Abstract
Background
Technology such as wearable technology and self-management applications could improve the care of patients with chronic obstructive pulmonary disease (COPD) by real-time continuous monitoring, early detection of COPD and improved self-management. However, patients have not been willing to use technology when it is too difficult to use, interferes with their daily lives or threatens their identity, independence and self-care.
Methods
We conducted a qualitative study to determine what patients with COPD would like to see in a wearable device and a mobile application to help manage their condition. Semi-structured interviews were conducted, recorded and transcribed. Thematic analysis was used to identify themes and concepts.
Results
We interviewed 14 people with COPD with an average age of 69 years. Participants perceived that the technology could improve their ability to manage their condition both in daily life and during exacerbations by connecting how they feel and by knowing their oxygen saturation, heart rate and activity. The technology may help them address feelings of fear and panic associated with exacerbations and may provide reassurance and connectedness. Some people with COPD wanted their healthcare providers to have access to their data, while others were concerned about inundating them with too much information. Of note, people wanted to maintain control of the information; to make connections with the data, but also in order to be alerted when a possible exacerbation occurs.
Conclusion
Patients perceived significant potential for wearables and apps to help manage their condition.
Short abstract
In-depth interviews with COPD patients found that they face significant challenges managing their condition. Patients perceive significant potential for wearables to help with self-management and alerting them to a possible exacerbation. http://bit.ly/2xcyBlB
Introduction
Patients with chronic obstructive pulmonary disease (COPD) often seek care only when experiencing an exacerbation that is severe. Affordable, wearable technology such as smartwatches that monitor heart rate, respiratory rate, physical activity and coughing may help predict early exacerbations and can lead to improved patient care [1–3]. An app designed to help self-management can provide patients with feedback of their physiological parameters, which may give them more awareness and control over their condition. A mobile application could give patients access to resources that can help with disease management, such as weather information or daily breathing exercises. In patients with COPD, self-management has been shown to increase quality of life and reduce respiratory-related hospital admissions [4].
However, technology is not effective if it is not used. A recent systematic review of COPD self-management apps highlighted the difficulties with maintaining the engagement of apps over time [5]. Patients are not willing to use technology when it is difficult to use, threatens their identity, independence and self-care, disrupts their relationship with their primary care provider and interferes with their daily lives [6]. In our previous work, we found that it was feasible for people with COPD to use wearables for real-time data collection, but many people were not interested in participating or did not complete the study. We found that patients with COPD wanted more from a wearable device [7].
In this study, we sought to engage patients in the development of a wearable and a self-management app by conducting in-depth, semi-structured interviews to explore the needs and preferences of COPD patients.
Methods
Study design
We conducted a qualitative study to determine what patients with COPD would like to have in a wearable device and mobile application to help manage their condition. This study is part of a larger ongoing project to develop wearables for patients with COPD to improve self-management and detect acute exacerbations early [7, 8].
Participants
Between October 2017 and March 2018, we recruited patients with COPD by posting advertisements in respirology clinics, approaching patients admitted with COPD and by asking participants to suggest other people with COPD. Anyone who had been given a diagnosis of COPD by a healthcare professional, who spoke English and who did not have a cognitive barrier was eligible to participate. We conducted purposive sampling to select participants who did and did not use different technology such as computers, smartphones, smartphone apps and wearables.
Data collection
An interview guide was developed by the research team and contained questions that explored 1) the challenges that people with COPD face in their lives; 2) how an app and self-management tool would be able to help them; and 3) what they would find easy to use in a wearable and an app. Semi-structured interviews were conducted by a trained interviewer using an interview guide and were audio-recorded and transcribed verbatim. Interview duration was 45 min to 1 h. Interviews were conducted in person at Toronto General Hospital (n=3) and over the phone (n=11). Patients did not know the interviewer outside of the research study. Transcripts were read by members of the research team after every two to three interviews, and the interview guide was revised to explore fully both anticipated as well as unanticipated responses. Interviews continued until the team felt that saturation of themes was achieved.
