Abstract
Background
Neck pain is one of the three most frequently reported complaints of the musculoskeletal system. Treatments for neck pain are varied, as are perceptions of benefit. Acupuncture has been used as an alternative to more conventional treatment for musculoskeletal pain. This review summarises the most current scientific evidence on the effectiveness of acupuncture for acute, subacute and chronic neck pain. This update replaces our 2006 Cochrane review update on this topic.
Objectives
To determine the effects of acupuncture for adults with neck pain, with focus on pain relief, disability or functional measures, patient satisfaction and global perceived effect.
Search methods
We searched the Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE, EMBASE, the Manual, Alternative and Natural Therapy Index System (MANTIS), the Cumulative Index to Nursing and Allied Health Literature (CINAHL) and the Index to Chiropractic Literature (ICL) from their beginning to August 2015. We searched reference lists, two trial registers and the acupuncture database Traditional Chinese Medical Literature Analysis and Retrieval System (TCMLARS) in China to 2005.
Selection criteria
We included published trials that used random assignment to intervention groups, in full text or abstract form. We excluded quasi‐randomised controlled trials (RCTs).
Data collection and analysis
Two review authors made independent decisions for each step of the review: article inclusion, data abstraction and assessment of quality of trial methods. We assessed study quality by using the Cochrane Back Review Group 'Risk of bias' tool. We used consensus to resolve disagreements, and when clinical heterogeneity was absent, we combined studies by using random‐effects meta‐analysis models.
Main results
Of the 27 included studies, three represented individuals with whiplash‐associated disorders (WADs) ranging from acute to chronic (205 participants), five explored chronic myofascial neck pain (186 participants), five chronic pain due to arthritic changes (542 participants), six chronic non‐specific neck pain (4011 participants), two neck pain with radicular signs (43 participants) and six subacute or chronic mechanical neck pain (5111 participants).
For mechanical neck pain, we found that acupuncture is beneficial at immediate‐term follow‐up compared with sham acupuncture for pain intensity; at short‐term follow‐up compared with sham or inactive treatment for pain intensity; at short‐term follow‐up compared with sham treatment for disability; and at short‐term follow‐up compared with wait‐list control for pain intensity and neck disability improvement. Statistical pooling was appropriate for acupuncture compared with sham for short‐term outcomes due to statistical homogeneity (P value = 0.83; I2 = 20%). Results of the meta‐analysis favoured acupuncture (standardised mean difference (SMD) ‐0.23, 95% confidence interval (CI) ‐0.20 to ‐0.07; P value = 0.0006). This effect does not seem sustainable over the long term. Whether subsequent repeated sessions would be successful was not examined by investigators in our primary studies.
Acupuncture appears to be a safe treatment modality, as adverse effects are minor. Reported adverse effects include increased pain, bruising, fainting, worsening of symptoms, local swelling and dizziness. These studies reported no life‐threatening adverse effects and found that acupuncture treatments were cost‐effective.
Since the time of our previous review, the quality of RCTs has improved, and we have assessed many of them as having low risk of bias. However, few large trials have provided high‐quality evidence.
Authors' conclusions
Moderate‐quality evidence suggests that acupuncture relieves pain better than sham acupuncture, as measured at completion of treatment and at short‐term follow‐up, and that those who received acupuncture report less pain and disability at short‐term follow‐up than those on a wait‐list. Moderate‐quality evidence also indicates that acupuncture is more effective than inactive treatment for relieving pain at short‐term follow‐up.
Keywords: Humans, Acupuncture Therapy, Chronic Pain, Chronic Pain/etiology, Chronic Pain/therapy, Neck Pain, Neck Pain/etiology, Neck Pain/therapy, Pain Measurement, Pain Measurement/adverse effects, Randomized Controlled Trials as Topic, Treatment Outcome, Whiplash Injuries, Whiplash Injuries/therapy
Acupuncture for neck disorders
Review question
We reviewed the evidence on effects of acupuncture on function, disability, patient satisfaction and global perceived effect among individuals with neck pain.
Background
Neck pain is one of the three most frequently reported complaints of the musculoskeletal system. Treatments for neck pain are varied, as are perceptions of benefit. Acupuncture is sometimes used as an alternative to more conventional treatment for musculoskeletal pain. In this review, acupuncture was defined as stimulation of one or more specific points on the body by insertion of needles to achieve a therapeutic effect. Acupuncture typically includes manual stimulation of needles, but variations are common, such as electrical or heat stimulation of the needles, which is called moxibustion (moxa herb, Artemisia vulgaris, is burned at the handle end of the needle). Injection acupuncture, in which herbal extracts are injected into acupuncture points, is occasionally used as well.
Study characteristics
We included in this review 27 trials (5462 participants) that examined effects of acupuncture for acute to chronic neck pain (lasting a few days to at least three months). Acupuncture was compared with sham acupuncture, wait‐list or inactive treatment (e.g. sham laser). The evidence is current to August 2015.
Key results
Researchers described variability in populations studied, acupuncture techniques used and outcomes measured, so we could not combine the results of these trials to get an overall picture of the effectiveness of acupuncture. Therefore, we could draw only limited conclusions.
Individuals with chronic neck pain who received acupuncture reported better pain relief immediately after treatment and in the short term compared to those who received sham treatments. Individuals with chronic neck pain who received acupuncture reported better pain relief and improvement in disability in the short term than those who were on a wait‐list.
Acupuncture treatments appear to be safe, and investigators have reported only minor and short‐lasting side effects.
Quality of the evidence
The quality of the evidence used to determine whether acupuncture is helpful remains low or moderate. Limitations in the evidence include few study participants, the tendency of researchers to not keep track of who dropped out of the study and they did not make sure that patients who entered the study were randomly assigned to a group. These types of flaws introduce bias into the studies and therefore affect how strongly we believe the results.
Summary of findings
Summary of findings for the main comparison.
| Acupuncture compared with sham for chronic neck pain | ||||||
|
Patient or population: patients with chronic mechanical neck pain (pain for more than 90 days) Settings: varied, mostly at university or hospital clinics Intervention: acupuncture Comparison: sham | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Sham | Acupuncture | |||||
| Pain intensity (VAS) short term | Mean pain intensity ranged across sham groups from 3 points on a 0 to 10 scale to 47 points on a 0 to 100 scale |
Mean pain intensity in intervention groups was 0.23 standard deviations lower (0.20 to 0.07 higher) |
‐0.23 (‐0.20 to ‐0.07) | 560 (8 studies) |
⊕⊕⊕⊝ Moderate Limitations: ‐1 Inconsistency: 0 Indirectness: 0 Imprecision: 0 Other: 0 |
Statistical pooling was appropriate in this instance because of statistical homogeneity. Results of the meta‐analysis favoured acupuncture |
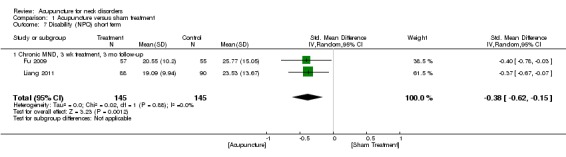
| Disability (NPQ) short term | Mean disability ranged across control groups from 24 points on a 0 to 100 scale to 26 points on a 0 to 100 scale |
Mean disability in intervention groups was 0.38 standard deviations lower (0.62 to 0.15 higher) | ‐0.38 (‐0.62 to ‐0.15) | 290 (2 studies) |
⊕⊕⊝⊝ Low Limitations: ‐1 Inconsistency: 0 Indirectness: 0 Imprecision: ‐1 Other: 0 |
Two small trials were in favour of acupuncture. On the basis of the GRADE scale, quality level of evidence was downgraded to low because only 1 of the 2 studies (50%) was at low risk with small sample size |
| Disability (NDI) short term | Mean disability ranged across control groups from 11 points on a 0 to 100 scale to 15 points on a 0 to 100 scale | Mean disability in intervention groups ranged from 3 points on a 0 to 10 scale to 11 points on a 0 to 100 scale | ‐‐ | 173 (3 studies) | N/A | All 3 studies, 2 with low risk of bias, did not show a statistically significant result in favour of acupuncture |
| Quality of life (SF‐36) short term | Mean quality of life across control groups ranged from 86 points on a 0 to 100 scale to 86 points on a 0 to 100 scale |
Mean quality of life in intervention groups ranged from 84 points on a 0 to 100 scale to 85 points on a 0 to 100 scale |
‐‐ | 178 (1 study) |
⊕⊕⊝⊝ Low Limitations: 0 Inconsistency: 0 Indirectness: ‐1 Imprecision: ‐1 Other: 0 |
One study with low risk of bias favoured acupuncture |
| *The basis for the assumed risk (e.g. median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI) CI: confidence interval; RR: risk ratio | ||||||
| Adverse effects were reported in 14 studies and included increased pain, bruising, fainting, worsening of symptoms, local swelling and dizziness. No life‐threatening adverse effects were noted by these studies. GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate Very low quality: We are very uncertain about the estimate | ||||||
Summary of findings 2.
| Acupuncture compared with inactive treatments for chronic neck pain | ||||||
|
Patient or population: patients with chronic neck pain (pain for more than 90 days) Settings: primary care, general practitioners' clinics to secondary care, outpatient pain clinics or speciality clinics Intervention: acupuncture Comparison: inactive treatments | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Inactive treatment | Acupuncture | |||||
| Pain intensity (VAS) short term | Mean pain intensity ranged across control groups from 17 points on a 0 to 100 scale to 31 points on a 0 to 100 scale |
Mean pain intensity in intervention groups was 17 points on a 0 to 100 scale to 9 points on a 0 to 10 scale |
‐‐ | 404 (5 studies) |
⊕⊕⊕⊝ Moderate Limitations: 0 Inconsistency: 0 Indirectness: 0 Imprecision: ‐1 Other: 0 |
Five studies (n = 461) assessed participants with mechanical neck disorders. Four were at low risk of bias. Statistical pooling was inappropriate in this instance because of statistical heterogeneity. Four of these studies favoured acupuncture |
| Pain pressure threshold short term | Mean pain pressure threshold ranged across control groups from 0 points on a 0 to 10 scale to 7 points on a 0 to 10 scale |
Mean pain pressure threshold in intervention groups ranged from 0.2 points on a 0 to 10 scale to 7 points on a 0 to 10 scale |
‐‐ | 132 (2 studies) |
N/A | Two studies with low risk of bias did not favour acupuncture |
|
Disability (NDI) short term Function (NPQ) short term |
Mean disability ranged across control groups from 12 points on a 0 to 100 scale to 13 points on a 0 to 100 scale Mean function across control groups was 13 points on a 0 to 100 scale |
Mean disability in intervention groups ranged from 11 points on a 0 to 100 scale to 12 points on a 0 to 100 scale Mean function in intervention groups was 30 points on a 0 to 100 scale |
‐‐ | 118 (1 study) 123 (1 study) |
N/A ⊕⊕⊝⊝ Low Limitations: 0 Inconsistency: 0 Indirectness: ‐1 Imprecision: ‐1 Other: 0 |
One study with low risk of bias did not favour acupuncture One study with low risk of bias favoured acupuncture |
| Quality of life (SF‐36, Functional Component) short term | Mean function ranged across control groups from 0.7 points on a 0 to 10 scale to 5 points on a 0 to 10 scale |
Mean function in intervention groups ranged from 41 points on a 0 to 100 scale to 9 points on a 0 to 10 scale |
‐‐ | 143 (2 studies) |
N/A | Two studies with low risk of bias did not favour acupuncture |
| *The basis for the assumed risk (e.g. median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI) CI: confidence interval; RR: risk ratio | ||||||
| Adverse effects were reported in 14 studies and included increased pain, bruising, fainting, worsening of symptoms, local swelling and dizziness. No life‐threatening adverse effects were noted by these studies. GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate Very low quality: We are very uncertain about the estimate | ||||||
Summary of findings 3.
| Acupuncture compared with wait‐list control for chronic neck pain | ||||||
|
Patient or population: patients with chronic neck pain (pain for more than 90 days) Settings: primary care newspaper advertisement or recruited through participating physicians Intervention: acupuncture Comparison: wait‐list control | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Wait‐list control | Acupuncture | |||||
| Pain intensity (VAS) short term | Mean pain intensity across control groups was 5 points on a 0 to 10 scale |
Mean pain intensity in intervention groups was 4 points on a 0 to 10 scale | ‐‐ | 30 (1 study) |
⊕⊕⊕⊝ Moderate Limitations: 0 Inconsistency: 0 Indirectness: ‐1 Imprecision: 0 Other: 0 |
One trial with low risk of bias showed a small reduction in pain. Moderate evidence supporting acupuncture is helpful |
| Disability (neck and pain disability scale) short term | Mean disability across control groups was 6 points on a 0 to 100 scale | Mean disability in intervention groups was 29 points on a 0 to 100 scale |
‐‐ | 3451 (1 study) |
⊕⊕⊕⊝ Moderate Limitations: 0 Inconsistency: 0 Indirectness: ‐1 Imprecision: 0 Other: 0 |
One large study with low risk of bias favoured acupuncture |
| Quality of life (SF‐36 mental score) short term | Mean quality of life score across control groups was 1 point on a 0 to 10 scale | Mean quality of life score in intervention groups was 4 points on a 0 to 10 scale |
‐‐ | 3451 (1 study) |
N/A | One large study showed no statistically significant findings in favour of acupuncture |
| *The basis for the assumed risk (e.g. median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI) CI: confidence interval; RR: risk ratio | ||||||
| Adverse effects were reported in 14 studies and included increased pain, bruising, fainting, worsening of symptoms, local swelling and dizziness. No life‐threatening adverse effects were noted by these studies Cost of care was calculated in 1 study, which found that acupuncture treatment was cost‐effective GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate Very low quality: We are very uncertain about the estimate | ||||||
Background
Description of the condition
Neck pain is a common health impairment among individuals of all ages in the general population (Cote 2004; Haldeman 2008; Hogg‐Johnson 2008; Miller 2010). In fact, according to Haldeman 2008, “most people can expect to experience some degree of neck pain in their lifetime”. The prevalence of neck pain in adults over a 12‐month period ranges from 30% to 50% (Carroll 2008; Hogg‐Johnson 2008). Furthermore, neck pain is a commonly recurring condition. Neck pain appears to be episodic in nature and therefore frequently recurs in 50% to 80% of people one to five years after a prior incident (Carroll 2008; Cote 2004). Symptoms of neck pain range from mildly discomforting to severely disabling and can interfere with daily activities and quality of life. Moreover, incidents of neck pain can be associated with headache, arm pain or even neurological or sensory deficits (Haldeman 2008). Neck pain has a substantial impact on healthcare costs; the economic burden of neck pain is widespread because it affects patients, insurers, governments and employers through sick leave, disability, visits to healthcare providers and loss of productivity (Haldeman 2008; Haraldsson 2006; Miller 2010).
Description of the intervention
A variety of conventional treatments are used to address neck pain, including massage, physiotherapy, exercise, muscle relaxants and steroid injections (Fu 2009SR; Haraldsson 2006; Irnich 2001). Acupuncture has been used increasingly as an alternative to more conventional treatment for musculoskeletal pain. It is defined as stimulation of a certain point or points on the body by insertion of needles to achieve a therapeutic effect. Acupuncture typically includes manual stimulation of needles, but variations are commonly used, such as electrical and heat stimulation of needles, which is called moxibustion (the moxa herb Artemisia vulgaris is burned at the handle end of the needle).
How the intervention might work
Research evidence indicates that acupuncture involves the release of neurotransmitters and hormones such as endorphins (Han 2004), serotonin (Zhang 2012) and adenosine triphosphate (ATP) (Goldman 2010).
Best evidence suggests that the release of β‐endorphin triggered by acupuncture acts both as a neurotransmitter involved in central descending pain inhibitory pathways and as a hormone released into the blood flow. In addition, evidence indicates that central release of dynorphines and the expression level of the opioid antagonist cholecystokinin octapeptide (CCK‐8) (Tang 1997) may play a role in central mechanisms of acupuncture‐induced analgesia. In the peripheral nervous system, β‐endorphin seems to be released from keratinocytes when activated by increased extracellular endocannabinoid concentrations after acupuncture in an inflammatory pain model (Chen 2009).
Likewise, serotonin is known to be involved in the analgesic effect of acupuncture by affecting transmission of pain signals at central and peripheral levels. Similar to oestrogen, serotonin seems to be indirectly involved in the antinociceptive effect of acupuncture by sensitising peripheral afferents and thereby activating endogenous pain control. In contrast, an increase in extracellular ATP concentration may act directly on afferent neurons expressing purinergic receptors, leading to nerve fibre activation, which in turn causes antinociceptive spinal or supraspinal reactions.
Such mechanisms of endogenous pain control triggered by Aδ‐ and C‐fiber activation are generally distinguished according to the respective neural structures and neurotransmitters involved and are termed diffuse noxious inhibitory control (DNIC), segmental inhibition and descending pain control pathways (Zhao 2008).
Effects of acupuncture on muscles and fascia have also been described (Langevin 2006). When effects of acupuncture are approached from the perspective of mechanical tissue manipulation, it can be concluded that existing evidence shows effects of acupuncture on structure and alignment of connective tissue or fasciae (Langevin 2006). Conversely, a reduction in muscle tone through acupuncture has been proposed, but this proposal is based mainly on observations of clinical improvement after acupuncture, such as increased cervical range of motion in patients with neck pain (Irnich 2001). Moreover, recent brain imaging studies have revealed that acupuncture alters brain activation patterns in areas associated with pain processing (Huang 2012SR).
Why it is important to do this review
According to several existing reviews, including our own (Trinh 2006), moderate‐quality evidence indicates that acupuncture is effective in the short term for relieving neck pain (Fu 2009; Furlan 2012; Graham 2013; Gross 2007; Vernon 2009). Randomised controlled trials (RCTs) included in these reviews were based on small population samples (Irnich 2011; Linde 2007), and more recent studies are likely to have used improved methods.
Given the heavy public health and economic burden caused by neck pain and the fact that many sufferers consult complementary and alternative medicine practitioners for relief of their symptoms, a systematic review with new and updated evidence of these practices was justified. The purpose of this review was to include more recent studies in an effort to reveal updated evidence for the use of acupuncture to relieve neck pain and to examine long‐term effects that were absent from previous studies. This review summarises the most current scientific evidence on the effectiveness of acupuncture for acute, subacute and chronic neck pain.
Objectives
To determine the effects of acupuncture for adults with neck pain, with focus on pain relief, disability or functional measures, patient satisfaction and global perceived effect.
Methods
Criteria for considering studies for this review
Types of studies
We included published randomised controlled trials (RCTs) in full text or abstract form. We included abstracts if sufficient information for analyses could be obtained from study authors. We excluded quasi‐RCTs and clinical controlled trials (CCTs) because we found numerous RCTs for this update. This is different from the approach presented in the protocol.
Types of participants
Participants were adults (18 years or older) with the following neck disorders.
Mechanical neck disorders (MNDs), including whiplash‐associated disorders (WADs) categories 1 and 2 (Spitzer 1987; Spitzer 1995), myofascial pain syndrome (MPS) and degenerative changes (DCs) (Schumacher 1993).
Neck disorder with headache (Olesen 1988; Olesen 1997; Sjaastad 1990).
Neck disorders with radicular symptoms (NDRs), including WAD category 3 (Spitzer 1987; Spitzer 1995).
For the purposes of this review, we defined symptom duration as acute (< 30 days), subacute (30 days to 90 days) or chronic (≥ 90 days).
We excluded studies if they investigated neck disorders with:
definite or possible long tract signs (e.g. myelopathies);
neck pain caused by other pathological entities (Schumacher 1993);
neck pain related to neurological disease (e.g. spasmodic torticollis);
neck pain related to fracture and dislocation;
headache not of cervical origin;
co‐existing headache when neck pain was not dominant or when headache was not provoked by neck movement or sustained neck posture; or
'mixed' headache.
Types of interventions
Studies must have used acupuncture techniques involving insertion of needles. Stimulation of needles may involve manual, electrical, heat, laser or other forms of stimulation. Control groups were treated with sham acupuncture (some form of mock or pretend), wait‐list control or inactive treatment control (e.g. sham transcutaneous electrical nerve stimulation (TENS)).
Types of outcome measures
Primary outcomes
Pain relief (e.g. visual analogue scale (VAS), numerical rating scale (NRS)), disability or functional measures (e.g. Neck Disability Index (NDI), quality of life (e.g. Short Form (SF)‐36), activities of daily living (ADLs)), patient satisfaction questionnaires and global perceived effect were the outcomes of interest.
Secondary outcomes
When available, we examined adverse effects and costs of treatment.
The duration of the follow‐up period was defined as:
immediately post treatment: up to one day;
short‐term follow‐up: between one day and three months;
intermediate‐term follow‐up: longer than three months to less than one year; or
long‐term follow‐up: one year and longer.
Search methods for identification of studies
Electronic searches
We searched the following databases from their inception to August 2015.
Cochrane Central Register of Controlled Trials (CENTRAL, which includes the Cochrane Back Review Group (CBRG) Trials Register; Ovid, August 2015).
MEDLINE (Ovid, 1950 to August 2015 week 4).
EMBASE (Ovid, 1980 to August 2015).
Manual, Alternative and Natural Therapy Indexing System (MANTIS; Ovid, 1980 to November 2013 last available access date).
Cumulative Index to Nursing and Allied Health Literature (CINAHL; EBSCO, 1982 to August 2015).
Index to Chiropractic Literature (ICL; August 2015).
ClinicalTrials.gov (August 2015).
World Health Organization (WHO) International Clinical Trials Registry Platform (ICTRP) (August 2015).
The Chinese Cochrane Centre searched the Traditional Chinese Medical Literature Analysis and Retrieval System (TCMLARS) in China in September 2005. We did not further update the TCMLARS search, as this search yielded no RCTs previously.
See Appendix 1 for the search strategies used for CENTRAL, MEDLINE, EMBASE, MANTIS, CINAHL and ICL. Subject headings (MeSHs) and keywords included anatomical terms, disorder or syndrome terms, treatment terms and methodological terms consistent with those advised by the CBRG (Furlan 2009).
Searching other resources
We also screened references, communicated with the Trials Search Co‐ordinator of the CBRG, contacted identified content experts and reviewed our own personal files.
Data collection and analysis
We used standard methodological procedures as expected by The Cochrane Collaboration and the CBRG.
Selection of studies
At least two review authors independently identified citations, selected studies and abstracted data. We resolved disagreements through consensus.
If additional information was required to assess the appropriateness of a study for selection, we contacted study authors for clarification. If this was not forthcoming, we allowed a consensus process to determine selection status. If the article or citation posting was written in a non‐English language, one investigator and a translator with a health sciences background conducted study selection in an unblinded manner.
Data extraction and management
Two review authors independently extracted raw data for demographics, descriptions of treatment and all outcomes from full manuscripts onto pre‐designed forms.
Using the Chi2 test, we calculated agreement between investigators for study identification, selection and validity processes before reaching consensus (Graham 2012). We used the quadratic weighted kappa statistic (Kw) (Cicchetti 1976) to measure agreement.
Assessment of risk of bias in included studies
At least two review authors independently assessed each selected study for methodological quality using pre‐piloted forms based on the CBRG risk of bias (RoB) assessment tool (12 criteria) (Furlan 2009). See Appendix 2 for operationalisation of the RoB tool. We rated each item as having high, low or unclear risk and entered ratings into the RoB table. A consensus team met to reach a final assessment based on an overview of RoB items; we used no pre‐defined cutoff score for the RoB assessment. We deemed an RCT acceptable for inclusion if we found no fatal methodological flaws (e.g. randomisation, allocation concealment, drop‐outs, intention‐to‐treat (ITT) analyses were done appropriately and were well reported).
Measures of treatment effect
We used descriptive statistics to provide a summary description of groups, interventions, outcomes, adverse effects of treatment and costs of care. We reported results on the basis of the sample size analysed.
We calculated standardised mean differences (SMDs) and 95% confidence intervals (95% CIs) for outcomes reported in a continuous data format. We used the SMD because different measures were frequently used to address the same clinical outcome. Effect size (SMD) is a unitless measure reported in standard deviation units. Generally, effect size can be interpreted as small (‐0.20), medium (‐0.50) or large (‐0.80), as defined by Cohen (Cohen 1988).
For dichotomous outcomes, we calculated risk ratios (RRs) and 95% CIs for outcome rates in the treatment versus control group. For undesirable outcomes, RR less than one represents a beneficial treatment.
When neither continuous nor dichotomous data were available, we extracted findings and statistical significance as reported by authors of the original study and noted them in the Characteristics of included studies tables.
Unit of analysis issues
For clinical trials using a simple parallel‐group design, we collected from each participant and analysed a single measurement for each outcome. For clinical trials using a cross‐over design, we collected from each participant and analysed measurements of each outcome for each participant from each of the interventions. We analysed only the first phase of the cross‐over study and included no cluster‐randomised trials in this review.
Dealing with missing data
When data were not extractable, we contacted the primary authors.
When neither continuous nor dichotomous data were available, we extracted findings and presented statistical significance as reported by study authors.
Assessment of heterogeneity
We considered the following possible sources of heterogeneity: symptom duration (acute vs chronic); subtype of neck pain (e.g. WAD); intervention type (traditional acupuncture vs trigger point needling); characteristics of treatment (e.g. dosage, technique); and outcomes (pain relief, measures of function and disability, patient satisfaction, quality of life).
A P value for the Chi2 test (test of heterogeneity) less than 0.05 or an I2 value greater than 25% would indicate significant statistical heterogeneity. However, because an acupuncture review includes few studies, the test of heterogeneity might not have the power to detect a difference even when one exists; therefore, we determined that subgroups were statistically heterogeneous if I2 values were greater than 25% despite failure to reject the null hypothesis with the Chi2 test.
Assessment of reporting biases
When a published protocol was available, we compared outcomes reported a priori with outcomes of interest in the RCT.
Data synthesis
Before calculating a pooled effect measure, we assessed the appropriateness of pooling on clinical grounds. We planned to combine outcome measures from individual trials by performing a meta‐analysis when possible (clinical comparability of populations, interventions and outcomes between trials). We planned to use a random‐effects model for these meta‐analyses.
We considered each subgroup (e.g. 1.1) to be clinically homogeneous. We meta‐analysed each subgroup unless we noted statistical heterogeneity. When a meta‐analysis was not possible, we described qualitatively in the text the results of clinically comparable trials.
Regardless of whether available data were sufficient for use in quantitative analyses to summarise the data, we assessed the overall quality of the evidence for each outcome. To accomplish this, we used the GRADE (Grades of Recommendation, Assessment, Development and Evaluation Working Group) approach, as recommended in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011) and adapted in the updated CBRG method guidelines (Furlan 2009). We considered that the following factors may decrease the quality of the evidence, study design and risk of bias, inconsistency of results, indirectness (not generalisable), imprecision (sparse data) and other factors (e.g. reporting bias). We reduced our rating of the quality of the evidence for a specific outcome by one level according to the performance of studies against these five factors.
High‐quality evidence: Findings are consistent among at least 75% of RCTs with low risk of bias; consistent, direct and precise data; and no known or suspected publication bias. Further research is unlikely to change the estimate or our confidence in the results.
Moderate‐quality evidence: One of the domains is not met. Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate.
Low‐quality evidence: Two domains are not met. Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate.
Very low‐quality evidence: Three domains are not met. We are very uncertain about the results.
No evidence: We identified no RCTs that addressed this outcome.
Subgroup analysis and investigation of heterogeneity
We did not plan to perform a subgroup analysis.
Sensitivity analysis
We planned to conduct a sensitivity analysis on risks of bias or meta‐regression by type of neck pain and duration of symptoms. However, we did not find sufficient data for any of these categories.
Results
Description of studies
We selected 27 trials (N = 5462) for inclusion in this review (Figure 1). Duration of the disorder and disorder subtypes were as follow.
Figure 1.
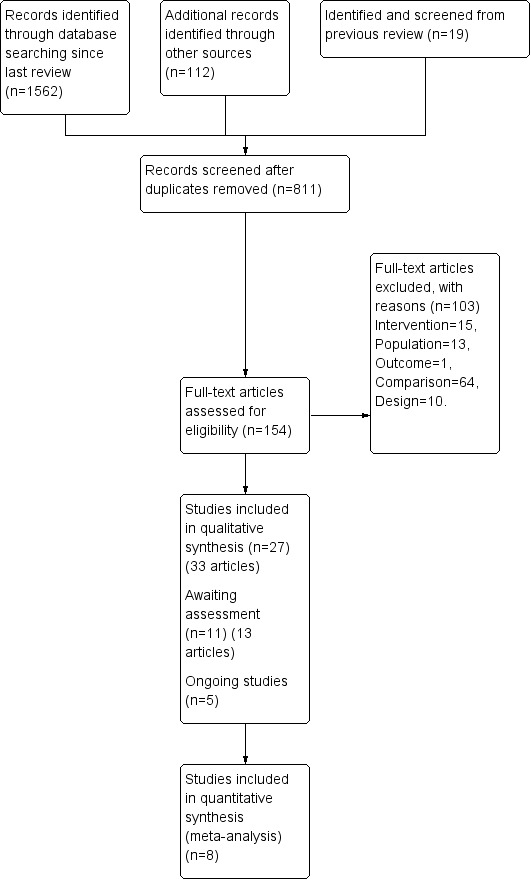
Study flow diagram.
Acute and subacute WAD (n = 1) (Tough 2010).
Subacute and chronic WAD (n = 2) (Cameron 2011; Kwak 2012).
Chronic myofascial neck pain (n = 5) (Birch 1998; Chou 2009; Ilbuldu 2004; Sun 2010; Tsai 2010).
Chronic pain due to osteoarthritic cervical degenerative changes (n = 5) (Fu 2009; Liang 2009; Thomas 1991; White 2000; White 2004).
Chronic non‐specific neck pain (n = 6) (He 2004; He 2005; Itoh 2007; Nabeta 2002; Vas 2006; Witt 2006).
Neck pain with radicular findings (n = 2) (Coan 1982; Petrie 1983).
Subacute or chronic mechanical neck pain (n = 6) (Irnich 2001; Irnich 2002; Liang 2011; Petrie 1986; Sahin 2010; Seidel 2002).
Results of the search
We identified and screened 1562 citation postings and retrieved 154 studies for more detailed evaluation. We included 27 RCTs in this review (Figure 1). We identified no RCTs through the Chinese language search. Additionally, five studies were protocols (Calamita 2015; Kim 2014; Liang 2012; Que 2013; Sun 2014) and two were conference proceeding abstracts (Amos 2012; Liguori 2012) that are awaiting assessment. One study is awaiting translation (Simma‐Kletscha 2009), and four further studies are awaiting completion (Bar‐Haim 2012; Cerezo‐Tellez 2014; Choi 2011; Guo 2014). We found three studies that provided additional analyses for the primary study (see Witt 2006). We found four studies after analysis was complete; these are also awaiting assessment (Mejuto‐Vázquez 2014; Sterling 2015; Wilke 2014; Zhang SP 2013).
See Characteristics of included studies tables for additional details on study design, numbers randomised/analysed, treatments selected, co‐interventions provided, absolute benefits noted, results reported, SMDs, RRs, ITT analyses, side effects and costs of care. Agreement between pairs of independent review authors from diverse professional backgrounds regarding inclusion of studies was excellent, with an estimated Kw = 0.9425 (standard error 0.020).
Included studies
Of the 27 included studies, three represented individuals with WAD (205 participants), five chronic myofascial neck pain (186 participants), five chronic pain due to arthritic changes (n = 506), six chronic non‐specific neck pain (4011 participants), two neck pain with radicular signs (43 participants) and six subacute or chronic mechanical neck pain (511 participants).
Excluded studies
We excluded 103 trials after reviewing the full report. Of these, we excluded 13 studies on the basis of participant characteristics: Two RCTs included participants with a neck disorder excluded from this review (i.e. ankylosing spondylitis) (Emery 1986) and spinal cord stenosis (Li 2006); three included headaches not of cervical origin (Coeytaux 2005; Venancio 2008; Venancio 2009); seven included participants with pain from other areas as well (head, shoulder or back) (Gallacchi 1981; Gallacchi 1983; Gaw 1975; Giles 2003; Kisiel 1996; Lundeburg 1988; Muller 2005); and one included participants who did not have neck pain (Sato 2014). Furthermore, we excluded two abstracts (Johnson 2000; Teng 1973) because they did not appear to describe RCTs. We excluded 64 studies on the basis of the comparison performed: Six studies included acupuncture as the control (Fernandez‐Carnero 2014; Guo 2013; Harvey 2015; Li 2013; Wang G 2014; Zhang J 2013); 31 compared acupuncture types (Ceccherelli 2006; Ceccherilli 2014; Dong 2012; Fu 2007; Gil 2015; Huang 2008; Jia 2007; Jin 2012; Kai 2008; Li 2004; Liu 2008; Lixing 2000; Lu 2006; Myburgh 2012; Nakajima 2015; Pecos‐Martin 2015; Sator‐Katzenschlager 2003; Shang 2002; Shuangquan 2003; Sun 2013; Wan 2013; Wang 2007; Wang 2008; Xu 2012; Yang 2009; Yoon 2009; Yu 2003; Zeng 2005; Zhao 2004; Zhu 2006; Zhuang 2004); 27 compared acupuncture versus active treatment (Bahadir 2009; Cho 2014; David 1998; Edwards 2003; Eroglu 2013; Falkenberg 2007; Franca 2008; Fu 2005; Fu 2014; Ga 2007b; Giles 1999; Hu 2014; Huang 2012; Hudson 2010; Li 2006; Liu 2013; MacPherson 2013; McLean 2013; Rayegani 2014; Salter 2006; Tobbackx 2013; Yang 2013; Yoshimizu 2012; Zhang 2003; Zhang J 2008; Zhou 2014; Ziaeifar 2014). In addition, we excluded 15 RCTs on the basis of the intervention provided: eight by type (i.e. EMG needle, mini‐scalpel, injection needle) (Calvo‐Trujillo 2013; Chu 1997; Lin 2004; Ma 2010; Seo 2014; Zhang X‐Z 2013; Zheng 2014; Zhi 2008) and seven additional studies that used acupuncture as part of a multi‐modal approach (Cohen 2014; Gallego Sendarrubias 2015; Guanygue 2001; Hayek 2014; Hudson 2010; Lundeburg 1991; Soderlund 2001) and could not isolate the acupuncture effect. We excluded eight studies because they were not randomised or were quasi‐randomised (Ga 2007a; Hua 2009; Loy 1983; Luo 2010; Pan 2008; Peng 1987; Xue 2007; Zhang 1996). We excluded one study because investigators did not perform between‐group comparisons (Zhu 2002). (See Characteristics of excluded studies tables.)
Risk of bias in included studies
We assessed methodological quality using CBRG guidelines (Furlan 2009). Please see Figure 2 for these results. We assessed 12 of the 27 included studies (44%) as having fatal flaws, including selection, performance, attrition (related to lack of ITT principles) and reporting biases. Other potential sources of bias included inadequate reporting of co‐interventions and participant compliance.
