Abstract
In this ecological study, we examined the associations between state-level income inequality and pregnancy-related mortality among non-Hispanic (NH) black and NH white populations across the US. We estimated total population and race-specific 5-year pregnancy-related mortality ratios in each state based on national death and live birth records from 2011 to 2015. We obtained data on Gini coefficients for income inequality and population-level characteristics from the US Census American Community Survey. Poisson regression with robust standard errors estimated pregnancy-related mortality rate ratios (RR) and 95% confidence intervals (CI) associated with a one unit increase in income inequality overall and separately within black and white populations. Adjusted linear regression models estimated the associations between income inequality and magnitude of the absolute and relative racial inequity in pregnancy-related mortality within states. Across all states, increasing contemporaneous income inequality was associated with a 15% and 5-year lagged inequality with 14% increase in pregnancy-related mortality among black women (aRR = 1.15, 95% CI = 1.05; 1.25 and aRR = 1.14, 95% CI = 1.04; 1.24, respectively) after controlling for states’ racial compositions and socio-economic conditions. In addition, both lagged and contemporaneous income inequality were associated with larger absolute and relative racial inequities in pregnancy-related mortality. These findings highlight the role of contextual factors in contributing to pregnancy-related mortality among black women and the persistent racial inequity in maternal death in the US.
Keywords: Income inequality, Pregnancy-related mortality, Race, Health disparities
Highlights
-
•
Considerable racial disparities persist in reproductive health outcomes in the US.
-
•
Higher state-level income inequality was significantly associated with black but not white PRM.
-
•
State income inequality was also linked to increasing racal inequity in PRM across the US.
-
•
Contextual factors contribute significantly to black PRM and racial inequity in maternal death in the US.
1. Introduction and background
Since the mid-1950s, medical advances and improvements in maternal health care as well as education and overall standards of living in the US have drastically reduced incidence of maternal mortality. However, in the past 25 years, there has been no further reduction in maternal mortality and today the US has the highest maternal mortality ratio among developed countries (Kassebaum et al., 2016; WHO, 2016). Moreover, incidence of these deaths appears to be increasing (MacDorman, Declercq, Cabral, & Morton, 2016). While the increasing trend is due, at least in part, to improvements in identification and reporting of maternal deaths (Joseph et al., 2017), perhaps more distressing is the persistent, vast, and increasing mortality gap between Non-Hispanic (NH) black and all other women in the US (Creanga, Syverson, Seed, & Callaghan, 2017; Petersen et al., 2019). Nationally, from 2011 to 2015 the pregnancy-related mortality ratio among NH black women (42.8 deaths per 100,000 live births) was over 3 times higher than among NH whites (13 deaths per 100,000 live births) (CDC, 2019). There is an urgent and growing need to understand the reasons behind this vast inequity and examine broader society and structural conditions that potentially contribute to excess mortality among NH black women. Recent studies have begun to illuminate how social, political, economic, and environmental conditions contribute to racial/ethnic disparities in health (Bailey et al., 2017; White, Haas, & Williams, 2012; Williams & Jackson, 2005); however, little is known about the influence of social and contextual factors on maternal mortality among different racial/ethnic groups in the US.
Income inequality, the degree of unequal distribution of income within a population, has been a growing public health concern and an important ecological factor hypothesized to adversely affect health (Kawachi & Kennedy, 1999; Pickett & Wilkinson, 2015). Income inequality has been also on the rise in the US – between 1980 and 2017, the after-tax income inequality increased by 19.6% (Fontenot, Semega, & Kollar, 2018). While this dramatic surge has been driven largely by rising income among the wealthiest 10%, since 2001, the real income among the poor and middle-class Americans has barely changed or even declined (Bor, Cohen, & Galea, 2017). In addition, a recent report found that unequal income growth has been accompanied by considerable variations in income inequality observed across the states (Sommeiller & Price, 2018). While effects of area-specific income inequality on population and individual health outcomes have been demonstrated (Kondo et al., 2012; Lochner, Pamuk, Makuc, Kennedy, & Kawachi, 2001; Lynch, Smith, Kaplan, & House, 2000; Subramanian & Kawachi, 2006; Zimmerman & Bell, 2006), this has not been applied to understanding racial health inequities and adverse maternal outcomes. The present study addresses this gap by examining the association between the state-level income inequality and pregnancy-related mortality (PRM) among NH black and NH white populations across the US (black and white, hereafter).
1.1. Pregnancy-related mortality in the U.S
Maternal mortality is an important health status indicator, but remains unacceptably high in the US, and is even increasing. The US maternal mortality ratio (MMR) – defined as the number of maternal deaths per 100,000 live births – increased from 16.9 to 26.4 per 100,000 live births from 1990 to 2015, while the global MMR declined by 30% (Kassebaum et al., 2016). Similarly, the PRM ratio – defined as maternal death during pregnancy or within 1 year from any cause related to or aggravated by the pregnancy or its management (CDC, 2019) – has more than doubled from 7.2 deaths per 100,000 live births in 1987 to 17.2 deaths per 100,000 live births in 2011–2015 (Petersen et al., 2019). While this increase may be partially attributed to enhanced surveillance of PRM data and past underestimation of maternal deaths (see Joseph et al., 2017), there remains a legitimately increasing trend in US maternal death in the opposite direction than the international trend (MacDorman et al., 2016).
Pregnancy-related deaths result from direct causes including hemorrhage, infections, hypertensive disorders of pregnancy, and obstructed labor (Berg, Callaghan, Syverson, & Henderson, 2010; Creanga et al., 2015; Khan, Wojdyla, Say, Gulmezoglu, & Van Look, 2006). Indirect causes represent over 30% of the total PRM and include pre-existing or concurrent diseases (e.g. cardiovascular conditions, cardiomyopathy) that are not complications of pregnancy but that are aggravated during pregnancy (Petersen et al., 2019). In addition, over 50% of maternal deaths happen after a live birth and another approximately 30% occur during pregnancy and up to 20% occur on the day of delivery (Creanga et al., 2017; Petersen et al., 2019). Among the established individual-level risk factors for PRM are older maternal age, low educational attainment, obesity, and chronic health conditions (Callaghan, 2012; King, 2012). A recent study on population-level risk factors found that the increase in state-level maternal mortality could be attributed to the proportion of women of childbearing age who were obese (31%), did not have a high school diploma (5.3%), and the proportion of births to women with diabetes (17%), who attended fewer than 10 prenatal visits (4.9%), and were African American (2%) (Nelson, Moniz, & Davis, 2018).