Data analysis and reflexivity
We used an inductive thematic analysis to search for themes and concepts in relation to our research question across the interviews [9]. Our epistemological viewpoint was constructivist. We co-constructed meaning with our participants as we moved through the interviews. Interviews were transcribed verbatim and uploaded onto a qualitative data management system (NVivo 10; QSR International, Melbourne, Australia) which facilitated coding and analysis. Anonymised transcripts were coded independently by two researchers (TS and RW), who began by familiarising themselves with the transcripts and discussing general ideas and patterns apparent in the data. The next stage involved each coder individually going through the interviews and coding segments of the interviews that were relevant to our research questions. Throughout this stage, researchers met regularly to compare and discuss the codes and resolve any discrepancies. The codes were then grouped into larger themes which were related to the research question. The final step was a research team meeting to review the themes and subthemes and to discuss final interpretations and modifications.
We aimed to be reflective in our own backgrounds and experiences for the duration of the coding and analysis. RW, AG and SG are all scientists and physicians; AG's research and practice focuses on respiratory disease. TS recently completed her MA in disability policy.
Ethics
The study was conducted in accordance with the amended Declaration of Helsinki. The protocol was approved by the University Health Network research ethics board (17-5198) and informed consent was obtained from all patients.
Results
14 people were interviewed. Characteristics are summarised in table 1. Individuals' use of technology is shown in table 2. Results are presented as 1) current experiences and challenges with COPD care and how information technology could affect them and 2) barriers to using the technology (figure 1).
TABLE 1.
Participant characteristics
| Subjects n | 14 |
| Female | 50 |
| Age years | 69 (62–81) |
| Years since COPD diagnosis | 9.1 (1–17) |
| Total number of previous COPD exacerbations | 5.6 (0–32) |
| Number of previous ED visits for COPD | 1.1 (0–3) |
| Number of previous hospitalisations for COPD | 0.93 (0–3) |
| Long-term oxygen therapy | 5 (36) |
| Household income based on postal code CAD | 33 400±15 800 |
Data are presented as %, mean (range), n (%) or median±sd, unless otherwise stated. COPD: chronic obstructive pulmonary disease; ED: emergency department; CAD: Canadian dollar.
TABLE 2.
Technology use of individual participants
| Participant | Sex | Age (rounded to nearest decade) | Uses a computer (desktop or laptop) | Uses a smartphone | Uses phone apps | Uses or has used wearable technology |
| 1 | M | 70 | Yes | Yes | No | No |
| 2 | M | 80 | Yes | Yes | No | Yes |
| 5 | F | 60 | Yes | Yes | Yes | Yes |
| 7 | M | 60 | No | Yes | No | No |
| 11 | M | 60 | No | Yes | Yes | Yes |
| 17 | F | 80 | No | Yes | No | No |
| 28 | F | 60 | Yes | Yes | Yes | No |
| 38 | M | 70 | Yes | Yes | No | Yes |
| 40 | M | 60 | Yes | Yes | Yes | No |
| 41 | M | 70 | Yes | No | No | Yes |
| 43 | F | 70 | Yes | Yes | Yes | No |
| 56 | F | 80 | Yes | Yes | Yes | Yes |
| 66 | F | 70 | No | Yes | No | Yes |
| 88 | F | 70 | Yes | No | No | Yes |
M: male; F: female.
FIGURE 1.
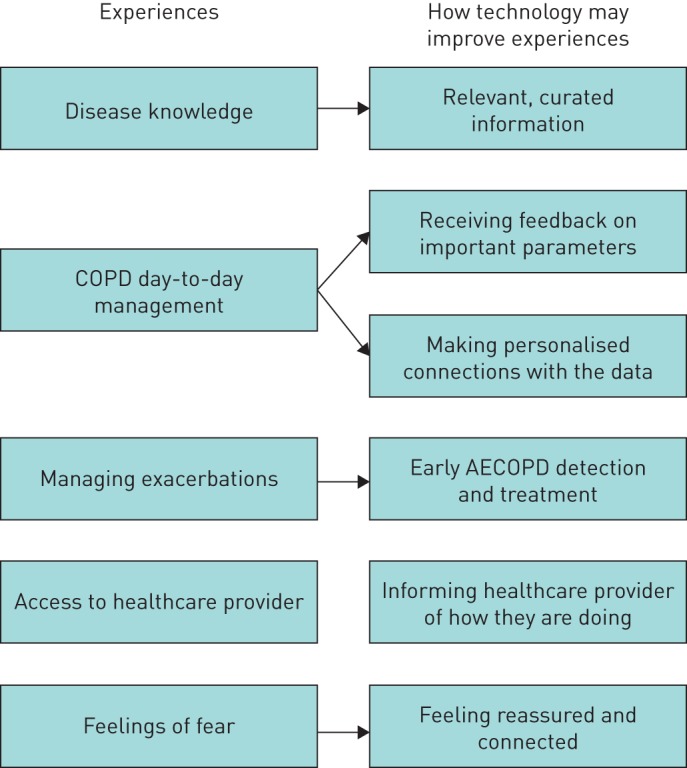
Patient experiences and challenges of current chronic obstructive pulmonary disease (COPD) care and how technology may address them. AECOPD: acute exacerbations of COPD.
