Abstract
Background
Childhood constipation is a common problem with substantial health, economic and emotional burdens. Existing therapeutic options, mainly pharmacological, are not consistently effective, and some are associated with adverse effects after prolonged use. Transcutaneous electrical stimulation (TES), a non‐pharmacological approach, is postulated to facilitate bowel movement by modulating the nerves of the large bowel via the application of electrical current transmitted through the abdominal wall.
Objectives
Our main objective was to evaluate the effectiveness and safety of TES when employed to improve bowel function and constipation‐related symptoms in children with constipation.
Search methods
We searched MEDLINE (PubMed) (1950 to July 2015), the Cochrane Central Register of Controlled Trials (CENTRAL) (The Cochrane Library, Issue 7, 2015), EMBASE (1980 to July 2015), the Cochrane IBD Group Specialized Register, trial registries and conference proceedings to identify applicable studies .
Selection criteria
Randomized controlled trials that assessed any type of TES, administered at home or in a clinical setting, compared to no treatment, a sham TES, other forms of nerve stimulation or any other pharmaceutical or non‐pharmaceutical measures used to treat constipation in children were considered for inclusion.
Data collection and analysis
Two authors independently assessed studies for inclusion, extracted data and assessed risk of bias of the included studies. We calculated the risk ratio (RR) and corresponding 95% confidence interval (CI) for categorical outcomes data and the mean difference (MD) and corresponding 95% CI for continuous outcomes. We evaluated the overall quality of the evidence supporting the outcomes assessed in this review using the GRADE criteria.
Main results
One study from Australia including 46 children aged 8 to 18 years was eligible for inclusion. There were multiple reports identified, including one unpublished report, that focused on different outcomes of the same study. The study had unclear risk of selection bias, high risks of performance, detection and attrition biases, and low risks of reporting biases.
We are very uncertain about the effects of TES on bowel movements, colonic transit, soiling symptoms and quality of life due to high risk of bias, indirectness and imprecision. For our outcomes of interest the 95% CI of most analysis results include potential benefit and no effect. There is insufficient evidence to determine the effect of TES on bowel movements and colonic transit. The study reported that 16/21 children in the TES group and 15/21 in the sham group had > 3 complete spontaneous bowel movements (CSBM) per week (RR 1.07, 95% CI 0.74 to 1.53; very low‐quality evidence). Ten out of 14 children in the TES group had improved colonic transit compared to 1/7 in the sham group (RR 5.00, 95% CI 0.79 to 31.63; very low‐quality evidence). Mean colonic transit rate, measured as the position of the geometric centre of the radioactive substance ingested along the intestinal tract, was higher in children who received TES compared to sham (MD 1.05, 95% CI 0.36 to 1.74; one study, 30 participants; very low‐quality evidence). The radiological assessment of colonic transit outcomes means that these results might not translate to important improvement in clinical symptoms or increased bowel movements. There is insufficient evidence to determine the effect of TES on symptoms and quality of life (QoL) outcomes. Nine out of 13 children in the TES group had improved soiling‐related symptoms compared to 4/12 sham participants (RR 2.08, 95% CI 0.86 to 5.00; very low‐quality evidence). Four out of 8 TES participants reported an improvement in QoL compared to 1/8 sham participants (RR 4.00, 95% CI 0.56 to 28.40; very low‐quality evidence). The effects of TES on self‐perceived (MD 5.00, 95% CI ‐1.21 to 11.21; one study, 33 participants; very low‐quality evidence) or parent‐perceived QoL (MD ‐0.20, 95% CI ‐7.57 to 7.17, one study, 33 participants; very low‐quality evidence) are uncertain. No adverse effects were reported in the included study.
Authors' conclusions
The results for the outcomes assessed in this review are uncertain. Thus no firm conclusions regarding the efficacy and safety of TES in children with chronic constipation can be drawn. Further randomized controlled trials assessing TES for the management of childhood constipation should be conducted. Future trials should include clear documentation of methodologies, especially measures to evaluate the effectiveness of blinding, and incorporate patient‐important outcomes such as the number of patients with improved CSBM, improved clinical symptoms and quality of life.
Plain language summary
Transcutaneous electrical stimulation (TES) for treating long‐term constipation in children.
Review question
We reviewed the evidence about the effectiveness and safety of TES in improving constipation in children.
Background
Childhood constipation is a common problem with substantial health, economic and emotional burdens. Currently, most treatment options include the use of laxatives with diet modification. None of the common medications used are found to be consistently effective, and there are concerns regarding side effects and dependence, especially following long‐term use of laxatives. TES is a newer, non‐pharmacological mode of treatment that involves placing the electrodes on the belly of affected children, which generates small electrical wave forms (interferential current) across the belly wall in a dose that is well below a level that may cause concern, aiming to stimulate the bowel to improve bowel motion.
Search Date
We included research evidence that was current to July 2015.
Study characteristics
We included a single study with 11 reports that focused on results for different outcomes. The participants of the included study were 46 children aged 8 to 18 years recruited from the clinic of a tertiary hospital in Melbourne, Australia who were diagnosed with long‐term constipation either based on their symptoms and/or X‐ray studies. The studies divided the patients into two groups, one receiving the actual TES , with electrodes placed on their belly and electrical current running, and the other receiving sham stimulation, with identical device administered but without the electrical current. The participants were followed‐up for up to four years, although only outcome information up until the follow‐up period of two months were available in this review.
Source of funding
The study was funded by the Australian National Health and Medical Research Council and Murdoch Children's Research Institute Theme Investment Grants.
Key results
There was not enough information on certain aspects of the trial methodologies from the reports gathered, although it was clear that the physiotherapists who administered the TES treatment or sham treatment were aware of which group the patients were allocated to. The knowledge of the participants' allocated group might have influenced the way the actual and sham therapies were administered, as well as the way some of the outcome data, such as symptoms of constipation and soiling and quality of life, might have been reported by the therapist as well as the patients and their carers. This raised concerns regarding the overall methodological quality of the study.
The very low quality evidence for all of the results means that we are uncertain about the effects of TES when compared with sham stimulation. Overall, there were no differences between children who received TES and sham stimulation in the number of children with improved complete spontaneous bowel movements, improved bowel movements (as assessed by X‐Ray with special contrast), improved symptoms related to soiling and quality of life. There were also no differences between the two groups in the average change in the quality of life scores after the therapy, as assessed by the children themselves as well as their parents. The only difference noted was in mean bowel transit rate, namely, distance travelled by the radioactive substance along the bowel, in which children who received TES had their radioactive substance slightly further down their bowel compared to children who received a sham stimulation. However, it was unclear whether such a difference in distance travelled in the bowel translated to any meaningful differences in defaecation and constipation‐related symptoms. No side effects were reported in the study.
Quality of evidence
Overall, this study included a small number of patients and we had concerns regarding the methods resulting in very low quality evidence for all the outcomes assessed.
Authors' conclusions
The results for the outcomes assessed in this review are uncertain. Thus no firm conclusions regarding the effectiveness and side effects of TES in children with chronic constipation can be drawn. Further studies assessing TES for the management of constipation are needed. We suggest that future research should provide clear documentation on specific methods in the conduct of the trials, and include outcomes that are important for patients, such as spontaneous or complete bowel movements or improvement in constipation‐related symptoms along with assessments of quality of life.
Summary of findings
Summary of findings for the main comparison. Transcutaneous electrical stimulation for treating chronic constipation in children.
| Research question: In children with chronic constipation, does the use of transcutaneous electrical stimulation (TES) improved bowel motion, symptoms and other major outcomes compared with the use of sham stimulation? | ||||||
| Patient or population: children with chronic constipation Setting: hospital clinics Intervention: transcutaneous electrical stimulation (TES) Comparison: sham stimulation | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Risk with sham stimulation | Risk with transcutaneous electrical stimulation | |||||
| Number of participants with improved complete spontaneous bowel movement (CSBM) of greater than three times per week at two‐month follow‐up | 714 per 10001 | 764 per 1000 (529 to 1000) | RR 1.07 (0.74 to 1.53) | 42 (1 RCT) | ⊕⊝⊝⊝ VERY LOW 2,3 | |
| Number of participants with improved colonic transit assessed with: Radioisotope studies | 143 per 10001 | 714 per 1000 (113 to 1000) | RR 5.00 (0.79 to 31.63) | 21 (1 RCT) | ⊕⊝⊝⊝ VERY LOW 2,34, | |
| Colonic transit rate (geometric centre of radioactive substance). Unit indicates position along with intestinal tract. Scale from: 1 (small intestine) to 5 (rectosigmoid area). | The mean colonic transit rate (geometric centre of radioactive substance) was 3.27 unit in the "Distance of geometric centre along the intestinal tract" | The mean colonic transit rate (geometric centre of radioactive substance) in the intervention group was 1.05 unit more (0.36 more to 1.74 more) | ‐ | 30 (1 RCT) | ⊕⊝⊝⊝ VERY LOW 2,3,4 | |
| Number of participants with improved symptoms related to soiling | 333 per 10001 | 693 per 1000 (287 to 1000) | RR 2.08 (0.86 to 5.00) | 25 (1 RCT) | ⊕⊝⊝⊝ VERY LOW 2,3 | |
| Number of participants with improved quality of life assessed with: Peds QL 4.0 Generic Scales (higher scores indicates better quality of life) Scale from: 0 to 100 | 125 per 10001 | 500 per 1000 (70 to 1000) | RR 4.00 (0.56 to 28.40) | 16 (1 RCT) | ⊕⊝⊝⊝ VERY LOW 2,3 | |
| Self‐perceived QoL (change from baseline) measured using Peds QL 4.0 Generic Core Scales, scoring 0‐100 points, higher score indicates better quality of life) | The mean self‐perceived QoL (change from baseline) was 3.2 points | The mean change in self‐perceived QoL in the intervention group was 5 points higher (1.21 lower to 11.21 higher) | ‐ | 33 (1 RCT) | ⊕⊝⊝⊝ VERY LOW 2,3 | |
| Parent‐perceived QoL (change from baseline) measured using PedsQL 4.0 Generic Core Scales, scoring 0‐100 points, higher score indicates better quality of life) |
The mean parent‐perceived QoL (change from baseline) was 0.4 points | The mean change in parent‐perceived QoL in the intervention group was 0.2 points lower (7.57 lower to 7.17 higher) | ‐ | 33 (1 RCT) | ⊕⊝⊝⊝ VERY LOW 2,3 | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio; OR: Odds ratio; | ||||||
| GRADE Working Group grades of evidence High quality: We are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low quality: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low quality: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | ||||||
1 The sham group risk estimate comes from the control arm of the included trial.
2 We downgraded one level due to unclear risk of selection bias and high risk of performance and detection bias with some subjective outcomes assessed
3 We downgraded two levels due to serious imprecision with very few events in the outcomes concerned, as they were far short of the optimal information size.