Considerable racial disparities persist in reproductive health outcomes in the US. Research has shown that black women are at over 3 times higher risk of dying from pregnancy complications than white women (Creanga et al., 2015; Petersen et al., 2019). Black women are also more likely to give birth to low-birthweight infants, and their newborns experience higher infant death rates not associated with biological differences, even after controlling for socioeconomic factors (Rosenthal & Lobel, 2011). The literature on maternal health posits that structural inequities and racial discrimination are sources of chronic stress among black women and partly responsible for the persistence of racial health inequities (Dominguez, 2008; Wallace, Crear-Perry, Richardson, Tarver, & Theall, 2017; 2015). Overall, this literature highlights the need to better understand the societal contexts into which women are born, live, and reproduce, and to critically examine the role of social and structural determinants of maternal health in order to institute systemic changes needed to reduce the incidence of maternal death and advance population health equity (Berg et al., 2010; Creanga et al., 2017; Nelson et al., 2018).
1.2. Income inequality and health
Over the past decades, the impact of area-specific income inequality on individual and aggregate health outcomes has been examined (see, for a review, Bor et al., 2017; Kondo et al., 2012; Pickett & Wilkinson, 2015). Multilevel studies found significant associations between area-level income inequality and life expectancy (Kaplan, Pamuk, Lynch, Cohen, & Balfour, 1996; Rasella, Aquino, & Barreto, 2013), mental illness (Cifuentes et al., 2008), self-reported overall health (Zimmerman & Bell, 2006), and infant mortality (Olson, Diekema, Elliott, & Renier, 2010; Wallace, Mendola, Chen, Hwang, & Grantz, 2016). Detrimental effects of higher income inequality are also well established on aggregate health outcomes such as self-rated health and prevalence of depressive symptoms (Kahn, Wise, Kennedy, & Kawachi, 2000; Kondo et al., 2009), life expectancy or mortality risk (Hill & Jorgenson, 2018; Lochner et al., 2001), and prevalence and more adverse profile of health-related risk behaviors (Diez-Roux, Link, & Northridge, 2000). However, research is not unanimous as some studies have failed to detect the effects of income inequality on health outcomes (see e.g. Lorgelly & Lindley, 2008; Mellor & Milyo, 2003). Reviews indicate that stronger and more consistent health effects of income inequality appear at larger geographical scales such as country or state as opposed to metropolitan statistical areas (MSA) or counties (Kondo et al., 2009; Subramanian & Kawachi, 2004).
Several pathways have been proposed to explain the relationship between income inequality and health, including the mediating roles of social capital, individual comparisons, and macro-level policies and public spending (Kawachi & Kennedy, 1999; Pickett & Wilkinson, 2015). Psychosocial pathways posit that higher income inequality erodes social capital and trust which in turn negatively affects health through a political climate that is less supportive of policies that aim to sustain public health. Alternatively, a neo-materialist perspective postulates that the relationship between income inequality and health is contingent on public underinvestment in social and health services which in turn impedes individuals’ access to educational and employment opportunities, material goods and health care (Lynch et al., 2000). Finally, higher income inequality may cause increased social comparisons and resulting frustrations (Kawachi & Kennedy, 1999). Employing varying units of geographical aggregation, numerous studies have tested these pathways providing ample explanatory evidence through which area-level income inequality affect individual and population health (see Pickett & Wilkinson, 2015 for a review and discussion).
Health effects have also been hypothesized to depend on prolonged exposure of unequal distribution of income within a population, suggesting that the impact of state-level income inequality is likely to manifest after several years rather than instantaneously and ought to be empirically tested in lagged effect models (Kondo et al., 2012; Mellor & Milyo, 2003; Subramanian & Kawachi, 2004). For instance, a recent study found significant associations between two-year lagged state-level income inequality and black infant mortality as well as racial inequities in infant mortality rates from 1992 to 2007 (Siddiqi, Jones, Bruce, & Erwin, 2016). Given the crucial importance of the socioeconomic conditions within the society as young women enter family planning stages, we examine the delayed association of income inequality on PRM in the US.
1.3. Income inequality and maternal health
Socioeconomic inequality and state-level policies may play a larger role in women's health as compared to men's health as they shape access to services and resources (i.e. prenatal care, affordable housing, children's health care, family leave) that are especially central in women's lives (Montez, Zajacova, & Hayward, 2016; Stafford, Cummins, Macintyre, Ellaway, & Marmot, 2005). Prior studies have found significant associations between area-level socioeconomic conditions and women's BMI (Robert & Reither, 2004), self-rated health (Stafford et al., 2005), increased levels of health-related risk behaviors (Diez-Roux et al., 2000), and mortality (Montez et al., 2016). A recent systematic review reported greater impact of income inequality on mental health among women suggesting that women living in the context of higher income inequality are at a higher risk and prevalence of mental illnesses than men (Patel et al., 2018). Overall, women are more vulnerable to the adverse processes related to income inequality and the unequitable distribution of public resources as they are more likely than men to be socioeconomically-disadvantaged, raise children, and use health care systems (Montez et al., 2016).
Very few studies have examined the effect of income inequality on maternal and birth outcomes. A cross-sectional study in the US found that high state-level income inequality was associated with an increased risk of poor mental and physical health among women with young children (Kahn et al., 2000). In addition, low-income women living in states with high income inequality had a higher risk of developing depressive symptoms and reporting fair/poor health as compared to low-income women residing in the states with low income inequality. Living in high or medium inequality areas at the time of birth was associated with a higher risk of preterm (Huynh, Parker, Harper, Pamuk, & Schoendorf, 2005) and low weight birth (Nkansah-Amankra, Dhawain, Hussey, & Luchok, 2010). A recent US study also found that living in a state when income inequality expanded over the course of the year leading up to delivery increased preterm birth risk regardless of the degree of initial inequality and controlling for simultaneous changes in absolute income, poverty, and unemployment levels (Wallace et al., 2016).
Yet, contextual influences on maternal mortality are understudied. Globally, several ecological studies have found associations between maternal mortality and women's education, health insurance coverage, health expenditure per person, and poverty (Cárdenas-Cárdenas et al., 2015; Koch et al., 2012; Muldoon et al., 2011). However, most studies that have investigated contextual socioeconomic factors in low- and middle- income countries overlooked unequal distribution of income as an important explanatory factor (see, for instance, Alvarez, Gil, Hernández, & Gil, 2009; Muldoon et al., 2011) or failed to find a relationship between area-level income inequality and maternal mortality (Tajik et al., 2012). In addition, while prolonged experiences of socioeconomic context may have a more robust effect on maternal and birth outcomes (Lu & Halfon, 2003; Wallace et al., 2016), no studies have investigated delayed associations.
