 | 4 | 66.7% |
| Mongolia | 1 | 1 | 100.0% |
| New Zealand | 43 | 27 | 62.8% |
| Philippines | 10 | 10 | 100.0% |
| Singapore | 7 | 7 | 100.0% |
| South Korea | 17 | 12 | 70.6% |
| Taiwan | 35 | 23 | 65.7% |
| Subtotal (across 11/11 countries with CR; 100.0%) | 978 | 263 | 26.9% |
| Total (across 93/111 countries; 83.7%) | 3373 | 1082 | 32.1% |
– = unknown; CR = cardiac rehabilitation; WHO = World Health Organization.
Random sub-sample of 2632 programs (all CR programs were contacted in countries with ≤ 350 programs; otherwise, a random subsample of 250 were contacted).
Sub-sample surveyed only, and therefore response rates actually higher (e.g., for Scotland the lead of each health region was surveyed, and there was a 100% response).
Fig. 1.
Acute coronary syndrome, stable coronary artery disease, revascularization and heart failure as accepted indications⁎, by country.
CR = cardiac rehabilitation.
⁎≥80% of responding programs in country accept guideline-recommended indications of myocardial infarction/acute coronary syndrome, stable coronary artery disease, post-percutaneous coronary intervention, coronary artery bypass graft surgery and heart failure patients.
Most (n = 775; 72.8%) programs were in an urban area. They were most often located in a hospital (n = 851, 80.6%), which was most-commonly a referral/tertiary center (n = 484; 46.1%). Most programs were part of a cardiology (n = 392, 37.5%), or physical medicine and rehabilitation (PMR) department (n = 251, 24.0%). The mean duration of supervised CR was 10.9 ± 9.4 (standard deviation; median = 8) weeks, and frequency of sessions/week 2.5 ± 1.3 (median = 2.5). Alternative models (i.e., not center-based; e.g., home-based) were offered by 285 (31.1%) programs, in 51 (45.9%) countries with CR (further detail elsewhere) [36].
3.1. Accepted Indications for CR
The most common cardiac indications accepted (Fig. 1) included those recommended in guidelines (all > 80%; by region in Supplemental Table 1 and country in Supplemental Table 2). Among programs in hospitals that offered the procedures listed, ≥ 80% of programs accepted patients receiving these procedures. There were statistically significant regional differences in acceptance of 3 non-cardiac indications (Supplemental Table 1).
3.2. CR Providers
The provider type with overall responsibility for the CR program was most often a cardiologist (n = 479, 48.4%), followed by nurses (n = 168, 17.0%), and then physiatrists/PMR specialists (n = 123, 12.4%). Overall, 680 (69.1%) programs were headed by some type of physician, and this did not vary by WHO region. Other physician types with overall responsibility included: sports medicine (n = 18, 52.9%) and family physicians (n = 6, 17.6%); other non-physician healthcare providers with overall responsibility included: some form of administrator (i.e., manager, director; n = 6, 46.2%) and occupational therapists (n = 4, 30.8%).
Professionals on the team were most often nurses, dietitians, physiotherapists, and cardiologists (Table 2; 4 varied by region; country-level data for most common shown in Supplemental Table 3). Other types of physicians on the CR team included: specialists in internal medicine (n = 32, 29.4%), and general/family physicians (n = 24, 22.0%). Other non-physician healthcare providers on the CR team included: occupational therapists (n = 52, 35.4%) and other types of exercise professionals. The median total number of staff per program (including those part-time) was 5.5 (Q25-Q75 = 4.0–7.5; Table 2); this did not differ by region (association with program volumes reported elsewhere) [35]. Whether programs offer patients individual consultations with physicians and nurses is shown by WHO region in Supplemental Table 4.
Table 2.
| n (%) | African (n = 18) | Americas (n = 261) | EMR (n = 24) | European (n = 484) | SEAR (n = 32) | Western Pacific (n = 263) | Total (N = 1082) | pc |
|---|---|---|---|---|---|---|---|---|
| Personnel on CR team | ||||||||
| Nurse | 3 (21.4%)¶ |
175 (77.1%) *** †† ‖‖‖ |
20 (95.2%) †† |
367 (94.1%) *** |
22 (75.9%) |
229 (93.5%) ‖‖‖ |
816 (88.1%) |
< 0.001 |
| Dietitian | 14 (87.5%) | 171 (75.3%) | 18 (85.7%) | 305 (79.2%) |
25 (89.3%) | 206 (84.4%) | 739 (80.2%) |
0.82 |
| Physiotherapist | 11 (73.3%) |
143 (63.3%) | 14 (66.7%) |
347 (89.0%) | 23 (85.2%) | 195 (79.6%) | 733 (79.3%) |
0.07 |
| Cardiologist | 9 (60.0%) |
177 (77.6%) | 18 (85.7%) | 324 (83.1%) | 28 (96.6%) |