Figure 2.
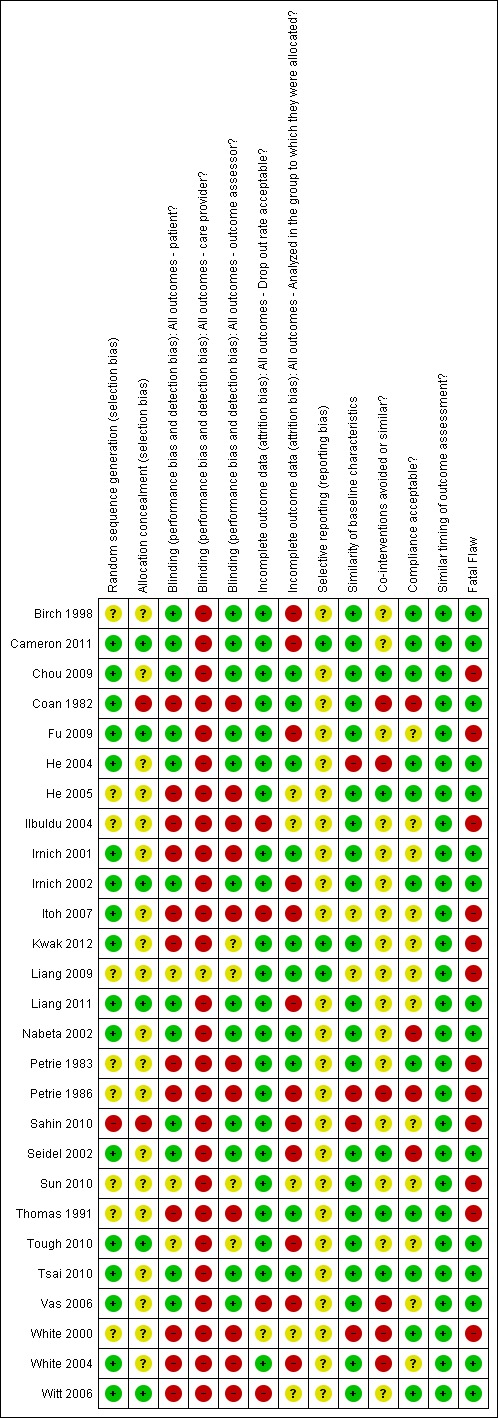
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
We found that six of the 27 included studies had low risk of bias on the basis of allocation; 19 had uncertain risk of bias; and two had high risk of bias. We discussed effects of risks of bias on review results for each subgroup separately under Effects of interventions.
Blinding
We found that 12 of the 27 included studies had low risk of bias on blinding of participants; 12 studies had uncertain risk of bias, and three had high risk of bias. We discussed effects of risks of bias on review results for each subgroup separately under Effects of interventions.
Incomplete outcome data
We found that two of the 27 included studies had low risk of bias on drop‐out rate; four studies had uncertain risk of bias, and one had high risk of bias. We discussed effects of risks of bias on review results for each subgroup separately under Effects of interventions.
Selective reporting
We found that three of the 27 included studies had low risk of bias; 24 studies had uncertain risk of bias, and no study had high risk of bias. We discussed effects of risks of bias on review results for each subgroup separately under Effects of interventions.
Other potential sources of bias
We assessed 12 of the 27 included studies (44%) as having fatal flaws, including selection, performance, attrition (related to lack of ITT principles) and reporting biases. Other potential sources of bias included inadequate reporting of co‐interventions and participant compliance.
Effects of interventions
See: Table 1; Table 2; Table 3
Acupuncture versus sham acupuncture
Pain intensity (VAS) post treatment
Eleven studies (n = 712) included participants with mechanical neck disorders or myofascial pain syndrome. Eight of these eleven studies favoured acupuncture over sham acupuncture. One study (Sahin 2010) did not favour acupuncture. However, this study had a fatal methodological flaw involving randomisation issues and the small number of participants recruited compared with the number of participants needed for its sample size calculation. This study was terminated early and is considered to have high risk of bias. Itoh 2007 studied two methods of acupuncture compared with sham acupuncture. The trigger point treatment was significantly different from sham, and the standard acupuncture treatment was not significantly different from sham. We considered this study to have high risk of bias. Thomas 1991, a study with high risk of bias, also did not favour acupuncture for individuals with osteoarthritis.
These studies involved various methods of sham acupuncture or pretend acupuncture treatments. In some studies, sham group needles did not penetrate the skin (Chou 2009; Itoh 2007). Some studies defined their sham treatments as superficial needle insertions (Fu 2009; Sun 2010; Thomas 1991; Tsai 2010); three studies use a sham control group for whom needles were placed at some distance (1 to 2 cm) from the acupuncture points (He 2004; Liang 2011; Sahin 2010) or in a remote dermatome (White 2000). Birch 1998 used predetermined irrelevant points in his control group.
We considered five of these 11 studies to have low risk of bias (Birch 1998; Chou 2009; He 2004; Liang 2011; Tsai 2010) and six studies to have high risk of bias (Fu 2009; Itoh 2007; Sahin 2010; Sun 2010; Thomas 1991; White 2000).
Statistical pooling was inappropriate in this instance because of statistical heterogeneity (P value = 0.00001; I2 = 83%). Moderate‐quality evidence suggests that acupuncture is beneficial for individuals with chronic mechanical neck pain for pain intensity immediately following treatment. (Please see Analysis 1.1.) On the basis of the GRADE scale, we downgraded the quality level of evidence to moderate because only five of the 11 studies (46%) presented low risk.
Analysis 1.1.
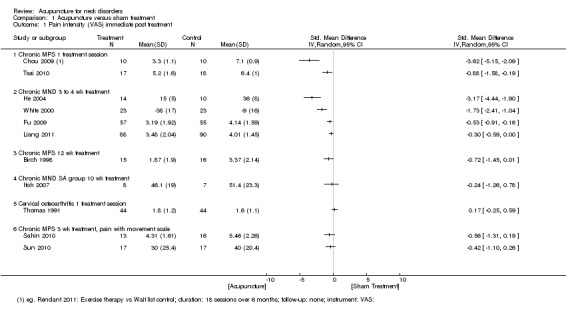
Comparison 1 Acupuncture versus sham treatment, Outcome 1 Pain intensity (VAS) immediate post treatment.
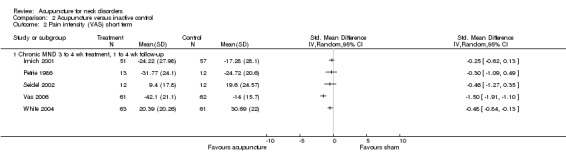
Pain intensity (VAS) short term
We assigned eight studies (n = 560) (Cameron 2011; Fu 2009; Liang 2011; Nabeta 2002; Sahin 2010; Sun 2010; Tough 2010; Itoh 2007) to this category. (Please see Analysis 1.2.) Statistical pooling was appropriate in this instance because of statistical homogeneity (P value = 0.83; I2 = 0%). Results of the meta‐analysis favoured acupuncture (P value = 0.006). We considered four studies (Fu 2009; Itoh 2007; Sahin 2010; Sun 2010) to have high risk of bias. On the basis of the GRADE scale, we downgraded the quality level to moderate because only four of the eight studies (50%) presented low risk.
Analysis 1.2.
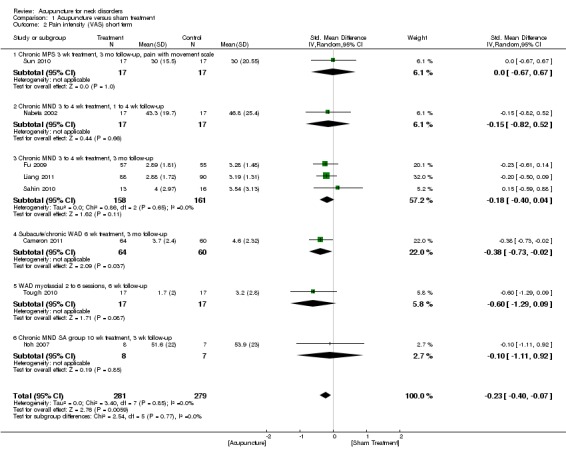
Comparison 1 Acupuncture versus sham treatment, Outcome 2 Pain intensity (VAS) short term.
Pain intensity (VAS) intermediate term
Two studies (n = 158) presented low risk of bias: one involving participants with whiplash (Cameron 2011) and the other involving participants with mechanical neck disorders (He 2004). Both studies favoured acupuncture. (Please see Analysis 1.3.) Statistical pooling was inappropriate in this instance because of statistical heterogeneity (P value = 0.06; I2 = 71%). On the basis of the GRADE scale, we downgraded the quality level of evidence to moderate as the result of imprecision.
Analysis 1.3.
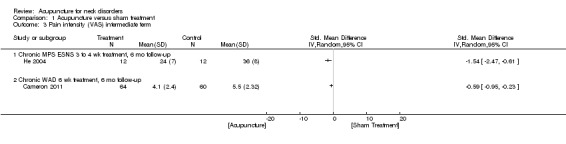
Comparison 1 Acupuncture versus sham treatment, Outcome 3 Pain intensity (VAS) intermediate term.
Pain intensity (VAS) long term
One study (n = 24) with low risk of bias involved participants with mechanical neck disorders (He 2004). This study favoured acupuncture. (Please see Analysis 1.4.)
Analysis 1.4.
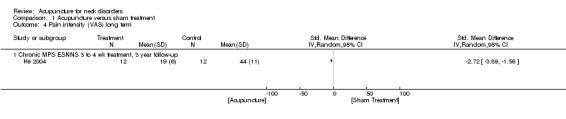
Comparison 1 Acupuncture versus sham treatment, Outcome 4 Pain intensity (VAS) long term.
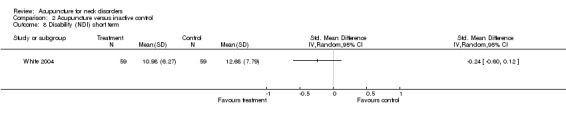
Disability and quality of life
No convincing evidence favoured acupuncture in all other measures such as disability (NDI) or quality of life over the short term, the intermediate term or the long term. (Please see Analysis 1.5, Analysis 1.6, Analysis 1.7, Analysis 1.8, Analysis 1.9, Analysis 1.10, and Analysis 1.11.) Statistical pooling for Analysis 1.6 and Analysis 1.8 were inappropriate in this instance because of heterogeneity.
Analysis 1.5.
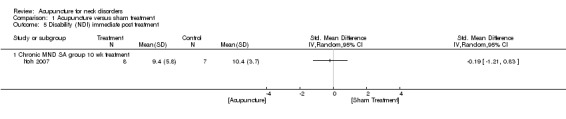
Comparison 1 Acupuncture versus sham treatment, Outcome 5 Disability (NDI) immediate post treatment.
Analysis 1.6.
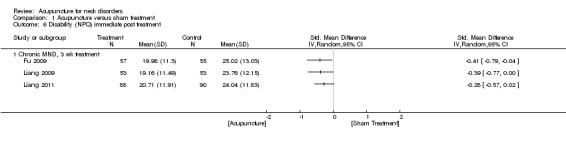
Comparison 1 Acupuncture versus sham treatment, Outcome 6 Disability (NPQ) immediate post treatment.
Analysis 1.7.
Comparison 1 Acupuncture versus sham treatment, Outcome 7 Disability (NPQ) short term.
Analysis 1.8.
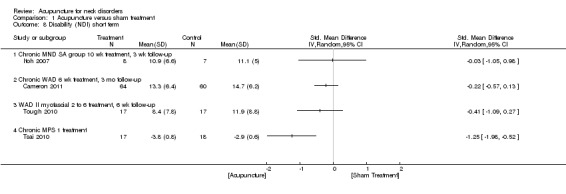
Comparison 1 Acupuncture versus sham treatment, Outcome 8 Disability (NDI) short term.
Analysis 1.9.
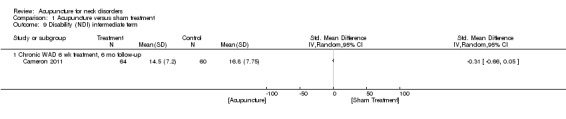
Comparison 1 Acupuncture versus sham treatment, Outcome 9 Disability (NDI) intermediate term.
Analysis 1.10.
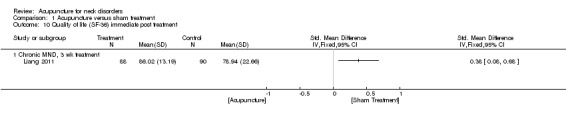
Comparison 1 Acupuncture versus sham treatment, Outcome 10 Quality of life (SF‐36) immediate post treatment.
Analysis 1.11.
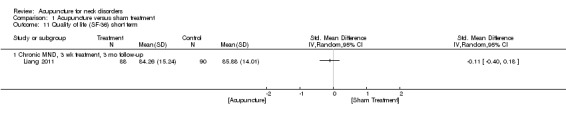
Comparison 1 Acupuncture versus sham treatment, Outcome 11 Quality of life (SF‐36) short term.
Some evidence suggests that acupuncture may be more beneficial than sham acupuncture for disability (Northwick Park Pain Questionnaire (NPQ)). Two studies (n = 290) involved participants with mechanical neck disorders, one with low risk of bias (Liang 2011) and the other with high risk of bias (Fu 2009). Meta‐analysis favoured acupuncture (P value = 0.001). (Please see Analysis 1.7.) Statistical pooling was appropriate in this instance because of statistical homogeneity (P value = 0.88; I2 = 0%). On the basis of the GRADE scale, we downgraded the quality level of evidence to moderate because only one of the two studies (50%) presented low risk.
Acupuncture versus inactive treatment
Pain intensity (VAS) immediate post treatment
We assigned five studies (n = 245) to this category (Ilbuldu 2004; Irnich 2002; Petrie 1986; Seidel 2002; Thomas 1991). We considered two of these studies (Irnich 2002; Seidel 2002) to have low risk of bias and three to have high risk of bias (Ilbuldu 2004; Petrie 1986; Thomas 1991). Statistical pooling was inappropriate in this instance because of statistical heterogeneity (P value = 0.20; I2 = 33%). Most of these studies ‐ four of the five ‐ did not favour acupuncture (Ilbuldu 2004; Petrie 1986; Seidel 2002; Thomas 1991). (Please see Analysis 2.1.)
Analysis 2.1.
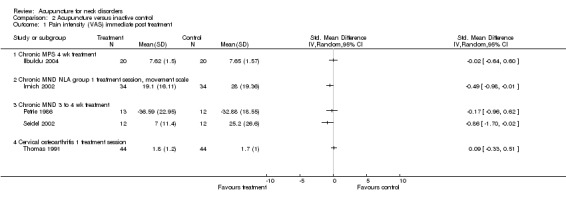
Comparison 2 Acupuncture versus inactive control, Outcome 1 Pain intensity (VAS) immediate post treatment.
Pain intensity (VAS) short term
Five studies (n = 404) (Irnich 2001; Petrie 1986; Seidel 2002; Vas 2006; White 2004) assessed participants with mechanical neck disorders. Petrie 1986 found no differences between groups (Petrie 1986). Another study compared acupuncture versus sham laser and reported no differences (Irnich 2001). However, Vickers 2004 used regression analysis and adjusted for baseline pain in re‐analysing this study (Vickers 2004) and showed that acupuncture resulted in a 9.4‐point greater reduction in pain over sham laser (0.9 to 18.0 points; P value = 0.031). Another study compared acupuncture versus sham laser (Seidel 2002) and showed statistically significant results favouring acupuncture at four‐week follow‐up. One study compared acupuncture versus sham electroacupuncture stimulator and yielded positive results at one‐week follow‐up, but these results were not sustained at eight‐week follow‐up (White 2004). Vas and colleagues also favoured acupuncture over inactive treatment (Vas 2006).
Statistical pooling was inappropriate in this instance because of statistical heterogeneity (P value = 0.0001; I2 = 83%). We considered four of these studies (Irnich 2001; Seidel 2002; Vas 2006; White 2004) to have low risk of bias and one study (Petrie 1986) (n = 26) to have high risk of bias.
On the basis of the GRADE scale, we determined that evidence should be rated as high quality because criteria such as design, limitations, inconsistency of results, indirectness, imprecision and other factors were met. However, because of the small sample size of these studies, it is highly possible that future research may change the estimate or our confidence in the results. Therefore, we downgraded the quality level of evidence to moderate. Moderate‐quality evidence suggests that acupuncture is beneficial for individuals with chronic mechanical neck pain for pain intensity at short‐term follow‐up. (Please see Analysis 2.2.)
Analysis 2.2.
Comparison 2 Acupuncture versus inactive control, Outcome 2 Pain intensity (VAS) short term.
Pain intensity (VAS) intermediate term
Three studies (n = 318) assessed participants with mechanical neck disorders (Vas 2006; White 2004) or myofascial pain syndrome (Ilbuldu 2004). One of these studies favoured acupuncture over inactive treatment (Vas 2006). We considered two of these studies (Vas 2006; White 2004) to have low risk of bias. Statistical pooling was inappropriate in this instance because of statistical heterogeneity (P value = 0.21; I2 = 36%).
Low‐quality evidence suggests that acupuncture is beneficial for individuals with chronic mechanical neck pain for pain intensity at intermediate‐term follow‐up. We downgraded the quality of evidence because of risk of bias (< 75% of the studies presented low risk) and inconsistency of results. (Please see Analysis 2.3.)
Analysis 2.3.
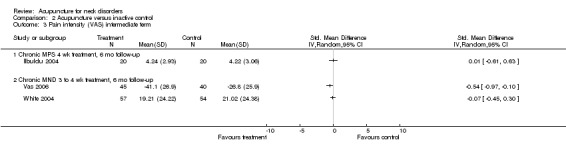
Comparison 2 Acupuncture versus inactive control, Outcome 3 Pain intensity (VAS) intermediate term.
Pain intensity (VAS) long term
We considered White 2004 (n = 124) to have low risk of bias; this study did not favour acupuncture treatment. No evidence suggests that acupuncture is effective for long‐term pain relief. (Please see Analysis 2.4.)
Analysis 2.4.
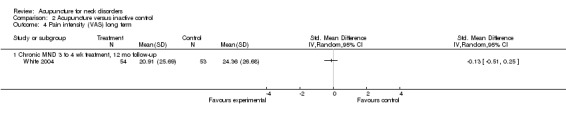
Comparison 2 Acupuncture versus inactive control, Outcome 4 Pain intensity (VAS) long term.
Disability and quality of life
No convincing evidence favoured acupuncture in all other measures such as disability (NDI) and quality of life over the short term, the intermediate term or the long term. (Please see Analysis 2.5, Analysis 2.6, Analysis 2.7, Analysis 2.8, Analysis 2.9, Analysis 2.10, Analysis 2.11, Analysis 2.12, Analysis 2.13 and Analysis 2.14.) Statistical pooling for Analysis 2.5, Analysis 2.6 and Analysis 2.14 were inappropriate in this instance because of heterogeneity.
Analysis 2.5.
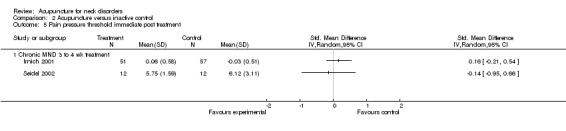
Comparison 2 Acupuncture versus inactive control, Outcome 5 Pain pressure threshold immediate post treatment.
Analysis 2.6.
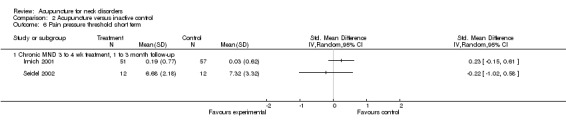
Comparison 2 Acupuncture versus inactive control, Outcome 6 Pain pressure threshold short term.
Analysis 2.7.
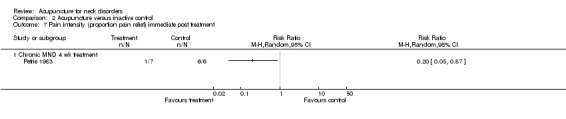
Comparison 2 Acupuncture versus inactive control, Outcome 7 Pain intensity (proportion pain relief) immediate post treatment.
Analysis 2.8.
Comparison 2 Acupuncture versus inactive control, Outcome 8 Disability (NDI) short term.
Analysis 2.9.
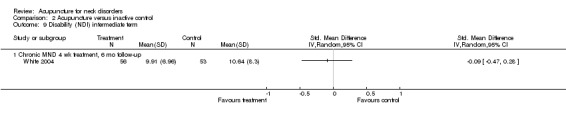
Comparison 2 Acupuncture versus inactive control, Outcome 9 Disability (NDI) intermediate term.
Analysis 2.10.
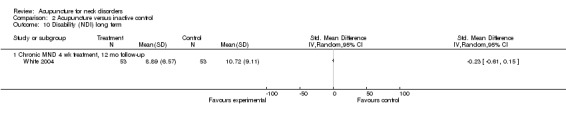
Comparison 2 Acupuncture versus inactive control, Outcome 10 Disability (NDI) long term.
Analysis 2.11.
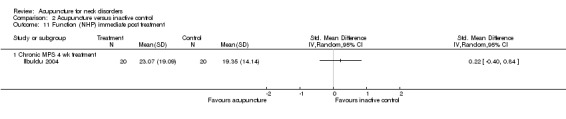
Comparison 2 Acupuncture versus inactive control, Outcome 11 Function (NHP) immediate post treatment.
Analysis 2.12.
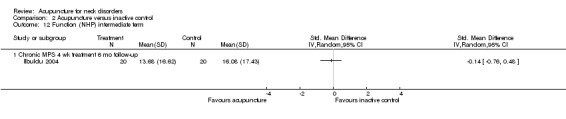
Comparison 2 Acupuncture versus inactive control, Outcome 12 Function (NHP) intermediate term.
Analysis 2.13.
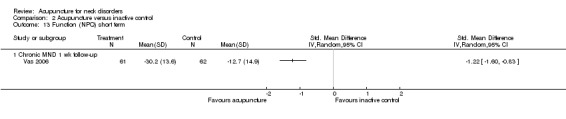
Comparison 2 Acupuncture versus inactive control, Outcome 13 Function (NPQ) short term.
Analysis 2.14.
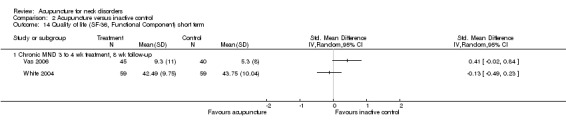
Comparison 2 Acupuncture versus inactive control, Outcome 14 Quality of life (SF‐36, Functional Component) short term.
Acupuncture versus wait‐list control
Pain intensity (VAS) at short‐term follow‐up
One study (n = 30) involving participants with mechanical neck disorders with radicular symptoms (Coan 1982) favoured acupuncture for short‐term pain relief. This study had low risk of bias. However, no evidence suggests that this improvement was sustained to intermediate follow‐up. (Please see Analysis 3.1.)
Analysis 3.1.
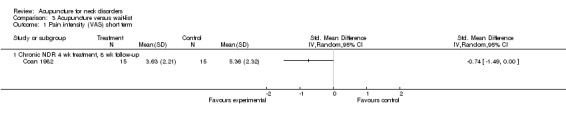
Comparison 3 Acupuncture versus wait‐list, Outcome 1 Pain intensity (VAS) short term.
Disability and quality of life
One study (n = 3766) involving participants with mechanical neck disorders (Witt 2006) favoured acupuncture for short‐term NDI improvement. This study had low risk of bias, but no evidence suggests that this improvement was sustained to intermediate follow‐up. (Please see Analysis 3.2.)
Analysis 3.2.
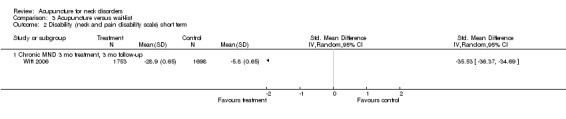
Comparison 3 Acupuncture versus wait‐list, Outcome 2 Disability (neck and pain disability scale) short term.
No convincing evidence favoured acupuncture in all other measures such as quality of life over the short term or the intermediate term regarding physical or mental scores (SF‐36). In fact, some evidence suggests that results favoured control on the basis of a single study in each category. (Please see Analysis 3.3, Analysis 3.4, Analysis 3.5 and Analysis 3.6.)
Analysis 3.3.
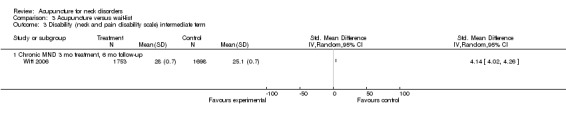
Comparison 3 Acupuncture versus wait‐list, Outcome 3 Disability (neck and pain disability scale) intermediate term.
Analysis 3.4.
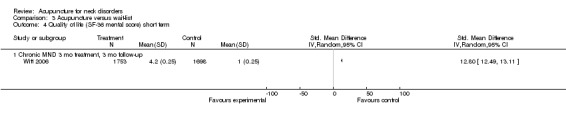
Comparison 3 Acupuncture versus wait‐list, Outcome 4 Quality of life (SF‐36 mental score) short term.
Analysis 3.5.
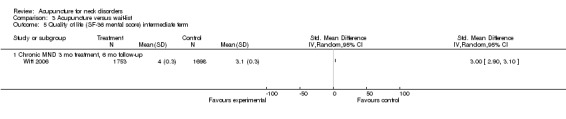
Comparison 3 Acupuncture versus wait‐list, Outcome 5 Quality of life (SF‐36 mental score) intermediate term.
Analysis 3.6.
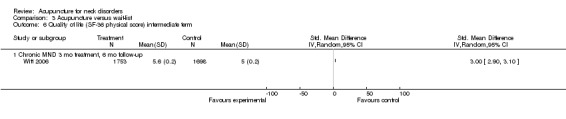
Comparison 3 Acupuncture versus wait‐list, Outcome 6 Quality of life (SF‐36 physical score) intermediate term.
Fourteen studies reported adverse effects (Cameron 2011; Fu 2009; Irnich 2001; Irnich 2002; Itoh 2007; Kwak 2012; Liang 2011; Nabeta 2002; Seidel 2002; Sun 2010; Tough 2010; Vas 2006; White 2004; Witt 2006), which included increased pain, bruising, fainting, worsening of symptoms, local swelling and dizziness. (See Characteristics of included studies table for full details.) These studies noted no life‐threatening adverse effects.
One large multi‐centre trial reported costs of care (Witt 2006) and indicated that acupuncture is cost‐effective.
For a summary of results, please see Table 1, Table 2 and Table 3.
Discussion
Summary of main results
For mechanical neck pain, we found that acupuncture is more beneficial at immediate‐term follow‐up compared with sham treatments for pain intensity; at short‐term follow‐up compared with sham treatments and inactive treatments for pain intensity; at short term follow‐up compared with sham treatments for disability (Northwick Park Pain Questionnaire (NPQ)) and at short‐term follow‐up compared with wait‐list control for pain intensity and Neck Disability Index (NDI) improvement. Effects do not seem sustainable over the long term. Our primary studies did not examine whether subsequent repeated sessions will be successful.
Overall completeness and applicability of evidence
In this review, we limited our trials to include acupuncture interventions in the experimental arm and no acupuncture interventions in the control arm. Control arms could be given sham acupuncture, an inactive treatment or no treatment. In this way, we could better study the effects of acupuncture. Our challenge remains determining what constitutes acupuncture treatments. In other Cochrane reviews such as acupuncture for back pain, acupuncture is defined as treatment that uses some type of standardised acupuncture points, whereas dry needling is treatment that uses acupuncture needles over trigger points. We found insufficient studies on dry needling alone to justify separating this needling treatment method for examination in a separate review.
We found that the number of acupuncture treatment sessions was associated with outcomes (Ezzo 2000). Ideally, treatment should consist of six or more acupuncture sessions. One study (Irnich 2002) intentionally studied the effects of a single treatment. Five studies provided underdosing with fewer than six treatment sessions (Chou 2009; Ilbuldu 2004; Nabeta 2002; Tsai 2010; Vas 2006). All remaining studies were adequately dosed on the basis of this variable alone.
Quality of the evidence
The most difficult challenge faced in this review was clinical heterogeneity, which appeared at many levels, as in sample group included, acupuncture interventions provided and outcomes measured. Acupuncture interventions and sham therapies were quite varied. Among sham therapies, treatment varied from a non‐insertion type of inactivated transcutaneous electrical nerve stimulation (TENS) or laser to insertion of needles at different locations or at different depths. The qualitative method of synthesising evidence has its limitations. We determined consistency of evidence by group consensus, but this method is sensitive to how studies are categorised because meeting the criteria for a certain level of evidence depends on the number of studies included within a category.
Fortunately, the quality of acupuncture studies for neck pain seems to have improved over time. We classified many studies identified in the latest update of our search as having low risk of bias.
Potential biases in the review process
Weaknesses of this review rest with limitations in the primary studies. Furthermore, many studies did not report details of drop‐outs. We avoided language bias by including all languages during study selection; however, we did not search non‐English language databases, and we did not search Chinese databases beyond 2005.
Our approach to summarising the literature has several strengths. We used a comprehensive, librarian‐assisted search of multiple databases. We relied on teams of healthcare professionals to decide on article relevance and to assess study quality. At least two review authors extracted data, and the principal investigator verified data entry. We used a group consensus approach, coupled with the Cochrane Back Review Group risk of bias assessment tool. We avoided professional bias inherent in having members of a single profession evaluate the literature for that profession.
Agreements and disagreements with other studies or reviews
Our findings are similar to those of our past review in 2006 (Trinh 2006) and to those of Fu et al in 2009 (Fu 2009). This is consistent with other reviews on acupuncture for migraine headache prophylaxis (Linde 2009), elbow pain (Trinh 2004), tension headache (Linde 2009a) and back pain (Furlan 2005). The result is not surprising. The findings of our review of other therapies for neck disorders were disappointing. It appears that the effect size of treatments for neck disorders is small even for therapies (such as injections) believed to have a large clinical effect. It is likely that in a clinical setting, both specific and non‐specific effects of treatments are evident, whereas in a randomised controlled trial (RCT), investigators observe non‐specific effects of treatments in both experimental and control groups. Therefore, the difference is seen in the specific effects of treatment, and these effects may be smaller than those observed clinically.
Authors' conclusions
For mechanical neck pain, we found that acupuncture is beneficial immediately following treatment and at short‐term follow‐up compared with sham treatments for pain intensity; at short‐term follow‐up compared with sham treatments for disability (NPQ); at short‐term follow‐up compared with inactive treatments for pain intensity; and at short‐term follow‐up compared with wait‐list control for pain intensity and neck disability improvement. Effects do not seem sustainable over the long term. Acupuncture treatments appear to be relatively safe.
Acupuncture trials with adequate sample size are needed to examine the long‐term efficacy or effectiveness of acupuncture compared with sham acupuncture.
Acknowledgements
Thank you to the primary authors who responded to requests for information. We also thank our volunteers, our translators and the Cochrane Back Review Group editors.
Appendices
Appendix 1. Computerised search strategy
CENTRAL‐OVID
August 25, 2015
1. Neck Pain/
2. exp Brachial Plexus Neuropathies/
3. exp neck injuries/ or exp whiplash injuries/
4. cervical pain.mp.
5. neckache.mp.
6. whiplash.mp.
7. cervicodynia.mp.
8. cervicalgia.mp.
9. brachialgia.mp.
10. brachial neuritis.mp.
11. brachial neuralgia.mp.
12. neck pain.mp.
13. neck injur*.mp.
14. brachial plexus neuropath*.mp.
15. brachial plexus neuritis.mp.
16. thoracic outlet syndrome/ or cervical rib syndrome/
17. Torticollis/
18. exp brachial plexus neuropathies/ or exp brachial plexus neuritis/
19. cervico brachial neuralgia.ti,ab.
20. cervicobrachial neuralgia.ti,ab.
21. (monoradicul* or monoradicl*).tw.
22. or/1‐21
23. exp headache/ and cervic*.tw.
24. exp genital diseases, female/
25. genital disease*.mp.
26. or/24‐25
27. 23 not 26
28. 22 or 27
29. neck/
30. neck muscles/
31. exp cervical plexus/
32. exp cervical vertebrae/
33. atlanto‐axial joint/
34. atlanto‐occipital joint/
35. Cervical Atlas/
36. spinal nerve roots/
37. exp brachial plexus/
38. (odontoid* or cervical or occip* or atlant*).tw.
39. axis/ or odontoid process/
40. Thoracic Vertebrae/
41. cervical vertebrae.mp.
42. cervical plexus.mp.
43. cervical spine.mp.
44. (neck adj3 muscles).mp.
45. (brachial adj3 plexus).mp.
46. (thoracic adj3 vertebrae).mp.
47. neck.mp.
48. (thoracic adj3 spine).mp.
49. (thoracic adj3 outlet).mp.
50. trapezius.mp.
51. cervical.mp.
52. cervico*.mp.
53. 51 or 52
54. exp genital diseases, female/
55. genital disease*.mp.
56. exp *Uterus/
57. 54 or 55 or 56
58. 53 not 57
59. 29 or 30 or 31 or 32 or 33 or 34 or 35 or 36 or 37 or 38 or 39 or 40 or 41 or 42 or 43 or 44 or 45 or 46 or 47 or 48 or 49 or 50 or 58
60. exp pain/
61. exp injuries/
62. pain.mp.
63. ache.mp.
64. sore.mp.
65. stiff.mp.
66. discomfort.mp.
67. injur*.mp.
68. neuropath*.mp.
69. or/60‐68
70. 59 and 69
71. Radiculopathy/
72. exp temporomandibular joint disorders/ or exp temporomandibular joint dysfunction syndrome/
73. myofascial pain syndromes/
74. exp "Sprains and Strains"/
75. exp Spinal Osteophytosis/
76. exp Neuritis/
77. Polyradiculopathy/
78. exp Arthritis/
79. Fibromyalgia/
80. spondylitis/ or discitis/
81. spondylosis/ or spondylolysis/ or spondylolisthesis/
82. radiculopathy.mp.
83. radiculitis.mp.
84. temporomandibular.mp.
85. myofascial pain syndrome*.mp.
86. thoracic outlet syndrome*.mp.
87. spinal osteophytosis.mp.
88. neuritis.mp.
89. spondylosis.mp.
90. spondylitis.mp.
91. spondylolisthesis.mp.
92. or/71‐91
93. 59 and 92
94. exp neck/
95. exp cervical vertebrae/
96. Thoracic Vertebrae/
97. neck.mp.
98. (thoracic adj3 vertebrae).mp.
99. cervical.mp.
100. cervico*.mp.
101. 99 or 100
102. exp genital diseases, female/
103. genital disease*.mp.