1.4. Study aims
The objectives guiding this study were two-fold: 1) to examine the associations between state-level income inequality and PRM among black and white populations across the US, and 2) to estimate the association between state income inequality and both absolute and relative racial inequities in PRM. Drawing on the prior evidence outlining more pronounced effects of income inequality on women's health, we hypothesized that incidence of PRM would be higher in states with larger income inequality. Additionally, we argue that black women are particularly vulnerable to the unequal income distribution as they are more likely to belong to lower socioeconomic groups and live in resource-limited environments that have harmful exposures and lack opportunities to achieve and maintain health. Moreover, their disproportionate representation in the lower end of the distribution relative to whites is a manifestation of structural racism – the purposeful social and political processes that perpetuate racial oppression of non-white communities and an increasingly hypothesized driver of population health inequities (Bailey et al., 2017; Krieger et al., 2016). Thus, we anticipate the adverse impact of income inequality to be more prominent among the black population. With respect to racial inequities in PRM, we hypothesized that the absolute and relative inequities in PRM would be larger in states with higher income inequality. Finally, we hypothesized that the prolonged exposure to income inequality would be detrimental to women's health as the pathways through which state income disparities are assumed to shape population health involve some persistent exposure to the detrimental climate/context (e.g. limited resources) that in turn may cause psychosocial stress and lead to adverse health outcomes. Therefore, we hypothesized that our study outcomes would be associated with both contemporaneous and lagged income inequality.
2. Methods
2.1. Data sources
The estimates for 2011–2015 PRM ratios across all 50 states and the District of Columbia were derived from annual mortality and natality files, data provided by the National Center for Health Statistics (NCHS). We identified all pregnancy-related deaths based on ICD-10 code for underlying cause of death in Chapter XV [Pregnancy, childbirth and the puerperium (O00–O99)]. The natality file contained all birth certificates for infants born in the given calendar year, for the purposes of computing PRM ratios (pregnancy-related deaths per 100,000 live births). The data contain geographic identifiers for maternal state of residence (Federal Information Processing System codes) for all 50 states and the District of Columbia. Contextual data, including 5-year estimates of state-level Gini coefficients, median household income, the percentage of unemployed population, the percentage of population with BA or higher degree, and the percentage of the black population in each state, were retrieved from the US Census Bureau's American Community Survey (ACS). As de-identified data, this study was exempt from the ethics approval process.
2.2. Measures
The outcome of interest was pregnancy-related mortality, defined as a death while pregnant or within 1 year following the end of a pregnancy, from any cause related to or aggravated by the pregnancy or its management (CDC, 2019). Due to the relative rarity of maternal deaths annually, we computed the 5-year (2011–2015) pregnancy-related mortality ratios (deaths per 100,000 live births) for the total population, and separately for black and white women in each state. In order to ensure stable ratios estimation, total population and race-specific PRM were calculated only in states with a minimum of 5 deaths within the 5-year period. As a result, Alaska, Delaware, and DC were excluded from the analysis of the white population, and 20 states (Alaska, Delaware, Hawaii, Idaho, Maine, Massachusetts, Montana, Nebraska, Nevada, New Hampshire, New Mexico, North Dakota, Oregon, Rhode Island, South Dakota, Utah, Vermont, and Wyoming) were excluded from the analysis of the black population. Analyses for the total, white, and black populations were conducted with the samples of 51, 48, and 31 states, respectively. In addition, absolute (black PRM - white PRM) and relative (black PRM/white PRM) racial inequity in PRM were calculated in the 30 states with sufficient sizes of each racial group.
The Gini coefficient is a measure of statistical dispersion that is frequently used to describe the distribution of resources in a population and is an indicator of income inequality. It ranges from 0 to 1 with the lower value indicating more equitable distribution of income. We used two measures: 5-year average estimate of Gini coefficients for 2011–2015 (contemporaneous income inequality) and averaged 5-year estimate of Gini coefficient for 2006–2010 (approximately a 5-year lag). We scaled the Gini coefficients to a 0–100 range.
Covariates that were potential confounders were included in adjusted models: the ACS 2011–2015 5-year average of state-level median income (to isolate the independent effect of relative income distribution represented by the Gini coefficient); the percentage of the black population (only used in the adjusted models for the total population PRM and to predict racial inequities in PRM); percent college graduates, and percent unemployed population.
2.3. Statistical analysis
We conducted descriptive analyses to characterize the variation of state-level income inequality and PRM (for the total population and separately among black and white populations) across the US. We also plotted trends over time in income inequality (annual estimates of Gini, 2006–2015) and PRM for the total population and stratified by race (5-year estimates, 2009–2015).
We fitted separate models for the total PRM, white PRM, black PRM, absolute PRM inequities, and relative PRM inequities. First, modified Poisson regression with robust standard errors to account for clustering within states estimated the unadjusted association between income inequality (lagged and contemporaneous, separately) and PRM for the total state population. Second, we estimated rate ratios (RR) and 95% confidence intervals (CI) controlling for the confounders listed above. We fitted separate models to examine the adjusted effects of the lagged and contemporaneous income inequality, then ran race-stratified models, adjusting for the same set of covariates (excluding the percentage of black population in the state). In testing the effects of contemporaneous income inequality across these models, we also adjusted for the change in income inequality over time (i.e. the difference between contemporaneous and lagged Gini coefficients).
Finally, we fitted a set of linear regression models to estimate the associations between income inequality and the absolute (black-white) and relative (black/white) PRM rate ratio, adjusting for state median household income, the size of the black population, percent of college graduates, unemployment, and the change in income inequality over time. Again, we ran separate models to examine the adjusted effects of the lagged and contemporaneous income inequality. These models were weighted by the total number of live births in each state to account for the varying contribution of each state by population size to the relative or absolute racial inequity (the dependent variable). All statistical analyses were performed with SAS 9.4.
3. Results
3.1. Descriptive statistics
From 2011 to 2015, overall PRM averaged almost 26 deaths per 100,000 live births across all 50 states and DC (see Table 1). Nationally, PRM among black women averaged 61 per 100,000 live births (the estimate among white women was 23.3 per 100,000 live births) and exceeded the estimate among whites in every state by 2.5-fold, on average. In addition, the absolute difference in PRM between blacks and whites was nearly 35 deaths per 100,000 live births, although there were considerable variations in the absolute and relative racial equities in PRM across the states.
Table 1.