Experiences with current COPD care
Issue: disease knowledge
Participants had varied perceptions about their knowledge of COPD. Some felt they had sufficient information about their condition, especially those who had attended pulmonary rehabilitation. However, others stated that they did not receive enough information about their condition, especially in the beginning, and they had to learn and acquire knowledge as their disease progressed. Some used the internet to gain information; however, there was concern about the accuracy of the information.
Interviewer: Was it easy to learn about COPD?
P40: Yeah, it wasn't hard at all. I actually just punched COPD into Google and there you go.
Interviewer: How do you/did you obtain information about COPD?
P11: I don't really use the internet for medical stuff, I usually ask a doctor, I don't rely on information on the internet for anything medical really
Relevant, curated information
Participants desired more information from their healthcare providers, including more detailed information on what exactly COPD is, how to manage symptoms, and what to do when symptoms worsen. Some commented that they would also want to see educational videos and have a source for looking up material about their condition or new medications. They desired general information on COPD as well very specific data such as the current air quality and weather.
P38: I think when you're meeting a physician or even in a hospital situation it would be nice, it would be nice to have some material there that the doctor would give you, that say here are some pros and cons, here are some things you need to look out for. If these things start to happen this is what you should do. …. As far as I can see there isn't really anything there.
Issue: living with COPD
Most participants expressed difficulty with managing their condition on a day-to-day basis and completing activities of daily living. They highlighted examples of tasks that used to be second nature, such as showering, doing dishes or grocery shopping, which now took a lot of preparation and time to complete. These hardships were often linked to decreased quality of life. Many participants described a change that they had to make to their lifestyle or home after being diagnosed with COPD.
P41: I'm managing on the medications I have now but it's not improving the quality of my life. We need to find something, if there's anything available to increase the quality of life. I get very tired very quickly, I'm very limited by what I can do, I need to break my tasks down all the time. I was telling my doctor the other day, it takes me a half an hour to have a shower. I bird bath in the sink and do my head, then I have to sit down for 5 min. Then I do my torso and sit down for 5 min, then I do my lower half and rinse off all the soap. It's a process, doing the dishes is a process, they're all coping mechanisms.
Several participants expressed not being aware of how to engage in physical activities with COPD and not knowing what their safe zone is. They described times where their heart rate would go up and they did not know why, which induced panic and further escalated their heart rate.
Participants listed many exacerbation triggers and described their many strategies they used to avoid an exacerbation of symptoms. Participants accepted that this was their new normal and that they would have to continue using coping mechanisms to maintain their health.
Receiving feedback on important parameters
Many of our participants felt that they could be doing a better job with self-management and paying attention to their symptoms. They expressed an interest in using a wearable device that monitored symptoms of COPD and help them to manage. Almost everyone said that real-time monitoring of oxygen saturation would give them peace of mind. In addition, participants wanted information on their heart rate, blood pressure, activity, sleep and coughing. They felt this information would prevent them from overdoing it, encourage them to take a break or take their medication if necessary, and would allow them understand why they may be feeling certain symptoms.
P88: Well, it would be useful to me to know when my oxygen level was dropping, ahead of me suddenly gasping for breath and thinking, “I need to go and sit down”. That would be really helpful to me. I think if I had something like that, I might be more in my own head, more observant of not letting myself get to that point, for sure. Also, heart rate and blood pressure.
Making personalised connections to the data
Participants described that the technology would be able to help them make connections between how they are feeling and what their body is doing. People struggled with understanding the relationship of their condition and different triggers to their heart rate and blood pressure. They would put off going to the doctor or starting a treatment plan because they were unable to recognise early symptoms. Real-time monitoring could confirm that there was a need to see a healthcare professional and would be encouragement to get early treatment. It could allow people to better understand their symptoms so they would feel safer engaging in activities.