104. exp *Uterus/
105. or/102‐104
106. 101 not 105
107. (thoracic adj3 spine).mp.
108. cervical spine.mp.
109. 94 or 95 or 96 or 97 or 98 or 106 or 107 or 108
110. Intervertebral Disk/
111. (disc or discs).mp.
112. (disk or disks).mp.
113. 110 or 111 or 112
114. 109 and 113
115. herniat*.mp.
116. slipped.mp.
117. prolapse*.mp.
118. displace*.mp.
119. degenerat*.mp.
120. (bulge or bulged or bulging).mp.
121. 115 or 116 or 117 or 118 or 119 or 120
122. 114 and 121
123. intervertebral disk degeneration/ or intervertebral disk displacement/
124. intervertebral disk displacement.mp.
125. intervertebral disc displacement.mp.
126. intervertebral disk degeneration.mp.
127. intervertebral disc degeneration.mp.
128. 123 or 124 or 125 or 126 or 127
129. 109 and 128
130. 28 or 70 or 93 or 122 or 129
131. animals/ not (animals/ and humans/)
132. 130 not 131
133. exp *neoplasms/
134. exp *wounds, penetrating/
135. 133 or 134
136. 132 not 135
137. Neck Pain/rh, th [Rehabilitation, Therapy]
138. exp Brachial Plexus Neuropathies/rh, th
139. exp neck injuries/rh, th or exp whiplash injuries/rh, th
140. thoracic outlet syndrome/rh, th or cervical rib syndrome/rh, th
141. Torticollis/rh, th
142. exp brachial plexus neuropathies/rh, th or exp brachial plexus neuritis/rh, th
143. or/137‐142
144. Radiculopathy/rh, th
145. exp temporomandibular joint disorders/rh, th or exp temporomandibular joint dysfunction syndrome/rh, th
146. myofascial pain syndromes/rh, th
147. exp "Sprains and Strains"/rh, th
148. exp Spinal Osteophytosis/rh, th
149. exp Neuritis/rh, th
150. Polyradiculopathy/rh, th
151. exp Arthritis/rh, th
152. Fibromyalgia/rh, th
153. spondylitis/rh, th or discitis/rh, th
154. spondylosis/rh, th or spondylolysis/rh, th or spondylolisthesis/rh, th
155. or/144‐154
156. 59 and 155
157. acupuncture/ or chiropractic/
158. exp Musculoskeletal Manipulations/
159. massage.tw.
160. mobili?ation.tw.
161. Acupuncture Therapy/
162. (acupuncture or acu‐puncture or needling or acupressure or mox?bustion).tw.
163. ((neck or spine or spinal or cervical or chiropractic* or musculoskeletal* or musculo‐skeletal*) adj3 (adjust* or manipulat* or mobiliz* or mobilis*)).tw.
164. (manual adj therap*).tw.
165. (manipulati* adj (therap* or medicine)).tw.
166. (massag* or reflexolog* or rolfing or zone therap*).tw.
167. Nimmo.mp.
168. exp Vibration/tu [Therapeutic Use]
169. (vibration adj5 (therap* or treatment*)).tw.
170. (Chih Ya or Shiatsu or Shiatzu or Zhi Ya).tw.
171. (flexion adj2 distraction*).tw.
172. (myofascial adj3 (release or therap*)).tw.
173. muscle energy technique*.tw.
174. trigger point.tw.
175. proprioceptive Neuromuscular Facilitation*.tw.
176. cyriax friction.tw.
177. (lomilomi or lomi‐lomi or trager).tw.
178. aston patterning.tw.
179. (strain adj counterstrain).tw.
180. (craniosacral therap* or cranio‐sacral therap*).tw.
181. (amma or ammo or effleuurage or petrissage or hacking or tapotment).tw.
182. Complementary Therapies/
183. ((complement* or alternat* or osteopthic*) adj (therap* or medicine)).tw.
184. (Tui Na or Tuina).tw.
185. or/157‐184
186. 136 and 185
187. 143 or 156 or 186
188. animals/ not (animals/ and humans/)
189. 187 not 188
MEDLINE‐OVID
August 25, 2015
1. Neck Pain/
2. exp Brachial Plexus Neuropathies/
3. exp neck injuries/ or exp whiplash injuries/
4. cervical pain.mp.
5. neckache.mp.
6. whiplash.mp.
7. cervicodynia.mp.
8. cervicalgia.mp.
9. brachialgia.mp.
10. brachial neuritis.mp.
11. brachial neuralgia.mp.
12. neck pain.mp.
13. neck injur*.mp.
14. brachial plexus neuropath*.mp.
15. brachial plexus neuritis.mp.
16. thoracic outlet syndrome/ or cervical rib syndrome/
17. Torticollis/
18. exp brachial plexus neuropathies/ or exp brachial plexus neuritis/
19. cervico brachial neuralgia.ti,ab.
20. cervicobrachial neuralgia.ti,ab.
21. (monoradicul* or monoradicl*).tw.
22. or/1‐21
23. exp headache/ and cervic*.tw.
24. exp genital diseases, female/
25. genital disease*.mp.
26. or/24‐25
27. 23 not 26
28. 22 or 27
29. neck/
30. neck muscles/
31. exp cervical plexus/
32. exp cervical vertebrae/
33. atlanto‐axial joint/
34. atlanto‐occipital joint/
35. Cervical Atlas/
36. spinal nerve roots/
37. exp brachial plexus/
38. (odontoid* or cervical or occip* or atlant*).tw.
39. axis/ or odontoid process/
40. Thoracic Vertebrae/
41. cervical vertebrae.mp.
42. cervical plexus.mp.
43. cervical spine.mp.
44. (neck adj3 muscles).mp.
45. (brachial adj3 plexus).mp.
46. (thoracic adj3 vertebrae).mp.
47. neck.mp.
48. (thoracic adj3 spine).mp.
49. (thoracic adj3 outlet).mp.
50. trapezius.mp.
51. cervical.mp.
52. cervico*.mp.
53. 51 or 52
54. exp genital diseases, female/
55. genital disease*.mp.
56. exp *Uterus/
57. 54 or 55 or 56
58. 53 not 57
59. 29 or 30 or 31 or 32 or 33 or 34 or 35 or 36 or 37 or 38 or 39 or 40 or 41 or 42 or 43 or 44 or 45 or 46 or 47 or 48 or 49 or 50 or 58
60. exp pain/
61. exp injuries/
62. pain.mp.
63. ache.mp.
64. sore.mp.
65. stiff.mp.
66. discomfort.mp.
67. injur*.mp.
68. neuropath*.mp.
69. or/60‐68
70. 59 and 69
71. Radiculopathy/
72. exp temporomandibular joint disorders/ or exp temporomandibular joint dysfunction syndrome/
73. myofascial pain syndromes/
74. exp "Sprains and Strains"/
75. exp Spinal Osteophytosis/
76. exp Neuritis/
77. Polyradiculopathy/
78. exp Arthritis/
79. Fibromyalgia/
80. spondylitis/ or discitis/
81. spondylosis/ or spondylolysis/ or spondylolisthesis/
82. radiculopathy.mp.
83. radiculitis.mp.
84. temporomandibular.mp.
85. myofascial pain syndrome*.mp.
86. thoracic outlet syndrome*.mp.
87. spinal osteophytosis.mp.
88. neuritis.mp.
89. spondylosis.mp.
90. spondylitis.mp.
91. spondylolisthesis.mp.
92. or/71‐91
93. 59 and 92
94. exp neck/
95. exp cervical vertebrae/
96. Thoracic Vertebrae/
97. neck.mp.
98. (thoracic adj3 vertebrae).mp.
99. cervical.mp.
100. cervico*.mp.
101. 99 or 100
102. exp genital diseases, female/
103. genital disease*.mp.
104. exp *Uterus/
105. or/102‐104
106. 101 not 105
107. (thoracic adj3 spine).mp.
108. cervical spine.mp.
109. 94 or 95 or 96 or 97 or 98 or 106 or 107 or 108
110. Intervertebral Disk/
111. (disc or discs).mp.
112. (disk or disks).mp.
113. 110 or 111 or 112
114. 109 and 113
115. herniat*.mp.
116. slipped.mp.
117. prolapse*.mp.
118. displace*.mp.
119. degenerat*.mp.
120. (bulge or bulged or bulging).mp.
121. 115 or 116 or 117 or 118 or 119 or 120
122. 114 and 121
123. intervertebral disk degeneration/ or intervertebral disk displacement/
124. intervertebral disk displacement.mp.
125. intervertebral disc displacement.mp.
126. intervertebral disk degeneration.mp.
127. intervertebral disc degeneration.mp.
128. 123 or 124 or 125 or 126 or 127
129. 109 and 128
130. 28 or 70 or 93 or 122 or 129
131. animals/ not (animals/ and humans/)
132. 130 not 131
133. exp *neoplasms/
134. exp *wounds, penetrating/
135. 133 or 134
136. 132 not 135
137. Neck Pain/rh, th [Rehabilitation, Therapy]
138. exp Brachial Plexus Neuropathies/rh, th
139. exp neck injuries/rh, th or exp whiplash injuries/rh, th
140. thoracic outlet syndrome/rh, th or cervical rib syndrome/rh, th
141. Torticollis/rh, th
142. exp brachial plexus neuropathies/rh, th or exp brachial plexus neuritis/rh, th
143. or/137‐142
144. Radiculopathy/rh, th
145. exp temporomandibular joint disorders/rh, th or exp temporomandibular joint dysfunction syndrome/rh, th
146. myofascial pain syndromes/rh, th
147. exp "Sprains and Strains"/rh, th
148. exp Spinal Osteophytosis/rh, th
149. exp Neuritis/rh, th
150. Polyradiculopathy/rh, th
151. exp Arthritis/rh, th
152. Fibromyalgia/rh, th
153. spondylitis/rh, th or discitis/rh, th
154. spondylosis/rh, th or spondylolysis/rh, th or spondylolisthesis/rh, th
155. or/144‐154
156. 59 and 155
157. acupuncture/ or chiropractic/
158. exp Musculoskeletal Manipulations/
159. massage.tw.
160. mobili?ation.tw.
161. Acupuncture Therapy/
162. (acupuncture or acu‐puncture or needling or acupressure or mox?bustion).tw.
163. ((neck or spine or spinal or cervical or chiropractic* or musculoskeletal* or musculo‐skeletal*) adj3 (adjust* or manipulat* or mobiliz* or mobilis*)).tw.
164. (manual adj therap*).tw.
165. (manipulati* adj (therap* or medicine)).tw.
166. (massag* or reflexolog* or rolfing or zone therap*).tw.
167. Nimmo.mp.
168. exp Vibration/tu [Therapeutic Use]
169. (vibration adj5 (therap* or treatment*)).tw.
170. (Chih Ya or Shiatsu or Shiatzu or Zhi Ya).tw.
171. (flexion adj2 distraction*).tw.
172. (myofascial adj3 (release or therap*)).tw.
173. muscle energy technique*.tw.
174. trigger point.tw.
175. proprioceptive Neuromuscular Facilitation*.tw.
176. cyriax friction.tw.
177. (lomilomi or lomi‐lomi or trager).tw.
178. aston patterning.tw.
179. (strain adj counterstrain).tw.
180. (craniosacral therap* or cranio‐sacral therap*).tw.
181. (amma or ammo or effleuurage or petrissage or hacking or tapotment).tw.
182. Complementary Therapies/
183. ((complement* or alternat* or osteopthic*) adj (therap* or medicine)).tw.
184. (Tui Na or Tuina).tw.
185. or/157‐184
186. 136 and 185
187. 143 or 156 or 186
188. animals/ not (animals/ and humans/)
189. 187 not 188
190. exp randomized controlled trials as topic/
191. randomized controlled trial.pt.
192. controlled clinical trial.pt.
193. (random* or sham or placebo*).tw.
194. placebos/
195. random allocation/
196. single blind method/
197. double blind method/
198. ((singl* or doubl* or trebl* or tripl*) adj25 (blind* or dumm* or mask*)).ti,ab.
199. (rct or rcts).tw.
200. (control* adj2 (study or studies or trial*)).tw.
201. or/190‐200
202. 189 and 201
EMBASE‐OVID
August 25, 2015
1. neck pain/
2. brachial plexus neuropathy/
3. neck injury/ or whiplash injury/
4. cervical pain.mp.
5. neckache.mp.
6. whiplash.mp.
7. cervicodynia.mp.
8. cervicalgia.mp.
9. brachialgia/
10. brachialgia.mp.
11. brachial neuritis.mp.
12. brachial neuralgia.mp.
13. neck pain.mp.
14. neck injur*.mp.
15. brachial plexus neuropath*.mp.
16. brachial plexus neuritis.mp.
17. thorax outlet syndrome/
18. torticollis/
19. cervico brachial neuralgia.ti,ab.
20. cervicobrachial neuralgia.ti,ab.
21. (monoradicul* or monoradicl*).tw.
22. or/1‐21
23. exp headache/ and cervic*.tw.
24. exp gynecologic disease/
25. genital disease*.mp.
26. exp *uterine cervix/
27. or/24‐26
28. 23 not 27
29. 22 or 28
30. neck/ or neck muscle/
31. cervical plexus/
32. cervical spine/
33. atlantoaxial joint/
34. atlantooccipital joint/
35. atlas/
36. "spinal root"/
37. brachial plexus/
38. (odontoid* or cervical or occip* or atlant*).tw.
39. odontoid process/
40. cervical vertebra.mp.
41. cervical vertebrae.mp.
42. cervical plexus.mp.
43. cervical spine.mp.
44. (neck adj3 muscles).mp.
45. (brachial adj3 plexus).mp.
46. (thoracic adj3 vertebra?).mp.
47. neck.mp.
48. (thoracic adj3 spine).mp.
49. (thoracic adj3 outlet).mp.
50. trapezius.mp.
51. cervical.mp.
52. cervico*.mp.
53. 51 or 52
54. exp gynecologic disease/
55. genital disease*.mp.
56. exp *uterine cervix/
57. 54 or 55 or 56
58. 53 not 57
59. 30 or 31 or 32 or 33 or 34 or 35 or 36 or 37 or 38 or 39 or 40 or 41 or 42 or 43 or 44 or 45 or 46 or 47 or 48 or 49 or 50 or 58
60. exp pain/
61. exp injury/
62. pain.mp.
63. ache.mp.
64. sore.mp.
65. stiff.mp.
66. discomfort.mp.
67. injur*.mp.
68. neuropath*.mp.
69. or/60‐68
70. radiculopathy/
71. temporomandibular joint disorder/
72. myofascial pain/
73. spondylosis/ or cervical spondylosis/
74. neuritis/
75. exp arthritis/
76. fibromyalgia/
77. exp spondylitis/
78. diskitis/
79. spondylolisthesis/
80. radiculopathy.mp.
81. radiculitis.mp.
82. temporomandibular.mp.
83. myofascial pain syndrome*.mp.
84. spinal osteophytosis.mp.
85. neuritis.mp.
86. spondylosis.mp.
87. spondylitis.mp.
88. spondylolisthesis.mp.
89. or/70‐88
90. 59 and 89
91. neck/
92. cervical spine/
93. neck.mp.
94. (thoracic adj3 vertebra?).mp.
95. cervical.mp.
96. cervico*.mp.
97. exp gynecologic disease/
98. genital disease*.mp.
99. exp *uterine cervix/
100. or/97‐99
101. 95 or 96
102. 101 not 100
103. (thoracic adj3 spine).mp.
104. cervical spine.mp.
105. 91 or 92 or 93 or 94 or 102 or 103 or 104
106. intervertebral disk/
107. (disc or discs).mp.
108. (disk or disks).mp.
109. 106 or 107 or 108
110. 105 and 109
111. herniat*.mp.
112. slipped.mp.
113. prolapse*.mp.
114. displace*.mp.
115. degenerat*.mp.
116. (bulge or bulged or bulging).mp.
117. 110 or 111 or 112 or 113 or 114 or 115 or 116
118. 110 and 117
119. intervertebral disk hernia/
120. intervertebral disk degeneration/
121. intervertebral disc degeneration.mp.
122. intervertebral disk degeneration.mp.
123. intervertebral disc displacement.mp.
124. intervertebral disk displacement.mp.
125. 119 or 120 or 121 or 122 or 123 or 124
126. 105 and 125
127. 59 and 69
128. 29 or 90 or 118 or 126 or 127
129. exp *neoplasm/
130. exp *penetrating trauma/
131. 129 or 130
132. 128 not 131
133. neck pain/rh, th
134. brachial plexus neuropathy/rh, th
135. neck injury/ or whiplash injury/rh, th
136. brachialgia/rh, th
137. thorax outlet syndrome/rh, th
138. Torticollis/rh, th
139. Radiculopathy/rh, th
140. temporomandibular joint disorder/rh, th
141. myofascial pain/rh, th
142. spondylosis/rh, th or cervical spondylosis/rh, th
143. neuritis/rh, th
144. exp arthritis/rh, th
145. Fibromyalgia/rh, th
146. exp spondylitis/rh, th
147. diskitis/rh, th
148. spondylolisthesis/rh, th
149. acupuncture/ or acupressure/ or acupuncture analgesia/
150. exp manipulative medicine/
151. massage.tw.
152. mobili?ation.tw.
153. (acupuncture or acu‐puncture or needling or acupressure or mox?bustion).tw.
154. ((neck or spine or spinal or cervical or chiropractic* or musculoskeletal* or musculo‐skeletal*) adj3 (adjust* or manipulat* or mobiliz* or mobilis*)).tw.
155. (manual adj therap*).tw.
156. (manipulati* adj (therap* or medicine)).tw.
157. (massag* or reflexolog* or rolfing or zone therap*).tw.
158. Nimmo.tw.
159. (vibration adj5 (therap* or treatment*)).tw.
160. (Chih Ya or Shiatsu or Shiatzu or Zhi Ya).tw.
161. (flexion adj2 distraction*).tw.
162. (myofascial adj3 (release or therap*)).tw.
163. muscle energy technique*.tw.
164. trigger point.tw.
165. proprioceptive Neuromuscular Facilitation*.tw.
166. cyriax friction.tw.
167. (lomilomi or lomi‐lomi or trager).tw.
168. aston patterning.tw.
169. (strain adj counterstrain).tw.
170. (craniosacral therap* or cranio‐sacral therap*).tw.
171. (amma or ammo or effleuurage or petrissage or hacking or tapotment).tw.
172. alternative medicine/
173. ((complement* or alternat* or osteopthic*) adj (therap* or medicine)).tw.
174. (Tui Na or Tuina).tw.
175. (swedish massage or rolfing).tw.
176. therapeutic touch.mp.
177. massotherapy.tw.
178. effleurage.mp.
179. or/149‐178
180. 132 and 179
181. 133 or 134 or 135 or 136 or 137 or 138
182. or/139‐148
183. 59 and 182
184. 180 or 181 or 183
185. randomized controlled trial/
186. controlled clinical trial/
187. (random* or sham or placebo*).tw.
188. placebo/
189. randomization/
190. single blind procedure/
191. double blind procedure/
192. ((singl* or doubl* or trebl* or tripl*) adj5 (blind* or dumm*or mask*)).ti,ab.
193. (rct or rcts).tw.
194. (control* adj2 (study or studies or tiral*)).tw.
195. or/185‐194
196. human/
197. nonhuman/
198. animal/
199. animal experiment/
200. or/197‐199
201. 200 not (200 and 196)
202. 195 not 201
203. 184 and 202
MANTIS‐OVID
November 2013 (last available access)
1 neck pain.mp. [mp=title, abstract, descriptors]
2 brachial plexus neuropathies.mp. [mp=title, abstract, descriptors]
3 neck injuries.mp. [mp=title, abstract, descriptors]
4 cervical pain.mp. [mp=title, abstract, descriptors]
5 neckache.mp. [mp=title, abstract, descriptors]
6 whiplash.mp. [mp=title, abstract, descriptors]
7 cervicodynia.mp. [mp=title, abstract, descriptors]
8 cervicalgia.mp. [mp=title, abstract, descriptors]
9 brachialgia.mp. [mp=title, abstract, descriptors]
10 brachial neuritis.mp. [mp=title, abstract, descriptors]
11 brachial neuralgia.mp. [mp=title, abstract, descriptors]
12 brachial plexus neuropath*.mp. [mp=title, abstract, descriptors]
13 brachial plexus neuritis.mp. [mp=title, abstract, descriptors]
14 (thoracic outlet syndrome or cervical rib syndrome).mp. [mp=title, abstract, descriptors]
15 torticollis.mp. [mp=title, abstract, descriptors]
16 cervico brachial neuralgia.mp. [mp=title, abstract, descriptors]
17 (monoradicul* or monoradicl*).tw.
18 or/1‐17
19 headache.mp. and cervic*.tw. [mp=title, abstract, descriptors]
20 genital diseases, female.mp. [mp=title, abstract, descriptors]
21 genital disease*.mp. [mp=title, abstract, descriptors]
22 or/20‐21
23 19 not 22
24 18 or 23
25 neck.mp. [mp=title, abstract, descriptors]
26 neck muscles.mp. [mp=title, abstract, descriptors]
27 cervical plexus.mp. [mp=title, abstract, descriptors]
28 cervical vertebrae.mp. [mp=title, abstract, descriptors]
29 atlanto‐axial joint.mp. [mp=title, abstract, descriptors]
30 atlanto‐occipital joint.mp. [mp=title, abstract, descriptors]
31 cervical atlas.mp. [mp=title, abstract, descriptors]
32 spinal nerve roots.mp. [mp=title, abstract, descriptors]
33 brachial plexus.mp. [mp=title, abstract, descriptors]
34 (odontoid* or cervical or occip* or atlant*).tw.
35 (axis or odontoid process).mp. [mp=title, abstract, descriptors]
36 thoracic vertebrae.mp. [mp=title, abstract, descriptors]
37 cervical vertebrae.mp. [mp=title, abstract, descriptors]
38 cervical plexus.mp. [mp=title, abstract, descriptors]
39 cervical spine.mp. [mp=title, abstract, descriptors]
40 (neck adj3 muscles).mp. [mp=title, abstract, descriptors]
41 (brachial adj3 plexus).mp. [mp=title, abstract, descriptors]
42 (thoracic adj3 vertebrae).mp. [mp=title, abstract, descriptors]
43 (thoracic adj3 spine).mp. [mp=title, abstract, descriptors]
44 (thoracic adj3 outlet).mp. [mp=title, abstract, descriptors]
45 trapezius.mp. [mp=title, abstract, descriptors]
46 cervical.mp. [mp=title, abstract, descriptors]
47 cervico*.mp. [mp=title, abstract, descriptors]
48 46 or 47
49 genital diseases, female.mp. [mp=title, abstract, descriptors]
50 genital disease*.mp. [mp=title, abstract, descriptors]
51 uterus.mp. [mp=title, abstract, descriptors]
52 49 or 50 or 51
53 48 not 52
54 25 or 26 or 27 or 28 or 29 or 30 or 31 or 32 or 33 or 34 or 35 or 36
or 37 or 38 or 39 or 40 or 41 or 42 or 43 or 44 or 45 or 53
55 pain.mp. [mp=title, abstract, descriptors]
56 injuries.mp. [mp=title, abstract, descriptors]
57 ache.mp. [mp=title, abstract, descriptors]
58 sore.mp. [mp=title, abstract, descriptors]
59 stiff.mp. [mp=title, abstract, descriptors]
60 discomfort.mp. [mp=title, abstract, descriptors]
61 injur*.mp. [mp=title, abstract, descriptors]
62 neuropath*.mp. [mp=title, abstract, descriptors]
63 or/55‐62
64 54 and 63
65 radiculopathy.mp. [mp=title, abstract, descriptors]
66 (temporomandibular joint disorders or temporomandibular joint dysfunction syndrome).mp. [mp=title, abstract, descriptors]
67 myofascial pain syndromes.mp. [mp=title, abstract, descriptors]
68 "sprains and strains".mp. [mp=title, abstract, descriptors]
69 spinal osteophytosis.mp. [mp=title, abstract, descriptors]
70 neuritis.mp. [mp=title, abstract, descriptors]
71 polyradiculopathy.mp. [mp=title, abstract, descriptors]
72 arthritis.mp. [mp=title, abstract, descriptors]
73 fibromyalgia.mp. [mp=title, abstract, descriptors]
74 (spondylitis or discitis).mp. [mp=title, abstract, descriptors]
75 (spondylosis or spondylolysis or spondylolisthesis).mp. [mp=title, abstract, descriptors]
76 radiculitis.mp. [mp=title, abstract, descriptors]
77 tempomandibular.mp. [mp=title, abstract, descriptors]
78 myofascial pain syndrome*.mp. [mp=title, abstract, descriptors]
79 thoracic outlet syndrome*.mp. [mp=title, abstract, descriptors]
80 spinal osteophytosis.mp. [mp=title, abstract, descriptors]
81 neuritis.mp. [mp=title, abstract, descriptors]
82 spondylosis.mp. [mp=title, abstract, descriptors]
83 spondylitis.mp. [mp=title, abstract, descriptors]
84 spondylolisthesis.mp. [mp=title, abstract, descriptors]
85 or/65‐84
86 54 and 85
87 neck.mp. [mp=title, abstract, descriptors]
88 cervical vertebrae.mp. [mp=title, abstract, descriptors]
89 thoracic vertebrae.mp. [mp=title, abstract, descriptors]
90 (thoracic adj3 vertebrae).mp. [mp=title, abstract, descriptors]
91 cervical.mp. [mp=title, abstract, descriptors]
92 cervico*.mp. [mp=title, abstract, descriptors]
93 91 or 92
94 genital diseases, female.mp. [mp=title, abstract, descriptors]
95 genital disease*.mp. [mp=title, abstract, descriptors]
96 uterus.mp. [mp=title, abstract, descriptors]
97 or/94‐96
98 93 not 97
99 (thoracic adj3 spine).mp. [mp=title, abstract, descriptors]
100 cervical spine.mp. [mp=title, abstract, descriptors]
101 87 or 88 or 89 or 90 or 98 or 99 or 100
102 intervertebral disk.mp. [mp=title, abstract, descriptors]
103 (disc or discs).mp. [mp=title, abstract, descriptors]
104 (disk or disks).mp. [mp=title, abstract, descriptors]
105 102 or 103 or 104
106 101 and 105
107 herniat*.mp. [mp=title, abstract, descriptors]
108 slipped.mp. [mp=title, abstract, descriptors]
109 prolapse*.mp. [mp=title, abstract, descriptors]
110 displace*.mp. [mp=title, abstract, descriptors]
111 degenerat*.mp. [mp=title, abstract, descriptors]
112 (bulge or bulged or bulging).mp. [mp=title, abstract, descriptors]
113 107 or 108 or 109 or 110 or 111 or 112
114 106 and 113
115 intervertebral disk displacement.mp. [mp=title, abstract, descriptors]
116 intervertebral disc displacement.mp. [mp=title, abstract, descriptors]
117 intervertebral disk degeneration.mp. [mp=title, abstract, descriptors]
118 intervertebral disc degeneration.mp. [mp=title, abstract, descriptors]
119 115 or 116 or 117 or 118
120 101 and 119
121 24 or 64 or 86 or 106 or 114 or 120
122 (animals not (animals and humans)).mp. [mp=title, abstract, descriptors]
123 121 not 122
124 neoplasms.mp. [mp=title, abstract, descriptors]
125 wounds, penetrating.mp. [mp=title, abstract, descriptors]
126 124 or 125
127 123 not 126
128 rehabilitation.mp. [mp=title, abstract, descriptors]
129 therapy.mp. [mp=title, abstract, descriptors]
130 128 or 129
131 (neck pain or brachial plexus neuropathies or neck injuries or whiplash or thoracic outlet syndrome or cervical rib syndrome or torticollis or brachial plexus neuritis).mp. [mp=title, abstract, descriptors]
132 (temporomandibular joint disorder or temporomandibular joint dysfunction syndrome).mp. [mp=title, abstract, descriptors]
133 (myofascial pain syndromes or "sprains and strains").mp. [mp=title, abstract, descriptors]
134 (radiculopathy or osteophytosis or neuritis or polyradiculopathy or arthritis or fibromyalgia or spondylitis or spondylosis or spondylolysis or spondylolisthesis).mp. [mp=title, abstract, descriptors]
135 131 or 132 or 133 or 134
136 130 and 135
137 54 and 136
138 (acupuncture or chiropractic).mp. [mp=title, abstract, descriptors]
139 musculoskeletal manipulation*.mp. [mp=title, abstract, descriptors]
140 massage.mp. [mp=title, abstract, descriptors]
141 mobili?ation.mp. [mp=title, abstract, descriptors]
142 acupuncture therapy.mp. [mp=title, abstract, descriptors]
143 (acupuncture or acu‐puncture or needling or acupressure or mox?bustion).mp. [mp=title, abstract, descriptors]
144 ((neck or spine or spinal or cervical or chiropractic* or musculoskeletal*) adj3 (adjust* or manipulat* or mobiliz* or mobilis*)).mp. [mp=title, abstract, descriptors]
145 (manual adj therap*).mp. [mp=title, abstract, descriptors]
146 (manipulati* adj (therap* or medicine)).mp. [mp=title, abstract, descriptors]
147 (massag* or reflexolog* or rolfing or zone therap*).mp. [mp=title, abstract, descriptors]
148 Nimmo.mp. [mp=title, abstract, descriptors]
149 vibration therapy.mp. [mp=title, abstract, descriptors]
150 (vibration adj5 (therap* or treatment*)).mp. [mp=title, abstract, descriptors]
151 (ChihYa or Shiatsu or Shiatzu or ZhiYa).mp. [mp=title, abstract, descriptors]
152 (flexion adj2 distraction*).mp. [mp=title, abstract, descriptors]
153 (myofascial adj3 (release or therap*)).mp. [mp=title, abstract, descriptors]
154 muscle energy technique*.mp. [mp=title, abstract, descriptors]
155 trigger point.mp. [mp=title, abstract, descriptors]
156 proprioceptive neuromuscular facilitation*.mp. [mp=title, abstract, descriptors]
157 cyriax friction.mp. [mp=title, abstract, descriptors]
158 (lomilomi or lomi‐lomi or trager).mp. [mp=title, abstract, descriptors]
159 aston patterning.mp. [mp=title, abstract, descriptors]
160 (strain adj counterstrain).mp. [mp=title, abstract, descriptors]
161 (craniosacraltherap* or cranio‐sacral therap* or craniosacral therap*).mp. [mp=title, abstract, descriptors]
162 (amma or ammo or effleuurage or effleurage or petrissage or hacking or tapotment).mp. [mp=title, abstract, descriptors]
163 complementary therapies.mp. [mp=title, abstract, descriptors]
164 ((complement* or alternat* or osteopathic*) adj (therap* or medicine)).mp. [mp=title, abstract, descriptors]
165 (Tui Na or Tuina).mp. [mp=title, abstract, descriptors]
166 or/138‐165
167 127 and 166
168 136 or 137 or 167
169 (animals not (animals and humans)).mp. [mp=title, abstract, descriptors]
170 168 not 169
171 randomized controlled trial*.mp. [mp=title, abstract, descriptors]
172 controlled clinical trial*.mp. [mp=title, abstract, descriptors]
173 (random* or sham or placebo*).mp. [mp=title, abstract, descriptors]
174 placebos.mp. [mp=title, abstract, descriptors]
175 random allocation.mp. [mp=title, abstract, descriptors]
176 single blind method.mp. [mp=title, abstract, descriptors]
177 double blind method.mp. [mp=title, abstract, descriptors]
178 ((singl* or doubl* or trebl* or tripl*) adj25 (blind* or dumm*or mask*)).mp. [mp=title, abstract, descriptors]
179 (rct or rcts).mp. [mp=title, abstract, descriptors]
180 (control* adj2 (study or studies or trial*)).mp. [mp=title, abstract, descriptors]
181 or/171‐180
182 170 and 181
183 (guideline* or practice guideline*).mp. [mp=title, abstract, descriptors]
184 (guideline* or guidance* or recommendation*).ti.
185 consensus.ti.
186 183 or 184 or 185
187 170 and 186
188 meta‐analysis.mp. [mp=title, abstract, descriptors]
189 (metaanaly* or meta analy* or met analy* or metanaly*).mp. [mp=title, abstract, descriptors]
190 (collaborative research or collaborative review* or collaborative overview*).mp. [mp=title, abstract, descriptors]
191 (integrative research or integrative review* or integrative overview*).mp. [mp=title, abstract, descriptors]
192 (quantitative adj3 (research or review* or overview*)).mp. [mp=title, abstract, descriptors]
193 (research integration or research overview*).mp. [mp=title, abstract, descriptors]
194 (systematic* adj3 (review* or overview*)).mp. [mp=title, abstract, descriptors]
195 (methodologic* adj3 (review* or overview*)).mp. [mp=title, abstract, descriptors]
196 technology assessment biomedical.mp. [mp=title, abstract, descriptors]
197 (hta or thas or technology assessment*).mp. [mp=title, abstract, descriptors]
198 ((hand adj2 search*) or (manual* adj search*)).mp. [mp=title, abstract, descriptors]
199 ((electronic adj database*) or (bibliographic* adj database*)).mp. [mp=title, abstract, descriptors]
200 ((data adj2 abstract*) or (data adj2 extract*)).mp. [mp=title, abstract, descriptors]
201 (analys* adj3 (pool or pooled or pooling)).mp. [mp=title, abstract, descriptors]
202 mantel haenszel.mp. [mp=title, abstract, descriptors]
203 (cochrane or pubmed or pub med or medline or embase or psycinfo or psyclit or psychinfo or psychlit or cinahl or science citation index).ab.