Mean and distribution of pregnancy-related mortality rates, state-level income inequality and state-level characteristics, 2011–2015.
| Mean (SD) | Min | Max | IQR | |
|---|---|---|---|---|
| PRM per 100,000 live births (N = 51) | 25.6 (11.3) | 6.9 | 56.9 | 12.4 |
| NH black PRM per 100,000 live births (N = 31)a | 61.0 | 24.1 | 169.7 | 35.2 |
| (27.6) | ||||
| NH white PRM per 100,000 live births (N = 48) a | 23.3 | 5.8 | 53.2 | 9.2 |
| (10.1) | ||||
| Absolute racial inequity in PRM (N = 30) | 34.8 (21.2) | 4.2 | 123.2 | 23.7 |
| Relative racial inequity in PRM (N = 30) | 2.5 (0.8) | 1.2 | 4.6 | 2.9 |
| Lagged income inequality (Gini coefficient 2006–2010 estimate) | 45.2 (2.2) | 41.2 | 53.5 | 2.9 |
| Contemporaneous income inequality (Gini coefficient 2011–2015 estimate) | 46.2 (2.1) | 41.8 | 53.2 | 2.8 |
| State median household income, 2015 inflation-adjusted dollars | 54,636 (9157) | 39,665 | 74,551 | 13,220 |
| NH Black population (% of state population) | 12.3 (10.9) | 10.9 | 48.9 | 16.1 |
| College graduates (% of state population age 25 and older) | 29.5 (6.1) | 19.2 | 54.6 | 6.4 |
| Unemployment (% of state civilian population age 16 and older) | 7.6 (1.7) | 2.9 | 10.5 | 2.8 |
b Racial inequities in PRM were calculated for the states that had PRM ratios for both black and white populations.
aBlack PRM ratios were calculated only in states with a minimum of 5 black maternal deaths within the 5-year period, and white PRM ratios were calculated only in states with a minimum of 5 white maternal deaths within the same period.
The average estimates of income inequality, both contemporaneous and lagged, are within the 45–47 range and are more comparable to Gini coefficients observed among South American countries (e.g. Ecuador, Chile, Costa Rica) than those of more advanced economies (e.g. Scandinavian or Western European countries) (World Bank, 2017). Contemporaneous and lagged income inequality varied across the states ranging from the lowest Gini coefficient of 41.8 (average of 2011–2015) and 41.2 (average of 2006–2010) in Alaska and the highest of 53.2 (average of 2011–2015) and 53.5 (average of 2006–2010) in DC.
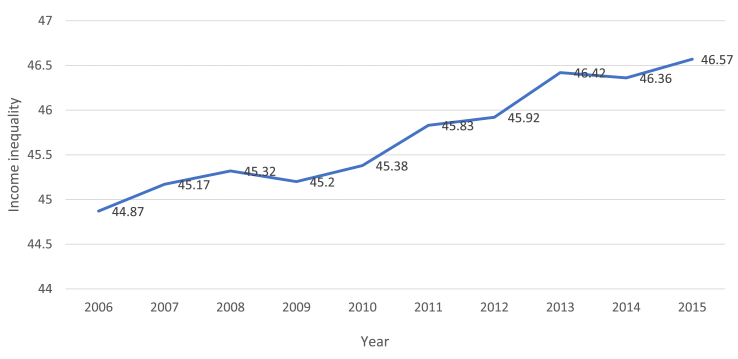
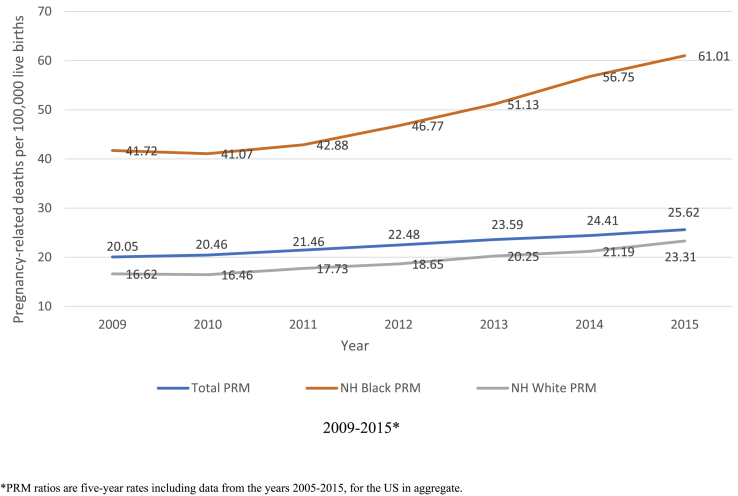
Income inequality fluctuates over the period 2006–2015 but has a discernible overall upward trend (Fig. 1), and both the overall and white PRM ratios increased relatively slightly over this period (Fig. 2). The most striking increase is seen in black PRM ratios where the 5-year estimates increased by 46% from nearly 42 maternal deaths per 100,000 live births in 2006–2009 to 61 in 2011–2015.
Fig. 1.
Trends in income inequality in the US, 2006–2015.
Fig. 2.
Trends in overall and race-stratified pregnancy-related mortality (PRM) in the US, 2009–2015*.
3.2. Associations between the lagged and contemporaneous state-level income inequality and PRM among the total, NH black and NH white populations
There was no significant association between income inequality and PRM for the total population (Table 2), but the association was significant among black women. Increasing income inequality was associated with 14% (the 5-year lag) or 15% increase (contemporaneous) in PRM among black women (aRR = 1.14, 95% CI = 1.04; 1.24 and aRR = 1.15, 95% CI = 1.05; 1.24, respectively), independent of covariates. None of the income inequality measures were significantly associated with PRM among white women.
Table 2.
Overall and race-specific PRM rate ratios (RR) and 95% confidence intervals (CI) for associations with income inequality indicators.
| Overall PRM |
Black PRM |
White PRM |
||||
|---|---|---|---|---|---|---|
| RR | 95% CI | RR | 95% CI | RR | 95% CI | |
| Lagged income inequality | 1.03 | (0.95; 1.10) | 1.14a | (1.04; 1.24) | 1.04 | (0.96; 1.14) |
| Contemporaneous income inequality | 1.06 | (0.99; 1.13) | 1.15 a | (1.05; 1.25) | 1.08 | (0.98; 1.18) |
| State median income | 1.01 | (0.73; 1.39) | 1.16 | (0.70; 1.96) | 1.12 | (0.75; 1.67) |
| NH Black population | 1.03b | (1.01; 1.04) | n/a | n/a | n/a | n/a |
| College graduates | 0.97 | (0.93; 1.02) | 0.98 | (0.91; 1.05) | 0.95 | (0.89; 1.02) |
| Unemployment | 0.93 | (0.86; 1.00) | 1.01 | (0.87; 1.17) | 0.98 | (0.89; 1.07) |
p<.05.
p < 0.01.
3.3. Associations between the lagged and contemporaneous state-level income inequality and the absolute and relative racial equity in PRM
In addition, both lagged and contemporaneous income inequality were associated with increases in the absolute and relative racial inequities in PRM (see Table 3). A one-unit increase in lagged income inequality was associated with an additional 5.7 per 100,000 excess black deaths and a 20% increase in the excess risk experienced by black women relative to whites (absolute PRM difference beta = 5.7, 95%CI = 2.5, 8.9; relative PRM ratio beta = 0.20, 95% CI = 0.1, 0.3). Similarly, a one-unit increase in contemporaneous income inequality was associated with an additional 5.3 per 100,000 black deaths and a 14% increase in the excess risk experienced by black women relative to whites (absolute PRM difference beta = 5.3, 95%CI = 1.8; 8.9; relative PRM ratio beta = 0.14, 95% CI = 0.00; 0.28).