P5: at one point I was enrolled into a program at [hospital X]…. As I was exercising, they became very startled because they were monitoring heart rate and because of my arrhythmia and COPD, my heart rate can go up beyond what it looks like it should be for that level of exercise…They suggested to look for something else and that's when I found out about the pulmonary rehab program, which taught me how to learn and feel comfortable with a heart rate that was elevated and understand what it was I needed to do to push myself… So if we could have my oxygen level and heart rate while I was exercising, it would help to alleviate their fears a little and my own as well. So I think that kind of device can be helpful even if, in my case, I don't have terrible COPD but I know that exercising is really important and I would like to be able to do it with some security.
Issue: managing exacerbations
Action plans (a set of instructions to follow in the event of an exacerbation) are considered to be an important component to help patients manage exacerbations. Several participants said that they did not have an action plan. Some were unaware of the concept, while others knew that they should have one but had never had the conversation with their healthcare provider to create one.
Interviewer: Do you have a COPD action plan?
P28: No.
Interviewer: So what do you do if you're having an exacerbation?
P28: Last time I couldn't get out of bed. I think I had a touch of the flu, too. Then the following week I went to see my doctor and she gave me antibiotics.
When asked to describe how they manage their symptoms once they worsen, some people mentioned having rescue medications described on their action plans. However, some had less developed plans on what to do when they had an exacerbation. Some participants’ plans were to call an ambulance or go to the emergency department as they stated they were often already pretty far into the exacerbation by the time they recognised they are having one.
P2: One of the pieces of advice I've been given by medical people, because my level of lung function is so bad, if I feel anything is coming, like the flu, or anything else, do not wait to get an appointment with the GP, just head to the Emerg because it can overtake you so fast, in fact that's what happened.
P41: Again, I associate it with a cold, so if the cold isn't getting any better than I start taking extra vitamin C, taking extra Echinacea to try to ward that off. I do start to put together a little travelling bag in case I need to go to the hospital, I do that while I'm still functional and able to get around. If I know it's going to be an exacerbation I basically call an ambulance and go to the hospital. But then again, if you know it's going to get to that point you're already pretty far into the process.
Detection and treatment of early acute exacerbation of COPD
Participants agreed that early exacerbation detection could encourage them to start monitoring their condition immediately and begin early treatment. An area of concern was that sometimes symptom onset seemed very sudden and they did not know why. They indicated that they would want to be alerted first if the wearable device detected an exacerbation. It would then help them begin their action plan and move through the instructions agreed upon with their respirologist or healthcare provider. Primarily, participants wanted control over the information. One participant described the struggle to know how they are doing and wanted more objective data on whether they were doing better or worse.
Interviewer: Okay. What do you think should happen if the watch feels that you're getting an exacerbation? What should the watch do or what should it signal?
P56: Well, I think what would be nice to know should you see a doctor? Should you not see a doctor? Or some kind of a healthcare provider. It would be nice. As I said, I'm not that stupid but I feel pretty stupid about this whole thing. I really don't have enough education as far as my health is concerned. I think it would be a reinforcement would be nice to know, “Yes, you do…” Mind you, when I was at the hospital Wednesday they said, “You're doing better.” I think, “Did I?” I don't know. I think I should have a little more education somehow
Issue: access to healthcare provider
Most of our participants expressed great satisfaction with their healthcare providers. Some also felt that they had good access to their respirologist and saw them frequently; however, others only saw their respirologist once or twice a year. Despite the relationship with their healthcare provider, very few patients thought that they could communicate in a timely manner with their healthcare provider in urgent situations.
Informing the healthcare provider
When asked if it would be valuable for their healthcare provider see the data from the wearable, patients had differing views. Some participants thought that the information from the wearables would be valuable for their COPD physician to see. Some were concerned about their physician being annoyed or overloaded by all the data or unnecessary alerts. They did feel that the information provided to their physician should be a summary of their data and that they should receive an alert only in extreme situations.
P17: I don't know if my respirologist want to be bothered with tons and tons of patient data
Interviewer: Do you think it would be useful if all your information that this wearable collects, so your heart rate, oxygen saturation, if this information was sent to your healthcare provider?
P11: Oh yeah, for sure, you should see my file at Dr X's office, it's like a big encyclopedia thick, you know it's pretty thick, like file, so the more information they have the better. You'd have to ask the doctor, I think the more information the better
P38: The other piece being cumulative, or a month, 2 months, 3 months, so you can send your cumulative results and they can take a look and say that the trend lines look ok and you can just file it, or the trend lines look problematic and we should look into it. I don't think on a day-to-day basis it should send it. They wouldn't want to see it, they're so busy. But if you did it once a month or once a quarter,
Issue: emotions of fear and sadness
Strong emotions from participants were described both when they were diagnosed with COPD as well as during exacerbations. They described being upset with the diagnosis and feeling panic and fear during exacerbations. The panic and fear would increase anxiety and result in even more shortness of breath. Patients described that the whole process of going to a hospital was difficult and draining for them, both physically and emotionally. Those who had been to the emergency department for an exacerbation were in constant fear of having to go through it again.