204 or/188‐203
205 170 and 204
206 182 or 187 or 205
207 limit 206 to yr="2006 ‐Current"
CINAHL‐EBSCO
August 2015
S151 S90 or S104 or S150
S150 S82 and S149
S149 S105 or S106 or S107 or S108 or S109 or S110 or S111 or S112 or S113 or S114 or S115 or S116 or S117 or S118 or S119 or S120 or S121 or S122 or S123 or S124 or S125 or S126 or S127 or S128 or S129 or S130 or S131 or S132 or S133 or S134 or S135 or S136 or S137 or S138 or S139 or S140 or S141 or S142 or S143 or S144 or S145 or S146 or S147 or S148
S148 TX faradic
S147 MH biofeedback
S146 TX Relaxation Therapy
S145 MH Relaxation Therapy
S144 TX alexander N3 technique OR TX alexander N3 method
S143 TX Feldenkrais
S142 TX postur* correction
S141 MH ice
S140 TX Cryoanesthesia
S139 MH Cryoanesthesia
S138 TX vapocoolant spray
S137 (MH "Hyperthermia, Induced")
S136 MH Hydrotherapy
S135 MH cryotherapy
S134 TX repetitive magnetic stimulation
S133 (MH "Physical Therapy+")
S132 (MH "Physical Therapy Modalities+")
S131 MH lasers
S130 (MH "Phototherapy+")
S129 MH Ultrasonic Therapy
S128 (MH "Rehabilitation+")
S127 TX Laser Therapy
S126 (MH "Laser Therapy")
S125 TX traction
S124 MH traction
S123 TX pillow* OR TX collar*
S122 "Occlusal Splints"
S121 TX oral splints
S120 (MH "Periodontal Splints")
S119 TX taping
S118 TX kinesiotaping
S117 (MH "Orthoses")
S116 (MH "Electric Stimulation")
S115 (MH "Magnet Therapy")
S114 MH electromagnetics
S113 (MH "Electromagnetic Fields")
S112 "pulsed electromagnetic field"
S111 TX pulsed electro magnetic field
S110 (MH "Electrical Stimulation, Functional") OR (MH "Electrical Stimulation, Neuromuscular")
S109 (MH "Therapeutic Exercise+")
S108 (MH "Exertion")
S107 (MH "Exercise+")
S106 (MH "Exercise+")
S105 (MH "Combined Modality Therapy+")
S104 S34 and S103
S103 S91 or S92 or S93 or S94 or S95 or S96 or S97 or S98 or S99 or S100 or S101 or S102
S102 (MH "Spondylolisthesis/RH")
S101 (MH "Spondylolysis/RH") OR (MH "Spondylosis/RH")
S100 (MH "Spondylitis, Ankylosing/RH")
S99 (MH "Fibromyalgia/RH")
S98 (MH "Arthritis+/RH")
S97 (MH "Polyradiculopathy/RH")
S96 (MH "Neuritis/RH")
S95 (MH "Spinal Osteophytosis/RH")
S94 (MH "Sprains and Strains/RH")
S93 (MH "Myofascial Pain Syndromes/RH")
S92 (MH "Temporomandibular Joint Syndrome/RH") OR (MH "Temporomandibular Joint Diseases/RH")
S91 (MH "Radiculopathy/RH")
S90 S83 or S84 or S85 or S86 or S87 or S88 or S89
S89 (MH "Brachial Plexus Neuritis/RH")
S88 (MH "Torticollis/RH")
S87 (MH "Thoracic Outlet Syndrome/RH")
S86 (MH "Whiplash Injuries/RH")
S85 (MH "Neck Injuries/RH")
S84 (MH "Brachial Plexus Neuropathies/RH")
S83 (MH "Neck Pain/RH")
S82 S78 NOT S81
S81 S79 or S80
S80 (MM "Pregnancy+")
S79 (MM "Abortion, Induced+")
S78 S74 NOT S77
S77 S75 or S76
S76 (MM "Wounds, Penetrating+")
S75 (MM "Neoplasms+")
S74 S16 or S41 or S56 or S69 or S73
S73 S63 and S72
S72 S70 or S71
S71 TX intervertebral disk displacement or TX intervertebral disc displacement or TX intervertebral disk degeneration or TX intervertebral disc degeneration
S70 (MH "Intervertebral Disk Displacement")
S69 S67 and S68
S68 TX herniat* or TX slipped or TX prolapse* or TX displace* or TX degenerat* or TX ( bulged OR bulge OR bulging )
S67 S63 and S66
S66 S64 or S65
S65 TX disc or TX discs or TX disk or TX disks
S64 (MH "Intervertebral Disk")
S63 S61 NOT S62
S62 (MM "Genital Diseases, Female+") or ( (MM "Cervix") or (MM "Cervix Diseases") )
S61 S57 or S58 or S59 or S60
S60 TX thoracic N3 spine or TX cervical spine or TX cervico*
S59 TX neck or TX thoracic N3 vertebr*
S58 (MH "Thoracic Vertebrae")
S57 (MH "Neck")
S56 S34 and S55
S55 S42 or S43 or S44 or S45 or S46 or S47 or S48 or S49 or S50 or S51 or S52 or S53 or S54
S54 TX neuritis or TX spondylosis or TX spondylitis or TX spondylolisthesis
S53 TX myofascial pain syndome* or TX thoracic outlet syndrome* or TX spinalosteophytosis
S52 TX radiculopathy or TX radiculitis or TX temporomandibular
S51 (MH "Spondylolysis") or (MH "Spondylolisthesis+")
S50 (MH "Fibromyalgia")
S49 (MH "Arthritis+")
S48 (MH "Polyradiculopathy")
S47 (MH "Neuritis+")
S46 (MH "Spinal Osteophytosis")
S45 (MH "Sprains and Strains+")
S44 (MH "Myofascial Pain Syndromes+")
S43 (MH "Temporomandibular Joint Diseases+") or (MH "Temporomandibular Joint Syndrome")
S42 (MH "Radiculopathy")
S41 S34 and S40
S40 S35 or S36 or S37 or S38 or S39
S39 (MH "Neuralgia")
S38 TX stiff or TX discomfort or TX injur* or TX neuropath*
S37 TX pain or TX ache* or TX sore
S36 (MH "Wounds and Injuries+")
S35 (MH "Pain+")
S34 S33 NOT S32
S33 S17 or S18 or S19 or S20 or S21 or S22 or S23 or S24 or S25 or S26 or S27 or S28 or S29 or S30 or S31
S32 (MM "Genital Diseases, Female+") or ( (MM "Cervix") or (MM "Cervix Diseases") )
S31 TX trapezius or TX cervico*
S30 TX thoracic N3 spine or TX thoracic N3 outlet
S29 TX neck
S28 TX thoracic N3 verteb*
S27 TX brachial N3 plexus
S26 TX neck n3 muscles
S25 (MH "Thoracic Vertebrae")
S24 TX ondontoid* or TX cervical or TX occip* or TX atlant*
S23 (MH "Brachial Plexus+")
S22 (MH "Spinal Nerve Roots+")
S21 (MH "Atlanto‐Axial Joint") or (MH "Atlanto‐Occipital Joint")
S20 (MH "Cervical Vertebrae+") or (MH "Cervical Atlas")
S19 (MH "Cervical Plexus+")
S18 (MH "Neck")
S17 (MH "Neck Muscles+")
S16 S10 or S15
S15 S11 NOT S14
S14 S12 or S13
S13 (MM "Cervix") or (MM "Cervix Diseases")
S12 (MM "Genital Diseases, Female+")
S11 (MH "Headache+") and TX cervic*
S10 S1 or S2 or S3 or S4 or S5 or S6 or S7 or S8 or S9
S9 (MH "Brachial Plexus Neuritis")
S8 TX cervical brachial neuralgia
S7 TX cervical rib sydrome* or TX cervico brachial neuralgia or TX cervicobrachial neuralgia or TX monoradicul* or TX monoradicl*
S6 (MH "Thoracic Outlet Syndrome") or (MH "Torticollis")
S5 TX brachial neuralgia or TX neck pain or TX neck injur* or TX brachial plexus neuropath* or TX brachial plexus neuralgia or TX brachial plexus neuritis
S4 TX cervicalgia or TX brachialgia or TX brachial neuritis
S3 TX cervical pain or TX neckache or TX neck ache or TX whiplash or TX cervicodynia
S2 (MH "Neck Injuries+")
S1 (MH "Neck Pain") or (MH "Brachial Plexus Neuropathies") or (MH "Brachial Plexus Neuritis")
ICL
August 2015
S1 Subject:"Neck Pain" OR Subject:"Brachial Plexus Neuritis" OR All Fields:"brachial plexus neuropathies"
S2 All Fields:brachial plexus neuropathy
S4 Subject:"Neck Injuries" OR Subject:"Whiplash Injuries" OR Subject:"Cervical Vertebrae / abnormalities"
S5 All Fields:"cervical pain" OR All Fields:neckache OR All Fields:whiplash
S6 All Fields:cervicodynia OR All Fields:cervicalgia OR All Fields:brachialgia
S7 All Fields:"brachial neuritis" OR All Fields:"brachial neuralgia" OR All Fields:"neck pain"
S8 Subject:"Thoracic Outlet Syndrome" OR Subject:"Torticollis" OR All Fields:cervical rib syndrom*
S11 All Fields:cerv* AND All Fields:headache*
S12 All Fields:monoradicul* OR All Fields:monoradicl*
S13 S1 OR S2 OR S4 OR S5 OR S6 OR S7 OR S8 OR S11 OR S12
S14 Subject:"Neck" OR Subject:"Neck Muscles" OR Subject:"Cervical Vertebrae"
S16 Subject:"Cervical Atlas" OR Subject:"Atlanto‐Axial Joint" OR Subject:"Atlanto‐Occipital Joint"
S17 Subject:"Atlas" OR Subject:"Spinal Nerve Roots" OR All Fields:"brachial plexus"
S18 All Fields:ondontoid* OR All Fields:occip* OR All Fields:atlant*
S20 Subject:"Odontoid Process" OR Subject:"Thoracic Vertebrae" OR All Fields:"cervical vertebrae"
S21 All Fields:"cervical spine" OR All Fields:trapezius OR All Fields:cervico*
S22 S14 OR S16 OR S17 OR S18 OR S20 OR S21
S23 Subject:"Pain" OR All Fields:sore OR All Fields:stiff
S24 All Fields:ache OR All Fields:pain OR All Fields:discomfort
S25 All Fields:injur* OR All Fields:neuropath*
S26 S23 OR S24 OR S25
S27 S22 AND S26
S28 Subject:"Radiculopathy" OR Subject:"Temporomandibular Joint Disorders" OR Subject:"Temporomandibular Joint Dysfunction Syndrome"
S30 Subject:"Myofascial Pain Syndromes" OR Subject:"Sprains and Strains" OR Subject:"Spinal Osteophytosis"
S31 Subject:"Neuritis" OR Subject:"Polyradiculoneuritis" OR Subject:"Arthritis"
S32 Subject:"Fibromyalgia" OR Subject:"Discitis" OR Subject:"Spondylitis"
S33 Subject:"Spondylolisthesis" OR Subject:"Spondylolysis" OR Subject:"Spondylosis"
S34 S28 OR S30 OR S31 OR S32 OR S33
S35 S22 AND S34
S36 Subject:"Neck" OR Subject:"Cervical Vertebrae" OR Subject:"Thoracic Vertebrae"
S37 All Fields:"thoracic spine" OR All Fields:"cervical spine" OR All Fields:cervico*
S38 S36 OR S37
S39 All Fields:herniat* OR All Fields:slipped OR All Fields:prolapse*
S40 All Fields:displace* OR All Fields:degenerat*
S41 All Fields:bulge OR All Fields:bulged OR All Fields:bulging
S42 S39 OR S40 OR S41
S43 S38 AND S42
S44 Subject:"Intervertebral Disk Displacement" OR All Fields:"intervertebral disk degeneration" OR All Fields:"intervertebral disc degeneration"
S45 All Fields:"Intervertebral Disk Displacement" OR All Fields:"intervertebral disc displacement"
S46 S44 OR S45
S47 S38 AND S46
S48 S13 OR S27 OR S35 OR S43 OR S47
S49 Year: from 2014 to 2015
S50 S48 AND S49
S51 Subject:"Randomized Controlled Trials as Topic" OR Subject:"Controlled Clinical Trials" OR Subject:"Placebos"
S52 All Fields:random* OR All Fields:sham OR All Fields:placebo*
S53 All Fields:clinical trial* OR All Fields:"controlled study" OR All Fields:"controlled studies"
S54 All Fields:RCT OR All Fields:RCTs
S55 S51 OR S52 OR S53 OR S54
S56 S50 AND S55
Appendix 2. Criteria for assessing risk of bias for internal validity
Random sequence generation (selection bias)
Selection bias (biased allocation to interventions) due to inadequate generation of a randomised sequence
Risk of selection bias is low if investigators describe a random component in the sequence generation process such as referring to a random number table, using a computer random number generator, tossing a coin, shuffling cards or envelopes, throwing dice, drawing lots and minimising (minimisation may be implemented without a random element, and this is considered to be equivalent to being random).
Risk of selection bias is high if investigators describe a non‐random component in the sequence generation process such as sequence generated by odd or even date of birth, date (or day) of admission, hospital or clinic record number; or allocation by judgement of the clinician, preference of the participant, results of a laboratory test or series of tests, or availability of the intervention.
Allocation concealment (selection bias)
Selection bias (biased allocation to interventions) due to inadequate concealment of allocations before assignment
Risk of selection bias is low if participants and investigators enrolling participants could not foresee assignment because one of the following, or an equivalent method, was used to conceal allocation: central allocation (including telephone, web‐based and pharmacy‐controlled randomisation); sequentially numbered drug containers of identical appearance; or sequentially numbered, opaque, sealed envelopes.
Risk of bias is high if participants or investigators enrolling participants could possibly foresee assignments and thus introduce selection bias, such as allocation based on using an open random allocation schedule (e.g. list of random numbers); assignment envelopes were used without appropriate safeguards (e.g. if envelopes were unsealed or non‐opaque or not sequentially numbered); alternation or rotation; date of birth; case record number; or other explicitly unconcealed procedures.
Blinding of participants
Performance bias due to knowledge of allocated interventions by participants during the study
Risk of performance bias is low if blinding of participants was ensured and it was unlikely that blinding could have been broken; or if no blinding or incomplete blinding was provided but the review authors judged that the outcome is not likely to be influenced by lack of blinding.
Blinding of personnel/care providers (performance bias)
Performance bias due to knowledge of allocated interventions by personnel/care providers during the study
Risk of performance bias is low if blinding of personnel was ensured and it was unlikely that blinding could have been broken; or if no blinding or incomplete blinding was provided but the review authors judged that the outcome is not likely to be influenced by lack of blinding.
Blinding of outcome assessor (detection bias)
Detection bias due to knowledge of allocated interventions by outcome assessors
Risk of detection bias is low if blinding of the outcome assessment was ensured and it was unlikely that blinding could have been broken; or if no blinding or incomplete blinding was provided but the review authors judged that the outcome is not likely to be influenced by lack of blinding, or:
for patient‐reported outcomes in which the participant was the outcome assessor (e.g. pain, disability): Risk of bias for outcome assessors is low if risk of bias for participant blinding is low (Boutron 2005);
for outcome criteria that are clinical or therapeutic events that will be determined by the interaction between participants and care providers (e.g. co‐interventions, length of hospitalisation, treatment failure), in which the care provider is the outcome assessor: Risk of bias for outcome assessors is low if risk of bias for care providers is low (Boutron 2005); and
for outcome criteria that are assessed from data from medical forms: Risk of bias is low if the treatment or adverse effects of the treatment could not be noticed in the extracted data (Boutron 2005).
Incomplete outcome data (attrition bias)
Attrition bias due to amount, nature or handling of incomplete outcome data
Risk of attrition bias is low if no outcome data were missing; reasons for missing outcome data were unlikely to be related to the true outcome (for survival data, censoring is unlikely to be introducing bias); missing outcome data were balanced in numbers, with similar reasons for missing data across groups; for dichotomous outcome data, the proportion of missing outcomes compared with the observed event risk was not enough to have a clinically relevant impact on the intervention effect estimate; for continuous outcome data, the plausible effect size (difference in means or standardised difference in means) among missing outcomes was not enough to have a clinically relevant impact on observed effect size, or missing data were imputed using appropriate methods (if drop‐outs were very large, imputation using even 'acceptable' methods may still suggest high risk of bias) (van Tulder 2003). The percentage of withdrawals and drop‐outs should not exceed 20% for short‐term follow‐up and 30% for long‐term follow‐up and should not lead to substantial bias (these percentages are commonly used but arbitrary and are not supported by the literature) (van Tulder 2003).
Selective reporting (reporting bias)
Reporting bias due to selective outcome reporting
Risk of reporting bias is low if the study protocol is available and all of the study's pre‐specified (primary and secondary) outcomes of interest in the review have been reported in the pre‐specified way, or if the study protocol is not available but it is clear that published reports include all expected outcomes, including those that were pre‐specified (convincing text of this nature may be uncommon).
Risk of reporting bias is high if not all of the study's pre‐specified primary outcomes have been reported; one or more primary outcomes were reported using measurements, analysis methods or subsets of the data (e.g. subscales) that were not pre‐specified; one or more reported primary outcomes were not pre‐specified (unless clear justification for their reporting is provided, such as an unexpected adverse effect); one or more outcomes of interest in the review were reported incompletely so that they cannot be entered into a meta‐analysis; or the study report fails to include results for a key outcome that would be expected to have been reported for such a study.
Group similarity at baseline (selection bias)
Bias due to dissimilarity at baseline for the most important prognostic indicators.
Risk of bias is low if groups were similar at baseline for demographic factors, value of main outcome measure(s) and important prognostic factors (examples in the field of back and neck pain are duration and severity of complaints, vocational status and percentage of participants with neurological symptoms) (van Tulder 2003).
Co‐interventions (performance bias)
Bias because co‐interventions were different across groups
Risk of bias is low if no co‐interventions were provided, or if they were similar between index and control groups (van Tulder 2003).
Compliance (performance bias)
Bias due to inappropriate compliance with interventions across groups
Risk of bias is low if compliance with the interventions was acceptable and was based on reported intensity/dosage, duration, number and frequency for both index and control intervention(s). For single‐session interventions (e.g. surgery), this item is irrelevant (van Tulder 2003).
Intention‐to‐treat analysis
Risk of bias is low if all randomised participants were reported/analysed in the group to which they were allocated by randomisation.
Timing of outcome assessments (detection bias)
Bias because important outcomes were not measured at the same time across groups
Risk of bias is low if all important outcome assessments for all intervention groups were measured at the same time (van Tulder 2003).
Other bias
Bias due to problems not covered elsewhere in the table
Risk of bias is low if the study appears to be free of other sources of bias not addressed elsewhere (e.g. study funding).
Appendix 3. Questions for clinical relevance
Are patients described in sufficient detail that you can decide whether they are comparable with those whom you see in your practice?
Are interventions and treatment settings described well enough that you can provide the same for your patients?
Were all clinically relevant outcomes measured and reported?
Is the size of the effect clinically important?
Are likely treatment benefits worth potential harms?
Data and analyses
Comparison 1.
Acupuncture versus sham treatment
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Pain intensity (VAS) immediate post treatment | 11 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.1 Chronic MPS 1 treatment session | 2 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Chronic MND 3 to 4 wk treatment | 4 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 Chronic MPS 12 wk treatment | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.4 Chronic MND SA group 10 wk treatment | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.5 Cervical osteoarthritis 1 treatment session | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.6 Chronic MPS 3 wk treatment, pain with movement scale | 2 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Pain intensity (VAS) short term | 8 | 560 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.23 [‐0.40, ‐0.07] |
| 2.1 Chronic MPS 3 wk treatment, 3 mo follow‐up, pain with movement scale | 1 | 34 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [‐0.67, 0.67] |
| 2.2 Chronic MND 3 to 4 wk treatment, 1 to 4 wk follow‐up | 1 | 34 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.15 [‐0.82, 0.52] |
| 2.3 Chronic MND 3 to 4 wk treatment, 3 mo follow‐up | 3 | 319 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.18 [‐0.40, 0.04] |
| 2.4 Subacute/chronic WAD 6 wk treatment, 3 mo follow‐up | 1 | 124 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.38 [‐0.73, ‐0.02] |
| 2.5 WAD myofascial 2 to 6 sessions, 6 wk follow‐up | 1 | 34 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.60 [‐1.29, 0.09] |
| 2.6 Chronic MND SA group 10 wk treatment, 3 wk follow‐up | 1 | 15 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.10 [‐1.11, 0.92] |
| 3 Pain intensity (VAS) intermediate term | 2 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 3.1 Chronic MPS ESNS 3 to 4 wk treatment, 6 mo follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Chronic WAD 6 wk treatment, 6 mo follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Pain intensity (VAS) long term | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.1 Chronic MPS ESNNS 3 to 4 wk treatment, 3 year follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Disability (NDI) immediate post treatment | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 5.1 Chronic MND SA group 10 wk treatment | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Disability (NPQ) immediate post treatment | 3 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6.1 Chronic MND, 3 wk treatment | 3 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Disability (NPQ) short term | 2 | 290 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.38 [‐0.62, ‐0.15] |
| 7.1 Chronic MND, 3 wk treatment, 3 mo follow‐up | 2 | 290 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.38 [‐0.62, ‐0.15] |
| 8 Disability (NDI) short term | 4 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 8.1 Chronic MND SA group 10 wk treatment, 3 wk follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.2 Chronic WAD 6 wk treatment, 3 mo follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.3 WAD II myofascial 2 to 6 treatment, 6 wk follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.4 Chronic MPS 1 treatment | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 9 Disability (NDI) intermediate term | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 9.1 Chronic WAD 6 wk treatment, 6 mo follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 10 Quality of life (SF‐36) immediate post treatment | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 10.1 Chronic MND, 3 wk treatment | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 11 Quality of life (SF‐36) short term | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 11.1 Chronic MND, 3 wk treatment, 3 mo follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
Comparison 2.
Acupuncture versus inactive control
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Pain intensity (VAS) immediate post treatment | 5 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.1 Chronic MPS 4 wk treatment | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Chronic MND NLA group 1 treatment session, movement scale | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 Chronic MND 3 to 4 wk treatment | 2 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.4 Cervical osteoarthritis 1 treatment session | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Pain intensity (VAS) short term | 5 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2.1 Chronic MND 3 to 4 wk treatment, 1 to 4 wk follow‐up | 5 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Pain intensity (VAS) intermediate term | 3 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 3.1 Chronic MPS 4 wk treatment, 6 mo follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Chronic MND 3 to 4 wk treatment, 6 mo follow‐up | 2 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Pain intensity (VAS) long term | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.1 Chronic MND 3 to 4 wk treatment, 12 mo follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Pain pressure threshold immediate post treatment | 2 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 5.1 Chronic MND 3 to 4 wk treatment | 2 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Pain pressure threshold short term | 2 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6.1 Chronic MND 3 to 4 wk treatment, 1 to 3 month follow‐up | 2 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Pain intensity (proportion pain relief) immediate post treatment | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 7.1 Chronic MND 4 wk treatment | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 8 Disability (NDI) short term | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 9 Disability (NDI) intermediate term | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 9.1 Chronic MND 4 wk treatment, 6 mo follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 10 Disability (NDI) long term | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 10.1 Chronic MND 4 wk treatment, 12 mo follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 11 Function (NHP) immediate post treatment | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 11.1 Chronic MPS 4 wk treatment | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 12 Function (NHP) intermediate term | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 12.1 Chronic MPS 4 wk treatment 6 mo follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 13 Function (NPQ) short term | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 13.1 Chronic MND 1 wk follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 14 Quality of life (SF‐36, Functional Component) short term | 2 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 14.1 Chronic MND 3 to 4 wk treatment, 8 wk follow‐up | 2 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
Comparison 3.
Acupuncture versus wait‐list
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Pain intensity (VAS) short term | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.1 Chronic NDR 4 wk treatment, 8 wk follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Disability (neck and pain disability scale) short term | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2.1 Chronic MND 3 mo treatment, 3 mo follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Disability (neck and pain disability scale) intermediate term | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 3.1 Chronic MND 3 mo treatment, 6 mo follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Quality of life (SF‐36 mental score) short term | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.1 Chronic MND 3 mo treatment, 3 mo follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Quality of life (SF‐36 mental score) intermediate term | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 5.1 Chronic MND 3 mo treatment, 6 mo follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Quality of life (SF‐36 physical score) intermediate term | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6.1 Chronic MND 3 mo treatment, 6 mo follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
What's new
| Date | Event | Description |
|---|---|---|
| 16 November 2016 | Amended | We have received comments on this review and have withdrawn it from the Library while comments are being addressed. |
History
Protocol first published: Issue 3, 2004 Review first published: Issue 3, 2006
| Date | Event | Description |
|---|---|---|
| 31 December 2015 | New citation required and conclusions have changed | The previous version of this review included 10 studies that focused on chronic neck pain. In this review, we included 27 studies representing acupuncture for a variety of acute and chronic neck disorders |
| 31 December 2015 | New search has been performed | The 'Risk of bias' assessment tool (Furlan 2009) was utilised for this update. Previously, according to our protocol, Jadad 1996 and van Tulder 2003 assessment tools were used Methods: inclusion criteria different from protocol; now only RCTs included |
| 22 May 2014 | Amended | Contact details updated |
| 19 June 2008 | Amended | Converted to new review format |
Differences between protocol and review
We included only randomised controlled trials (RCTs) in this update. In the original review, we included RCTs and quasi‐RCTs, as per protocol.
We used the risk of bias assessment tool of the Cochrane Back Review Group (Furlan 2009) for this update. We previously used the assessment tools used in Jadad 1996 and van Tulder 2003.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | RCT Number analysed/randomised: 36/46 Intention‐to‐treat: NR Power analysis: NR Funding source: intramural grant from the Anesthesia Department of Brigham and Women's Hospital, Boston, MA | |
| Participants | Myofascial neck pain lasting ≥ 6 months Participant recruitment: hospital‐based pain management centre, neurology clinic, public announcement |
|
| Interventions | INDEX TREATMENT Group 1 ‐ relevant acupuncture (believed to be effective for the condition treated) Pre‐determined relevant points; shallow needling (2 to 3 mm) used with copper wire containing silicone diode applied for stage 1 of session (10 minutes); infrared lamp also used over points during stage 2 of treatment (10 minutes). Treatment done without Deqi by a licensed acupuncturist with 13 years of experience COMPARISON TREATMENT 1 Group 2 ‐ irrelevant acupuncture Same treatment dosage and duration as Group 1, using pre‐determined irrelevant points with copper wire attached but connections severed (stage 1) and placebo light (no heat during stage 2) COMPARISON TREATMENT 2 Group 3 ‐ medical control NSAID 500 mg OD Trilisate, no acupuncture CO‐INTERVENTION Avoided Treatment schedule: 14 sessions over 12 weeks, with each session averaging 30 minutes in duration Duration of follow‐up: immediate post treatment |
|
| Outcomes | PAIN INTENSITY (VAS 0 to 10 scale) Baseline mean: relevant 4.8, irrelevant 4.7, control 4.9 End of study mean: relevant 1.87, irrelevant 3.37, control 4.73 Absolute benefit: relevant 2.93, irrelevant 1.33, control 0.17 Reported results: Relevant acupuncture group had significantly lower pain scores, including hourly ratings SMD ‐2.52 (95% CI random ‐3.49 to ‐1.54) immediate post treatment Reasons for drop‐out: 2 moved, 6 not specified, 2 lost to contact Adverse effects: NR Costs of care: NR |
|
| Notes | ‐‐ | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes ‐ patient? | Low risk | Adequately described |
| Blinding (performance bias and detection bias) All outcomes ‐ care provider? | High risk | Not possible |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessor? | Low risk | Participant blinded as outcome assessor of self reports |
| Incomplete outcome data (attrition bias) All outcomes ‐ Drop out rate acceptable? | Low risk | Described and acceptable |
| Incomplete outcome data (attrition bias) All outcomes ‐ Analyzed in the group to which they were allocated? | High risk | Did not analyse; all randomised |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics | Low risk | Reported to be similar |
| Co‐interventions avoided or similar? | Unclear risk | Not reported |
| Compliance acceptable? | Low risk | Each participant attended 14 sessions, twice weekly |
| Similar timing of outcome assessment? | Low risk | All assessed at 12 weeks |
| Fatal Flaw | Low risk | Acceptable |
| Methods | RCT Number analysed/randomised: 116/124 Intention‐to‐treat: reported but not done Power analysis: calculated Funding source: government organisational funds | |
| Participants | Subacute and chronic WAD Participant recruitment: newspaper advertisement University Clinic, Sydney, Australia |
|
| Interventions | INDEX TREATMENT Group 1 ‐ real electroacupuncture (EAP) Acupuncture points = GB39, GB20, L114, SI6 bilaterally 1 to 1.5 cm depth; electrodes attached to needles at 2 acupuncture points in the cervical area, plus 1 in each wrist and ankle 2 to 5 Hz 1.5 v; unable to feel the current COMPARISON TREATMENT Group 2 ‐ simulated EAP Same treatment dosage and duration as Group 1, points 20 to 30 mm from selected points; same attachment of electrodes but machine not turned on CO‐INTERVENTION Comparable between groups; included medication, physiotherapy and chiropractic therapy Treatment schedule: 2 sessions/wk over 6 weeks, with each session averaging 30 minutes in duration Duration of follow‐up: 3 and 6 months |
|
| Outcomes | PAIN INTENSITY (VAS 10 cm scale) Baseline mean: real EAP 5.3, simulated 5.8 End of study mean: real EAP 4.1, simulated 5.5 Absolute benefit: real EAP 1.2, simulated 0.3 Reported results: significant favouring real EAP group SMD ‐0.38 (95% CI random ‐0.73 to ‐0.02) at 3 months SMD ‐0.59 (95% CI random ‐0.95 to ‐0.23) at 6 months FUNCTION (NDI 50 point scale) Baseline mean: real EAP 15.6, simulated 18.7 End of study mean: real EAP 14.5, simulated 16.8 Absolute benefit: real EAP 1.1, simulated 1.9 Reported results: not significant SMD ‐0.22 (95% CI random ‐0.57 to 0.13) at 3 months SMD ‐0.31 (95% CI random ‐0.66 to 0.05) at 6 months Quality of life (SF‐36, Physical Component) Baseline mean: real EAP 43.6, simulated 41.3 End of study mean: real EAP 41.9, simulated 38.3 Absolute benefit: real EAP 1.7, simulated 3.0 Reported results: not significant Reasons for drop‐out: 8 in control group, no reasons given Adverse effects: similar in both groups, including slight pain, sweating and decreased blood pressure Costs of care: NR |
|
| Notes | ‐‐ | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sequence generated by random numbers table |
| Allocation concealment (selection bias) | Low risk | Numbered opaque envelopes |
| Blinding (performance bias and detection bias) All outcomes ‐ patient? | Low risk | Adequately blinded |
| Blinding (performance bias and detection bias) All outcomes ‐ care provider? | High risk | Not possible |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessor? | Low risk | Adequately blinded participant as outcome assessor of self reports |
| Incomplete outcome data (attrition bias) All outcomes ‐ Drop out rate acceptable? | Low risk | Described and adequate |
| Incomplete outcome data (attrition bias) All outcomes ‐ Analyzed in the group to which they were allocated? | High risk | Not all in control group analysed (52/60) |
| Selective reporting (reporting bias) | Low risk | Protocol provided by study author (grey literature) |
| Similarity of baseline characteristics | Low risk | Reported to be similar |
| Co‐interventions avoided or similar? | Unclear risk | Reported as no evidence of imbalance but no results provided |
| Compliance acceptable? | Low risk | Reported and acceptable |
| Similar timing of outcome assessment? | Low risk | Baseline, 3 and 6 months |
| Fatal Flaw | Low risk | Acceptable |
| Methods | RCT Number Analysed/randomised: 10/10 Intention‐to‐treat: calculated Power analysis: NR Funding source: none | |
| Participants | Chronic myofascial neck pain Participant recruitment: pain control clinic, Taiwan |
|
| Interventions | INDEX TREATMENT Remote acupuncture group (RA) Acupuncture points ‐ TE5, LI11; the needle was manipulated for the Deqi. First, TE5 was inserted and manipulated for 15 seconds; after 5 minutes, LI11 was treated in the same way. Five minutes later, both needles were manipulated for 15 seconds at the same time; manipulation stopped and needles remained inserted for 3 minutes COMPARISON TREATMENT Sham acupuncture Sham acupuncture needle inserted into rubber connector taped onto skin at TE5 and LI11; needle contacted skin but did not penetrate. No manipulation of needle CO‐INTERVENTION Avoided Treatment schedule: 1 session Duration of follow‐up: immediate post treatment |
|
| Outcomes | PAIN INTENSITY (0 to 10 VAS scale) Baseline mean: RA 7.4, sham 7.4 End of study mean: RA 3.3, sham 7.1 Absolute benefit: RA 4.1, sham 0.3 Reported results: significant favouring acupuncture SMD ‐3.62 (95% CI random ‐5.15 to ‐2.09) immediate post treatment Drop‐outs: none Adverse effects: NR Costs of care: NR |
|
| Notes | ‐‐ | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sequence was generated from a computerised randomisation programme |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes ‐ patient? | Low risk | Described in the report |
| Blinding (performance bias and detection bias) All outcomes ‐ care provider? | High risk | Not possible |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessor? | Low risk | Described in the report |