4 Indirectness, improved radiologically‐assessed colonic transit might not translate to important improvement in clinical symptoms or increased bowel motion.
Background
Description of the condition
Constipation is a common problem in children. Globally, the prevalence of constipation ranges from around 0.7 to 30% of the paediatric population depending on the diagnostic criteria used (NICE 2010, van den Berg 2006). Less than five per cent of these children have an underlying organic cause for their constipation (Tabbers 2011). Around 3% of general paediatric outpatient visits and approximately 25% of paediatric gastroenterology consultations are related to a perceived defecation disorder, a major proportion of which is constipation (NASPGHAN 2006). Childhood constipation is associated with substantial financial and emotional burden for the affected children and their caregivers (Walia 2009). One report estimates the costs of managing constipation in children to be around USD 3.9 billion per year in the USA alone (Mugie 2011). The pathophysiology of constipation is multifactorial but the end result is disordered bowel movements with impacted faeces in the gut (NASPGHAN 2006).
Description of the intervention
Currently, there are several available interventions used to treat constipation as recommended by established guidelines such as the National Institute of Clinical Excellence (NICE). These include various forms of laxatives (e.g. lactulose, milk of magnesia, liquid paraffin, senna and polyethylene glycol), non‐pharmacological therapies such as biofeedback and behavioural therapy, and some newer treatment options like probiotics (NICE 2010). Most of the treatment options mentioned above have been assessed in Cochrane reviews that are either published or in development (Aboumarzouk 2011; Candy 2011; Coggrave 2006; Evans 2007; Gordon 2012; Lee‐Robichaud 2010; Mowatt 2007; Price 2001; Shariff 2009). None of these treatment options appear to be consistently effective for the majority of children. Continued exploration of treatment modalities with a favourable benefit‐harm balance is therefore warranted to provide treatment options to suit different groups of affected children.
One of the newer modes of therapy to facilitate bowel motion in patients with constipation is transcutaneous electrical stimulation (TES) (Sluka 2003). Its use for other purposes, such as pain management for various conditions is more well‐established (Dowswell 2009; Khadilkar 2005; Mulvey 2010; Nnoaham 2008; Rutjes 2009; Walsh 2009).
How the intervention might work
TES is a form of electrical stimulation, usually an interferential current, used to stimulate the nerve. The TES device consists of a voltage generator of electrical pulse, interconnecting wire or cable, and electrodes that are attached to the skin. The low voltage electrical impulse generated by this device may travel across the skin and act as a stimulus to the appropriate peripheral nerves (Sluka 2003), or may travel deep into the abdominal cavity affecting the bowel directly. Presently, the precise mechanism of the effect is unknown. One theory that which has been postulated is that TES acts centrally by re‐balancing excitatory and inhibitory information and returning the neural drive to a more normal status (Sluka 2003).
An interferential stimulator is used for treating slow‐transit constipation. The pad electrodes are placed over the skin surface of the abdomen and the paraspinal regions. Four electrodes are placed, two on the anterior abdominal wall at the level of the umbilicus (i.e. navel), and two on the paraspinal region in between the distal thoracic and upper lumbar spine (i.e. T9 to L2) (Chase 2005). The TES device produces two out‐of‐phase currents with different amplitudes that interfer with each other. The resulting sinusoidal currents cross within the body and stimulate the peripheral nerves. The mechanisms of action leading to beneficial therapeutic effects are still unclear, although it is postulated that TES improves bowel movement via neuromodulation of the extrinsic neural control of the large bowel or modulation of reflexes that inhibit large bowel function. By using colonic manometry, it has been shown that TES increases colonic propagating pressure waves (Clarke 2012; van Wunnik 2011).
There have been some adverse events reported for sacral nerve stimulation, which bears some similarity to the TES therapy covered in this review but required surgical implantation of electrodes. These included pain or discomfort at the electrode attachment site, electrode migration and infection (Norderval 2011; van Wunnik 2011, van Wunnik 2012). However, some studies that evaluated TES did not report any adverse effects (Eleouet 2010; Ismail 2009).
Why it is important to do this review
The current uncertainties on the role of TES, a non‐pharmacological mode of therapy, in treating childhood constipation, a disorder that is generally difficult to treat, warrants a regularly updated Cochrane systematic review to inform current practice and make recommendations for future research.
Objectives
Our main objective was to evaluate the effectiveness and safety of TES when employed to improve bowel function and constipation‐related symptoms in children with constipation.
Methods
Criteria for considering studies for this review
Types of studies
We included randomised controlled trials and randomised cross‐over studies in which patients had their TES device 'disabled' at different periods in the study.
Types of participants
We included studies that enrolled children (aged 0 to 18 years) with a diagnosis of functional constipation with or without accompanying incontinence. We accepted various definitions of constipation in the included studies, which might be based on diagnosis by a physician or report by patient or caregivers or all three, or via the use of consensus criteria such as the ROME III criteria for functional gastrointestinal disorders (ROME III). We excluded studies that assessed patients with constipation due to secondary causes, such as intestinal obstruction due to structural lesions, endocrine disorders such as hypothyroidism, metabolic or neurological problems, neuromuscular disorders, pregnancy or participants who were on medications that affected gastrointestinal motility as an adverse effect.
Types of interventions
Studies where a TES treatment, administered either in clinical setting or at home, and applied either transabdominally, sacrally or via other means are compared to no treatment, a sham TES treatment, other forms of nerve stimulation or any other pharmaceutical or non‐pharmaceutical measures used to treat constipation were considered for inclusion. We accepted all types of devices used for the purpose of TES and all dosing regimes (i.e. using TES in different intensities such as number of times applied per day).
Types of outcome measures
Primary outcomes
Primary outcomes included the following.
1. Global or clinical improvement in constipation as defined by the included studies. For example, clinical improvement could be measured by the frequency of defaecations per week and could potentially be expressed as a mean number of defaecations or as the proportion of patients who meet a pre‐specified threshold (e.g. greater than three defaecations per week).
2. Spontaneous bowel movements (SBM) and complete spontaneous bowel movements (CSBM). SBM is defined as the passage of a stool without the use of laxative, and CSBM is defined as SBM associated with a sense of complete evacuation (Mueller‐Lissner 2010). SBM and CSBM could be measured by frequency per week and could be expressed as a mean number of SBM or CSBM or as the proportion of patients who meet a pre‐specified threshold (e.g. greater than three SBM or CSBM per week).
Secondary outcomes
Secondary outcomes included the following.
1. Improvement in symptoms associated with constipation (e.g. perceived ease of defaecation, abdominal pain or distension, stool consistency).
2. Improvement in bowel transit time, bowel activity or propagating contractions measured over a defined time period, for example, weekly.
3. Improvement in faecal soiling.
4. Improvement in growth (for example, weight in relation to centile or weight gain), measured at a defined intervals over the course of the study, for example, three monthly or six monthly.
5. The proportion of patients who experienced an adverse event.
6. The proportion of patients who experienced a serious adverse event.
Search methods for identification of studies
We followed recommendations from the Cochrane Handbook for Systematic Reviews of Interventions for conducting the literature search (Lefebvre 2011).
Electronic searches
We searched the following databases:
MEDLINE (PubMed, National Library of Medicine) (1950 to July 2015);
The Cochrane Central Register of Controlled Trials (CENTRAL, part of The Cochrane Library, issue 7, 2015); and
Ovid EMBASE (1980 to July 2015).
We used the MEDLINE search strategy that combines our key terms and MeSH searches with the Cochrane Highly Sensitive Search Strategy for identifying randomised trials in MEDLINE: sensitivity‐ and precision‐maximising version (Lefebvre 2011). We adapted this search strategy where appropriate for the other databases. We did not apply any restriction based on language. The detailed search strategies for MEDLINE, CENTRAL and EMBASE are provided in Appendix 1; Appendix 2 and Appendix 3.
We also screened through the records of the Cochrane IBD Group Specialized Register. Additionally, we searched the following trial registries for details of ongoing clinical trials and unpublished studies:
ClinicalTrials.gov (http://www.clinicaltrials.gov/);
Australia and New Zealand Clinical Trials Registry (http://www.anzctr.org.au/);
WHO International Clinical Trials Registry Platform (http://apps.who.int/trialsearch/Default.aspx); and
EU Clinical Trials Register (https://www.clinicaltrialsregister.eu/).
Additionally, we searched for conference proceedings that are not included in CENTRAL or the review group specialized trials register from the following sources:
Digestive Disease Week (http://ddw.scientificposters.com/index.cfm);
United European Gastroenterology Week (https://www.ueg.eu/week/past‐future/future‐ueg‐week/); and
The North American Society of Pediatric Gastroenterology, and Nutrition (NASPGHAN) annual meeting archive (http://www.naspghan.org/wmspage.cfm?parm1=62).
Searching other resources
We searched the reference lists of papers identified by the above strategies to identify studies that might have been missed by the electronic searches. We also inspected the references lists of relevant Cochrane reviews for additional relevant studies.
Data collection and analysis
Selection of studies
Two review authors (RTN and KMT) independently screened titles and abstracts to identify potentially eligible studies.Two authors (KMT and NML) independently assessed the full‐text of potentially eligible studies to determine eligibility for inclusion. We recorded reasons for excluding ineligible studies, and resolved any disagreement through discussion and consensus. We sought the input of a third author (WSL) who acted as the arbiter where necessary. The process of study selection was recorded in a PRISMA flow diagram.
Data extraction and management
We extracted data using a dedicated data collection form, which was piloted on one included study. We included the following study characteristics and outcome data in the data collection form.
1. Methods: study design, location, setting and duration.
2. Participants: number, mean age, median age or age range, gender, underlying conditions, diagnostic criteria if applicable, inclusion and exclusion criteria.
3. Interventions: description of the components of the intervention and comparison.
4. Outcomes: description of primary and secondary outcomes specified and collected, and at which time points reported.
5. Notes: funding for trial, and notable conflicts of interest of trial authors.
Two review authors (KMT and RTN) independently extracted outcome data from included studies. We noted in the 'Characteristics of included studies' table and in the results if outcome data reported was not suitable for meta‐analysis. Any disagreement was resolved through discussion and consensus and we sought the input of a third author (NML) who acted as the arbiter where necessary. The data was entered into Review Manager (RevMan 5.3) (RevMan 2014) by one review author with the rest of the review authors participated in double‐checking for accuracy.