P41: It's a horrible feeling because you don't know what to do to help yourself and anything that you do doesn't work. It's a great deal of panic. It feels like you're breathing through a wet wash cloth. Every time you take a breath in you're gasping because you feel like you haven't gotten enough air in and once you breathe out you're not letting out enough either, so it escalates very quickly from being just an ordinary cold to less than in a day it will turn into an exacerbation because it hadn't gotten caught soon enough. It's terrifying, when you get to the hospital it's even more terrifying because I know that it's COPD and I know that it's an exacerbation but all of the people in the ER treating me have to do their own series of tests before they'll agree that yes, it's COPD. So for the initial period that you're in the hospital they're not treating you, they're just trying to manage you and make you more comfortable, so that is also very frightening. The whole process is exhausting because you're constantly fighting that air starvation, you're just constantly fighting to be able to breathe. It's exhausting.
Feeling reassured and connected
Participants felt that having a system to monitor their condition would ease their mind and provide a feeling of security. They described times where they would ignore their symptoms, or overwork themselves without realising it. Participants stated that being constantly monitored was similar to having a security blanket.
P38: I think psychologically it should give you a bit of a boost knowing that you had an electronic monitor of your health on a regular basis instead of leaving things up to chance.
P88: I do, because one of the problems is I've spent so many years denying the fact that there's anything wrong with my lungs that I still don't feel that I react soon enough, and I could really get myself in trouble because I could, “Well, I just have one more thing I have to do, and when I get this done, or this done, or…” because I do a lot of volunteering…and ignore it, because…Well, this has nothing to do with COPD, but I finally ate my dinner at 10:00 last night. So if I had something like that, it might sort of boink up and say, “You're having a problem!” Or whatever. It's somebody sort of watching me.
Barriers to adoption
Factors that may influence the use and uptake of wearables and self-management apps included variable mastery of technology by COPD patients, the design of the wearables, accuracy of the technology, concerns about being a “prisoner of the numbers” and financial concerns (table 3).
TABLE 3.
Barriers in the use of wearables and apps in chronic obstructive pulmonary disease (COPD) self-management
| Variable technology use | In our sample, there was varied use of technology by patients, from avid users to people who used minimal technology. Although most participants used cellphones and apps in their daily life, there were some who preferred using their phones as little as possible and only carried them for emergencies |
| Interviewer: Do you have a cell phone? | |
| P41: I do but I'm not good at it. I only use it for emergency purposes and there's all these little pictures on there that I don't care about. It keeps doing things I don't want it to do so I just carry it with me for emergency purposes | |
| Wearable design | Participants had specific desires for the design of the wearable device. They wanted it to be stylish and would prefer options of styles and sizes. They did not want to stick out while wearing it as they did not want to be identified as having a medical condition requiring a monitoring device |
| P17 Well, I guess the watch part of it would be okay. Everybody wears them, so it's not like it would be too distinguished or to stick out too much… as long as, yeah, as everybody would just look at it as being normal so you wouldn't stick out in a crowd or nothing. That's another thing. You don't want to stick out in a crowd | |
| Accuracy and technical issues of wearable | Participants were concerned about how accurate the device would be and did not want to use something that was inaccurate or had technical problems. Error messages and meaningless flashing or beeping was an area of concern. Some mentioned that they had given up their Fitbits or smartwatches due to technical issues and inaccurate data |
| P2: But, I have the latest Fitbit and it really is quite inaccurate. If you are aware, I drive a motorcycle, if I go on the bike for half an hour it says I've climbed like 50 flights of stairs. It misses things like, stairs, my office, where I am sitting right now I am up and down the stairs all day. I would estimate I am up and down the stairs 8–10 times and it typically shows 4–5. And sleep, they try their best to give you your sleep, and that is something I'm really interested in, I'll give you an example, they disregard periods that could be sleep. If you sit still for 2 h enough it might say you were napping. If I wake up from sleep after 45 min after a disturbance, the next day when I look at my sleep, it threw away that 45 min | |
| “Prisoner of the numbers” | Participants also were concerned about being a “prisoner of the numbers”, where they would feel they would need to keep checking the device to know how they were doing, and the device would dominate their lives. Small changes in oxygen saturation are common, and they did not want to be constantly checking their watch and worrying if their oxygen saturation dropped a little more than average |