| Incomplete outcome data (attrition bias) All outcomes ‐ Drop out rate acceptable? | Low risk | No drop‐outs |
| Incomplete outcome data (attrition bias) All outcomes ‐ Analyzed in the group to which they were allocated? | Low risk | All randomised participants were analysed |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics | Low risk | Reported to be similar |
| Co‐interventions avoided or similar? | Low risk | Avoided by design (pre/post) |
| Compliance acceptable? | Low risk | Acceptable by design (pre/post) |
| Similar timing of outcome assessment? | Low risk | Immediate post |
| Fatal Flaw | High risk | Main problem involves reporting errors and statistical analyses. No estimate of differences between groups, only percent changes between groups; only evidence of improvement in abstract results was noted within groups, not between groups; Table 1 P values are incorrect for pain duration and initial pain; no P values should be provided for % change data |
| Methods | RCT Number analysed/randomised: 30/30 Intention‐to‐treat: NR Power analysis: NR Funding source: NR | |
| Participants | Chronic mechanical neck disorder with radicular symptoms or signs Participant recruitment: newspaper advertisement | |
| Interventions | INDEX TREATMENT Acupuncture (treatment group) Technique according to classical oriental meridian theory healing by stimulating energy flow in the body; acupuncture points varied between participants and varied from day to day; electroacupuncture and moxibustion were used in some participants; other treatment parameters were not specified COMPARISON Wait‐list (control group) Treatment schedule: 3 to 4 sessions/wk over 4 weeks Duration of follow‐up: 8 weeks CO‐INTERVENTION Comparable between index and control groups for medication use only |
|
| Outcomes | PAIN (VAS scale 0 to 10) Baseline mean: acupuncture 6.0, control 5.3 End of study mean: acupuncture 3.6, control 5.4 Absolute benefit: acupuncture 2.4, control ‐0.1 Reported results: significant improvement favouring acupuncture SMD ‐0.74 (95% random CI ‐1.49 to 0.00) at 8 weeks Reasons for drop‐out: NA Adverse effects: NR Costs of care: NR |
|
| Notes | ‐‐ | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Equally sized and folded papers in a box, half marked A, the other half B |
| Allocation concealment (selection bias) | High risk | Papers not concealed |
| Blinding (performance bias and detection bias) All outcomes ‐ patient? | High risk | Not blinded |
| Blinding (performance bias and detection bias) All outcomes ‐ care provider? | High risk | Not possible |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessor? | High risk | Participant as outcome assessor not blinded |
| Incomplete outcome data (attrition bias) All outcomes ‐ Drop out rate acceptable? | Low risk | No drop‐outs |
| Incomplete outcome data (attrition bias) All outcomes ‐ Analyzed in the group to which they were allocated? | Low risk | No missing data |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics | Low risk | Reported to be similar |
| Co‐interventions avoided or similar? | High risk | Only medications reported, no other interventions mentioned |
| Compliance acceptable? | High risk | Not reported |
| Similar timing of outcome assessment? | Low risk | 8 weeks after treatment |
| Fatal Flaw | Low risk | Acceptable |
| Methods | RCT Number Analysed/randomised: 112/117 Intention‐to‐treat: NR Power analysis: NR Funding source: State Ministry of Science and Technology | |
| Participants | Chronic cervical spondylosis Participant recruitment: Acupuncture Department of Guangdong Provincial Traditional Chinese Medicine Hospital, China |
|
| Interventions | INDEX TREATMENT Acupuncture group Acupuncture points ‐ Du14, ExHN15, SI15 needles inserted to muscle layer manipulated for Deqi, then remained inserted for 20 minutes; infrared radiation COMPARISON TREATMENT Sham Superficial insertion 1 cm apart laterally from acupuncture points. Remained for 20 minutes, no manipulation; infrared radiation CO‐INTERVENTION NR Treatment schedule: once every other day for 9 sessions over 18 days Duration of follow‐up: immediate post treatment, 4 weeks, 3 months |
|
| Outcomes | PAIN INTENSITY (0 to 10 VAS scale) Baseline mean: acupuncture 5.14, sham 5.58 End of study mean: acupuncture 2.89, sham 3.28 at 3 month follow‐up Absolute benefit: acupuncture 2.25, sham 2.30 Reported results: significant immediate post treatment favouring acupuncture but not over long term SMD ‐0.53 (95% CI random ‐0.91 to ‐0.16) immediate post treatment SMD ‐0.59 (95% CI random ‐0.97 to ‐0.21) at 4 weeks SMD ‐0.23 (95% CI random ‐0.61 to 0.14) at 3 months Northwick Park Pain Questionnaire (NPQ) (0 to 100) Baseline mean: acupuncture 33.63, sham 33.21 End of study mean: acupuncture 20.55, sham 25.77 Absolute benefit: acupuncture 13.08, sham 7.44 Reported results: significant immediate post treatment favouring acupuncture but not over long term SMD ‐0.41 (95% CI random ‐0.79 to ‐0.04) immediate post treatment SMD ‐0.50 (95% CI random ‐0.88 to ‐0.12) at 4 weeks SMD ‐0.40 (95% CI random ‐0.78 to ‐0.03) at 3 months Reasons for drop‐out: 2 fainted, 3 inconvenient (rate 4.27%) Adverse effects: 1 in each group fainted Costs of care: NR |
|
| Notes | ‐‐ | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computerised sequence number and grouping address on a randomising card |
| Allocation concealment (selection bias) | Low risk | Use of sealed opaque envelopes |
| Blinding (performance bias and detection bias) All outcomes ‐ patient? | Low risk | Described adequately in the report |
| Blinding (performance bias and detection bias) All outcomes ‐ care provider? | High risk | Not possible |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessor? | Low risk | Participant as outcome assessor |
| Incomplete outcome data (attrition bias) All outcomes ‐ Drop out rate acceptable? | Low risk | Described and acceptable 4.27% |
| Incomplete outcome data (attrition bias) All outcomes ‐ Analyzed in the group to which they were allocated? | High risk | Not all randomised participants were analysed |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics | Low risk | Reported to be similar |
| Co‐interventions avoided or similar? | Unclear risk | Not reported |
| Compliance acceptable? | Unclear risk | Not reported |
| Similar timing of outcome assessment? | Low risk | Post, 4 weeks, 12 weeks |
| Fatal Flaw | High risk | No sample size justifications; multiple comparisons should have been done; analysis should have been stratified by syndrome type; time lines between points on graph are distorted |
| Methods | RCT Number analysed/randomised: 24/24 Intention‐to‐treat: NR Power analysis: NR Funding source: NR | |
| Participants | Chronic neck pain Participant recruitment: selected from 5 large companies in Oslo by the company's occupational physician, Norway |
|
| Interventions | INDEX TREATMENT Acupuncture 16 body points, 6 ear points, electrostimulation COMPARISON TREATMENT Placebo 10 to 14 mm distal to real points or 4 to 6 mm for ear points; electrostimulation set up but no voltage CO‐INTERVENTION Reported, see 'Risk of bias' Treatment schedule: 3 times per week, over 3 to 4 weeks, for a total of 10 treatments, with each session averaging 45 minutes in duration Duration of follow‐up: immediate post treatment, 6 months, 3 years |
|
| Outcomes | PAIN INTENSITY (0 to 100 VAS scale) Baseline mean: acupuncture 57, placebo 48 End of study mean: acupuncture 15, placebo 36 immediate post treatment Absolute benefit: acupuncture 42, placebo 12 Reported results: statistically significant favouring acupuncture at immediate post and 6 month follow‐up SMD ‐3.17 (95% CI random ‐4.44 to ‐1.90) immediate post treatment SMD ‐1.54 (95% CI random ‐2.47 to ‐0.61) at 6 months SMD ‐2.72 (95% CI random ‐3.89 to ‐1.56) at 3 years Drop‐outs: none Adverse effects: NR Costs of care: NR |
|
| Notes | ‐‐ | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation by draw with replacement |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes ‐ patient? | Low risk | Described in report |
| Blinding (performance bias and detection bias) All outcomes ‐ care provider? | High risk | Not possible |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessor? | Low risk | Described in report |
| Incomplete outcome data (attrition bias) All outcomes ‐ Drop out rate acceptable? | Low risk | No drop‐outs |
| Incomplete outcome data (attrition bias) All outcomes ‐ Analyzed in the group to which they were allocated? | Low risk | All participants randomised were analysed, described in report |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics | High risk | Not similar with respect to PPT and duration of symptoms; also headache baseline information not provided |
| Co‐interventions avoided or similar? | High risk | 21% of the intervention group and 50% of the control group received other treatment |
| Compliance acceptable? | Low risk | All participants completed all 10 treatments |
| Similar timing of outcome assessment? | Low risk | All assessed immediate post, 6 months, 3 years |
| Fatal Flaw | Low risk | Acceptable |
| Methods | RCT Number analysed/randomised: 24/24 Intention‐to‐treat: NR Power analysis: NR Funding source: NR | |
| Participants | Chronic neck pain Participant recruitment: selected from 5 large companies in Oslo by the company's occupational physician, Norway |
|
| Interventions | INDEX TREATMENT Acupuncture 16 body points, 6 ear points, electrostimulation COMPARISON TREATMENT Placebo 10 to 14 mm distal to real points or 4 to 6 mm for ear points; electrostimulation but no voltage CO‐INTERVENTION Reported, see 'Risk of bias' Treatment schedule: 3 times/wk over 3 to 4 weeks for a total of 10 treatments, with each session averaging 45 minutes in duration Duration of follow‐up: immediate post treatment, 6 months, 3 years |
|
| Outcomes | PAIN INTENSITY (0 to 100 VAS scale) Baseline mean: acupuncture 57, placebo 48 End of study mean: acupuncture 15, placebo 36 at immediate post Absolute benefit: acupuncture 42, placebo 12 Reported results: statistically significant favouring acupuncture at immediate post and 3 year follow‐up SMD ‐3.17 (95% CI random ‐4.44 to ‐1.90) immediate post treatment SMD ‐1.75 (95% CI random ‐3.01 to ‐0.49) at 6 months SMD ‐3.33 (95% CI random ‐4.78 to ‐1.88) at 3 years Drop‐outs: none Adverse effects: NR Costs of care: NR |
|
| Notes | ‐‐ | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported adequately |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes ‐ patient? | High risk | Interventions perceivably different |
| Blinding (performance bias and detection bias) All outcomes ‐ care provider? | High risk | Not possible |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessor? | High risk | Participant as outcome assessor not blinded |
| Incomplete outcome data (attrition bias) All outcomes ‐ Drop out rate acceptable? | Low risk | No drop‐outs |
| Incomplete outcome data (attrition bias) All outcomes ‐ Analyzed in the group to which they were allocated? | Unclear risk | Not reported |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics | Low risk | Reported to be similar |
| Co‐interventions avoided or similar? | Low risk | Reported to be similar |
| Compliance acceptable? | Low risk | Each participant received 3 treatments/wk to a total of 10 |
| Similar timing of outcome assessment? | Low risk | All assessed at 6 months and 3 years |
| Fatal Flaw | Low risk | Acceptable |
| Methods | RCT Number analysed/randomised: 60/60 Intention‐to‐treat: NR Power analysis: NR Funding source: NR |
|
| Participants | Chronic myofascial pain syndrome | |
| Interventions | INDEX TREATMENT Dry needling (dn) upper trapezius COMPARISON TREATMENT Placebo laser CO‐INTERVENTION Paracetamol as needed Treatment schedule: dn once/wk over 4 weeks, placebo laser 3 sessions/wk over 4 weeks Duration of follow‐up: immediate post treatment and 6 months |
|
| Outcomes | PAIN INTENSITY (VAS activity 10 cm scale) Baseline mean: dn 7.62, placebo 7.65 End of study mean: dn 4.24, placebo 4.22 Absolute benefit: dn 3.38, placebo 3.43 Reported results: significant differences favouring laser compared with dn and placebo post treatment only SMD ‐0.02 (95% CI random ‐0.64 to 0.60) immediate post treatment SMD 0.01 (95% CI random ‐0.61 to 0.63 at 6 months FUNCTION: Nottingham Health Profile Physical Activity Component (0 to 100) Baseline mean: dn 32.80, placebo 25.59 End of study mean: dn 13.68, placebo 16.08 Absolute benefit: dn 19.12, placebo 9.51 Reported results: significant differences favouring laser compared with dn and placebo SMD 0.22 (95% CI random ‐0.40 to 0.84) immediate post treatment SMD ‐0.14 (95% CI random ‐0.76 to 0.48) at 6 months Adverse effects: NR Costs of care: NR |
|
| Notes | ‐‐ | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes ‐ patient? | High risk | Interventions perceivably different |
| Blinding (performance bias and detection bias) All outcomes ‐ care provider? | High risk | Not possible |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessor? | High risk | Participant as outcome assessor not blinded |
| Incomplete outcome data (attrition bias) All outcomes ‐ Drop out rate acceptable? | High risk | Not described, no n's in tables |
| Incomplete outcome data (attrition bias) All outcomes ‐ Analyzed in the group to which they were allocated? | Unclear risk | Not reported |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics | Low risk | Reported to be similar |
| Co‐interventions avoided or similar? | Unclear risk | Followed medication use only |
| Compliance acceptable? | Unclear risk | Not reported |
| Similar timing of outcome assessment? | Low risk | All assessed immediately post treatment and at 6 months |
| Fatal Flaw | High risk | Unclear randomisation, allocation concealment; drops‐outs not described; unclear whether ITT done |
| Methods | RCT Number analysed/randomised: 177/177 Intention‐to‐treat: reported Power analysis: NR Funding source: German Ministry for Education and Research. Manuscript preparation supported by German Medical Acupuncture Association | |
| Participants | Chronic mechanical neck disorder Participant recruitment: outpatient departments at the University of Munich |
|
| Interventions | INDEX TREATMENT Acupuncture TCM plus ear acupuncture and dry needling of myofascial points. Local points ‐ UB10, active myofascial trigger points were located predominantly in the trapezius (nearby GB20) and levator scapulae (nearby SI14). Distal points ‐ SI3, UB60, Liv3, GB34, TW5, ear point (cervical spine) COMPARISON TREATMENT Sham laser acupuncture (control) Laser pen inactivated ‐ each point treated for 2 minutes CO‐INTERVENTION Not reported Treatment schedule: 5 sessions over 3 weeks, each session 30 minutes in duration Duration of follow‐up: 12 weeks |
|
| Outcomes | PAIN INTENSITY (VAS 100‐point scale) for motion‐related pain Baseline mean: acupuncture 54.15, sham laser acupuncture 57.15 End of study mean: acupuncture 28.27, sham laser acupuncture 40.82 Absolute benefit: acupuncture 25.88, sham laser acupuncture 16.33 Reported results: no significant differences between groups SMD ‐0.25 (95% CI random ‐0.62 to 0.13) at 1 week SMD ‐0.00 (95% CI random ‐0.38 to 0.38) at 3 months PAIN PRESSURE THRESHOLD (PPT kg/cm2) Baseline mean: acupuncture 1.07, sham laser acupuncture 1.05 End of study mean: acupuncture 0.19, sham laser acupuncture 0.03 Absolute benefit: acupuncture 0.88, sham laser acupuncture 1.02 Reported results: no significant differences between groups SMD 0.16 (95% CI random ‐0.21 to 0.54) immediate post treatment SMD 0.23 (95% CI random ‐0.15 to 0.61) at 3 months Reasons for drop‐out: withdrew, refused treatment, accident, diagnosed with other medical condition, lost to follow‐up Adverse effects: For acupuncture, complaints of slight pain and low blood pressure. For sham laser acupuncture, complaints of slight pain, low blood pressure and sweating Costs of care: NR |
|
| Notes | ‐‐ | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Block randomisation stratified for 2 centres |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes ‐ patient? | High risk | Interventions perceivably different |
| Blinding (performance bias and detection bias) All outcomes ‐ care provider? | High risk | Not possible |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessor? | High risk | Participant not blinded, then participant as outcome assessor would not be blinded either |
| Incomplete outcome data (attrition bias) All outcomes ‐ Drop out rate acceptable? | Low risk | Described and adequate |
| Incomplete outcome data (attrition bias) All outcomes ‐ Analyzed in the group to which they were allocated? | Low risk | Reported in text |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics | Low risk | Reported to be similar |
| Co‐interventions avoided or similar? | Unclear risk | Not reported |
| Compliance acceptable? | Unclear risk | Not reported |
| Similar timing of outcome assessment? | Low risk | Assessed immediate post treatment, 3 days after first treatment, 1 week and 3 months |
| Fatal Flaw | Low risk | Acceptable |
| Methods | RCT, cross‐over Number analysed/randomised: 34/36 Intention‐to‐treat: NA Power analysis: NR Funding source: German Ministry for Education and Research | |
| Participants | Chronic neck disorder without radicular symptoms Participant recruitment: out‐patients from the Department of Physical Medicine and Rehabilitation and the Interdisciplinary Pain Unit at the University of Munich |
|
| Interventions | INDEX TREATMENT 1 Non‐local needle acupuncture (NLA) at distant points according to the theory of channels of TCM and varied individually by therapist INDEX TREATMENT 2 Dry needling (dn) of local myofascial trigger points with strong manual stimulation of 'ah shi' points COMPARISON TREATMENT Sham laser acupuncture (SHAM) CO‐INTERVENTION Not reported Treatment schedule: each participant treated once with all interventions with a 1‐week wash‐out period and each session averaging 30 minutes in duration Duration of follow‐up: immediately following completion of each treatment |
|
| Outcomes | PAIN INTENSITY (VAS 100 mm scale) for motion‐related pain Baseline mean: acupuncture (NLA) 35.0, (dn) 33.4, sham laser acupuncture 30.4 End of study mean: acupuncture (NLA) 19.1, (dn) 29.2, sham laser acupuncture 28.0 Absolute benefit: acupuncture (NLA) 15.9, (dn) 4.2, sham laser acupuncture 2.4 Reported results: NLA effective, dn not effective when compared with the sham SMD 0.49 (95% CI random ‐0.98 to ‐0.01) NLA group immediate post treatment SMD 0.06 (95% CI random ‐0.42 to 0.54) dn group immediate post treatment Reasons for drop‐out: NA Adverse effects: no serious adverse effects; however, 3 participants had mild hypotonia and sweating (1 from NLA and 2 from dn groups) Costs of care: NR |
|
| Notes | ‐‐ | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Cross‐over design, 6 possible sequences assigned to a number from 1 to 6, random list for 36 participants was then prepared by rolling dice |
| Allocation concealment (selection bias) | Low risk | Fully concealed |
| Blinding (performance bias and detection bias) All outcomes ‐ patient? | Low risk | Participant reported as blinded |
| Blinding (performance bias and detection bias) All outcomes ‐ care provider? | High risk | Not possible for acupuncture group, only sham laser acupuncture had caregiver blinded |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessor? | Low risk | Participant blinded as outcome assessor |
| Incomplete outcome data (attrition bias) All outcomes ‐ Drop out rate acceptable? | Low risk | Reported and acceptable |
| Incomplete outcome data (attrition bias) All outcomes ‐ Analyzed in the group to which they were allocated? | High risk | Not all randomised participants were analysed |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics | Low risk | Reported to be similar |
| Co‐interventions avoided or similar? | Unclear risk | Not reported |
| Compliance acceptable? | Low risk | Each participant received 1 treatment with each intervention with 1‐week wash‐out period between |
| Similar timing of outcome assessment? | Low risk | Assessed immediate post treatment |
| Fatal Flaw | Low risk | Acceptable |
| Methods | RCT Number analysed/randomised: 31/40 Intention‐to‐treat: not calculated Power analysis: not calculated Location: Japan Funding source: Japan Society of Acupuncture and Moxibustion |
|
| Participants | Chronic neck pain, no radicular signs Participant recruitment: Participants were recruited from the Meiji University of Oriental Medicine Hospital |
|
| Interventions | INDEX TREATMENT 1 Standard acupuncture (SA) Acupuncture points local: GB20, GB21, BL10, BL11, SI12, SI13; distal TE5, LI4, SI3 Inserted needles into the muscle (depth of 20 mm) using 'sparrow pecking' technique; manipulation stopped when participants reached Deqi, and needles were left in place for an additional 10 minutes INDEX TREATMENT 2 Trigger point acupuncture (TrP) Local needling of myofascial trigger points (mean number of insertions 2.3) Needles were inserted 20 mm into the skin over the trigger point by the 'sparrow pecking' technique. Manipulation was stopped when the local twitch response was elicited, and the needle was left in place for an additional 10 minutes INDEX TREATMENT 3: Non‐trigger point acupuncture (non‐TrP) Non‐TrP group received the same treatment as above but at non‐tender points (mean number of insertions 2.4). The non‐tender point chosen had no tenderness nor taut muscle band. However, the point was selected in the same muscle but away from the trigger point by 50 mm COMPARISON TREATMENT Sham acupuncture (SH) SH groups received treatment at trigger points. Similar stainless steel needles were used, but the tips had been cut off and smoothed to prevent penetration of the skin by the needle with the 'sparrow pecking' technique. Simulation of needle extraction was performed after 10 minutes (mean number of insertions 2.6) CO‐INTERVENTION Not specified Treatment schedule: 6 treatments within 10 weeks; applied in 2 phases of 3 treatments: 3 treatments within first 3 weeks, no treatment from week 4 to 7 and 3 treatments from week 7 to 10 Duration of follow‐up: 3 weeks |
|
| Outcomes | Groups PAIN INTENSITY (VAS 0 to 100 mm) Baseline mean: SA 69.5, TrP 67.0, non‐TrP 70.9, SH 64.1 End of study mean: SA 51.6, TrP 11.0, non‐TrP 57.6, SH 53.9 Absolute benefit: SA 17.9, TrP 56.0, non‐TrP 13.3, SH 10.2 Reported results: statistically significant improvement in the TrP group only SA vs SH: SMD ‐0.24 (95% CI random ‐1.26 to 0.78) immediate post treatment SA vs SH: SMD ‐0.10 (95% CI random ‐1.11 to 0.92) at 3 weeks TrP vs SH: SMD ‐2.77 (95% CI random ‐4.31 to ‐1.24) immediate post treatment TrP vs SH: SMD ‐2.37 (95% CI random ‐3.78 to ‐0.95) at 3 weeks Non‐TrP vs SH: SMD 0.23 (95% CI random ‐0.79 to 1.25) immediate post treatment Non‐TrP vs SH: SMD ‐0.01 (95% CI random ‐1.03 to 1.00) at 3 weeks DISABILITY: NECK DISABILITY INDEX (NDI 0 to 50 point scale) Baseline mean: SA 12.6, TrP 13.0, non‐TrP 15.1, SH 12.0 End of study mean: SA 10.9, TrP 3.1, non‐TrP 12.0, SH 11.1 Absolute benefit: SA 1.7, TrP 9.9, non‐TrP 3.1, SH 0.9 Reported results: TrP group demonstrated greatest improvement SA vs SH: SMD ‐0.19 (95% CI random ‐1.21 to 0.83) immediate post treatment SA vs SH: SMD ‐0.03 (95% CI random ‐1.05 to 0.98) at 3 weeks TrP vs SH: SMD ‐2.81 (95% CI random ‐4.36 to ‐1.26) immediate post treatment TPA vs SH: SMD ‐1.82 (95% CI random ‐3.09 to ‐0.56) at 3 weeks Non‐TrP vs SH: SMD 0.38 (95% CI random ‐0.65 to 1.41) immediate post treatment Non‐TrP vs SH: SMD 0.18 (95% CI random ‐0.84 to 1.20) at 3 weeks Drop‐outs due to no response to treatment: SA 1, TPA 1, NTPA 1, SH 1 Drop‐outs due to adverse effects: deterioration of symptoms, not specified SA 1, TPA 1, NTPA 0, SH 1 Costs of care: NR |
|
| Notes | ‐‐ | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomisation |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes ‐ patient? | High risk | Participants not adequately blinded |
| Blinding (performance bias and detection bias) All outcomes ‐ care provider? | High risk | Not possible |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessor? | High risk | Participant as outcome assessor not blinded adequately |
| Incomplete outcome data (attrition bias) All outcomes ‐ Drop out rate acceptable? | High risk | Discrepancy between Table 2, Figure 3 and text |
| Incomplete outcome data (attrition bias) All outcomes ‐ Analyzed in the group to which they were allocated? | High risk | n's in Figure 3 do not add up |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics | Unclear risk | Table 2 gives only baseline info on those who completed the trial, not those randomised |
| Co‐interventions avoided or similar? | Unclear risk | Not reported |
| Compliance acceptable? | Unclear risk | Not reported |
| Similar timing of outcome assessment? | Low risk | Assessed immediately post treatment |
| Fatal Flaw | High risk | Numbers in flow charts and tables do not add up |
| Methods | RCT Number analysed/randomised: 40/40 Intention‐to‐treat: reported Power analysis: NR Funding source: University of Tsukuba, Japan |
|
| Participants | WAD symptoms 3 months or longer Participant recruitment: through advertisements in local newspapers and on the homepage of the Kyung Hee Medical Center |
|
| Interventions | INDEX TREATMENT Acupuncture Acupuncture points from the gallbladder (GB), small intestine (SI), bladder (BL), triple energiser (TE) and large intestine (LI) meridian systems located on shoulder, neck, head and upper limbs. Needles (length 40 mm; diameter 0.16 mm, SEIRIN Co. Ltd) were inserted perpendicularly to a depth of 1.0 to 2.0 cm in place for 15 minutes COMPARISON Wait‐list CO‐INTERVENTION Both groups maintained their usual care, including physiotherapy, exercise and sufficient rest Treatment schedule: Treatment consisted of 6 sessions, 3×/wk for 2 weeks No follow‐up |
|
| Outcomes | PAIN INTENSITY (0 to 10 VAS scale) Baseline mean: acupuncture 4.59, wait‐list 4.88 End of study mean: acupuncture 2.74, wait‐list 4.47 immediate post treatment Absolute benefit: acupuncture 1.85, wait‐list 0.41 Reported results: statistically significant favouring acupuncture Drop‐outs: none Adverse effects: 3 acupuncture participants reported mild adverse events (2 with bruising, 1 with fatigue) No serious side effects reported Costs of care: NR |
|
| Notes | Unable to reach study author to obtain necessary data for abstraction | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computerised number table generated random sequences |
| Allocation concealment (selection bias) | Unclear risk | Envelopes sealed but not sequentially numbered (numbers inside) |
| Blinding (performance bias and detection bias) All outcomes ‐ patient? | High risk | Not possible because of design |
| Blinding (performance bias and detection bias) All outcomes ‐ care provider? | High risk | Not possible because of design |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessor? | Unclear risk | Participant was the outcome assessor with self reports |
| Incomplete outcome data (attrition bias) All outcomes ‐ Drop out rate acceptable? | Low risk | No drop‐outs |
| Incomplete outcome data (attrition bias) All outcomes ‐ Analyzed in the group to which they were allocated? | Low risk | Acceptable |
| Selective reporting (reporting bias) | Low risk | See registration |
| Similarity of baseline characteristics | Low risk | Reported as similar in Tables 2, 3, 5 |
| Co‐interventions avoided or similar? | Unclear risk | Not reported |
| Compliance acceptable? | Unclear risk | Not reported |
| Similar timing of outcome assessment? | Low risk | Baseline and 2 weeks |
| Fatal Flaw | High risk | Flawed; wrong analysis was used; Figure 2 should use independent t‐test, not paired t‐test |
| Methods | RCT Number analysed/randomised: 53/54 Intention‐to‐treat: NA Power analysis: NR Funding source: NR |
|
| Participants | Chronic neck disorder associated with degenerative changes ‐ cervical spondylosis Participant recruitment: Guangdong Provincial Hospital of TCM |
|
| Interventions | INDEX TREATMENT Routine acupuncture Treated with routine acupuncture at GV 14, Ex‐HN 15 and SI 15 with 40 mm long needles (diameter of 0.30 mm). Needles were retained for 20 minutes after Deqi was achieved COMPARISON TREATMENT Sham acupuncture Sham acupuncture. Needled at 1 cm lateral to Ex‐HN 15 and SI 15 (needles were 40 mm long with a diameter of 0.22 mm). Needles were retained for 20 minutes CO‐INTERVENTION Infrared radiation as adjuvant treatment, comparable between index and control groups Treatment schedule: Treatment consisted of 9 sessions, applied 3 times a week (every other day) over a period of 3 weeks No follow‐up |
|
| Outcomes | QUALITY OF LIFE: Northwick Park Neck Pain Questionnaire (up to 100, low score = better) Baseline mean: routine acupuncture 35.32, sham acupuncture 31.96 End of study mean: routine acupuncture 19.16, sham acupuncture 23.76 Absolute benefit: routine acupuncture 16.16, sham acupuncture 8.2 Reported results: Both groups showed improvement SMD ‐0.39 (95% CI random ‐0.77 to ‐0.00) immediate post treatment Adverse effects: NR Costs of care: NR |
|
| Notes | ‐‐ | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding (performance bias and detection bias) All outcomes ‐ patient? | Unclear risk | Not described |
| Blinding (performance bias and detection bias) All outcomes ‐ care provider? | Unclear risk | Not described |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessor? | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes ‐ Drop out rate acceptable? | Low risk | No drop‐outs |
| Incomplete outcome data (attrition bias) All outcomes ‐ Analyzed in the group to which they were allocated? | Low risk | As described |
| Selective reporting (reporting bias) | Low risk | None reported |
| Similarity of baseline characteristics | Unclear risk | Not described |
| Co‐interventions avoided or similar? | Unclear risk | Not described |
| Compliance acceptable? | Unclear risk | Not described |
| Similar timing of outcome assessment? | Low risk | Similar at baseline and 3 weeks |
| Fatal Flaw | High risk | Reporting flaws |
| Methods | RCT, pilot Number analysed/randomised: 178/190 Intention‐to‐treat: Not all randomised participants were analysed Power analysis: calculated 90% Funding source: NR | |
| Participants | Chronic mechanical neck disorder Participant recruitment: outpatient clinic of Guangdong Provincial Hospital of Chinese Medicine in Guangzhou, China |
|
| Interventions | INDEX TREATMENT Acupuncture group Acupuncture points ‐ Du14, SI15 and Ex‐HN15 bilaterally manually stimulated on insertion for Deqi. Needles were inserted into the muscle (to a depth of 20 mm), left in place for 20 minutes. During treatment, participants received infrared irradiation on the cervical region COMPARISON TREATMENT Sham Participants in the control group received placebo acupuncture on the sham points, which were 1 cm lateral to the standard acupuncture points selected in the study group. Needles were inserted into the skin to a depth of approximately 3 mm and remained in the subcutaneous tissues with no manual stimulation. During treatment, participants in the control group also received infrared irradiation on the cervical region CO‐INTERVENTION NR Treatment schedule: 3 weeks, total 9 sessions, with each session averaging 20 minutes in duration Duration of follow‐up: immediate post, 4 weeks, 3 months |
|
| Outcomes | PAIN INTENSITY (VAS 10 cm scale) Baseline mean: acupuncture 5.30, sham 5.49 End of study mean: acupuncture 2.88, sham 3.19 Absolute benefit: acupuncture 2.48, sham 2.3 Reported results: significant favouring acupuncture SMD ‐0.30 (95% CI random ‐0.59 to ‐0.00) immediate post treatment SMD ‐0.40 (95% CI random ‐0.69 to ‐0.10) at 4 weeks SMD ‐0.20 (95% CI random ‐0.50 to 0.09) at 3 months NECK DISABILITY: NPQ Baseline mean: acupuncture 32.73, sham 33.04 End of study mean: acupuncture 19.09, sham 23.53 Absolute benefit: acupuncture 13/64, sham 9.51 Reported results: significant favouring acupuncture SMD ‐0.28 (95% CI random ‐0.57 to 0.02) immediate post treatment SMD ‐0.37 (95% CI random ‐0.67 to ‐0.07) at 4 weeks SMD ‐0.37 (95% CI random ‐0.67 to ‐0.07) at 3 months QUALITY OF LIFE: SF‐36 (Physical Component ‐ higher = better) Baseline mean: acupuncture 80.79, sham 79.22 End of study mean: acupuncture 84.26, sham 85.88 Absolute benefit: 3.47, sham 6.66 Reported results: no significant differences between groups SMD 0.38 (95% CI random 0.08 to 0.68) immediate post treatment SMD ‐0.05 (95% CI random ‐0.35 to 0.24) at 4 weeks SMD ‐0.11 (95% CI random ‐0.40 to 0.18) at 3 months Reasons for drop‐out: 5 drop‐outs in treatment group: 3 due to fear of pain and 2 for inconvenience. 7 drop‐outs in sham group: 4 due to fear of pain and 3 due to inconvenience Adverse effects: local bleeding, fainting: 3 participants in treatment and 4 in control; local numbness, aching or bleeding at points: 4 participants in treatment and 2 in control. All adverse events transient and resolved, although those who fainted decided to withdraw from the study Costs of care: NR |
|
| Notes | ‐‐ | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random numbers were generated by computer software |
| Allocation concealment (selection bias) | Low risk | Sealed opaque envelopes |
| Blinding (performance bias and detection bias) All outcomes ‐ patient? | Low risk | Reported as blinded |
| Blinding (performance bias and detection bias) All outcomes ‐ care provider? | High risk | Not possible |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessor? | Low risk | Participant blinded as outcome assessor |
| Incomplete outcome data (attrition bias) All outcomes ‐ Drop out rate acceptable? | Low risk | Reported in text and acceptable |
| Incomplete outcome data (attrition bias) All outcomes ‐ Analyzed in the group to which they were allocated? | High risk | Not all randomised participants were analysed |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics | Low risk | Reported to be similar |
| Co‐interventions avoided or similar? | Unclear risk | Not reported |
| Compliance acceptable? | Unclear risk | Not reported |
| Similar timing of outcome assessment? | Low risk | Assessed immediate post treatment, 4 weeks, 3 months |
| Fatal Flaw | Low risk | Acceptable |
| Methods | RCT Number analysed/randomised: 34/34 Intention‐to‐treat: calculated Power analysis: NR Funding source: NR | |
| Participants | Chronic neck pain, no radicular signs Participant recruitment: students from an acupuncture school in Japan |
|
| Interventions | Treatment was provided to 'tender points' on the posterior aspect of the neck and upper back "All tender points were carefully detected where the subjects felt dull pain and stiffness (neck, shoulder, and back) and were used for the acupuncture treatment. All tender points were treated in each group” INDEX TREATMENT 'Sparrow pecking' acupuncture Disposable stainless needles (0.2 mm × 40 mm) were inserted into the muscle to a depth of about 20 mm, and the ‘sparrow pecking’ technique was applied. When the participant felt Deqi, the manipulation was stopped and the needle was retained for 5 more minutes COMPARISON TREATMENT Simulated 'sparrow pecking' acupuncture with no needle insertion For sham acupuncture, similar stainless needles (0.2 mm × 40 mm) were used, but the tips had previously been cut off to prevent the needle from penetrating the skin. The cut ends were smoothed with sandpaper manually under clean conditions. The acupuncturist pretended to insert the needle and to use the sparrow pecking technique, then removed the needles. Simulation of needle extraction was performed after 5 minutes CO‐INTERVENTION Not specified Duration of treatment: once/wk for 3 weeks Duration of follow‐up: 9 days |