Assessment of risk of bias in included studies
Two review authors (NML and KMT) independently assessed the quality of each included study using the Cochrane risk of bias tool (Higgins 2011a). We resolved any disagreements by discussion leading to consensus. We assessed the following domains.
1. Random sequence generation.
2. Allocation concealment.
3. Blinding of participants and personnel.
4. Blinding of outcome assessment.
5. Incomplete outcome data.
6. Selective outcome reporting.
7. Other bias.
Each item was rated as high, low or unclear risk of bias, and a justification from the study report was supplied to support the judgement as appropriate. When considering treatment effects, we took into account the risk of bias, including unclear risk of bias, for the studies that contribute to that outcome.
Measures of treatment effect
We reported the risk ratio (RR) and corresponding 95% confidence interval (CI) for dichotomous outcomes. We would have reported the risk difference (RD) and corresponding 95% CI if there were moderate or good quality evidence which showed a significant difference between the two groups. For continuous outcomes we reported the mean difference (MD) and corresponding 95% CI, or standardised mean difference (SMD) and corresponding 95% CI as appropriate. If included studies only report effect estimates and 95% CI or standard errors we would have entered these data into RevMan using the generic inverse variance method. If the outcomes were measured using a scale, we would have standardised the direction of the scale in terms of the severity of the outcome with accompanying explanation.
Unit of analysis issues
Had we included a cross‐over study, we would have incorporated data only from the first interventional phase of the studies if possible, to avoid contaminating effect of the cross‐over. If this was not possible, we would have analysed data as presented by the authors, and performed sensitivity analysis to assess the impact of excluding data from such studies.
Had we identified a trial with multiple arms of comparison, we would have included only the relevant arms. If two comparisons (e.g. TES method A versus a sham TES procedure and TES method B versus a sham TES procedure) were combined in the same meta‐analysis, we would have halved the control group to avoid double‐counting.
Had we identified studies with repeated observations on participants, we would have included data only at the level of the participants, for example, the number of participants who experienced any adverse event (either single or multiple times). For participants who were enrolled multiple times, we would have only included data from the first enrolment. If this was impossible, we will include the data as reported by the authors, and perform a sensitivity analysis excluding studies where participants were enrolled multiple times.
Dealing with missing data
We assessed the drop‐out rate from each study and looked for explanations for non‐completion of the studies. We considered a drop‐out rate higher than the control group event rate to be significant. If we found a significant drop‐out rate with no reasonable explanation, we would judge the study to have a high risk of bias for incomplete outcome data. If necessary study authors would be contacted to request missing data and the reasons for non‐completion. We would have performed sensitivity analyses if there were sufficient studies for a comparison to evaluate the impact of excluding studies with significant drop‐out rates on the magnitude and direction of the effect estimate .
After assessing drop‐out rates and the reasons for drop‐out, we would handle missing data based on the recommendations of the Cochrane handbook of Interventional Reviews, Chapter 16.1.2 (Higgins 2011b). If drop‐outs appeared to occur at random, we would analyse only the available data. If drop‐outs did not appear to be random, we would impute the missing data by assuming that all missing participants had a poor outcome for dichotomous outcomes and by imputing outcome values from the mean and standard deviation for continuous outcomes.
Assessment of heterogeneity
Had there been more than one included study for each outcome, we would inspect the forest plots to globally assess the variation in the treatment effects of individual trials. We would then assess the included studies in terms of similarity of population, intervention, outcome and follow‐up. We considered populations to be similar when they were of similar age range and underlying pathology leading to constipation. We considered interventions to be similar when they involved nerve stimulation through the skin. We considered all outcomes that measured the same construct to be similar. For example, the number of bowel movements over a period of time or the amount of stool passed. However, we would regard objective measurement of outcomes such as the frequency of bowel movements and subjective report of outcomes such as the ease of bowel movements to be different. We considered follow‐up times of up to one month as short‐term, one to six months as medium‐term and more than six months as long‐term. We would only pool data in a meta‐analysis if studies were similar in terms of population, intervention, outcome and follow‐up (to be determined by consensus). In cases where there were some differences among the studies and we were unsure of the significance of these differences, we would perform a sensitivity analyses to assess the impact of including and excluding these studies.
We planned to use the Chi2 test and the I2 statistic to evaluate statistical heterogeneity. If the Chi2 test showed statistically significant heterogeneity, as indicated by a p value of less than 0.1, we would quantify the degree of heterogeneity using the I2 statistic. In this review, we defined an I2 statistic of 50% or higher as substantial heterogeneity. In such cases, we would explore possible causes for the heterogeneity by prespecified subgroup analyses. If the degree of heterogeneity was excessive, as indicated by an I2 statistic of more than 75% which was not contributed predominantly by a single study, we would consider not pooling the studies for meta‐analysis.
Assessment of reporting biases
We compared the outcomes reported in the results against the outcomes listed in the study protocol or the methods section of the manuscript. The study authors would be contacted for clarification where necessary. For studies where critical outcomes are missing, we searched for the study protocol, either from PubMed, the relevant trial registry, the web link provided by the study or directly from the study authors, to establish whether these outcomes were prespecified.
Where possible, a sensitivity analysis would be performed to explore the impact of excluding studies with a high risk of reporting bias.
Assessment of publication bias
We planned to screen for publication bias by using a funnel plot if there were sufficient studies (at least ten) included in the analysis. If publication bias was suspected as indicated by significant asymmetry of the funnel plot, we would have included a statement in our results and the summary of findings table with a corresponding note of caution in the discussion.
Data synthesis
For dichotomous outcomes we reported the pooled RR and corresponding 95% CI. In the case of statistically significant results, we would have reported the pooled risk difference (RD) and 95% CI and the number needed to treat for an additional beneficial outcome (NNTB) or for an additional harmful outcome (NNTH) as appropriate. For continuous outcomes we reported the pooled MD or SMD and corresponding 95% CI as appropriate. We planned to use a fixed‐effect model to pool data, unless there were significant unexplained heterogeneity identified, in which case we would have used a random‐effects model. If possible, we analysed all data on an intention‐to‐treat basis. We would have provided a narrative description of any skewed data reported as medians and interquartile ranges.
Summary of findings table
We used the GRADE approach (Schünemann 2011), to assess the overall quality of evidence for the following seven outcomes: i) number of participants with improved CSBM, ii) number of participants with improved colonic transit, iii) colonic transit rate, iv) number of participants with improved symptoms related to soiling, v) number of patients with improved quality of life, vi) self‐perceived quality of life, and vii) parent‐perceived quality of life. We created a 'Summary of findings' table using the GRADEpro software to report the results of the GRADE analysis. Outcomes from pooling of randomised trials start as high quality evidence, but were downgraded due to risk of bias, inconsistency of effect, imprecision, indirectness or publication bias. Reasons for downgrading the quality of the included studies were reported in the footnotes of the 'Summary of findings' table as well as in the results under the Effects of interventions.
Subgroup analysis and investigation of heterogeneity
We planned to conduct the following subgroup analyses if sufficient data were available.
1. Studies that enrolled patients with the purpose of achieving bowel clearance (i.e. remission) and studies that enrolled patients with the purpose of maintaining regular bowel clearance (i.e. maintenance).
2. Studies that employed TES differently, for instance, transabdominally versus sacrally.
3. Studies that assessed different comparisons, for example, medication or other form of nerve stimulation.
4. Studies that employed TES in different doses or intensities (i.e. current frequency and amplitude).
5. Studies with different duration of treatment.
6. Patients of different age groups, for instance, infants, young and older children.
Sensitivity analysis
We planned to perform sensitivity analysis, defined a priori, to assess the robustness of our conclusions had sufficient data been available. Potential sensitivity analyses would have included the following.
1. Fixed‐effect versus random‐effects models.
2. Excluding studies judged to be at high risk of selection bias.
3. Excluding studies judged to be at high risk of attrition bias.
4. Excluding studies judged to be at high risk of performance or detection bias.
5. Excluding studies judged to be at high risk of reporting bias.
6. Excluding cross‐over studies and studies with multiple enrolment of the same participants.
Results
Description of studies
Results of the search
The initial search yielded 480 records, including 130 from MEDLINE (PubMed), 190 from EMBASE, 153 from CENTRAL and 7 from the Cochrane IBD Group Specialized Register. There were no additional records identified by supplementary Internet searches. After removing duplicates, there were 436 records in total. After inspecting titles and abstracts, we short listed 22 articles that appeared to be relevant for a detailed assessment of eligibility. We then excluded 12 articles with reasons, leaving 10 articles for further assessment. All 10 articles were reports from the same research institute that were very similar in terms of population, setting, date of research and intervention administered, although each report focussed on different sets of outcomes. Seven of these 10 articles were initially identified as clearly eligible, while the remaining three articles appeared to report very similar information to one of the included reports, and it was initially placed under awaiting classification while we made further correspondence with the authors to seek clarification on the exact number of studies conducted over the period reported by the 10 reports and the degree of overlap among the reports.
Further correspondence with one of the authors (Yik 2015 (pers comm)), confirmed that all of the above mentioned 10 articles reported various outcomes at different time points for the same study. An additional reference, of an unpublished manuscript that contained further information on the trial methodology of the study, was provided following correspondence with the authors and is included as the primary reference for the study (Chase 2015). Therefore, a single study (with 11 references) was included in this review.
The flow diagram of the studies from the initial search to the meta‐analysis is shown in Figure 1. A description of the single included study is displayed in the Characteristics of included studies table, and the excluded studies with the reasons for exclusion are given in the Characteristics of excluded studies table.
1.

Study flow diagram.
Included studies
The included study was a single‐centre randomised controlled trial conducted in Melbourne, Australia, by a team of researchers from the Murdoch Children's Research Institute. The study recruited children aged 8 to 18 years in the hospital clinic setting. These children were diagnosed with slow‐transit constipation (STC) using either clinical criteria (e.g. Rome II) or by radioisotope nuclear transit study performed within the previous year. Forty‐six children (24 boys and 18 girls) were randomised and 42 completed the study, with 21 children allocated to each group. Two children from each group did not complete the study. Among the 11 articles that reported various aspects of the same study, four were in full text, including a manuscript that is not yet published, and the remaining were abstract publications. Data from three of the articles included as secondary references were reported in a format that were unsuitable for meta‐analysis. The study was funded by the Australian National Health and Medical Research Council and Murdoch Childrens Research Institute Theme Investment Grants.