165 (67.9%) | 721 (77.9%) |
0.51 |
| Administrative assistant/secretary | 10 (71.4%) | 157 (69.8%) ** |
14 (70.0%) | 289 (75.7%) ††† ‖ |
13 (46.4%) ‖ |
113 (47.3%) ** ††† |
596 (65.6%) |
0.001 |
| Psychologist | 6 (40.0%) |
104 (46.2%) * |
7 (33.3%) |
280 (72.4%) * † |
17 (60.7%) |
113 (47.9%) † |
527 (57.8%) |
< 0.05 |
| Kinesiologist/exercise specialist | 12 (75.0%) |
134 (59.3%) | 10 (47.6%) | 201 (52.5%) | 8 (28.6%) |
112 (46.9%) | 477 (52.2%) |
0.36 |
| Physiatrist/PM&R | 5 (35.7%) |
49 (22.6%) | 13 (65.0%) |
199 (52.5%) | 10 (35.7%) | 114 (47.3%) | 389 (43.4%) |
0.43 |
| Social worker | 2 (14.3%) |
71 (32.6%) |
8 (40.0%) |
167 (4.0.2%) | 6 (20.7%) |
126 (52.1%) | 380 (42.2%) |
0.20 |
| Pharmacist | 1 (7.1%) ‖ |
55 (25.7%) |
4 (20.0%) |
119 (31.7%) ‖ |
8 (28.6%) |
179 (74.0%) ¶¶¶ | 366 (41.0%) |
0.001 |
| Psychiatrist | 3 (21.4%) |
31 (14.4%) |
11 (55.0%) |
95 (25.5%) |
11 (40.7%) |
57 (24.2%) |
208 (23.5%) |
0.10 |
| Sports medicine physician | 9 (56.3%) |
37 (17.0%) | 12 (57.1%) | 71 (19.2%) | 3 (10.7%) |
51 (21.4%) |
183 (20.5%) |
0.21 |
| Community health worker | 1 (7.1%) |
17 (7.9%) | 3 (14.3%) |
69 (18.5%) |
3 (15.4%) |
72 (30.3%) |
166 (18.7%) |
0.43 |
| Other physician | 3 (21.4%) |
88 (41.3%) | 10 (50.0%) |
156 (42.2%) | 17 (58.6%) | 60 (26.3%) |
334 (38.2%) |
0.43 |
| Other non-physicians | 3 (30.0%) |
43 (37.4%) |
3 (27.3%) |
65 (33.5%) | 8 (57.1%) |
49 (29.7%) | 171 (33.6%) |
0.66 |
| Total # of program staff | 4.7 ± 2.6 | 5.2 ± 2.2 | 6.4 ± 2.2 | 6.5 ± 3.1 | 5.5 ± 3.0 | 5.5 ± 2.7 | 5.9 ± 2.8 | 0.08 |
| CR staff present during exercise | ||||||||
| Physiotherapist | 8 (80.0%) |
120 (57.1%) | 11 (68.8%) | 261 (81.1%) | 20 (83.3%) | 157 (74.8%) | 577 (72.9%) |
0.29 |
| Nurse | 1 (10.0%) |
138 (65.4%) |
16 (94.1%) | 223 (69.7%) | 16 (66.7%) | 181 (84.6%) | 575 (72.2%) |
0.08 |
| Kinesiologist/exercise specialist | 11 (78.6%) | 116 (57.1%) | 6 (40.0%) |
123 (42.0%) | 6 (26.1%) |
59 (30.1%) | 321 (43.1%) |
0.06 |
| Cardiologist | 0 (0.0%) |
57 (28.2%) | 3 (20.0%) |
98 (3.0.9%) | 12 (48.0%) | 76 (38.6%) | 246 (32.6%) |
0.64 |
| Physiatrist/PM&R | 1 (11.1%) |
33 (17.1%) | 6 (42.9%) |
63 (21.9%) | 3 (13.0%) |
66 (33.7%) | 172 (23.8%) |
0.98 |
| Dietitian | 2 (22.2%) |
24 (13.0%) *** |
10 (66.7%) *** ‖‖‖ ††† ◊◊ |
27 (10.1%) ‖‖‖ |
4 (17.4%) ◊◊ |
18 (9.3%) ††† |
85 (12.3%) |
0.001 |
| Sports medicine physician | 8 (57.1%) |
15 (8.2%) |
8 (47.1%) |
27 (9.8%) |
0 (0.0%) |
21 (11.0%) | 79 (11.2%) |
0.29 |
| Other physician | 1 (11.1%) |
25 (13.3%) | 5 (38.5%) |
25 (9.1%) |
6 (24.0%) |
16 (8.6%) |
78 (11.2%) |
0.08 |
| Community health worker | 0 (0.0%) |
2 (1.1%) |
1 (7.1%) |
6 (2.3%) |
0 (0.0%) |
23 (12.2%) | 32 (4.7%) |
0.25 |
| Other | 2 (25.0%) |
39 (29.3%) | 1 (33.3%) |
37 (18.5%) | 2 (11.8%) |
35 (23.8%) | 116 (22.8%) |
0.50 |
| Total # of program staff present during exercise sessions (mean ± SD) | 2.6 ± 1.4 | 2.8 ± 1.4 | 4.5 ± 2.3 | 2.9 ± 1.8 | 3.1 ± 1.4 | 3.4 ± 2.1 | 3.1 ± 1.8 | 0.28 |
| Number patients served per staff member (mean ± SD) | 3.2 ± 1.7 * |
4.4 ± 3.1 | 2.8 ± 1.3 ††† |
5.8 ± 12.1 * ††† ‖‖ |
3.1 ± 1.4 | 4.2 ± 3.4 ‖‖ |
4.8 ± 8.0 | < 0.05 |
For pairwise comparisons *ǂ†◊‖¶: one symbol = p < .05; two symbols = p < .01; 3 symbols = p < .001.
¶Statistically significantly different from all regions.
CR = Cardiac Rehabilitation; EMR = Eastern Mediterranean Region; PM&R = Physical Medicine and Rehabilitation; SEAR = South-East Asia Region; SD = standard deviation.
Note: Due to missing data, percentages are computed where the denominator is the number of valid responses from responding programs.
Data shown by country for most common healthcare professional types on CR team in Supplemental Table 3.
Full-time personnel counted as 1 and part-time personnel counted as 0.50.
Test for statistically significant differences by region, using generalized linear mixed models which accounted for clustering of programs within countries.
Physiotherapists and nurses were most commonly present during exercise sessions, with no variation in total number present during exercise (median = 3.0, Q25-Q75 = 2.0–4.0; Table 2). Supplemental Table 5 displays cardiopulmonary resuscitation training of personnel supervising exercise by WHO region and country. The median staff-to-patient ratio during supervised exercise was 2.0 (Q25-Q75 = 1.0–3.0) to 8.0 (Q25-Q75 = 4.0–12.0), respectively (Table 2 displays that statistically significantly more patients were served per staff member in Europe).