|
| Outcomes | PAIN INTENSITY: VAS Baseline mean: acupuncture 60.5, sham 48.8 End of study mean: acupuncture 43.3, sham 46.8 Absolute benefit: acupuncture 17.2, sham 2.0 Reported results: significant favouring acupuncture SMD ‐0.15 (95% CI random ‐0.82 to 0.52) at 9 days Reasons for drop‐out: NR Adverse effects: none Costs of care: NR |
|
| Notes | ‐‐ | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computerised randomisation programme |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes ‐ patient? | Low risk | Reported as blinded |
| Blinding (performance bias and detection bias) All outcomes ‐ care provider? | High risk | Not possible |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessor? | Low risk | Participant as outcome assessor was blinded |
| Incomplete outcome data (attrition bias) All outcomes ‐ Drop out rate acceptable? | Low risk | No drop‐outs |
| Incomplete outcome data (attrition bias) All outcomes ‐ Analyzed in the group to which they were allocated? | Low risk | No drop‐outs |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics | Low risk | Reported to be similar but baseline VAS different by 11.7 |
| Co‐interventions avoided or similar? | Unclear risk | Not reported |
| Compliance acceptable? | High risk | Some participants did not receive all treatment |
| Similar timing of outcome assessment? | Low risk | 9 days |
| Fatal Flaw | Low risk | Acceptable |
| Methods | RCT Number analysed/randomised: 13/13 Intention‐to‐treat: NR Power analysis: NR Funding source: NR | |
| Participants | Chronic mechanical neck disorder with radicular signs or symptoms Participant recruitment: out‐patients from Addenbrooke's Hospital, Cambridge, UK |
|
| Interventions | INDEX TREATMENT Acupuncture group 5 standard points used ‐ Du14, GB20 bilateral, GB21 bilateral; 28 g needle used to achieve sensation of Teh Chi (Deqi); needles manipulated after insertion and on removal COMPARISON Placebo TNS group Sham electrical stimulation with lead electrode applied to each side of the neck, 5 cm lateral to C7 CO‐INTERVENTION Comparable between index and control groups Treatment schedule: 4 weeks (2 times/wk), with each session averaging 20 minutes Duration of follow‐up: none |
|
| Outcomes | PAIN INTENSITY: pain relief score (5 point scale) Baseline mean: NR End of study mean: NR Reported results: significant improvement favouring acupuncture Reasons for drop‐out: NA Adverse effects: NR Costs of care: NR |
|
| Notes | ‐‐ | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Reported only as randomly assigned |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes ‐ patient? | High risk | Interventions perceivably different |
| Blinding (performance bias and detection bias) All outcomes ‐ care provider? | High risk | Not possible |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessor? | High risk | Participant as outcome assessor not blinded |
| Incomplete outcome data (attrition bias) All outcomes ‐ Drop out rate acceptable? | Low risk | No drop‐outs |
| Incomplete outcome data (attrition bias) All outcomes ‐ Analyzed in the group to which they were allocated? | Low risk | All randomised participants analysed |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics | Low risk | Appears similar |
| Co‐interventions avoided or similar? | Unclear risk | Not reported |
| Compliance acceptable? | Low risk | All participants treated twice weekly for 4 weeks |
| Similar timing of outcome assessment? | Low risk | Assessed immediately post treatment |
| Fatal Flaw | High risk | Randomisation and allocation concealment details not reported |
| Methods | RCT Number analysed/randomised: 25/26 Intention‐to‐treat: NR Power analysis: reported Funding source: NR | |
| Participants | Chronic mechanical neck disorder Participant recruitment: hospitalised patients from Queen Elizabeth Hospital, Palmersion North, New Zealand |
|
| Interventions | INDEX TREATMENT Acupuncture group 5 predetermined acupuncture points ‐ Du14, GB20 and GB21 bilaterally manually stimulated on insertion to Teh Chi (Deqi) and at 5‐minute intervals COMPARISON TREATMENT Sham TNS TNS electrodes placed at the base of the neck connected to an oscilloscope display without a currentExaminer re‐entered the room at 5 minute intervals to check display CO‐INTERVENTION Analgesics comparable between groups Treatment schedule: 2 sessions/wk for 4 weeks, with each session averaging 20 minutes in duration Duration of follow‐up: 4 weeks |
|
| Outcomes | PAIN INTENSITY (4 item VAS scale) Baseline mean: acupuncture 47.08, sham TNS 31.67 End of study mean: acupuncture 31.77, sham TNS 24.72 Absolute benefit: acupuncture 15.31, sham TNS 6.95 Reported results: no significant differences between groups SMD ‐0.17 (95% CI random ‐0.62 to 0.96) immediate post treatment SMD ‐0.30 (95% CI random ‐1.09 to 0.49) at 4 weeks Reasons for drop‐out: unrelated surgery, loss to follow‐up Adverse effects: NR Costs of care: NR | |
| Notes | ‐‐ | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not adequately described |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes ‐ patient? | High risk | Interventions perceivably different |
| Blinding (performance bias and detection bias) All outcomes ‐ care provider? | High risk | Not possible |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessor? | High risk | Participant as outcome assessor not blinded |
| Incomplete outcome data (attrition bias) All outcomes ‐ Drop out rate acceptable? | Low risk | Drop‐outs described and acceptable |
| Incomplete outcome data (attrition bias) All outcomes ‐ Analyzed in the group to which they were allocated? | High risk | All randomised participants were not analysed |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics | High risk | Acupuncture group had more daily use of NSAIDs and pain scores with statistically significant differences |
| Co‐interventions avoided or similar? | High risk | Not reported |
| Compliance acceptable? | High risk | Not all participants received the scheduled 8 treatments |
| Similar timing of outcome assessment? | Low risk | Assessed immediate post treatment |
| Fatal Flaw | High risk | Due to inadequate reporting |
| Methods | RCT Number analysed/randomised: 29/31 Intention‐to‐treat: NR Power analysis: NR Funding source: NR | |
| Participants | Chronic myofascial neck pain Participant recruitment: patients recruited from the clinic of the Department of Physical Medicine and Rehabilitation in Turkey |
|
| Interventions | INDEX TREATMENT Electroacupuncture group (EAP) 7 acupuncture points ‐ Du14 and GB20, GB21, LI4, UB10, UB60, TE5 all bilaterally and manually stimulated on insertion to Teh Chi (Deqi), EAP added after 1 to 4 Hz, 200 µs COMPARISON TREATMENT Sham EAP Same points as the treatment group; needles inserted 1 to 2 cm away from the meridian points. No Deqi. EAP stimulated, then turned off CO‐INTERVENTION NR Treatment schedule: 10 sessions over 3 weeks, with each session averaging 30 minutes in duration Duration of follow‐up: immediate post treatment, 3 months |
|
| Outcomes | PAIN INTENSITY (10 point VAS (movement) scale) Baseline mean: EAP 7.38, sham EAP 6.19 End of study mean: EAP 4.50, sham EAP 4.50 Absolute benefit: EAP 2.88, sham EAP 1.69 Reported results: not significant, including pain at rest SMD ‐0.56 (95% CI random ‐1.31 to 0.19) immediate post treatment SMD 0.00 (95% CI random ‐0.73 to 0.73) at 3 months Reasons for drop‐out: 2 participants in the EAP group: 1 unable to obtain permission from work to attend; 1 planning a pregnancy Adverse effects: NR Costs of care: NR |
|
| Notes | ‐‐ | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Not described |
| Allocation concealment (selection bias) | High risk | Names sealed in opaque envelopes. Envelopes were then allocated randomly into 2 groups. After the doctor examined participants, she gave the names of those who were included in the study to someone else, who prepared the envelopes |
| Blinding (performance bias and detection bias) All outcomes ‐ patient? | Low risk | Reported as blinded |
| Blinding (performance bias and detection bias) All outcomes ‐ care provider? | High risk | Not possible |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessor? | Low risk | Participant blinded as outcome assessor |
| Incomplete outcome data (attrition bias) All outcomes ‐ Drop out rate acceptable? | Low risk | Described and acceptable |
| Incomplete outcome data (attrition bias) All outcomes ‐ Analyzed in the group to which they were allocated? | High risk | All randomised participants not analysed |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics | High risk | VAS pain scores > 10% difference |
| Co‐interventions avoided or similar? | Unclear risk | Not reported |
| Compliance acceptable? | Unclear risk | Not reported |
| Similar timing of outcome assessment? | Low risk | Assessed immediate post treatment and 3 months |
| Fatal Flaw | High risk | Randomisation not performed properly; planned to recruit 80 participants but enrolled only 31 |
| Methods | RCT Number Analysed/randomised: 48/51 Intention‐to‐treat: NR Power analysis: NR Funding source: NR | |
| Participants | Chronic mechanical neck disorder: cervical tendomyosis Participant recruitment: NR |
|
| Interventions | INDEX TREATMENT Conventional meridian acupuncture (Acu) 15 minutes per session; maximum 15 needles per session. Option of 15 acupuncture points was available. Seirin needles 7, 0.3 × 30 mm and 0.2 × 15 mm. Insertion until the Deqi response was achieved COMPARISON TREATMENT Placebo LASER (LLLT0) Outcome power: 0 mV, Meridian acupuncture points same as acupuncture group CO‐INTERVENTION Avoided in trial design Treatment schedule: 4 weeks, 2 sessions per week ‐ total 8 sessions Duration of follow‐up: 4 weeks |
|
| Outcomes | PAIN INTENSITY: VAS (mm) Baseline mean: Acu 39.3, LLLT0 34.1 End of study mean: Acu 7.0, LLLT0 25.2 Absolute benefit: Acu 32.3, LLLT0 8.9 SMD ‐0.86 (95% CI random ‐1.70 to ‐0.02) at immediate post SMD ‐0.46 (95% CI random ‐1.27 to 0.35) at 4 week follow‐up Reported results: statistically significant favouring acupuncture immediate post treatment and at 4 week follow‐up TENDERNESS (pressure pain threshold ‐ PPT) Baseline mean: Acu 4.13, LLLT0 5.05 End of study mean: Acu 5.75, LLLT0 6.12 Absolute benefit: Acu 1.62, LLLT0 1.07 Reported results: not significant SMD ‐0.14 (95% CI random ‐0.95 to 0.66) at immediate post SMD ‐0.22 (95% CI random ‐1.02 to 0.58) at 4 week follow‐up Reasons for drop‐out: NR Adverse effects: reported for control and for index treatment; not specified Costs of care: NR |
|
| Notes | ‐‐ | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Reported randomised double‐blinded |
| Allocation concealment (selection bias) | Unclear risk | Possibly adequate |
| Blinding (performance bias and detection bias) All outcomes ‐ patient? | Low risk | Reported as blinded |
| Blinding (performance bias and detection bias) All outcomes ‐ care provider? | High risk | Not possible |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessor? | Low risk | Paticipant blinded as outcome assessor |
| Incomplete outcome data (attrition bias) All outcomes ‐ Drop out rate acceptable? | Low risk | Reported and acceptable |
| Incomplete outcome data (attrition bias) All outcomes ‐ Analyzed in the group to which they were allocated? | High risk | Not all randomised participants were analysed |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics | Low risk | Reported to be similar |
| Co‐interventions avoided or similar? | Low risk | Avoided |
| Compliance acceptable? | High risk | Not acceptable |
| Similar timing of outcome assessment? | Low risk | Assessed at 4 weeks |
| Fatal Flaw | Low risk | Acceptable |
| Methods | RCT Number analysed/randomised: 34/35 Intention‐to‐treat: calculated Power analysis: calculated 90% Funding source: NR | |
| Participants | Myofascial neck pain syndrome (MPS) Participant recruitment: Department of Neurology at Nantou Hospital, Department of Health |
|
| Interventions | INDEX TREATMENT Acupuncture group 5 predetermined acupuncture points ‐ TE14, GB20, SI3 bilaterally manually stimulated on insertion to Qi COMPARISON TREATMENT Sham acupuncture Same points as treatment group. Inserted into subcutaneous tissue at 2 mm depth. No manual stimulation CO‐INTERVENTION NR Treatment schedule: 2 sessions/wk for 3 consecutive weeks, with each session averaging 20 minutes in duration Duration of follow‐up: immediate post, 4 weeks, 12 weeks |
|
| Outcomes | PAIN INTENSITY (100 point VAS (movement) scale) Baseline mean: acupuncture 50, sham acupuncture 50 End of study mean: acupuncture 30, sham acupuncture 30 Absolute benefit: acupuncture 20, sham acupuncture 20 Reported results: no significance differences between groups SMD ‐0.42 (95% CI random ‐1.10 to 0.26) immediate post treatment SMD ‐0.54 (95% CI random ‐1.22 to 0.15) at 4 weeks SMD 0.00 (95% CI random ‐0.67 to 0.67) at 12 weeks Reasons for drop‐out: discontinued because of Chinese herb use Adverse effects: 1 participant in treatment group experienced ecchymosis, 1 in control group experienced slight dizziness; both were transient and resolved Costs of care: NR |
|
| Notes | ‐‐ | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not clear if adequately done |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes ‐ patient? | Unclear risk | Some participant were not naive to acupuncture |
| Blinding (performance bias and detection bias) All outcomes ‐ care provider? | High risk | Not possible |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessor? | Unclear risk | Unclear whether participant was blinded and was also the outcome assessor |
| Incomplete outcome data (attrition bias) All outcomes ‐ Drop out rate acceptable? | Low risk | Reported and acceptable |
| Incomplete outcome data (attrition bias) All outcomes ‐ Analyzed in the group to which they were allocated? | Unclear risk | Appears 1 randomised participant may not have been analysed |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics | Low risk | Reported to be similar |
| Co‐interventions avoided or similar? | Unclear risk | Not reported |
| Compliance acceptable? | Unclear risk | Not specifically and clearly reported |
| Similar timing of outcome assessment? | Low risk | Assessed after 6 treatments, 4 weeks, 12 weeks |
| Fatal Flaw | High risk | Randomisation not clearly done properly; participants do not appear to have been blinded; ITT not done; missing data handled by last observation carried forward; all P values in Table 2 within‐group changes; scores in Table 3 do not look credible |
| Methods | RCT cross‐over Number analysed/randomised: 132/132 Power analysis: Post hoc analysis suggested 70 participants per group were needed Intention‐to‐treat analysis: NA Funding source: NR |
|
| Participants | Chronic mechanical neck disorder, cervical osteoarthritis Participant recruitment: Sweden |
|
| Interventions | INDEX TREATMENT Acupuncture (Acu): LI3 and GB20 bilaterally, DU14, DU16, DU20 with manual stimulation for 10s for Deqi every 5 minutes, 40 minute session COMPARISON TREATMENT Sham acupuncture: needles inserted superficially, not manually stimulated CO‐INTERVENTION Instructed to take no pain medication 24 hours before trials Duration of treatment: 1 session Duration of follow‐up: 2 hours |
|
| Outcomes | PAIN INTENSITY (VAS 0 to 10) Baseline: acupuncture 2.5, placebo acupuncture 2.0, placebo diazepam 1.9 End of study mean: acupuncture 1.8, placebo 1.6, placebo diazepam 1.7 Absolute benefit: acupuncture 0.7, placebo 0.4, placebo diazepam 0.2 Reported results: not significant when acupuncture was compared with placebo acupuncture but statistically significant when acupuncture was compared with placebo diazepam vs placebo acupuncture: SMD 0.17 (95% CI random ‐0.25 to 0.59) immediate post treatment vs placebo diazepam: SMD 0.09 (95% CI random ‐0.33 to 0.51) immediate post treatment Adverse effects: NR Costs of care: NR |
|
| Notes | ‐‐ | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Only described as randomised to order |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes ‐ patient? | High risk | Interventions perceivably different |
| Blinding (performance bias and detection bias) All outcomes ‐ care provider? | High risk | Not possible |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessor? | High risk | Participant not blinded as outcome assessor |
| Incomplete outcome data (attrition bias) All outcomes ‐ Drop out rate acceptable? | Low risk | No drop‐outs |
| Incomplete outcome data (attrition bias) All outcomes ‐ Analyzed in the group to which they were allocated? | Low risk | All randomised participants were analysed |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics | Low risk | Each participant received all treatments |
| Co‐interventions avoided or similar? | Low risk | Avoided |
| Compliance acceptable? | Low risk | All participants received all treatments |
| Similar timing of outcome assessment? | Low risk | Immediate post treatment |
| Fatal Flaw | High risk | Improper error terms for analysis (SD should not be used for within‐patient analysis); randomisation and concealment not described; no adjustments made for order; balancing not apparent |
| Methods | RCT pilot/feasibility study Number analysed/randomised: 34/41 Intention‐to‐treat: calculated but not reported Power analysis: reported Funding source: NR |
|
| Participants | WAD myofascial pain (injury of 2 to 16 week duration) Participant recruitment: Derriford Hospital Physiotherapy Department, UK |
|
| Interventions | INDEX TREATMENT Acupuncture group Trigger point needling using 0.25 mm × 30 to 40 mm length, 6 to 7 sparrow pecking into each MTrP (muscles treated not described) COMPARISON Sham acupuncture Same procedure as treatment group; however, a sham needle 0.30 mm × 50 mm cut, and blunted end was tapped against the skin, with sparrow pecking motion CO‐INTERVENTION Participant education, heat, analgesics and exercise (home therapy) Treatment schedule: 1 session/wk, total 2 to 6 treatments depending on participant response Duration of follow‐up: 6 weeks |
|
| Outcomes | PAIN INTENSITY (SF‐McGill Pain Questionnaire, VAS component 10 cm scale) Baseline mean: acupuncture 4.9, sham acupuncture 5.0 End of study mean: acupuncture 1.7, sham acupuncture 3.2 Absolute benefit: acupuncture 3.2, sham acupuncture 1.8 Reported results: not significant SMD ‐0.60 (95% CI random ‐1.29 to 0.09) at 6 weeks DISABILITY: NECK DISABILITY INDEX (NDI 0 to 50 point scale) Baseline mean: acupuncture 18.6, sham acupuncture 20.5 End of study mean: acupuncture 8.4, sham acupuncture 11.9 Absolute benefit: acupuncture 10.2, sham acupuncture 8.6 Reported results: not significant SMD ‐0.41 (95% CI random ‐1.09 to 0.27) at 6 weeks Reasons for drop‐out: increased pain (stopped attending: 3 acupuncture, 4 sham) Adverse effects: increased pain (16/20 acupuncture, 9/20 sham) Costs of care: NR |
|
| Notes | ‐‐ | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Reported as random allocation sequence, computer‐generated using block size of 4 |
| Allocation concealment (selection bias) | Low risk | Held centrally by the pharmacy department at the research site; allocation concealed from the investigator until after participant enrolment |
| Blinding (performance bias and detection bias) All outcomes ‐ patient? | Unclear risk | Unclear whether sham was indistinguishable |
| Blinding (performance bias and detection bias) All outcomes ‐ care provider? | High risk | Not possible because of design |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessor? | Unclear risk | Participant was the outcome assessor with self reports |
| Incomplete outcome data (attrition bias) All outcomes ‐ Drop out rate acceptable? | Low risk | Acceptable at 17% |
| Incomplete outcome data (attrition bias) All outcomes ‐ Analyzed in the group to which they were allocated? | High risk | Only participants who completed the study were included; ITT done only for P value |
| Selective reporting (reporting bias) | Unclear risk | No protocol available |
| Similarity of baseline characteristics | Low risk | Reported as similar Tables 1 and 2 |
| Co‐interventions avoided or similar? | Unclear risk | Not reported |
| Compliance acceptable? | Unclear risk | Exercise booklet given; unsure whether participants received all acupuncture treatment prescribed |
| Similar timing of outcome assessment? | Low risk | Baseline, 3 and 6 weeks |
| Fatal Flaw | Low risk | Acceptable |
| Methods | RCT Number analysed/randomised: 35/35 Intention‐to‐treat: NA Power analysis: NR Funding source: NR | |
| Participants | Chronic myofascial neck pain Participant recruitment: teaching hospital, Taiwan |
|
| Interventions | INDEX TREATMENT Acupuncture group Dry needling, used a 25‐hypodermic needle (0.5 mm in diameter). Manual stimulation of the needle to the MTrP region of the extensor carpi radialis longus muscle to elicit a local twitch response. 1 to 2 minutes COMPARISON Sham acupuncture Same procedure as treatment group; however, needle was maintained in the subcutaneous tissue CO‐INTERVENTION Avoided Treatment schedule: 1 session Duration of follow‐up: immediate post treatment |
|
| Outcomes | PAIN INTENSITY (0 to 10 VAS scale) Baseline mean: acupuncture 7.3, sham acupuncture 7.2 End of study mean: acupuncture 5.2, sham acupuncture 6.4 Absolute benefit: acupuncture 2.1, sham acupuncture 0.8 Reported results: significant favouring acupuncture SMD ‐0.88 (95% CI random ‐1.58 to ‐0.19) immediate post treatment PRESSURE PAIN THRESHOLD (PPT, kg/cm2) Baseline mean: acupuncture 2.3, sham acupuncture 2.5 End of study mean: acupuncture 3.8, sham acupuncture 2.9 Absolute benefit: acupuncture 1.5, sham acupuncture 0.4 Reported results: significant favouring acupuncture SMD ‐1.25 (95% CI random ‐0.52 to ‐1.98) immediate post treatment Reasons for drop‐out: none Adverse effects: NR Costs of care: NR |
|
| Notes | ‐‐ | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computerised randomisation programme |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes ‐ patient? | Low risk | Reported in text |
| Blinding (performance bias and detection bias) All outcomes ‐ care provider? | High risk | Not possible |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessor? | Low risk | Participant blinded as outcome assessor |
| Incomplete outcome data (attrition bias) All outcomes ‐ Drop out rate acceptable? | Low risk | No drop‐outs |
| Incomplete outcome data (attrition bias) All outcomes ‐ Analyzed in the group to which they were allocated? | Low risk | All randomised participants were analysed |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics | Low risk | Reported to be similar |
| Co‐interventions avoided or similar? | Low risk | Avoided by pre/post design |
| Compliance acceptable? | Low risk | Acceptable by design |
| Similar timing of outcome assessment? | Low risk | Immediate post treatment |
| Fatal Flaw | Low risk | Acceptable |
| Methods | RCT Number analysed/randomised: 85/123 Intention‐to‐treat: calculated (although ITT stated, not all analysed at T2, only T1) Power analysis: calculated (90% power, alpha = 5%, 49 participants needed for experimental group and 46 for control group) Funding source: NR | |
| Participants | Non‐specific cervical disorder, uncomplicated Participant recruitment: Participants were referred to the Pain Treatment Unit at a Primary Attention Healthcare Centre in Spain by general practitioners in the municipality |
|
| Interventions | INDEX TREATMENT Acupuncture Points were selected according to pain characteristics and accompanying symptoms on the basis of traditional Chinese treatment methods. Puncture was bilateral, with sterile, single‐use needles (25 mm × 0.25 mm or 40 mm × 0.25 mm). Puncture was effected by determining the Deqi. Needles were kept in place for 30 minutes and were manually stimulated every 10 minutes. After the needles were removed, Vaccaria seeds were applied in the ear auricle and were taped there until the following treatment session. Participants were told to apply pressure to each ear point for a series of 10 repeats 3 times per day COMPARISON TREATMENT TENS placebo Applied using TRANSMED 911 transcutaneous nerve stimulation units that had been adjusted beforehand to prevent current through the electrodes. Electrodes were placed at Jianjing (GB 21) bilateral acupuncture point for 30 minutes. Participant's state was checked every 10 minutes, and the TENS‐placebo potentiometer adjusted CO‐INTERVENTION Not avoided but comparable; both groups were provided with analgesic rescue medications once weekly Duration of treatment: 3 weeks Treatment consisted of 5 sessions over 3 weeks (2 in each of first 2 weeks and once in the third week) Duration of follow‐up: 6 months |
|
| Outcomes | PAIN INTENSITY (VAS 100 mm scale related to motion) Baseline mean: acupuncture 68.7, placebo TENS 72.3 End of study mean: acupuncture 27.6, placebo TENS 45.5 Absolute benefit: acupuncture 41.1, placebo TENS 26.8 SMD ‐1.50 (95% CI random ‐1.91 to ‐1.10) at 1 week SMD ‐0.54 (95% CI random ‐0.97 to ‐0.10) at 6 months FUNCTION (DISCAPACITY): Northwick Park Pain Questionnaire (NPQ 0 to 100 scale) Baseline mean: acupuncture 52.7, placebo TENS 56.5 End of study mean: acupuncture 22.5, placebo TENS 43.8 Absolute benefit: acupuncture 30.2, placebo TENS 12.7 Reported results: significant at 1 week after final treatment SMD ‐1.22 (95% CI random ‐1.60 to ‐0.83) at 1 week 6 month follow‐up for this outcome: NR QUALITY OF LIFE: SF‐36 (Physical Component ‐ higher = better) Baseline mean: acupuncture 36.7, placebo TENS 37.6 End of study mean: acupuncture 27.4, placebo TENS 32.3 Absolute benefit: acupuncture 9.3, placebo TENS 5.3 Results: significant difference at 1 week favouring acupuncture but not at 6 months SMD ‐0.57 (95% CI random ‐0.93 to ‐0.21) at 1 week SMD 0.41 (95% CI random ‐0.02 to 0.84) at 6 months Reasons for drop‐out: personal reasons, pregnancy, fear Adverse effects: mild for both groups (4 in treatment group, 2 in control group) Reported for control: increase in symptoms Reported for index treatment: swelling or bruising of the hand Costs of care: NR |
|
| Notes | ‐‐ | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computerised generated randomisation |
| Allocation concealment (selection bias) | Unclear risk | Opaque envelopes not reported as sequentially numbered |
| Blinding (performance bias and detection bias) All outcomes ‐ patient? | Low risk | Reported in text as participant blinded |
| Blinding (performance bias and detection bias) All outcomes ‐ care provider? | High risk | Not possible |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessor? | Low risk | Blinded participant as outcome assessor |
| Incomplete outcome data (attrition bias) All outcomes ‐ Drop out rate acceptable? | High risk | Drop‐out approximately 35% at long term |
| Incomplete outcome data (attrition bias) All outcomes ‐ Analyzed in the group to which they were allocated? | High risk | Not reported for long term |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics | Low risk | Reported to be similar |
| Co‐interventions avoided or similar? | High risk | Reported only on medication use |
| Compliance acceptable? | Unclear risk | Unsure whether ear seed protocol was followed by each participant |
| Similar timing of outcome assessment? | Low risk | Assessed at 1 week and 6 months |
| Fatal Flaw | Low risk | Acceptable |
| Methods | RCT/cross‐over Number analysed/randomised: 68/68 Intention‐to‐treat: NR Power analysis: NR Funding source: Forest Park Institute, Ambulatory Anesthesia Research Foundation, White Mountain Institute | |
| Participants | Chronic mechanical neck disorder, degenerative changes Participant recruitment: Eugene McDermott Centre for Pain Management, Department of Anesthesiology and Pain Management, University of Texas Southwestern Medical Centre, Dallas, Texas |
|
| Interventions | INDEX TREATMENT 1 Local dermatomal stimulation 10 acupuncture‐like needle probes inserted 2 to 4 cm into soft tissue/paraspinous muscles in the cervical region, alternating frequency of 15 Hz to 30 Hz to produce gentle tapping sensation without muscle contraction COMPARISON TREATMENT 1 Remote dermatomal stimulation 10 acupuncture‐like needle probes inserted into soft tissue/paraspinous muscle in the lower back region with identical electrical therapy characteristics of the local dermatomal stimulation group COMPARISON TREATMENT 2 Control needles only Needles inserted into the cervical region without electrical stimulation CO‐INTERVENTION Analgesics comparable between groups Treatment schedule: 3 times/wk for 3 consecutive weeks, with 1 week off between modalities and each session averaging 30 minutes in duration Duration of follow‐up: 24 hours after completion of each 3 week treatment period |
|
| Outcomes | PAIN INTENSITY (10 cm VAS scale) Baseline mean: NR End of study mean: NR Reported results: significant differences between groups favouring local dermatomal stimulation Reasons for drop‐out: NA Adverse effects: NR Costs of care: NR |
|
| Notes | ‐‐ | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes ‐ patient? | High risk | Interventions perceivably different |
| Blinding (performance bias and detection bias) All outcomes ‐ care provider? | High risk | Not possible |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessor? | High risk | Participant as outcome assessor not blinded |
| Incomplete outcome data (attrition bias) All outcomes ‐ Drop out rate acceptable? | Unclear risk | Inadequate description |
| Incomplete outcome data (attrition bias) All outcomes ‐ Analyzed in the group to which they were allocated? | Unclear risk | Unclear whether all analysed |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics | High risk | Means given as 1 group in total |
| Co‐interventions avoided or similar? | High risk | Medication use not similar |
| Compliance acceptable? | Low risk | Acceptable |
| Similar timing of outcome assessment? | Low risk | Immediate post treatment |
| Fatal Flaw | High risk | Inadequate reporting |
| Methods | RCT Number analysed/randomised: 124/135 Intention‐to‐treat: NR Power analysis: calculated Funding source: Henry Smiths Charity, Hospital Savings Association, Laing Foundation. | |
| Participants | Chronic mechanical neck disorder Participant recruitment: out‐patient departments of Southampton General Hospital and Salisbury District Hospital, United Kingdom |
|
| Interventions | INDEX TREATMENT Acupuncture with single‐use needles, points based on individualised western acupuncture techniques previously reported as effective in neck pain, 6 points on average, with each session averaging 20 minutes in duration. Manual stimulation to Deqi. 8 treatments over 4 weeks provided by physiotherapists with 7 years of experience COMPARISON TREATMENT Mock TENS electroacupuncture stimulator; up to 8 points could be stimulated at 1 time; session time not reported CO‐INTERVENTION Comparable between index and control groups Treatment schedule: Both groups received 8 sessions over 4 weeks Duration of follow‐up: 1 and 8 weeks, 6 and 12 months |
|
| Outcomes | PAIN INTENSITY (100 mm VAS scale) Baseline mean: acupuncture 49.6, mock TENS 54.1 End of study mean: acupuncture 20.91, mock TENS 24.36 Absolute benefit: acupuncture 28.69, mock TENS 29.74 Reported results: Acupuncture reduced pain, with no clinically effective difference between groups SMD ‐0.48 (95% CI random ‐0.84 to ‐0.13) at 1 week SMD ‐0.29 (95% CI random ‐0.66 to 0.07) at 8 weeks SMD ‐0.07 (95% CI random‐0.45 to 0.30) at 6 months SMD ‐0.13 (95% CI random ‐0.51 to 0.25) at 1 year DISABILITY (NDI 0 to 50 point scale) SMD ‐0.08 (95% CI random ‐0.43 to 0.27) at 1 week SMD ‐0.24 (95% CI random ‐0.60 to 0.12) at 8 weeks SMD ‐0.09 (95% CI random ‐0.47 to 0.28) at 6 months SMD ‐0.23 (95% CI random ‐0.61 to 0.15) at 1 year QUALITY OF LIFE (SF‐36, Physical Component) SMD 0.07 (95% CI random ‐0.28 to 0.42) at 1 week SMD ‐0.13 (95% CI random ‐0.49 to 0.23) at 8 weeks Time points at 6 months and 1 year not reported for this outcome Reported results: significant improvement in both treatment groups Adverse effects: Acupuncture group reported increase in the following symptoms: faintness, slight swelling of hand, bruise, mild headache, euphoria and enhanced vision, dizziness; placebo group reported discomfort during treatment, mild headache, tiredness, faintness, nausea, tingling in the thumb, dizziness, uncomfortable cold feeling of electrodes Costs of care: NR |
|
| Notes | ‐‐ | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Adequate |
| Allocation concealment (selection bias) | Unclear risk | Sealed envelopes; unclear whether opaque and sequentially numbered |
| Blinding (performance bias and detection bias) All outcomes ‐ patient? | High risk | Interventions perceivably different |
| Blinding (performance bias and detection bias) All outcomes ‐ care provider? | High risk | Not possible |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessor? | High risk | Participant as outcome assessor not blinded |
| Incomplete outcome data (attrition bias) All outcomes ‐ Drop out rate acceptable? | Low risk | Acceptable |
| Incomplete outcome data (attrition bias) All outcomes ‐ Analyzed in the group to which they were allocated? | High risk | Not all randomised participants were analysed |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics | Low risk | Reported to be similar |
| Co‐interventions avoided or similar? | High risk | Medication use not similar |
| Compliance acceptable? | Unclear risk | Not described |
| Similar timing of outcome assessment? | Low risk | 6 months and 1 year |
| Fatal Flaw | Low risk | Acceptable |
| Methods | RCT Number analysed/randomised: 3036/3766 Intention‐to‐treat: calculated Power analysis: calculated Funding source: NR | |
| Participants | Chronic neck pain Participant recruitment: Participants with neck pain asked a participating physician for acupuncture, or physician considered acupuncture to be adequate treatment |
|
| Interventions | INDEX TREATMENT Immediate acupuncture treatment plus additional conventional treatment as needed Participants could be treated individually, and numbers of needles and acupuncture points used were chosen at the discretion of physicians. Only needle acupuncture (with disposable 1‐time needles) and manual stimulation were allowed, whereas other forms of acupuncture treatment were not allowed COMPARISON TREATMENT Conventional treatment; delayed acupuncture treatment 3 months after study onset Control group was not allowed to use any kind of acupuncture during first 3 months CO‐INTERVENTION Comparable between index and control groups. Participants were free to use conventional routine medical care as offered by German social health insurance funds Treatment schedule: Each participant in the randomised acupuncture group received up to 15 acupuncture sessions during first 3 months and no acupuncture sessions between 3 and 6 months Duration of treatment: 3 months Duration of follow‐up: 3 months after treatment |