The participants had STC for more than two years. The specific findings that defined STC was retention of radioisotope in the ascending or transverse colon but not rectosigmoid at 48 hours. The included participants had received medical therapies including diet, laxatives or behaviour modification without satisfactory results. Children with organic disorders such as Hirschsprung Disease, celiac disease, hypothyroidism or allergies that may impact on bowel function, children who had undergone bowel surgery, those in whom the use of electrical current was contraindicated (for example, children with cardiac pacemakers), children who had received electrical stimulation before, children with significant neurological disorders and those unable to complete the questionnaire or bowel diaries were excluded.
Two children from each group did not complete the study. The authors stated that at baseline, there were no significant differences between the two groups in gender, age, frequencies of abdominal pain, defecation or faecal incontinence. The intervention consisted of TES using interferential therapy where electrical currents were delivered via electrodes that were placed below the costal margin to around the level of umbilicus and at the back, paraspinally from the levels of T9 to L2. Stimulation was applied for 20 minutes per session by the physiotherapist, three times per week for four weeks. The participants were allocated to receive either TES or sham stimulation for four weeks and then were followed up for two months. Radioisotope transit studies were performed pre‐intervention and two months post intervention in selected participants.
Outcomes included the number of participants with improved CSBM, symptoms of soiling, colonic transit rates and quality of life. In two of the secondary publications, the Holschneider continence score and Templeton score were used respectively to measure continence. These reported outcomes were consistent with some of the the pre‐specified outcomes of our review, including the primary outcome of CSBM, measured by frequency per week and could be expressed as a mean number of SBM or CSBM or as the proportion of patients who meet a pre‐specified threshold (e.g. greater than three SBM or CSBM per week).
A secondary publication of the included study Chase 2015 (i.e. Clarke 2009) reported results in the form of mean differences pre‐ and post‐intervention (change scores) and accompanying P values without any additional information for the outcomes self‐perceived and parent‐perceived quality of life. We derived the standard deviation (SD) for the change score, which was required for meta‐analysis, by following the steps recommended in Chapter 7.7.3.3. of the Cochrane Handbook for Systematic Reviews of Intervention (Higgins 2011c): We converted the P value to a T value, and the T value to a standard error (SE) by dividing the mean difference with the T value (MD/t). We then converted the SE to a SD of the change by multiplying SE by the square root of the number of patients in each group.
Excluded studies
We excluded 12 studies based on one or more of the following:
1. Study design (10 articles): the studies were mainly single‐group before‐and‐after studies (nine studies) or retrospective audit (one study).
2. Article type (one article) (Thomas 2013): the article was a literature review on the effect of sacral nerve stimulation on adults and children with slow‐transit constipation.
4. Population (one article): Moeller 2015 described a study that evaluated transcutaneous electrical nerve stimulation in children with overactive bladder.
A description of each study is available in the Characteristics of excluded studies table.
Risk of bias in included studies
Overall, Chase 2015 had a mixed risk of bias profile, including an unclear risk of selection bias, high risk of performance , detection and attrition biases, low risks of reporting biases and high risk for "other bias" due to a unit of analysis issue. The risk of bias analysis is summarized in Figure 2. We are still awaiting further information from the trialists regarding the risk of bias of the included study, which might include additional information on the risk of bias that related to unpublished data. A detailed description of the risk of bias is provided in the Characteristics of included studies. The following are summaries of our risk of bias assessment for each major domain.
2.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
Chase 2015 was given an unclear risk of bias for random sequence generation and allocation concealment, as the methods of random sequence generation and allocation process were not described in sufficient detail to enable an assessment on whether random sequence generation and allocation were independent from each other. For instance, the study reported the use of block randomisation but did not report the methods used to generate the randomisation list, and the investigators used sealed envelopes without reporting whether the envelops were opaque.
Blinding
Chase 2015 was judged to have a high risk of bias for blinding of patients and personnel, as the authors clearly stated that the physiotherapists who administered the intervention could not be blinded. Additionally, it was unclear whether the patients could discern the presence or absence of electrical current across their abdominal wall, despite the measures taken by the investigators to standardise to administration of active and sham TES. The physiotherapists who administered the TES were also responsible for the collection of at least some data, making the study at high risk of detection bias.
Incomplete outcome data
In Chase 2015, four out of 46 participants who were initially randomised did not complete the study, two of whom were from each group. Despite the low number of non‐completers for the main outcome of CSBM, there appeared to be only subsets of the total 42 participants who were included for the other outcomes, as reported in different secondary publications of the same study. For example, only 21 participants (14 in the TES group and 7 in the control group) were included for the outcome 'number of participants with improved colonic transit', and 16 participants (8 in each group) were included for the outcome 'number of participants with improved quality of life'. Considering the overall participation rate across all outcomes, we decided to rate the study as high risk of bias for incomplete outcome data.
Selective reporting
For Chase 2015, all the outcomes that were pre‐specified in the methods were reported in sufficient detail in the results, either in the main manuscript or in the secondary study publications. We have therefore judged the study to be at low risk of bias for selective outcome reporting. We further confirmed this by checking the outcomes pre‐specified for the trial entry in the Australian New Zealand Clinical Trials Registry (ACTRN12610000418077) in (http://www.anzctr.org.au/default.aspx).
Other potential sources of bias
There was a unit of analysis issue noted in one secondary publication of the study, in which some children underwent multiple radioisotope studies, and the authors did not adjust the results to account for clustering. Therefore the study was rated as high risk of bias for other biases.
Effects of interventions
See: Table 1
Out of the 11 reports for the single included study, data from two reports were unsuitable for meta‐analysis. Leong 2011 reported combined data for all participants without separating the data into the TES and control groups, while Southwell 2010 reported the mean scores and the standard error of the mean for each group without reporting the number of participants in each group. We are awaiting further information from the authors.
Out of eight pre‐defined outcomes in this review, data were available for only three outcomes (number of patients with improved CSBM, improvement in bowel transit time and improvement in symptoms related to soiling). Each of these outcomes was reported in three different secondary publications , and only included a subset of the total 42 participants who had undergone a particular type of evaluation that was relevant to the reported outcome. The total number of participants varied across different outcomes, and not all outcomes had a balanced number of participants between the two groups. Quality of life, which was not pre‐specified in our protocol, was evaluated in one report of the included study and presented below.
Comparison: TES versus sham stimulation
Primary outcomes
1. Global or clinical improvement in constipation: not evaluated by the included study.
2. Spontaneous bowel movements (SBM) and CSBM: There was no statistically significant difference between children who received TES versus those who received sham stimulation in the number of children with greater than three CSBM per week. Seventy‐six per cent (16/21) of children in the TES group had improved CSBM compared to 71% (15/21) of children in the sham group (RR 1.07, 95% CI 0.74 to 1.53, one study, 42 participants; Analysis 1.1). A GRADE analysis indicated that the overall quality of the evidence supporting this outcome was very low due to high risk of bias and serious imprecision (See Table 1).
1.1. Analysis.

Comparison 1 Transcutaneous electrical stimulation versus sham stimulation, Outcome 1 Number of participants with improved complete spontaneous bowel movement (CSBM) of greater than three times per week at two‐month follow‐up.
Secondary outcomes
1. Improvement in symptoms associated with constipation (e.g. perceived ease of defaecation, abdominal pain or distension, stool consistency): the secondary publication that reported this outcome reported overall results for both groups combined. We are awaiting the disaggregated data.
2. Improvement in bowel transit time, bowel activity or propagating contractions measured over a defined time period, for example, weekly.
a). Number of participants with improved colonic transit: There was no statistically significant difference between children who received TES versus those who received sham stimulation in the proportion of children with improved colonic transit. Seventy‐one per cent (10/14) of children in the TES group had improved colonic transit compared to 14% (1/7) of the sham group (RR 5.00, 95% CI 0.79 to 31.63; one study, 21 participants; Analysis 1.2). A GRADE analysis indicated that the overall quality of the evidence supporting this outcome was very low due to high risk of bias, serious imprecision and indirectness (See Table 1).
1.2. Analysis.

Comparison 1 Transcutaneous electrical stimulation versus sham stimulation, Outcome 2 Number of participants with improved colonic transit.
b). Colonic transit rate, as measured by the geometric centre of the radioactive substance ingested: Children who received TES had a significantly faster colonic transit rate compared to children who received sham stimulation (MD 1.05, 95% CI 0.36 to 1.74; one study, 30 participants; Analysis 1.3). A GRADE analysis indicated that the overall quality of the evidence supporting this outcome was very low due to high risk of bias, serious imprecision and indirectness (See Table 1).
1.3. Analysis.

Comparison 1 Transcutaneous electrical stimulation versus sham stimulation, Outcome 3 Colonic transit rate (geometric centre of radioactive substance).
3. Number of participants with improved symptoms related to soiling: There was no statistically significant difference between two groups in the number of children with improved symptoms related to soiling. Sixty‐nine per cent (9/13) of children in the TES group had improved symptoms related to soiling compared to 33% (4/12) of sham participants (RR 2.08, 95% CI 0.86 to 5.00; one study, 25 participants; Analysis 1.4). A GRADE analysis indicated that the overall quality of the evidence supporting this outcome was very low due to high risk of bias and serious imprecision (See Table 1).
1.4. Analysis.
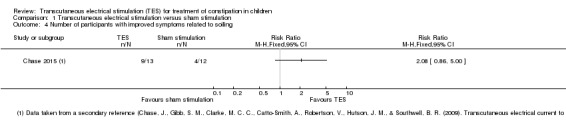
Comparison 1 Transcutaneous electrical stimulation versus sham stimulation, Outcome 4 Number of participants with improved symptoms related to soiling.
4. Improvement in growth: not evaluated by the included study.
5. The proportion of patients who experience an adverse event: the included study reported no adverse events in either group.
6. The proportion of patients who experience a serious adverse event: the included study reported no adverse events in either group.
7. Quality of life:
a). Number of participants with improved quality of life: There was no statistically significant difference between two groups in the number of children with improved quality of life. Fifty per cent (4/8) of TES participants reported an improvement in quality of life compared to 12% (1/8) of sham participants (RR 4.00, 95% CI 0.56 to 28.40; one study, 16 participants; Analysis 1.5). A GRADE analysis indicated that the overall quality of the evidence supporting this outcome was very low due to high risk of bias and serious imprecision (See Table 1).
1.5. Analysis.

Comparison 1 Transcutaneous electrical stimulation versus sham stimulation, Outcome 5 Number of participants with improved quality of life.
b). Change in self‐perceived quality of life (using PedsQL 4.0 Generic Core Scales, scoring 0‐100, higher scores indicate better quality of life): There was no significant difference between two groups in the degree of change in self‐perceived quality of life (MD 5.00, 95% CI ‐1.21 to 11.21; one study, 33 participants; Analysis 1.6). A GRADE analysis indicated that the overall quality of the evidence supporting this outcome was very low due to high risk of bias and serious imprecision (See Table 1).