3.3. Core Components Delivered
Initial assessment (likely a reflection of inclusion criteria), risk factor management and patient education were the most frequently-delivered (Table 3; country-level data for key components shown in Supplemental Table 6), and on average, patients received 8.5 ± 10.8 (median = 6) education sessions per program, with each session lasting 47.0 ± 29.7 (median = 45) minutes (further detail elsewhere [35]; also regarding dose of exercise [37]). The median number of core components offered by programs was 8.7 (Q25-Q75 = 8.0–10.0). Supplemental Table 7 displays CR components and other elements delivered, by region by WHO region. There were statistically significant regional differences in the elements of exercise (lower in Western Pacific), tobacco cessation counseling (lower in the Americas), return-to-work (lower in the Americas), and women-only classes (higher in Eastern Mediterranean).
Table 3.
Cardiac rehabilitation components and other elements delivered, by region.
| n (%) | African (n = 18) | Americas (n = 261) | EMR (n = 24) | European (n = 484) | SEAR (n = 32) | Western Pacific (n = 263) | Total (N = 1082) | pb |
|---|---|---|---|---|---|---|---|---|
| Initial assessmenta | 16 (100.0%) | 236 (99.6%) | 21 (100.0%) | 394 (99.0%) | 29 (100.0%) |
243 (97.6%) | 939 (98.8%) | 0.99 |
| Management of CV risk factorsa | 15 (100.0%) | 226 (96.2%) | 21 (100.0%) | 393 (98.5%) | 29 (100.0%) |
244 (99.2%) | 928 (98.2%) | 0.92 |
| Patient educationa | 15 (100.0%) | 223 (97.8%) | 21 (100.0%) | 374 (97.1%) | 26 (96.3%) | 236 (95.2%) | 895 (96.9%) | 1.0 |
| Exercise traininga | 16 (100.0%) * †† ǂǂǂ |
230 (97.0%) * ‡ |
19 (90.5%) |
390 (97.3%) †† ◊ |
28 (96.6%) | 215 (86.7%) ǂǂǂ ◊ ‡ |
898 (94.3%) | < 0.05 |
| Heart rate measurement training/exercise intensity monitoring | 15 (93.8%) |
235 (99.6%) | 20 (95.2%) |
379 (95.7%) | 29 (100.0%) |
210 (85.4%) | 888 (94.1%) | 0.34 |
| Risk assessmenta | 15 (93.8%) |
220 (96.1%) | 18 (100.0%) | 318 (94.4%) | 23 (92.0%) | 194 (89.0%) | 788 (93.5%) | 0.78 |
| Assessment of Comorbidities | 15 (100.0%) | 218 (92.8%) | 19 (90.5%) |
378 (95.7%) | 25 (92.6%) | 222 (89.2%) | 877 (93.1%) | 0.60 |
| Nutrition counselinga | 12 (75.0%) |
211 (89.0%) | 20 (95.2%) |
376 (94.5%) | 28 (96.6%) | 233 (94.0%) | 880 (92.7%) | 0.58 |
| End of program re-assessmenta | 16 (100.0%) | 217 (93.1%) | 19 (90.5%) |
364 (91.9%) | 23 (82.1%) | 219 (89.4%) | 858 (91.4%) | 0.82 |
| Resistance training | 15 (93.8%) |
220 (94.0%) | 15 (71.4%) |
363 (91.2%) | 28 (96.6%) | 217 (87.9%) | 858 (90.8%) | 0.23 |
| Depression screening | 11 (73.3%) |
193 (81.8%) | 19 (90.5%) |
367 (92.2%) | 20 (69.0%) | 206 (83.4%) | 816 (86.3%) | 0.11 |
| Communication of assessment results to patients' primary care providera | 16 (100.0%) | 191 (80.9%) | 15 (71.4%) |
333 (85.4%) | 22 (78.6%) | 211 (85.4%) | 788 (84.0%) | 0.69 |
| Stress managementa | 10 (66.7%) |
184 (78.3%) | 17 (81.0%) |
341 (85.9%) | 22 (75.9%) | 197 (79.8%) | 771 (81.7%) | 0.52 |
| Psychological counseling | 9 (60.0%) |
166 (70.6%) | 18 (85.7%) | 343 (86.2%) | 22 (75.9%) | 194 (78.2%) | 752 (79.5%) | 0.12 |
| Prescription and/or titration of medications | 12 (75.0%) |
167 (70.8%) | 20 (95.2%) |
352 (88.4%) | 27 (93.1%) | 173 (70.0%) | 751 (79.3%) | 0.10 |
| Other functional capacity test | 14 (93.3%) |
182 (78.4%) | 14 (70.0%) |
330 (84.6%) | 25 (89.3%) | 169 (69.0%) | 734 (78.9%) | 0.26 |
| Smoking cessation sessions/classesa | 8 (53.3%) |
138 (58.5%) *** † ‡‡‡ ǂǂǂ |
15 (75.0%) † |
318 (79.9%) *** |
25 (86.2%) ǂǂǂ |
188 (76.4%) ‡‡‡ |
692 (73.3%) | 0.001 |
| Follow-up post-program | 14 (87.5%) |
156 (66.4%) | 14 (70.0%) |
256 (65.0%) | 23 (79.3%) | 199 (80.9%) | 662 (70.4%) | 0.07 |
| Exercise stress test | 13 (81.3%) |
144 (62.3%) | 18 (90.0%) |
310 (78.5%) | 25 (86.2%) |
146 (59.3%) | 656 (70.0%) | 0.71 |
| Vocational counseling/return-to-worka | 7 (46.7%) |
107 (46.1%) *** ǂǂ |
15 (71.4%) |
296 (75.1%) *** |
18 (64.3%) | 171 (70.1%) ǂǂ |
614 (65.7%) | 0.001 |
| Electronic patient charting | 11 (78.6%) |
144 (68.2%) | 12 (57.1%) |
166 (63.4%) | 11 (40.7%) | 128 (54.0%) | 472 (61.1%) | 0.48 |
| Assessment of strength | 12 (80.0%) |
88 (38.3%) | 11 (52.4%) |
183 (46.7%) | 15 (51.7%) | 138 (57.3%) | 447 (48.2%) | 0.21 |
| Alternative forms of exercise (e.g., yoga, dance) | 6 (40.0%) |
81 (34.8%) | 6 (30.0%) |
136 (34.7%) | 16 (57.1%) |
110 (44.9%) | 355 (38.0%) | 0.65 |
| Women-only classes | 3 (20.0%) |
19 (8.2%) ** |
11 (52.4%) ** ǂ †† ‡ |
45 (11.6%) ǂ |
3 (10.7%) ‡ |
29 (11.8%) †† |
110 (11.8%) |
< 0.01 |
| Other | 2 (66.7) |
26 (27.4%) | 1 (14.3%) |
30 (18.2%) | 6 (40.0%) | 48 (36.9%) | 113 (27.2%) | 0.09 |
| Total elements (mean ± SD) | 19.6 ± 3.0 | 19.1 ± 3.7 | 20.0 ± 3.4 | 20.2 ± 3.7 | 19.3 ± 3.9 | 18.5 ± 5.0 | 19.5 ± 4.1 | 0.38 |
| Total core (/11)a | 8.4 ± 1.4 | 8.6 ± 1.7 | 8.9 ± 1.7 | 9.0 ± 1.8 | 8.6 ± 1.7 | 8.4 ± 2.1 | 8.7 ± 1.9 | 0.77 |
EMR = Eastern Mediterranean Region; SEAR = South-East Asia Region; SD = standard deviation.