| P41: I've asked here and my doctor about getting one of the little oximeters and they all advise against it because then you become a prisoner of the numbers. I see people here who have an oximeter and they are a prisoner of the numbers. “Oh it shouldn't have gone down 2 it should only have gone down 1, maybe it will go back up by 3 tomorrow” | |
| Cost | Participants were concerned about the cost of the device as many were on a fixed income. Specifically, they acknowledged concerns about costs of medications or inability to afford a device like a Fitbit |
| P38: Maybe also some of the LG watches can be offered on a prescription basis. I notice that they're 3–4–5 hundred dollars and that's very expensive. For someone with a COPD condition to say that they want to buy one to monitor themselves, if a doctor was to say that this is something that is necessary and provide a subsidy that would be a lot easier |
Discussion
In this qualitative study of 14 people with COPD, we found that technology such as wearables and self-management apps were viewed favourably. Our participants felt that such devices may help COPD patients to manage the significant challenges associated with their condition. Specifically, participants perceived that the technology could improve their ability to manage their condition both in daily life and during exacerbations. This would occur by connecting their how they feel to physiological parameters such as oxygen saturation, heart rate and activity. It would also occur through early detection of exacerbations. Technology may address feelings of fear and panic associated with exacerbations and provide reassurance and connectedness. Barriers to technology use include the varied nature of technology use among people with COPD, wearable design, the cost, accuracy issues and whether the technology may make people with COPD feel less well.
Qualitative studies have examined different components of wearable use, monitoring values and self-management apps in COPD, including the investigation of a wearable vest [10], a multicomponent mobile health application [11] and the effect of self-monitoring oxygen saturation [12]. They found that patients use information about their oxygen values to track their health, make connections with their symptoms and judge when to contact healthcare providers [12]. They described a sense of security patients have with self-monitoring [11, 12].
This study adds further information on how technology may improve the care of people with COPD by helping them overcome issues that they face. People with COPD saw great potential for a wearable and an app to improve care through facilitating their self-management. It could help people understand their condition better, understand what to do when things got worse and notify them first when things were deteriorating. Importantly, patients did not see it as a method for others to manage their condition. In fact, they were concerned about the negative impact too much information would have on their healthcare providers. Different patients' perceptions of sharing data with healthcare providers highlight this tension. Patients may not want to overload their clinician with a lot of data or may be displaying the stoicism of patients with COPD that has been described previously [13]. But providing this data may be useful to clinicians in optimising their care. Further work is necessary to determine what, and how much, information is helpful to share with the healthcare team. Our study also raises the concern that this technology may increase the “sick” role, as patients will have heightened illness anxiety. While this hypervigilance has been described previously in patients with COPD, providing them with a wearable with near-continuous recordings may make it worse [14].
A limitation to our study was that the majority of the research team is interested in developing a wearable device for COPD patients. Preconceptions may have influenced data collection and analysis. We did use well-established methodological approaches (reflexivity, double-coding, discussions with a qualitative research expert) to minimise this potential for bias. In addition, our participants were drawn from an academic health science centre in a large urban setting, and their opinions may not reflect other demographic or socioeconomic groups or people who were not interested in participating in the study. Thus, it may not be generalisable to all patients with COPD. A larger prospective study would better determine who would benefit from this technology. However, we do think that the barriers to use (table 2) should be addressed, to make the technology appealing to the majority of patients with COPD.
Future research should incorporate these findings in the co-design of wearable technology with people with COPD. Involving people with COPD in the design will be crucial to ensure key components to aid self-management are effective and to ensure barriers are addressed as well. Further research is also necessary to understand how COPD healthcare providers would want to use wearable data and how they perceive it could improve the care of their patients with COPD.
In summary, patients perceive significant potential for wearables to help manage their condition. Of note, patients want to maintain control of the information, to make connections with the data, but also to be alerted when a possible exacerbation occurs. Some people with COPD were concerned about overloading their healthcare providers with the data while others wanted them to have their physiological data.
Acknowledgements
These data were previously presented at the Age-Well conference on October 16, 2018, in Vancouver, Canada.