1.6. Analysis.

Comparison 1 Transcutaneous electrical stimulation versus sham stimulation, Outcome 6 Self‐perceived QoL.
c). Change in parent‐perceived quality of life (using PedsQL 4.0 Generic Core Scales, scoring 0‐100, higher scores indicate better quality of life): There was no significant difference between two groups in the degree of change parent‐perceived quality of life (MD ‐0.20, 95% CI ‐7.57 to 7.17; one study, 33 participants; Analysis 1.7). A GRADE analysis indicated that the overall quality of the evidence supporting this outcomes was very low due to high risk of bias and serious imprecision (See Table 1).
1.7. Analysis.

Comparison 1 Transcutaneous electrical stimulation versus sham stimulation, Outcome 7 Parent‐perceived QoL.
4. Subgroup analyses
We did not perform any subgroup analysis, as all comparisons involved only one included study.
5. Sensitivity analysis
We did not perform any sensitivity analysis, as all comparisons involved only one included study.
Discussion
Summary of main results
Although weak evidence suggests that TES might increase the overall colonic transit rate, there was no clear evidence of differences between children who received TES and children who received sham stimulation on the number of children with greater than three CSBM per week, improved colonic transit, improved symptoms related to soiling and improved quality of life. There were also no significant differences between the two groups in the degree of change in self‐perceived as well as parent‐perceived quality of life. However, all outcomes were contributed by a single study with small number of participants, hence all comparisons were underpowered to detect a statistically significant difference should one exist. Moreover, data for the outcome colonic transit rate was unadjusted for clustering due to multiple radioisotope studies in some participants.
Overall completeness and applicability of evidence
We identified a single study that contained the population, intervention, comparison and outcomes that matched our prespecified selection criteria. However, this study was small, and conducted at a single research institute in Australia. The study included multiple reports, each focusing on different outcomes. The body of evidence that we have gathered reflects the focused interest of one research group for an intervention that is still not widely assessed and practised.
Quality of the evidence
Overall, the evidence supporting the outcomes we assessed in this systematic review is of very low quality. The major reasons for downgrading the quality of evidence were serious imprecision which was related to the small sample size and low event rates, as well as unclear risk of selection bias and high risk of performance, detection and attrition biases in the single included study (see Table 1). Although Chase 2015 included a detailed description of how the administration of TES and sham stimulation were standardised despite non‐blinding of the physiotherapists who administered the intervention, it was unclear how effective such measures were in masking the intervention from the participants, as it was reasonable to suspect that the presence and absence of electrical current across the abdominal wall could be felt by the participants. One possible way to measure the knowledge or perception of the participants regarding group assignment would be to administer a survey asking which group the participants thought they were allocated to and the reason for stating so. However, this was not assessed in the included study.
Potential biases in the review process
A strength of this review includes a comprehensive search from multiple sources to identify all relevant studies. However, this review is limited by a lack of important information on trial methodologies and the non‐availability of some major outcome data. Moreover, for the only outcome that showed a significant difference between the TES and the sham group (colonic transit rate), there were unit of analysis issues due to multiple assessments for some patients without making corresponding statistical adjustments for clustering in the outcome estimates.
Agreements and disagreements with other studies or reviews
To date, there is no other systematic review that assesses the effectiveness and safety of TES for children with chronic constipation. One narrative review that evaluated sacral nerve stimulation for constipation included 13 mainly non‐randomised studies, of which three were conducted in children (all non‐RCTs), reported that sacral nerve stimulation improved constipation‐related symptoms in up to 87% of participants (Thomas 2013).
Several non‐randomised studies conducted at the same research institute as our included study reported that the use of TES in children with chronic constipation increased defaecation, improved colonic transit, reduced soiling and abdominal pain and improved quality of life without any reported adverse effects (Chase 2005; Chase 2009; Ismail 2009; Yik 2012a; Yik 2013a). The results of these non‐randomised studies appear to be inconsistent with the findings of our review. However, in view of the quality of evidence gathered in this review, it is premature to explain the apparent differences between the findings of our review and those in the aforementioned studies.
Authors' conclusions
Implications for practice.
The results for the outcomes assessed in this review are uncertain. Thus no firm conclusions regarding the efficacy and safety of TES in children with chronic constipation can be drawn.
Implications for research.
Further RCTs that assess the effectiveness and safety of TES for children with constipation should be conducted. These studies should clearly document methodologies including methods used for random sequence generation and allocation concealment as well as measures to evaluate the effectiveness of blinding, such as the use of patient survey regarding knowledge or perception of group assignment . Patient‐important outcomes, such as spontaneous bowel movements and complete spontaneous bowel movements, symptoms related to constipation and soiling and quality of life should also be included.
Feedback
Feedback regarding forest plots and conclusions
Summary
Re Cochrane Review
Ng RT, Lee WS, Ang HL, Teo KM, Yik YI, Lai NM. Transcutaneous electrical stimulation (TES) for treatment of constipation in children. Cochrane Database Syst Rev. 2016;7:CD010873.
This paper reviewed electrical stimulation to treat constipation in children. I officially reviewed the protocol for your journal. I was interested to see the review appear.
I have a concern and hope you can help. Most of the graphs in the manuscript appear to be misinterpreted. In my interpretation, they show small advantage to the treatment over control but are reported as small advantage to control. I have checked with my statistician who supports my interpretation of the graphs. Could you please have one of your graph experts check this paper. If I am correct the conclusion of the paper will be reversed.
Please let me know the outcome.
Dr Bridget Southwell (BScHons, MSc, Phd, AGAF)
NHMRC Senior Research Fellow Head of Surgical Research Group Murdoch Childrens Research Institute Royal Children’s Hospital Melbourne
Reply
The forest plot left and right labels were mislabelled by mistake. This error has been corrected and conclusions have been modified as appropriate to read, "The results for the outcomes assessed in this review are uncertain. Thus no firm conclusions regarding the efficacy and safety of TES in children with chronic constipation can be drawn."
Contributors
Nai Ming Lai (Contact author), Nilesh Chande (IBD Group, Cordinating Editor) and John K MacDonald (IBD Group, Managing Editor)
What's new
| Date | Event | Description |
|---|---|---|
| 18 October 2016 | New citation required and conclusions have changed | The conclusions have been revised based on feedback |
| 18 October 2016 | Amended | The forest plots have been corrected and the conclusions revised based on feedback |
Acknowledgements
Partial funding for the Cochrane IBD Group (April 1, 2016 ‐ March 31, 2018) has been provided by Crohn's and Colitis Canada (CCC).
WSL was partly funded by a research grant from the Ministry of Higher Education, Malaysia (UM.C/625/HIR/MOHE/CHAN/13/1).
The authors would like to acknowledge the editors and peer reviewers for their comments on the draft review and John MacDonald for his assistance with copy‐editing the review.
Appendices
Appendix 1. Medline search strategy
Search child*[Title/Abstract]
Search Child[MeSH Terms]
Search Paediatric[Title/Abstract]
Search Adolescent[Title/Abstract]
Search Infant*[Title/Abstract]
Search Neonat*[Title/Abstract]
Search Toddler*[Title/Abstract]
Search (#1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7)
Search constipat*[Title/Abstract]
Search constipation[MeSH Terms]
Search faecal impaction[Title/Abstract]
Search impact*[Title/Abstract]
Search obstipation[Title/Abstract]
Search retent*[Title/Abstract]
Search defecat*[Title/Abstract]
Search evacuat*[Title/Abstract]
Search stool*[Title/Abstract]
Search transit[Title/Abstract]
Search peristal*[Title/Abstract]
Search motility[Title/Abstract]
Search activit*[Title/Abstract]
Search incomplete evaluation[Title/Abstract]
Search strain*[Title/Abstract]
Search (#9 OR #10 OR #11 OR #12 OR #13 OR #14 OR #15 OR #16 OR #17 OR #18 OR #19 OR #20 OR #21 OR #22 OR #23)
Search bowel[Title/Abstract]
Search abdom*[Title/Abstract]
Search (#25 OR #26)
Search function*[Title/Abstract]
Search habit*[Title/Abstract]
Search movement*[Title/Abstract]
Search symptom*[Title/Abstract]
Search motion* [Title/Abstract]
Search (#28 OR #29 OR #30 OR #31 OR #32)
Search #27 AND #33
Search #24 OR #34
Search nerve stimulat*[Title/Abstract]
Search electro‐acupuncture[Title/Abstract]
Search electroacupuncture[Title/Abstract]
Search neuro‐modulation[Title/Abstract]
Search neuromodulation [Title/Abstract]
Search trans‐abdominal stimulat*[Title/Abstract]
Search sacral nerve stimulat*[Title/Abstract]
Search transcutaneous electr* stimulat*[Title/Abstract]
Search interferential electr* stimulat*[Title/Abstract]
Search "medtronic"[Title/Abstract]
Search "SXDZ‐100"[Title/Abstract]
Search "SDZ‐II"[Title/Abstract]
Search "ST 25"[Title/Abstract]
Search "TE 6"[Title/Abstract]
Search "ST 36"[Title/Abstract]
Search "ST 37"[Title/Abstract]
Search (#36 OR #37 OR #38 OR #39 OR #40 OR #41 OR #42 OR #43 OR #44 OR #45 OR #46 OR #47 OR #48 OR #49 OR #50 OR #51)
Search controlled clinical trial[Publication Type]
Search randomized controlled trial[Publication Type]
Search randomized[Title/Abstract]
Search placebo[Title/Abstract]
Search therapy[MeSH Major Topic]
Search randomly[Title/Abstract]
Search trial[Title]
Search ( #53 OR #54 OR #55 OR #56 OR #57 OR #58 OR #59)
Search (animals [mh] NOT humans [mh])
Search (#60 NOT #61)
Search (#8 AND #35 AND #52 AND #62)
Appendix 2. CENTRAL search strategy
#1 child*:ti,ab,kw in Trials #2 MeSH descriptor: [Child] explode all trees #3 paediatric:ti,ab,kw #4 adolescent:ti,ab,kw #5 infant*:ti,ab,kw #6 neonat*:ti,ab,kw #7 toddler*:ti,ab,kw #8 #1 or #2 or #3 or #4 or #5 or #6 or #7 #9 constipat*:ti,ab,kw #10 MeSH descriptor: [Constipation] explode all trees #11 faecal impaction:ti,ab,kw #12 impact*:ti,ab,kw #13 obstipation:ti,ab,kw #14 retent*:ti,ab,kw #15 defecat*:ti,ab,kw #16 evacuat*:ti,ab,kw #17 stool*:ti,ab,kw #18 transit:ti,ab,kw #19 peristal*:ti,ab,kw #20 motility:ti,ab,kw #21 activit*:ti,ab,kw #22 incomplete evacuation:ti,ab,kw #23 strain*:ti,ab,kw #24 #9 or #10 or #11 or #12 or #13 or #14 or #15 or #16 or #17 or #18 or #19 or #20 or #21 or #22 or #23 #25 bowel:ti,ab,kw #26 abdo*:ti,ab,kw #27 #25 or #26 #28 function*:ti,ab,kw #29 habit*:ti,ab,kw #30 movement*:ti,ab,kw #31 symptom*:ti,ab,kw #32 motion*:ti,ab,kw #33 #28 or #29 or #30 or #31 or #32 #34 #27 and #33 #35 #24 or #34 #36 nerve stimulat*:ti,ab,kw #37 electro‐acupuncture:ti,ab,kw #38 electroacupuncture:ti,ab,kw #39 neuro‐modulation:ti,ab,kw #40 neuromodulation:ti,ab,kw #41 trans‐abdominal stimulat*:ti,ab,kw #42 sacral nerve stimulat*:ti,ab,kw #43 transcutaneous electr* stimulat*:ti,ab,kw #44 interferential electr* stimulat*:ti,ab,kw #45 "medtronic":ti,ab,kw #46 "SXDZ‐100":ti,ab,kw #47 "SDZ‐II":ti,ab,kw #48 "ST 25":ti,ab,kw #49 "TE 6":ti,ab,kw #50 "ST 36":ti,ab,kw #51 "ST 37":ti,ab,kw #52 #36 or #37 or #38 or #39 or #40 or #41 or #42 or #43 or #44 or #45 or #46 or #47 or #48 or #49 or #50 or #51 #53 #8 and #35 and #52
Appendix 3. EMBASE search strategy
1. child*: TI,AB
2. exp Child/
3. Paediatric: TI,AB
4. Adolescent: TI,AB
5. Infant*: TI, AB
6. Neonat*: TI,AB
7. Toddler*: TI,AB
8. 1 or 2 or 3 or 4 or 5 or 6 or 7
9. constipat*: TI,AB
10. exp constipation/
11. faecal impaction: TI,AB
12. impact*: TI,AB
13. obstipation: TI,AB
14. retent*: TI,AB
15. defecat*: TI,AB
16. evacuat*: TI,AB
17. stool*: TI,AB
18. transit: TI,AB
19. peristal*: TI,AB
20. motility: TI,AB
21. activit*: TI,AB
22. incomplete evaluation: TI,AB
23. strain*: TI,AB
24. 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23