For pairwise comparisons *ǂ‡†◊: one symbol = p < .05; two symbols = p < .01; 3 symbols = p < .001.
Quality indicator/core component.
Test for significant differences by region, using generalized linear mixed models which accounted for clustering of programs within countries.
With regard to the core component of initial assessment, blood pressure, tobacco use, physical inactivity, body mass index, harmful use of alcohol, lipids, and diet assessment were all above 90% (Supplemental Table 8; median = 12.0 assessed, Q25-Q75 = 11.0–14.0; no statistically significant regional variation). Other risk factors assessed included: family history/genetics (n = 22, 12.3%). Over 95% of programs assessed some element of adiposity, and almost 90% assessed blood glucose in some manner (Table 4).
Table 4.
Cardiac rehabilitation quality indicators, by region.
| Mean ± SD or n (%) | African (n = 18) | Americas (n = 261) | EMR (n = 24) | European (n = 484) | SEAR (n = 32) | Western Pacific (n = 263) | Total (N = 1082) | pd |
|---|---|---|---|---|---|---|---|---|
| Time to enrolment (weeks)b | 6.8 ± 4.0 | 4.2 ± 4.3 | 5.2 ± 5.8 | 3.6 ± 3.7 | 2.4 ± 1.4 | 2.6 ± 1.9 | 3.5 ± 3.6 | 0.11 |
| Component quality | ||||||||
| Initial assessment | 16 (100.0%) |
236 (99.6%) |
21 (100.0%) |
394 (99.0%) |
29 (100.0%) | 243 (97.6%) |
939 (98.8%) |
0.98 |
| Management of CV risk factors | 15 (100.0%) |
226 (96.2%) |
21 (100.0%) |
393 (98.5%) |
29 (100.0%) |
244 (99.2%) | 928 (98.2%) |
0.92 |
| Patient education | 15 (100.0%) | 223 (97.8%) | 21 (100.0%) | 374 (97.1%) | 26 (96.3%) | 236 (95.2%) | 895 (96.9%) | 1.0 |
| Exercise counseling/prescription and/or training | 16 (100.0%) ø †† ǂǂǂ |
230 (97.0%) ø ‡ |
19 (90.5%) |
390 (97.3%) †† ◊ |
28 (96.6%) | 215 (86.7%) ǂǂǂ ◊ ‡ |
898 (94.3%) | < 0.05 |
| Risk assessment | 15 (93.8%) | 220 (96.1%) | 18 (100.0%) | 318 (94.4%) | 23 (92.0%) | 194 (89.0%) | 788 (93.5%) | 0.99 |
| Nutrition counseling | 12 (75.0%) |
211 (89.0%) | 20 (95.2%) |
376 (94.5%) |
28 (96.6%) |
233 (94.0%) |
880 (92.7%) |
0.58 |
| End of program re-assessment | 16 (100.0%) |
217 (93.1%) |
19 (90.5%) | 364 (91.9%) |
23 (82.1%) |
219 (89.4%) |
858 (91.4%) |
0.82 |
| Communication with a primary care provider | 16 (100.0%) | 191 (80.9%) | 15 (71.4%) |
333 (85.4%) | 22 (78.6%) | 211 (85.4%) | 788 (84.0%) | 0.69 |
| Stress management | 10 (66.7%) |
184 (78.3%) |
17 (81.0%) |
341 (85.9%) |
22 (75.9%) |
197 (79.8%) |
771 (81.7%) |
0.52 |
| Tobacco cessation interventions | 8 (53.3%) |
138 (58.5%) øøø † ‡‡‡ ǂǂǂ |
15 (75.0%) † |
318 (79.9%) øøø |
25 (86.2%) ǂǂǂ |
188 (76.4%) ‡‡‡ |
692 (73.3%) | 0.001 |
| Vocational counseling/support for return to work | 7 (46.7%) |
107 (46.1%) *** ǂǂ |
15 (71.4%) |
296 (75.1%) *** |
18 (64.3%) | 171 (70.1%) ǂǂ |
614 (65.7%) | 0.001 |
| Risk factor assessment quality | ||||||||
| Blood pressure | 16 (100.0%) |
234 (99.6%) | 21 (100.0%) | 385 (98.7%) | 29 (100.0%) | 243 (99.2%) | 928 (99.1%) |
0.99 |
| Tobacco use | 16 (100.0%) | 231 (98.3%) |
21 (100.0%) | 382 (97.4%) |
28 (96.6%) |
241 (98.4%) |
919 (98.0%) |
0.99 |
| Adipositya | 16 (100.0%) | 226 (96.2%) | 21 (100.0%) | 378 (96.2%) | 29 (100.0%) | 220 (93.6%) | 900 (95.8%) |
0.88 |
| Physical inactivity | 16 (100.0%) | 220 (94.0%) | 20 (95.2%) |
371 (95.6%) | 24 (82.8%) |
228 (93.4%) | 879 (94.3%) | 0.28 |
| Lipids | 12 (75.0%) |
218 (92.8%) | 21 (100.0%) | 365 (93.1%) | 28 (96.6%) |
212 (86.5%) | 853 (91.03%) | 0.46 |
| Poor diet | 14 (87.5%) | 217 (92.7%) | 20 (95.2%) | 358 (91.8%) | 21 (75.0%) | 210 (86.4%) | 840 (90.1%) | 0.23 |
| Glucose/HbA1c | 14 (87.5%) |
212 (90.2%) |
21 (100.0%) | 347 (89.0%) |
26 (96.3%) |
202 (83.5%) |
827 (88.4%) |
0.99 |
| Depression | 13 (81.3%) |
192 (83.1%) |
18 (85.7%) |
352 (90.5%) |
19 (65.5%) |
203 (83.5%) |
797 (85.8%) |
0.60 |
| # Quality/20c | 16.0 | 17.0 | 17.0 | 20.0 | 18.0 | 19.0 | 18.0 | 0.77 |
| Quality rank | 5 | 4 | 4 | 1 | 3 | 2 | 3 |
For pairwise comparisons •‡ø£†¥∂◊: one symbol = p < .05; two symbols = p < .01; 3 symbols = p < .001.