|
| Outcomes | HEALTH AND WELL‐BEING Neck and pain disability assessed by validated neck and pain disability scale developed by Wheeler Baseline mean: 55.0 immediate acupuncture (randomised), 56.0 (immediate acupuncture non‐randomised), 53.9 delayed acupuncture % reduction in neck pain and disability Time 1 (3 months): 28.9 immediate acupuncture (randomised), 31.7 immediate acupuncture (non‐randomised), 5.8 delayed acupuncture Time 2 (6 months): 28.0 immediate acupuncture (randomised), 30.6 immediate acupuncture (non‐randomised), 25.1 delayed acupuncture Reported results: significant at time 1 SMD ‐35.53 (95% CI random ‐36.37 to ‐34.69) at 3 month follow‐up SMD 4.14 (95% CI random 4.02 to 4.26) at 6 month follow‐up SF‐36 PHYSICAL COMPONENT SCORE Baseline mean: 37.6 immediate acupuncture (randomised), 36.7 immediate acupuncture (non‐randomised), 38.1 delayed acupuncture Time 1 (3 months): 5.8 immediate acupuncture (randomised), 6.8 immediate acupuncture (non‐randomised), 4.7 delayed acupuncture Time 2 (6 months): 5.6 immediate acupuncture (randomised), 6.8 immediate acupuncture (non‐randomised), 0.7 delayed acupuncture SMD 22.99 (95% CI random 22.45 to 23.54) at 3 month follow‐up SMD 3.00 (95% CI random 2.90 to 3.10) at 6 month follow‐up SF‐36 MENTAL COMPONENT SCORE Baseline mean: 43.1 immediate acupuncture (randomised), 42.8 immediate acupuncture (non‐randomised), 43.8 delayed acupuncture Time 1 (3 months): 4.2 immediate acupuncture (randomised), 4.7 immediate acupuncture (non‐randomised), 3.1 delayed acupuncture Time 2 (6 months): 4.0 immediate acupuncture (randomised), 4.8 immediate acupuncture (non‐randomised), 3.1 delayed acupuncture SMD 12.80 (95% CI random 12.49 to 13.11) at 3 month follow‐up SMD 3.00 (95% CI random 2.90 to 3.10) at 6 month follow‐up Reasons for drop‐out: 315 participants could not be included in the ITT analysis because the study office did not receive the consent form Adverse effects: 8.9% of cases (n = 1005); 1216 side effects were reported: 57% minor local bleeding or hematoma, 10% pain (e.g. needling pain), 4% vegetative symptoms, 29% other Costs of care: acupuncture treatment associated with higher costs (€925.53 ± 1551.06 vs €648.06 ± 1459.13); however according to assumed threshold values beyond 3 month follow‐up, acupuncture appears cost‐effective. Also, over‐the‐counter medications were not included in the cost of routine care |
|
| Notes | ‐‐ | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomised using a central telephone randomisation procedure |
| Allocation concealment (selection bias) | Low risk | Study office included participants into the study |
| Blinding (performance bias and detection bias) All outcomes ‐ patient? | High risk | Not possible |
| Blinding (performance bias and detection bias) All outcomes ‐ care provider? | High risk | Not possible |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessor? | High risk | Participant as outcome assessor not blinded |
| Incomplete outcome data (attrition bias) All outcomes ‐ Drop out rate acceptable? | High risk | Drop‐outs not adequately described |
| Incomplete outcome data (attrition bias) All outcomes ‐ Analyzed in the group to which they were allocated? | Unclear risk | Unclear whether ITT was done correctly |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics | Low risk | Reported to be similar |
| Co‐interventions avoided or similar? | Unclear risk | Not reported |
| Compliance acceptable? | Low risk | Most participants (77.3%) received 5 to 10 sessions, whereas 17.7% received more than 10 sessions and 5% fewer than 5 sessions |
| Similar timing of outcome assessment? | Low risk | Assessed at 3 and 6 months |
| Fatal Flaw | Low risk | Acceptable |
Abbreviations: BL = bladder CI = confidence interval cm = centimetre dn = dry needling EAP = electroacupuncture
g = gauge GB = gallbladderITT = intention‐to‐treat LI = large intestine LLLT0 = placebo intestine mg = milligram mm = millimetreMPS = myofascial neck pain syndrome MTrP = muscles treated not described NA = not applicable NDI = Neck Disability Index NLA = non‐local needle electroacupuncture NPQ = Northwick Park Pain Questionnaire NR = not reported NSAID = non‐steroidal anti‐inflammatory drug NTPA = non‐trigger point acupuncture OD = daily PPT = pain pressure threshold RA = remote acupuncture RCT = randomised controlled trial SA = standard acupuncture SD = standard deviation SF‐36 = Short Form‐36 SH = sham treatment SI = small intestine SMD = standardised mean difference TCM = Traditional Chinese Medicine TE = triple energiser TENS = transcutaneous electrical nerve stimulation TNS = transcutaneous nerve stimulation TPA = trigger point acupuncture TrP = trigger point acupuncture VAS = visual analogue scale WAD = whiplash‐associated disorder
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Bahadir 2009 | Comparison: acupuncture vs active treatment (ultrasound) |
| Calvo‐Trujillo 2013 | Intervention: auto‐acupressure, not acupuncture Comparison: active treatment (paracetamol and/or ibuprofen and tetrazepam) |
| Ceccherelli 2006 | Comparison: 1 acupuncture type vs another |
| Ceccherilli 2014 | Comparison: 3 acupuncture doses compared |
| Cho 2014 | Comparison: acupuncture vs active treatment (NSAID) |
| Chu 1997 | Intervention (EMG needle) |
| Coeytaux 2005 | Population: migraine and tension‐type headaches, others not specified as cervicogenic Comparison: acupuncture vs active treatment (medical management) |
| Cohen 2014 | Intervention: acupuncture portion of multi‐modal treatment |
| David 1998 | Comparison: acupuncture vs active treatment (mobilisation) |
| Dong 2012 | Comparison: 1 acupuncture type vs another |
| Edwards 2003 | Comparison: multi‐modal treatment acupuncture vs active treatment (stretching) |
| Emery 1986 | Population: ankylosing spondylitis |
| Eroglu 2013 | Comparison: acupuncture vs active treatment (lidocaine injection or oral flurbiprofen) |
| Falkenberg 2007 | Comparison: acupuncture portion of multi‐modal treatment vs active treatment (usual care) |
| Fernandez‐Carnero 2014 | Comparison: acupuncture received in both groups as control |
| Franca 2008 | Comparison: acupuncture vs active treatment (exercise) |
| Fu 2005 | Comparison: acupuncture vs active treatment (lidocaine) |
| Fu 2007 | Comparison: 1 acupuncture insertion direction vs another |
| Fu 2014 | Comparison: electroacupuncture vs active treatment (traction and low‐frequency therapy) |
| Ga 2007a | Design: quasi‐RCT Comparison: acupuncture vs active treatment (lidocaine) |
| Ga 2007b | Comparison: acupuncture vs active treatment (lidocaine) |
| Gallacchi 1981 | Population: tendomyotonic cervical and lumbar syndrome; unable to separate data |
| Gallacchi 1983 | Population: rheumatoid arthritis |
| Gallego Sendarrubias 2015 | Intervention: acupuncture combined with manual therapy; not a stand‐alone treatment |
| Gaw 1975 | Population: pain in many areas; unable to separate data |
| Gil 2015 | Intervention: individual vs group acupuncture |
| Giles 1999 | Comparison: acupuncture vs active treatment (medication) |
| Giles 2003 | Population: neck and low back; unable to split data |
| Guanygue 2001 | Comparison: included other treatments with acupuncture; the effect of acupuncture could not be isolated |
| Guo 2013 | Comparison: acupuncture portion of the control |
| Harvey 2015 | Comparison: sham acupuncture vs lidocaine injection (no real acupuncture compared) |
| Hayek 2014 | Comparison: acupuncture may be part of multi‐modal treatment vs epidural steroid injections (ESI) with depo‐methylprednisolone |
| Hu 2014 | Comparison: electroacupuncture vs active treatment (bloodletting and cupping ‐ CAM intervention) |
| Hua 2009 | Design: quasi‐RCT Comparison: electroacupuncture portion of control |
| Huang 2008 | Comparison: 1 acupuncture type vs another |
| Huang 2012 | Comparison: acupuncture vs active treatment (traction, magnetic therapy) Outcome: blood flow; no participant‐specific outcomes |
| Hudson 2010 | Comparison: acupuncture portion of multi‐modal usual care active treatment (2 participants) |
| Jia 2007 | Comparison: 1 acupuncture type vs another |
| Jin 2012 | Comparison: 1 acupuncture type vs another |
| Johnson 2000 | Abstract; did not appear to be RCT; unable to contact study author |
| Kai 2008 | Comparison: 1 acupuncture type vs another |
| Kisiel 1996 | Population: neck and shoulder pain; cannot split data |
| Li 2004 | Comparison: 1 acupuncture type vs another |
| Li 2006 | Population: spinal cord stenosis Comparison: acupuncture vs active treatment (manipulation/traction) |
| Li 2013 | Comparison: acupuncture received in both groups as control |
| Lin 2004 | Intervention: scalpel technique |
| Liu 2008 | Comparison: 1 acupuncture type vs another |
| Liu 2013 | Comparison: acupuncture vs active treatment (intravenous drip with 5% glucose 250 mL and compound Salvia miltiorrhiza injection and mechanical traction) |
| Lixing 2000 | Comparison: acupuncture vs acupuncture with moxibustion |
| Llamas‐Ramas 2014 | Comparison: acupuncture vs active treatment (trigger point manual therapy) |
| Loy 1983 | Design: quasi‐RCT Comparison: acupuncture vs active treatment (traction and shortwave diathermy) |
| Lu 2006 | Comparison: 1 acupuncture type vs another |
| Lundeburg 1988 | Population: head and neck pain included; unable to obtain split data |
| Lundeburg 1991 | Comparison: multi‐modal; effects of acupuncture unknown |
| Luo 2010 | Design: non‐RCT |
| Ma 2010 | Intervention: mini‐scalpel |
| MacPherson 2013 | Comparison: acupuncture vs active treatment (Alexander lessons, postural awareness, usual care) |
| McLean 2013 | Comparison: acupuncture portion of multi‐modal usual care active treatment (4 participants) |
| Muller 2005 | Comparison: see excluded Giles 2003; this is LT follow‐up |
| Myburgh 2012 | Comparison: 1 acupuncture type vs another |
| Nakajima 2015 | Comparison: 1 type of acupuncture vs another |
| Pan 2008 | Design: quasi‐RCT Population: occipital neuralgia |
| Pecos‐Martin 2015 | Comparison: 1 acupuncture type vs another |
| Peng 1987 | Design: non‐RCT |
| Rayegani 2014 | Comparison: acupuncture vs active treatment (physiotherapy including heat, TENS, ultrasound, passive and self stretching) |
| Salter 2006 | Comparison: acupuncture vs active treatment (GP care in both groups) |
| Sato 2014 | Population: individuals with latent trigger points in upper trapezius, no neck pain |
| Sator‐Katzenschlager 2003 | Comparison: 1 acupuncture type vs another |
| Seo 2014 | Intervention: bee venom acupuncture (BVA) injected with syringe Comparison: acupuncture vs active treatment (NSAID) |
| Shang 2002 | Comparison: 1 acupuncture type vs another |
| Shuangquan 2003 | Comparison: 1 acupuncture type vs another |
| Soderlund 2001 | Comparison: multi‐modal; effects of acupuncture unknown |
| Sun 2013 | Comparison: acupuncture vs electroacupuncture (protocol) |
| Takakura 2014 | Population: individuals with functional neck stiffness without pain |
| Teng 1973 | Abstract; did not appear to be RCT; unable to obtain further information |
| Tobbackx 2013 | Comparison: active treatment (relaxation therapy) |
| Venancio 2008 | Population: tension‐type and/or migraine headaches Comparison: acupuncture vs active treatment (lidocaine) |
| Venancio 2009 | Population: tension‐type and/or migraine headaches Comparison: active treatment (lidocaine or Botox) |
| Wan 2013 | Comparison: 1 acupuncture type vs another vs active treatment (oral Jing fukang granule) |
| Wang 2007 | Comparison: 1 acupuncture type vs another |
| Wang 2008 | Comparison: 1 acupuncture type vs another |
| Wang G 2014 | Comparison: acupuncture in both groups as control |
| Xu 2012 | Comparison: 1 acupuncture type vs another |
| Xue 2007 | Design: quasi‐RCT Comparison: 1 acupuncture type vs another |
| Yang 2009 | Comparison: 1 acupuncture type vs another |
| Yang 2013 | Comparison: acupuncture vs active treatment (Chinese manipulation) |
| Yoon 2009 | Comparison: 3 types of acupuncture needles compared |
| Yoshimizu 2012 | Comparison: acupuncture vs active treatment (TENS) |
| Yu 2003 | Comparison: 1 acupuncture type vs another |
| Zeng 2005 | Comparison: 1 acupuncture type vs another |
| Zhang 1996 | Design: appeared to be before/after study or case series report Population: included myelopathy |
| Zhang 2003 | Comparison: acupuncture vs active treatment (traction) |
| Zhang J 2008 | Comparison: electroacupuncture vs active treatment (laser) |
| Zhang J 2013 | Comparison: acupuncture received in both groups as control |
| Zhang X‐Z 2013 | Intervention: 1 acupuncture type vs another |
| Zhao 2004 | Comparison: acupuncture with moxibustion |
| Zheng 2014 | Intervention: mini‐scalpel acupuncture Comparison: 1 acupuncture type vs another |
| Zhi 2008 | Intervention: injection‐type needle |
| Zhou 2014 | Comparison; acupuncture vs active treatment (moxibustion) |
| Zhu 2002 | Outcome: no between‐group comparison analysed |
| Zhu 2006 | Comparison: acupuncture vs needle‐knife therapy |
| Zhuang 2004 | Comparison: 1 acupuncture type vs another |
| Ziaeifar 2014 | Comparison: acupuncture vs active treatment (massage) |
Characteristics of studies awaiting assessment [ordered by study ID]
| Methods | Abstract for RCT |
| Participants | 67 acute neck and back pain |
| Interventions | Acupuncture vs sham acupuncture plus standard ER care (medication not described) |
| Outcomes | Numeric Rating Scale (NRS), ROM, Symptom Checklist (SCL) questionnaire and overall satisfaction |
| Notes | Await full study, contact study author |
| Methods | RCT |
| Participants | 65 patients with acute or subacute/chronic simple back or neck pain |
| Interventions | Acupuncture vs placebo acupuncture vs no treatment |
| Outcomes | Pain (NPS) |
| Notes | clinicaltrials.gov |
| Methods | RCT |
| Participants | 44 patients with myofascial neck pain |
| Interventions | Acupuncture + stretching vs same stretching |
| Outcomes | Pain (VAS), pressure pain threshold |
| Notes | clinicaltrials.gov |
| Methods | RCT |
| Participants | 40 patients with whiplash‐associated disorder |
| Interventions | Acupuncture vs wait‐list |
| Outcomes | Pain (VAS), post‐needling pain, pressure pain threshold, range of motion, quality of life (SF‐36), Depression Scale, Cornell Medical Index (CMI) |
| Notes | clinicaltrials.gov |
| Methods | Guo Y |
| Participants | 154 with unspecific duration of neck pain |
| Interventions | Acupuncture vs sham acupuncture |
| Outcomes | Pain (NPQ, VAS), quality of life (SF‐36), participant satisfaction |
| Notes | http://apps.who.int/trialsearch/AdvSearch.aspx |
| Methods | Abstract for RCT |
| Participants | 60 patients with unilateral cervicobrachialgia |
| Interventions | Abdominal acupuncture vs sham abdominal acupuncture |
| Outcomes | VAS for pain and hypomobility (ROM) |
| Notes | Await full study, contact study author |
| Methods | RCT |
| Participants | 17 patients with acute mechanical idiopathic unilateral neck pain |
| Interventions | Dry needling of trigger points vs no treatment control |
| Outcomes | Numeric Pain Rating Scale (NPRS), pressure pain threshold (PPT) for pain, range of motion |
| Notes | ‐‐ |
| Methods | RCT |
| Participants | 23 patients with acute symptoms of craniomandibular disorder |
| Interventions | Acupuncture vs sham laser |
| Outcomes | Pain intensity (VAS), functional muscle test, ability to open the mouth, axiographic evaluation |
| Notes | German; awaiting translation |
| Methods | Protocol for double‐blind RCT |
| Participants | 120 participants with chronic whiplash, grade II |
| Interventions | Dry needling, advice and exercise vs sham dry needling, advice and exercise |
| Outcomes | Neck Disability Index (NDI), participant‐perceived recovery |
| Notes | ‐‐ |
| Methods | RCT, cross‐over design |
| Participants | 19 patients with myofascial neck pain |
| Interventions | Acupuncture, acupuncture plus stretching vs placebo laser acupuncture |
| Outcomes | Mechanical pain threshold, motion‐related pain (visual analogue scale ‐ VAS) and cervical range of motion, range of motion |
| Notes | ‐‐ |
| Methods | RCT |
| Participants | 206 patients with chronic neck pain |
| Interventions | Electroacupuncture vs sham laser acupuncture |
| Outcomes | Neck Pain Disability Northwick Park Neck Pain Questionnaire (NPQ), Quality of Life SF‐36 health survey, use of medication for neck pain, sick leave |
| Notes | ‐‐ |
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | Evaluation of immediate effect of acupuncture on pain, cervical range of motion and electromyographic activity of the upper trapezius muscle in patients with non‐specific neck pain: study protocol for a randomised controlled trial |
| Methods | Protocol for RCT cross‐over design, 1 week wash‐out period |
| Participants | 12 participants with neck pain, 12 healthy participants |
| Interventions | Acupuncture vs placebo acupuncture |
| Outcomes | EMG activity of upper trapezius, NPRS for neck pain and cervical range of motion (CROM) |
| Starting date | ‐‐ |
| Contact information | ‐‐ |
| Notes | ‐‐ |
| Trial name or title | Acupuncture as analgesia for non‐emergent acute non‐specific neck pain, ankle sprain and primary headache in an emergency department setting: a protocol for a parallel‐group, randomised, controlled pilot trial |
| Methods | Protocol for RCT |
| Participants | 40 patients with non‐emergent acute neck pain, ankle sprain or primary headache |
| Interventions | Acupuncture + standard emergency department care vs same |
| Outcomes | Numeric Rating Scale for pain (NRS), Neck Disability Index (NDI), participant‐reported overall improvement |
| Starting date | ‐‐ |
| Contact information | ‐‐ |
| Notes | To be determined if number of participants with neck pain is sufficient and extractable data are available and/or if primary headaches are of cervical origin |
| Trial name or title | Optimised acupuncture treatment for neck pain caused by cervical spondylosis: a study protocol of a multi‐centre randomised controlled trial |
| Methods | Protocol for RCT |
| Participants | 945 patients with cervical spondylosis |
| Interventions | Acupuncture vs sham acupuncture vs shallow acupuncture |
| Outcomes | Northwick Park Pain Questionnaire (NPQ), McGill Pain Questionnaire (MPQ) and SF‐36 for pain and disability |
| Starting date | ‐‐ |
| Contact information | ‐‐ |
| Notes | ‐‐ |
| Trial name or title | Effectiveness of acupuncture intervention for neck pain caused by cervical spondylosis: study protocol for a randomised controlled trial |
| Methods | Protocol for RCT |
| Participants | 456 patients with neck pain caused by cervical spondylosis |
| Interventions | Acupuncture vs sham acupuncture |
| Outcomes | NPQ, MPQ and SF‐36 for pain and disability |
| Starting date | ‐‐ |
| Contact information | ‐‐ |
| Notes | ‐‐ |
| Trial name or title | Acupuncture at Houxi (SI 3) acupoint for acute neck pain caused by stiff neck: study protocol for a pilot randomised controlled trial. |
| Methods | Protocol for pilot RCT |
| Participants | 36 patients with acute neck pain and stiffness |
| Interventions | Acupuncture + massage vs massage |
| Outcomes | NPQ, SF‐MPQ |
| Starting date | ‐‐ |
| Contact information | ‐‐ |
| Notes | ‐‐ |
Contributions of authors
Primary reviewers for this review ‐ Trinh K, Graham N, Irnich D, Cameron ID, Forget M.
Statistician ‐ Trinh K, Goldsmith CH (Cervical Overview Group ‐ COG). Methodological quality assessment ‐ COG Validity Team; Burnie S, Empey B, Forget M, Goldsmith CH, Graham N, LeBlanc F, Szeto G. Study identification and selection ‐ Brunarski D, Graham N, Gross A, Haines T (COG). Research librarian ‐ Rice M. Data abstraction, synthesis, manuscript preparation, public responsibility, grants, administration ‐ primary review authors. Final synthesis ‐ primary review authors.
Sources of support
Internal sources
No sources of support supplied
External sources
-
Candian Institute of Health Research, Canada.
Knowledge Synthesis Grant "Synthesizing Research Evidence into Clinical Recommendations for Managing Neck Pain"
Declarations of interest
D Irnich is an author of two included studies. He did not take part in data extraction.
Use of raters from diverse professional backgrounds (sports medicine physician, rheumatologist, occupational health physician, physiatrist, statistician, physiotherapist, manual therapist, chiropractor, massage therapist) should serve to limit any conflicts of interest that might have been present during the review process.
Notes
We have received comments on this review and have withdrawn it from the Library while comments are being addressed.
Withdrawn from publication for reasons stated in the review
References
References to studies included in this review
- Birch S, Jamison R. Controlled trial of Japanese acupuncture for chronic myofascial neck pain: assessment of specific and nonspecific effects of treatment. Clinical Journal of Pain 1998;14:248‐55. [CO2002:2756] [DOI] [PubMed] [Google Scholar]
- Cameron ID, Wang E. World Congress on Neck Pain Conference Proceedings. Los Angeles, 2008. [Google Scholar]; Cameron ID, Wang E, Sindhusake D. A randomized trial comparing acupuncture and simulated acupuncture for subacute and chronic whiplash. Spine 2011;36(26):E1659‐65. [DOI] [PubMed] [Google Scholar]
- Chou L‐W, Hsieh Y‐L, Kao M‐J, Hong C‐Z. Remote influences of acupuncture on the pain intensity and the amplitude changes of endplate noise in the myofascial trigger point of the upper trapezius muscle. Archives of Physical Medicine and Rehabilitation 2009;90:905‐12. [DOI] [PubMed] [Google Scholar]
- Coan RM, Wong G, Coan PL. The acupuncture treatment of neck pain: a randomized controlled study. American Journal of Chinese Medicine 1982;9(4):326‐32. [DOI] [PubMed] [Google Scholar]
- Fu W‐B, Liang Z‐H, Zhu X‐P, Yu P, Zhang J‐F. Analysis on the effect of acupuncture in treating cervical spondylosis with different syndrome types. Chinese Journal of Integrative Medicine 2009;15(6):426‐30. [DOI] [PubMed] [Google Scholar]
- He D, Veiersted KB, Hostmark AT, Medbo JI. Effect of acupuncture treatment on chronic neck pain and shoulder pain in sedentary female workers: a 6‐month and 3‐year follow‐up study. Pain 2004;109(3):299‐307. [CO2006] [DOI] [PubMed] [Google Scholar]
- He D, Hostmark AT, Veiersted KB, Medbo JI. Effect of intensive acupuncture on pain‐related social and psychological variables for women with chronic neck and shoulder pain ‐ an RCT with six month and three year follow up. Acupuncture in Medicine 2005;23(2):52‐61. [C)2007] [DOI] [PubMed] [Google Scholar]
- Ilbuldu E, Cakmak A, Disci R, Aydin R. Comparison of laser, dry needling, and placebo laser treatments in myofascial pain syndrome. Photomedicine and Laser Surgery 2004;22(4):306‐11. [CO2006] [DOI] [PubMed] [Google Scholar]
- Irnich D, Behrens N, Molzen H, Konig A, Gleditsch J, Krauss M, et al. Randomized trial of acupuncture compared with conventional massage and "sham" laser acupuncture for treatment of chronic neck pain. BMJ 2001;322:1574‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]; König A, Radke S, Molzen H, Haase M, Müller C, Drexler D, et al. Randomised trial of acupuncture compared with conventional massage and "sham" laser acupuncture for treatment of chronic neck pain ‐ range of motion analysis [Randomisierte studie zur akupunktur in vergleich mit konventioneller massage und schein‐laserakupunktur in der behandlung chronischer HWS‐Beschwerden ‐ Bewegungsanalyse]. Zeitschrift für Orthopädie und ihre Grenzgebiete 2003;141(4):395‐400 [Other: CO2004]. [DOI] [PubMed] [Google Scholar]
- Irnich D, Behrens N, Gleditsch JM, Stor W, Schreiber, MA, Schopd P, et al. Immediate effects of dry needling and acupuncture at distant points in chronic neck pain: results of a randomized, double‐blind, sham‐controlled crossover trial. Pain 2002;99:83‐9. [CO2004;] [DOI] [PubMed] [Google Scholar]
- Itoh K, Katsumi Y, Hirota S, Kitakoji H. Randomised trial of trigger point acupuncture compared with other acupuncture for treatment of chronic neck pain. Complementary Therapies in Medicine 2007;15:172‐9. [CO2007] [DOI] [PubMed] [Google Scholar]
- Kwak HY, Kim JI, Park JM, Lee SH, Yu HS, Lee JD, et al. Acupuncture for whiplash‐associated disorder: a randomized, waiting‐list controlled, pilot trial. European Journal of Integrative Medicine 2012;4(2):151‐8. [Google Scholar]
- Liang ZH, Yang YH, Yu P, Zhu XP, Wu ZL, Zhang JF, et al. Logistic regression analysis on therapeutic effect of acupuncture on neck pain caused by cervical spondylosis and factors influencing therapeutic effect [in Chinese]. Chinese Acupuncture & Moxibustion 2009;29(3):173‐6. [CO2010] [PubMed] [Google Scholar]
- Liang Z, Zhu X, Yang X, Fu W, Lu A. Assessment of a traditional acupuncture therapy for chronic neck pain: a pilot randomised controlled study. Complementary Therapies in Medicine 2011;195:526‐32. [DOI] [PubMed] [Google Scholar]
- Nabeta T, Kawakita K. Relief of chronic neck and shoulder pain by manual acupuncture to tender points ‐ a sham‐controlled randomized trial. Complementary Therapies in Medicine 2002;10:217‐22. [CO2006] [DOI] [PubMed] [Google Scholar]
- Petrie JP, Langley GB. Acupuncture in the treatment of chronic cervical pain. A pilot study. Clinical and Experimental Rheumatology 1983;1:333‐5. [PubMed] [Google Scholar]
- Petrie JP, Hazleman BL. A controlled study of acupuncture in neck pain. British Journal of Rheumatology 1986;25:271‐5. [CO97: 180] [DOI] [PubMed] [Google Scholar]
- Sahin N, Ozcan E, Sezen K, Karatas O, Issever H. Efficacy of acupuncture in patients with chronic neck pain ‐ a randomised, sham controlled trial. Acupuncture and Electro‐Therapeutics Research International Journal 2010;35:17‐27. [DOI] [PubMed] [Google Scholar]
- Seidel U, Uhlemann C. A randomised controlled double‐blind trial comparing dosed laser therapy on acupuncture points and acupuncture for chronic cervical syndrome [in German]. Deutsche Zeitschrift fur Akupunkture 2002;45:258‐69. [CO2003] [Google Scholar]
- Sun M‐Y, Hsieh C‐L, Cheng Y‐Y, Hung H‐C, Li T‐C, Yen S‐M, et al. The therapeutic effects of acupuncture on patients with chronic neck myofascial pain syndrome: a single‐blind randomized controlled trial. The American Journal of Chinese Medicine 2010;38(5):849‐59. [DOI] [PubMed] [Google Scholar]
- Thomas M, Eriksson SV, Lundeberg T. A comparative study of diazepam and acupuncture in patients with osteoarthritis pain: a placebo controlled study. American Journal of Chinese Medicine 1991;19:95‐100. [DOI] [PubMed] [Google Scholar]
- Tough EA, White AR, Richards SH, Campbell JL. Myofascial trigger point needling for whiplash associated pain ‐ a feasibility study. Manual Therapy 2010;15:529‐35. [DOI] [PubMed] [Google Scholar]
- Tsai C‐T, Hsieh L‐F, Kuan T‐S, Kao MJ, Chou L‐W, Hong C‐Z. Remote effects of dry needling on the irritability of the myofascial trigger point in the upper trapezius muscle. American Journal of Physical Medicine and Rehabilitation 2010;89(2):133‐40. [DOI] [PubMed] [Google Scholar]
- Vas J, Perea‐Milla E, Méndez C, Sánchez Navarro C, León Rubio JM, Brioso M. Efficacy and safety of acupuncture for chronic uncomplicated neck pain: a randomised controlled study. Pain 2006;126(1):245‐55. [CO2007] [DOI] [PubMed] [Google Scholar]
- White PF, Craig WF, Vakharia AS, Ghoname EA, Ahmed HE, Hamza MA. Percutaneous neuromodulation therapy: does the location of electrical stimulation effect the acute analgesic response?. Anesthesia Analgesic 2000;91:949‐54. [DOI] [PubMed] [Google Scholar]
- White P, Lewith G, Prescott P, Conway J. Acupuncture versus placebo for the treatment of chronic mechanical neck pain. Annals of Internal Medicine 2004;141:920‐8. [co2004:] [DOI] [PubMed] [Google Scholar]
- Willich SN, Reinhold T, Selim D, Jena S, Brinkhaus B, Witt CM. Cost‐effectiveness of acupuncture treatment in patients with chronic neck pain. Pain 2006;125:107‐13. [DOI] [PubMed] [Google Scholar]; Witt CM, Brinkhaus B, Reinhold T, Willich SN. Efficacy, effectiveness, safety and costs of acupuncture for chronic pain – results of a large research initiative. Acupuncture in Medicine 2006;24(Suppl):S33‐9. [Google Scholar]; Witt CM, Jena S, Brinkhaus B, Liecker B, Wegscheider K, Willich SN. Acupuncture for patients with chronic neck pain. Pain 2006;125:98‐106. [CO2007] [DOI] [PubMed] [Google Scholar]; Witt CM, Ludtke R, Wegscheider K, Willich SN. Physician characteristics and variation in treatment outcomes: are better qualified and experienced physicians more successful in treating patients with chronic pain with acupuncture?. The Journal of Pain 2010;11(5):431‐5. [DOI] [PubMed] [Google Scholar]; Witt CM, Schutzler L, Ludtke R, Wegscheider K, Willich SN. Patient characteristics and variation in treatment outcomes. Which patients benefit most from acupuncture for chronic pain?. Clinical Journal of Pain 2011;27:550‐5. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
- Bahadir C, Majlesi J, Unalan H. The effect of high‐power pain threshold ultrasound therapy on the electrical activity of trigger points and local twitch response on electromyography: a preliminary study. Journal of Musculoskeletal Pain 2009;17(2):162‐72. [CO2007] [Google Scholar]
- Calvo‐Trujillo S. Effectiveness of the Auto‐acupressure for Diminishing Neck Pain of Benign Origin, 2013. http://ClinicalTrials.gov/show/NCT01855893.
- Ceccherelli F, Tortora P, Nassimbeni C, Casale R, Gagliardi G, Giron G. The therapeutic efficacy of somatic acupuncture is not increased by auriculotherapy: a randomised, blind control study in cervical myofascial pain. Complementary Therapies in Medicine 2006;14:47‐52. [CO2010] [DOI] [PubMed] [Google Scholar]
- Ceccherelli F, Marino E, Caliendo A, Dezzoni R, Roveri A, Gagliardi G. 3, 5, 11 needles: looking for the perfect number of needles ‐ a randomized and controlled study. Acupuncture & Electro‐Therapeutics Research International Journal 2014;39:241‐58. [DOI] [PubMed] [Google Scholar]
- Cho J‐H, Nam D‐H, Kim K‐T, Lee J‐H. Acupuncture with non‐steroidal anti‐inflammatory drugs (NSAIDs) versus acupuncture or NSAIDs alone for the treatment of chronic neck pain: an assessor‐blinded randomised controlled pilot study. Acupuncture Medicine 2014;32:17‐23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chu J. Does EMG (dry needling) reduce myofascial pain symptoms due to cervical nerve root irritation?. Electromyography and Clinical Neurophysiology 1997;37:259‐72. [CO2006] [PubMed] [Google Scholar]
- Coeytaux RR, Kaufman JS, Kaptchuk TJ, Chen W, Miller W, Callahan LF, et al. A randomized, controlled trial of acupuncture for chronic daily headache. Headache 2005;45:1113‐23. [DOI] [PubMed] [Google Scholar]
- Cohen SP. Conservative Therapy Versus Epidual Steroids for Cervical Radiculopathy. clinicaltrials.gov NCT01144923.
- David J, Modi S, ALuko AA, Robertshaw C, Farebrother J. Chronic neck pain: a comparison of acupuncture treatment and physiotherapy. British Journal of Rheumatology 1998;37:1118‐22. [CO97:3489] [DOI] [PubMed] [Google Scholar]
- Dong W, Lin X. Clinical observation on cervical spondylosis of neck type treated with acupuncture at original and terminal points of trapezius. Chinese Acupuncture & Moxibustion 2012;32(3):211‐4. [PubMed] [Google Scholar]
- Edwards J, Knowles N. Superficial dry needling and active stretching in the treatment of myofascial pain ‐ a randomized controlled trial. Acupuncture in Medicine 2003;21(3):80‐6. [CO2010] [DOI] [PubMed] [Google Scholar]
- Emery P, Lythgoe S. The effect of acupuncture on ankylosing spondylitis. British Journal of Rheumatology 1986;25:132‐3. [CO97] [DOI] [PubMed] [Google Scholar]
- Eroglu PK, Yilmaz O, Bodur H, Ates C. A comparison of the efficacy of dry needling, lidocaine injection, and oral flurbiprofen treatments in patients with myofascial pain syndrome: a double‐blind (for injection, groups only), randomized clinical trial. Turkish Journal of Rheumatology 2013;28(1):38‐46. [Google Scholar]
- Falkenberg T. Integrative Medicine for Back and Neck Pain ‐ A Pragmatic Randomized Clinical Pilot Trial. http://ClinicalTrials.gov/show/NCT00565942. [DOI] [PMC free article] [PubMed]
- Fernandez‐Carnero J. Immediate Effects of Dry Needling and TENS in Chronic Neck Pain. http://ClinicalTrials.gov/show/NCT02230709.
- França DL, Senna‐Fernandes V, Cortez CM, Jackson MN, Bernardo‐Filho M, Guimarães MA. Tension neck syndrome treated by acupuncture combined with physiotherapy: a comparative clinical trial (pilot study). Complementary Therapies in Medicine 2008;16:268‐77. [CO2009] [DOI] [PubMed] [Google Scholar]
- Fu WB, Zhang HL, Fan L. Treatment of cervical spondylopathy by needle pricking: a clinical observation of 56 cases [in Chinese]. New Journal of Traditional Chinese Medicine 2005;37(4):65‐6. [CO2009] [Google Scholar]
- Fu ZH, Wang JH, Sun JH, Chen XY, Xu JG. Fu's subcutaneous needling: possible clinical evidence of the subcutaneous connective tissue in acupuncture. The Journal of Alternative and Complementary Medicine 2007;13(1):47‐51. [CO2007] [DOI] [PubMed] [Google Scholar]
- Fu Q. Clinical Study on Electroacupuncture Therapy for Chronic Neck Pain. clinicaltrials.gov NCT01674387.
- Ga H, Koh HJ, Choi JH, Kim CH. Intramuscular and nerve root stimulation vs lidocaine injection to trigger points in myofascial pain syndrome. Journal of Rehabilitation Medicine 2007;39(5):374‐8. [CO2010] [DOI] [PubMed] [Google Scholar]
- Ga H, Choi JH, Park CH, Yoon HJ. Dry needling of trigger points with and without paraspinal needling in myofascial pain syndromes in elderly patients. The Journal of Alternative and Complementary Medicine 2007;13(6):617‐23. [CO2010] [DOI] [PubMed] [Google Scholar]
- Gallacchi G, Mueller W, Plattner GR, Schnorrenberger CC. Acupuncture and laser treatment in cervical and lumbar syndrome [Akupunktur‐ und Laserstrahlbehandlung beim Zervikal‐ und Lumbalsyndrom]. Schweizische Medizinische Wochenschrift 1981;111(37):1360‐6. [CO97] [PubMed] [Google Scholar]
- Gallacchi G, Müller W. Acupuncture ‐ a yielding therapy in rheumatology? [Akupunktur ‐ bringt sie etwas?]. Schweizerische Rundschau fur Medizin Praxis 1983;72:779‐82. [CO2010] [PubMed] [Google Scholar]
- Gallego Sendarrubias G. Dry Needling in Patients with Chronic Neck Pain. clinicaltrials.gov NCT02435966.
- Gaw AC, Chang LW, Shaw L‐C. Efficacy of acupuncture on osteoarthritic pain. New England Journal of Medicine 1975;293:375‐8. [CO97] [DOI] [PubMed] [Google Scholar]
- Gil EN. Acupuncture Approaches for Chronic Pain (AADDOPT‐2). clinicaltrials.gov NCT02456727.
- Giles LG, Müeller R. Chronic spinal pain syndromes: a clinical pilot trial comparing acupuncture, a nonsteroidal anti‐inflammatory drug and spinal manipulation. Journal of Manipulative and Physiological Therapeutics 1999;22(6):376‐81. [CO2002] [DOI] [PubMed] [Google Scholar]
- Giles LG, Muller R. Chronic spinal pain: a randomized clinical trial comparing medication, acupuncture, and spinal manipulation. Spine 2003;28(14):1490‐503. [CO2007] [DOI] [PubMed] [Google Scholar]
- Guangyue W, Fenglin Q. Treatment of 482 cases of cervical spondylopathy by combining point‐injection and needle‐warming via moxibustion. Journal of Traditional Chinese Medicine 2001;21(1):31‐3. [CO2002:2979] [PubMed] [Google Scholar]
- Guo J, Wang C, Congcong Y. Clinical study of acupuncture combined with massage method of Tongdu in treating neck strain. International Journal of Clinical Acupuncture 2013;22(2):66‐8. [Google Scholar]
- Harvey D. Lidocaine Injection Versus Sham Needling in Treating Whiplash Associated Disorder, 2015. http://clinicalTrials.gov/show/NCT02060734.