25. bowel: TI,AB
26. abdom*: TI,AB
27. 25 or 26
28. function*: TI,AB
29. habit*: TI,AB
30. movement*: TI,AB
31. symptom*: TI,AB
32. motion*: TI,AB
33. 28 or 29 or 30 or 31 or 32
34. 27 and 33
35. 24 or 34
36. nerve stimulat*: TI,AB
37. electro‐acupuncture: TI,AB
38. electroacupuncture: TI,AB
39. neuro‐modulation: TI,AB
40. neuromodulation: TI,AB
41. trans‐abdominal stimulat*: TI,AB
42. sacral nerve stimulat*: TI,AB
43. transcutaneous electr* stimulat*: TI,AB
44. inferential electr* stimulat*: TI,AB
45. "medtronic": TI,AB
46. "SXDZ‐100": TI,AB
47. "SDZ‐II": TI,AB
48. "ST 25": TI,AB
49. "TE 6": TI,AB
50. "ST 36": TI,AB
51. "ST 37": TI,AB
52. 36 or 37 or 38 or 39 or 40 or 41 or 42 or 43 or 44 or 45 or 46 or 47 or 48 or 49 or 50 or 51
53. random&: TI,AB
54. cross over*: TI,AB
55. crossover*: TI,AB
56. exp randomized controlled trial/
57. randomized: TI,AB
58. placebo: TI,AB
59. therapy/
60. randomly: TI,AB
61. trial: TI
62. 53 or 54 or 55 or 56 or 57 or 58 or 59 or 60 or 61
63. 8 and 35 and 52 and 62
Data and analyses
Comparison 1. Transcutaneous electrical stimulation versus sham stimulation.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Number of participants with improved complete spontaneous bowel movement (CSBM) of greater than three times per week at two‐month follow‐up | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2 Number of participants with improved colonic transit | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3 Colonic transit rate (geometric centre of radioactive substance) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4 Number of participants with improved symptoms related to soiling | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 5 Number of participants with improved quality of life | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 6 Self‐perceived QoL | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 7 Parent‐perceived QoL | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Chase 2015.
| Methods | Single‐Centre RCT (Australia) | |
| Participants | Children aged 8‐18 years with slow‐transit constipation (STC) for more than 2 years Inclusion criteria: “All children had >2 years chronic constipation not responding to standard medical therapies (diet, laxatives, behaviour modification). STC was diagnosed by radionuclear transit studies performed within the previous year. STC was defined by retention of radioisotope in the ascending/ transverse colon but not rectosigmoid at 48 hours.” Exclusion criteria: “Children with Hirschsprung Disease, celiac disease, hypothyroidism or allergies that may impact on bowel function were excluded Children were excluded after bowel surgery (except for appendix stoma for antegrade colonic enemas), any contraindication to electrical current (eg. cardiac pacemaker), or previous electrical stimulation Children with neurological disorders or children/families with conditions that did not allow them to complete the questionnaires or bowel diaries were also excluded.” Forty‐six children in total were randomised, and 42 completed the study (21 from each group) Two children from each group did not complete the study |
|
| Interventions | Transcutaneous electrical stimulation (TES) delivered by trained physiotherapists using two channels of alternating current, one at a fixed frequency (4 kHz), while the other varied from 4080 to 4150Hz, producing a varying beat frequency of 80‐150 Hz. using 4 electrodes on the participants' belly and back, covering spinal outflow of T9 to L2 Two electrodes were placed paraspinally (T9‐L2), with the paired electrode positioned diagonally opposite on the anterior abdominal wall below the costal margin Stimulation was applied for 20 minutes per session by the physiotherapist, three times per week for four weeks Participants were allocated to receive either real or sham stimulation for four weeks and then were followed up for two months Radioisotope transit studies were performed pre and two months post intervention. Follow‐up period for the study was two months |
|
| Outcomes | Complete spontaneous bowel movement (CSBM), specifically, the number of participants with greater than 3 CSBM per week, soiling, colonic transit rate (measured by the geometric centre position of the radio‐isotope in the bowel) and quality of life (PedsQL) | |
| Notes | This unpublished manuscript reports the same study as five other reports that were identified as eligible studies in this review (Chase 2009a; Clarke 2009; Clarke 2009a; Leong 2011; Southwell 2010) The other articles reported either interim analysis results or selected outcomes of the study, and they are classified as secondary references of this study The study was jointly funded by the National Health and Medical Research Council, Australia (Project Grants 384434, 546432, Senior Research Fellowship 436916‐ BRS) and Murdoch Childrens Research Institute Theme Investment Grants |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomisation, page 7 ”Instructions for active or sham stimulation were randomised (in blocks of 6) and sealed into numbered envelopes before recruitment. For each child recruited, the next envelope was mailed to the treating physiotherapist.” The method employed to generate random sequence was not stated |
| Allocation concealment (selection bias) | Unclear risk | Randomisation, page 7 ”Instructions for active or sham stimulation were randomised (in blocks of 6) and sealed into numbered envelopes before recruitment. For each child recruited, the next envelope was mailed to the treating physiotherapist” There was insufficient description on the generation of random sequence generation to enable an assessment of whether randomisation was performed independently from allocation. It was also unclear whether the envelops used were opaque |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding “Patients and all trial staff (except for treating physiotherapist) were blinded to treatment. Because machines were connected to 240 V power, the treating physiotherapists could not be blinded Physiotherapists were given a written script and trained to present stimulations in identical fashion with both machines and to offer no other advice or intervention, thus ensuring patients received identical treatment with each machine" Active and sham stimulation “For sham stimulation, one machine was factory altered to deliver no current, but with output lights and dials indicating changing intensity levels to match active machines" The authors have stated that treating personnel (physiotherapist) could not be blinded, so the study was judged to have high risk of bias in terms of blinding of personnel The authors made a detailed explanation on the setting up of sham stimulation and measures to standardise the administration of active and sham IFTs to ensure that the patients and/or carers were unaware of the allocation that they received. However, it was unclear how effective the measures were, as the presence or absence of electrical currents might be felt by the patient, hence undermining the effectiveness of the efforts to mask the the patients” |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Blinding ”... physiotherapists mailed the treatment record and daily diary to the trial office. Blinded data entry was performed during the trial (CC, DR) and analysis was performed on conclusion of the trial by staff (KI, HA, YIY) not involved with the patients. The code was broken for final analysis” Despite blinding in data entry and analysis, It appeared that the physiotherapists were the assessors of at least some of the outcomes, including the subjective outcomes of symptoms as would be recorded in the diary. As the physiotherapists were clearly stated to be unblinded, the study was accorded high risk in the domain of blinding of outcome assessment. it was unclear whether the assessors of the other outcomes, such as colonic transit, were blinded to the allocation of the participants |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Four out of 46 participants (two each group) did not complete the trials. The reasons given were: two participants lost their bowel diaries, and two “violated the trial protocol”. It was unclear whether the four participants underwent assessments of other outcomes such as colonic transit study Despite the relatively small number of participants with missing data for the major outcome of CSBM, it appeared that different subsets of the total participant group were included in different outcomes (as presented in different reports of the same study) For example, only 21 participants (14 in the TES group and 7 in the control group) were included in the outcome "number of participants with improved colonic transit, and as low as 16 participants (8 in each group) were included in the outcome (number of participants with improved quality of life) Considering the overall participation rate across all the outcomes, we decided to accord the study high risk under the domain of incomplete outcome data |
| Selective reporting (reporting bias) | Low risk | All major outcomes specified in the methods, including CSBM, soiling, colonic transit rate, soiling, abdominal pain and quality of life (PedsQL) were reported in the results in the primary and/or secondary references |
| Other bias | High risk | In one of the secondary references that reported the outcome of colonic transit (Clarke et al 2009), there were 61 radio imaging studies performed on 26 children, meaning some children undertook multiple studies The studies were taken as the unit of reporting rather than the participants The authors do not appear to have adjusted their data to account for this clustering effect, either by undertaking some form of generalised estimating equation or taking the mean reading of all radio imaging studies for each participant |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Chase 2005 | This was a single‐group pilot study of eight children (7‐16 years) assessing the effects of TESIC in children who had chronic treatment‐resistant constipation and soiling who had failed various treatment options Excluded on the basis of study design |
| Chase 2009 | This was a non‐randomised pilot study that assessed the effectiveness of daily home TESIC in improving the bowel habits of children with slow‐transit constipation This study recruited children who were poor responders in a previous RCT on TESIC and slow‐transit constipation Excluded on the basis of study design |
| Clarke 2012 | This was a non‐randomised single‐group before‐and‐after study evaluating the colonic propagating sequence of a group of children with slow‐transit‐constipation following the application of TESIC Excluded on the basis of study design |
| Dwyer 2014 | A prospective cohort study that evaluated the use of sacral neuro‐modulation in children with dysfunctional elimination syndrome, which included bowel or bladder dysfunction Excluded on the basis on study design and population assessed |
| Ismail 2009 | A non‐randomised follow‐up study that evaluated the effectiveness of daily TES application at home in participants who responded poorly to thrice‐weekly application of TES in an RCT Excluded on the basis of study design |
| Moeller 2015 | A randomised double‐blind controlled trial that evaluated the acute effect of transcutaneous electrical nerve stimulation on rectal motility in children with overactive bladder Excluded on the basis of population |
| Thomas 2013 | A literature review assessing the effect of sacral nerve stimulation in adults and children with slow‐transit constipation Excluded on the basis of article type |
| Yik 2012a | This was a non‐randomised single‐group before‐and‐after study that evaluated the colonic propagating sequence of a group of children with slow‐transit‐constipation following the application of TESIC Excluded on the basis of study design |
| Yik 2012b | This was a non‐randomised single‐group before‐and‐after study that evaluated the clinical symptoms of a group of children with slow‐transit‐constipation following the application of daily TES at home in addition to laxative treatment Excluded on the basis of study design |
| Yik 2012c | This retrospective audit aimed to determine if TES use affected appendicostomy formation rates Excluded on the basis of study design |
| Yik 2013a | A single‐group before‐and‐after study that assessed the effects of TES delivered initially in the physical therapist’s clinic for 4 weeks then at home in 62 children with clinical symptoms related to constipation Published in abstract form Excluded on the basis of study design |
| Yik 2013b | A single‐group non‐comparative study that assessed the effects of TES initially at physical therapist’s clinic for 4 weeks then at home for 3‐6 months in 62 children with clinical symptoms related to constipation Published in abstract form The data set reported were similar to (Yik 2013a) Excluded on the basis of study design |
TESIC: transcutaneous electrical stimulation using interferential current.