Footnotes
Author contributions: R.C. Wu and T. Son had full access to all the data in the study, and take responsibility for the integrity of the data and accuracy of the analysis, including and especially any adverse effects. R.C. Wu, S. Ginsburg, A.S. Gershon and T. Son contributed substantially to the study design, data analysis and interpretation, and the writing of the manuscript. R.C. Wu confirms that the study objectives and procedures are honestly disclosed. Moreover, he has reviewed study execution data and confirms that procedures were followed to an extent that convinces all authors that the results are valid and generalisable to a population similar to that enrolled in the study.
Support statement: This study was supported by the Innovation Fund of the Alternative Funding Plan for the Academic Health Sciences Centres of Ontario as well as AGE-WELL NCE Inc. R.C. Wu is supported by an award from the Mak Pak Chiu and Mak-Soo Lai Hing Chair in General Internal Medicine, University of Toronto. Funding information for this article has been deposited with the Crossref Funder Registry.
Conflict of interest: R.C. Wu reports that he is the lead of a team that is actively trying to develop a wearable to aid in the self-management of patients with COPD. This includes a potential collaboration with Samsung Research America. They may be providing funding for his team to conduct a trial that enrolls patients to use a COPD app and a Samsung smartwatch. They have not provided any funding to date.
Conflict of interest: S. Ginsburg has nothing to disclose.
Conflict of interest: T. Son has nothing to disclose.
Conflict of interest: A.S. Gershon has nothing to disclose.
References
- 1.AARP. Health Innovation Frontiers: Untapped Market Opportunities for 50+ Washington, AARP; 2014. [Google Scholar]
- 2.Yañez AM, Guerrero D, Pérez de Alejo R, et al. Monitoring breathing rate at home allows early identification of COPD exacerbations. Chest 2012; 142: 1524–1529. [DOI] [PubMed] [Google Scholar]
- 3.Pedone C, Chiurco D, Scarlata S, et al. Efficacy of multiparametric telemonitoring on respiratory outcomes in elderly people with COPD: a randomized controlled trial. BMC Health Serv Res 2013; 13: 82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Effing T, Monninkhof EM, van der Valk PD, et al. Self-management education for patients with chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2007; 4: CD002990. [DOI] [PubMed] [Google Scholar]
- 5.Sobnath DD, Philip N, Kayyali R, et al. Features of a mobile support app for patients with chronic obstructive pulmonary disease: literature review and current applications. JMIR Mhealth Uhealth 2017; 5: e17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sanders C, Rogers A, Bowen R, et al. Exploring barriers to participation and adoption of telehealth and telecare within the Whole System Demonstrator trial: a qualitative study. BMC Health Serv Res 2012; 12: 220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wu R, Liaqat D, de Lara E, et al. Feasibility of using a smartwatch to intensively monitor patients with chronic obstructive pulmonary disease: prospective cohort study. JMIR Mhealth Uhealth 2018; 6: e10046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liaqat D, Wu R, Gershon AS, et al. Challenges with Real-World Smartwatch based Audio Monitoring. Paper presented at: WearSys'18: 4th ACM Workshop on Wearable Systems and Applications 2018; Munich, Germany.
- 9.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006; 3: 77–101. [Google Scholar]
- 10.Kayyali R, Savickas V, Spruit MA, et al. Qualitative investigation into a wearable system for chronic obstructive pulmonary disease: the stakeholders’ perspective. BMJ Open 2016; 6: e011657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Williams V, Price J, Hardinge M, et al. Using a mobile health application to support self-management in COPD: a qualitative study. Br J Gen Pract 2014; 64: e392–e400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Huniche L, Dinesen B, Nielsen C, et al. Patients’ use of self-monitored readings for managing everyday life with COPD: a qualitative study. Telemed J E Health 2013; 19: 396–402. [DOI] [PubMed] [Google Scholar]
- 13.Jones I, Kirby A, Ormiston P, et al. The needs of patients dying of chronic obstructive pulmonary disease in the community. Fam Pract 2004; 21: 310–313. [DOI] [PubMed] [Google Scholar]
- 14.Middlemass JB, Vos J, Siriwardena AN. Perceptions on use of home telemonitoring in patients with long term conditions – concordance with the Health Information Technology Acceptance Model: a qualitative collective case study. BMC Med Inform Decis Mak 2017; 17: 89. [DOI] [PMC free article] [PubMed] [Google Scholar]