CR = Cardiac Rehabilitation; EMR = Eastern Mediterranean Region; SEAR = South-East Asia Region; SD = standard deviation.
Note: Overall quality by country shown in Supplemental Table 9. Due to missing data, percentages are computed where the denominator is the number of valid responses from responding programs.
Waist or hip circumference or body mass index.
Benchmark is 4 weeks.
Number ≥ 75% (or < 4 weeks for wait time).
Test for statistically significant differences by region, using generalized linear mixed models which accounted for clustering of programs within countries.
Functional capacity tests such as the six-minute walk (n = 224, 65.1%) were used more often than a graded exercise stress test (Table 3). Almost 95% of programs monitored exercise intensity. Overall, 441 (51.8%) programs monitored patients using telemetry during supervised exercise, 391 (46.0%) used another method of monitoring (e.g., perceived exertion, heart rate; with some reporting both), and 129 (15.2%) did not monitor during exercise (Supplemental Fig. 1).
Where programs were led by a physician (generalist or specialist), patients were statistically significantly more likely to be prescribed medications (89.8% vs 58.3%; p < 0.0001) than where programs were not led by physicians. Programs with nurses or nurse-practitioners on staff full or part-time were statistically significantly more likely to offer the following components: management of cardiovascular risk factors (99.2% vs 92.2%; p < 0.001), nutrition counseling (95.1% vs 79.7%; p < 0.001), depression screening (88.8% vs 73.4%; p < 0.001), psychological counseling (83.0% vs 58.5%; p < 0.001), tobacco cessation interventions (77.5% vs 51.8%; p < 0.001), counseling regarding return-to-work (68.7% vs 48.9%; p < 0.001), stress management (83.8% vs 68.3%; p < 0.001), and women-only classes (13.3% vs 6.4%; p = 0.01).
3.4. Overall Quality
Structure and process quality were under the benchmark of 75% of programs globally for only two indicators: tobacco cessation and return-to-work counseling (Table 4). There was statistically significant regional variation for these indicators (lower in Americas), as well as exercise (lower in Western Pacific). Total quality was very high and did not differ regionally (by country in Supplemental Table 9).
4. Discussion
In this first-ever global CR survey, the overall high quality of CR in the half of countries where it is available was established. However, deficits were identified, as were statistically significant global variations. Most programs appropriately accepted patients following acute coronary syndrome and revascularization, but fewer accepted those with heart failure, and stable coronary artery disease. Programs on average consisted of six staff members, with most commonly a cardiologist as medical director, with nurses, dietitians, physiotherapists, and administrative assistants on staff. Programs on average offered 9 of 11 recommended core components, typically initial assessment, management of risk factors, patient education, exercise, and nutrition counseling; tobacco cessation and vocational counseling/return-to-work (although not applicable to all patients) were not as consistently offered.
4.1. Accepted Indications for CR
Given capacity constraints on CR programs to treat indicated patients, it was interesting to observe that well over half of programs accepted high-risk primary prevention patients, and almost half accepted patients with peripheral arterial disease and diabetes as a primary indication. This may suggest providers see the value of preventive care delivered in CR for other conditions with common risk factors, particularly in Africa. How resources for treatment of these other conditions could buttress resources and budgets for CR programs should be explored.
4.2. CR Providers
Recommendations throughout the world are for multidisciplinary involvement in the delivery of CR [21], [27], without specific delineation of types (some exceptions [19], [23]), likely in recognition of differences in availability of trained healthcare professionals, scope of practice, and especially resources. While it was encouraging to find the average program had six staff, the most efficient number in terms of optimizing patient volumes warrants empirical consideration.
Globally, approximately 70% of programs were headed by some form of physician, and the costs versus safety impacts of this should be weighed empirically. For instance, models of care where physicians are available for consultation based on pre-specified criteria versus all patients having an individual consult with a physician may be more cost-effective (as per 2/3rds of programs).
The limited availability of mental healthcare professionals, and even pharmacists given the importance of optimal medical therapy, was somewhat disconcerting. Nurses did appear to be offering these components however, and overall played a key role in ensuring delivery of most components. Given the effect of multidisciplinary team composition on clinical outcomes is not established empirically, it is perhaps most important to ensure someone on staff has competence to deliver each of the core components [19], [22], [38].
Staff-to-patient ratios varied statistically significantly by region (higher in Europe), which may be due to variation in the number and nature of available staff, the nature of patients served and their level of risk, among other factors [39]. Globally, programs in all regions generally have one staff member to four patients (and on average there were 3 staff in each exercise session). Whether greater efficiency could be achieved by serving more patients per session (while maintaining safety), or through approaches to initiating new patients (who need more attention; i.e., staggered/rolling start or group) should be explored.