TES: transcutaneous electrical stimulation.
Differences between protocol and review
Title change: after comments given by the content expert (YIY) who joined the author team at the review stage, the intervention component of our title was changed from transcutaneous electrical nerve stimulation (TENS) to transcutaneous electrical stimulation (TES) to broaden the scope of the intervention. Changes were made in the corresponding term used throughout the review.
Contributions of authors
WSL and NML conceived the review.
NML and RTN drafted the search strategy.
YIY provided an unpublished manuscript which contained additional information on the conduct of the trial which was not available in other trial reports.
RTN, NML, KMT, HLA , YIY and WSL wrote and revised the review.
Sources of support
Internal sources
University of Malaya Paediatric and Child Health Research Group, Malaysia.
External sources
No sources of support supplied
Declarations of interest
Ruey Terng Ng: None known,
Way Seah Lee: None known
Hak Lee Ang: None known
Kai Ming Teo: has stock or stock options held by investment firms whose investment might or might not include pharmaceutical companies or relevant companies; has received travel expenses from milk companies to to attend paediatric or gastroenterology conferences; and has received funds from milk and drug companies to attend lunch and dinner meetings and conferences. These financial activities are outside the scope of this review.
Yee Ian Yik has an intellectual conflict of interest, being an author of the included study. However, he was not involved in determination of eligibility, risk of bias assessment or data extraction.
Nai Ming Lai: None known
Edited (conclusions changed)
References
References to studies included in this review
Chase 2015 {published and unpublished data}
- Chase J, Gibb S M, Clarke M C C, Catto‐Smith A, Robertson V, Hutson J M, et al. Transcutaneous electrical current to overcome slow transit constipation in children ‐ An RCT. Neurogastroenterology and Motility 2009;21:78. [Google Scholar]
- Chase JW, Clarke MCC, Gibb S, Hutson JM, Catto‐Smith AG, Robertson V, et al. Transcutaneous electrical stimulation to treat childhood slow transit constipation ‐ a randomised placebo controlled trial (Abstract). Australian and New Zealand Continence Journal. 2008:114.
- Chase JW, Clarke MCC, Gibb SM, Catto‐Smith AG, Robertson VJ, King SK, et al. Transabdominal electrical stimulation increases colonic activity in paediatric slow transit constipation. Data on file. [DOI] [PubMed]
- Clarke M C, Chase J W, Gibb S, Robertson V J, Catto‐Smith A, Hutson J M, et al. Decreased colonic transit time after transcutaneous interferential electrical stimulation in children with slow transit constipation. Journal of Pediatric Surgery 2009;44:408‐12. [DOI] [PubMed] [Google Scholar]
- Clarke MC, Chase JW, Gibb S, Hutson JM, Southwell BR. Improvement of quality of life in children with slow transit constipation after treatment with transcutaneous electrical stimulation. Journal of Pediatric Surgery 2009;44:1268‐72; discussion 1272. [DOI] [PubMed] [Google Scholar]
- Leong L C, Yik Y I, Catto‐Smith A G, Robertson V J, Hutson J M, Southwell B R. Long‐term effects of transabdominal electrical stimulation in treating children with slow‐transit constipation. Journal of Pediatric Surgery 2011;46:2309‐12. [DOI] [PubMed] [Google Scholar]
- Leong LCY, Yik YI, Farmer P, Hutson JM, Southwell BR. Long‐term effects of transabdominal electrical stimulation on paediatric slow‐transit constipation. Journal of Gastroenterology and Hepatology 2011;26:91. [Google Scholar]
- Southwell B. Transabdominal electrical stimulation to treat slow transit constipation in children. Neuromodulation 2012;15:63. [Google Scholar]
- Southwell B R. Transabdominal electrical stimulation increases colonic activity in pediatric slow transit constipation: Results from a blinded randomised‐control trial. Gastroenterology 2010;138:S109. [Google Scholar]
- Southwell BR, Clarke MC, Chase J, Hutson JM. Transcutaneous electrical current to overcome slow transit constipation in children. Neurogastroenterology and Motility. Blackwell Publishing Ltd, 2008:735ii. [DOI: 10.1111/j.1365-2982.2008.01121.x] [DOI]
- Yik YI, Clarke MC, Catto‐Smith AG, Robertson VJ, Sutcliffe JR, Chase JW, et al. Slow‐transit constipation with concurrent upper gastrointestinal dysmotility and its response to transcutaneous electrical stimulation. Pediatric Surgery International 2011;27:705‐11. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Chase 2005 {published data only}
- Chase J, Robertson V J, Southwell B, Hutson J, Gibb S. Pilot study using transcutaneous electrical stimulation (interferential current) to treat chronic treatment‐resistant constipation and soiling in children. Journal of Gastroenterology and Hepatology 2005;20:1054‐61. [DOI] [PubMed] [Google Scholar]
Chase 2009 {published data only}
- Chase J, Gibb S, Ismail KA, Clarke MCC, Catto‐Smith AG, Robertson VJ, et al. Daily transcutaneous electrical stimulation (using interferential current) at home increased defecation in children with slow transit constipation: A pilot study. Neurogastroenterology and Motility 2009;21:3. [Google Scholar]
Clarke 2012 {published data only}
- Clarke MC, Catto‐Smith AG, King SK, Dinning PG, Cook IJ, Chase JW, et al. Transabdominal electrical stimulation increases colonic propagating pressure waves in paediatric slow transit constipation. Journal of Pediatric Surgery 2012;47:2279‐84. [DOI] [PubMed] [Google Scholar]
Dwyer 2014 {published data only}
- Dwyer ME, Vandersteen DR, Hollatz P, Reinberg YE. Sacral neuromodulation for the dysfunctional elimination syndrome: a 10‐year single‐center experience with 105 consecutive children. Urology 2014;84:911‐7. [DOI] [PubMed] [Google Scholar]
Ismail 2009 {published data only}
- Ismail KA, Chase J, Gibb S, Clarke M, Catto‐Smith AG, Robertson VJ, et al. Daily transabdominal electrical stimulation at home increased defecation in children with slow‐transit constipation: a pilot study. Journal of Pediatric Surgery 2009;44:2388‐92. [DOI] [PubMed] [Google Scholar]
Moeller 2015 {published data only}
- Moeller Joensson I, Hagstroem S, Siggaard C, Bower W, Djurhuus JC, Krogh K. Transcutaneous electrical nerve stimulation increases rectal activity in children. Journal of Pediatric Gastroenterology and Nutrition 2015;61:80‐4. [DOI] [PubMed] [Google Scholar]
Thomas 2013 {published data only}
- Thomas GP, Dudding TC, Rahbour G, Nicholls RJ, Vaizey CJ. Sacral nerve stimulation for constipation. British Journal of Surgery 2013;100:174‐81. [DOI] [PubMed] [Google Scholar]
Yik 2012a {published data only}
- Yik YI, Ismail KA, Hutson JM, Southwell BR. Home transcutaneous electrical stimulation to treat children with slow‐transit constipation. Journal of Pediatric Surgery 2012;47:1285‐90. [DOI] [PubMed] [Google Scholar]
Yik 2012b {published data only}
- Yik YI, Ismail KA, Hutson JM, Southwell BR. Daily transabdominal electrical stimulation reduces soiling in children with slow‐transit constipation. Gastroenterology 2012;142:S812‐3. [Google Scholar]
Yik 2012c {published data only}
- Yik YI, Leong LC, Hutson JM, Southwell BR. The impact of transcutaneous electrical stimulation therapy on appendicostomy operation rates for children with chronic constipation‐‐a single‐institution experience. Journal of Pediatric Surgery 2012;47:1421‐6. [DOI] [PubMed] [Google Scholar]
Yik 2013a {published data only}
- Yik YI, Ismail K, Hutson J, Southwell B. Home‐based transabdominal electrical stimulation slowly improves treatment‐resistant chronic constipation in children. Neuromodulation 2013;16:e102. [Google Scholar]
Yik 2013b {published data only}
- Yik YI, Ismail KA, Hutson JM, Southwell BR. Transabdominal electrical stimulation using interferential current is able to treat chronic constipation in children. Neuromodulation 2013;16:e13. [Google Scholar]
Additional references
Aboumarzouk 2011
- Aboumarzouk OM, Agarwal T, Antakia R, Shariff U, Nelson RL. Cisapride for intestinal constipation. Cochrane Database of Systematic Reviews 2011, Issue 1. [DOI: 10.1002/14651858.CD007780.pub2] [DOI] [PubMed] [Google Scholar]
Candy 2011