Table 3.
Linear regression coefficients (B) and 95% confidence interval (CI) for the associations between income inequality indicators and the absolute and relative racial inequity in PRM.
| Absolute inequities in PRM (black-white PRM difference) |
Relative inequities in PRM (black/white PRM ratio) |
|||
|---|---|---|---|---|
| B | 95% CI | B | 95% CI | |
| Lagged income inequality | 5.7b | (2.47; 8.98) | 0.20 a | (0.07; 0.32) |
| Contemporaneous income inequality | 5.34a | (1.78; 8.89) | 0.14 a | (0.00; 0.28) |
| State median income | 26.33 a | (0.62; 52.04) | 0.42 | (-0.16; 0.99) |
| NH Black population | 0.13 | (-0.63; 0.88) | −0.01 | (-0.04; 0.02) |
| College graduates | −3.71 | (-6.72; −0.70) | −0.02 | (-0.13; 0.09) |
| Unemployment | −2.17 | (-6.09; 1.74) | 0.13 | (-0.04; 0.29) |
p<.05.
p < 0.01.
4. Discussion
Pregnancy-related mortality remains a significant concern in the US and experience of maternal death divides the population along racial lines. Income inequality has been rising in the US at a rate highest among the economically developed countries in the north (OECD, 2017). To our knowledge, this was one of the first studies to examine the associations between state-level income inequality and pregnancy-related mortality and racial inequity in maternal death in the US. Using vital records data from 2011 to 2015, we found that state-level income inequality – both contemporaneous and lagged – was significantly associated with black but not white PRM and contributed to increasing racial inequity in PRM across the US.
The lack of significant association between income inequality and PRM among white women suggests that income inequality may contribute to the persisting racial inequity in maternal death. Our study provides important evidence on how structural and contextual inequalities shape health outcomes across racial lines and challenges prior studies positing that income inequality has a “social pollution” effect on population health outcomes as it exerts a comparable contextual effect across all population sub-groups (Subramanian & Kawachi, 2004; 2006). Our findings add to the literature by showing that black women may be particularly vulnerable to the adverse consequences of unequal economic conditions. In the US, black women face greater structural constraints, limited opportunities, and psychosocial stresses induced by individual and institutional discrimination and structural racism that impinge on their lived experiences, circumstances and health compared to white women (Mendez, Hogan, & Culhane, 2014; Williams, 2008). Disadvantageous social conditions driven by structural racism – such as unequal distribution of income and resources – force many black women to live in poor and segregated neighborhood with low-quality housing, high crime rates, lack of health resources and harmful environmental exposures (Bailey et al., 2017). In addition, research has shown that states with higher income inequality have higher levels of racial/ethnic prejudice (Connor, Sarafidis, Zyphur, Keltner, & Chen, 2019; Kennedy, Kawachi, Lochner, Jones, & Prothrow-Stith, 1997). Further investigation of the intricate links between income inequality and structural racism is crucial to elucidate the pathways through which unequal income distribution may cause detrimental health effects among black women and engender population health inequities.
Moreover, our findings highlight the importance of considering the relative distribution of resources, and the problematic economic, political, and social relationships that underlie the unequal distribution across a population in understanding racial health inequities (Krieger et al., 2016). It may therefore be not only the degree to which black populations are deprived of material resources as a result of structural racism, but the degree to which whites are privileged with greater access to resources, and the extent of the gap between the two that perpetuates disproportionate mortality among black women. Our findings thus suggest the harmful health effects resulting from one's place in the social hierarchy (Wilkinson, 1997) and highlight the need to employ measures that determine health effects of societal distribution of concentrations of extreme wealth and deprivation (Krieger et al., 2016).
Persisting racial inequities in maternal death and the differential impact of income inequality on PRM suggests that causes of health disparities may lie beyond the scope of individual characteristics or behaviors and thus improving the health of pregnant women will need to extend beyond addressing medical conditions to optimizing social determinants of their health. Greater income inequality coexists with other material deprivations – including lack of investment in housing, education and public transport, and limited access of healthcare and healthy foods – that are relevant to health (Lynch et al., 2000). Such community and societal conditions have been recognized in the recent data from 13 state maternal mortality review committees (MMRCs) as important contributing factors related to PRM (Petersen et al., 2019). Identifying policy-amenable conditions and implementing social and public health policies that reduce racial inequities which systematically disadvantage black women could play an important role in national attempts to reduce and eliminate the racial disparities in and overall maternal mortality.
Our study found evidence of a five-year lagged effect of income inequality suggesting that limiting investigations of income inequality and health to only contemporaneous measures may overlook the importance of prolonged exposure and fail to demonstrate evidence of a relationship that requires sufficient time to detect (Blakely, Kennedy, Glass, & Kawachi, 2000). This also highlights the value of utilizing the life-course approach in further investigating how structural inequalities may shape women's contexts that eventually contributes to reduced health (Bernstein & Merkatz, 2010; Lu & Halfon, 2003). To properly determine whether the prolonged exposure to income inequality results in cumulative disadvantage that in turn affects maternal health requires considering multiple lagged effects of structural inequities spanning through women's early and formative years. While our study used a cross-sectional ecological design, longitudinal or panel data are required to better understand the dynamics of state income inequality and health and to identify income-related health inequalities resulting from persistent social disadvantage.
Finally, our findings support previous research that has reported significant associations between income inequality and health on a state level (e.g. Kondo et al., 2012). Importantly, our study provides compelling evidence to include race-stratified models and between-race measures when investigating associations between health and societal conditions and structural factors related to resource distribution (also see Wallace et al., 2017). Future studies should examine the effects of other societal conditions – including indicators of structural racism – on adverse maternal health outcomes. The joint effects of structural racism and areal-level income inequality require particular attention as higher levels of co-occurring racial and socioeconomic inequality have been shown to increase the risk of adverse birth outcomes (Wallace, Mendola, Liu, & Grantz, 2015). In addition, while it was beyond the scope of the present study to examine the potential pathways explaining the association between income inequality and maternal mortality, future research should examine the role of institutional and political mechanisms (e.g. social spending across the US or reproductive health policies) as well as theoretically viable psychosocial factors (e.g. racial bias, chronic stress, social capital) in mediating the relationship between socioeconomic inequality and maternal health.