4.3. Core Components Delivered
Overall, delivery of the core components was high, but this varied regionally and the quality of what was delivered in each component was not assessed. However, some important elements of secondary prevention recommendations for CVD [5] were not commonly offered in CR, likely due to limited resources. Elements which are particularly important in low-resource settings were also unfortunately infrequently offered [26], [27], namely tobacco cessation intervention/counseling services and counseling for return-to-work.
4.4. Policy Implications
While overall results reflect high quality, a global CR program certification system may ensure more programs meet internationally-agreed, evidence-based minimum standards [26], [27]. The American (http://www.aacvpr.org/Program-Certification) and British (http://www.cardiacrehabilitation.org.uk/bacpr-nacr-certification.htm) CR societies have launched such programs in recent years. Perhaps the International Council of Cardiovascular Prevention and Rehabilitation (www.globalcardiacrehab.com) could work with these associations, among others, to develop a certification program applicable to countries around the world. A global certification program for CR providers of multiple disciplines (including trainees) has recently been developed, covering all core components (http://globalcardiacrehab.com/training-opportunities/certification/) [26], [27]. This may also promote improvement in the quality of CR around the world.
4.5. Limitations
Caution is necessary when interpreting the findings, particularly due to limits on generalizability and potential bias. Firstly, response rates to online surveys are notoriously low; in the current study country response rate was very high, but program response rates were moderate. Future replication will enable greater confidence in the findings. Second, it may not have been possible to identify all programs. Thirdly and on a related note, programs would be more comprehensively identified in countries with societies and those affiliated with prominent academic centers (i.e., ascertainment bias). Taken together, the quality of service at responding centers may be higher than what is observed in an average CR program, and therefore results may reflect somewhat higher-quality service provision than reality.
Fourth, respondents may have been inclined to respond in a socially-desirable manner, such that results were skewed to reflect better quality CR provision. However, participants were informed that their responses were confidential. Fifth, responses were not verified in a random sub-sample of programs, and hence the validity of self-report is unknown. For example, programs may have reported screening for depression, but utilized a non-psychometrically-validated tool. Finally, the significance of the inferential tests reported herein should not be interpreted to suggest significance from a health system, practice or clinical perspective. Tests of regional differences should be considered exploratory at this stage, with future research needed to further investigate.
5. Conclusion
CR programs were characterized globally for the first time, and results suggested that where offered, quality is high. However, gaps in the delivery of CR services were identified, as well as statistically significant variation by WHO region. In particular, more consistent delivery of tobacco cessation and return-to-work counseling should be promoted. Appropriateness of physician leadership, staff-to-patient ratios and acceptance of non-cardiac patients require further investigation. Resources, policy changes, and certification systems are needed to ensure all programs meet minimum standards for CR delivery [26], [27] which ensure optimal patient safety and outcomes.
5.1. Directions for Future Research
More needs to be known about the impact of each quality indicator on patient safety and outcomes, in diverse contexts, such that efforts can be directed to ensure key indicators are met universally. Indeed, while the survey assessed structure and process indicators of programs, how these translate to patient outcomes cannot be ascertained. Field tests of CR programs, examining the how and what is delivered in each core component, and degree of control of identified risk factors achieved is warranted, thus also validating survey items. For countries with a national registry [40], and it would be ideal to link this structural program data to the patient-level data in the registry to determine the degree of quality of CR. Moreover, CR delivery could then be benchmarked across these countries.
The following are the supplementary data related to this article.
Monitoring during supervised exercise, by country.
Supplementary tables
Supplementary material 1
Supplementary material 2
Supplementary material 3
Funding
This project was supported by a research grant from York University's Faculty of Health. The funder had no role in study design, data collection, data analysis, interpretation or writing of the report.
Author's Contributions
M.S. contributed to study design including measures, was responsible for data acquisition (i.e., surveying identified programs), conducting data analysis, and co-drafted the manuscript. K.T.A. identified countries with cardiac rehabilitation and contacted champions to collect data from programs. FLJ had substantial contributions to conception and design of work; facilitation of data collection in South America; EP assisted in data cleaning and drafting display items; RD, RB, BBW, WD, AA, ASB, CAS, JSK, LC, TJY, DS, KA, GG, VG, DV, EV, JC, EK, IY, CK, BB, ERE, RF, BR, DG, AS, SYC, BR, JCM, LM, GB, RS, HL, MS, ES, AH, ETP, MA, LN, EA, HK, ZE, SF, JH, EP, SD, CS, CZ, BP, AK, NS, CB, RT, and DH arranged data collection from the cardiac rehabilitation programs in their country (sampling) and revised the manuscript critically for important intellectual content. S.L.G. was responsible for the conception and design of the work, interpretation of the data, and drafting the manuscript. All authors had full access to all of the data (including statistical reports and tables) in the study and can take responsibility for the integrity of the data and the accuracy of the data analysis. All authors interpreted data and critically revised and approved the final manuscript. MS is the guarantor. The corresponding author attests that all listed authors meet authorship criteria.
Declaration of Competing Interest
Dr. Derman reports some financial activities that were outside the submitted work (i.e., grants from International Olympic and Paralympic Committees, as well as personal fees from 2 advisory boards). All other authors declare no financial or personal interests related to the work.
Acknowledgments
On behalf of the International Council of Cardiovascular Prevention and Rehabilitation through which this study was undertaken, the Global CR Program Survey Investigators are grateful to all other national champions who collaborated to identify and reach programs in their country or region, namely: Dr. Alexander Aleksiev, Dr. Aashish Contractor, Dr. Robyn Gallagher, Dr. Martin Heine, Dr. Artur Herdy, Dr. Borut Jug, Dr. Josef Niebauer, Dr. Batgerel Oidov, Dr. Henrik Schirmer, Mrs. Maria Mooney, Dr. Fernando Sepuvelda, the Korean Academy of Cardiopulmonary Rehabilitation Medicine (KACPRM), the British Association of Cardiovascular Prevention and Rehabilitation (BACPR), the Brazilian Association of Cardiorespiratory Physiotherapy and Intensive Care Physiotherapy (ASSOBRAFIR), the World Heart Federation (WHF; who also formally endorsed the study protocol), and the International Society of Physical and Rehabilitation Medicine (ISPRM).