- Candy B, Jones L, Goodman ML, Drake R, Tookman A. Laxatives or methylnaltrexone for the management of constipation in palliative care patients. Cochrane Database of Systematic Reviews 2011, Issue 1. [DOI: 10.1002/14651858.CD003448.pub3] [DOI] [PubMed] [Google Scholar]
Coggrave 2006
- Coggrave M, Wiesel P, Norton CC. Management of faecal incontinence and constipation in adults with central neurological diseases. Cochrane Database of Systematic Reviews 2006, Issue 2. [DOI: 10.1002/14651858.CD002115.pub3] [DOI] [PubMed] [Google Scholar]
Dowswell 2009
- Dowswell T, Bedwell C, Lavender T, Neilson JP. Transcutaneous electrical nerve stimulation (TENS) for pain management in labour. Cochrane Database of Systematic Reviews 2009, Issue 2. [DOI: 10.1002/14651858.CD007214.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Eleouet 2010
- Eleouet M, Siproudhis L, Guillou N, Couedic J, Bouguen G, Bretagne JF. Chronic posterior tibial nerve transcutaneous electrical nerve stimulation (TENS) to treat fecal incontinence (FI). International Journal of Colorectal Disease 2010;25(9):1127‐32. [PUBMED: 20549220] [DOI] [PubMed] [Google Scholar]
Evans 2007
- Evans BW, Clark WK, Moore DJ, Whorwell PJ. Tegaserod for the treatment of irritable bowel syndrome and chronic constipation. Cochrane Database of Systematic Reviews 2007, Issue 4. [DOI: 10.1002/14651858.CD003960.pub3] [DOI] [PubMed] [Google Scholar]
Gordon 2012
- Gordon M, Naidoo K, Akobeng AK, Thomas AG. Osmotic and stimulant laxatives for the management of childhood constipation. Cochrane Database of Systematic Reviews 2012, Issue 7. [DOI: 10.1002/14651858.CD009118.pub2] [DOI] [PubMed] [Google Scholar]
Higgins 2011a
- Higgins JPT, Altman DG, Sterne JAC (editors). Chapter 8: Assessing risk of bias in included studies. In: Higgins JPT, Green S editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org. [Google Scholar]
Higgins 2011b
- Higgins JPT, Deeks JJ, Altman DG (editors). Chapter 16: Special topics in statistics. In: Higgins JPT, Green S editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org. [Google Scholar]
Higgins 2011c
- Higgins JPT, Deeks JJ (editors). Chapter 7: Selecting studies and collecting data. In: Higgins JPT, Green S editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org. [Google Scholar]
Khadilkar 2005
- Khadilkar A, Milne S, Brosseau L, Robinson V, Saginur M, Shea B, et al. Transcutaneous electrical nerve stimulation (TENS) for chronic low‐back pain. Cochrane Database of Systematic Reviews 2005, Issue 3. [DOI: 10.1002/14651858.CD003008.pub3] [DOI] [PubMed] [Google Scholar]
Lee‐Robichaud 2010
- Lee‐Robichaud H, Thomas K, Morgan J, Nelson RL. Lactulose versus polyethylene glycol for chronic constipation. Cochrane Database of Systematic Reviews 2010, Issue 7. [DOI: 10.1002/14651858.CD007570.pub2] [DOI] [PubMed] [Google Scholar]
Lefebvre 2011
- Lefebvre C, Manheimer E, Glanville J. Chapter 6: Searching for studies. In: Higgins JPT, Green S editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org. [Google Scholar]
Mowatt 2007
- Mowatt G, Glazener Cathryn MA, Jarrett M. Sacral nerve stimulation for faecal incontinence and constipation in adults. Cochrane Database of Systematic Reviews 2007, Issue 3. [DOI: 10.1002/14651858.CD004464.pub2] [DOI] [PubMed] [Google Scholar]
Mueller‐Lissner 2010
- Mueller‐Lissner S, Kamm MA, Wald A, Hinkel U, Koehler U, Richter E, et al. Multicenter, 4‐week, double‐blind, randomized, placebo‐controlled trial of sodium picosulfate in patients with chronic constipation. American Journal of Gastroenterology 2010;105(4):897‐903. [PUBMED: 20179697] [DOI] [PubMed] [Google Scholar]
Mugie 2011
- Mugie SM, Lorenzo C, Benninga MA. Constipation in childhood. Nature Reviews. Gastroenterology & Hepatology 2011;8(9):502‐11. [PUBMED: 21808283] [DOI] [PubMed] [Google Scholar]
Mulvey 2010
- Mulvey MR, Bagnall AM, Johnson MI, Marchant PR. Transcutaneous electrical nerve stimulation (TENS) for phantom pain and stump pain following amputation in adults. Cochrane Database of Systematic Reviews 2010, Issue 5. [DOI: 10.1002/14651858.CD007264.pub2] [DOI] [PubMed] [Google Scholar]
NASPGHAN 2006
- NASPGHAN Constipation Guideline Committee. Evaluation and treatment of constipation in infants and children: recommendations of the North American Society for Pediatric Gastroenterology, Hepatology and Nutrition. Journal of Pediatric Gastroenterology and Nutrition 2006;43(3):e1‐13. [PUBMED: 16954945] [DOI] [PubMed] [Google Scholar]
NICE 2010
- National Institute for Health and Care Excellence (NICE). Constipation in children and young people: Diagnosis and management of idiopathic childhood constipation in primary and secondary care. NICE Clinical Guideline 99. May 2010:http://guidance.nice.org.uk/cg99.
Nnoaham 2008
- Nnoaham KE, Kumbang J. Transcutaneous electrical nerve stimulation (TENS) for chronic pain. Cochrane Database of Systematic Reviews 2008, Issue 3. [DOI: 10.1002/14651858.CD003222.pub2] [DOI] [PubMed] [Google Scholar]
Norderval 2011
- Norderval S, Rydningen M, Lindsetmo RO, Lein D, Vonen B. Sacral nerve stimulation. Tidsskrift for Den Norske Legeforening 2011;131(12):1190‐3. [PUBMED: 21694745] [DOI] [PubMed] [Google Scholar]
Price 2001
- Price KJ, Elliot TM. Stimulant laxatives for constipation and soiling in children. Cochrane Database of Systematic Reviews 2001, Issue 3. [DOI: 10.1002/14651858.CD002040] [DOI] [PMC free article] [PubMed] [Google Scholar]
RevMan 2014 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan) 5.3. Version 5.2. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 20124.
ROME III
- Rome Foundation. Rome III diagnostic criteria for functional gastrointestinal disorders. www.romecriteria.org/assets/pdf/19_RomeIII_apA_885‐898.pdf (accessed 28 November 2013). [PubMed]
Rutjes 2009
- Rutjes AWS, Nüesch E, Sterchi R, Kalichman L, Hendriks E, Osiri M, et al. Transcutaneous electrostimulation for osteoarthritis of the knee. Cochrane Database of Systematic Reviews 2009, Issue 4. [DOI: 10.1002/14651858.CD002823.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Schünemann 2011
- Schünemann H, Oxman AD, Higgins JPT, Vist GE, Glasziou P, Guyatt GH. Presenting results and 'Summary of findings' tables. Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org. Vol. 5.1.0, Wiley, 2011:Available from www.cochrane‐handbook.org. [Google Scholar]
Shariff 2009
- Shariff U, Aboumarzouk OM, Nelson RL. Antibiotics for the management of constipation predominant irritable bowel syndrome and chronic constipation. Cochrane Database of Systematic Reviews 2009, Issue 1. [DOI: 10.1002/14651858.CD007518] [DOI] [Google Scholar]
Sluka 2003
- Sluka KA, Walsh D. Transcutaneous electrical nerve stimulation: basic science mechanisms and clinical effectiveness. Journal of Pain 2003;4(3):109‐21. [PUBMED: 14622708] [DOI] [PubMed] [Google Scholar]
Tabbers 2011
- Tabbers MM, Boluyt N, Berger MY, Benninga MA. Clinical practice: diagnosis and treatment of functional constipation. European Journal of Pediatrics 2011;170(8):955‐63. [PUBMED: 21701812] [DOI] [PubMed] [Google Scholar]
van den Berg 2006
- Berg MM, Benninga MA, Lorenzo C. Epidemiology of childhood constipation: a systematic review. American Journal of Gastroenterology 2006;101(10):2401‐9. [PUBMED: 17032205] [DOI] [PubMed] [Google Scholar]
van Wunnik 2011
- Wunnik BP, Baeten CG, Southwell BR. Neuromodulation for constipation: sacral and transcutaneous stimulation. Best Practice and Research. Clinical Gastroenterology 2011;25(1):181‐91. [PUBMED: 21382589] [DOI] [PubMed] [Google Scholar]
van Wunnik 2012
- Wunnik BP, Peeters B, Govaert B, Nieman FH, Benninga MA, Baeten CG. Sacral neuromodulation therapy: a promising treatment for adolescents with refractory functional constipation. Diseases of the Colon and Rectum 2012;55(3):278‐85. [PUBMED: 22469794] [DOI] [PubMed] [Google Scholar]
Walia 2009
- Walia R, Mahajan L, Steffen R. Recent advances in chronic constipation. Current Opinion in Pediatrics 2009;21(5):661‐6. [PUBMED: 19606041] [DOI] [PubMed] [Google Scholar]
Walsh 2009
- Walsh DM, Howe TE, Johnson MI, Sluka KA. Transcutaneous electrical nerve stimulation for acute pain. Cochrane Database of Systematic Reviews 2009, Issue 2. [DOI: 10.1002/14651858.CD006142.pub2] [DOI] [PubMed] [Google Scholar]
Yik 2015 (pers comm)
- Yik 2015. Re: Early draft ‐ Cochrane review of TENS for childhood constipation. E‐mail to: Nai Ming Lai 19 July 2015.