Our study has several limitations. First, we have relied on vital statistics to measure PRM, which may include misclassification of some cases where incorrect ICD-10 code was assigned for underlying cause of death. Moreover, variation in implementation of enhanced surveillance of maternal death (gradual adoption of the 2003 update to the US Standard Certificate of Death, including the pregnancy status checkbox) may have resulted in differing degrees of case misclassification across states and years. In response to rising concern about maternal death, maternal mortality review committees have been mobilizing in some (but not all) states across the country in order to verify and confirm cases of pregnancy-related death; however, until these data become comprehensive and are made available for research purposes, national vital records remain the only national source of population-level data on maternal death. In addition, given that PRM is a relatively rare event, our analysis included 5-year estimates of this measure and excluded states with a fewer than 5 deaths within the 5-year period (which resulted in data on black PRM from only 31 states). However, this overcomes the limitation of large variation in unstable rates based on small numbers of cases within a relatively small population. Second, we conducted the analysis at the state-level, a geographic unit of analysis that does not capture local-area variation. Nonetheless, our findings have relevant implications for policy and resource allocation decisions that typically occur at the state-level. Third, while multi-level, longitudinal and panel analysis would allow for exploration of associations with a causal framework, we fit cross-sectional pooled models in order to increase the precision of our estimates and to minimize heterogeneity bias. In addition, while the Gini coefficient is one of the most commonly utilized measures of income inequality, future studies may consider employing different and/or multiple measures of income inequality, e.g. Atkinson, Theil, Robin Hood indices as well as income share measures. Finally, there may be additional state-level factors associated with both income inequality and PRM that we were unable to control for, and thus we acknowledge the possibility of residual confounding.
5. Conclusions
Although pregnancy-related mortality has increased in the US, there is a dearth of research that explores a link between state-level socio-economic inequalities and PRM in the country. This study is the first to examine the contemporaneous and lagged effects of state-level income inequality on PRM. It provides evidence regarding the importance of the state-level as an influential context for racial inequities in PRM and finds that unequal income distribution can be particularly harmful to black women's health. Efforts to reduce maternal death in the US should continue to expand beyond individual- and clinical-level risk factors to explore the harmful contexts in which all women live, with a particular focus on women from racially-oppressed groups who continue to experience broad social and health inequities. Implementing a set of federal, state and local policies that remediate increasing trends in income inequality in the US may begin to address the underlying structural factors that cause these disparities and advance maternal population health equity.
Ethics approval: not required
Analysis presented in the manuscript used de-identified secondary data and was exempt from institutional review board approval.
Acknowledgement
Financial support and role of the funding source This work was supported in part by the Eunice Kennedy Shriver National Institute of Child Health and Human Development grant number R01HD092653. Its contents are solely the responsibility of the authors and do not necessarily represent the official position of National Institutes of Health. The funder had no involvement in the study design, analysis, or interpretation of data, writing of the report, or the decision to submit the article for publication.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ssmph.2019.100477.
Contributor Information
Dovile Vilda, Email: dvilda@tulane.edu.
Maeve Wallace, Email: mwallace@tulane.edu.
Lauren Dyer, Email: ldyer3@tulane.edu.
Emily Harville, Email: eharvill@tulane.edu.
Katherine Theall, Email: ktheall@tulane.edu.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Alvarez J.L., Gil R., Hernández V., Gil A. Factors associated with maternal mortality in Sub-Saharan Africa: An ecological study. BMC Public Health. 2009;9(1):462. doi: 10.1186/1471-2458-9-462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bailey Z.D., Krieger N., Agenor M., Graves J., Linos N., Bassett M.T. Structural racism and health inequities in the USA: Evidence and interventions. The Lancet. 2017;389(10077):1453–1463. doi: 10.1016/S0140-6736(17)30569-X. [DOI] [PubMed] [Google Scholar]
- Berg C.J., Callaghan W.M., Syverson C., Henderson Z. Pregnancy-related mortality in the United States, 1998 to 2005. Obstetrics & Gynecology. 2010;116(6):1302–1309. doi: 10.1097/AOG.0b013e3181fdfb11. [DOI] [PubMed] [Google Scholar]
- Bernstein P.S., Merkatz I.R. A life course perspective on women's reproductive health and the outcome of pregnancy. Journal of Women's Health. 2010;19(3):555–560. doi: 10.1089/jwh.2009.1397. [DOI] [PubMed] [Google Scholar]
- Blakely T.A., Kennedy B.P., Glass R., Kawachi I. What is the lag time between income inequality and health status? Journal of Epidemiology & Community Health. 2000;54(4):318. doi: 10.1136/jech.54.4.318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bor J., Cohen G.H., Galea S. Population health in an era of rising income inequality: USA, 1980–2015. The Lancet. 2017;389(10077):1475–1490. doi: 10.1016/S0140-6736(17)30571-8. [DOI] [PubMed] [Google Scholar]
- Callaghan W.M. Overview of maternal mortality in the United States. Seminars in Perinatology. 2012;36(1):2–6. doi: 10.1053/j.semperi.2011.09.002. [DOI] [PubMed] [Google Scholar]
- Cárdenas-Cárdenas L.M., Cotes-Cantillo K., Chaparro-Narvaez P.E., Fernandez-Nino J.A., Paternina-Caicedo A., Castaneda-Orjuela C. Maternal mortality in Colombia in 2011: A two level ecological study. PLoS One. 2015;10(3) doi: 10.1371/journal.pone.0118944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CDC (Centers for Disease Control and Prevention) Pregnancy-related deaths. 2019. http://www.cdc.gov/reproductivehealth/maternalinfanthealth/pregnancy-relatedmortality.htm Retrieved from.