We are also grateful to Dr. Carmen Terzic who shared the CR program survey administered in Latin America with the investigative team; this work informed development of the survey administered in this study. We also thank Dr. Ellen Schraa for input on the cost items in the survey.
References
- 1.Anderson L., Oldridge N., Thompson D.R. Exercise-based cardiac rehabilitation for coronary heart disease. J Am Coll Cardiol. 2016;67:1–12. doi: 10.1016/j.jacc.2015.10.044. [DOI] [PubMed] [Google Scholar]
- 2.Thomas R.J., King M., Lui K. AACVPR/ACC/AHA 2007 performance measures on cardiac rehabilitation for referral to and delivery of cardiac rehabilitation/secondary prevention services. J Am Coll Cardiol. 2007;50:1400–1433. doi: 10.1016/j.jacc.2007.04.033. [DOI] [PubMed] [Google Scholar]
- 3.Woodruffe S., Neubeck L., Clark R.A. Australian Cardiovascular Health and Rehabilitation Association (ACRA) core components of cardiovascular disease secondary prevention and cardiac rehabilitation 2014. Hear Lung Circ. 2015;24:430–441. doi: 10.1016/j.hlc.2014.12.008. [DOI] [PubMed] [Google Scholar]
- 4.Grace S.L., Poirier P., Norris C.M. Pan-Canadian development of cardiac rehabilitation and secondary prevention quality indicators. Can J Cardiol. 2014;30:945–948. doi: 10.1016/j.cjca.2014.04.003. [DOI] [PubMed] [Google Scholar]
- 5.Piepoli M.F., Corra U., Adamopoulos S. Secondary prevention in the clinical management of patients with cardiovascular diseases. Eur J Prev Cardiol. 2014;21:664–681. doi: 10.1177/2047487312449597. [DOI] [PubMed] [Google Scholar]
- 6.Grace S.L., Parsons T.L., Duhamel T.A. The quality of cardiac rehabilitation in Canada: a report of the Canadian cardiac rehab registry. Can J Cardiol. 2014;30:1452–1455. doi: 10.1016/j.cjca.2014.06.016. [DOI] [PubMed] [Google Scholar]
- 7.Doherty P., Salman A., Furze G. Does cardiac rehabilitation meet minimum standards: an observational study using UK national audit? Open Hear. 2017;4:1–5. doi: 10.1136/openhrt-2016-000519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pesah E., Supervia M., Turk-Adawi K. A review of cardiac rehabilitation delivery around the world. Prog Cardiovasc Dis. 2017;60:267–280. doi: 10.1016/j.pcad.2017.08.007. [DOI] [PubMed] [Google Scholar]
- 9.Smith S.C., Benjamin E.J., Bonow R.O. AHA/ACCF guideline AHA/ACCF secondary prevention and risk reduction therapy for patients with coronary and other atherosclerotic vascular disease: 2011 update a guideline from the American Heart Association and American College. Circulation. 2011;124:2458–2473. doi: 10.1161/CIR.0b013e318235eb4d. [DOI] [PubMed] [Google Scholar]
- 10.Yancy C.W., Jessup M., Bozkurt B. ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2013. 2013;62:e147–e239. doi: 10.1016/j.jacc.2013.05.019. [DOI] [PubMed] [Google Scholar]
- 11.Long L., Mordi I.R., Bridges C. Exercise-based cardiac rehabilitation for adults with heart failure. Cochrane Database Syst Rev. 2019;1 doi: 10.1002/14651858.CD003331.pub5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hillis L.D., Smith P.K., Anderson J.L. ACCF/AHA guideline for coronary artery bypass graft surgery: a report of the American College of Cardiology Foundation/American Heart Association task force on practice guidelines. Circulation. 2011;124:e652–e735. doi: 10.1161/CIR.0b013e31823c074e. 2011. [DOI] [PubMed] [Google Scholar]
- 13.Levine G.N., Bates E.R., Blankenship J.C. ACCF/AHA/SCAI guideline for percutaneous coronary intervention. J Am Coll Cardiol. 2011;58:1–79. doi: 10.1016/j.jacc.2011.08.007. 2012. [DOI] [PubMed] [Google Scholar]
- 14.Montalescot G., Sechtem U., Achenbach S. ESC guidelines on the management of stable coronary artery disease: the task force on the management of stable coronary artery disease of the European Society of Cardiology. Eur Heart J. 2013;34:2949–3003. doi: 10.1093/eurheartj/eht296. 2013. [DOI] [PubMed] [Google Scholar]
- 15.Sibilitz K.L., Berg S.K., Tang L.H. Exercise-based cardiac rehabilitation for adults after heart valve surgery. Cochrane Database Syst Rev. 2016;3 doi: 10.1002/14651858.CD010876.pub2. [DOI] [PubMed] [Google Scholar]
- 16.Anderson L., Nguyen T.T., Dall C.H. Exercise-based cardiac rehabilitation in heart transplant recipients. Cochrane Database Syst Rev. 2017;4 doi: 10.1002/14651858.CD012264.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Risom S.S., Zwisler A.-D., Johansen P.P. Exercise-based cardiac rehabilitation for adults with atrial fibrillation. Cochrane Database Syst Rev. 2017;2 doi: 10.1002/14651858.CD011197.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Strategic Commissioning Development Unit Case for change - cardiac rehabilitation services. 2010. https://www.gov.uk/government/publications
- 19.Price K.J., Gordon B.A., Bird S.R. A review of guidelines for cardiac rehabilitation exercise programmes: is there an international consensus? Eur J Prev Cardiol. 2016;23:1715–1733. doi: 10.1177/2047487316657669. [DOI] [PubMed] [Google Scholar]