- Hayek S, Fisher R. Randomized, Comparative‐Effectiveness Study Comparing Epidural Steroid Injections to Conservative Management With Medications and Physical Therapy in Patients With Cervical Radiculopathy, 2014. http://clinicalTrials.gov/show/NCT01144923.
- Hu A, Yang H. Comparison of efficacy between electroacupuncture and the combination of collateral bloodletting, cupping, and acupoint application for cervical spondylosis radiculopathy (CRS). World Journal of Acupuncture ‐ Moxibustion 2014;24(3):25‐9. [Google Scholar]
- Hua Y. Clinical observation on treatment of cervical spondylotic radiculopathy with combined electroacupuncture tuina and traction. Journal of Acupuncture and Tuina Science 2009;7:156‐8. [Google Scholar]
- Huang YF, Wang TF, Liu Y, Zhang SX. Clinical observation on Jiquan (HT 1) for treatment of cervical spondylosis of nerve root type [in Chinese]. Chinese Acupuncture & Moxibustion 2008;28(6):427‐8. [CO2009] [PubMed] [Google Scholar]
- Huang LJ, Luo WJ, Zhang KB, Geng JH. Efficacy observation on cervical spondylosis of vertebral artery type treated with warm needling and rehabilitation physiotherapy therapy. World Journal of Acupuncture ‐ Moxibustion 2012;22(2):12‐6. [Google Scholar]
- Hudson JS, Ryan CG. Multimodal group rehabilitation compared to usual care for patients with chronic neck pain: a pilot study. Manual Therapy 2010;15:552‐6. [DOI] [PubMed] [Google Scholar]
- Jia CS, Shi J, Ma XS, Li XF, Wang Y, Wang JL. Comparison of the analgesic effect of acupuncture between otopoint‐penetrative needling and otopoint‐straight needling for cervical type and nerve‐root type cervicospondylopathy [in Chinese]. Acupuncture Research 2007;32(3):186‐9. [CO2009] [PubMed] [Google Scholar]
- Jin C, Lun X, Jin S, Xia D, Huang Y, Xiao H, et al. A clinical observation on treating stiff neck by the combination of superficial needling at Bo's abdominal acupoints and Luozhen point. International Journal of Clincal Acupuncture 2012;21(3):87‐90. [Google Scholar]
- Johnson R, Prasad K, Wong L, Varley G. Use of acupuncture following whiplash type injuries to the neck. Journal of Bone and Joint Surgery (British) 2000;82‐B(Suppl III):1. [CO2003] [Google Scholar]
- Kai L, Dan WEI, Jia‐kang LI. Acupuncture plus Acupoint‐injection for treatment of cervical spondylosis of vertebroarterial type. Journal of Traditional Chinese Medicine 2008;28(4):243‐4. [DOI] [PubMed] [Google Scholar]
- Kisiel AC, Lind C. Pain relief with physical therapy and manual acupuncture in myofascial neck and shoulder pain [Smartlindring med fysikalisk terapi och manuell akupunktur vid myofaciella nack‐ och skuldersmärtor]. Sjukgymnasten 1996;12:24‐31. [CO97] [Google Scholar]
- Li XH, Li DJ. Therapeutic effect of centro‐square needling Dazhui (GV 14) on cervical spondylosis [in Chinese]. Chinese Acupuncture & Moxibustion 2004;24(7):455‐6. [CO2009] [Google Scholar]
- Li DJ, Wang J, Gao Q, Hou JS. Interventional effects of cervical local‐point traction manipulation plus silver needle heat conductive treatment for cervical spinal canal stenosis [in Chinese]. Chinese Journal of Clinical Rehabilitation 2006;10(43):7‐10. [CO2009] [Google Scholar]
- Li Y, Fu R. Therapeutic effect and blood rheology of patients with cervical spondylosis treated with acupuncture combined with massage. International Journal of Clinical Acupuncture 2013;22(2):61‐3. [Google Scholar]
- Lin MN, Liu XX, Liu JH, Zhang AP, Xu SL, Guo JH. Needle scalpel combined with massage therapy and simple massage therapy for nerve‐root type cervical spondylopathy: a randomized controlled analysis on 100 patients. Chinese Journal of Clinical Rehabilitation 2004;8(23):4920‐1. [CO2010] [Google Scholar]
- Liu MY, Nie RR, Zhou RG, Liao WZ. Observation on therapeutic effect of acupuncture at "cervical three points" combined with cake‐separated moxibustion on cervical hyperosteogeny [in Chinese]. Chinese Acupuncture & Moxibustion 2008;28(12):877‐9. [CO2010] [PubMed] [Google Scholar]
- Liu M, Mu J, Zheng S, Ren C. Efficacy observation on cervical spondylosis of nerve root type treated by the warm needling at Jiajl EX‐B 2 and tapping with plum‐blossom needle. World Journal of Acupuncture ‐ Moxibustion 2014;23(4):6‐10. [Google Scholar]
- Lixing Z. Twenty one cases of vertebral‐artery‐type cervical spondylosis treated with acupuncture and moxibustion. Journal of Traditional Chinese Medicine 2000;20(4):280‐1. [CO2006] [PubMed] [Google Scholar]
- Llamas‐Ramos R, Pecos‐Martin D, Gallego‐Izquierdo T, Llamas‐Ramos I, Plaza‐Manzano G, Ortega‐Santiago R, et al. Comparison of the short‐term outcomes between trigger point dry needling and trigger point manual therapy for the management of chronic mechanical neck pain: a randomized clinical trial. Journal of Orthopaedic & Sports Physical Therapy 2014;44(11):852‐61. [DOI] [PubMed] [Google Scholar]
- Loy T. Treatment of cervical spondylosis: electroacupuncture versus physiotherapy. The Medical Journal of Australia 1983;2:32‐4. [PubMed] [Google Scholar]
- Lü YX, Shan QH. Clinical observation on treatment of cervicogenic headache with turtle‐probing needle at Tianzhu (BL 10) [in Chinese]. Chinese Acupuncture & Moxibustion 2006;26(11):796‐8. [CO2009] [PubMed] [Google Scholar]
- Lundeburg T, Hurtig T, Lundeburg S, Thomas M. Long‐term results of acupuncture in chronic head and neck pain. The Pain Clinic 1988;2(1):15‐31. [CO02;2947] [Google Scholar]
- Lundeburg T, Eriksson SV, Lundeberg S, Thomas M. Effect of acupuncture and naloxone in patients with osteoarthritis pain. A sham acupuncture controlled study. The Pain Clinic 1991;4(3):155‐61. [Google Scholar]
- Luo B, Han J. Cervical spondylosis treated by acupuncture at Ligou (LR 5) combined with movement therapy. Journal of Traditional Chinese Medicine 2010;30(2):113‐7. [DOI] [PubMed] [Google Scholar]
- Ma C, Wu S, Li G, Xiao X, Mai M, Yan T. Comparison of miniscalpel‐needle release, acupuncture needling, and stretching exercise to trigger point in myofascial pain syndrome. The Clinical Journal of Pain 2010;26(3):251‐7. [DOI] [PubMed] [Google Scholar]
- Macpherson H, Tilbrook, HE, Richmond SJ, Atkin K, Ballard K, Bland M, et al. Alexander technique lessons, acupuncture sessions or usual care for patients with chronic neck pain (ATLAS): study protocol for a randomised controlled trial. Trials 2013;14:209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLean SM, Klaber Moffett JA, Sharp DM, Gardiner E. A randomised controlled trial comparing graded exercise treatment and usual physiotherapy for patients with non‐specific neck pain (the GET UP neck pain trial). Manual Therapy 2013;18:199‐205. [DOI] [PubMed] [Google Scholar]
- Muller R, Giles LG. Long‐term follow‐up of a randomized clinical trial assessing the efficacy of medication, acupuncture, and spinal manipulation for chronic mechanical spinal pain syndromes. Journal of Manipulative and Physiological Therapeutics 2005;28(1):3‐11. [CO2009] [DOI] [PubMed] [Google Scholar]
- Myburgh C, Hartvigsen J, Aagaard P, Holsgaard‐Larsen A. Skeletal muscle contractility, self‐reported pain and tissue sensitivity in females with neck/shoulder pain and upper trapezius myofascial trigger points– a randomized intervention study. Chiropractic & Manual Therapies 2012;20:36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakajima M, Inoue M, Itoi M, Kitakoji H. Difference in clinical effect between deep and superficial acupuncture needle insertion for neck‐shoulder pain: a randomized controlled clinical trial pilot study. Journal of the Japanese Society of Balneology, Climatology and Physical Medicine 2015;78(3):216‐27. [Google Scholar]
- Pan C, Tan G. Forty‐two cases of greater occipital neuralgia treated by acupuncture plus acupoint‐injection. Journal of Traditional Chinese Medicine 2008;28(3):175‐7. [DOI] [PubMed] [Google Scholar]
- Pecos‐Martın D, Montanez‐Aguilera F, Gallego‐Izquierdo T, Urraca‐Gesto A, Gomez‐Conesa A, Romero‐Franco N, et al. Effectiveness of dry needling on the lower trapezius in patients with mechanical neck pain: a randomized controlled trial. Archives of Physical Medicine and Rehabilitation 2015;96:775‐81. [DOI] [PubMed] [Google Scholar]
- Peng A, Behar S, Shyh‐Jong Y. Long‐term therapeutic effects of electro‐acupuncture for chronic neck and shoulder pain ‐ a double blind study. Acupuncture & Electrotherapeutics Research 1987;12(1):37‐44. [CO2010] [DOI] [PubMed] [Google Scholar]
- Rayegani SM, Bayat M, Hasan Bahrami M, Raeissadat SA, Kargozar E. Comparison of dry needling and physiotherapy in treatment of myofascial pain syndrome. Clinical Rheumatology 2014;33:859‐64. [DOI] [PubMed] [Google Scholar]
- Salter GC, Roman M, Bland MJ, MacPherson H. Acupuncture for chronic neck pain: a pilot for a randomised controlled trial. BMC Musculoskeletal Disorders 2006;7:99. [CO2010] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sato K, Oliveira A, Lima A. Effectiveness of dry needling reduction myofascial trigger point pain in the trapezius muscle. The Journal of Pain 2014;S1:S117. [Google Scholar]
- Sator‐Katzenschlager SM, Szeles JC, Scharbert G, Michalek‐Sauberer A, Kober A, Heinze G, et al. Electrical stimulation of auricular acupuncture points is more effective than conventional manual auricular acupuncture in chronic cervical pain: a pilot study. Anesthesia & Analgesia 2003;97:1469‐73. [CO2010] [DOI] [PubMed] [Google Scholar]
- Seo B‐K, Lee J‐H, Kim P‐K, Baek Y‐H, Jo D‐J, Lee S. Bee venom acupuncture, NSAIDs or combined treatment for chronic neck pain: study protocol for a randomized, assessor‐blind trial. Trials 2014;15:132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shang XK, Meng XW, Dong HY, Liu GW. Clinical observations on the treatment of nerve‐root cervical spondylopathy by the combination of adjacent and remote acupoints [in Chinese]. Shanghai Journal of Acupuncture and Moxibustion 2002;21(6):12‐3. [CO2009] [Google Scholar]
- Shuangquan Y. The therapeutic effects of triple puncture and routine body needling for cervical spondylosis. Journal of Traditional Chinese Medicine 2003;23(4):282‐3. [PubMed] [Google Scholar]
- Söderlund A, Lindberg P. Cognitive behavioural components in physiotherapy management of chronic whiplash associated disorders (WAD) ‐ a randomised group study. Physiotherapy Theory and Practice 2001;17:229‐38. [CO2003] [PubMed] [Google Scholar]
- Sun Z, Yue J, Zhang Q. Electroacupuncture at Jing‐jiaji points for neck pain caused by cervical spondylosis: a study protocol for a randomized controlled pilot trial. Trials 2013;14:360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takakura N, Takayama M, Kawase T, Kaptchuk T, Kong J, Yajima H. Design of a randomised acupuncture trial on functional neck/shoulder stiffness with two placebo controls. BMC Complementary and Alternative Medicine 2014;14:246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teng C. Effect of acupuncture and physical therapy. Archive of Physical Medicine and Rehabilitation 1973;53:601. [CO97] [Google Scholar]
- Tobbackx Y, Meeus M, Wauters L, DeVilder P, Roose J, Verhaeghe T, et al. Does acupuncture activate endogenous analgesia in chronic whiplash‐associated disorders? A randomized crossover trial. European Journal of Pain 2013;17:279‐89. [DOI] [PubMed] [Google Scholar]
- Venâncio Rde A, Alencar FG, Zamperini C. Different substances and dry‐needling injections in patients with myofascial pain and headaches. The Journal of Craniomandibular Practice 2008;26(2):96‐103. [CO2010] [DOI] [PubMed] [Google Scholar]
- Venancio Rde A, Alencar FG, Zamperini C. Botulinum toxin, lidocaine, and dry‐needling injections in patients with myofascial pain and headaches. The Journal of Craniomandibular Practice 2009;27(1):46‐53. [CO2010] [DOI] [PubMed] [Google Scholar]
- Wan B, Huang W, Zhang Y, Zhang H. Influence of electroacupuncture with penetration needling method on comprehensive pain in patients with cervical spondylotic radiculopathy. Chinese Acupuncture & Moxibustion 2013;33(5):407‐10. [PubMed] [Google Scholar]
- Wang XL, Huang HY. Observation on therapeutic effect of long‐time needle retention at Baihui (GV 20) on vertebroarterial cervical spondylopathy [Article in Chinese]. Chinese Acupuncture & Moxibustion 2007;27(6):415‐6. [CO2010] [PubMed] [Google Scholar]
- Wang XL. Observation on therapeutic effect of Shu‐needling therapy as main on cervical spondylosis of nerve root type [in Chinese]. Chinese Acupuncture & Moxibustion 2008;28(7):497‐8. [CO2009] [PubMed] [Google Scholar]
- Wang G, Gao Q, Hou J, Li J. Effects of temperature on chronic trapezius myofascial pain syndrome during dry needling therapy. Evidence‐Based Complementary and Alternative Medicine 2014;638268:1‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu S, Liang Z, Fu W. Chronic neck pain of cervical spondylosis treated with acupuncture and moxibustion in terms of the heart and kidney theory: a randomized controlled trial. Chinese Acupuncture & Moxibustion 2012;32(9):769‐75. [PubMed] [Google Scholar]
- Xue B, Fan L, Hu L. Clinical observation on cervical spondylopathy vertebroarterial type treated by electro‐acupuncture. Journal of Traditional Chinese Medicine 2007;27(1):39‐42. [CO2010] [PubMed] [Google Scholar]
- Yang T, Sun F, Zhou YL. Clinical observation on acupoint sticking therapy for treatment of chronic pain of cervical intervertebral disc [in Chinese]. Chinese Acupuncture & Moxibustion 2009;29(3):197‐9. [CO2010] [PubMed] [Google Scholar]
- Yang J, Zhang J, Yu J, Han J. Treatment of cervical spondylosis by spinal balancing combined with intervention of pathway of qi: a randomized controlled study. Chinese Acpuncture & Moxibustion 2013;33(7):582‐6. [PubMed] [Google Scholar]
- Yoon S‐H, Rah UW, Sheen SS, Cho KH. Comparison of 3 needle sizes for trigger point injection in myofascial pain syndrome of upper and middle trapezius muscle: a Rrandomized controlled trial. Archives of Physical Medicine and Rehabilitation 2009;90:1332‐9. [DOI] [PubMed] [Google Scholar]
- Yoshimizu M, Teo AR, Masahiko A, Kiyohara K, Kawamur T. Relief of chronic shoulder and neck pain by electro‐acupuncture and transcutaneous electrical nervous stimulation: a randomized crossover trial. Medical Acupuncture 2012;24(2):97‐103. [Google Scholar]
- Yu SQ. The therapeutic effects of triple puncture and routine body needling for cervical spondylosis. Journal of Traditional Chinese Medicine 2003;23(4):282‐3. [CO2006] [PubMed] [Google Scholar]
- Zeng L. Treatment of cervical spondylopathy by point‐through‐point acupuncture [in Chinese]. Shanghai Journal of Acupuncture and Moxibustion 2005;24(7):9‐10. [CO2009] [Google Scholar]
- Zhang H. A study of cervical spondylosis treated with the chrysanthemum pillow with median hole and electroacupuncture. Journal of Chinese Medicine 1996;51:18‐20. [CO1997] [Google Scholar]
- Zhang HL, Jin R. A randomized controlled trial of electroacupuncture and traction for treatment of nerve‐root type cervical spondylosis [in Chinese]. Chinese Acupuncture & Moxibustion 2003;23(11):637‐9. [CO2010] [Google Scholar]
- Zhang J. Electroacupuncture and Laser Therapy on Neck Pain. https://clinicaltrials.gov/ct2/show/NCT00618878 NCT00618878.
- Zhang J. Ashi point massage combined with warming needle acupuncture in treating 40 cases of cervicogenic headache. International Journal of Clinical Acupuncture 2013;22(3):117‐9. [Google Scholar]
- Zhange X‐Z, Wang L‐L, Liu Y‐Q. Clinical observation on cervical headache treated with acupuncture and fire needling technique. Chinese Acupuncture & Moxibustion 2013;33(11):989‐92. [PubMed] [Google Scholar]
- Zhao ZY, Cai DJ, Liang FR. Observation on therapeutic effect of Shencongding moxibustion on cervical headache [in Chinese]. Chinese Acupuncture & Moxibustion 2004;24(6):389‐91. [CO2009] [Google Scholar]
- Zheng Y, Shi D, Wu X, Gu M, Ai Z, Tang K, et al. Ultrasound‐guided miniscalpel‐needle release versus dry needling for chronic neck pain: a randomized controlled trial. Evidence‐Based Complementary and Alternative Medicine 2014;235817:1‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhi L, Feng C, Tu C. Controlled randomized trial on therapeutic effects of acupotomy‐injection combined with Feng's spinal manipulation (FSM) for treating cervical spondylotic radiculopathy. China Journal of Orthopaedics and Traumatology 2008;21(6):421‐4. [CO2009] [PubMed] [Google Scholar]
- Zhou J, Li X, Zhao J, Wang L‐S, Wang L, Yang Y. Treatment of 30 patients with cervical spondylotic radiculopathy by acupuncture plus warming‐needle moxibustion: a randomized controlled trial. World Journal of Acupuncture ‐ Moxibustion 2014;24(4):24‐8. [Google Scholar]
- Zhu XM, Polus B. A controlled trial on acupuncture for chronic neck pain. American Journal of Chinese Medicine 2002;30(1):13‐28. [DOI] [PubMed] [Google Scholar]
- Zhu HZ, Quan WC, Zhang XF, Qiao JL, Liu ZJ, Fu P, et al. Evaluation on clinical therapeutic effect of needle‐knife therapy on cervical spondylosis. Chinese Acupuncture & Moxibustion 2006;26(5):316‐8. [CO2009] [PubMed] [Google Scholar]
- Zhuang LX, Zhu FP. Effect of pressed acupuncture at baihui acupoint on thromboxane A2 and prostacyclin in treating vertebral artery type of cervical spondylosis. Chinese Journal of Clinical Rehabilitation 2004;8(30):6672‐3. [CO2009] [Google Scholar]
- Ziaeifar M, Arab AM, Karimi N, Nourbakhsh MR. The effect of dry needling on pain, pressure pain threshold and disability in patients with a myofascial trigger point in the upper trapezius muscle. Journal of Bodywork & Movement Therapies 2014;18:298‐305. [DOI] [PubMed] [Google Scholar]
References to studies awaiting assessment
- Amos Z, Yoav M, Guy A, Adi F, Yigal M, Shmuel BH. A randomised controlled trial of an integrative approach utilising acupuncture for back and neck pain in an emergency department setting. European Journal of Integrative Medicine 2012;4S:23‐4. [Google Scholar]
- Bar‐Haim S. Acupuncture for Back and Neck Pain in an Emergency Room Setting. clinicaltrials.gov NCT00859365.
- Cerezo‐Tellez E. Dry Needling of the Trapezius Muscle in Office Workers With Neck Pain. Randomised, Single Blinded Clinical Trial, 2014. http://ClinicalTrials.gov/show/NCT02219386. [DOI] [PMC free article] [PubMed]
- Choi DY. Acupuncture for Whiplash Associated Disorder. http://ClinicalTrials.gov/show/NCT01395511.
- Guo Y. Efficacy of Abdominal Acupuncture for Neck Pain: A Randomized Controlled Trial. http://apps.who.int/trialsearch/AdvSearch.aspx ChiCTR‐TRC‐14004932. [DOI] [PMC free article] [PubMed]
- Liguori S, Liguori A, Petti F. Abdominal acupuncture and cervicobrachialgia: is it a real possibility for setting a double‐blind trial in acupuncture research?. European Journal of Integrative Medicine 2012;4S:31. [Google Scholar]
- Mejuto‐Vázquez MJ, Salom‐Marino J, Ortega‐Santiago R, Truyols‐Domínguez S, Fernández‐de‐las‐Peñas C. Short‐term changes in neck pain, widespread pressure pain sensitivity, and cervical range of motion after the application of trigger point dry needling in patients with acute mechanical neck pain: a randomized clinical trial. Journal of Orthopaedic & Sports Physical Therapy 2014;44(4):252‐60. [DOI] [PubMed] [Google Scholar]
- Simma‐Kletschka I, Gleditsch J, Simma L, Piehslinger E. Microsystems acupuncture in craniomandibular pain syndromes – a randomised controlled trial. Deutsche Zeitschrift fur Akupunktur 2009;52:7‐11. [Google Scholar]
- Sterling M, Valentin S, Vincenzino B, Souvlis T, Connelly LB. Dry needling and exercise for chronic whiplash ‐ a randomised controlled trial. BMC Musculoskeletal Disorders 2009;10:160. [DOI] [PMC free article] [PubMed] [Google Scholar]; Sterling M, Vincenzino B, Souvlis T, Connelly LB. Dry‐needling and exercise for chronic whiplash‐associated disorders: a randomized single‐blind placebo‐controlled trial. Pain 2015;156(4):635‐43. [DOI] [PubMed] [Google Scholar]
- Wilke J, Vogt L, Niederera D, Hübscher M, Rothmayra J, Ivkovic D, et al. Short‐term effects of acupuncture and stretching on myofascial trigger point pain of the neck: a blinded, placebo‐controlled RCT. Complementary Therapies in Medicine 2014;22:835‐41. [DOI] [PubMed] [Google Scholar]
- Zhang SP. Electrotherapy for Chronic Neck Pain. clinicaltrials.gov NCT00826215. ; Zhang SP, Chiu TTW, Chiu A. Long‐term efficacy of electroacupuncture for chronic neck pain: a randomised controlled trial. Hong Kong Medical Journal 2013;19(Suppl 9):S36‐9. [PubMed] [Google Scholar]
References to ongoing studies
- Calamita S, Biasotto‐Gonzalez D, Melo N, Meira dos Santos D, Lassa R, Mendonça F, et al. Evaluation of the immediate effect of acupuncture on pain, cervical range of motion and electromyographic activity of the upper trapezius muscle in patients with nonspecific neck pain: study protocol for a randomized controlled trial. Trials 2015;16:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim K‐H, Ryu‐J‐H, Park MR, Kim YI, Min MK, Park YM, et al. Acupuncture as analgesia for non‐emergent acute non‐specific neck pain, ankle sprain and primary headache in an emergency department setting: a protocol for a parallel group, randomised, controlled pilot trial. BMJ Open 2014;4:1‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang Z‐H, Di Z, Jiang S, Xu S‐J, Zhu X‐P, Fu W‐B. The optimized acupuncture treatment for neck pain caused by cervical spondylosis: a study protocol of a multi‐centre randomized controlled trial. Trials 2012;13:107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Que Q, Ye X, Su Q, Weng Y, Chu J, Mei L, et al. Effectiveness of acupuncture intervention for neck pain caused by cervical spondylosis: study protocol for a randomized controlled trial. Trials 2013;14:186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun Z, Yue J, Tian H, Zhang Q. Acupuncture at Houxi (SI 3) acupoint for acute neck pain caused by stiff neck: study protocol for a pilot randomised controlled trial. BMJ Open 2014;4:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Additional references
- Boutron I, Moher D, Tugwell P, Giraudeau B, Poiraudeau S, Nizard R, et al. A checklist to evaluate a report of a non pharmacological trial (CLEAR NPT) was developed using consensus. Journal of Clinical Epidemiology 2005;58:1233‐40. [DOI] [PubMed] [Google Scholar]
- Carroll LJ, Hogg‐Johnson S, Velde G, Haldeman S, Holm LW, Carragee EJ, et al. Course and prognostic factors for neck pain in the general population ‐ results of the bone and joint decade 2000‐2010 task force on neck pain and its associated disorders. Spine 2008;33(4S): S75‐82. [DOI] [PubMed] [Google Scholar]
- Chen LI, Zhang J, Li F, Qiu Y, Wang L, Li YH, et al. Endogenous anandamide and cannabinoid receptor‐2 contribute to electroacupuncture analgesia in rats. Journal of Pain 2009;10(7):732‐9. [DOI] [PubMed] [Google Scholar]
- Cicchetti DV. Assessing inter‐rater reliability for rating scales: resolving some basic issues. British Journal of Psychiatry 1976;129:452‐6. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical Power Analysis for the Behavioural Sciences. 2nd Edition. Hilldale, NJ: Lawrence Erlbaum Associates, 1988:Lawance Erlbaum. [Google Scholar]
- Cote P, Cassidy J, Carroll L, Kristman V. The annual incidence and course of neck pain in the general population: a population‐based cohort study. Pain 2004;112(3):267‐73. [DOI] [PubMed] [Google Scholar]
- Ezzo J, Berman B, Hadhazy VA, Jadad AR, Lao L, Singh BB. Is acupuncture effective for the treatment of chronic pain? A systematic review. Pain 2000;86:217‐25. [DOI] [PubMed] [Google Scholar]
- Fu L‐M, Li J‐T, Wu W‐S. Randomized controlled trials of acupuncture for neck pain: systematic review and meta‐analysis. Journal of Alternative and Complementary Medicine 2009;15(2):133‐45. [DOI] [PubMed] [Google Scholar]
- Furlan AD, Tulder MW, Cherkin DC, Tsukayama H, Lao L, Koes BW, et al. Acupuncture and dry needling for low back pain: an updated systematic review within the framework of The Cochrane Collaboration. Spine 2005;30:944‐63. [DOI] [PubMed] [Google Scholar]
- Furlan A, Pennick V, Bombardier C, Tulder M. Updated method guidelines for systematic reviews in The Cochrane Collaboration Back Review Group. Spine 2009;34(18):1929‐41. [DOI] [PubMed] [Google Scholar]
- Furlan AD, Yazdi F, Tsertsvadze A, Gross A, Tulder M, Santaguida L, et al. A systematic review and meta‐analysis of efficacy, cost‐effectiveness, and safety of selected complementary and alternative medicine for neck and low‐back pain. Evidence‐Based Complementary and Alternative Medicine 2012;2012:1‐61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldman N, Chen M, Fujita T, Xu Q, Peng W, Liu W, et al. Adenosine A1 receptors mediate local anti‐nociceptive effects of acupuncture. Nature Neuroscience 2010;13(7):883‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graham N, Haines T, Goldsmith CH, Gross A, Burnie S, Shahzad U, et al. Reliability of 3 assessment tools used to evaluate randomized controlled trials for treatment of neck pain. Spine 2012;37(6):515‐22. [DOI] [PubMed] [Google Scholar]
- Graham N, Gross AR, Carlesso LC, Santaguida PL, MacDermid JC, Walton D, et al. An ICON overview on physical modalities for neck pain and associated disorders. Open Orthopaedics Journal 2013;7(Suppl 4 M6):440‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross AR, Goldsmith C, Hoving JL, Haines T, Peloso P, Aker P, et al. Conservative management of mechanical neck disorders: a systematic review. The Journal of Rheumatology 2007;34(3):1083‐102. [PubMed] [Google Scholar]
- Haldeman S, Carroll LJ, Cassidy JD. The empowerment of people with neck pain: Introduction ‐ The bone and joint decade 2000‐2010 task force on neck pain and its associated disorders. Spine 2008;33(4S):S8‐13. [DOI] [PubMed] [Google Scholar]
- Han JS. Acupuncture and endorphins. Neuroscience Letters 2004;361(1‐3):258‐61. [DOI] [PubMed] [Google Scholar]
- Haraldsson B, Gross A, Myers CD, Ezzo J, Morien A, Goldsmith CH, et al. Massage for mechanical neck disorders. Cochrane Database of Systematic Reviews 2006;3(CD004871):1. [DOI] [PubMed] [Google Scholar]
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. www.cochrane‐handbook.org 2011;5.1.0:1. [Google Scholar]
- Hogg‐Johnson S, Velde G, Carroll LJ, Holm LW, Cassidy JD, Guzman J, et al. The burden and determinants of neck pain in the general population ‐ results of the bone and joint decade 2000‐2010 task force on neck pain and its associated disorders. Spine 2008;33(4S):S39‐51. [DOI] [PubMed] [Google Scholar]
- Huang W, Pach D, Napadow V, Park K, Long X, Neumann J, et al. Characterizing acupuncture stimuli using brain imaging with FMRI ‐ a systematic review and meta‐analysis of the literature. PLoS One 2012;7(4):e32960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Irnich D, Salih N, Offenbächer M, Fleckenstein J. Is sham laser a valid control for acupuncture trials?. Journal of Evidence‐Based Complementary & Alternative Medicine 2011;2011(485945):8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jadad AR, Moore RA, Corroll D, Jenkinson C, Reynolds DJ, Gavagha DJ, et al. Assessing the quality of reports of randomized controlled trials: is blinding necessary?. Controlled Clinical Trials 1996;17(1):1‐12. [DOI] [PubMed] [Google Scholar]
- Langevin HM, Bouffard NA, Badger GJ, Churchill DL, Howe AK. Subcutaneous tissue fibroblast cytoskeletal remodeling induced by acupuncture: evidence for a mechanotransduction‐based mechanism. Journal of Cell Physiology 2006;207:767‐74. [DOI] [PubMed] [Google Scholar]
- Linde K, Witt CM, Streng A, Weidenhammer W, Wagenpfeil S, Brinkhaus B, et al. The impact of patient expectations on outcomes in four randomized controlled trials of acupuncture in patients with chronic pain. Pain 2007;128(3):264‐71. [DOI] [PubMed] [Google Scholar]
- Linde K, Allais G, Brinkhaus B, Manheimer E, Vicker A, White A. Acupuncture for migraine prophylaxis. Cochrane Database of Systematic Reviews 2009;1(1):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linde K, Allais G, Brinkhaus B, Manheimer E, Vicker A, White A. Acupuncture for tension‐type headache. Cochrane Database of Systematic Reviews 2009;1(1):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller J, Gross A, D'Sylva J, Burnie SJ, Goldsmith CH, Graham N, et al. Manual therapy and exercise for neck pain: a systematic review. Manual Therapy 2010;15:334‐54. [PubMed] [Google Scholar]
- Olesen J. Classification and diagnostic criteria for headache disorders, cranial neuralgias and facial pain. Cephalalgia 1988;8(7):61‐2. [PubMed] [Google Scholar]
- Olesen J, Gobel H. ICD‐10 Guide for Headaches. Guide to the classification, diagnosis and assessment of headaches in accordance with the Tenth Revision of the International Classification of Diseases and Related Health Problems and Its Application to Neurology. Cephalagia 1997;17(Suppl 19):29‐30. [Google Scholar]
- Schumacher HR, Klippel JH, Koopman WJ (eds). Primer on the Rheumatic Diseases. 10th Edition. Atlanta: Arthritis Foundation, 1993. [Google Scholar]
- Sjaastad O, Fredriksen TA, Pfaffenrath V. Cervicogenic headache: diagnostic criteria. Headache 1990;30:725‐6. [DOI] [PubMed] [Google Scholar]
- Spitzer WO, Leblanc FE, Dupuis M. Scientific approach to the assessment and management of activity related spinal disorders. Spine 1987;Suppl 7:S1‐59. [PubMed] [Google Scholar]
- Spitzer WO, Skovron ML, Salmi LR, Cassidy JD, Duranceau J, Suissa S, et al. Scientific monograph of the Quebec Task Force on Whiplash‐Associated Disorders: redefining "whiplash" and its management. Spine 1995;Suppl:1S‐73S. [PubMed] [Google Scholar]
- Tang NM, Dong HW, Wang XM, Tsui ZC, Han JS. Cholecystokinin antisense RNA increases the analgesic effect induced by electroacupuncture or low dose morphine: conversion of low responder rats into high responders. Pain 1997;71(1):71‐80. [DOI] [PubMed] [Google Scholar]
- Trinh KV, Phillips S, Ho E, Damsma K. Acupuncture in alleviation of lateral epicondyle pain. Rheumatology 2004;43:1085‐90. [DOI] [PubMed] [Google Scholar]
- Trinh KV, Graham N, Gross AR, Goldsmith CH, Wang E, Cameron ID, et al. Acupuncture for neck disorders. Cochrane Database of Systematic Reviews 2006;3(CD004870):1. [DOI] [PubMed] [Google Scholar]
- Tulder M, Furlan A, Bombardier C, Bouter L, Editorial Board of the Cochrane Collaboration Back Review Group. Updated method guidelines for systematic reviews in The Cochrane Collaboration Back Review Group. Spine 2003;28(12):1290‐9. [DOI] [PubMed] [Google Scholar]
- Vernon H, Schneider M. Chiropractic management of myofascial trigger points and myofascial pain syndrome: a systematic review of the literature. Journal of Manipulative and Physiological Therapeutics 2009;32(1):14‐24. [DOI] [PubMed] [Google Scholar]
- Vickers AJ. Statistical re‐analysis of four recent randomized trials of acupuncture for pain using analysis of covariance. Clinical Journal of Pain 2004;20(5):319‐23. [DOI] [PubMed] [Google Scholar]
- Zhang Y, Zhang RX, Zhang M, Shen XY, Xin J, Ren K, et al. Electroacupuncture inhibition of hyperalgesia in an inflammatory pain rat model: involvement of distinct spinal serotonin and norepinephrine receptor subtypes. British Journal of Anaesthesia 2012;109(2):245‐52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao ZQ. Neural mechanism underlying acupuncture analgesia. Progress in Neurobiology 2008;85(4):355‐75. [DOI] [PubMed] [Google Scholar]