- Cifuentes M., G S., S T., R G., D K., Punnett L. The association of major depressive episodes with income inequality and the human development index. Social Science & Medicine. 2008;67(4):529–539. doi: 10.1016/j.socscimed.2008.04.003. [DOI] [PubMed] [Google Scholar]
- Connor P., Sarafidis V., Zyphur M.J., Keltner D., Chen S. Income inequality and white-on-black racial bias in the United States: Evidence from project implicit and google trends. Psychological Science. 2019;30(2):205–222. doi: 10.1177/0956797618815441. [DOI] [PubMed] [Google Scholar]
- Creanga A.A., Berg C., Syverson C., Seed K., Bruce F., Callaghan W.M. Pregnancy-related mortality in the United States, 2006-2010. Obstetrics & Gynecology. 2015;125(1):5–12. doi: 10.1097/AOG.0000000000000564. [DOI] [PubMed] [Google Scholar]
- Creanga A.A., Syverson C., Seed K., Callaghan W.M. Pregnancy-related mortality in the United States, 2011-2013. Obstetrics & Gynecology. 2017;130(2):366–373. doi: 10.1097/AOG.0000000000002114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diez-Roux A.V., Link B.G., Northridge M.E. A multilevel analysis of income inequality and cardiovascular disease risk factors. Social Science & Medicine. 2000;50(5):673–687. doi: 10.1016/s0277-9536(99)00320-2. [DOI] [PubMed] [Google Scholar]
- Dominguez T.P. Race, racism, and racial disparities in adverse birth outcomes. Clinical Obstetrics and Gynecology. 2008;51(2):360–370. doi: 10.1097/GRF.0b013e31816f28de. [DOI] [PubMed] [Google Scholar]
- Fontenot K., Semega J., Kollar M. P6Vols. 0–263. U.S. Government Printing Office; Washington, DC: 2018. (Income and poverty in the United States: 2017). [Google Scholar]
- Hill T.D., Jorgenson A. Bring out your dead!: A study of income inequality and life expectancy in the United States, 2000-2010. Health & Place. 2018;49:1–6. doi: 10.1016/j.healthplace.2017.11.001. [DOI] [PubMed] [Google Scholar]
- Huynh M., Parker J.D., Harper S., Pamuk E., Schoendorf K.C. Contextual effect of income inequality on birth outcomes. International Journal of Epidemiology. 2005;34(4):888–895. doi: 10.1093/ije/dyi092. [DOI] [PubMed] [Google Scholar]
- Joseph K.S., Lisonkova S., Muraca G.M., Razaz N., Sabr Y., Mehrabadi A. Factors underlying the temporal increase in maternal mortality in the United States. Obstetrics & Gynecology. 2017;129(1):91–100. doi: 10.1097/AOG.0000000000001810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahn R.S., Wise P.H., Kennedy B.P., Kawachi I. State income inequality, household income, and maternal mental and physical health: Cross sectional national survey. BMJ. 2000;321(7272):1311–1315. doi: 10.1136/bmj.321.7272.1311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaplan G.A., Pamuk E.R., Lynch J.W., Cohen R.D., Balfour J.L. Inequality in income and mortality in the United States: Analysis of mortality and potential pathways. BMJ. 1996;312(7037):999–1003. doi: 10.1136/bmj.312.7037.999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kassebaum N.J., Bertozzi-Villa A., Coggeshall M.S., Shackelford K.A., Steiner C., Heuton K.R.…Lozano R. Global, regional, and national levels and causes of maternal mortality during 1990-2013: A systematic analysis for the global burden of disease study 2015. The Lancet. 2016;388(10053):1775–1812. doi: 10.1016/S0140-6736(16)31470-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawachi I., Kennedy B.P. Income inequality and health: Pathways and mechanisms. Health Services Research. 1999;34(1 Pt 2):215–227. [PMC free article] [PubMed] [Google Scholar]
- Kennedy B.P., Kawachi I., Lochner K., Jones C., Prothrow-Stith D. Dis)respect and black mortality. Ethnicity & Disease. 1997;7(3):207–214. [PubMed] [Google Scholar]
- Khan K.S., Wojdyla D., Say L., Gulmezoglu A.M., Van Look P.F. WHO analysis of causes of maternal death: A systematic review. The Lancet. 2006;367(9516):1066–1074. doi: 10.1016/S0140-6736(06)68397-9. [DOI] [PubMed] [Google Scholar]
- King J.C. Maternal mortality in the United States--why is it important and what are we doing about it? Seminars in Perinatology. 2012;36(1):14–18. doi: 10.1053/j.semperi.2011.09.004. [DOI] [PubMed] [Google Scholar]
- Koch E., Thorp J., Bravo M., Gatica S., Romero C.X., Aguilera H. Women's education level, maternal health facilities, abortion legislation and maternal deaths: A natural experiment in Chile from 1957 to 2007. PLoS One. 2012;7(5) doi: 10.1371/journal.pone.0036613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kondo N., Sembajwe G., Kawachi I., van Dam R.M., Subramanian S., Yamagata Z. Income inequality, mortality, and self rated health: Meta-analysis of multilevel studies. BMJ. 2009;339:b4471. doi: 10.1136/bmj.b4471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kondo N., van Dam R.M., Sembajwe G., Subramanian S.V., Kawachi I., Yamagata Z. Income inequality and health: The role of population size, inequality threshold, period effects and lag effects. Journal of Epidemiology & Community Health. 2012;66(6):e11. doi: 10.1136/jech-2011-200321. [DOI] [PubMed] [Google Scholar]
- Krieger N., Waterman P.D., Spasojevic J., Li W., Maduro G., Van Wye G. Public health monitoring of privilege and deprivation with the index of concentration at the extremes. American Journal of Public Health. 2016;106(2):256–263. doi: 10.2105/AJPH.2015.302955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lochner K., Pamuk E., Makuc D., Kennedy B.P., Kawachi I. State-level income inequality and individual mortality risk: A prospective, multilevel study. American Journal of Public Health. 2001;91(3):385–391. doi: 10.2105/ajph.91.3.385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lorgelly P.K., Lindley J. What is the relationship between income inequality and health? Evidence from the BHPS. Health Economics. 2008;17(2):249–265. doi: 10.1002/hec.1254. [DOI] [PubMed] [Google Scholar]
- Lu M.C., Halfon N. Racial and ethnic disparities in birth outcomes: A life-course perspective. Maternal and Child Health Journal. 2003;7(1):13–30. doi: 10.1023/a:1022537516969. [DOI] [PubMed] [Google Scholar]
- Lynch J.W., Smith G.D., Kaplan G.A., House J.S. Income inequality and mortality: Importance to health of individual income, psychosocial environment, or material conditions. BMJ. 2000;320(7243):1200–1204. doi: 10.1136/bmj.320.7243.1200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacDorman M.F., Declercq E., Cabral H., Morton C. Recent increases in the U.S. Maternal mortality rate: Disentangling trends from measurement issues. Obstetrics & Gynecology. 2016;128(3):447–455. doi: 10.1097/AOG.0000000000001556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mellor J.M., Milyo J. Is exposure to income inequality a public health concern? Lagged effects of income inequality on individual and population health. Health Services Research. 2003;38(1Pt1):137–151. doi: 10.1111/1475-6773.00109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mendez D.D., Hogan V.K., Culhane J.F. Institutional racism, neighborhood factors, stress, and preterm birth. Ethnicity and Health. 2014;19(5):479–499. doi: 10.1080/13557858.2013.846300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montez J.K., Zajacova A., Hayward M.D. Explaining inequalities in women's mortality between U.S. States. SSM - Population Health. 2016;2:561–571. doi: 10.1016/j.ssmph.2016.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muldoon K.A., Galway L.P., Nakajima M., Kanters S., Hogg R.S., Bendavid E. Health system determinants of infant, child and maternal mortality: A cross-sectional study of UN member countries. Globalization and Health. 2011;7:42. doi: 10.1186/1744-8603-7-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson D.B., Moniz M.H., Davis M.M. Population-level factors associated with maternal mortality in the United States, 1997-2012. BMC Public Health. 2018;18(1) doi: 10.1186/s12889-018-5935-2. 1007-1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nkansah-Amankra S., Dhawain A., Hussey J.R., Luchok K.J. Maternal social support and neighborhood income inequality as predictors of low birth weight and preterm birth outcome disparities: Analysis of South Carolina pregnancy risk assessment and monitoring system survey, 2000-2003. Maternal and Child Health Journal. 2010;14(5):774–785. doi: 10.1007/s10995-009-0508-8. [DOI] [PubMed] [Google Scholar]
- OECD Income inequality (indicator) 2017. https://data.oecd.org/inequality/income-inequality.htm Retrieved from.