- 20.Babu A.S., Lopez-Jimenez F., Thomas R.J. Advocacy for outpatient cardiac rehabilitation globally. BMC Health Serv Res. 2016;16:471. doi: 10.1186/s12913-016-1658-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Buckley J., Doherty P., Furze G. Standards and core components for cardiovascular disease prevention and rehabilitation. 2017. http://www.bacpr.com/resources/AC6_BACPRStandards&CoreComponents2017.pdf London UK. [DOI] [PMC free article] [PubMed]
- 22.Hamm L.F., Sanderson B.K., Ades P.A. Core competencies for cardiac rehabilitation/secondary prevention professionals: 2010 update: position statement of the American Association of Cardiovascular and Pulmonary Rehabilitation. J Cardiopulm Rehabil Prev. 2011;31:2–10. doi: 10.1097/HCR.0b013e318203999d. [DOI] [PubMed] [Google Scholar]
- 23.Gómez-Gonzáleza A., Miranda-Calderínb G., Pleguezuelos-Cobosc E. Recommendations of the Cardio-Respiratory Rehabilitation Society (SORECAR) on cardiac rehabilitation in ischemic heart disease. Rehabilitacion. 2015;49:102–124. [Google Scholar]
- 24.Balady G.J., Chaitman B., Driscoll D. Recommendations for cardiovascular screening, staffing, and emergency policies at health/fitness facilities. Circulation. 1998;97:2283–2293. doi: 10.1161/01.cir.97.22.2283. [DOI] [PubMed] [Google Scholar]
- 25.Balady G.J., Williams M.A., Ades P.A. Core components of cardiac rehabilitation/secondary prevention programs: 2007 update. Circulation. 2007;115:2675–2682. doi: 10.1161/CIRCULATIONAHA.106.180945. [DOI] [PubMed] [Google Scholar]
- 26.Grace S.L., Turk-Adawi K.I., Contractor A. Cardiac rehabilitation delivery model for low-resource settings. Heart. 2016;102:1449–1455. doi: 10.1136/heartjnl-2015-309209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Grace S.L., Turk-Adawi K.I., Contractor A. Cardiac rehabilitation delivery model for low-resource settings: an International Council of Cardiovascular Prevention and Rehabilitation consensus statement. Prog Cardiovasc Dis. 2016;59:1–20. doi: 10.1016/j.pcad.2016.08.004. [DOI] [PubMed] [Google Scholar]
- 28.Turk-Adawi K., Sarrafzadegan N., Grace S.L. Global availability of cardiac rehabilitation. Nat Rev Cardiol. 2014;11:586–596. doi: 10.1038/nrcardio.2014.98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ragupathi L., Stribling J., Yakunina Y. Availability, use, and barriers to cardiac rehabilitation in LMIC. Glob Heart. 2016;12:323–334. doi: 10.1016/j.gheart.2016.09.004. [DOI] [PubMed] [Google Scholar]
- 30.Turk-Adawi K.I., Terzic C., Bjarnason-Wehrens B. Cardiac rehabilitation in Canada and Arab countries: comparing availability and program characteristics. BMC Health Serv Res. 2015;15:521. doi: 10.1186/s12913-015-1183-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Polyzotis P.A., Tan Y., Prior P.L. Cardiac rehabilitation services in Ontario: components, models and underserved groups. J Cardiovasc Med. 2012;13:727–734. doi: 10.2459/JCM.0b013e32835794c1. [DOI] [PubMed] [Google Scholar]
- 32.Cortes-Bergoderi M., Lopez-Jimenez F., Herdy A.H. Availability and characteristics of cardiovascular rehabilitation programs in South America. J Cardiopulm Rehabil Prev. 2013;33:33–41. doi: 10.1097/HCR.0b013e318272153e. [DOI] [PubMed] [Google Scholar]
- 33.Bjarnason-Wehrens B., McGee H., Zwisler A.-D. Cardiac rehabilitation in Europe: results from the European Cardiac Rehabilitation Inventory Survey. Eur J Cardiovasc Prev Rehabil. 2010;17:410–418. doi: 10.1097/HJR.0b013e328334f42d. [DOI] [PubMed] [Google Scholar]
- 34.Donabedian A. Quality assessment and assurance: unity of purpose, diversity of means. Inquiry. 1988;25:173–192. [PubMed] [Google Scholar]
- 35.Turk-Adawi K., Supervia Pola M., Lopez Jimenez F. Cardiac rehabilitation availability and density around the globe. eClinicalMedicine. 2019 doi: 10.1016/j.eclinm.2019.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ghisi G.L.M., Pesah E., Turk-Adawi K. Alternative models of cardiac rehabilitation around the globe. J Clin Med. 2018;7:1–13. doi: 10.3390/jcm7090260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chaves G., Turk-Adawi K., Supervia M., Santiago Pio C., Lopez-Jimenez F., Abdel-Hadi R., El-Heneidy A.A., Grace SL. Cardiac rehabilitation dose around the globe: variation and drivers. Circ Cardiovasc Qual Outcomes. 2019 doi: 10.1161/CIRCOUTCOMES.119.005453. [DOI] [PubMed] [Google Scholar]
- 38.Pedersen B.K., Saltin B. 2015. Exercise as medicine – evidence for prescribing exercise as therapy in 26 different chronic diseases; pp. 1–72. Suppl. 3. [DOI] [PubMed] [Google Scholar]
- 39.AACVPR . 5th ed. Human Kinetics; Champaign, IL: 2013. American Association of Cardiovascular and Pulmonary Rehabilitation. Guidelines for cardiovascular and secondary prevention programs. [Google Scholar]
- 40.Poffley A., Thomas E., Grace S.L. A systematic review of cardiac rehabilitation registries. Eur J Prev Cardiol. 2017;24:1596–1609. doi: 10.1177/2047487317724576. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Monitoring during supervised exercise, by country.
Supplementary tables
Supplementary material 1
Supplementary material 2
Supplementary material 3