- Olson M.E., Diekema D., Elliott B.A., Renier C.M. Impact of income and income inequality on infant health outcomes in the United States. Pediatrics. 2010;126(6):1165–1173. doi: 10.1542/peds.2009-3378. [DOI] [PubMed] [Google Scholar]
- Patel V., Burns J.K., Dhingra M., Tarver L., Kohrt B.A., Lund C. Income inequality and depression: A systematic review and meta-analysis of the association and a scoping review of mechanisms. World Psychiatry. 2018;17(1):76–89. doi: 10.1002/wps.20492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petersen E., Davis N.L., Goodman D., Cox S., Mayes N., Johnston E.…Barfield W. Vital signs: Pregnancy-related deaths, United States, 2011–2015, and strategies for prevention, 13 states, 2013–2017. MMWR - Morbidity and Mortality Weekly Report. 2019;68:423–429. doi: 10.15585/mmwr.mm6818e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pickett K.E., Wilkinson R.G. Income inequality and health: A causal review. Social Science & Medicine. 2015;128:316–326. doi: 10.1016/j.socscimed.2014.12.031. [DOI] [PubMed] [Google Scholar]
- Rasella D., Aquino R., Barreto M.L. Impact of income inequality on life expectancy in a highly unequal developing country: The case of Brazil. Journal of Epidemiology & Community Health. 2013;67(8):661–666. doi: 10.1136/jech-2012-201426. [DOI] [PubMed] [Google Scholar]
- Robert S.A., Reither E.N. A multilevel analysis of race, community disadvantage, and body mass index among adults in the US. Social Science & Medicine. 2004;59(12):2421–2434. doi: 10.1016/j.socscimed.2004.03.034. [DOI] [PubMed] [Google Scholar]
- Rosenthal L., Lobel M. Explaining racial disparities in adverse birth outcomes: Unique sources of stress for Black American women. Social Science & Medicine. 2011;72(6):977–983. doi: 10.1016/j.socscimed.2011.01.013. [DOI] [PubMed] [Google Scholar]
- Siddiqi A., Jones M.K., Bruce D.J., Erwin P.C. Do racial inequities in infant mortality correspond to variations in societal conditions? A study of state-level income inequality in the U.S., 1992-2007. Social Science & Medicine. 2016;164:49–58. doi: 10.1016/j.socscimed.2016.07.013. [DOI] [PubMed] [Google Scholar]
- Sommeiller E., Price M. Economic Policy Institute; Washington, DC: 2018. The new gilded age: Income inequality in the U.S. by state, metropolitan area, and county. [Google Scholar]
- Stafford M., Cummins S., Macintyre S., Ellaway A., Marmot M. Gender differences in the associations between health and neighbourhood environment. Social Science & Medicine. 2005;60(8):1681–1692. doi: 10.1016/j.socscimed.2004.08.028. [DOI] [PubMed] [Google Scholar]
- Subramanian S.V., Kawachi I. Income inequality and health: What have we learned so far? Epidemiologic Reviews. 2004;26(1):78–91. doi: 10.1093/epirev/mxh003. [DOI] [PubMed] [Google Scholar]
- Subramanian S.V., Kawachi I. Whose health is affected by income inequality? A multilevel interaction analysis of contemporaneous and lagged effects of state income inequality on individual self-rated health in the United States. Health & Place. 2006;12(2):141–156. doi: 10.1016/j.healthplace.2004.11.001. [DOI] [PubMed] [Google Scholar]
- Tajik P., Nedjat S., Afshar N.E., Changizi N., Yazdizadeh B., Azemikhah A.…Majdzadeh R. Inequality in maternal mortality in Iran: An ecologic study. International Journal of Preventive Medicine. 2012;3(2):116–121. [PMC free article] [PubMed] [Google Scholar]
- Wallace M., Crear-Perry J., Richardson L., Tarver M., Theall K. Separate and unequal: Structural racism and infant mortality in the US. Health & Place. 2017;45:140–144. doi: 10.1016/j.healthplace.2017.03.012. [DOI] [PubMed] [Google Scholar]
- Wallace M.E., Mendola P., Chen Z., Hwang B.S., Grantz K.L. Preterm birth in the context of increasing income inequality. Maternal and Child Health Journal. 2016;20(1):164–171. doi: 10.1007/s10995-015-1816-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallace M.E., Mendola P., Liu D., Grantz K.L. Joint effects of structural racism and income inequality on small-for-gestational-age birth. American Journal of Public Health. 2015;105(8):1681–1688. doi: 10.2105/AJPH.2015.302613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White K., Haas J.S., Williams D.R. Elucidating the role of place in health care disparities: The example of racial/ethnic residential segregation. Health Services Research. 2012;47(3 Pt 2):1278–1299. doi: 10.1111/j.1475-6773.2012.01410.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO, UNFPA, World Bank . 2016. Trends in maternal mortality: 1990 to 2015.https://data.worldbank.org/indicator/SH.STA.MMRT?name_desc=true (2016). Trends in maternal mortality: 1990 to 2015. Retrieved from. [Google Scholar]
- Wilkinson R.G. Socioeconomic determinants of health: Health inequalities: Relative or absolute material standards? BMJ. 1997;314(7080):591. doi: 10.1136/bmj.314.7080.591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams D.R. Racial/ethnic variations in women's health: The social embeddedness of health. American Journal of Public Health. 2008;92(4):588–597. doi: 10.2105/ajph.92.4.588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams D.R., Jackson P.B. Social sources of racial disparities in health. Health Affairs. 2005;24(2):325–334. doi: 10.1377/hlthaff.24.2.325. [DOI] [PubMed] [Google Scholar]
- World Bank Gini index (World Bank estimate) – country ranking. 2017. https://data.worldbank.org/indicator/SI.POV.GINI?page=4 Retrieved from.
- Zimmerman F.J., Bell J.F. Income inequality and physical and mental health: Testing associations consistent with proposed causal pathways. Journal of Epidemiology & Community Health. 2006;60(6):513–521. doi: 10.1136/jech.2005.040154. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.